Abstract
Background:
Various exercises have been proposed to mitigate chronic low back pain (LBP). However, to date, no one particular exercise has been shown to be superior. Hence, the aim of this study was to compare the efficiency between 2 exercises: the individualized graded lumbar stabilization exercise (IGLSE) and walking exercise (WE).
Methods:
A randomized controlled trial was conducted in 48 participants with chronic LBP. After screening, participants were randomized to 1 of 4 groups: flexibility exercise, WE, stabilization exercise (SE), and stabilization with WE (SWE) groups. Participants underwent each exercise for 6 weeks. The primary outcome was visual analog scale (VAS) of LBP during rest and physical activity. Secondary outcomes were as follows: VAS of radiating pain measured during rest and physical activity; frequency of medication use (number of times/day); Oswestry disability index; Beck depression inventory; endurances of specific posture; and strength of lumbar extensor muscles.
Results:
LBP during physical activity was significantly decreased in all 4 groups. Exercise frequency was significantly increased in the SE and WE groups; exercise time was significantly increased in the SE group. The endurance of supine, side lying, and prone posture were significantly improved in the WE and SWE groups.
Conclusions:
Lumbar SE and WE can be recommended for patients with chronic LBP because they not only relieve back pain but also prevent chronic back pain through improving muscle endurance.
Keywords: low back pain, lumbar stabilization exercise, walking
1. Introduction
Low back pain (LBP) is one of the most common musculoskeletal disorders, with a prevalence rate of 80%.[1] In some patients, the initial acute pain may continue during a 3-month period and eventually develop into chronic LBP. Chronic LBP is associated with histomorphologic and structural changes in the paraspinalis muscles. These back muscles are smaller, contain fat, and show a degree of atrophic changes in select muscle fibers.[2] Therefore, the lumbar paraspinalis muscles are weak with excessive fatigability.[3,4] Furthermore, poor coordination of the paraspinalis muscles has been associated with chronic LBP.[5] These contribute to a vicious cycle of LBP and deconditioning syndrome.
Exercise can improve back extension strength, mobility, endurance, and functional disability.[6,7] Various exercises, such as lumbar stabilization exercise (SE), motor control exercise, core exercise, lumbar flexion exercise, walking exercise (WE), and bracing exercise, have been proposed to mitigate chronic LBP. These exercises focus on lumbar stabilization and core strengthening.[8] However, to date, no one particular exercise has been shown to be superior.[9–11]
Lumbar SE is primarily aimed at improving neuromuscular control, strength, and endurance of the muscles, which are considered to be central to the maintenance of dynamic spinal and trunk stability. It is considered as a safe exercise with the advantages of having multiple stages, as well as cost-effectiveness.[12,13] Each individual has different lumbar muscular strengths, and therefore, lumbar SE programs should be individualized, comprising of various postures with varying intensities to maximize therapeutic benefit to a particular individual.[13] To improve compliance, the intensity level of each exercise can be modified according to each patient's capacity, with changes in the postures of the upper and lower extremities or neck as well as changes in the duration of exercise time.[13] Therefore, individualized graded lumbar SE (IGLSE) will allow for a customized exercise program that caters to the needs of a specific patient. IGLSE is not only safe, as it has the ability to strengthen the lumbar musculature without flexion or extension, but it also has the potential to offer high compliance owing to the graded protocol with modifiable intensity.
Moreover, walking is highly recommended to rehabilitate patients with LBP. It is relatively easy to comply with and is highly cost-effective.[14] It leads to enhanced isometric endurance by increasing muscular endurance and has the potential to eventually prevent LBP.[15]
The aim of this study was to investigate the efficiency of IGLSE and WE. We hypothesize that these 2 exercises are highly effective in alleviating LBP and increasing compliance because of their customizability.
2. Materials and method
This study was a prospective randomized controlled clinical trial with 4 groups: flexibility exercise (FE) group, WE group, SE group, and stabilization with WE (SWE) group. Subjects in this study were part of a clinical trial (NCT02938169). The study and all procedures were approved by the Institutional Review Board of Seoul National University Bundang Hospital (B-1604-344-004).
2.1. Subjects
This study was conducted between May of 2016 and April of 2017. Patients complaining of chronic LBP were recruited from the rehabilitation outpatient clinic. The inclusion criteria were subjects older than 20 years with intermittent chronic LBP of >3 months. The exclusion criteria were as follows: a pain intensity of below VAS 40 during physical activity, neurologic motor weakness, deformity (scoliosis with cobb's angle exceeding 10 degrees), history of recent lumbar or abdominal surgery, systemic inflammatory disease or psychiatric disease, severe knee or hip arthritis that may interfere with WE, pregnancy, and previous exercise treatment for lumbar paraspinalis muscles within 3 months. The physical examination was done by a physical medicine and rehabilitation specialist.
2.2. Sample Size Calculation
One way analysis of variance (ANOVA) power analysis was performed with the help of a statistical team to compare the average values of the four groups. As a result, the power of 82% was obtained when 10 patients were allocated to each group. As a result, 15 patients were assigned to each group to account for a dropout rate of 30%.
2.3. Randomization
Consenting participants were randomly allocated to 1 of 4 study groups, following the predetermined and computer-generated random allocation sequences that were prepared by a statistician not involved in participant recruitment. The randomization schedule was only accessible by 2 individuals: the statistician and the primary investigators.
2.4. Blinding
It was not possible to blind participants and physiotherapists given the nature of the exercise therapy and evaluation. One researcher blinded to group allocation measured the outcomes at pre-, immediately post-, and 6 weeks post-exercise program. Statisticians and primary investigators were unaware of the group allocation until data analyses were complete.
2.5. Exercise protocol
Participants underwent each exercise for 30∼60 minutes, 5 times a week, for a total duration of 6 weeks. All participants were educated on the correct posture and abdominal bracing method, and received a pamphlet explaining good postures and abdominal bracing method for preventing LBP. Light abdominal bracing exercise (10%–20% of maximal bracing) was recommended for all times; maximal bracing was recommended for 5 to 7 seconds, intermittently.
The education session was performed at the clinic by a trained physical therapist at the first visit. Moreover, a printed pamphlet with instructions on how to perform the exercises was given to each patient. The exercises were performed at home All participants underwent a telephone interview every 2 weeks to confirm the current pain status, degree of exercise compliance, and to adjust the exercise level. Telephone communication also acted as an encouragement to exercise, promoting compliance.
The FE group received stretching exercise for the abdominal muscle, quadriceps, hamstring, tensor fascia lata, piriformis muscle, and quadratus lumborum muscles for 30 minutes (Fig. 1 A). The WE group performed fast walking on flat ground with abdominal bracing for 30 minutes. The SE group was educated on IGLSE, focusing on the modifiable intensity level based on the exercise capacities of each participant. The IGLSE protocol consisted of 2 parts: stretching exercises and SEs (Fig. 1 B). All participants performed stretching exercises for 5 minutes as a warm-up before beginning the SEs for 25 minutes. This program ranged from easy to difficult, based on participants’ exercise capacity. Each exercise level had 7 basic positions: supine, dead bug, side lying, prone, bird dog, bridge, and plank (5 levels, Fig. 1 B). We gradually increased the degree of instability until the most unstable posture was achieved. At the beginning, participants were placed into a level with moderate difficulty. To challenge the stabilization of all trunk muscles (anterior, lateral, and posterior), including the transverse abdominis, rectus abdominis, erector spinae and multifidus, internal oblique abdominals, and quadrates lumborum, participants were instructed to complete all 5 exercise positions in each session. Patients repeated each of the 7 postures 5times for about 30 seconds each, to the best of their ability, for a total of 25 minutes.[12,13] The SWE group performed IGES for 30 minutes and walking for an additional 30 minutes.
Figure 1.
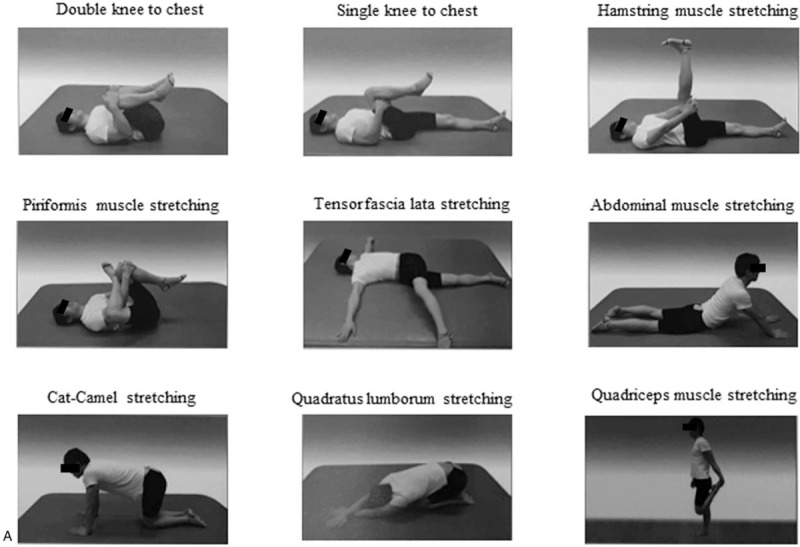
These figures show the exercise protocol for flexibility and lumbar stabilization exercises. Flexibility exercise consisted of stretching in the abdominal muscle, quadriceps, hamstring, tensor fascia lata, piriformis, and quadratus lumborum muscles (A). The stabilization exercise group was educated with individualized graded lumbar stabilization exercise (IGLSE). The IGLSE protocol consisted of 2 parts: the stretching exercises and stabilization exercises (B). After the stretching exercises of 5 minutes, patients were instructed to complete the stabilization exercises for 25 minutes. Each level had 7 basic positions: supine, dead bug, side-lying, prone, bird dog, bridge, and plank positions (5 levels). At the beginning, patients were placed into an exercise level with moderate difficulty, with gradual increase in difficulty with increased patient capacity. Squared figures show a specific posture used to measure the muscular endurance for the secondary outcome. Endurance was measured on 3 postures (supine, side-lying, and prone), respectively.
2.6. Outcome measurement
The primary outcome was the changes of VAS of LBP from the baseline to the follow-up. VAS was measured during rest and physical activity. The secondary outcomes included VAS of radiating pain measured during rest and physical activity, frequency of medication use (number of taking medications / day), endurances of specific posture (Fig. 2, squared posture), and strength of lumbar extensor muscles. Endurance was measured in 3 postures (supine, side-lying, and prone).[12] The strength of lumbar extensor was measured with the manual muscle tester (FEI 12-0380 Lafayette Manual Muscle Tester, Fabrication Enterprises Inc.) in sitting position. In addition, Oswestry Disability Index and Beck depression inventory were measured to identify kinesiophobia, psychosocial aspects, and the disability for LBP.
Figure 1 (Continued).
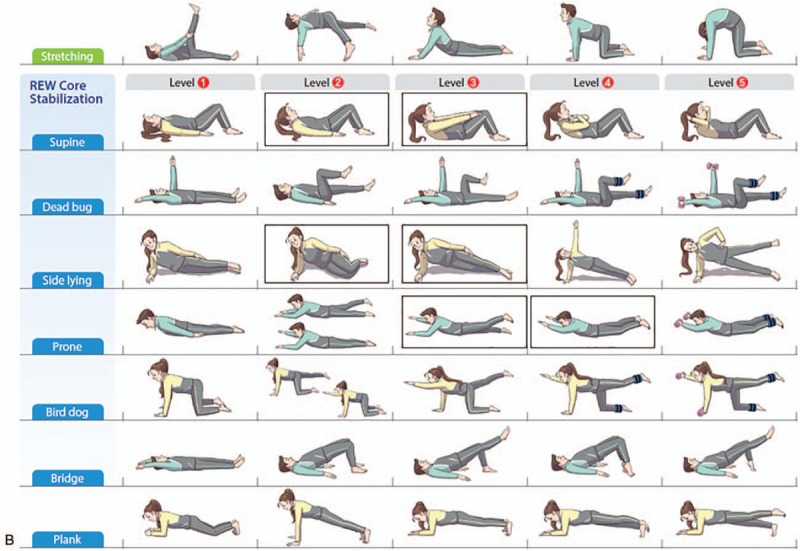
These figures show the exercise protocol for flexibility and lumbar stabilization exercises. Flexibility exercise consisted of stretching in the abdominal muscle, quadriceps, hamstring, tensor fascia lata, piriformis, and quadratus lumborum muscles (A). The stabilization exercise group was educated with individualized graded lumbar stabilization exercise (IGLSE). The IGLSE protocol consisted of 2 parts: the stretching exercises and stabilization exercises (B). After the stretching exercises of 5 minutes, patients were instructed to complete the stabilization exercises for 25 minutes. Each level had 7 basic positions: supine, dead bug, side-lying, prone, bird dog, bridge, and plank positions (5 levels). At the beginning, patients were placed into an exercise level with moderate difficulty, with gradual increase in difficulty with increased patient capacity. Squared figures show a specific posture used to measure the muscular endurance for the secondary outcome. Endurance was measured on 3 postures (supine, side-lying, and prone), respectively.
The first follow-up evaluation was done within 2 weeks after the completion of the 6-week exercise program, and all the initial evaluations were rechecked (immediately post-exercise program). The second follow-up evaluation was performed 12 weeks after the start of the program (6 weeks post-exercise program). At this evaluation, frequency and duration of exercise, as well as VAS of back pain and radiating pain during rest and physical activity, were rechecked via telephone questionnaire to investigate the long-term compliance and effectiveness of the exercise treatment. Participants were advised to continue the exercise routine for the full duration of the program and that the second follow-up evaluation would be performed at the 12th week.
2.7. Statistical Methods
SPSS 21.0 software (SPSS Inc, Chicago, IL) was used for all statistical analyses. Wilcoxon signed rank test was used to compare the variables before and after the exercise in each group. Kruskal-Wallis test was used to compare the 4 groups. Repeated measures ANOVA was used to compare the pain scores (VAS) at various time points: 1st week (preexercise program), 6th week (immediately post-exercise program), and 12th week (6 weeks post-exercise program). The results are presented as the mean ± standard deviation. P values of <.05 were considered statistically significant.
3. Results
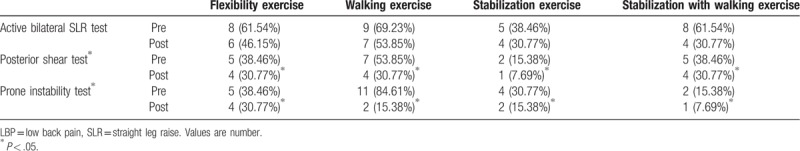
A total of 60 patients were enrolled in the study. They were randomly assigned to 1 of the 4 groups, based on the type of exercise: the FE group (n = 15), WE group (n = 15), SE group (n = 15), and SWE group (n = 15). Two patients in the FE group, 2 patients in the WE group, 5 patients in the SE group, and 3 patients in the SWE group dropped out for personal reasons. The remaining 48 subjects completed the 6-week exercise program without incident. After 12 weeks, the exercise amount, LBP, and radiating pain were examined via a telephone interview. Thirteen patients in the FE group, 12 in the WE group, 10 in the SE group, and 12 in the SWE group were followed up at 6 weeks after the end of the program (Fig. 2).
The demographic data of this study are shown in Table 1. The mean age of the entire study population was 54.81 years. There was no statistically significant difference with respect to age, sex, exercise frequency, exercise amount, and the frequency of medication use among the groups (Table 2). There was no significant difference in VAS of LBP and radiating pain during rest and physical activity at baseline. LBP during physical activity was significantly decreased in all four groups after the 6-week exercise program; LBP during rest was significantly decreased in the FE group and in the SE group (Table 2). Moreover, the frequency of medication use was decreased significantly in the FE group. Exercise frequency was significantly increased in the SE and WE groups, and exercise time was significantly increased in the SE group. According to these results, the highest compliance was seen in the SE group (Table 2).
Table 1.
Demographic data.
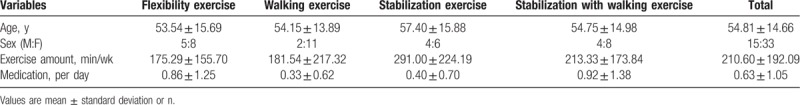
Table 2.
Comparison between preexercise, after 6 weeks, and 12 weeks of exercise in 4 groups.
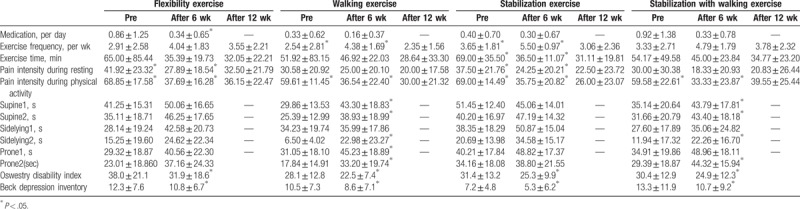
The WE and SWE groups showed a significant increase in the endurance to maintain prone, supine, and side-lying positions (Table 2). Moreover, the Oswestry disability index and Beck depression inventory were significantly improved in all 4 groups, and there was no significant difference between the 4 groups. In addition, there was no statistically significant difference between the 4 groups with respect to LBP and radiating pain at pre-, immediately post-, and 6 weeks-post exercise time points using the repeated measures ANOVA (Table 2, Fig. 3). Although statistically insignificant, the SE and WE groups showed more continuous improvement in LBP during rest and physical activity than the FE group (Figure 3A, B, D).
Figure 2.
This figure shows the study flow diagram.
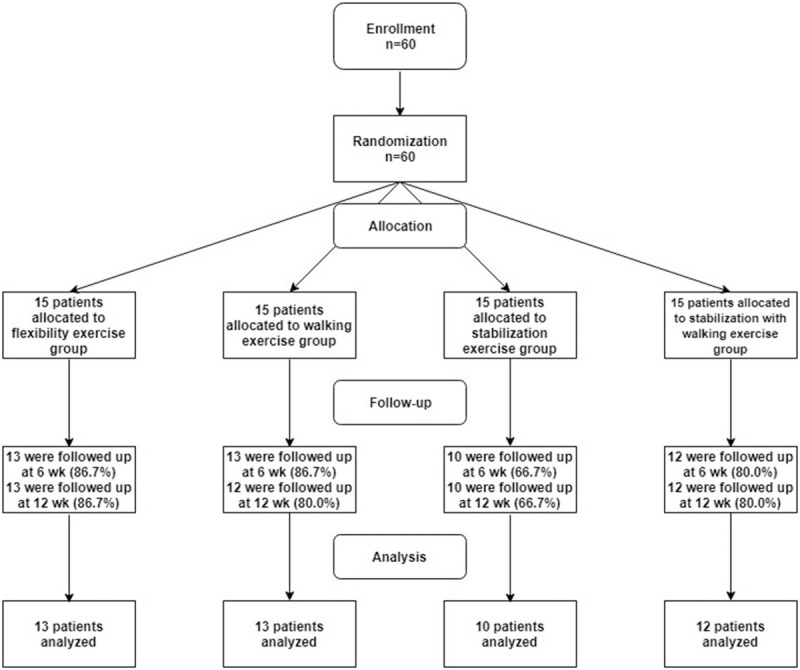
Table 3 shows the results of core stability. All groups showed a statically significant improvement in the posterior shear test and prone instability tests (Fisher exact test, P value of posterior shear test was .043 and the P value of prone instability test was .002). Additionally, improvement of prone instability test showed the largest improvement in the WE group and smallest improvement in the FE group (Table 3).
Table 3.
Comparison of tests for examination of LBP.
4. Discussion
LBP is a public health problem worldwide because of its socioeconomic and psychological impacts, as well as the limitations of its preventive or curative treatments proposed to date.[16] The efficiency—in terms of pain relief and functional restoration—of the therapeutic approaches based on active exercise has been demonstrated in several previous studies.[17,18] Based on literature review, physical exercise can help those suffering from chronic LBP by allowing the resumption of daily activities.[19] In particular, the supervised exercise therapy is recommended by the European Guidelines for Management of Chronic Non-Specific LBP as the first-line treatment.[20] However, these guidelines do not recommend a particular exercise; hence, the choice of exercise for chronic LBP largely depends on the preferences of patients and/or therapists, as well as cost and safety.[21–24] It is important for an exercise therapy to be simple, cost-effective, and easy to perform to maximize compliance.
Given these considerations, IGLSE and WE appear to be most appropriate, and as such, we evaluated the effectiveness and compliance of these 2 exercises. For ethical reasons, we were unable to use a placebo group for comparison; therefore, we compared these 2 exercises to a widely popular and highly efficacious FE.
Although we anticipated higher efficiency of IGLSE and WE than FE, LBP during physical activity was improved in all 4 groups, and there were no significant differences between the groups. We believe the reason for this is likely because the participants were correctly educated on lumbar posture and bracing exercise (Fig. 4A). Correct posture is a simple but very important way to keep many intricate structures of the back and spine healthy. The myoelectric silencing of the erector spinae muscles in the trunk flexion posture suggests increased load sharing on passive structures; tissues have been found to fail under excessive loading conditions and shown to be a source of LBP.[25] The correct lumbar posture emphasizes the significance of lumbar lordosis, which is effective in the prevention of lumbar disc protrusion. Moreover, abdominal bracing exercise is one of the most effective ways to induce a higher activation of deep abdominal muscles, such as the internal oblique muscle; this is so even when compared with dynamic exercises that involve flexion/extension movements of the trunk.[26,27] We educated the participants on the proper protocol and verified every 2 weeks whether they were performing the exercises as instructed. We believe that played a major role in all 4 groups showing significant improvement in pain relief. Moreover, although not significant, it is thought that the decrease in radiating pain, as shown in Figure 3C and D, may be because of the spontaneous regression of herniated lumbar disc[28,29] and improvement of stability of the paraspinalis muscles and lumbar lordosis.
Figure 3.
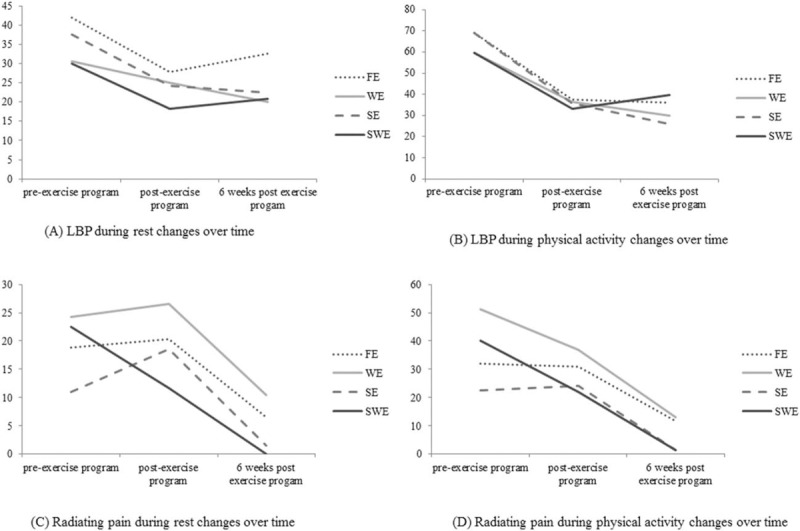
These figures show the changes of LBP and radiating pain during rest and physical activity, although statistically insignificant, the stabilization exercise group and walking exercise group showed more continuous improvement of LBP during rest and physical activity than the flexibility exercise group (A, B, D).
Figure 4.
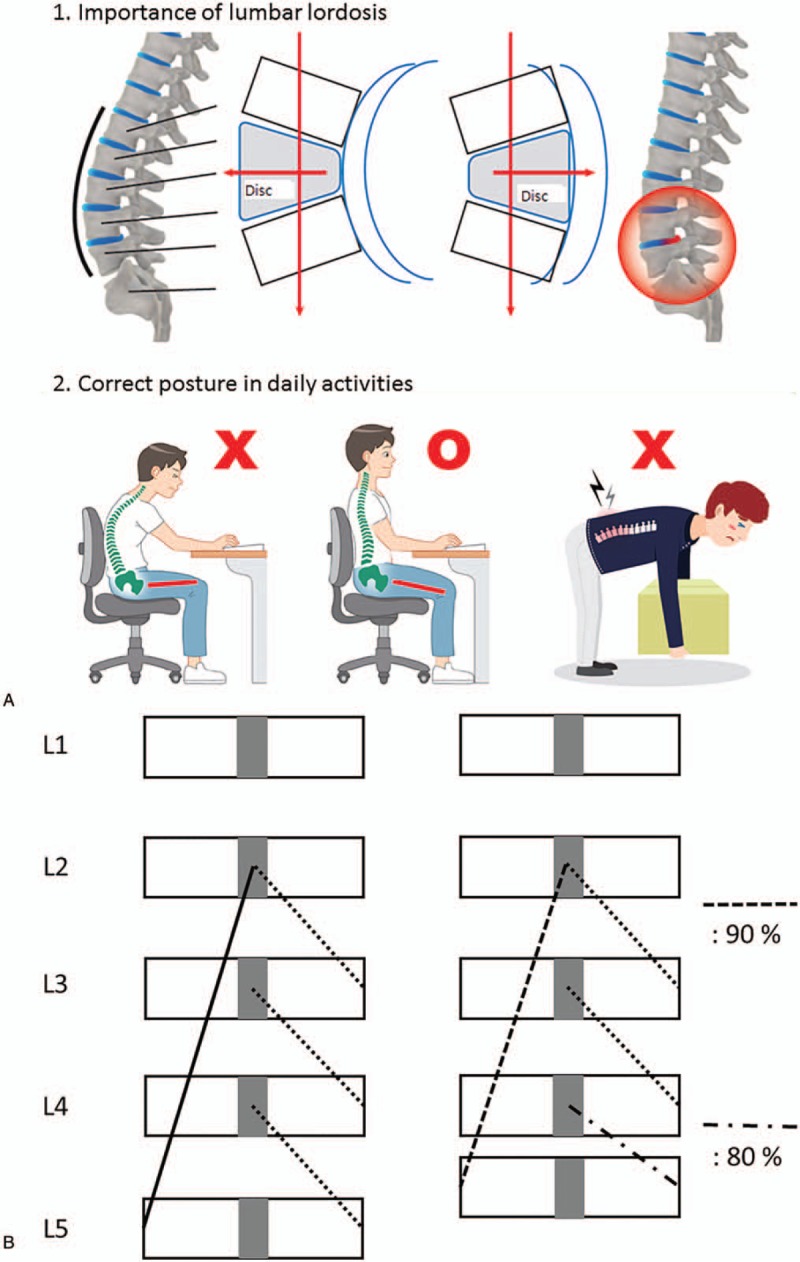
Figure (A) shows the pamphlet illustrating the correct postures. The correct lumbar posture emphasizes the significance of lumbar lordosis, which is effective in preventing lumbar disc protrusion (A). Figure (B) shows the rationale of why we adapted lumbar stabilization exercise that activates not only the deep muscles but also the superficial muscles simultaneously rather than motor control exercise. When lumbar 4-5 disc herniation develop, more loosening is developed at the multifidus muscle (eg, 20%) than the erector spinae muscle (eg, 10%). As a consequence, contraction of the deep multifidus muscles in these patients develops later than healthy population because of muscular loosening (B).
In a previous study, the size and quality of lumbar paraspinalis muscles were shown to be important factors for preventing relapse of LBP.[4] Patients with chronic LBP tend to develop reduced lumbar muscle strength due to pain-induced movement reduction. Therefore, patients with chronic LBP should pay close attention to various exercises that optimize the improvement of spinal muscle weakness. To strengthen lumbar paraspinalis muscles, we adapted IGLSE and WE. In the present study, WE showed a significant lumbar strengthening effect. Walking is widely accepted as a good choice for general back exercise and rehabilitation programs, as it strengthens the back muscles and reduces rigidity of motion.[15] Previous gait analysis showed that chronic LBP patients tend to have a slower walking speed when compared with healthy control subjects; moreover, it also showed diminishing normal velocity-induced transverse counter-rotation between the thorax and pelvis.[30] WE induces isometric contractions by increasing muscular activation, which may eventually lead to the prevention of LBP.[31] In the present study, we recommended fast walking while maintaining proper posture. Previous study showed that fast WE activates lumbar multifidus muscles more than slow WE and that increasing walking slope activates the mid-lumbar muscles more than lower lumbar muscles.[31] Prolonged activation of lumbar paraspinalis muscles have muscular strengthening effects; therefore, the paraspinalis strengthening effect may be greater in WE s than in other exercises.
Motor control exercise intervention focuses on the activation of deep trunk muscles and targets the restoration of control and co-ordination of these muscles, progressing to more complex and functional tasks that integrate the activation of deep and global trunk muscles.[21,32] Our hypothesis is that delayed activation of deep trunk muscles is not the cause of chronic LBP, but a consequence of disc space narrowing or spinal stenosis. For example, when the lumbar erector spinae muscles—which contract the long segments of the vertebrae—loosen 10% and when multifidus muscles—which contract the short segments—loosen 20%, disc space narrowing tends to develop (Fig. 4B). As a consequence, contraction of deep multifidus muscles in these patients develops later than the healthy population owing to muscular loosening. Therefore, we adapted a lumbar SE that activates not only the deep muscles, but also the superficial muscles simultaneously, and also developed the IGLSE, which can easily be applied to improve compliance. The present study showed that exercise frequency and exercise time, which can be used to measure compliance, were significantly increased in the SE group, suggesting high compliance (Table 2). In this exercise protocol, patients were initially placed into an adequate, yet somewhat difficult exercise level, with an incremental increase in the degree of difficulty within a 30-minute period.[12] Increased muscular activations in various postures were proved with previous surface electromyography.[13] We found that multiple postural changes may be beneficial to ensure better compliance with exercises, as both motivation and positive perception of exercises are necessary for treatment compliance. The short duration programs and minimal postures in the 7 basic positions and hospital-based home exercise programs are thought to be the main factors of high compliance.[12]
At the 6th week, the exercise time of the 4 groups was 35∼46 minutes. According to the study design, the exercise time of the SWE group should be twice as long as that of the other groups. However, the patients who have chronic LBP usually show atrophic changes in lumbar paraspinalis muscles.[2,4] So, it seemed that 60 minutes of exercise was difficult to do in chronic LBP patients. In fact, the frequency of exercise was significantly increased in the WE and SE groups after the study compared with before the study; however, this trend was not observed in the SWE group. It is assumed that compliance may fall with prolonged exercise time that exceeds patient ability. In future studies, it would be important to select an exercise program of around 30 minutes.
The present study suggested that the stabilization and WE s might have some favorable effects on the muscle strength and physical endurance. Considering the efficiency of the WE and the SE on reducing pain and improving the physical endurance, it is recommended that these interventions should be applied to treat chronic LBP.
4.1. Study limitation
There are some limitations of this study. First, the causes of LBP were heterogeneous. Nonetheless, this study is still valuable as the purpose of the study was to determine an effective exercise method to solve general LBP. Second, the full extent of the effect of SE, WE, and FE on LBP may be limited as abdominal bracing exercise and correct posture training were performed in all 4 groups owing to ethical reasons. Third, the short study period may be a limiting factor of this study. In the next study, it will be necessary to examine the effects of lumbar SE in chronic LBP by lengthening the study period. Fourth, the drug type and potency were not considered in this study. The lack of comparability of drug potency may be a limitation. Fifth, the American College of Sports Medicine minimum exercise guidelines recommend 20 minutes of aerobic activity, 3 days per week, and 1 set of 8 to 12 resistance exercises to train the major muscle groups 2 days per week. However, in this study, the exercise frequency was 5 times a week to increase exercise compliance. Further studies are needed to better evaluate and determine the proper frequency of the SEs. Sixth, we measured the endurance of the lumbar extensor muscle in the same manner as in the previous our study.[12] The reliability of this study would have been better if Biering-Sorensen test was performed.
5. Conclusion
The present study showed that lumbar SE and WE significantly improved chronic LBP. WE and stabilization with WE significantly improved muscular endurance of back muscles. Moreover, walking and SEs also improved the core stability. It is also worth noting that patients in the WE and SE groups were much more compliant than those in the other exercise groups. This study suggests that lumbar SE and WE should be recommended to patients with chronic LBP because they help not only to relieve back pain but also to prevent chronic back pain through the improvement of muscle endurance.
Acknowledgment
The authors gratefully appreciate MRCC team of Seoul National University Bundang Hospital for their work in the area of statistics in this study
Author contributions
Conceptualization: Ju Seok Ryu.
Formal analysis: Jee Hyun Suh, Gwang Pyo Jung.
Investigation: Hayoung Kim.
Supervision: Jin Young Ko.
Writing – original draft: Jee Hyun Suh.
Writing – review & editing: Ju Seok Ryu.
Footnotes
Abbreviations: FE = flexibility exercise, IGLSE = individualized graded lumbar stabilization exercise, LBP = low back pain, SE = stabilization exercise, SWE = stabilization with walking exercise, VAS = visual analog scale, WE = walking exercise.
This work was supported by Research Resettlement Fund for the new faculty of SNU. This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2016R1D1A1B03935130 to Ju Seok Ryu, MD, PhD (Department of Rehabilitation Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam-si, Gyeonggi-do, South Korea).
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
The authors report no conflicts of interest.
Suppliers: a. SPSS for Windows version 21.0, SPSS Inc., Chicago, Illinois, USA.
References
- [1].Waddell G. 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine (Phila Pa 1976) 1987;12:632–44. [DOI] [PubMed] [Google Scholar]
- [2].Arokoski JP, Valta T, Airaksinen O, et al. Back and abdominal muscle function during stabilization exercises. Arch Phys Med Rehabil 2001;82:1089–98. [DOI] [PubMed] [Google Scholar]
- [3].Roy SH, De Luca CJ, Casavant DA. Lumbar muscle fatigue and chronic lower back pain. Spine (Phila Pa 1976) 1989;14:992–1001. [DOI] [PubMed] [Google Scholar]
- [4].Lee HI, Lee ST, Kim M, et al. Sex differences in predicting chronicity of low-back pain after acute trauma using lumbar muscle area. Am J Phys Med Rehabil 2015;94:123–30. [DOI] [PubMed] [Google Scholar]
- [5].Magnusson ML, Aleksiev A, Wilder DG, et al. European Spine Society–the AcroMed Prize for Spinal Research 1995. Unexpected load and asymmetric posture as etiologic factors in low back pain. Eur Spine J 1996;5:23–35. [DOI] [PubMed] [Google Scholar]
- [6].Manniche C, Hesselsoe G, Bentzen L, et al. Clinical trial of intensive muscle training for chronic low back pain. Lancet 1988;2:1473–6. [DOI] [PubMed] [Google Scholar]
- [7].Manniche C, Lundberg E, Christensen I, et al. Intensive dynamic back exercises for chronic low back pain: a clinical trial. Pain 1991;47:53–63. [DOI] [PubMed] [Google Scholar]
- [8].O'Sullivan PB, Phyty GD, Twomey LT, et al. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine (Phila Pa 1976) 1997;22:2959–67. [DOI] [PubMed] [Google Scholar]
- [9].Geneen LJ, Moore RA, Clarke C, et al. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev 2017;1:Cd011279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Yamato TP, Maher CG, Saragiotto BT, et al. Pilates for low back pain: complete republication of a cochrane review. Spine (Phila Pa 1976) 2016;41:1013–21. [DOI] [PubMed] [Google Scholar]
- [11].Saragiotto BT, Maher CG, Yamato TP, et al. Motor control exercise for nonspecific low back pain: a cochrane review. Spine (Phila Pa 1976) 2016;41:1284–95. [DOI] [PubMed] [Google Scholar]
- [12].Lee HS, Kim DJ, Oh Y, et al. The effect of individualized gradable stabilization exercises in patients with chronic low back pain: case-control study. J Back Musculoskelet Rehabil 2016;29:603–10. [DOI] [PubMed] [Google Scholar]
- [13].Kim CR, Park DK, Lee ST, et al. Electromyographic changes in trunk muscles during graded lumbar stabilization exercises. PM R 2016;8:979–89. [DOI] [PubMed] [Google Scholar]
- [14].Hurley DA, Tully MA, Lonsdale C, et al. Supervised walking in comparison with fitness training for chronic back pain in physiotherapy: results of the SWIFT single-blinded randomized controlled trial (ISRCTN17592092). Pain 2015;156:131–47. [DOI] [PubMed] [Google Scholar]
- [15].Callaghan JP, Patla AE, McGill SM. Low back three-dimensional joint forces, kinematics, and kinetics during walking. Clin Biomech (Bristol, Avon) 1999;14:203–16. [DOI] [PubMed] [Google Scholar]
- [16].Abenhaim L, Rossignol M, Valat JP, et al. The role of activity in the therapeutic management of back pain. Report of the International Paris Task Force on Back Pain. Spine (Phila Pa 1976) 2000;25:1S–33S. [DOI] [PubMed] [Google Scholar]
- [17].Chambon X, Paysant J, Maureira JJ, et al. [Comparative study of effort training in deconditioned patients with and without pain. A preliminary study]. Ann Readapt Med Phys 2003;46:198–204. [DOI] [PubMed] [Google Scholar]
- [18].Chatzitheodorou D, Kabitsis C, Malliou P, et al. A pilot study of the effects of high-intensity aerobic exercise versus passive interventions on pain, disability, psychological strain, and serum cortisol concentrations in people with chronic low back pain. Phys Ther 2007;87:304–12. [DOI] [PubMed] [Google Scholar]
- [19].Hayden JA, van Tulder MW, Malmivaara AV, et al. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med 2005;142:765–75. [DOI] [PubMed] [Google Scholar]
- [20].Airaksinen O, Brox JI, Cedraschi C, et al. and Pain CBWGoGfCLB. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 2006;15suppl 2:S192–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Saragiotto BT, Maher CG, Yamato TP, et al. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev 2016;Cd012004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Shamsi M, Sarrafzadeh J, Jamshidi A, et al. Comparison of spinal stability following motor control and general exercises in nonspecific chronic low back pain patients. Clin Biomech (Bristol, Avon) 2017;48:42–8. [DOI] [PubMed] [Google Scholar]
- [23].Smith BE, Littlewood C, May S. An update of stabilisation exercises for low back pain: a systematic review with meta-analysis. BMC Musculoskelet Disord 2014;15:416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Geneen LJ, Moore RA, Clarke C, et al. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev 2017;4:Cd011279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Colloca CJ, Hinrichs RN. The biomechanical and clinical significance of the lumbar erector spinae flexion-relaxation phenomenon: a review of literature. J Manipulative Physiol Ther 2005;28:623–31. [DOI] [PubMed] [Google Scholar]
- [26].Maeo S, Takahashi T, Takai Y, et al. Trunk muscle activities during abdominal bracing: comparison among muscles and exercises. J Sports Sci Med 2013;12:467–74. [PMC free article] [PubMed] [Google Scholar]
- [27].Aleksiev AR. Ten-year follow-up of strengthening versus flexibility exercises with or without abdominal bracing in recurrent low back pain. Spine (Phila Pa 1976) 2014;39:997–1003. [DOI] [PubMed] [Google Scholar]
- [28].Chang CW, Lai PH, Yip CM, et al. Spontaneous regression of lumbar herniated disc. J Chin Med Assoc 2009;72:650–3. [DOI] [PubMed] [Google Scholar]
- [29].Autio RA, Karppinen J, Niinimaki J, et al. Determinants of spontaneous resorption of intervertebral disc herniations. Spine (Phila Pa 1976) 2006;31:1247–52. [DOI] [PubMed] [Google Scholar]
- [30].Lamoth CJ, Meijer OG, Daffertshofer A, et al. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: changes in motor control. Eur Spine J 2006;15:23–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Lee HS, Shim JS, Lee ST, et al. Facilitating effects of fast and slope walking on paraspinal muscles. Ann Rehabil Med 2014;38:514–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Standaert CJ, Weinstein SM, Rumpeltes J. Evidence-informed management of chronic low back pain with lumbar stabilization exercises. Spine J 2008;8:114–20. [DOI] [PubMed] [Google Scholar]


