Abstract
Background: Research on antipsychotics and early mortality in schizophrenia has arisen from Western countries and results show that mortality from natural causes is obviously increased in schizophrenia. China, differs largely from Western countries in health and social welfare systems, and Asian patients are more susceptible to side-effects and might require less antipsychotics than their Western counterparts. We, therefore, investigated the association between antipsychotic use and increased mortality from natural causes among patients with schizophrenia in China.
Methods: We conducted a population-based nested case–control study using patients’ hardcopy archives obtained from the Severe Mental Health Disorder Systems of Chengdu between January 1, 2006 and December 31, 2013. We identified all schizophrenic patients aged 18–65 years who died of natural causes in 2013 (N=157), and their age- and gender-matched controls (N=444).
Results: Antipsychotic use was more frequent in controls than in cases (59.9% vs 32.5%). Risk of death decreased significantly in those receiving antipsychotic monotherapy (adjusted odds ratio=0.27, 95% CI=0.16–0.46) and antipsychotic polypharmacy (adjusted odds ratio=0.29, 95% CI=0.12–0.70) than antipsychotic-free patients. Compared with monotherapy, antipsychotic-free treatment was associated with prominently increased mortality (adjusted odds ratio=3.64, 95% CI=2.18–6.08). When stratified by age and gender, the results remained unchanged.
Conclusion: Antipsychotic monotherapy significantly decreased mortality from natural causes in schizophrenic patients while antipsychotic polypharmacy did not contribute to the excess mortality and deserves further clarification. We need to improve the physical health of schizophrenic patients and promote health education among community mental health staff and primary caregivers.
Keywords: antipsychotics, polypharmacy, mortality, odds ratio, schizophrenia
Introduction
Schizophrenia, a chronic and debilitating disorder with a lifetime prevalence of nearly 1%,1 is characterized by positive, negative, cognitive, and affective symptoms, and may arise from neurodevelopmental and neurodegenerative pathophysiologic processes.2,3 Patients with schizophrenia have a life expectancy about 10–20 years shorter than the general population,4 hence the name “a life-shortening disease”.5 Nevertheless, causes of schizophrenia have not been fully understood. Although suicide accounts for about 30% of the total excess mortality, approximately two-thirds of the excess mortality among patients with schizophrenia result from natural causes such as cardiovascular disease, obesity-related cancer, diabetes, and chronic obstructive pulmonary disease.6,7 Underlying mechanisms that might explain the excess mortality of natural causes in patients with schizophrenia compared with the general population include unhealthy lifestyles, such as smoking, drinking, substance abuse, physical inactivity, and antipsychotics use.8–10 The efficacy of antipsychotic drugs has been established over the past half-century for the treatment of acute episodes (National Institute for Clinical Excellence, 2009), and for maintenance treatment by substantially reducing the risk of relapse.11,12 For people with schizophrenia, long-term antipsychotic use is usually accompanied by adverse effects such as weight gain, metabolic syndrome, diabetes, and ischemic heart disease, demonstrating their important role in increased mortality.
The relationship between cumulative antipsychotic exposure and mortality among patients with schizophrenia has been heatedly debated during the past decade. Nevertheless, whether long-term use is tied to either increased or decreased mortality remains unknown. To our knowledge, only one systematic review suggested that long-term exposure to antipsychotics might be associated with increased mortality, making it urgent to conduct more rigorously designed prospective studies.13 Minna Torniainen et al, reviewed that the cumulative antipsychotic exposure displays a U-shaped curve for overall mortality, and that the highest risk of death was observed among patients with schizophrenia who had no antipsychotic use. Their study, however, did not control for the effect of concomitant psychotropic medications. Tiihonen et al, reported that long-term use of antipsychotics was associated with a 15–40% lower mortality than no antipsychotic use, especially for clozapine,4,14 but residual biases including health behavior, general health status, quality of life, and economic and lifestyle factors were not eliminated. What is more, survival bias, which is crucially important, has not been addressed in most previous studies on cumulative antipsychotic exposure. As for current antipsychotic use associated with mortality, some previous prospective cohort studies on patients with schizophrenia, which were fairly large and representative, showed similar results of a lower mortality among those with current antipsychotic use than those without.4,15–19 Nevertheless, such association identified may not necessarily mean causality because those studies were observational, which led to potential selection bias. Thus, the putative role of antipsychotic use in the excess mortality of schizophrenic patients and how much schizophrenia per se contributes to the risk of death remain largely unidentified.
Treatment optimization for patients with schizophrenia has historically been a challenge. Current guidelines for the pharmacological treatment of schizophrenia recommend antipsychotic monotherapy; however, the use of a combination of antipsychotics (polypharmacy) is a widely applied clinical practice. Some previous studies reviewed that antipsychotic polypharmacy remains prevalent in the UK, and that it was prescribed to 38% of all psychiatric inpatients and 16% of those with schizophrenia living in the community.20,21 However, concomitant use of more than one antipsychotic should be avoided in general practice owing to scarce evidence of increased efficacy and to a higher risk for adverse effects22-24 such as weight gain, metabolic syndrome, diabetes, and ischemic heart disease, some of which are even life-threatening.25 To investigate the possible association between antipsychotics and mortality from natural causes, we conducted the present study on schizophrenic patients identified from the Severe Mental Health Disorder System of Chengdu, Sichuan Province, China.
Materials and methods
Data source
We proceeded to a population-based nested case–control study through the Severe Mental Health Disorder Administration (referred to as the System thereafter) of Chengdu, Sichuan Province, which includes all severe schizophrenic patients in Chengdu. The administration assigned a civil registration number that is unique to every Chengdu citizen at birth or immigration. These archives encompass civil registration number, date of admission, lifestyle factors (smoking and alcohol intake), geographic location, current and past somatic comorbidities (cancer, diabetes, cardiovascular disease, respiratory disease, cerebrovascular disease), primary family caregivers (mostly parents, spouses, or adult children), education, profession, vital status (dead, alive), date of death, psychotropic pharmacological treatments, and the sociodemographic and clinical variables such as diagnostic codes. All diseases were diagnosed on the basis of physical examination, findings of the screening phase, and medical history and symptoms, and coded according to the World Health Organization International Classification of Diseases, the Tenth Revision (ICD-10). All admissions to the severe mental health disorder system have been registered from 2006 onwards. Ethical approval was obtained from the West China Hospital Ethics Committee of Sichuan University and was conducted in accordance with the latest version of the Helsinki Declaration (line 96–98).
Study population
We identified from the System all patients aged 18–65 years as of January 1, 2013 with a registered diagnosis of schizophrenia and without any other mental health disorder diagnoses (ICD-10: F20) during the study period between January 1, 2006 and December 31, 2013. Both main and auxiliary diagnoses were encompassed.
Selection of cases and controls
We identified all patients from the study population who died between January 1, and December 31, 2013. The manner of death was identified from death certificates which are written generally by ordinary physicians, or by forensic specialists if death is sudden or crime is suspected. Cases included were defined as patients who died of natural causes. Patients who died of suicide, homicide, or an accident or patients for whom the manner of death was unknown were excluded.
To improve efficiency and reduce the number of required patients, we aimed to select three age- and gender-matched controls per case from the study population. Controls had to be alive at the date of death of the respective cases, and this date was designated as the index date.
Exposure definition
We defined current drug use as at least one prescription filled within 90 days before the date of death or the index date. Patients were excluded if their records of psychotropic pharmacological treatments were unknown or if their hardcopy archives were missing. Antipsychotics were classified into typical and atypical agents. Antipsychotic monotherapy was defined as filling of at least one prescription for a single antipsychotic within 90 days prior to the date of death or the index date. Antipsychotic polypharmacy was defined as filling of at least one prescription for two or more different antipsychotics during the 90 days before the date of death or the index date. At the same time, we also assessed psychotropic co-medication during the 90 days prior to death or the index date: current use of benzodiazepines, benzhexol, and antiepileptics.
Statistical analysis
Chi-square test and independent samples t-test were used for comparison between groups. The variables were dichotomized after exclusion of the “Don’t know” answers. Conditional logistic regression was used to calculate crude and adjusted odds ratios (ORs) and 95% confidence intervals (CIs) of the association between antipsychotic use and natural death compared with no antipsychotics use. Then, the same method was used to calculate crude and adjusted ORs and 95% CIs of the association between antipsychotic polypharmacy and natural death compared with antipsychotic monotherapy as it represented the recommended therapy regimen. A univariate analysis including all potential confounders was performed. A multivariable analysis was then performed including all variables with p values <0.10 in univariate analysis in the final model. Statistical significance was defined as a p-value <0.05. To investigate effect-measure modification, we stratified our analyses by gender and age. All analyses were performed using Stata/SE14.0 for Windows.
Results
Sample characteristics
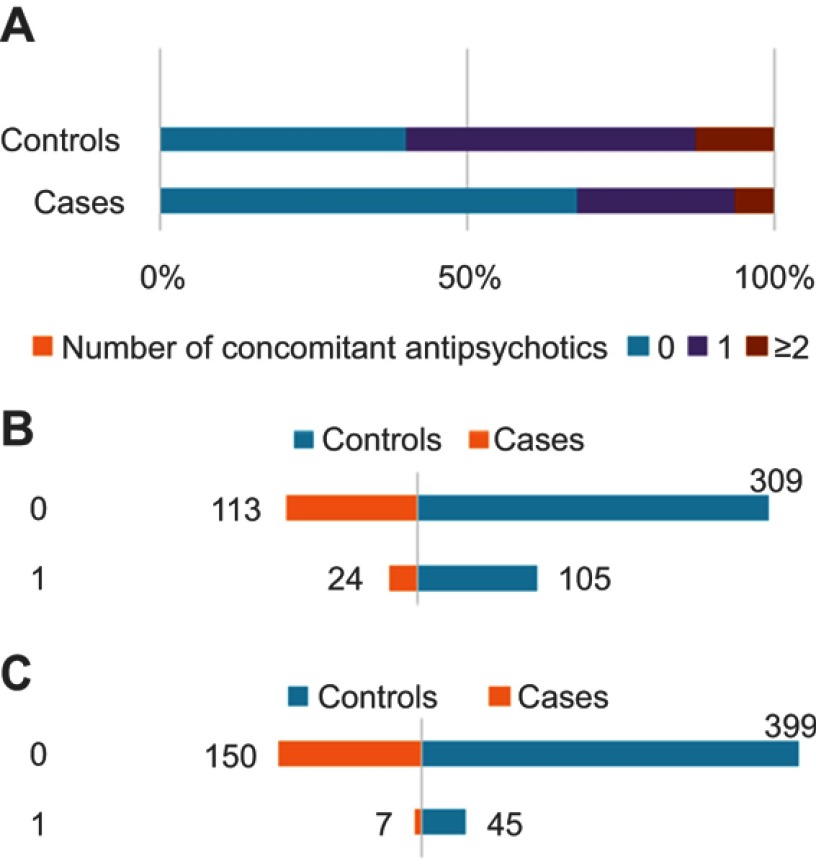
We identified 601 patients who were aged 18–65 years, diagnosed as schizophrenia and having no any other psychotic disorders, and were registered in the system from 2006 onwards. Of the 601 patients, 157 died between January 1 and December 31, 2013, and 444 matched controls (1–3 per case) meeting the inclusion criteria were also identified. Patient characteristics are shown in Figure 1 and Table 1. About two-thirds of cases and controls were male, and nearly 80% were between 40 and 65 years old. Antipsychotic use was more common in controls than in cases (59.9% vs 32.5%), especially antipsychotic monotherapy (47.1% vs 26.1%). No obvious difference was found between cases and controls with regard to the pattern of typical (11.6% vs 18.6%) and atypical antipsychotics use (16.3% vs 37.9%).
Figure 1.
Clinical characteristics of the 601 patients with schizophrenia.
Notes: (A) The number of concomitant antipsychotics use in the case and control group (0: no antipsychotic use;1: monotherapy;2: 2 or 2 more antipsychotic use). (B) The patient number of comorbidity in the case and control group (0: no comorbidity; 1: have comorbidity). (C) The patient number of benzhexol use in the case and control group (0: no benzhexol use; 1: benzhexol use).
Table 1.
Demographic and clinical characteristics of cases and controls
| Characteristics | Cases (N=157) N (%) | Controls (N=444) N (%) | p-value |
|---|---|---|---|
| Gender | 0.941 | ||
| Male | 102 (65.0) | 287 (64.6) | |
| Female | 55 (35.0) | 157 (35.4) | |
| Age (years) | 0.583 | ||
| 18–29 | 7 (4.5) | 9 (2.0) | |
| 30–39 | 14 (8.9) | 37 (8.3) | |
| 40–49 | 38 (24.2) | 117 (26.4) | |
| 50–59 | 57 (36.3) | 162 (36.5) | |
| 60–65 | 41 (26.1) | 119 (26.8) | |
| Mean age(year) | 51.7 | 52.3 | 0.442 |
| Number of concomitant antipsychotics | 0.001 | ||
| 0 | 106 (67.5) | 178 (40.1) | |
| 1 | 41 (26.1) | 209 (47.1) | |
| ≥2 | 10 (6.4) | 57 (12.8) | |
| Antiepileptics | 0.444 | ||
| Yes | 7 (4.5) | 14 (3.2) | |
| No | 150 (95.5) | 430 (96.8) | |
| Benzhexol | 0.030 | ||
| Yes | 7 (4.5) | 45 (10.1) | |
| No | 150 (95.5) | 399 (89.9) | |
| Benzodiazepine | 0.620 | ||
| Yes | 9(5.7) | 21 (4.7) | |
| No | 148(94.3) | 423 (95.3) | |
| Smokinga | 0.637 | ||
| Yes | 35 (22.3) | 109 (24.5) | |
| No | 118 (75.2) | 331 (74.5) | |
| Alcohol intakea | 0.421 | ||
| Yes | 35 (22.3) | 88 (19.8) | |
| No | 117 (74.5) | 353 (79.5) | |
| Comorbiditya | 0.060 | ||
| Yes | 24 (15.3) | 105 (23.6) | |
| No | 113 (72.0) | 309 (69.6) | |
| Marital statusa | 0.588 | ||
| Married | 100 (63.7) | 299 (67.3) | |
| Single | 50 (31.8) | 134 (30.2) | |
| Professiona | 0.641 | ||
| Farmer | 112 (71.3) | 319 (71.8) | |
| Other | 40 (25.5) | 103 (23.2) | |
| Education (years)a | 0.467 | ||
| 0 | 37 (23.6) | 120 (27.0) | |
| ≤9 | 101 (64.3) | 281 (63.3) | |
| >9 | 12(7.6) | 24 (5.4) | |
| Primary family caregiversa | 0.865 | ||
| First class relative | 102 (65.0) | 293 (66.0) | |
| Other | 49 (31.2) | 136 (30.6) | |
| Family historya | 0.704 | ||
| Positive | 5 (3.2) | 17 (3.8) | |
| Negative | 151 (96.2) | 422 (95.0) |
Note: aThe sample size does not correspond to 601 due to the presence of missing data.
Antipsychotics and mortality
Results of both the crude and adjusted conditional logistic regression analyses of the whole population are summarized (Table 2). Crude estimates for antipsychotics showed that compared with antipsychotic-free patients, the risk of mortality decreased significantly for antipsychotic monotherapy (p<0.001) and antipsychotic polypharmacy (p<0.01), even after adjusting for the variables in the final model. Besides, crude estimates for antipsychotics revealed that compared with antipsychotic monotherapy patients, the risk of death increased significantly in antipsychotic-free patients group (p<0.001); but no such difference was observed between antipsychotic monotherapy and antipsychotic polypharmacy even after adjusting for the variables in the final model.
Table 2.
Odds ratio of the association between mortality from natural causes and medication
| Group comparison | Crude OR | 95% CI | p-value | Adjusted OR | 95% CI | p-value |
|---|---|---|---|---|---|---|
| 1 vs 0 | 0.28 | 0.18–0.45 | 0.000 | 0.27 | 0.16–0.46 | 0.000 |
| 2 vs 0 | 0.27 | 0.13–0.58 | 0.001 | 0.29 | 0.12–0.70 | 0.005 |
| 0 vs 1 | 3.56 | 2.25–5.64 | 0.000 | 3.64 | 2.18–6.08 | 0.000 |
| 2 vs 1 | 0.97 | 0.44–2.11 | 0.930 | 1.07 | 0.46–2.53 | 0.871 |
Notes: Adjusted for covariates in the final model of whole population (antipsychotics concomitant categories, comorbidity, and benzhexol); 0: no antipsychotic use; 1: monotherapy; 2: 2 or 2 more antipsychotic use.
Abbreviations: OR, odds ratio; CI, confidence interval.
Subgroup analysis
When stratifying by gender and age, the result was in line with the whole population indicating that the treatment effect of antipsychotics is better than antipsychotic-free; and antipsychotic polypharmacy did not contribute to the excess mortality (Table 3).
Table 3.
Odds ratio of the association between mortality from natural causes and medication, stratified by gender, age, and year
| Group comparison | Crude OR | 95% CI | p-value | Adjusted OR | 95%CI | p-value |
|---|---|---|---|---|---|---|
| 1 vs 0 | 0.41a | 0.24–0.71a | 0.002 | 0.42a | 0.23–0.77a | 0.005 |
| 0.13b | 0.06–0.32b | 0.000 | 0.11b | 0.04–0.30b | 0.000 | |
| 0.11c | 0.04–0.33c | 0.000 | 0.06c | 0.01–0.27c | 0.000 | |
| 0.10d | 0.03–0.34d | 0.000 | 0.09d | 0.02–0.34d | 0.000 | |
| 2 vs 0 | 0.31a | 0.13–0.77a | 0.012 | 0.33a | 0.11–0.95a | 0.041 |
| 0.23b | 0.06–0.89b | 0.034 | 0.22b | 0.05–0.97b | 0.046 | |
| 0.12c | 0.02–0.68c | 0.016 | 0.05c | 0.00–0.70c | 0.025 | |
| 0.13d | 0.01–1.12d | 0.063 | 0.08d | 0.01–1.43d | 0.087 | |
| 0 vs 1 | 2.43a | 1.40–4.21a | 0.002 | 2.39a | 1.30–4.39a | 0.005 |
| 7.50b | 3.17–17.74b | 0.000 | 9.45b | 3.35–26.63b | 0.000 | |
| 8.79c | 3.07–25.12c | 0.000 | 15.89c | 3.68–68.58c | 0.000 | |
| 9.61d | 2.96–31.18d | 0.000 | 11.70d | 2.97–46.03d | 0.000 | |
| 2 vs 1 | 0.76a | 0.30–1.90a | 0.553 | 0.79a | 0.28–2.23a | 0.651 |
| 1.74b | 0.40–7.61b | 0.463 | 2.09b | 0.44–9.77b | 0.351 | |
| 1.08c | 0.19–6.03c | 0.927 | 0.87c | 0.07–10.43c | 0.914 | |
| 1.23d | 0.13–11.73d | 0.857 | 0.99d | 0.08–12.94d | 0.997 |
Notes: aAdjusted for covariates in the final model of male (antipsychotics concomitant categories, comorbidity, and benzhexol). bAdjusted for covariates in the final model of female (antipsychotics concomitant categories, comorbidity, and benzhexol). cAdjusted for covariates in the final model during 40–49 years (antipsychotics concomitant categories, comorbidity, and benzhexol). dAdjusted for covariates in the final model during 60–65 years (antipsychotics concomitant categories, comorbidity, and benzhexol); 0: no antipsychotic use; 1: monotherapy; 2: 2 or 2 more antipsychotic use.
Abbreviations: OR, odds ratio; CI, confidence interval.
Discussion
In this population-based nested case–control study involving 601 patients with schizophrenia, we found the risk of mortality decreased significantly for antipsychotics use, especially antipsychotic monotherapy; and antipsychotics polypharmacy did not contribute to the excess mortality.
Antipsychotics
Our results showed a considerably decreased risk of natural death in schizophrenic patients with antipsychotics use. This finding was confirmed by some previous reports;4,15–18 however, contradictory findings have been reported by others. Two long-term prospective analyses of premature mortality in schizophrenia suggested that risk for death in schizophrenia was increased with the introduction of antipsychotics.26,27 A systematic review suggested that long-term exposure to antipsychotics may be linked to increased mortality, while underlining that more rigorously designed, prospective studies are urgently needed.13 Jones et al, also reported that the use of antipsychotic agents was associated with increased risk of all-cause and cardiac mortality, whilst patients treated with olanzapine were found to be at increased risk of cardiac mortality vs psychiatric nonusers.28
Antipsychotic polypharmacy
Literature on the association of mortality and antipsychotic polypharmacy is inconclusive.9 In the present study, we found no increased risk of natural death in schizophrenia patients receiving antipsychotic polypharmacy. This finding goes in line with some previous reports.17 However, contradictory findings on the association of mortality and antipsychotics have been reported. Joukamaa et al, reported that the risk of death increased if the patients were taking more than one neuroleptic drug, that is, a 2.5-fold increased risk of natural death per antipsychotic agent added to the treatment regimens.29 Waddington et al, found that receiving antipsychotics polypharmacy was associated with an increased risk of natural death (relative risk=2.46, 95% CIs=1.10–5.47) in a prospective, 10-year follow-up of 88 people with schizophrenia.30 Hollis et al, reported an increased risk of all-cause mortality in patients receiving antipsychotic polypharmacy (OR=5.32, 95% CIs=3.49–8.10).31 In a study conducted in France, the mortality among patients with chronic schizophrenia was associated with the dosage of neuroleptics.32 Among patients with schizophrenia, however, the correlation between antipsychotic exposure and overall mortality is not always linear. Compared with age- and gender-matched controls from the general population, the highest overall mortality was observed among patients with no antipsychotic exposure (hazard ratio [HR] =6.3, 95% CIs=5.5–7.3), followed by high exposure group (HR =5.7, 5.2–6.2), low exposure group (HR =4.1, 3.6–4.6), and moderate exposure group (HR =4.0, 3.7–4.4).16
As for the efficacy of antipsychotic polypharmacy and monotherapy, Essock et al, found that switching from polypharmacy to monotherapy was followed by treatment discontinuation more often and more quickly than polypharmacy was continued. However, two-thirds of patients succeeded in switching from polypharmacy to monotherapy and experienced a loss in body mass index without worsening of symptom control or increase in hospitalizations.24 In one small open label study in which 47 individuals switched to monotherapy, 10 (23%) worsened significantly, but 24 (55%) remained stable and 10 (23%) improved.33 These results support the reasonableness of prescribing guidelines encouraging trials of antipsychotic monotherapy for individuals receiving antipsychotic polypharmacy, with the caveat that patients should be free to return to polypharmacy if an adequate trial on antipsychotic monotherapy proves unsatisfactory. Nevertheless, a naturalistic study conducted in Hungary indicates the superiority of monotherapy over polypharmacy for second generation antipsychotics in terms of all-cause treatment discontinuation in schizophrenia, and polypharmacy was associated with a significantly lower likelihood of mortality and hospitalizations.34
Antipsychotic polypharmacy as a widely used prescription pattern in clinical practice may be explained by the lack of response to a single antipsychotic or the severity of the illness. Taken together, antipsychotic polypharmacy fortunately does not seem to shorten life spans of our patients in the observational study. Yet, we still intend to design a long-term prospective follow-up study in the future.
Strengths and limitations
The present study has quite a number of notable strengths. First, the study has a relatively large sample, as opposed to existing cohort counterparts, which has given it a big statistical power. Second, recall bias was avoided thanks to the comparatively complete registration of all filled prescriptions, which enabled us to assess the entire drug use pattern for all participants and to determine drug exposure immediately after death. Third, we excluded unnatural death and unknown manners of death, thus eliminating suicide as a potential confounder. Fourth, potential bias was further minimized as we adjusted for demographic and clinical variables, and adjusted for lifestyle factors (smoking and alcohol intake), which were potential risk factors for mortality of schizophrenia. Last but not the least essential, the present study is the first of its kind studying the Chinese population. To our knowledge, research on the association between antipsychotics and early mortality in schizophrenia has primarily derived from Western countries. China, however, differs largely from most Western countries in health and social welfare systems, and Asian patients are more susceptible to side-effects and might require less antipsychotic medication than their Western counterparts.35,36 This implies that the association between mortality and antipsychotic use for Western patients with schizophrenia may not be generalized to the Chinese population directly.
Despite these significant findings, however, our study still has some limitations. One is that we were unable to adjust precisely for all variables, which are known potential risk factors regarding mortality in schizophrenia,6,37 such as the general physical condition of patients. Although the government offers free physical examination, many patients with schizophrenia did not take the physical examination. This may be attributed to their low adherence as some of them are physically inactive and are reluctant to go to hospital or to the stigma of mental illness felt by themselves and their family. In addition, many psychiatrists have limited opportunity to exercise and consolidate the patients’ physical skills, thus unable to provide them with satisfactory physical assessments.38 Second, we could not ensure that antipsychotics were taken by the patients as prescribed because the monitoring over health education by community mental health staff is poor.39 A lot of primary caregivers could not fulfill their duty such as medicine management, hospital visit, financial help, and daily activities as they should have due to low socio-economic position, absence or inadequacy of professional medical knowledge and skills, time, and money.40 Third, we did not use the 30-item Positive and Negative Syndrome Scale to evaluate the severity of schizophrenia although it is the most widely used measure of illness severity and its total score is the gold standard primary efficacy measure in acute treatment studies of schizophrenia. Finally, we did not include long-stay patients in that exposure during this period is immeasurable because no prescription could be obtained during hospitalization.
Conclusion
In conclusion, antipsychotic monotherapy remains the optimal choice and in accordance with the guidelines; and antipsychotic polypharmacy did not cause excess mortality from natural causes in patients with schizophrenia. Nevertheless, antipsychotic polypharmacy should be used with caution and only when necessary because it lacks evidence of superior safety and increases costs and occurrence of side-effects. In addition, we need to improve physical health of patients with schizophrenia and further promote community health education among mental health workers and primary caregivers.
Acknowledgments
We thank Prof. Dongtao Lin, of Sichuan University for copyediting this manuscript and all individuals who have participated in this study. We acknowledge the support of the Severe Mental Health Disorder System of Chengdu, Sichuan Province. This research was partly funded by National Natural Science Foundation of China (Grant No. 81671344) and 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Insel TR. Rethinking schizophrenia. Nature. 2010;468(7321):187–193. doi: 10.1038/nature09552 [DOI] [PubMed] [Google Scholar]
- 2.Lieberman JA. Is schizophrenia a neurodegenerative disorder? A clinical and neurobiological perspective. Biol Psychiatry. 1999;46(6):729–739. [DOI] [PubMed] [Google Scholar]
- 3.Kim DH, Maneen MJ, Stahl SM. Building a better antipsychotic: receptor targets for the treatment of multiple symptom dimensions of schizophrenia. Neurotherapeutics. 2009;6(1):78–85. doi: 10.1016/j.nurt.2008.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tiihonen J, Lonnqvist J, Wahlbeck K, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet (London, England). 2009;374(9690):620–627. doi: 10.1016/S0140-6736(09)60742-X [DOI] [PubMed] [Google Scholar]
- 5.Allebeck P, Rodvall Y, Wistedt B. Incidence of rheumatoid arthritis among patients with schizophrenia, affective psychosis and neurosis. Acta Psychiatr Scand. 1985;71(6):615–619. [DOI] [PubMed] [Google Scholar]
- 6.Brown S. Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry. 1997;171:502–508. [DOI] [PubMed] [Google Scholar]
- 7.Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72(12):1172–1181. doi: 10.1001/jamapsychiatry.2015.1737 [DOI] [PubMed] [Google Scholar]
- 8.Jeste DV, Gladsjo JA, Lindamer LA, Lacro JP. Medical comorbidity in schizophrenia. Schizophr Bull. 1996;22(3):413–430. doi: 10.1093/schbul/22.3.413 [DOI] [PubMed] [Google Scholar]
- 9.Auquier P, Lancon C, Rouillon F, Lader M, Holmes C. Mortality in schizophrenia. Pharmacoepidemiol Drug Saf. 2006;15(12):873–879. doi: 10.1002/pds.1325 [DOI] [PubMed] [Google Scholar]
- 10.Brown S, Inskip H, Barraclough B. Causes of the excess mortality of schizophrenia. Br J Psychiatry. 2000;177:212–217. [DOI] [PubMed] [Google Scholar]
- 11.Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Davis JM. Maintenance treatment with antipsychotic drugs for schizophrenia. Cochrane Database of Syst Rev. 2012;5:Cd008016. [DOI] [PubMed] [Google Scholar]
- 12.Leucht S, Tardy M, Komossa K, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet (London, England). 2012;379(9831):2063–2071. doi: 10.1016/S0140-6736(12)60239-6 [DOI] [PubMed] [Google Scholar]
- 13.Weinmann S, Read J, Aderhold V. Influence of antipsychotics on mortality in schizophrenia: systematic review. Schizophr Res. 2009;113(1):1–11. doi: 10.1016/j.schres.2009.05.018 [DOI] [PubMed] [Google Scholar]
- 14.Tiihonen J, Mittendorfer-Rutz E, Torniainen M, Alexanderson K, Tanskanen A. Mortality and cumulative exposure to antipsychotics, antidepressants, and benzodiazepines in patients with schizophrenia: an observational follow-up study. Am J Psychiatry. 2016;173(6):600–606. doi: 10.1176/appi.ajp.2015.15050618 [DOI] [PubMed] [Google Scholar]
- 15.Tiihonen J, Haukka J, Taylor M, Haddad PM, Patel MX, Korhonen P. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry. 2011;168(6):603–609. doi: 10.1176/appi.ajp.2011.10081224 [DOI] [PubMed] [Google Scholar]
- 16.Torniainen M, Mittendorfer-Rutz E, Tanskanen A, et al. Antipsychotic treatment and mortality in schizophrenia. Schizophr Bull. 2015;41(3):656–663. doi: 10.1093/schbul/sbu164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baandrup L, Gasse C, Jensen VD, et al. Antipsychotic polypharmacy and risk of death from natural causes in patients with schizophrenia: a population-based nested case-control study. J Clin Psychiatry. 2010;71(2):103–108. doi: 10.4088/JCP.08m04818yel [DOI] [PubMed] [Google Scholar]
- 18.Crump C, Winkleby MA, Sundquist K, Sundquist J. Comorbidities and mortality in persons with schizophrenia: a swedish national cohort study. Am J Psychiatry. 2013;170(3):324–333. doi: 10.1176/appi.ajp.2012.12050599 [DOI] [PubMed] [Google Scholar]
- 19.Cullen BA, McGinty EE, Zhang Y, et al. Guideline-concordant antipsychotic use and mortality in schizophrenia. Schizophr Bull. 2013;39(5):1159–1168. doi: 10.1093/schbul/sbs097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mace S, Taylor D. Reducing the rates of prescribing high-dose antipsychotics and polypharmacy on psychiatric inpatient and intensive care units: results of a 6-year quality improvement programme. Ther Adv Psychopharmacol. 2015;5(1):4–12. doi: 10.1177/2045125314558054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel MX, Bishara D, Jayakumar S, et al. Quality of prescribing for schizophrenia: evidence from a national audit in England and Wales. Eur Neuropsychopharmacol. 2014;24(4):499–509. doi: 10.1016/j.euroneuro.2014.01.014 [DOI] [PubMed] [Google Scholar]
- 22.Correll CU, Rummel-Kluge C, Corves C, Kane JM, Leucht S. Antipsychotic combinations vs monotherapy in schizophrenia: a meta-analysis of randomized controlled trials. Schizophr Bull. 2009;35(2):443–457. doi: 10.1093/schbul/sbn018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Josiassen RC, Joseph A, Kohegyi E, et al. Clozapine augmented with risperidone in the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2005;162(1):130–136. doi: 10.1176/appi.ajp.162.1.130 [DOI] [PubMed] [Google Scholar]
- 24.Essock SM, Schooler NR, Stroup TS, et al. Effectiveness of switching from antipsychotic polypharmacy to monotherapy. Am J Psychiatry. 2011;168(7):702–708. doi: 10.1176/appi.ajp.2011.10060908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centorrino F, Goren JL, Hennen J, Salvatore P, Kelleher JP, Baldessarini RJ. Multiple versus single antipsychotic agents for hospitalized psychiatric patients: case-control study of risks versus benefits. Am J Psychiatry. 2004;161(4):700–706. doi: 10.1176/appi.ajp.161.4.700 [DOI] [PubMed] [Google Scholar]
- 26.Montout C, Casadebaig F, Lagnaoui R, et al. Neuroleptics and mortality in schizophrenia: prospective analysis of deaths in a French cohort of schizophrenic patients. Schizophr Res. 2002;57(2–3):147–156. [DOI] [PubMed] [Google Scholar]
- 27.Morgan MG, Scully PJ, Youssef HA, Kinsella A, Owens JM, Waddington JL. Prospective analysis of premature mortality in schizophrenia in relation to health service engagement: a 7.5-year study within an epidemiologically complete, homogeneous population in rural Ireland. Psychiatry Res. 2003;117(2):127–135. [DOI] [PubMed] [Google Scholar]
- 28.Jones ME, Campbell G, Patel D, et al. Risk of mortality (including sudden cardiac death) and major cardiovascular events in users of olanzapine and other antipsychotics: a study with the general practice research database. Cardiovasc Psychiatry Neurol. 2013;2013:647476. doi: 10.1155/2013/647476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joukamaa M, Heliovaara M, Knekt P, Aromaa A, Raitasalo R, Lehtinen V. Schizophrenia, neuroleptic medication and mortality. Br J Psychiatry. 2006;188:122–127. doi: 10.1192/bjp.188.2.122 [DOI] [PubMed] [Google Scholar]
- 30.Waddington JL, Youssef HA, Kinsella A. Mortality in schizophrenia. Antipsychotic polypharmacy and absence of adjunctive anticholinergics over the course of a 10-year prospective study. Br J Psychiatry. 1998;173:325–329. [DOI] [PubMed] [Google Scholar]
- 31.Hollis J, Touyz S, Grayson D, Forrester L. Antipsychotic medication dispensing and associated odds ratios of death in elderly veterans and war widows, 2001. Aust N Z J Psychiatry. 2006;40(11–12):981–986. doi: 10.1080/j.1440-1614.2006.01920.x [DOI] [PubMed] [Google Scholar]
- 32.Bralet MC, Yon V, Loas G, Noisette C. [Cause of mortality in schizophrenic patients: prospective study of years of a cohort of 150 chronic schizophrenic patients]. L’Encephale. 2000;26(6):32–41. [PubMed] [Google Scholar]
- 33.Suzuki T, Uchida H, Tanaka KF, et al. Revising polypharmacy to a single antipsychotic regimen for patients with chronic schizophrenia. Int J Neuropsychopharmacol. 2004;7(2):133–142. doi: 10.1017/S1461145703004012 [DOI] [PubMed] [Google Scholar]
- 34.Katona L, Czobor P, Bitter I. Real-world effectiveness of antipsychotic monotherapy vs. polypharmacy in schizophrenia: to switch or to combine? A nationwide study in Hungary. Schizophr Res. 2014;152(1):246–254. doi: 10.1016/j.schres.2013.10.034 [DOI] [PubMed] [Google Scholar]
- 35.Ungvari GS, Pang AH, Chiu HF, Wong CK, Lum FC. Psychotropic drug prescription in rehabilitation. A survey in Hong Kong. Soc Psychiatry Psychiatr Epidemiol. 1996;31(5):288–291. [DOI] [PubMed] [Google Scholar]
- 36.Chong MY, Tan CH, Fujii S, et al. Antipsychotic drug prescription for schizophrenia in East Asia: rationale for change. Psychiatry Clin Neurosci. 2004;58(1):61–67. [DOI] [PubMed] [Google Scholar]
- 37.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–1131. doi: 10.1001/archpsyc.64.10.1123 [DOI] [PubMed] [Google Scholar]
- 38.Rigby JC, Oswald AG. An evaluation of the performing and recording of physical examinations by psychiatric trainees. Br J Psychiatry. 1987;150:533–535. [DOI] [PubMed] [Google Scholar]
- 39.Gournay K. Setting clinical standards for care in schizophrenia. Nurs Times. 1996;92(7):36–37. [PubMed] [Google Scholar]
- 40.Yu Y, Tang BW, Liu ZW, Chen YM, Zhang XY, Xiao S. Who cares for the schizophrenia individuals in rural China – a profile of primary family caregivers. Compr Psychiatry. 2018;84:47–53. doi: 10.1016/j.comppsych.2018.04.002 [DOI] [PubMed] [Google Scholar]