Abstract
Statins are reported to reduce the risk of cancer, but the results of various published studies have been contradictory. We carried out an umbrella review to provide an overview and understand the strength of evidence, extent of potential biases, and validity of claimed associations between the use of statins and cancer incidence. We comprehensively re-analyzed the data of meta-analyses of randomized controlled trials (RCTs) and observational studies on associations between statin use and cancer incidence. We also assessed the strength of evidence of the re-analyzed outcomes, which were determined from the criteria including statistical significance of the p-value of random-effects, as well as fixed-effects meta-analyses, small study effects, between-study heterogeneity, and a 95% prediction interval. Using a conventional method to assess the significance of meta-analysis (p-value < 0.05), statins had a statistically significant effect on reducing cancer incidence in 10 of 18 types of cancer. When we graded the level of evidence, no cancer type showed convincing evidence, and four cancers (esophageal cancer, hematological cancer, leukemia, and liver cancer) showed suggestive evidence of a preventive effect. There was weak evidence of an association with six cancers, and no significance for the remaining eight cancers. None of the meta-analyses of RCTs on the association of statin and cancer incidence showed a statistical significance. Although there was a preventive effect of statin on cancer incidence in 10 of the 18 cancer types, the evidence supporting the use of statins to reduce cancer incidence was low. Therefore, the associations between statin use and cancer incidence should be carefully considered by clinicians.
Keywords: statin, cancer, meta-analysis, umbrella review
1. Introduction
Cancer places one of the biggest burdens on health care system in both highly developed and less developed countries, and its incidence and mortality have been increasing for decades mainly due to longer life expectancy [1]. Based on cancer statistics, 14.1 million new cancers occurred in 2012, while 8.2 million people died of cancer [2]. Despite the efforts of industry and physicians, overall survival and progression-free survival is still unsatisfactory for most cancer types.
Statins, competitively inhibiting 3-hydroxy-3-methylglutaryl coenzyme A reductase, have been used for lowering cholesterol levels [3]. Because of this effect of statin, statins have proven to be effective in reducing the risk of vascular diseases, such as coronary artery disease and stroke [4,5]. Besides their lipid-lowering effects, statins also exhibit anti-inflammatory, immunomodulatory and antithrombotic effects [6,7,8]. It has been proposed that statins also have anti-tumor effects. The mechanism of anti-tumor effect is poorly understood, but some in vitro studies indicate that statins suppress proliferation of tumor cells and angiogenesis [9,10]. Furthermore, epidemiologic studies, clinical trials and meta-analyses also support this benefit in different types of cancer, yet there is a lack of studies, and conflicting results on the relationship between statin use and cancer incidence [11,12,13].
To understand and evaluate the strength of the evidence of the effect of statins on reducing cancer incidence, we carried out an umbrella review and comprehensively re-analyzed the data of meta-analyses of randomized controlled trials (RCTs) and observational studies.
2. Materials and Methods
We performed an umbrella review of meta-analyses and systematic reviews reporting on the associations between statin use and the incidence of cancer. This umbrella review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14]. The PRISMA checklist is shown in the Supplementary Materials.
2.1. Literature Search
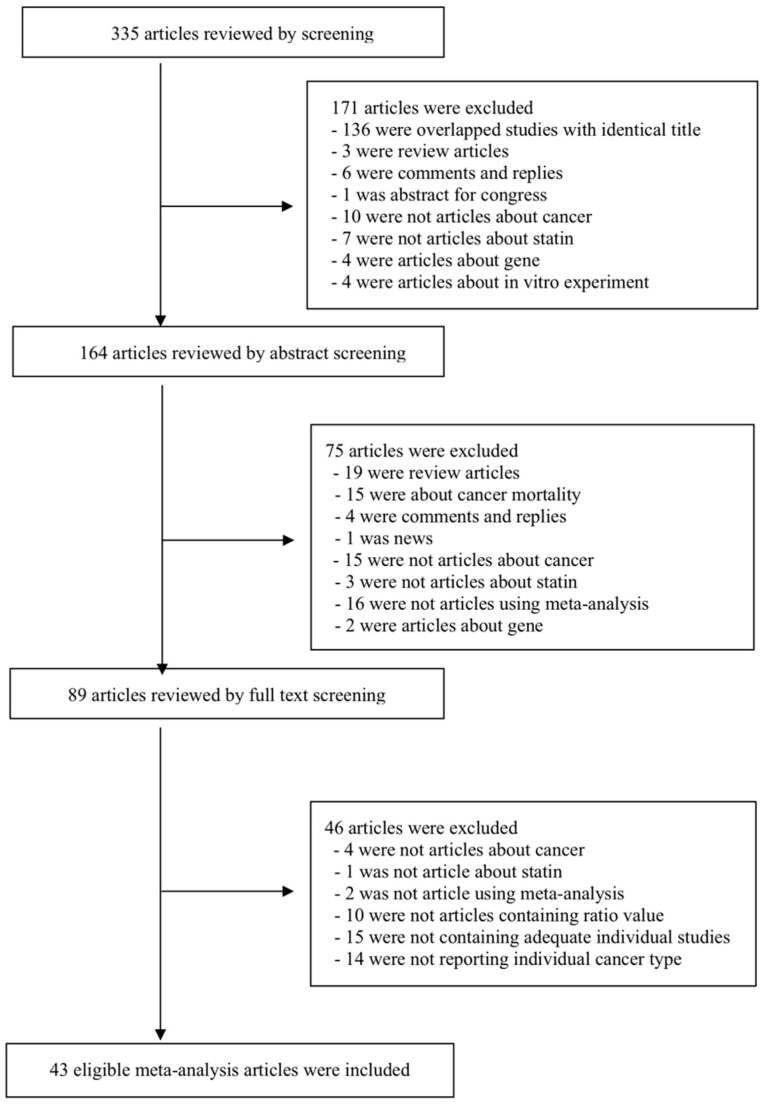
We searched the PubMed database and limited the articles to those written in English, regardless of the publication date. The final search was performed in August 2018. The keywords we used were the following: ‘(hydroxymethyl glutaryl-coa reductase inhibitor OR statin) AND (cancer OR neoplasm OR tumor) AND (meta-analysis OR systematic review)’. Meta analyses of either RCTs or observational studies were included in our search strategy. We reviewed the retrieved articles by examining the titles, the abstracts, and the full texts, then decided which article to include or exclude. We further searched the EMBASE database for potentially eligible meta-analyses, but no additional meta-analysis was included because the identified meta-analyses were lacking data necessary for performing re-analysis or overlapped with the PubMed search. The detailed search strategy is presented in Figure 1.
Figure 1.
Flow chart of the literature search.
2.2. Eligibility Criteria and Data Extraction
We included meta-analyses and systematic reviews of both RCTs and observational studies reporting on the relationship between statin use and cancer incidence. Observational studies included both cohort and case-control studies. We excluded review articles without meta-analysis, in vitro studies, and genetic studies. We also excluded meta-analyses lacking data necessary for performing re-analysis. If an article presented more than one meta-analysis, all meta-analyses were included and assessed separately by study design or cancer type.
Two investigators (G.H.J. and J.I.S) independently extracted the data, and discrepancies were resolved through consensus. We obtained the data from eligible meta-analyses and extracted and summarized the information on first author, year of publication, the type of cancer, the study design, the number of included studies, the number of cancer cases and total participants, and the random effects with a 95% confidence interval (CI). From the eligible studies, we also extracted the raw data of each individual study for further meta-analysis by combining all data by cancer and study design. If a single study consisted of both RCTs and observational studies, we separated the studies according to the study types (RCTs, observational studies, case-control, and cohort) and reported the results separately.
2.3. Statistical Analysis
We firstly re-analyzed each meta-analysis and reported the relationship between statin use and cancer incidence. In addition, if there were overlapping meta-analyses on the same topic, we combined all the individual studies from eligible meta-analyses according to the type of cancer and study design and performed a re-meta-analysis after eliminating overlapping individual studies and including missing individual studies. We presented the summary effect size, 95% CI, and p-value with both random- and fixed-effects. All re-analyses in this study were performed using the Comprehensive Meta-Analysis software ver.3.3.070 (Borestein, NH, USA).
2.4. Estimation of Summary Effects and Estimation of Prediction Interval
For each meta-analysis, we re-analyzed the individual studies and estimated the summary effects and 95% CI using both random- and fixed-effects methods [15]. We also calculated and presented the 95% prediction interval (PI), which address the dispersion of effects (in 95% of cases the true effect in a new study will fall within the PI) and further account for between-study heterogeneity [16], whereas CI reflects the accuracy of the mean.
2.5. Evaluation of Between-Study Heterogeneity and Small Study Effects
We assessed heterogeneity across the studies using the I2 metric of inconsistency and the p value of the X2-based Cochrane Q test. I2 values of <50%, 50%–75%, and >75% are usually judged to represent low or moderate, large and very large heterogeneity, respectively [17].
Publication bias was evaluated by using Egger’s regression test [18]. Small study effects were used for detecting publication and reporting bias [19,20]. When the Egger’s test was significant (p-value < 0.10) in random-effects meta-analyses, we decided that the study has small-study effects.
2.6. Determination of the Level of Evidence
We determined the level of evidence of each meta-analysis and re-analyzed the pooled meta-analysis to classify the strength of the evidence of the association between statin use and cancer incidence. The criteria were set according to the statistical significance by random and fixed-effects p-values, 95% PI, a small-study effects, a between-study heterogeneity, and concordance between the effect estimate of the largest study and summary estimate of the meta-analysis [21]. The criteria were as follows:
Convincing evidence: There was a statistical significance for the random-effect and fixed-effect p-values at p < 0.001. No small study effects or large between-study heterogeneity were found, and 95% PI rejected the null hypothesis. There was a concordance between the effect estimate of the largest study and the summary effect of the random-effects meta-analysis.
Suggestive evidence: There was statistical significance of random effects at p < 0.05, but a 95% PI included the null hypothesis. No small study effects or large between-study heterogeneity were found.
Weak evidence: There was a statistical significance of random effects at p < 0.05. Small study effects or large between-study heterogeneity were found.
Non-significant association: There was no statistical significance by random effect meta-analysis (p > 0.05)
However, if large heterogeneity was found, we rechecked the results to determine whether it might be due to differences in the direction of the effect or if it could be due to differences in the size of the association. In the latter case, we re-determined the level of evidence again.
3. Results
3.1. Characteristics of Studies Included in the Final Analyses
A total of 335 meta-analyses was retrieved from our PubMed database search, and 43 eligible meta-analyses were selected for re-analysis. At first, 171 articles, including 136 duplicate articles, were excluded by title screening. Another 75 articles were excluded after assessing the abstract, and 46 articles were finally excluded after full text screening. The detailed flow diagram is presented in Figure 1.
Forty-three meta-analyses eligible for our umbrella review investigated the associations between statin use and the incidence of 18 types of cancer [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64]. Information on 43 individual meta-analysis is presented in Supplementary Table S1.
3.2. Assessing the Effect of Statin on Cancer Incidence with Conventional Interpretation of Meta-Analyses Criteria (Random Effects p-Value < 0.05)
First, we summarized and re-analyzed the results of the previously reported meta-analysis for each stain-cancer incidence association, but there were sometimes discordant results among the meta-analyses of same statin-cancer association. Therefore, we pooled all the individual RCTs and observational studies extracted from eligible studies without missing or overlapping any studies and performed re-meta-analysis in 18 types of cancer to reach a final conclusion of association between statin use and the incidence of one cancer type. Among these, 10 associations (esophageal cancer, hematological cancer, leukemia, liver cancer, breast cancer, colorectal cancer, gastric cancer, lung cancer, lymphoma, and prostate cancer) were statistically significant under the conventional interpretation of meta-analysis criteria (p < 0.05), while eight associations (bladder cancer, endometrial cancer, gynecological cancer, kidney cancer, melanoma, myeloma, pancreatic cancer, and non-melanoma skin cancer) were not significant (Table 1).
Table 1.
Summary of meta-analyses by combining all the data on associations of the use of statin and the incidence of cancers.
| Cancer Type | No of Studies |
No of Total Participants |
Random Effects (RR, 95%CI) |
P (Random) |
Fixed Effects (RR, 95%CI) |
P (Fixed) | Largest Effect§ (RR, 95%CI) |
D/N/I | Egger | I2 (P) † | 95% PI (Random Effects) |
95% PI (Fixed Effects) |
Small Study Effects |
Concordant Direction | Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bladder cancer | 13 | 1,266,218 | 1.07 (0.95–1.21) | 0.282 | 1.12 (1.07–1.19) | <0.001 | 1.08 (0.99–1.19) | 0/11/2 | 0.851 | 62.6 (0.001) | 0.76–1.51 | 0.81–1.56 | No | Yes | Non-significant |
| Breast cancer | 62 | 3,884,629 | 0.91 (0.85–0.97) | 0.004 | 1.00 (0.97–1.02) | 0.724 | 1.04 (0.98–1.11) | 12/44/3 | 0.023 | 79.6 (<0.001) | 0.63–1.32 | 0.69–1.44 | Yes | No | Weak |
| Colorectal cancer | 59 | 13,855,147 | 0.92 (0.88–0.95) | <0.001 | 0.94 (0.93–0.96) | <0.001 | 0.88 (0.81–0.95) | 15/33/3 | 0.106 | 71.5 (<0.001) | 0.76–1.11 | 0.78–1.14 | No | Yes | Weak |
| Endometrial cancer | 15 | 878,885 | 0.94 (0.82–1.07) | 0.349 | 1.02 (0.97–1.08) | 0.423 | 1.05 (0.95–1.15) | 4/11/0 | 0.043 | 54.9 (<0.001) | 0.66–1.34 | 0.73–1.43 | Yes | Yes | Non-significant |
| Esophageal cancer | 27 | 3,158,414 | 0.70 (0.63–0.78) | <0.001 | 0.85 (0.71–0.89) | <0.001 | 0.68 (0.52–0.88) | 15/12/0 | 0.115 | 60.7 (<0.001) | 0.46–1.05 | 0.50–1.11 | No | Yes | Suggestive * |
| Gastric cancer | 16 | 5,396,224 | 0.74 (0.60–0.90) | 0.004 | 0.84 (0.79–0.88) | <0.001 | 0.97 (0.74–1.26) | 5/11/0 | 0.325 | 90.8 (<0.001) | 0.33–1.62 | 0.39–1.78 | No | No | Weak |
| Gynecological cancer | 23 | 928,721 | 0.89 (0.78–1.02) | 0.087 | 1.00 (0.93–1.06) | 0.899 | 1.05 (0.95–1.15) | 4/19/0 | 0.003 | 43.7 (0.014) | 0.62–1.29 | 0.70–1.41 | Yes | Yes | Non-significant |
| Hematological cancer | 34 | NA | 0.89 (0.82–0.96) | 0.005 | 0.86 (0.81–0.90) | <0.001 | NA ** | 7/26/1 | 0.161 | 46.7 (0.002) | 0.60–1.20 | 0.64–1.15 | No | - | Suggestive |
| Kidney cancer | 11 | 4,052,120 | 0.91 (0.70–1.17) | 0.457 | 0.94 (0.88–1.00) | 0.034 | 1.08 (0.99–1.18) | 2/9/0 | 0.722 | 88.7 (<0.001) | 0.39–2.09 | 0.43–2.05 | No | Yes | Non-significant |
| Leukemia | 9 | 1174 | 0.85 (0.74–0.98) | 0.031 | 0.83 (0.74–0.92) | 0.001 | 0.74 (0.62–0.87) | 2/7/0 | 0.120 | 25.0 (0.220) | 0.63–1.16 | 0.62–1.10 | No | Yes | Suggestive |
| Liver cancer | 27 | 2,622,626 | 0.58 (0.52–0.66) | <0.001 | 0.65 (0.62–0.68) | <0.001 | 0.52 (0.41–0.66) | 22/5/0 | 0.117 | 83.8 (<0.001) | 0.33–1.03 | 0.38–1.13 | No | Yes | Suggestive * |
| Lung cancer | 33 | 8,833,965 | 0.89 (0.80–0.99) | 0.036 | 0.82 (0.80–0.84) | <0.001 | 1.03 (0.94–1.21) | 5/28/0 | 0.265 | 94.9 (<0.001) | 0.51–1.57 | 0.47–1.42 | No | No | Weak |
| Lymphoma | 16 | 8863 | 0.85 (0.73–0.99) | 0.042 | 0.86 (0.80–0.92) | <0.001 | 0.96 (0.83–1.11) | 6/9/1 | 0.850 | 69.1 (<0.001) | 0.52–1.40 | 0.54–1.39 | No | No | Weak |
| Melanoma | 24 | 434,680 | 0.94 (0.86–1.03) | 0.204 | 0.94 (0.88–1.00) | 0.063 | 0.94 (0.88–1.00) | 3/21/0 | 0.836 | 26.0 (0.121) | 0.74–1.19 | 0.60–1.46 | No | No | Non-significant |
| Myeloma | 5 | 609 | 0.89 (0.53–1.51) | 0.674 | 0.89 (0.73–1.09) | 0.251 | 0.83 (0.61–1.12) | 2/2/1 | 0.983 | 81.0 (<0.001) | 0.14–5.73 | 0.17–4.78 | No | Yes | Non-significant |
| Pancreatic cancer | 20 | 2,832,052 | 0.89 (0.75–1.06) | 0.207 | 0.91 (0.86–0.97) | 0.003 | 1.10 (0.81–1.49) | 1/18/1 | 0.927 | 79.0 (<0.001) | 0.46–1.71 | 0.49–1.71 | No | Yes | Non-significant |
| Prostate cancer | 44 | NA | 0.94 (0.90–0.99) | 0.017 | 1.02 (1.00–1.04) | 0.056 | NA ** | 18/42/4 | 0.002 | 74.5 (<0.001) | 0.71–1.24 | 0.78–1.33 | Yes | - | Weak |
| Non-melanoma skin cancer | 17 | 1,240,281 | 1.07 (1.00–1.16) | 0.063 | 1.09 (1.06–1.13) | <0.001 | 1.09 (1.06–1.13) | 1/11/5 | 0.768 | 58.5 (0.001) | 0.88–1.31 | 0.90–1.32 | No | No | Non-significant |
D/N/I: Decreasing risk/No difference/Increasing risk; RR: Relative risk; CI: Confidence interval; PI: Prediction interval. § Relative risk (95% Confidence interval) of the largest study in each meta-analysis. † I2 metric of inconsistency (95% confidence interval of I2) and p-value of the Cochran Q test for evaluation of heterogeneity. * Suggestive level of evidence due to the greater number of studies that decrease risk in which a high heterogeneity is due to differences in the effect size of the association. ** Largest effect of study of hematologic and prostate cancer were not assessible due to lack of number of participants data in individual studies.
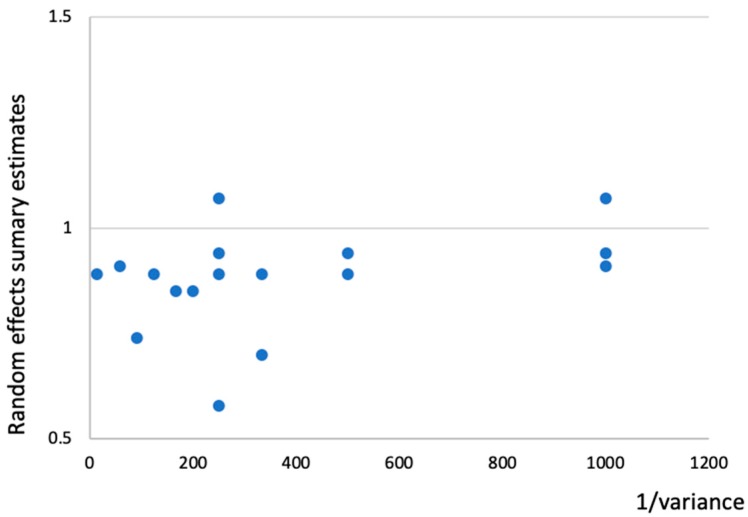
When associations of the meta-analysis summary effect sizes were analyzed with an inverse of the variance, meta-analyses with small variances showed a trend of summary effects towards 1.00 in cancer incidence, as shown in Figure 2.
Figure 2.
Association of meta-analysis summary effect sizes with the inverse of the variance in cancer incidence.
3.3. Assessing the Statin Effect on Cancer Incidence with Criteria by Previous Umbrella Review
We determined the level of evidence by not only using random effect p-values but also by using between-study heterogeneity, small study effects, and 95% PI according to the methods previously published [21]. Under the suggested criteria, we found that none of the associations showed convincing evidence, four associations (esophageal cancer, hematological cancer, leukemia and liver cancer) were found to show suggestive evidence. Six associations (breast cancer, colorectal cancer, gastric cancer, lung cancer, lymphoma, and prostate cancer) showed weak evidence. Details of the graded associations are presented in Table 1.
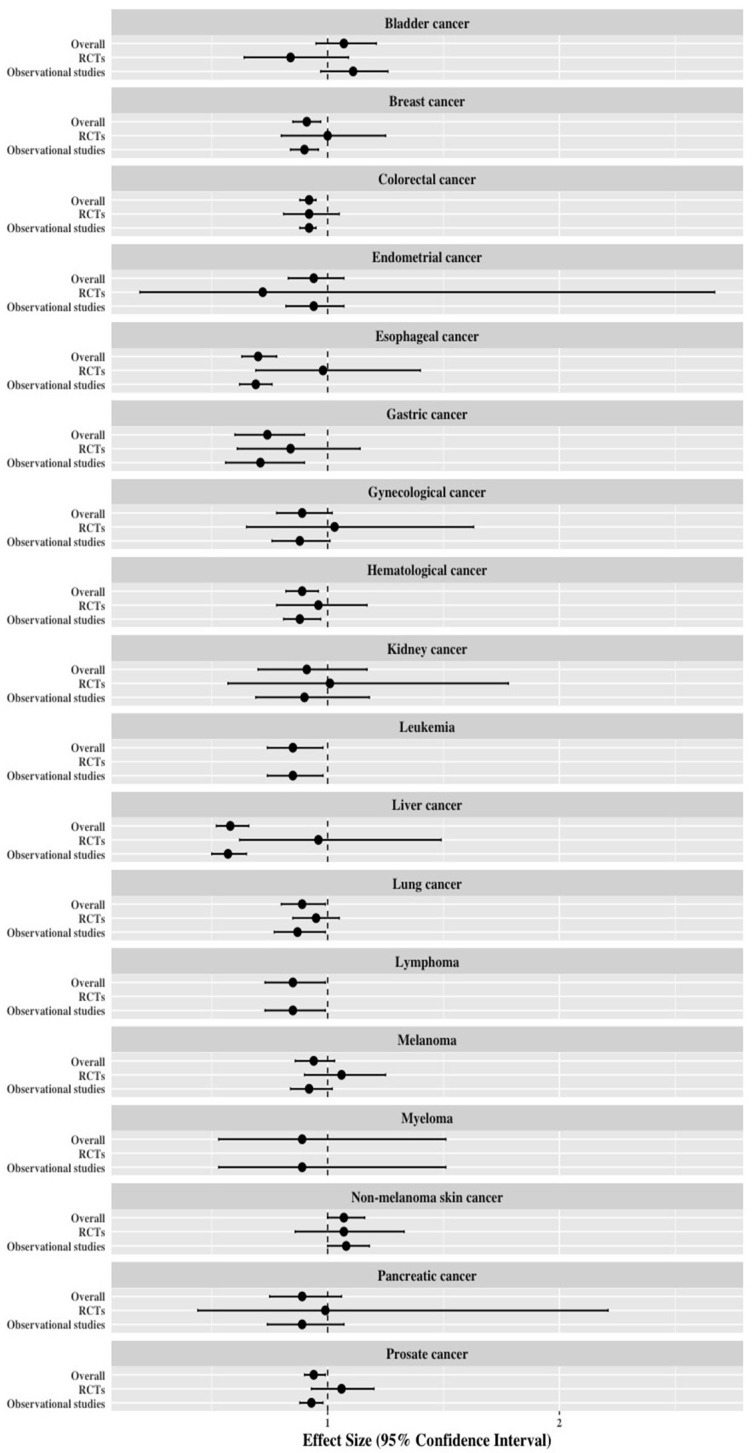
3.4. Re-Analysis of Meta-Analyses Separated by Study Design
In addition to the above process, we performed subgroup analyses of eligible meta-analyses by study designs (RCTs and observational studies) and carried out a re-meta-analysis of the pooled raw data in association with statin use and cancer incidence (Table 2). All overlapping individual studies were omitted while pooling the raw data. Details of the individual overlapping meta-analyses with different study designs on associations with statin and cancer incidence are summarized in Table 3
Table 2.
Re-analysis of the meta-analyses by study design.
| Cancer Type | Overall | Randomized Controlled Studies | Observational Studies * | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Random Effects (RR, 95%CI) |
p-Value | Evidence | No. of Studies | Random Effects (RR, 95%CI) |
p-Value | Evidence | No. of Studies | Random Effects (RR, 95%CI) |
p-Value | Evidence | |
| Bladder cancer | 13 | 1.07 (0.95–1.21) | 0.282 | Non-significant | 3 | 0.84 (0.64–1.09) | 0.180 | Non-significant | 10 | 1.11 (0.97–1.26) | 0.118 | Non-significant |
| Breast cancer | 62 | 0.91 (0.85–0.97) | 0.004 | Weak | 12 | 1.00 (0.80–1.25) | 0.661 | Non-significant | 50 | 0.90 (0.84–0.96) | 0.003 | Weak |
| Colorectal cancer | 59 | 0.92 (0.88–0.95) | <0.001 | Weak | 13 | 0.92 (0.81–1.05) | 0.214 | Non-significant | 46 | 0.92 (0.88–0.95) | <0.001 | Weak |
| Endometrial cancer | 15 | 0.94 (0.83–1.07) | 0.349 | Non-significant | 2 | 0.72 (0.19–2.67) | 0.621 | Non-significant | 13 | 0.94 (0.82–1.07) | 0.361 | Non-significant |
| Esophageal cancer | 27 | 0.70 (0.63–0.78) | <0.001 | Suggestive | 1 | 0.98 (0.69–1.40) | NR | Non-significant | 26 | 0.69 (0.62–0.76) | <0.001 | Suggestive |
| Gastric cancer | 16 | 0.74 (0.60–0.90) | 0.004 | Weak | 3 | 0.84 (0.61–1.14) | 0.259 | Non-significant | 13 | 0.71 (0.56–0.90) | 0.004 | Weak |
| Gynecological cancer | 23 | 0.89 (0.78–1.02) | 0.087 | Non-significant | 6 | 1.03 (0.65–1.63) | 0.902 | Non-significant | 17 | 0.88 (0.76–1.01) | 0.069 | Non-significant |
| Hematological cancer | 34 | 0.89 (0.82–0.96) | 0.005 | Suggestive | 8 | 0.96 (0.78–1.17) | 0.667 | Non-significant | 26 | 0.88 (0.81–0.97) | 0.006 | Suggestive |
| Kidney cancer | 11 | 0.91 (0.70–1.17) | 0.457 | Non-significant | 2 | 1.01 (0.57–1.78) | 0.985 | Non-significant | 9 | 0.90 (0.69–1.18) | 0.455 | Non-significant |
| Leukemia | 9 | 0.85 (0.74–0.98) | 0.031 | Suggestive | - | - | - | - | 9 | 0.85 (0.74–0.98) | 0.031 | Suggestive |
| Liver cancer | 27 | 0.58 (0.52–0.66) | <0.001 | Suggestive | 3 | 0.96 (0.62–1.49) | 0.867 | Non-significant | 24 | 0.57 (0.50–0.65) | <0.001 | Suggestive |
| Lung cancer | 33 | 0.89 (0.80–0.99) | 0.036 | Weak | 9 | 0.95 (0.85–1.05) | 0.324 | Non-significant | 24 | 0.87 (0.77–0.99) | 0.034 | Weak |
| Lymphoma | 16 | 0.85 (0.73–0.99) | 0.042 | Weak | - | - | - | - | 16 | 0.85 (0.73–0.99) | 0.042 | Weak |
| Melanoma | 24 | 0.94 (0.86–1.03) | 0.204 | Non-significant | 13 | 1.06 (0.90–1.25) | 0.474 | Non-significant | 11 | 0.92 (0.84–1.02) | 0.105 | Non-significant |
| Myeloma | 5 | 0.89 (0.53–1.51) | 0.674 | Non-significant | - | - | - | - | 5 | 0.89 (0.53–1.51) | 0.674 | Non-significant |
| Pancreatic cancer | 20 | 0.89 (0.75–1.06) | 0.207 | Non-significant | 3 | 0.99 (0.44–2.21) | 0.982 | Non-significant | 17 | 0.89 (0.74–1.07) | 0.202 | Non-significant |
| Prostate cancer | 64 | 0.94 (0.90–0.99) | 0.017 | Weak | 7 | 1.06 (0.93–1.20) | 0.386 | Non-significant | 57 | 0.93 (0.88–0.98) | 0.005 | Weak |
| Non-melanoma skin cancer | 17 | 1.07 (1.00–1.16) | 0.063 | Non-significant | 8 | 1.07 (0.86–1.33) | 0.519 | Non-significant | 9 | 1.08 (1.00–1.18) | 0.048 | Weak |
RR: Relative risk. * Observational studies include both cohort studies and case-control studies.
Table 3.
Summary of individual overlapping meta-analyses with different study designs on associations with statin and cancer incidence.
| Cancer Type | Overall | Randomized Controlled Trials | Observational Studies | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Meta-Analyses |
D/N/I | C/S/W | Number of Meta-Analyses |
D/N/I | C/S/W | Number of Meta-Analyses |
D/N/I | C/S/W | ||||
| Bladder cancer | 1 | 0/1/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | |||
| Breast cancer | 2 | 0/2/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | 3 | 1/2/0 | 0/1/0 | |||
| Colorectal cancer | 4 | 4/0/0 | 1/0/3 | 4 | 0/4/0 | 0/0/0 | 5 | 5/0/0 | 1/0/4 | |||
| Endometrial cancer | 1 | 0/1/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | |||
| Esophageal cancer | 2 | 2/0/0 | 1/0/1 | 0 | 0/0/0 | 0/0/0 | 6 | 6/0/0 | 2/4/0 | |||
| Gastric cancer | 2 | 2/0/0 | 0/0/2 | 1 | 0/1/0 | 0/0/0 | 2 | 2/0/0 | 0/0/2 | |||
| Gynecological cancer | 1 | 0/1/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | |||
| Hematological cancer | 2 | 1/1/0 | 0/0/1 | 2 | 0/2/0 | 0/0/0 | 2 | 1/1/0 | 0/0/1 | |||
| Kidney cancer | 1 | 0/0/1 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | |||
| Leukemia | 0 | 0/0/0 | 0/0/0 | 0 | 0/0/0 | 0/0/0 | 1 | 1/0/0 | 0/1/0 | |||
| Liver cancer | 3 | 3/0/0 | 1/1/1 | 0 | 0/0/0 | 0/0/0 | 1 | 1/0/0 | 0/1/0 | |||
| Lung cancer | 2 | 0/2/0 | 0/0/0 | 3 | 0/3/0 | 0/0/0 | 3 | 0/3/0 | 0/0/0 | |||
| Lymphoma | 0 | 0/0/0 | 0/0/0 | 0 | 0/0/0 | 0/0/0 | 2 | 1/1/0 | 0/0/1 | |||
| Melanoma | 1 | 0/1/0 | 0/0/0 | 3 | 0/3/0 | 0/0/0 | 0 | 0/0/0 | 0/0/0 | |||
| Myeloma | 0 | 0/0/0 | 0/0/0 | 0 | 0/0/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | |||
| Pancreatic cancer | 2 | 0/2/0 | 0/0/0 | 2 | 0/2/0 | 0/0/0 | 2 | 0/2/0 | 0/0/0 | |||
| Prostate cancer | 1 | 0/1/0 | 0/0/0 | 1 | 0/1/0 | 0/0/0 | 6 | 1/5/0 | 0/0/1 | |||
| Non-melanoma skin cancer | 2 | 0/1/1 | 0/0/1 | 1 | 0/1/0 | 0/0/0 | 1 | 0/0/1 | 0/0/1 | |||
D/N/I: Decreasing risk/No difference/Increasing risk; C/S/W: Convincing/Suggestive/Weak.
Of the 18 types of cancer, three cancer types (leukemia, lymphoma, and myeloma) did not have meta-analyses using RCTs. Among the other 15 cancer types, there was no statistically significant statin–cancer incidence association in meta-analyses of RCTs (Figure 3). For the 18 observational studies, four cancers (esophageal cancer, hematological cancer, leukemia, and liver cancer) showed suggestive evidence, seven cancers (breast cancer, colorectal cancer, gastric cancer, lung cancer, lymphoma, prostate cancer and non-melanoma skin cancer) showed weak evidence, and seven cancers (bladder cancer, endometrial cancer, gynecological cancer, kidney cancer, melanoma, myeloma and pancreatic cancer) were not statistically significant. Therefore, the most significant results of statin-cancer associations were determined by the results of the observational studies.
Figure 3.
Differences of effect size and 95% confidence interval among the meta-analysis of overall population, randomized controlled trials (RCTs), and observational studies in cancer incidence associated with statin use
4. Discussion
The purpose of this umbrella review of previous meta-analyses and re-analysis of meta-analyses, including all the individual studies, was to highlight the potential effects of statin use on cancer incidence. We re-analyzed the data from 43 meta-analyses to evaluate the associations between use of statins and cancer incidence. By only using a random-effects p-value, 10 of 18 associations of cancer incidence showed a statistically significant preventive effect of statin.
Although there was a weak or non-significant preventive effect of statin use on most cancer types, there was a suggestive level of evidence regarding the preventive effects of statin use on four cancer types (esophageal cancer, hematological cancer, leukemia, and liver cancer). Re-analysis of association between statin use and leukemia incidence was performed with one eligible meta-analysis [31] consisting of nine individual studies, which might be relatively a small number of individual studies for re-analysis. However, associations of the other three cancer types had an adequate number of individual studies (27 for esophageal cancer, 34 for hematological cancer, and 27 for liver cancer). A large number of the included studies for meta-analyses are considered to be valid [65], and, therefore, the outcomes for the 3 cancer types mentioned above might be plausible. Six types of cancer had weak evidence due to substantial publication bias and significant heterogeneity established by the value.
Although most of the re-analyses showed weak or non-significant evidence, the conventional interpretation of current meta-analysis is that there was preventive effect of statin use on cancer incidence in some cancer types, based on a random effects p-value, an effect size with 95% CI [66]. According to these criteria, 10 of 18 meta-analyses on cancer incidence outcomes demonstrated that statins have a preventive effect on cancer risk.
In addition, while most of the statistically significant individual meta-analyses showed that statins have a preventive effect on cancer, one meta-analysis of observational studies on association with statin and non-melanoma skin cancer suggested that there was a positive relationship between statin and non-melanoma skin cancer [24]. Yang et al. suggested that meta-analyses of observational studies might show more noteworthy result due to the characteristic of observational studies, since it may have advantage of examining rare occurrences of diseases such as cancer. However, the level of evidence in this study was weak, and it included only one meta-analysis. Therefore, we must scrutinize the validity of the results. Further meta-analyses with additional studies will be needed.
Our study evaluates the strength of evidence using multiple values presented or calculated in each meta-analysis. The strength of evidence reinforces the results from the meta-analyses and helps choose the best evidence. Various methods for assessing the evidence level are presented, yet there is no definite grading method for an umbrella review [67,68]. Recent umbrella reviews include the p-value of the meta-analysis, between-study heterogeneity, small study effect, and 95% PI for the grading the level of evidence, which is more related to quantitative values [20,21,69].
In addition, substantial heterogeneity is an issue in systematic review and meta-analysis. It is essential to explain and manage the heterogeneity to underline the validity of the respective findings [70]. Umbrella reviews that re-analyze meta-analyses include large number of individual studies, and, therefore, controlling their heterogeneity can be troublesome. Previous umbrella reviews determined a large heterogeneity of > 50–75%% as weak evidence [71,72]. However, this application should be applied cautiously, because heterogeneity can increase if the number of individual studies increases. In addition, if the heterogeneity is large, it can be due to differences in the direction of the effect, or it can be due to differences in the size of the association. In the latter case, therefore, we thought the level of evidence should be re-determined and upgraded the level of evidence from weak to suggestive.
In the eligible meta-analyses, overlapping meta-analyses on the same topic were frequently reported (Table 3). Overlapping meta-analyses may give an ambiguous result and should be acknowledged [73]. There are several ways to overcome this problem, and we carried out re-analysis by merging all the extracted individual studies with coherent data. Integration of data from meta-analyses might have more strengths than assembling existing reviews [74]. In our study, the incidence of lymphoma associated with statin use showed a statistically significant outcome with a weak level of evidence, but two other eligible individual meta-analyses of the same association were not significant (Supplementary Table S1). Also, re-analysis of the association of incidence of prostate cancer with statin use was graded as weak evidence, but recent meta-analysis performed by Raval et al. [29] was not significant. Raval et al. only included 27 individual studies, but our study included a total of 64 individual studies, which highlights that there may have been missing eligible studies even in the recent meta-analysis. The comparison of the results of our study and the largest meta-analysis are presented in Table 4.
Table 4.
Comparison of the results with number of included individual studies of our study and the largest meta-analysis.
| Type of Cancer | Randomized Controlled Trials | Observational Studies | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Our Study | Largest Meta-Analysis * | Our Study | Largest Meta-Analysis * | |||||||||
| No. of Study | Random Effects (RR 95% CI) | No. of Study | Random Effects (RR 95% CI) | No. of Study | Random Effects (RR 95% CI) | No. of Study | Random Effects (RR 95% CI) | |||||
| Bladder cancer | 3 | 0.84 (0.64–1.09) | 3 | 0.83 (0.64–1.09) | 10 | 1.11 (0.97–1.26) | 10 | 1.11 (0.97–1.26) | ||||
| Breast cancer | 12 | 1.00 (0.80–1.25) | 7 | 1.19 (0.81–1.73) | 50 | 0.90 (0.84–0.96) | 21 | 0.99 (0.94–1.04) | ||||
| Colorectal cancer | 13 | 0.92 (0.81–1.05) | 11 | 0.96 (0.85–1.08) | 46 | 0.92 (0.88–0.95) | 32 | 0.92 (0.87–0.96) | ||||
| Endometrial cancer | 2 | 0.72 (0.19–2.67) | 2 | 0.72 (0.19–2.67) | 13 | 0.94 (0.82–1.07) | 13 | 0.94 (0.82–1.07) | ||||
| Esophageal cancer | 1 | 0.98 (0.69–1.40) | - | - | 26 | 0.69 (0.62–0.76) | 10 | 0.59 (0.50–0.68) | ||||
| Gastric cancer | 3 | 0.84 (0.61–1.14) | 3 | 0.84 (0.61–1.14) | 13 | 0.71 (0.56–0.90) | 9 | 0.70 (0.53–0.93) | ||||
| Gynecological cancer | 6 | 1.03 (0.65–1.63) | 6 | 1.03 (0.65–1.63) | 17 | 0.88 (0.76–1.01) | 17 | 0.88 (0.76–1.01) | ||||
| Hematological cancer | 8 | 0.96 (0.78–1.17) | 6 | 0.92 (0.78–1.09) | 26 | 0.88 (0.81–0.97) | 22 | 0.88 (0.80–0.98) | ||||
| Kidney cancer | 2 | 1.01 (0.57–1.78) | 2 | 1.01 (0.57–1.78) | 9 | 0.90 (0.69–1.18) | 9 | 0.90 (0.69–1.18) | ||||
| Leukemia | - | - | - | - | 9 | 0.85 (0.74–0.98) | 9 | 0.85 (0.74–0.98) | ||||
| Liver cancer | 3 | 0.96 (0.62–1.49) | - | - | 24 | 0.57 (0.50–0.65) | 6 | 0.58 (0.46–0.74) | ||||
| Lung cancer | 9 | 0.95 (0.85–1.05) | 7 | 0.95 (0.84–1.09) | 24 | 0.87 (0.77–0.99) | 15 | 0.88 (0.75–1.03) | ||||
| Lymphoma | - | - | - | - | 16 | 0.85 (0.73–0.99) | 13 | 0.83 (0.69–0.99) | ||||
| Melanoma | 13 | 1.06 (0.90–1.25) | 9 | 0.92 (0.62–1.36) | 11 | 0.92 (0.84–1.02) | - | - | ||||
| Myeloma | - | - | - | - | 5 | 0.89 (0.53–1.51) | 5 | 0.89 (0.53–1.51) | ||||
| Pancreatic cancer | 3 | 0.99 (0.44–2.21) | 3 | 0.99 (0.44–2.21) | 17 | 0.89 (0.74–1.07) | 15 | 0.88 (0.73–1.07) | ||||
| Prostate cancer | 7 | 1.06 (0.93–1.20) | 6 | 1.06 (0.93–1.20) | 57 | 0.93 (0.88–0.98) | 27 | 0.90 (0.80–1.01) | ||||
| Non-melanoma skin cancer | 8 | 1.07 (0.86–1.33) | 7 | 1.09 (0.85–1.39) | 9 | 1.08 (1.00–1.18) | 5 | 1.11 (1.02–1.22) | ||||
RR: Relative risk; CI: Confidence interval. * Meta-analysis including largest number of individual studies.
Results of the meta-analysis can be influenced by study design. Aromataris et al. reported that the types of studies should be matched in systematic reviews, and meta-analyses to be considered for its primary objective [75]. In our study, no meta-analysis that included only RCTs showed a significant preventive effect of statin use on cancer incidence, but re-analyses of observational studies showed statistically significant findings in 11 of the 18 statin–cancer associations. Among these 11 associations, the results of the overall studies (RCTs and observational studies) were determined by those of observational studies in 10 cancers, except non-melanoma skin cancer, for which the results were determined by RCTs. The heterogeneity between overall study design and observational studies may be due to the relatively large number of observational studies included. In addition, observational studies tend to have more biases than RCTs [76], and some reports suggest that the outcomes of observed associations could be false positives or inflated if a large between-study heterogeneity is present [77,78]. However, meta-analysis of RCTs should be interpreted carefully because cancer events are not the primary endpoints of clinical trials. Besides, duration of treatment in clinical trials was relatively shorter than that in observational studies, so there may be an uncertainty of the association.
Our study has several limitations. First, we only assessed individual studies from systematic reviews and meta-analyses eligible for re-analysis, and, therefore, some very recent individual studies might have been missed. However, considering that even a very recent updated meta-analysis for one cancer missed many individual studies, even though thorough search strategy was performed using many search sites such as PubMed, Embase, Scopus, Cochrane database, etc., we think that one should also check the individual studies from previous meta-analyses when updating the meta-analysis. Second, individual studies can have biases, but assessing the quality of individual studies was beyond the scope of our review. Third, exploring the association between dose and types of statins and cancer incidence was also beyond the scope. Likewise, due to a lack of applicable data, we could not stratify the effect of statins by participant age or duration of treatment, which may be the parameter needed to evaluate the true association. Fourth, there were statistical limitations. A 95% PI and Egger p-value could not be assessed if there were only two or fewer individual studies. There were also some missing data in the largest study effect when there was no number of population data in individual studies. Finally, 95% PI, between-study heterogeneity, and publication bias may not be definitive criteria for assessing the strength of the evidence.
Nevertheless, in summary, we extensively re-analyzed meta-analyses on the associations between statin use and cancer incidence. In 10 of 18 studies there were significant relationships between statin use and cancer incidence. Although many meta-analyses of RCTs and observational studies reported significant associations between statin use and cancer incidence, only a small portion of these associations were without biases. Also, there was an individual meta-analysis reporting increased risk of cancer associated with statins use, which should be carefully interpreted by researchers and clinicians. Future studies should include more precise individual data, assessment of potential bias, and updated meta-analyses with more qualified RCTs and observational studies. We suggest that clinicians carefully consider the effects of statins on incidence of different types of cancer on the basis of the findings of our study.
Supplementary Materials
The following are available online at https://www.mdpi.com/2077-0383/8/6/819/s1, Table S1. Reanalysis of each meta-analysis on associations of the use of statin and the incidence of cancers, Table S2. PRISMA checklist
Author Contributions
G.H.J., K.H.L., J.Y.K., M.E., A.K., H.J.v.d.V., G.G., S.H.H. and J.I.S. conceived and designed the study. G.H.J. and J.I.S. acquired, collected, and analyzed the data. All authors participated in drafting the manuscript and finally approved of the version. J.I.S. is the guarantor.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Lozano R., Naghavi M., Foreman K., Lim S., Shibuya K., Aboyans V., Abraham J., Adair T., Aggarwal R., Ahn S.Y., et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torre L.A., Bray F., Siegel R.L., Ferlay J., Lortet-Tieulent J., Jemal A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 3.Baigent C., Keech A., Kearney P.M., Blackwell L., Buck G., Pollicino C., Kirby A., Sourjina T., Peto R., Collins R., et al. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–1278. doi: 10.1016/s0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 4.Hebert P.R., Gaziano J.M., Chan K.S., Hennekens C.H. Cholesterol lowering with statin drugs, risk of stroke, and total mortality. An overview of randomized trials. JAMA. 1997;278:313–321. doi: 10.1001/jama.1997.03550040069040. [DOI] [PubMed] [Google Scholar]
- 5.Nissen S.E., Tuzcu E.M., Schoenhagen P., Crowe T., Sasiela W.J., Tsai J., Orazem J., Magorien R.D., O’Shaughnessy C., Ganz P. Statin therapy, LDL cholesterol, C-reactive protein, and coronary artery disease. N. Engl. J. Med. 2005;352:29–38. doi: 10.1056/NEJMoa042000. [DOI] [PubMed] [Google Scholar]
- 6.Jain M.K., Ridker P.M. Anti-inflammatory effects of statins: Clinical evidence and basic mechanisms. Nat. Rev. Drug Discov. 2005;4:977–987. doi: 10.1038/nrd1901. [DOI] [PubMed] [Google Scholar]
- 7.Greenwood J., Steinman L., Zamvil S.S. Statin therapy and autoimmune disease: From protein prenylation to immunomodulation. Nat. Rev. Immunol. 2006;6:358–370. doi: 10.1038/nri1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khattab A.A., Ndrepepa G., Schulz S., Neumann F.J., Mehilli J., Buttner H.J., Pache J., Seyfarth M., Dirschinger J., Kastrati A., et al. Statin effect on thrombin inhibitor effectiveness during percutaneous coronary intervention: A post-hoc analysis from the ISAR-REACT 3 trial. Clin. Res. Cardiol. 2011;100:579–585. doi: 10.1007/s00392-011-0282-7. [DOI] [PubMed] [Google Scholar]
- 9.Jakobisiak M., Golab J. Potential antitumor effects of statins (Review) Int. J. Oncol. 2003;23:1055–1069. doi: 10.3892/ijo.23.4.1055. [DOI] [PubMed] [Google Scholar]
- 10.Zeichner S., Mihos C.G., Santana O. The pleiotropic effects and therapeutic potential of the hydroxy-methyl-glutaryl-CoA reductase inhibitors in malignancies: A comprehensive review. J. Cancer Res. Ther. 2012;8:176–183. doi: 10.4103/0973-1482.98967. [DOI] [PubMed] [Google Scholar]
- 11.Scandinavian Simvastatin Survival Study Group Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: The Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 12.Yokomichi H., Nagai A., Hirata M., Tamakoshi A., Kiyohara Y., Kamatani Y., Muto K., Ninomiya T., Matsuda K., Kubo M., et al. Statin use and all-cause and cancer mortality: BioBank Japan cohort. J. Epidemiol. 2017;27:S84–S91. doi: 10.1016/j.je.2016.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dale K.M., Coleman C.I., Henyan N.N., Kluger J., White C.M. Statins and cancer risk: A meta-analysis. JAMA. 2006;295:74–80. doi: 10.1001/jama.295.1.74. [DOI] [PubMed] [Google Scholar]
- 14.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gotzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Sacks H.S., Berrier J., Reitman D., Ancona-Berk V.A., Chalmers T.C. Meta-analyses of randomized controlled trials. N. Engl. J. Med. 1987;316:450–455. doi: 10.1056/NEJM198702193160806. [DOI] [PubMed] [Google Scholar]
- 16.Higgins J.P., Thompson S.G., Spiegelhalter D.J. A re-evaluation of random-effects meta-analysis. J. R. Stat. Soc. Ser. A Stat. Soc. 2009;172:137–159. doi: 10.1111/j.1467-985X.2008.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fletcher J. What is heterogeneity and is it important? BMJ. 2007;334:94–96. doi: 10.1136/bmj.39057.406644.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sterne J.A., Sutton A.J., Ioannidis J.P., Terrin N., Jones D.R., Lau J., Carpenter J., Rucker G., Harbord R.M., Schmid C.H., et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
- 20.Kyrgiou M., Kalliala I., Markozannes G., Gunter M.J., Paraskevaidis E., Gabra H., Martin-Hirsch P., Tsilidis K.K. Adiposity and cancer at major anatomical sites: Umbrella review of the literature. BMJ. 2017;356:j477. doi: 10.1136/bmj.j477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choi E.K., Park H.B., Lee K.H., Park J.H., Eisenhut M., van der Vliet H.J., Kim G., Shin J.I. Body mass index and 20 specific cancers: Re-analyses of dose-response meta-analyses of observational studies. Ann. Oncol. 2018;29:749–757. doi: 10.1093/annonc/mdx819. [DOI] [PubMed] [Google Scholar]
- 22.Jian-Yu E., Graber J.M., Lu S.E., Lin Y., Lu-Yao G., Tan X.L. Effect of Metformin and Statin Use on Survival in Pancreatic Cancer Patients: A Systematic Literature Review and Meta-analysis. Curr. Med. Chem. 2018;25:2595–2607. doi: 10.2174/0929867324666170412145232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ye X., Mneina A., Johnston J.B., Mahmud S.M. Associations between statin use and non-Hodgkin lymphoma (NHL) risk and survival: A meta-analysis. Hematol. Oncol. 2017;35:206–214. doi: 10.1002/hon.2265. [DOI] [PubMed] [Google Scholar]
- 24.Yang K., Marley A., Tang H., Song Y., Tang J.Y., Han J. Statin use and non-melanoma skin cancer risk: A meta-analysis of randomized controlled trials and observational studies. Oncotarget. 2017;8:75411–75417. doi: 10.18632/oncotarget.20034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang J., Zhu Q., Liu Q., Wang Y., Xie W., Hu L. Statin use and endometrial cancer risk: A meta-analysis. Oncotarget. 2017;8:62425–62434. doi: 10.18632/oncotarget.18658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomas T., Loke Y., Beales I.L.P. Systematic Review and Meta-analysis: Use of Statins Is Associated with a Reduced Incidence of Oesophageal Adenocarcinoma. J. Gastrointest. Cancer. 2017 doi: 10.1007/s12029-017-9983-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Islam M.M., Yang H.C., Nguyen P.A., Poly T.N., Huang C.W., Kekade S., Khalfan A.M., Debnath T., Li Y.J., Abdul S.S. Exploring association between statin use and breast cancer risk: An updated meta-analysis. Arch. Gynecol. Obstet. 2017;296:1043–1053. doi: 10.1007/s00404-017-4533-3. [DOI] [PubMed] [Google Scholar]
- 28.Zhong G.C., Liu Y., Ye Y.Y., Hao F.B., Wang K., Gong J.P. Meta-analysis of studies using statins as a reducer for primary liver cancer risk. Sci. Rep. 2016;6:26256. doi: 10.1038/srep26256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Raval A.D., Thakker D., Negi H., Vyas A., Kaur H., Salkini M.W. Association between statins and clinical outcomes among men with prostate cancer: A systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2016;19:151–162. doi: 10.1038/pcan.2015.58. [DOI] [PubMed] [Google Scholar]
- 30.Mansourian M., Haghjooy-Javanmard S., Eshraghi A., Vaseghi G., Hayatshahi A., Thomas J. Statins Use and Risk of Breast Cancer Recurrence and Death: A Systematic Review and Meta-Analysis of Observational Studies. J. Pharm. Pharm. Sci. 2016;19:72–81. doi: 10.18433/J3202B. [DOI] [PubMed] [Google Scholar]
- 31.Pradelli D., Soranna D., Zambon A., Catapano A., Mancia G., La Vecchia C., Corrao G. Statins use and the risk of all and subtype hematological malignancies: A meta-analysis of observational studies. Cancer Med. 2015;4:770–780. doi: 10.1002/cam4.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang X.L., Liu M., Qian J., Zheng J.H., Zhang X.P., Guo C.C., Geng J., Peng B., Che J.P., Wu Y. Statin use and risk of kidney cancer: A meta-analysis of observational studies and randomized trials. Br. J. Clin. Pharmacol. 2014;77:458–465. doi: 10.1111/bcp.12210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yi X., Jia W., Jin Y., Zhen S. Statin use is associated with reduced risk of haematological malignancies: Evidence from a meta-analysis. PLoS ONE. 2014;9:e87019. doi: 10.1371/journal.pone.0087019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shi M., Zheng H., Nie B., Gong W., Cui X. Statin use and risk of liver cancer: An update meta-analysis. BMJ Open. 2014;4:e005399. doi: 10.1136/bmjopen-2014-005399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ma Z., Wang W., Jin G., Chu P., Li H. Effect of statins on gastric cancer incidence: A meta-analysis of case control studies. J. Cancer Res. Ther. 2014;10:859–865. doi: 10.4103/0973-1482.138218. [DOI] [PubMed] [Google Scholar]
- 36.Lytras T., Nikolopoulos G., Bonovas S. Statins and the risk of colorectal cancer: An updated systematic review and meta-analysis of 40 studies. World J. Gastroenterol. 2014;20:1858–1870. doi: 10.3748/wjg.v20.i7.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu Y., Tang W., Wang J., Xie L., Li T., He Y., Deng Y., Peng Q., Li S., Qin X. Association between statin use and colorectal cancer risk: A meta-analysis of 42 studies. Cancer Causes Control. 2014;25:237–249. doi: 10.1007/s10552-013-0326-6. [DOI] [PubMed] [Google Scholar]
- 38.Liu Y., Qin A., Li T., Qin X., Li S. Effect of statin on risk of gynecologic cancers: A meta-analysis of observational studies and randomized controlled trials. Gynecol. Oncol. 2014;133:647–655. doi: 10.1016/j.ygyno.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 39.Zhang X.L., Geng J., Zhang X.P., Peng B., Che J.P., Yan Y., Wang G.C., Xia S.Q., Wu Y., Zheng J.H. Statin use and risk of bladder cancer: A meta-analysis. Cancer Causes Control. 2013;24:769–776. doi: 10.1007/s10552-013-0159-3. [DOI] [PubMed] [Google Scholar]
- 40.Wu X.D., Zeng K., Xue F.Q., Chen J.H., Chen Y.Q. Statins are associated with reduced risk of gastric cancer: A meta-analysis. Eur. J. Clin. Pharmacol. 2013;69:1855–1860. doi: 10.1007/s00228-013-1547-z. [DOI] [PubMed] [Google Scholar]
- 41.Wang J., Li C., Tao H., Cheng Y., Han L., Li X., Hu Y. Statin use and risk of lung cancer: A meta-analysis of observational studies and randomized controlled trials. PLoS ONE. 2013;8:e77950. doi: 10.1371/journal.pone.0077950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tan M., Song X., Zhang G., Peng A., Li X., Li M., Liu Y., Wang C. Statins and the risk of lung cancer: A meta-analysis. PLoS ONE. 2013;8:e57349. doi: 10.1371/journal.pone.0057349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Singh S., Singh P.P., Singh A.G., Murad M.H., Sanchez W. Statins are associated with a reduced risk of hepatocellular cancer: A systematic review and meta-analysis. Gastroenterology. 2013;144:323–332. doi: 10.1053/j.gastro.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 44.Singh S., Singh A.G., Singh P.P., Murad M.H., Iyer P.G. Statins are associated with reduced risk of esophageal cancer, particularly in patients with Barrett’s esophagus: A systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2013;11:620–629. doi: 10.1016/j.cgh.2012.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Singh P.P., Singh S. Statins are associated with reduced risk of gastric cancer: A systematic review and meta-analysis. Ann. Oncol. 2013;24:1721–1730. doi: 10.1093/annonc/mdt150. [DOI] [PubMed] [Google Scholar]
- 46.Scosyrev E., Tobis S., Donsky H., Wu G., Joseph J., Rashid H., Messing E. Statin use and the risk of biochemical recurrence of prostate cancer after definitive local therapy: A meta-analysis of eight cohort studies. BJU Int. 2013;111:E71–E77. doi: 10.1111/j.1464-410X.2012.11527.x. [DOI] [PubMed] [Google Scholar]
- 47.Pradelli D., Soranna D., Scotti L., Zambon A., Catapano A., Mancia G., La Vecchia C., Corrao G. Statins and primary liver cancer: A meta-analysis of observational studies. Eur. J. Cancer Prev. 2013;22:229–234. doi: 10.1097/CEJ.0b013e328358761a. [DOI] [PubMed] [Google Scholar]
- 48.Beales I.L., Hensley A., Loke Y. Reduced esophageal cancer incidence in statin users, particularly with cyclo-oxygenase inhibition. World J. Gastrointest. Pharmacol. Ther. 2013;4:69–79. doi: 10.4292/wjgpt.v4.i3.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Undela K., Srikanth V., Bansal D. Statin use and risk of breast cancer: A meta-analysis of observational studies. Breast Cancer Res. Treat. 2012;135:261–269. doi: 10.1007/s10549-012-2154-x. [DOI] [PubMed] [Google Scholar]
- 50.Mass A.Y., Agalliu I., Laze J., Lepor H. Preoperative statin therapy is not associated with biochemical recurrence after radical prostatectomy: Our experience and meta-analysis. J. Urol. 2012;188:786–791. doi: 10.1016/j.juro.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 51.Cui X., Xie Y., Chen M., Li J., Liao X., Shen J., Shi M., Li W., Zheng H., Jiang B. Statin use and risk of pancreatic cancer: A meta-analysis. Cancer Causes Control. 2012;23:1099–1111. doi: 10.1007/s10552-012-9979-9. [DOI] [PubMed] [Google Scholar]
- 52.Bansal D., Undela K., D’Cruz S., Schifano F. Statin use and risk of prostate cancer: A meta-analysis of observational studies. PLoS ONE. 2012;7:e46691. doi: 10.1371/journal.pone.0046691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alexandre L., Clark A.B., Cheong E., Lewis M.P., Hart A.R. Systematic review: Potential preventive effects of statins against oesophageal adenocarcinoma. Aliment. Pharmacol. Ther. 2012;36:301–311. doi: 10.1111/j.1365-2036.2012.05194.x. [DOI] [PubMed] [Google Scholar]
- 54.Bonovas S., Nikolopoulos G., Filioussi K., Peponi E., Bagos P., Sitaras N.M. Can statin therapy reduce the risk of melanoma? A meta-analysis of randomized controlled trials. Eur. J. Epidemiol. 2010;25:29–35. doi: 10.1007/s10654-009-9396-x. [DOI] [PubMed] [Google Scholar]
- 55.Bardou M., Barkun A., Martel M. Effect of statin therapy on colorectal cancer. Gut. 2010;59:1572–1585. doi: 10.1136/gut.2009.190900. [DOI] [PubMed] [Google Scholar]
- 56.Taylor M.L., Wells B.J., Smolak M.J. Statins and cancer: A meta-analysis of case-control studies. Eur. J. Cancer Prev. 2008;17:259–268. doi: 10.1097/CEJ.0b013e3282b721fe. [DOI] [PubMed] [Google Scholar]
- 57.Bonovas S., Filioussi K., Sitaras N.M. Statin use and the risk of prostate cancer: A metaanalysis of 6 randomized clinical trials and 13 observational studies. Int. J. Cancer. 2008;123:899–904. doi: 10.1002/ijc.23550. [DOI] [PubMed] [Google Scholar]
- 58.Bonovas S., Filioussi K., Sitaras N.M. Statins are not associated with a reduced risk of pancreatic cancer at the population level, when taken at low doses for managing hypercholesterolemia: Evidence from a meta-analysis of 12 studies. Am. J. Gastroenterol. 2008;103:2646–2651. doi: 10.1111/j.1572-0241.2008.02051.x. [DOI] [PubMed] [Google Scholar]
- 59.Bonovas S., Filioussi K., Tsantes A., Sitaras N.M. Use of statins and risk of haematological malignancies: A meta-analysis of six randomized clinical trials and eight observational studies. Br. J. Clin. Pharmacol. 2007;64:255–262. doi: 10.1111/j.1365-2125.2007.02959.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bonovas S., Filioussi K., Flordellis C.S., Sitaras N.M. Statins and the risk of colorectal cancer: A meta-analysis of 18 studies involving more than 1.5 million patients. J. Clin. Oncol. 2007;25:3462–3468. doi: 10.1200/JCO.2007.10.8936. [DOI] [PubMed] [Google Scholar]
- 61.Freeman S.R., Drake A.L., Heilig L.F., Graber M., McNealy K., Schilling L.M., Dellavalle R.P. Statins, fibrates, and melanoma risk: A systematic review and meta-analysis. J. Natl. Cancer Inst. 2006;98:1538–1546. doi: 10.1093/jnci/djj412. [DOI] [PubMed] [Google Scholar]
- 62.Bonovas S., Filioussi K., Tsavaris N., Sitaras N.M. Statins and cancer risk: A literature-based meta-analysis and meta-regression analysis of 35 randomized controlled trials. J. Clin. Oncol. 2006;24:4808–4817. doi: 10.1200/JCO.2006.06.3560. [DOI] [PubMed] [Google Scholar]
- 63.Dellavalle R.P., Drake A., Graber M., Heilig L.F., Hester E.J., Johnson K.R., McNealy K., Schilling L. Statins and fibrates for preventing melanoma. Cochrane Database Syst. Rev. 2005 doi: 10.1002/14651858.CD003697.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bonovas S., Filioussi K., Tsavaris N., Sitaras N.M. Use of statins and breast cancer: A meta-analysis of seven randomized clinical trials and nine observational studies. J. Clin. Oncol. 2005;23:8606–8612. doi: 10.1200/JCO.2005.02.7045. [DOI] [PubMed] [Google Scholar]
- 65.Berman N.G., Parker R.A. Meta-analysis: Neither quick nor easy. BMC Med. Res. Methodol. 2002;2:10. doi: 10.1186/1471-2288-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 67.Atkins D., Best D., Briss P.A., Eccles M., Falck-Ytter Y., Flottorp S., Guyatt G.H., Harbour R.T., Haugh M.C., Henry D., et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.He Y., Li X., Gasevic D., Brunt E., McLachlan F., Millenson M., Timofeeva M., Ioannidis J.P.A., Campbell H., Theodoratou E. Statins and Multiple Noncardiovascular Outcomes: Umbrella Review of Meta-analyses of Observational Studies and Randomized Controlled Trials. Ann. Intern. Med. 2018;169:543–553. doi: 10.7326/M18-0808. [DOI] [PubMed] [Google Scholar]
- 69.Markozannes G., Tzoulaki I., Karli D., Evangelou E., Ntzani E., Gunter M.J., Norat T., Ioannidis J.P., Tsilidis K.K. Diet, body size, physical activity and risk of prostate cancer: An umbrella review of the evidence. Eur. J. Cancer. 2016;69:61–69. doi: 10.1016/j.ejca.2016.09.026. [DOI] [PubMed] [Google Scholar]
- 70.Schroll J.B., Moustgaard R., Gotzsche P.C. Dealing with substantial heterogeneity in Cochrane reviews. Cross-sectional study. BMC Med. Res. Methodol. 2011;11:22. doi: 10.1186/1471-2288-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Belbasis L., Bellou V., Evangelou E., Ioannidis J.P., Tzoulaki I. Environmental risk factors and multiple sclerosis: An umbrella review of systematic reviews and meta-analyses. Lancet Neurol. 2015;14:263–273. doi: 10.1016/S1474-4422(14)70267-4. [DOI] [PubMed] [Google Scholar]
- 72.Tsilidis K.K., Kasimis J.C., Lopez D.S., Ntzani E.E., Ioannidis J.P. Type 2 diabetes and cancer: Umbrella review of meta-analyses of observational studies. BMJ. 2015;350:g7607. doi: 10.1136/bmj.g7607. [DOI] [PubMed] [Google Scholar]
- 73.Siontis K.C., Hernandez-Boussard T., Ioannidis J.P. Overlapping meta-analyses on the same topic: Survey of published studies. BMJ. 2013;347:f4501. doi: 10.1136/bmj.f4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ioannidis J.P. Integration of evidence from multiple meta-analyses: A primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ. 2009;181:488–493. doi: 10.1503/cmaj.081086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Aromataris E., Fernandez R., Godfrey C.M., Holly C., Khalil H., Tungpunkom P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Based Healthc. 2015;13:132–140. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 76.Ioannidis J.P. Contradicted and initially stronger effects in highly cited clinical research. JAMA. 2005;294:218–228. doi: 10.1001/jama.294.2.218. [DOI] [PubMed] [Google Scholar]
- 77.Ioannidis J.P. Why most discovered true associations are inflated. Epidemiology. 2008;19:640–648. doi: 10.1097/EDE.0b013e31818131e7. [DOI] [PubMed] [Google Scholar]
- 78.Ioannidis J.P. Why most published research findings are false. PLoS Med. 2005;2:e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.