Abstract
High altitude is a natural laboratory, within which the clinical study of human physiological response to hypobaric hypoxia (HH) is possible. Failure in the response results in progressive hypoxemia, inflammation and increased tissue oxidative stress (OxS). Thus, investigating temporal changes in key transcription factors (TFs) HIF-1α, HIF-2α, NF-κB and NRF2 mRNA levels, relative to OxS and inflammatory markers, may reveal molecular targets which contrast deleterious effects of hypoxia. Biological samples and clinical data from 15 healthy participants were collected at baseline and after rapid, passive ascent to 3830 m (24 h and 72 h). Gene expression was assessed by qPCR and ROS generation was determined by EPR spectroscopy. Oxidative damage and cytokine levels were estimated by immuno or enzymatic methods. Hypoxia transiently enhanced HIF-1α mRNA levels over time reaching a peak after 24 h. Whereas, HIF-2α and NRF2 mRNA levels increased over time. In contrast, the NF-κB mRNA levels remained unchanged. Plasma levels of IL-1β and IL-6 also remained within normal ranges. ROS production rate and markers of OxS damage were significantly increased over time. The analysis of TF-gene expression suggests that HIF-1α is a lead TF during sub-acute HH exposure. The prolongation of the HH exposure led to a switch between HIF-1α and HIF-2α/NRF2, suggesting the activation of new pathways. These results provide new insights regarding the temporal regulation of TFs, inflammatory state, and ROS homeostasis involved in human hypoxic response, potentially also relevant to the mediation of diseases that induce a hypoxic state.
Subject terms: Transcription, Biomarkers
Introduction
The human response to hypoxia is multifactorial involving the complex synergy of hematopoietic, respiratory and cardiovascular systems to maintain adequate tissue oxygenation; failure in the response results in progressive hypoxemia, inflammation and increased tissue oxidative stress (OxS)1. Specifically, cellular hypoxia is known to be both a primary homeostatic moderator as well as fundamental mechanism of injury in the pathogenesis of acute diseases, but also of chronic disorders such as: atherosclerosis, arthritis, obstructive sleep apnea syndrome (OSAS) and other cardiovascular, cerebrovascular and neurodegenerative diseases2–5. Cellular hypoxia is associated with the activation of a transcriptionally initiated response, mediated primarily by members of the hypoxia inducible factor (HIF) family (HIF-1α, HIF-2α and HIF-3α)6, and partially dependent on the accumulation of reactive oxygen species (ROS)7. Cellular oxygen sensitivity is achieved by two classes of enzymes, collectively termed HIF-hydroxylases (prolyl hydroxylases (PHD1–3)), also known as EGLN1–3 and factor inhibiting HIF (FIH). The regulation of HIF α-subunit protein stability is mainly achieved by oxygen-dependent posttranslational hydroxylation of conserved proline and asparagine residues. Under hypoxic conditions, these hydroxylation events are inhibited, leading to HIF-α protein accumulation and translocation to the nucleus. Subsequently, these HIF-α proteins will form a functional transcriptional complex that recognize the hypoxia response elements (HRE) elements of target genes8. HIF activation increases the expression of a number of genes, encoding proteins directed toward increasing tissue perfusion and oxygenation status, thus overcoming the initial hypoxic insult9. Since the 1990s10,11, previous research has shown that HIFs modulate the transcriptional response to hypoxia under both physiological and pathological conditions. This includes the expression of approximately 1000 genes that are broadly involved in the coordination of hypoxic adaptation; including those regulating metabolism, blood-vessel growth, cell division, inflammation and OxS response12,13.
However, the cellular response to hypoxia does not solely rely on members of the HIF family; other transcription factors (TF) are known to encode an extensive transcriptional program in response to a hypoxic stimulus14. Specifically, activation of nuclear factor kappa B (NF-κB) and nuclear factor (erythroid-derived 2)-like 2 (NRF2) are considered key regulating factors involved in the preservation of homeostasis in tissue and organs, attenuating oxidative damage, inflammation and modulating cellular adaptation. NF-κB and HIFs are considered the main players in inflammatory and innate immune responses with pro-or anti-inflammatory activity depending on which cell type is analyzed15–19. In particular, HIF-1α is widely expressed and is detected virtually in all innate and adaptive immune populations including macrophages, neutrophils, dendritic cells, and lymphocytes. Both NF-κB and HIF-1α could be considered master regulators of inflammatory gene expression involved in several relevant medical pathologies20. Conversely, NRF2 is the main TF involved in redox homeostasis and regulates a coordinated induction of anti-oxidant, and anti-inflammatory genes in response to OxS and inflammation21–23. It is clear that an extensive level of crosstalk between different TFs exists in response to a hypoxic insult, including a relationship between HIFs and NF-κB19,20, as well as NRF2 and NF-κB24. However, the timing and functional consequence of this concomitant induction of differing TFs during prolonged hypoxic exposure remains unclear.
Genomic studies have predominantly used cell culture and animal models to describe how exposure to hypoxia induces specific gene responses, as well as possible relationships between differing transcription factors12,25–27. However, the complex relationships between different TFs, also in relation to systemic effects of hypoxemia in humans in vivo, have not been fully elucidated yet. The decrease of partial pressure of oxygen with increasing altitude offers a unique experimental setting to investigate the cellular response to hypoxia in vivo28. In addition, white blood cells (WBC) have been recognized to be a viable in vivo model to investigate both continuous and intermittent hypoxia, inflammation and OxS in healthy humans29,30 and patients with cardiovascular diseases such as OSAS31,32.
We have hypothesized that acute hypobaric hypoxia (HH) exposure causes both increased inflammation and OxS, even in those subjects considered healthy, i.e. not exhibiting symptomology associated with altitude pathophysiology1. The proposition being that despite this collective initial increase in inflammatory and OxS response on immediate HH exposure, there exists a semi-concomitant activation of both anti-inflammatory and anti-OxS responses, differentially mediated by specific TFs depending on the duration of exposure ((i.e. sub-acute (≤24 h) or prolonged (72 h)). Specifically, we have investigated those molecular responses considered to monitor the expression pattern of the master cellular reprogramming transcription factors HIF-1α, HIF-2α, NF-κB (p65 subunit) and NRF2, both before and during sub-acute to prolonged HH exposure in healthy participants. Furthermore, we have compared the expression pattern among those aforementioned TFs, as well as pro-inflammatory cytokines (IL-1β and IL-6), ROS production and OxS biomarkers (for DNA, lipid and protein peroxidation damage) over a 3-day exposure to HH equivalent to 3830 m. Due to a lack of clear consensus within the literature, we also chose to investigate the plasma levels of pro-inflammatory cytokines (IL-1β and IL-6). Previously described to increase under hypoxic conditions33–35, other publications have refuted this proposition, describing any hypoxia induced elevation of circulating pro-inflammatory cytokines as non-significant in healthy individuals36,37. Conversely, there is striking evidence that IL-6 may even be involved in hypoxia-induced lung inflammation and pulmonary vascular remodeling and then with the occurrence of specific high-altitude disease states38. Thus, further highlighting the necessity to investigate the temporal influence of HH exposure on IL-6 expression and IL-1β, which is not only proven to stimulate the synthesis of IL-6, but has also been identified generally as a critical mediator of tissue inflammation39,40. This study gives a unique insight into regulatory processes governing the early phase of hypoxic response in relation to inflammation and OxS in humans in vivo, as well as providing new knowledge specific to the molecular regulation of HIFs, and other master TFs, in a cellular population also implied in the pathogenesis of several cardiovascular diseases.
Results
Clinical parameters tested are indicative of physiological response during exposure to HH
A detailed overview of clinical parameters at baseline (BL), 24 h and 72 h is shown in Table 1. After direct ascent to high altitude, peripheral oxygen saturation (SpO2) showed a significant modification over time (ANOVA P < 0.001) with a reduction at 24 h (−11%, P < 0.001) and a progressive increase between 24 h and 72 h (+5%, P = 0.001). SpO2 did not return to the baseline values for any participant during stay at 3800 m. The heart rate (HR) increased from baseline values up until 24 h (+35%, P < 0.001), then HR decreased (−10%, P < 0.24), remaining higher compared to baseline (+21%, P < 0.006). Similarly, the breath rate (BR) enhanced within 24 h and after 72 h compared to baseline values (respectively +22%, P = 0.01 and +19%, P = 0.02). All the subjects included in data analysis had a value of Lake Louise Score (LLS) < 3 during three days of exposure to high-altitude hypoxia.
Table 1.
The marked effects on human physiology of hypobaric hypoxia exposure over time is showed by the significative modification of blood capillary values SpO2 (peripheral capillary oxygen saturation) and clinical parameters such as Heart Rate (HR) and Breath Rate (BR).
| BL (n = 15) | 24 h (n = 14) | 72 h (n = 14) | Repeated measures ANOVA P | P after Bonferroni correction | |||
|---|---|---|---|---|---|---|---|
| Mean | Mean | Mean | 24 h vs. BL | 72 h vs. BL | 24 h vs 72h | ||
| SpO2, % | 98.93 ± 1.17 | 87.67 ± 3.48 | 91.71 ± 2.13 | <0.001 | <0.001 | <0.001 | 0.001 |
| HR, bpm | 61.53 ± 7.99 | 83.07 ± 10.6 | 74.57 ± 13.69 | <0.001 | <0.001 | 0.01 | 0.24 |
| BR*, rpm | 13 ± 2.42 | 15.86 ± 3.01 | 15.44* ± 3.57 | <0.001 | 0.01 | 0.02 | 0.87 |
| LLS | 0 ± 0 | 0.60 ± 0.74 | 0.36 ± 0.50 | 0.23 | 0.11 | 0.25 | 1 |
Only the BR seems to be less sensitive to hypoxia and its variations at specific time points are only marginally significant. Values are means ± SD. *BR was evaluated in 9 subjects.
Exposure to HH results in differential expression of key TFs in human WBCs that is also time exposition related
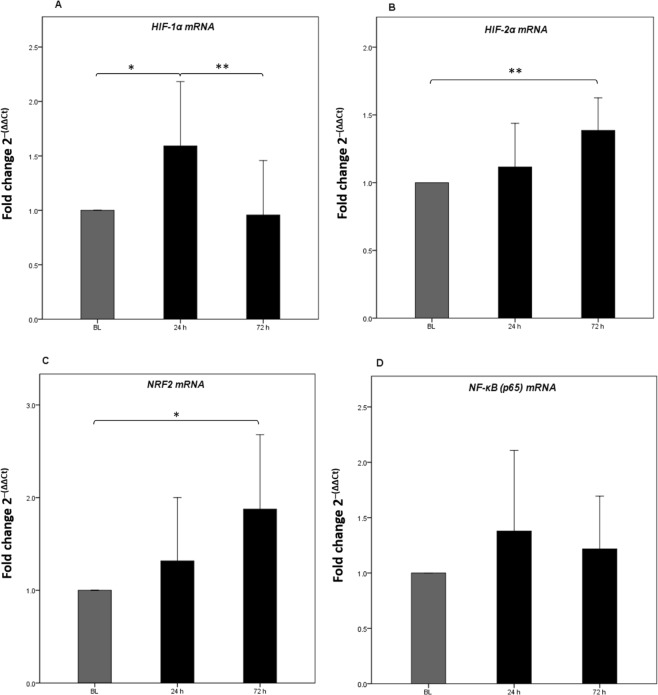
Gene expression of different TFs (HIF-1α, HIF-2α, NRF2 and p65 subunit of NF-κB) were determined at baseline (262 m) and after 24 h and 72 h of high altitude exposure (3830 m). HIF-1α mRNA levels presented a parabolic relationship with time of exposure (72 h) to HH (ANOVA P = 0.001). Specifically, HIF-1α mRNA levels increased significantly after 24 h (+59%, P = 0.01) of hypoxic exposure, and subsequently returned to values comparable to baseline levels after 72 h (Supplementary Table S1 and Fig. 1A). HIF-2α mRNA levels consistently increased over time (ANOVA P = 0.001), reaching a peak after 72 h of exposure (+41%, P < 0.001) (Supplementary Table S1 and Fig. 1B). Similarly, the NRF2 mRNA level increased constantly during hypoxic exposure (ANOVA P = 0.04), reaching a peak after 72 h (+87%, P < 0.001) (Supplementary Table S1 and Fig. 1C). Finally, in comparison to baseline values, p65 mRNA levels were not significantly different after either 24 h or 72 h of high altitude exposure (ANOVA P = 0.71) (Supplementary Table S1 and Fig. 1D).
Figure 1.
The relative quantification of mRNA levels for Transcription Factors HIF-1α, HIF-2α, NRF2 and NF-κB (p65) in white blood cells reveal that a hypobaric hypoxia stimulus inducts different TF expression patterns that is time dependent. (A) HIF-1α shows a transcription peak within 24 h, while HIF-2α (B) and NRF2 (C) show an expression peak after 72 h after the beginning of the stimulus. On the contrary, the NF-κB gene doesn’t show differences in its expression during the study (D). RQ was calculated as fold change using the 2−(ΔΔCt) method. The results of mRNA are the average of the values assessed after three reaction tests. Values are mean ± SD. *P < 0.05 and **P < 0.001 after Bonferroni correction.
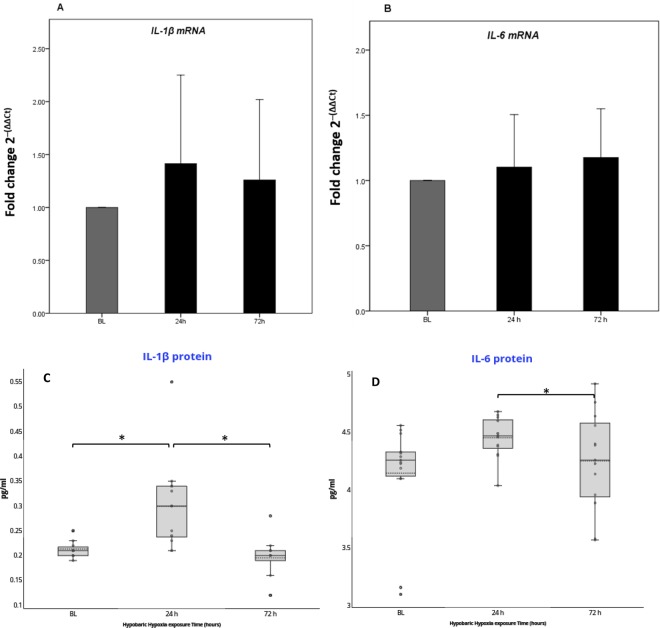
Direct measurement of circulating pro-inflammatory cytokines during prolonged HH exposure indicate swift mediation of inflammatory state in HA responders
Gene expression analysis of pro-inflammatory markers (IL-1β and IL-6) were determined at baseline (262 m) and after 24 h and 72 h of high altitude exposure (3830 m). IL-1β and IL-6 mRNA levels were not significantly modified during the 72 h period (ANOVA P = 0.65 and ANOVA P = 0.60 respectively) in WBCs (Supplementary Table S1 and Fig. 2A,B). On the contrary, IL-1β plasma levels significantly changed over time (ANOVA P = 0.001). Specifically, IL-1β plasma levels increased after 24 h (+25%, P < 0.02), and returned to baseline after 72 h (−2%, P = 0.77) (Supplementary Table S2 and Fig. 2C). IL-6 plasma levels did not significantly changed over time (ANOVA P = 0.07) (Supplementary Table S2 and Fig. 2D). However, we observed a significant reduction of IL-6 at 72 h of high altitude exposure, in comparison to values reported after 24 h (−5%, P = 0.04) (Supplementary Table S2 and Fig. 2D). Both plasma levels of IL-1β and IL-6 were considered in the normal range for the general population throughout the entire study period41,42. Within 24 h of exposure, 2 participants received a single dose of Paracetamol (500 mg). The adjustment of results for the use of paracetamol was performed, and no significant modifications were obtained (data not shown).
Figure 2.
Relative quantification of mRNA levels and protein plasma levels for pro-inflammatory cytokines in white blood cells reveal a slight increase in inflammatory state during HH exposure. (A,B) IL-1β and IL-6 mRNA quantification don’t reveal significant variation in mRNA production for both cytokines during hypoxia stimulus over time. The results of mRNA are the average of the values assessed after three reaction tests. Relative quantification of mRNA expression for pro-inflammatory cytokines was calculated as fold change using the 2−(ΔΔCt) method. Values are mean ± SD. (C,D) Only IL-1β circulating protein showed a slight transient increase after 24 h of HH exposure. The absolute values for both circulating proteins are in the normal range for general population. The median (continuous band) and the mean (dotted band) are represented inside the boxes. *P < 0.05 after Bonferroni correction.
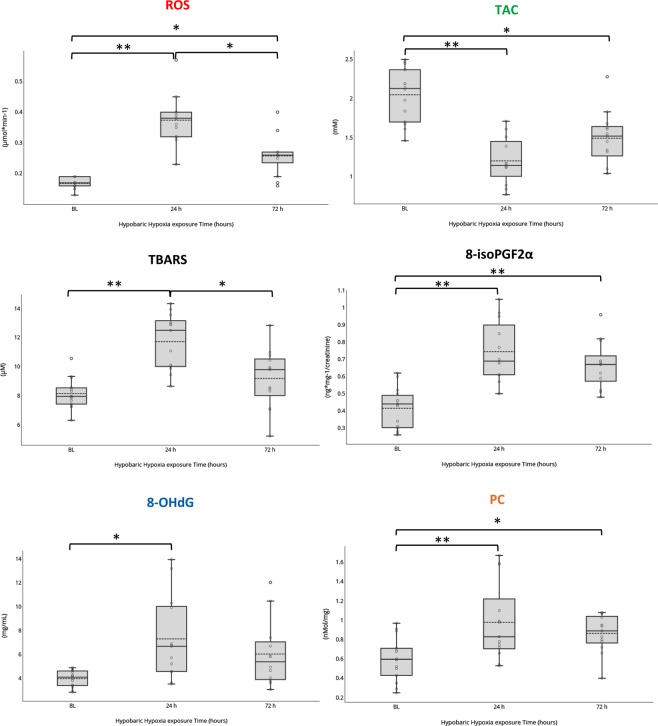
Direct 24 h exposure to HH induces marked increases in ROS, TBARS, 8-isoPGFα, 8-OHdG, PC and concomitant reduction in TAC
To determine biomarkers of oxidative stress at baseline and during high altitude exposure, we measured the levels of ROS production, TBARS (Thiobarbituric acid reactive substances, markers of lipid peroxidation), 8-isoprostanes (8-isoPGF2α, lipid oxidation products and potential disease mediators), 8-hydroxy-2′ -deoxyguanosine (8-OHdG, products of DNA oxidation), PC concentrations (protein oxidative carbonylation) and TAC (total antioxidant capacity, the sum of aqueous and lipid soluble low-molecular weight antioxidants) for the whole cohort (Supplementary Table S3). OxS biomarkers levels at baseline (262 m) were in agreement with previous values estimated for a healthy population43. The basal level values for 8-isoPGF2α and 8-OHdG considered for statistical analysis were obtained from a matching group of the general population.
Sub-acute HH exposure (24 h), led to changes in indices of OxS; namely: increased levels of ROS production as detected by EPR, TBARS, 8-isoPGF2α, 8-OHdG, PC, plus a decrease in total antioxidant capacity (TAC). Changes were detectable and reached a peak of +218% (ROS), +70% (TBARS), +54% (8-isoPGF2α) and +61% (PC) after 24 h (P < 0.001, P < 0.001, P = 0.001, P < 0.001 respectively) compared to baseline (Supplementary Table S3 and Fig. 3). Levels of 8-OHdG marker of DNA damages peaked after 24 h (+178%); the change was only slightly significant (P = 0.024) compared to BL. TAC values showed an exactly opposite pattern over time (ANOVA P < 0.001) with the lowest level of −60% after 24 h (P < 0.001) (Supplementary Table S3 and Fig. 3) and no restoring of the basal levels of antioxidant activity after the 72 h period of exposure (−25%, P = 0.001). Additionally, ROS production rate, TBARS, 8-isoPGF2α, 8-OHdG and PC concentrations significantly changed over time of exposure to HH within 72 h (ANOVA P < 0.001, P < 0.001, P = 0.002, P = 0.011, and P < 0.001 respectively) (Supplementary Table S3 and Fig. 3).
Figure 3.
Box and Whisker plots show the marked effects of hypobaric hypoxia exposure (3830 m) on ROS production and relative biomarkers of oxidative damage. Direct 24 h exposure to HH induces marked increases in ROS, TBARS, 8-isoPGF α, 8-OHdG, PC and concomitant reduction in TAC. After 72 h of exposure to hypoxia there is a partial recover of the basal conditions with a slight improve of the TAC and a reduction of ROS and cellular damages amounts. The median (continuous band) and the mean (dotted band) are represented inside the boxes. *P < 0.05 and **P < 0.001 after Bonferroni correction.
Correlation among TFs gene expression, inflammatory and oxidative markers and clinical variables
We chose to perform a correlation analysis in order to investigate the tendency to show a coordinated expression among TFs, other studied genes (i.e. IL-1β and IL-6) related to OxS and inflammatory circulating markers (i.e. IL-1β and IL-6), over time. In particular, the correlation analysis was chosen to provide information pertaining to which biological processes were interconnected and which displayed interdependence. The main aim was to identify which potential interactions may be of mechanistic importance in the early phase of human response to hypobaric hypoxic exposure.
Clinical variables showed a strong correlation with ROS and TAC but not with TFs and inflammation markers
SpO2 showed strong correlations with both ROS production (ANOVA r = −0.76, P < 0.001) and TAC (ANOVA r = +0.82, P < 0.001) over time (Table 2). TAC and ROS were also correlated (ANOVA r = −0.66, P < 0.001) (Table 2 and Supplementary Fig. S1).
Table 2.
SpO2 showed a strong correlation with ROS and TAC but a weak correlation with TFs and inflammation markers.
| correlation with | Clinic. | Transcritpion Factors | Oxidative stress | Inflammatory state | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SpO2 | HIF-1α | HIF-2α | NF-κB | NRF2 | ROS | TAC | IL-1β | IL-6 | IL-1β protein | IL-6 protein | ||||||||||||
| r | P | r | P | r | P | r | P | r | P | r | P | r | P | r | P | r | P | r | P | r | P | |
| SpO2 | — | |||||||||||||||||||||
| HIF-1α | −0.41 | 0.03 | — | |||||||||||||||||||
| HIF-2α | −0.33 | 0.09 | −0.19 | 0.34 | — | |||||||||||||||||
| NF-κB | −0.47 | 0.01 | 0.31 | 0.12 | 0.14 | 0.49 | — | |||||||||||||||
| NRF2 | −0.42 | 0.03 | −0.29 | 0.15 | 0.58 | 0.002 | 0.30 | 0.13 | — | |||||||||||||
| ROS | −0.76 | < 0.001 | 0.62 | < 0.001 | 0.15 | 0.46 | 0.46 | 0.02 | 0.15 | 0.45 | — | |||||||||||
| TAC | 0.82 | < 0.001 | −0.37 | 0.07 | −0.24 | 0.25 | −0.59 | 0.002 | −0.43 | 0.03 | −0.66 | < 0.001 | — | |||||||||
| IL-1β | −0.37 | 0.06 | 0.08 | 0.69 | 0.34 | 0.08 | 0.29 | 0.14 | 0.30 | 0.12 | 0.36 | 0.07 | −0.32 | 0.12 | — | |||||||
| IL-6 | −0.10 | 0.63 | 0.10 | 0.61 | 0.46 | 0.02 | 0.16 | 0.43 | 0.15 | 0.45 | 0.32 | 0.11 | −0.03 | 0.89 | 0.40 | 0.04 | — | |||||
| IL-1β protein | −0.46 | 0.02 | 0.38 | 0.06 | −0.13 | 0.52 | 0.49 | 0.01 | −0.02 | 0.92 | 0.47 | 0.02 | −0.35 | 0.08 | 0.32 | 0.12 | −0.06 | 0.76 | — | |||
| IL-6 protein | −0.44 | 0.02 | 0.26 | 0.21 | 0.21 | 0.32 | 0.47 | 0.02 | 0.17 | 0.43 | 0.34 | 0.09 | −0.47 | 0.02 | 0.18 | 0.40 | −0.04 | 0.84 | 0.37 | 0.05 | — | |
Additionally, the TFs showed a differential correlation with both OxS markers and inflammatory variables. In particular, HIF-1α mRNA was correlated with ROS over time, as well as HIF-2α with NRF2. All P-values were two sided, and differences were considered significant at P < 0.01; 0.01 < P < 0.05 were considered only marginally significant.
SpO2 showed a negative but marginally significant correlation with three out of four TFs investigated (HIF-1α, NF-κB and NRF2) (ANOVA r = −0.41, P = 0.03; ANOVA r = −0.47, P = 0.01 and ANOVA r = −0.42, P = 0.03 respectively).
SpO2 showed a marginally significant correlation with IL-1β and IL-6 protein levels in plasma (ANOVA r = −0.46, P = 0.02; ANOVA r = −0.44, P = 0.02). IL-1β and IL-6 protein concentrations showed a marginal significant correlation with ROS (ANOVA r = +0.47, P = 0.02 and r = +0.34, P = 0.09 respectively) and TAC (ANOVA r = −0.35, P = 0.08 and r = −0.47, P = 0.02 respectively) over time. Only a marginal significant correlation was identified between IL-1β mRNA and IL-6 mRNA (ANOVA r = +0.40, P = 0.04) levels in WBCs. On the contrary no correlations were observed between the mRNA of the two investigated interleukins and their protein concentrations in plasma (ANOVA r = +0.32, P = 0.12 and ANOVA r = −0.04, P = 0.84 respectively). Finally, IL-6 protein showed a marginally negative correlation with TAC (ANOVA r = −0.47, P = 0.02).
Transcription factors showed a differential correlation with each other, OxS markers and inflammatory variables
HIF-1α mRNA was not correlated with HIF-2α (ANOVA r = −0.19, P = 0.34) and NRF2 mRNA (ANOVA r = −0.29, P = 0.15) whereas HIF-2α mRNA levels were positively correlated with NRF2 gene expression over time (ANOVA r = +0.58, P = 0.002) (Table 2 and Supplementary Fig. S1).
HIF1α mRNA was positively correlated with ROS overtime (ANOVA r = +0.62, P < 0.001) (Table 2). HIF-2α mRNA levels showed a marginally significant correlation with the IL-6 mRNA levels over time (ANOVA r = +0.46, P = 0.02) (Table 2 and Supplementary Fig. S1).
NRF2 mRNA level was negatively correlated with TAC (ANOVA r = −0.43, P = 0.03). Significant correlations were identified involving NF-κB mRNA with TAC and ROS (ANOVA r = −0.59, P = 0.002 and ANOVA r = +0.46, P = 0.02). Only marginal positive correlations were identified involving NF-κB mRNA and plasma interleukins IL-1β and IL-6 overtime (ANOVA r = +0.49, P = 0.01 and ANOVA r = +0.47, P = 0.02 respectively).
Discussion
These data describe, for the first time in vivo in human WBCs, the differential regulation of specific transcription factors in response to both sub-acute (≤24 h) and prolonged (72 h) sedentary HH exposure in healthy participants post direct ascent to 3830 m. Specifically, these data highlight: i) the individual contribution of HIF-1α and other master TFs (HIF-2α, p65 and NRF2) involved in the mediation of an HH response; ii) the concurrent transcription pattern of these TFs, and iii) the relationship demonstrated with established inflammatory and OxS pathways over time. During this study confounding factors (e.g., physical exertion, changes in HH level, cardiovascular as well as other chronic diseases, and diet) were minimised. Therefore, we infer that our results reflect a ‘clean’ model for the interrogation of the early phase of WBC response to both a sub-acute and prolonged HH stimulus. This integrated analysis shows that HIF-1α is a lead TF during the sub-acute hypoxic response, preventing an excessive pro-inflammatory response, as well as contrasting the proposed collective repression of antioxidant activity under HH conditions. In addition, we have showed that the prolongation of HH stress led to a switch in predominant TF induction. In particular, after 24 h a significant increase in both the transcription of the HIF-2α isoform and NRF2 is evident. This relative, sustained increase is concomitant with a decline in HIF-1α transcription, thus suggesting the presence of a synchronized mechanism that led to an effective molecular anti-inflammatory “brake” in response to acute HH exposure. This anti-inflammatory activity is in direct contrast to the previous proposition for collective systemic inflammation.
HIF-1α mRNA levels demonstrated a transient increase within 72 h of HH exposure, reaching a peak after 24 h and returning to a basal level within 72h43,44. These in vivo results, in humans, demonstrate a preferential involvement of the HIF-1α gene transcription during the early phase of HH stress response. Equally, this parabolic response supports the hypothesis that HIF-1α steady state basal protein levels, plus post-transcriptional and post-translational regulations alone are not effective in response to such a direct HH exposure (helicopter ascent to 3830 m)43,45. Our results confirm that prolonged HH exposure appears to favor the transcription of the HIF-2α gene, with a progressive increase in expression after 24 h of exposure14. Which potentially indicates a definitive switch in HIFs regulation, from the initial cellular defense to a sudden hypoxic stressor, to that of a sustained cellular response to a prolonged hypoxic stimulus. Overall, our in vivo results in WBCs seem consistent with the HIF switch model observed in previous in vitro studies, both in vascular and bone development, and cancer stem cells25,46. Differences in downstream target genes12,25 could partially explain why HIF-1α drives the initial response to HH. HIF-1α leading the homeostatic defense with apoptotic and glycolytic enzyme target genes, whereas HIF-2α potentiating the physiological response during prolonged HH exposure via angiogenic and invasion target genes as showed also by recent studies of evolutionary genomics in populations living permanently at high-altitude47. Moreover, we demonstrated that NRF2 mRNA significantly increased in expression over time, reaching a peak after 72 h, in parallel to the expression of HIF-2α.
Previous experimental studies have suggested that NF-κB, and NRF2 are pleiotropic TFs that have been implicated in many cellular processes, including inflammation and OxS responses to hypoxic exposure21,23,48. The NF-κB subunits p50 and p65 are, in fact, activated by hypoxia and mediate the induction of HIF-1α mRNA via a transcriptional mechanism by binding to the HIF-1α promoter, thus suggesting a specific role of NF-κB in the maintenance of basal HIF-1α mRNA levels43. However, in this in vivo study the p65 mRNA levels were not significantly upregulated, neither were they correlated with HIF-1α gene expression or the expression of other TFs. In addition, only a slightly significant positive correlation with interleukin protein levels in plasma and a negative correlation with TAC response is observed as expected throughout 72 h of HH exposure. The lack of NF-κB subunit activation is reported in contrast with previous studies using hepatocellular carcinoma culture, HeLa cells and ex vivo cardiac and pulmonary tissues harvested from hypoxic mice, where an increased transcription of NF-κB isoforms was repeatedly demonstrated with the application of a hypoxic stimulus49,50. These findings may be explained by the fact that in those previous studies NF-κB isoform transcription and/or activation was heavily dependent on cellular type tested and specific experimental model. Currently, we cannot exclude the possibility that p65 expression could be significantly enhanced in specific white cell types, an effect which could have been masked in our study due to the consideration of a global WBC population. On the other hand, our findings are in agreement with the idea that HIF-1α could restrain the NF-κB response and thus prevent excessive and damaging pro-inflammatory responses16.
Several papers have previously reported that HH, similarly to cardiovascular diseases and other disease states, can lead to an increase in the inflammatory state33,34,51, accompanied by a significant increase in circulating pro-inflammatory cytokines. In correspondence, our results have shown a marginally negative correlation between SpO2, circulating IL-1β and IL-6 plasma levels. In the meanwhile, a marginally positive correlation among the two circulating cytokines was observed as expected by previously reported information39. IL-1β plasma levels transiently increased over 72 h, however the absolute value remained in the normal range expected for healthy individuals41. In addition, IL-6 plasma levels were also considered in the normal range for healthy individuals throughout our 72 h HH protocol45. In contrast with protein results at a cellular level, in WBCs, there was no significant increase of IL-1β mRNA and IL-6 mRNA and only a marginal significant positive correlation was observed between them over time. Therefore, no significant correlation was observed among investigated interleukin mRNA expression and their respective proteins, this is in agreement with the idea that circulating interleukins are released by different tissues and not exclusively by WBCs. Altogether, these data suggest that despite the expected initial increase in inflammation on rapid, direct ascent to HH, any major discrepancy in circulating pro-inflammatory cytokines may be quickly and progressively counteracted by an effective anti-inflammatory action. This activity is probably mediated primarily by HIF-1α19,23,24 and later surpassed by a concomitant upregulation of NRF252. Our in vivo results are in agreement with other papers that did not show increased plasma levels of pro-inflammatory cytokines in healthy and acute mountain sickness prone subjects36,37,53. Within this topic, with reference to similar studies, comparative analysis is challenging to complete and discrepancies are likely due to specific differences in study design, cytokine dosage protocol35 and statistical analysis.
HH exposure leads intrinsically to an increased OxS in healthy humans, as well as in animal models1,53,54. Our results confirm that OxS is strongly increased in particular within 24 h of exposure to HH, as shown up by the increased oxidative damage of biomolecules such as lipids, proteins and DNA. Moreover, the positive correlation among SpO2 and TAC, plus the contemporary negative correlations between SpO2 and TAC with ROS, both support the idea of an initial delay of effective antioxidant defense, followed by delayed ROS species scavenging1,3,55,56. Our results are in agreement with the idea that the pathways by which ROS could contribute to cell signaling responses to hypoxia involves the HIF family and NRF2. NRF2 is the guardian of redox homeostasis and regulates a coordinated induction of a battery of cytoprotective, anti-oxidant, and anti-inflammatory genes in response to OxS and inflammation21–23. NRF2 mRNA levels in WBC increased constantly over time showing a positive correlation with HIF-2α mRNA levels (ANOVA) and a positive correlation with TAC (ANOVA). Our in vivo results suggest that the HH-induced ROS formation leads to an effective HIF-1α and NRF2 activity, only after reaching a critical threshold that seems defined by both level of hypoxia and duration of exposure57,58. Indeed, these results demonstrate that within 72 h the ascent protocol used in this study was able to identify differing temporal regulation of pertinent cellular factors involved in hypoxic response. This includes, those factors necessary for initial hypoxic cellular defense (HIF-1α) and those considered more active in the regulation of prolonged cellular response (HIF-2 α and NRF2). However, the duration of the exposure was not long enough to characterise the level of expression in all selected factors, and therefore cannot be used to infer cellular regulation during a complete and effective acclimatisation.
The positive correlation between HIF-1α and ROS are in agreement with the idea that HIF-1α is stabilized in hypoxia via the hydroxylation of different prolyl group by proline hydroxylases, this activity has been shown to be sensitive to inhibition by ROS59. Finally, we consider the marginally significant positive correlation observed among the IL-1β protein with ROS, and the similarly marginal significant negative correlation of IL-6 protein with TAC, as potential inference for existing interdependent and interconnected processes among inflammation and OxS during hypoxia response in humans60,61.
The current study has several caveats. Firstly, TF protein levels and activities were not measured due to logistical and ethical limitations related to the study design (e.g. barometric pressure-decreased PAXgene blood RNA tubes sampling; repeated samples in humans in a field study at altitude). Nevertheless, transcriptional regulation is an important pre-cursor of functional TFs. Secondly, a larger sample size, with additional sampling time-points both during and after hypoxic exposure, including information related to individual “reoxygenation profiles” after return to sea level, would have improved our study model. In future studies, inclusion of information relating to the molecular impact of re-oxygenation post prolonged hypoxic exposure, could be pertinent when considering the mechanistic aspect of specific hypoxia related pathologies (i.e. ischemia-reperfusion). Equally, in this study it would have been helpful to determine novel TF-oriented markers, such as HIF-3α, p50 (NF-κB family member), and TLRF2. Nevertheless, the aim of the study was to try to describe for the first time, in humans in vivo, the temporal mediation of possible master TFs involved in the hypoxemic, inflammatory and OxS pathways in response to both sub-acute and prolonged HH exposure. Finally, it remains unknown as to when TFs like NRF2 and HIF-2α are, in fact, repressed; thus establishing a new steady state and avoiding deleterious effects of an excessive prolonged activation of target genes involved in angiogenesis and red blood cell formation. Further microRNAs and epigenetic studies are required to better elucidate the detailed aspects of the intricate and complex crosstalk between those TFs and pathways reportedly activated or repressed during hypoxic response20,24.
Conclusions
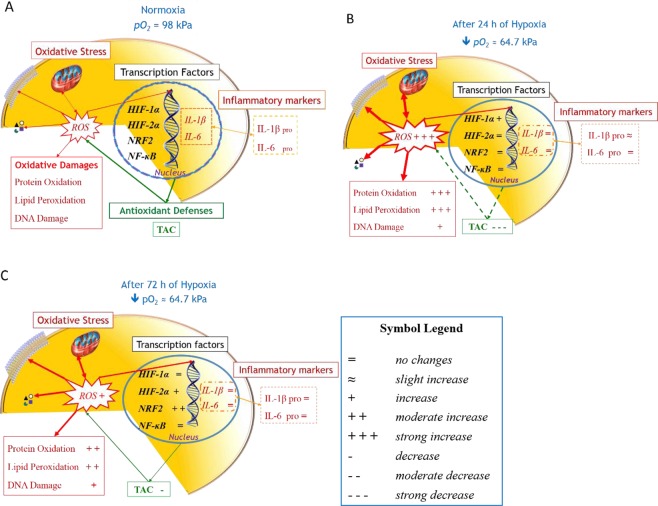
We have identified in vivo differential temporal regulation of molecular aspects of HIFs and other master TFs in healthy humans in direct response to HH-induced inflammation and OxS (Fig. 4). Our integrated analysis of TF-gene expression suggests that HIF-1α is a lead TF during the early phase of direct HH exposure, preventing an excessive pro-inflammatory response16 and contrasting the repression of antioxidant activity on initial exposure to high altitude (Fig. 4A,B). Correspondingly, we have showed that prolonged HH exposure results in the sequential induction of differentially mediated anti-inflammatory activity; most likely probably due to the contemporary repression of the pro-inflammatory role of NF-κB (Fig. 4C). Specifically, the activation of HIF-1α, HIF-2α and NRF2 appear to act in concert, in an attempt to establish an effective molecular anti-inflammatory “brake” in response to the evident systemic inflammation induced by prolonged HH. The in vivo values of ROS and OxS-damage biomarkers confirmed a prolonged transient increase, due to a delay in the activation (and effectiveness) of the NRF2-mediated antioxidant defenses. Results from humans exposed to an acute and prolonged hypoxic stimulus offer a unique means to evaluate in vivo the time-related response/counteraction measures to inflammation and OxS. Our results have demonstrated that the extensive transcriptional output of HIF in response to hypoxia is highly synchronized and integrated with additional signaling pathways; involving nutrient sensing, protein synthesis and other fundamental processes. All the aforementioned TFs and mechanisms have a clinical relevance and are considered potential therapeutic targets for cardiovascular and other diseases that are associated with OxS and inflammation3,13,62,63. The failure of supplementation with exogenous antioxidants vitamins for prevention or treatment of cardiovascular disease reinforced the idea of alternative approaches to counteract the deleterious effects of an excessive ROS production64,65. In particular, the therapeutic potential of phytochemical and synthetic compounds for NRF2 activation in attenuating oxidative damage associated in neurodegenerative diseases, cancer and cardiovascular diseases has been previously shown and discussed63–65. The beneficial role of HIF-1α activation is shown in the revascularisation and collateral circulation in ischemic brains in rodents66. On the contrary, it has been demonstrated that HIF-1α plays a role in the progression of atherosclerosis suggesting that the repression of its activity could lead to beneficial outcome for patients62.
Figure 4.
HH response in humans is governed by both spatial and temporal mediation of the OxS and inflammatory pathways via a series of micro and macro events. This schematic overview highlights qualitatively how pertinent relationships between crucial molecular transcription factors and both oxidative and inflammatory pathways involved in the cellular hypoxic response are mediated over time. The +, =, and − symbols refers to qualitative changes of variables during hypoxia exposure in comparison with baseline. (A) During normoxic conditions a well-balanced level of ROS cytokines and TFs mRNA turnover are present in the cells. (B) After 24 h of HH exposure HIF-1α mRNA transcription is enhanced but the level of OxS is also high, plus the existing antioxidant defenses fielded by the cell seem ineffective, results demonstrating a delayed induction of NRF2, in contrast to the immediate deleterious impact of ROS induction on key cellular biomolecules such as lipids, proteins and DNA. On the contrary, the slight increase in circulating IL-1β demonstrates an early attempt by the cell to mitigate the inflammation response. (C) After 72 h of exposure the situation is dramatically changed, showing a marked reduction of ROS production and a consequent reduction of damages on biomolecules, probably counteracted by the scavenging activity performed by antioxidant enzymes. Conversely, no significant modifications were shown by either inflammatory markers or NF-κB after 72 hours of constant, passive hypobaric hypoxic exposure.
To date, the hypoxic preconditioning is used as a therapeutic strategy to mitigate injuries in the cardiovascular system, stimulating and/or repressing factors that are important players in anti OxS and inflammation. Our in vivo study provides new details on the complexity of the cross-talk and temporal regulation of molecular mechanisms and factors (HIF-1α, HIF-2α and NRF2) involved in cellular response to ROS and inflammation during a hypoxic stimulus. Our results could influence the design of new clinical trials inclusive of hypoxic protocols or hypoxia mimetics for therapeutic use, where definition of TF induction with specific hypoxic doses remains to be defined. A separate focus could include testing the role of HIF-2α as a therapeutic target62,67, the aim to further distinguish protocols intended to study acute and/or chronic hypoxia pathologies.
Methods
Study design and participants
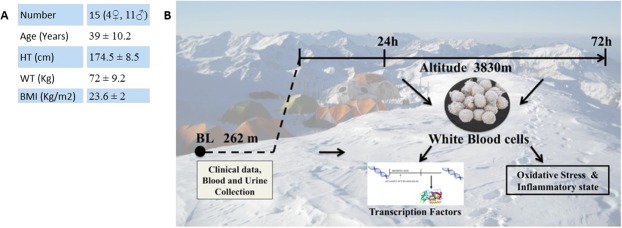
From the initial sample, including 19 healthy participants of European ancestry, 15 completed the experimental period. Participant’s characteristics are reported in Fig. 5A. Prior to the study, none of the participants were treated with either acetazolamide, non-steroidal, or steroidal anti-inflammatory agents. Exclusion criteria during selection were: age <18 years and habitual intake of antioxidant or anti-inflammatory substances at baseline visit; acute illness (infectious, cardiovascular, cerebrovascular or respiratory), and any prior acute high-altitude illness. One participant was undergoing hypertension therapy and one of the participants was reportedly a smoker. During the study, only non-steroidal anti-inflammatory agents were permitted after consultation with the study’s physician. Moreover, the Lake Louise Score (LLS)68 was assessed to evaluate the health status of participants. Subjects with a LLS ≥ 3 were excluded from the study.
Figure 5.
(A) Table of human volunteer characteristics, including age, height (HT), weight (WT), body mass index (BMI) (B). Outline of study design, and ascent profile.
Written informed consent was obtained from all participants. The study was approved by the Ethics Committee of Bolzano General Hospital (number 0073450-BZ), and conformed with the Declaration of Helsinki (2008). The study is registered at www.clinicaltrials.gov (registration number NCT01794130).
Two weeks prior to experimental ascent, participants underwent baseline medical examinations at the Institute of Mountain Emergency Medicine, Eurac Research, Bolzano, Italy (262 m). These examinations were subsequently repeated in a medical tent located near Mt. Ortles summit, Italy, both 24 h and 72 h post direct ascent by helicopter to 3830 m (Fig. 5B). Participants remained in tented accommodation at 3830 m for a total of three days, during which they were instructed to avoid any unnecessary physical exertion.
Clinical assessment and high altitude health conditions
Medical examinations included the assessment of: oxygen saturation (SpO2; Handheld Pulse Oximeter NBP-40, Nellcor Puritan Bennet Inc., Pleasanton, CA, USA); heart rate (HR) and breathing rate (BR). SpO2 and HR were both measured at rest in triplicate using the same device, care was taken to ensure signal stabilisation and that participants had warm hands on examination. Both were reported as an average of three consecutive measurements.
Throughout the study, the Lake Louise Score (LLS) and a number of alternative signs and symptoms were assessed to evaluate the health status of participants including dyspnea, cough, fatigue, cyanosis, and rales.
During the 3 day study period, those individuals who presented at least once with a LLS ≥ 3 (including a headache score ≥ 1) were considered bad responders and excluded.
Blood and urine samples collection
Venous blood samples were drawn from the antecubital vein, collected in heparinized tubes (Becton Dickinson Company, UK) centrifuged and separated. Plasma was stored in aliquots at −80 °C until analysis. In addition, urine samples were collected and stored at −80 °C. Moreover, for each participant 5 mL of venous blood were collected into two PAXgene® blood RNA tubes (i.e. 2 × 2.5 mL) (QIAGEN, Mississauga, Ontario) and stored in multiple aliquots at −80 °C until assayed for gene expression quantification.
Candidate genes expression levels
Blood processing, RNA isolation, mRNA determination
Total RNA from whole blood was extracted using the PAXgene® Blood RNA Kit (PreAnalytiX), according to the manufacturer’s instructions, to evaluate the white blood cell expression. RNA quantity and quality were determined by the ratio from the absorbance readings at 260 nm and 280 nm with a NanoDroP 2000C (Thermo Scientific, USA).
For gene expression, cDNA was synthesized with 200 ng of RNA extracted using iScript cDNA synthesis kit (Bio-Rad, Hercules, CA) according to the manufacturer’s instructions.
Genes expression
Quantitative real-time polymerase chain reaction assay was performed in a Bio-Rad CFX96 Real Time PCR detection system69. All the reactions were performed in 96-well plates, in triplicate. A negative control containing all reagents, but no cDNA template was included in all runs.
The PCR reaction was performed in a 25 μL final reaction volume, containing 200nmol of each primer and SsoFast EVAGreen SuperMix (Bio-Rad, USA). Primers were designed from sequences derived from the GenBank database using Primer 3 (Whitehead Institute, Massachusetts, USA) and Operon’s Oligo software (Operon, California, USA). Primers were purchased from Eurofins MWG (Ebersberg, Germany). The specific primers were (Eurofins): HIF-1α, Forward ACAAGCCACCTGAGGAGAG and reverse AAGTGGCAACTGATGAGCAAGC; HIF-2α, Forward TGTATGGTCAGCTCAGCCC and reverse GCTCCACCTGTGTAAGTCCC; IL-6, Forward TTAGAGTCTCAACCCCCAATAAAT and reverse TACATGTCTCCTTTCTCAGGGC; β-actin, Forward GAGCTACGAGCTGCCTGAC and reverse GGATGCCACAGGACTCCA. Validation of specificity of qPCR assay was performed by melting-curve analysis and agarose gel analysis. NF-κB (p65) (Hs00153294), IL-1β (Hs00174097), NRF2 (Hs00975961) gene expression were measured using Taqman primers (Applied Biosystems, USA). All procedures were performed according to the manufacturer protocols. β-Actin was used as reference gene. For each target gene, a calibration curve was generated with threshold cycle (Ct) values from serial dilutions of cDNA (from 106 to 10 copies/reaction) to determine reaction efficiencies, linearity, detection and quantification limits. Data analyses were performed with the Bio-Rad CFX Manager. The comparative cycle threshold method (ΔΔCt), which compares the difference between groups in cycle threshold values, was used to obtain the relative fold change of gene expression.
Inflammatory markers assay
Interleukin 1β (IL-1β) and Interleukin 6 (IL-6) plasma levels were determined by ELISA assay kit (ThermoFisher Scientific, CA, USA), based on the double-antibody “sandwich” technique according to the manufacturer’s instruction. The assay sensitivity was <0.92 pg.mL−1 and <0.06 pg.mL−1 for IL-6 and IL-1β respectively.
ROS detection and Oxidative damage assessment
Plasma ROS measurements
An X-band EPR instrument (E-scan-Bruker BioSpin, GmbH, MA) was used to determine ROS production. The instrument is designed to function with very low concentrations of paramagnetic species in small (50 μL) samples. For each recruited participant, the ROS production rate was determined by means of a recently implemented EPR method1,70.
Plasma Total Antioxidant Capacity (TAC) determination
TAC was measured via enzymatic kit (Cayman Chemical, Ann Arbor, MI, USA), based on the ability of antioxidants present in the plasma to inhibit the oxidation of 2,2-azinobis (3-ethylbenzithiazoline) sulfonic acid (ABTS) to the radical cation ABTS+ by a peroxidase. The amount of the produced ABTS+ was assessed by measuring the absorbance signals at 750 nm. TAC was evaluated by a Trolox (6-hydroxy-2,5,7,8-tetramethylchroman-2-carboxylic acid) standard curve and was expressed as trolox-equivalent antioxidant capacity concentration (mM).
Protein Carbonyls (PC) determination
The accumulation of oxidized proteins was measured by content of reactive carbonyls. A protein carbonyls assay kit (Cayman Chemical, Ann Arbor, MI, USA) was used to evaluate colorimetrically oxidized proteins at 370 nm. Values obtained were normalised to the total protein concentration in the final pellet (absorbance reading at 280 nm), to consider protein loss during the washing steps, as suggested in the kit’s user manual.
Plasma Thiobarbituric acid-reactive substances (TBARS) determination
The measurement of TBARS was determined by TBARS assay kit (Cayman Chemical, Ann Arbor, MI, USA), which allows a rapid photometric detection of the thiobarbituric acid malondialdehyde (TBAMDA) adduct at 532 nm.
Urine 8-isoprostane (8-isoPGF2α) determination
EIA assay was used for the determination of 8-iso PGF2α (Cayman Chemical, Ann Arbor, MI, USA). Samples and standards were read at a wavelength of 412 nm. The results were normalized by urine creatinine values.
Urine 8-OH-2-deoxyguanosine (8-OH-dG) determination
8-OH-dG was measured by immunoassay EIA kit (Cayman Chemical, Ann Arbor, MI, USA) as a biomarker for oxidative damage. Samples and standards were read at a wavelength of 412 nm. The results were normalized by urine creatinine values.
Creatinine: Urinary concentrations of 8-iso PGF2α and 8-OH-dG, as any urinary marker, vary considerably; therefore, the urinary parameters are usually standardised based on the amount of creatinine excreted in the urine when the collection of the 24 h urine is not possible. Indeed, in the absence of renal disease, the excretion rate of creatinine in an individual is relatively constant. Thus, urinary creatinine levels may be used as an index of standardisation. A creatinine assay kit (Cayman Chemical, Ann Arbor, MI, USA) was used to measure creatinine levels in urine samples.
Statistical analysis
The effect of HH exposure on the different clinical parameters and gene expression over time was evaluated by analysis of variance (ANOVA) for repeated measures of ΔCt for gene mRNA levels; comparison of two time-points was carried out by means of paired samples t-test and Bonferroni correction was applied. A correlation coefficient for repeated observations was used to detect if changes over time of two parameters were correlated. The relative quantification of genes was determined using the 2−ΔΔCt method.
Data were analyzed using SPSS 23.0 statistical software package (IBM Corp., Armonk, NY, USA). Variables such as sex, altitude of residence, and smoker status were considered in the statistical analysis, but no confounding influence was found on results (data not shown). All P-values were two sided, and differences were considered significant at P < 0.05; for correlation analysis P < 0.01 was considered significant and P < 0.05 marginally significant. Plotly software (Plotly Technologies Inc., Montréal, Québec, CA) was used to draw Box and Whisker plots (https://plot.ly/).
Supplementary information
Acknowledgements
The authors thank Georg Hofer (Department of Anesthesiology and Critical Care Medicine, General Hospital of Silandro, Italy), Karla Balkenhol, Michael Pohl and Emily Procter (Eurac Research, Institute of Mountain Emergency Medicine, Bolzano, Italy), and Piergiorgio Lochner (Department of Neurology, University of the Saarland, Homburg, Germany) for invaluable support during data and sample collection; and Tomas Dal Cappello (Eurac Research, Institute of Mountain Emergency Medicine, Bolzano, Italy) for support with the statistical analysis. The authors thank the Department of Innovation, Research and University of the Autonomous Province of Bozen/Bolzano for covering the Open Access publication costs.
Author Contributions
G.S., S.M. and H.B. contributed to study design and participated in clinical data collection and analysis. G.S., S.M., S.M.S., G.C., S.M., A.V. and A.G. contributed to biological sample data collection and analysis. S.M. and S.M.S. performed the statistical analysis. G.S., S.M., R.T., G.C., C.R., A.V. and M.F. contributed to interpretation of data. S.M., G.S., S.M.S., R.T., C.R. and M.F. did the literature review and wrote the manuscript. S.M. prepared Figs 2–5. S.M.S. prepared Fig. 1. All authors critically reviewed the final draft of the manuscript and have given approval for the version submitted.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-46391-6.
References
- 1.Strapazzon G, et al. Oxidative stress response to acute hypobaric hypoxia and its association with indirect measurement of increased intracranial pressure: a field study. Sci Rep. 2016;6:32426. doi: 10.1038/srep32426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merelli A, et al. Understanding the role of hypoxia inducible factor during neurodegeneration for new therapeutics opportunities. Curr Neuropharmacol. 2018;16(10):1484–1498. doi: 10.2174/1570159X16666180110130253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farías Jorge, Molina Víctor, Carrasco Rodrigo, Zepeda Andrea, Figueroa Elías, Letelier Pablo, Castillo Rodrigo. Antioxidant Therapeutic Strategies for Cardiovascular Conditions Associated with Oxidative Stress. Nutrients. 2017;9(9):966. doi: 10.3390/nu9090966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dumitrascu R, Heitmann J, Seeger W, Weissmann N, Schulz R. Obstructive sleep apnea, oxidative stress and cardiovascular disease: lessons from animal studies. Oxid Med Cell Longev. 2013;2013:234631. doi: 10.1155/2013/234631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levy P, et al. Sleep deprivation, sleep apnea and cardiovascular diseases. Front Biosci (Elite Ed). 2012;1;4:2007–21. doi: 10.2741/521. [DOI] [PubMed] [Google Scholar]
- 6.Majmundar AJ, Wong WJ, Simon MC. Hypoxia-inducible factors and the response to hypoxic stress. Mol Cell. 2010;22;40(2):294–309. doi: 10.1016/j.molcel.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Semenza GL. Hypoxia-inducible factors in physiology and medicine. Cell. 2012;148(3):399–408. doi: 10.1016/j.cell.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaakkola P, et al. Targeting of HIF-alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001;292(5516):468–472. doi: 10.1126/science.1059796. [DOI] [PubMed] [Google Scholar]
- 9.Semenza GL. O2-regulated gene expression: transcriptional control of cardiorespiratory physiology by HIF-1. J Appl Physiol. 2004;96(3):1173–1177. doi: 10.1152/japplphysiol.00770.2003. [DOI] [PubMed] [Google Scholar]
- 10.Wang GL, Semenza GL. General involvement of hypoxia-inducible factor 1 in transcriptional response to hypoxia. Proc Natl Acad Sci USA. 1993;90(9):4304–4308. doi: 10.1073/pnas.90.9.4304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Rourke JF, Pugh CW, Bartlett SM, Ratcliffe PJ. Identification of hypoxically inducible mRNAs in HeLa cells using differential-display PCR. Role of hypoxia-inducible factor-1. Eur J Biochem. 1996;15, 241(2):403–410. doi: 10.1111/j.1432-1033.1996.00403.x. [DOI] [PubMed] [Google Scholar]
- 12.Shomento SH, et al. Hypoxia-inducible factors 1alpha and 2alpha exert both distinct and overlapping functions in long bone development. J Cell Biochem. 2010;109(1):196–204. doi: 10.1002/jcb.22396. [DOI] [PubMed] [Google Scholar]
- 13.Simon MC. The hypoxia response pathways -Hats Off! N Engl J Med. 2016;375(17):1687–1689. doi: 10.1056/NEJMcibr1610065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koh MY, Powis G. Passing the baton: the HIF switch. Trends Biochem Sci. 2012;37(9):364–72. doi: 10.1016/j.tibs.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scholz CC, Taylor CT. Targeting the HIF pathway in inflammation and immunity. Curr Opin Pharmacol. 2013;13(4):646–653. doi: 10.1016/j.coph.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 16.Bandarra D, Biddlestone J, Mudie S, Müller HA, Rocha S. HIF-1α restricts NF-κB-dependent gene expression to control innate immunity signals. Dis Model Mech. 2015;8(2):169–181. doi: 10.1242/dmm.017285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biddlestone J, Bandarra D, Rocha S. The role of hypoxia in inflammatory disease (review) Int J Mol Med. 2015;35(4):859–869. doi: 10.3892/ijmm.2015.2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palazon A, Goldrath AW, Nizet V, Johnson RS. HIF transcription factors, inflammation, and immunity. Immunity. 2014;41(4):518–528. doi: 10.1016/j.immuni.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rius J, et al. NF-kappaB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1alpha. Nature. 2008;5;453(7196):807–811. doi: 10.1038/nature06905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.D’Ignazio L, Bandarra D, Rocha S. NF-κB and HIF crosstalk in immune responses. FEBS J. 2016;283(3):413–424. doi: 10.1111/febs.13578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nguyen T, Nioi P, Pickett BC. The NRF-2-antioxidant response element signaling pathway and its activation by oxidative Stress. J Biol Chem. 2009;284:13291–13295. doi: 10.1074/jbc.R900010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hayes JD, Dinkova-Kostova AT. The Nrf2 regulatory network provides an interface between redox and intermediary metabolism. Trends Biochem Sci. 2014;39(4):199–218. doi: 10.1016/j.tibs.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Buelna-Chontal M, Zazueta C. Redox activation of Nrf2 & NF-κB: a double end sword? Cell Signal. 2013;25(12):2548–2557. doi: 10.1016/j.cellsig.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 24.Wardyn JD, Ponsford AH, Sanderson CM. Dissecting molecular cross-talk between Nrf2 and NF-κB response pathways. Biochem Soc Trans. 2015;43(4):621–626. doi: 10.1042/BST20150014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koh MY, Lemos R, Jr., Liu X, Powis G. The hypoxia-associated factor switches cells from HIF-1α-to HIF-2α-dependent signaling promoting stem cell characteristics, aggressive tumor growth and invasion. Cancer Res. 2011;71(11):4015–4027. doi: 10.1158/0008-5472.CAN-10-4142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryan S, Taylor CT, McNicholas WT. Predictors of elevated nuclear factor-kappaB-dependent genes in obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2006;174(7):824–830. doi: 10.1164/rccm.200601-066OC. [DOI] [PubMed] [Google Scholar]
- 27.Polotsky VY, et al. Intermittent and sustained hypoxia induce a similar gene expression profile in human aortic endothelial cells. Physiol Genomics. 2010;41(3):306–314. doi: 10.1152/physiolgenomics.00091.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scherrer U, Allemann Y, Jayet PY, Rexhaj E, Sartori C. High altitude, a natural research laboratory for the study of cardiovascular physiology and pathophysiology. Prog Cardiovasc Dis. 2010;52(6):451–455. doi: 10.1016/j.pcad.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Mariggiò MA, et al. Peripheral blood lymphocytes: a model for monitoring physiological adaptation to high altitude. High Altitude Medicine and Biology. 2010;11(4):333–342. doi: 10.1089/ham.2009.1097. [DOI] [PubMed] [Google Scholar]
- 30.Polotsky VY, Bevans-Fonti S, Grigoryev DN, Punjabi NM. Intermittent hypoxia alters gene expression in peripheral blood mononuclear cells of healthy volunteers. PLoS One. 2015;10(12):1–10. doi: 10.1371/journal.pone.0144725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoffmann MS, et al. Microarray studies of genomic oxidative stress and cell cycle responses in obstructive sleep apnea. Antioxid Redox Signal. 2007;9:661–669. doi: 10.1089/ars.2007.1589. [DOI] [PubMed] [Google Scholar]
- 32.Arnardottir ES, Mackiewicz M, Gislason T, Teff KL, Pack AI. Molecular signatures of obstructive sleep apnea in adults: a review and perspective. Sleep. 2009;32:447–470. doi: 10.1093/sleep/32.4.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hartmann G, et al. High altitude increases circulating interleukin-6, interleukin-1 receptor antagonist and C-reactive protein. Cytokine. 2000;12(3):246–252. doi: 10.1006/cyto.1999.0533. [DOI] [PubMed] [Google Scholar]
- 34.Ghezzi P, et al. Hypoxia increases production of interleukin-1 and tumor necrosis factor by human mononuclear cells. Cytokine. 1991;3(3):189–194. doi: 10.1016/1043-4666(91)90015-6. [DOI] [PubMed] [Google Scholar]
- 35.Klausen T, Olsen NV, Poulsen TD, Richalet JP, Pedersen BK. Hypoxemia increases serum interleukin-6 in humans. Eur J Appl Physiol Occup Physiol. 1997;76(5):480–482. doi: 10.1007/s004210050278. [DOI] [PubMed] [Google Scholar]
- 36.Kleger GR, et al. Evidence against an increase in capillary permeability in subjects exposed to high altitude. J Appl Physiol. 1996;81(5):1917–1923. doi: 10.1152/jappl.1996.81.5.1917. [DOI] [PubMed] [Google Scholar]
- 37.Swenson ER, et al. Acute mountain sickness is not altered by a high carbohydrate diet nor associated with elevated circulating cytokines. Aviat Space Environ Med. 1997;68(6):499–503. [PubMed] [Google Scholar]
- 38.Savale L, et al. Impact of interleukin-6 on hypoxia-induced pulmonary hypertension and lung inflammation in mice. Respir Res. 2009;27:10–23. doi: 10.1186/1465-9921-10-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tosato. G, Jones KD. Interleukin-1 induces interleukin-6 production in peripheral blood monocytes. Blood. 1990;75(6):1305–1310. [PubMed] [Google Scholar]
- 40.Sironi M, et al. IL-1 stimulates IL-6 production in endothelial cells. J Immunol. 1989;142(2):549–553. [PubMed] [Google Scholar]
- 41.Di Iorio A, et al. Serum IL-1beta levels in health and disease: a population-based study. ‘The InCHIANTI study’. Cytokine. 2003;22(6):198–205. doi: 10.1016/S1043-4666(03)00152-2. [DOI] [PubMed] [Google Scholar]
- 42.Fernandez-Real JM, et al. Circulating interleukin 6 levels, blood pressure, and insulin sensitivity in apparently healthy men and women. J Clin Endocrinol Metab. 2001;86(3):1154–1159. doi: 10.1210/jcem.86.3.7305. [DOI] [PubMed] [Google Scholar]
- 43.Belaiba RS, et al. Hypoxia up-regulates hypoxia-inducible factor-1alpha transcription by involving phosphatidylinositol 3-kinase and nuclear factor kappaB in pulmonary artery smooth muscle cells. Mol Biol Cell. 2007;18(12):4691–4697. doi: 10.1091/mbc.e07-04-0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pialoux V, et al. Relationship between oxidative stress and HIF-1 alpha mRNA during sustained hypoxia in humans. Free Radic Biol Med. 2009;46(2):321–326. doi: 10.1016/j.freeradbiomed.2008.10.047. [DOI] [PubMed] [Google Scholar]
- 45.Wiener CM, Booth G, Semenza GL. In vivo expression of mRNAs encoding hypoxia-inducible factor 1. Biochem Biophys Res Commun. 1996;225(2):485–488. doi: 10.1006/bbrc.1996.1199. [DOI] [PubMed] [Google Scholar]
- 46.Holmquist-Mengelbier L, et al. Recruitment of HIF-1alpha and HIF-2alpha to common target genes is differentially regulated in neuroblastoma: HIF-2alpha promotes an aggressive phenotype. Cancer Cell. 2006;10(5):413–423. doi: 10.1016/j.ccr.2006.08.026. [DOI] [PubMed] [Google Scholar]
- 47.Gnecchi-Ruscone GA, et al. Evidence of Polygenic Adaptation to High Altitude from Tibetan and Sherpa Genomes. Genome Biol Evol. 2018;10(11):2919–2930. doi: 10.1093/gbe/evy233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Culver C, et al. Mechanism of hypoxia-induced NF-kappaB. Mol Cell Biol. 2010;30(20):4901–4921. doi: 10.1128/MCB.00409-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fitzpatrick SF, et al. An intact canonical NF-κB pathway is required for inflammatory gene expression in response to hypoxia. J Immunol. 2011;186(2):1091–1096. doi: 10.4049/jimmunol.1002256. [DOI] [PubMed] [Google Scholar]
- 50.Bruning U, et al. NFκB and HIF display synergistic behaviour during hypoxic inflammation. Cell Mol Life Sci. 2012;69(8):1319–1329. doi: 10.1007/s00018-011-0876-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klokker M, Kharazmi A, Galbo H, Bygbjerg I, Pedersen BK. Influence of in vivo hypobaric hypoxia on function of lymphocytes, neutrocytes, natural killer cells, and cytokines. J Appl Physiol. 1993;74(3):1100–1106. doi: 10.1152/jappl.1993.74.3.1100. [DOI] [PubMed] [Google Scholar]
- 52.Kobayashi EH, et al. Nrf2 suppresses macrophage inflammatory response by blocking proinflammatory cytokine transcription. Nat Commun. 2016;7:11624–11638. doi: 10.1038/ncomms11624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vani R, Reddy CS, Asha Devi S. Oxidative stress in erythrocytes: a study on the effect of antioxidant mixtures during intermittent exposures to high altitude. Int J Biometeorol. 2010;54(5):553–562. doi: 10.1007/s00484-010-0304-6. [DOI] [PubMed] [Google Scholar]
- 54.Irarrázaval S, et al. Oxidative stress in acute hypobaric hypoxia. High Alt Med Biol. 2017;18(2):128–134. doi: 10.1089/ham.2016.0119. [DOI] [PubMed] [Google Scholar]
- 55.Tissot van Patot MC, et al. Enhanced leukocyte HIF-1α and HIF-1 DNA binding in humans after rapid ascent to 4300 m. Free Radical Biology and Medicine. 2009;46(11):1551–1557. doi: 10.1016/j.freeradbiomed.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 56.Møller P, Loft S, Lundby C, Olsen NV. Acute hypoxia and hypoxic exercise induce DNA strand breaks and oxidative DNA damage in humans. FASEB J. 2001;15(7):1181–1186. doi: 10.1096/fj.00-0703com. [DOI] [PubMed] [Google Scholar]
- 57.Lisk C, et al. Nrf2 activation: a potential strategy for the prevention of acute mountain sickness. Free Radic Biol Med. 2013;63:264–273. doi: 10.1016/j.freeradbiomed.2013.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sethy NK, Singh M, Kumar R, Ilavazhagan G, Bhargava K. Upregulation of transcription factor NRF2-mediated oxidative stress response pathway in rat brain under short-term chronic hypobaric hypoxia. Funct Integr Genomics. 2011;11(1):119–137. doi: 10.1007/s10142-010-0195-y. [DOI] [PubMed] [Google Scholar]
- 59.Pan Y, et al. Multiple factors affecting cellular redox status and energy metabolism modulate hypoxia-inducible factor prolyl hydroxylase activity in vivo and in vitro. Mol Cell Biol. 2007;27:912–925. doi: 10.1128/MCB.01223-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim YW, West XZ, Byzova TV. Inflammation and oxidative stress in angiogenesis and vascular disease. J Mol Med (Berl) 2013;91(3):323–328. doi: 10.1007/s00109-013-1007-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med. 2010;49(11):1603–1616. doi: 10.1016/j.freeradbiomed.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jain T, Nikolopoulou EA, Xu Q, Qu A. Hypoxia inducible factor as a therapeutic target for atherosclerosis. Pharmacol Ther. 2018;183:22–33. doi: 10.1016/j.pharmthera.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 63.Reuland DJ, McCord JM, Hamilton KL. The role of Nrf2 in the attenuation of cardiovascular disease. Exerc Sport Sci Rev. 2013;41(3):162–168. doi: 10.1097/JES.0b013e3182948a1e. [DOI] [PubMed] [Google Scholar]
- 64.Donovan EL, McCord JM, Reuland DJ, Miller BF, Hamilton KL. Phytochemical activation of Nrf2 protects human coronary artery endothelial cells against an oxidative challenge. Oxid Med Cell Longev. 2012;2012:1–12. doi: 10.1155/2012/132931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Calkins MJ, et al. The Nrf2/ARE pathway as a potential therapeutic target in neurodegenerative disease. Antioxid Redox Signal. 2009;11(3):497–508. doi: 10.1089/ars.2008.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yang J, et al. Hypoxia inducible factor 1α plays a key role in remote ischemic preconditioning against stroke by modulating inflammatory responses in rats. J Am Heart Assoc. 2018;7(5):1–10. doi: 10.1161/JAHA.117.007589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Koeppen M, et al. Hypoxia-inducible factor 2-alpha-dependent induction of amphiregulin dampens myocardial ischemia-reperfusion injury. Nat Commun. 2018;9(1):816–829. doi: 10.1038/s41467-018-03105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sutton, J. R., Coates, G., Houston, C. S. Lake Louise consensus on definition and quantification of altitude illness. Hypoxia: Mountain Medicine Burlington, Vermont: Queen City Press; 327–30 (1992).
- 69.Cattelan A, et al. NAD(+)-dependent SIRT1 deactivation has a key role on ischemia-reperfusion-induced apoptosis. Vascul Pharmacol. 2015;70:35–44. doi: 10.1016/j.vph.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 70.Mrakic-Sposta S, Gussoni M, Montorsi M, Porcelli S, Vezzoli A. A quantitative method to monitor reactive oxygen species production by electron paramagnetic resonance in physiological and pathological conditions. Oxid Med Cell Longev. 2014;2014:1–10. doi: 10.1155/2014/306179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.