Abstract
Rationale:
The management of complete obstruction of anastomosis following colorectal surgery is challenging. Some modified minimally invasive methods have been reported to be successfully implemented in some cases. In this case report, we present a case to share our experience.
Patient concerns:
A 64-year-old man underwent low anterior resection and single barrel ileostomy for rectal cancer 5 months ago. Completely obstructed anastomotic stenosis was found during colonoscopy.
Diagnosis:
Colonoscopy showed the anastomosis at 8 cm from the anal verge was completely obstructed.
Interventions:
A small incision was made by a needle knife, and then the stenosis was sequentially dilated by using a wire-guided balloon dilator.
Outcomes:
The luminal continuity was reestablished. The patient underwent successful ileostomy closure 2 months later. At 18-months follow-up, no restenosis of the anastomosis was observed during colonoscopy.
Lessons:
Endoscopic small incision with a needle knife along with balloon dilation could be an alternative method for patients with complete obstruction of anastomosis after colorectal resection. But this procedure should be performed with great caution in selected patients and performed only by highly experienced endoscopists.
Keywords: anastomosis, balloon dilation, colorectal, endoscopy, needle knife
1. Introduction
Anastomotic stenosis after colorectal surgery is a well-known postsurgical complication with an incidence ranging from 3% to 30%,[1] resulting in troublesome stool passage. Consequently, patients may develop clinical symptoms, with signs of intestinal obstruction, seriously affecting their quality of life. The causes of anastomotic stenosis are remained not fully understood. But various factors, such as tissue ischemia, anastomotic leakage, inflammation, and radiotherapy have been cited in its pathogenesis.[2–5] Treatment mainly aims at reestablishment of luminal continuity, including conservative therapy, surgical revision, endoscopic balloon dilation, and placement of self-expandable metal stents.[6] The most widely used technique is endoscopic balloon dilation.
Complete obstruction of anastomosis is considered rare but has been described in certain patients.[7] Endoscopic balloon dilation for this condition is technically difficult because the inability to across the obstructed segment. Surgical revision is feasible but higher morbidity rate has been reported.[7,8] Therefore, modified minimally invasive therapy is an attractive idea for this condition, and has been reported to be successfully implemented in some cases.[9–13] Here, we present a case with complete obstruction of anastomosis after colorectal resection, which was successfully treated with the combination of endoscopic incision and balloon dilation.
2. Case report
A 64-year-old man with rectal cancer underwent low anterior resection and single barrel ileostomy. Five months after the procedure, he returned for the ileostomy takedown. Colonoscopy was performed as a preoperative evaluation, showing that the anastomosis at 8 cm from the anal verge was completely obstructed (Fig. 1). Traditional endoscopic therapy was ruled out because no orifice was detected at the anastomotic site. Surgical revision was recommended, but the patient preferred a minimally invasive approach. Therefore, a combination of endoscopic incision and balloon dilation was attempted under direct visualization, which was finally successfully performed. Because a prior single barrel ileostomy was conducted, resulting in the impossibility of approaching from the other side of the anastomosis. Thus, we carefully made a small incision with a needle knife (KD-1L, Olympus Optical Co, Japan) at the expected position of the lumen (Fig. 2, A, B). Then the stenosis was sequentially dilated to a maximum diameter of 18 mm for about 3 minutes by using a wire-guided balloon dilator (M00558430, Boston Scientific Co) through the biopsy channel of the colonoscope (CF-260AI, Olympus Optical Co, Japan) (Fig. 2, C, D). After removing the dilator, the colonoscope could be easily passed through the anastomosis. The luminal continuity was finally reestablished (Fig. 3A). During and after the procedure, no major bleeding or perforation was noted. Two months later, the patient underwent successful ileostomy closure, and then he started passing stool per rectum. At 18-months follow-up, no restenosis of the anastomosis was observed during colonoscopy (Fig. 3B).
Figure 1.
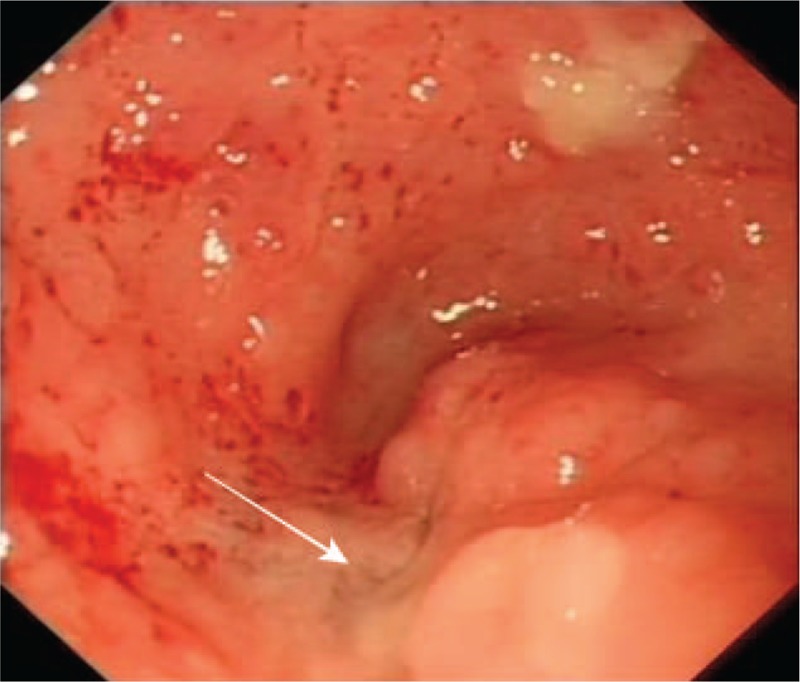
A completely obstructed anastomosis at 8 cm from the anal verge was identified. The expected position of the lumen was shown by white arrow.
Figure 2.
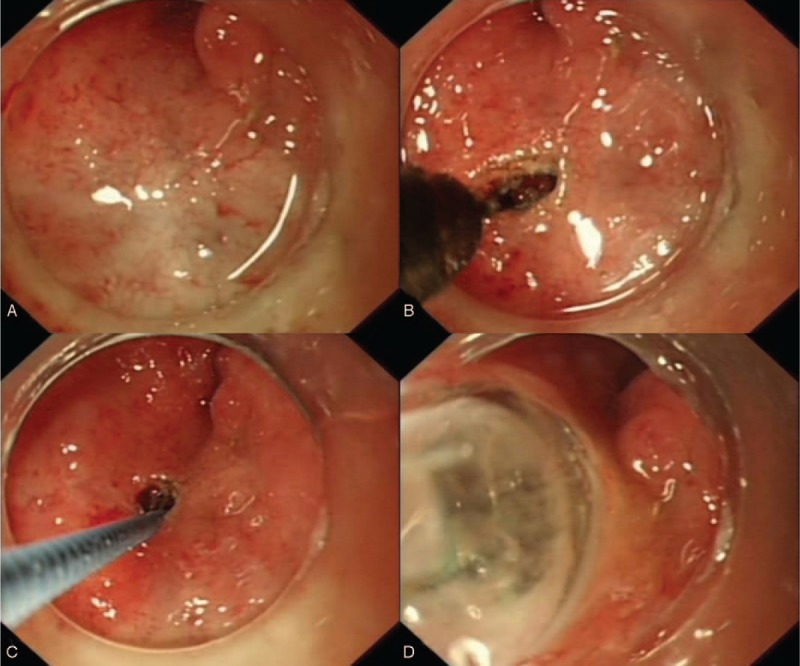
(A) Endoscopic view of the expected position of the lumen. (B) A small incision was made by using a needle knife. (C) A guidewire was passed through the small incision. (D) The stenosis was sequentially dilated to a maximum diameter of 18 mm.
Figure 3.
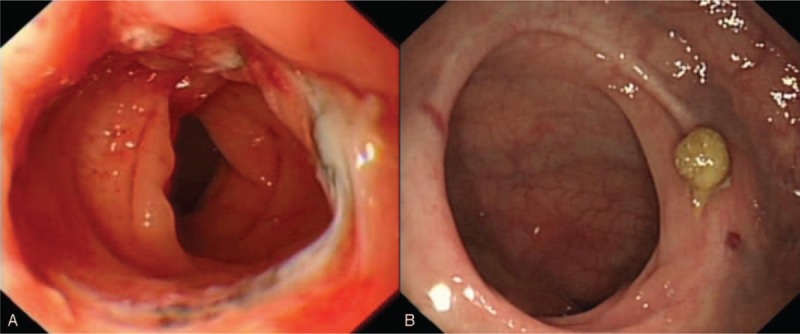
(A) The luminal continuity was reestablished after dilation. (B) No restenosis of the anastomosis was observed at 18 months after treatment.
3. Discussion
Anastomotic stenosis following low anterior resection is usually treated conservatively, by digital or by endoscopic balloon dilation.[14] Direct digital dilation is useful if the stenosis is located in the lower rectum. Endoscopic balloon dilation is the preferred method for the remaining patients who cannot undergo digital dilation.[15] However, completely obstructed anastomotic stenosis is nontraversable to traditional techniques and normally requires surgical intervention. But surgical treatment may be associated with perioperative and postoperative complications. Therefore, surgery should be avoided as far as possible.
There have been a few reports of modified minimally invasive therapy for treating patients with completely obstructed anastomotic stenosis. Kaushik et al [9] showed an endoscopic rendezvous technique, combining antegrade and retrograde endoscopy to facilitate dilation. The similar technique called computed tomography-guided endoscopic rendezvous technique was also reported.[13] These techniques require a complicated procedure involving 2 endoscopes, and there are unsuitable for patients who underwent single barrel ileostomy. A prototype front-view and forward array echoendoscope have been reported, but it was not a ubiquitous device.[10] Other methods included Artifon catheter puncture before balloon dilation and blunt penetration technique, which were both performed under fluoroscopy.[11,12]
In this case, considering endoscopic balloon dilation is a valid and safe method for the management of colorectal anastomotic stenosis, and single electrocautery incision may cause scar contraction and it is associated with high risk of perforation or bleeding,[16] so we made a small incision with a needle knife under direct visualization, and then performed balloon dilation. The advantage of this procedure is that it is simple and quick, but the implementation of this technique is challenging. Nonsurgical therapy for completely obstructed anastomotic stenosis is performed usually under fluoroscopic guidance. However, we performed this technique under direct visualization. Thus, the location of lumen must be precisely identified, avoiding serious complications such as bleeding or perforation caused by the needle knife being pushed through the wrong direction. According to our experience, some suggested methods used for the accurate identification of the luminal position are as follows: if the anastomosis with intact staples is observed during the procedure, the position may be located between the staples. The position may also be located at the previous stapled linear scar that is different in color from normal mucosal tissue. During the procedure, the endoscopist should always anticipate bleeding or perforation and be prepared as it occurs. The alternative plan, such as surgery should be available whenever necessary. It should also be noted that the success of this procedure depends on many factors, the precise luminal position, and the most important is that this procedure should be performed only by highly experienced endoscopists.
In conclusion, for cases with such completely obstructed anastomotic stenosis following colorectal resection, endoscopic small incision with a needle knife along with balloon dilation could be an alternative method. But this procedure should be performed with great caution in selected patients, whose luminal location must be precisely identified, and performed only by highly experienced endoscopists.
Author contributions
Supervision: Bing Hu.
Writing – original draft: Xianglei Yuan, Wei Liu.
Writing – review & editing: Liansong Ye, Mengjuan Wu, Bing Hu.
Footnotes
We acknowledge the funding support from Sichuan Province Science and Technology Department (China) (2017SZ0009).
Informed written consent was obtained from the patient for publication of this case report and accompanying images.
The authors have no conflicts of interest to disclose.
References
- [1].Hiranyakas A, Da Silva G, Denoya P, et al. Colorectal anastomotic stricture: is it associated with inadequate colonic mobilization. Tech Coloproctol 2013;17:371–5. [DOI] [PubMed] [Google Scholar]
- [2].Suchan KL, Muldner A, Manegold BC. Endoscopic treatment of postoperative colorectal anastomotic strictures. Surg Endosc 2003;17:1110–3. [DOI] [PubMed] [Google Scholar]
- [3].Bannura GC, Cumsille MA, Barrera AE, et al. Predictive factors of stenosis after stapled colorectal anastomosis: prospective analysis of 179 consecutive patients. World J Surg 2004;28:921–5. [DOI] [PubMed] [Google Scholar]
- [4].Schlegel RD, Dehni N, Parc R, et al. Results of reoperations in colorectal anastomotic strictures. Dis Colon Rectum 2001;44:1464–8. [DOI] [PubMed] [Google Scholar]
- [5].Lim M, Akhtar S, Sasapu K, et al. Clinical and subclinical leaks after low colorectal anastomosis: a clinical and radiologic study. Dis Colon Rectum 2006;49:1611–9. [DOI] [PubMed] [Google Scholar]
- [6].Repici A, Pagano N, Rando G, et al. A retrospective analysis of early and late outcome of biodegradable stent placement in the management of refractory anastomotic colorectal strictures. Surg Endosc 2013;27:2487–91. [DOI] [PubMed] [Google Scholar]
- [7].Lefevre JH, Bretagnol F, Maggiori L, et al. Redo surgery for failed colorectal or coloanal anastomosis: a valuable surgical challenge. Surgery 2011;149:65–71. [DOI] [PubMed] [Google Scholar]
- [8].Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kaushik N, Rubin J, McGrath K. Treatment of benign complete colonic anastomotic obstruction by using an endoscopic rendezvous technique. Gastrointest Endosc 2006;63:727–30. [DOI] [PubMed] [Google Scholar]
- [10].De Lusong MA, Shah JN, Soetikno R, et al. Treatment of a completely obstructed colonic anastomotic stricture by using a prototype forward-array echoendoscope and facilitated by SpyGlass (with videos). Gastrointest Endosc 2008;68:988–92. [DOI] [PubMed] [Google Scholar]
- [11].Curcio G, Spada M, di Francesco F, et al. Completely obstructed colorectal anastomosis: a new non-electrosurgical endoscopic approach before balloon dilatation. World J Gastroenterol 2010;16:4751–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Yazawa K, Morioka D, Matsumoto C, et al. Blunt penetration technique for treatment of a completely obstructed anastomosis after rectal resection: a case report. J Med Case Rep 2014;8:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Albertsmeier M, Rittler P, Hoffmann RT, et al. Treatment of a completely obstructed colonic anastomotic stricture using a CT-guided endoscopic rendezvous technique. Endoscopy 2011;43:E5–6. [DOI] [PubMed] [Google Scholar]
- [14].Bong JW, Lim SB. Transanal minimally invasive surgery as a treatment option for a completely occluded anastomosis after low anterior resection: a new approach to severe anastomotic stenosis. Asian J Endosc Surg 2019;12:175–7. [DOI] [PubMed] [Google Scholar]
- [15].Mukai M, Kishima K, Iizuka S, et al. Endoscopic hook knife cutting before balloon dilatation of a severe anastomotic stricture after rectal cancer resection. Endoscopy 2009;41:E193–4. [DOI] [PubMed] [Google Scholar]
- [16].Hagiwara A, Sakakura C, Shirasu M, et al. Sigmoidofiberscopic incision plus balloon dilatation for anastomotic cicatricial stricture after anterior resection of the rectum. World J Surg 1999;23:717–20. [DOI] [PubMed] [Google Scholar]


