Abstract
Background
In Japan and other countries, the number of patients with syphilis is increasing year by year. Recently, the cases of the pulmonary involvement in patients with secondary syphilis have been reported. However, it is still undetermined how to obtain a desirable specimen for a diagnosis of the pulmonary involvement, and how to treat it if not cured.
Case presentation
A 34-year-old man presented with cough and swelling of the right inguinal nodes. A physical examination revealed erythematous papular rash over the palms, soles and abdomen. A 4 cm mass in the right lower lobe of the lung was detected on computed tomography. He was diagnosed as having secondary syphilis, because he was tested positive for the rapid plasma reagin and Treponema pallidum hemagglutination assay. Amoxycillin and probenecid were orally administered for 2 weeks. Subsequently, rash and serological markers were improved, however, the lung mass remained unchanged in size. Transbronchial biopsy (TBB) confirmed the pulmonary involvement of syphilis using polymerase chain reaction techniques (tpp47- and polA-PCR). Furthermore, following surgical resection revealed the lung mass to be an abscess.
Conclusions
To our knowledge, this is the first surgically treated case of a lung abscess caused by syphilis, which was diagnosed by PCR techniques in TBB. This report could propose a useful diagnostic method for the pulmonary involvement of syphilis.
Keywords: Secondary syphilis, Lung abscess, Polymerase chain reaction, Transbronchial biopsy, Surgical treatment, Case report
Background
Syphilis is a sexually transmitted disease caused by infection with Treponema pallidum, which is classified into four stages (primary, secondary, latent and tertiary). If the patients with primary syphilis do not receive treatment, the bacterium will spread through their bloodstream, and set the stage for secondary syphilis. Syphilis can cause a wide range of systemic manifestations, such as papular rash, malaise, weight loss, muscle aches, generalized lymphadenopathy and meningitis [1]. In Japan and other countries, the number of patients with syphilis is increasing year by year [2–4]. Recently, several dozen reports showed the pulmonary involvement in patients with secondary syphilis [5–16]; however, it is still undetermined how to obtain a desirable specimen for a diagnosis of the pulmonary involvement, and how to treat it if not cured.
Here, we report a rare case of a lung abscess caused by secondary syphilis, that was definitely diagnosed by polymerase chain reaction (PCR) tests from the transbronchial biopsy (TBB) specimen and followed by surgery.
Case presentation
A 34-year-old Japanese heterosexual man presented to our hospital with a 4 cm heterogeneous mass in the right lower lobe (Fig. 2). He had had a symptom of productive coughing, sore throat and nasal discharge for 5 days, but he had no fever and no dyspnea, and his general condition was good. He had a medical history of minimal lesion nephrotic syndrome and had received corticosteroid therapy until 4 months prior to his first visit to our institution. He was a current smoker (15 pack-years). He had had sexual intercourse with a woman other than his wife 4 months prior to his first visit. Physical examination revealed right inguinal nontender enlarged lymph nodes, and erythematous papular rash over the palms, soles and abdomen (Fig. 1). However, cervical and supraclavicular lymph nodes were not palpable, and he did not have abnormal neurologic findings.
Fig. 2.
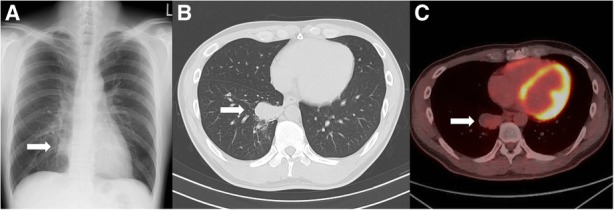
Images of the lung mass. a Chest X-ray on the first visit to our hospital. A mass lesion was shown in the right lower field (arrow), b Chest computed tomography on the first visit to our hospital. A single mass lesion (4 cm in size) was shown in the right lower lobe of the lung (arrow), c Fluorodeoxyglucose-positron emission tomography (FDG-PET) before the surgery, 4 months after the first visit. A single mass lesion was still remained in spite of the antibiotic treatment. It had abnormal uptake with a maximal standardized uptake value (SUV max) of 2.51 (arrow)
Fig. 1.

Erythematous popular rash. a: Erythematous popular rash over the solesm, b: Erythematous popular rash over the abdomen
C-reactive protein level was elevated at 1.02 mg/dL as shown in the laboratory tests (Table 1). The rapid plasma reagin (RPR) and Treponema pallidum hemagglutination test (TPHA) revealed titers 1:64 and 1:5,120, respectively, although Human immunodeficiency virus testing was negative. Chest X-ray (Fig. 2a) and computed tomography (Fig. 2b) revealed a single mass lesion (4 cm in size) in the right lower lobe, and enlarged lymph nodes (4.5 cm in size) in the right inguinal region.
Table 1.
Laboratory findings on the first visit to our institution
| < Blood cell count > | |
| White blood cell | 7,150 /μL |
| Red blood cell | 520 × 104 /μL |
| Hemoglobin | 14.8 g/dL |
| Platelet | 27.8 × 104 /μL |
| < Serum chemistry> | |
| Total protein | 8.1 g/dL |
| Albumin | 4.6 g/dL |
| Total-bilirubin | 0.5 mg/dL |
| Alkaline phosphatase | 252 IU/L |
| Aspartate transaminase | 15 IU/L |
| Alanine transaminase | 23 IU/L |
| γ-Glutamyl transpeptidase | 30 IU/L |
| Lactate dehydrogenase | 158 IU/L |
| Blood urea nitrogen | 11 mg/dL |
| Creatinine | 0.84 mg/dL |
| C-reactive protein | 1.02 mg/dL |
| Sodium | 141 mmol/L |
| Potassium | 4.4 mmol/L |
| Chlorine | 103 mmol/L |
| < Coagulation> | |
| Prothrombin time (International normalized ratio) | 1.09 |
| Activated partial thromboplastin time | 50 s |
| < Infection > | |
| Rapid plasma reagin test | Positive (titers 1:64) |
| Treponema pallidum hemagglutination test | Positive (titers 1:5,120) |
| Hepatitis B surface antigen | Negative |
| Hepatitis C antibody | Negative |
| Human immunodeficiency virus antibody | Negative |
| Aspergillus antigen | Negative |
| Cryptococcus antigen | Negative |
| < Tumor marker > | |
| Carcinoembryonic antigen | < 1 ng/mL |
| Soluble cytokeratin fragment | 0.5 ng/mL |
| Pro-gastrin releasing peptide | 27.0 pg/mL |
| <Autoantibody> | |
| Proteinase3-antineutrophil cytoplasmic antibody | < 1 U/mL |
| Myeroperoxidase-antineutrophil cytoplasmic antibody | < 1 U/mL |
Diagnosed as secondary syphilis, amoxycillin 1500 mg per day and probenecid 1000 mg per day were orally administered for 2 weeks. Subsequently, rash, inguinal lymph nodes and serological markers were improved (Fig. 3), however, the lung mass remained unchanged in size (Fig. 2c). TBB confirmed the pulmonary involvement of syphilis by PCR techniques (tpp47-, and polA-PCR) (Fig. 4), whereas malignancy and other possible infections such as bacteria and fungi were negative (Table 2). Five months after the first visit, right basal segmentectomy was performed to exclude other comorbid diseases, especially malignancy. The remained lung mass was an abscess and histological analysis showed the granuloma formation by epithelioid histiocytes and Langhans giant cells with necrosis (Fig. 5). The comprehensive PCR tests for multi-microbes were performed in the resected lung specimens, and no microbes were significantly positive (Table 2). Subsequently, penicillin G 2.4 million units per day was intravenously administered for 2 weeks, and the pulmonary involvement has resolved without relapse after 8 months follow-up.
Fig. 3.
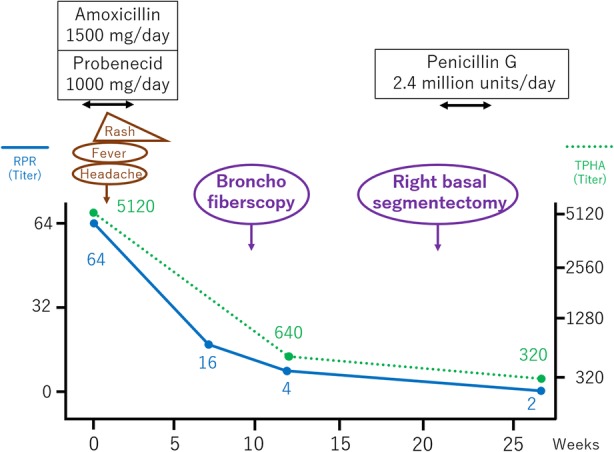
Clinical course of the treatment. The induction of the oral antibiotics caused fever, headache and exacerbation of erythematous papular rash on the next day, which was considered as Jarisch-Herxheimer reaction. Treatment for 2 weeks improved the rash and serological data. However, the lung mass had not changed in size. Surgical resection was followed, and then, additional intravenous antibiotics for 2 weeks was administered. Abbreviation; rapid plasma reagin test: RPR; Treponema pallidum hemagglutination test: TPHA
Fig. 4.
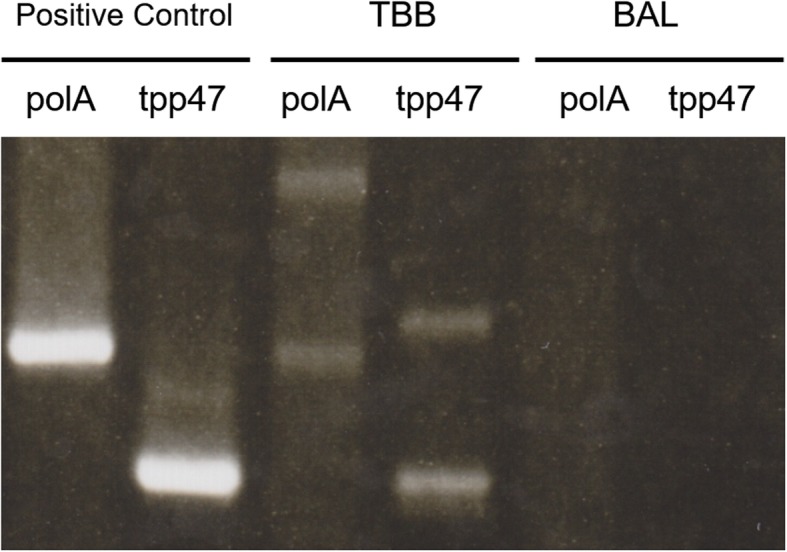
Electrophoresis of the amplified products from the lung mass with polymerase chain reaction (PCR) techniques. BAL was performed with 20 mL saline. The two types of gene fragments of Treponema pallidum (tpp47 and polA) acquired from bronchoalveolar lavage (BAL) and transbronchial biopsy (TBB) was amplified by PCR techniques. Both gene fragments were positive in samples from TBB, but not BAL
Table 2.
Microbiological analysis in specimens obtained by bronchofiberscopy and surgery
| 1. Bronchofiberscopy | ||
| PCR tests for Treponema pallidum | ||
| Bronchoalveolar lavage | Undetected | |
| TBB | Detected (tpp47-PCR and polA-PCR) | |
| Culture tests for bacteria and mycobacteria | ||
| Bronchoalveolar lavage | Undetected | |
| Lavage of forceps in TBB | Undetected | |
| 2. Surgery | ||
| Real-time PCR tests for Treponema pallidum | Undetected | |
| Culture test for bacteria in pus inside the abscess | Undetected | |
| Real-time PCR tests for multi-microbes [17] | ||
| Number | Bacteria name | Quantity |
| 1 | Staphylococcus aureus | Undetected |
| 2 | Bacillus anthracis | Undetected |
| 3 | Listeria monocytogenes | Undetected |
| 4 | Streptococcus pyogenes | Undetected |
| 5 | Streptococcus agalactiae | Undetected |
| 6 | Streptococcus mutans | Undetected |
| 7 | Streptococcus sobrinus | Undetected |
| 8 | Streptococcus sanguinis | Undetected |
| 9 | Streptococcus oralis | Undetected |
| 10 | Streptococcus salivaris | Undetected |
| 11 | Streptococcus pneumoniae | Undetected |
| 12 | Enterococcus faecalis | Undetected |
| 13 | Enterococcus faecium | Undetected |
| 14 | Clostridium tetani | Undetected |
| 15 | Clostridium difficile | Undetected |
| 16 | Peptostreptococcus anaerobius | Undetected |
| 17 | Actinomyces | Undetected |
| 18 | Corynebacterium diphtheriae | Undetected |
| 19 | Mycobacterium tuberculosis | Undetected |
| 20 | Mycobacterium laprae | Undetected |
| 21 | Mycobacterium chelonae | Undetected |
| 22 | Mycobacterium kansasii | Undetected |
| 23 | Mycobacterium avium complex | Undetected |
| 24 | Nocardia asteroids | Undetected |
| 25 | Bacteroides fragills | Undetected |
| 26 | Elizabethkingia meningosepticum | Undetected |
| 27 | Campylobacter jejuni | Undetected |
| 28 | Helicobacter cinaedi | Undetected |
| 29 | Helicobacter pylori | Undetected |
| 30 | Rickettsia prowazekii | Undetected |
| 31 | Rickettsia japonica | Undetected |
| 32 | Orientia tsutsugamushi | Undetected |
| 33 | Bartonella henselae | Undetected |
| 34 | Brucella | Undetected |
| 35 | Bordetella pertussis | Undetected |
| 36 | Burkhoderia mallei | Undetected |
| 37 | Burkhoderia cepacian | Undetected |
| 38 | Neisseria gonorrhoeae | Undetected |
| 39 | Neisseria meningitidis | Undetected |
| 40 | Francisella tularensis | Undetected |
| 41 | Legionella pneumophilia | Undetected |
| 42 | Moraxella catarrhalis | Undetected |
| 43 | Pseudomonas aeruginosa | Undetected |
| 44 | Acinetobacter baumannii | Undetected |
| 45 | Aeromonas hydrophia | Undetected |
| 46 | Vibrio cholerae | Undetected |
| 47 | Vibrio parahaemolyticus | Undetected |
| 48 | Vibrio vulnificus | Undetected |
| 49 | Haemophilus influenzae | Undetected |
| 50 | Escherichia coli | Undetected |
| 51 | Salmonella enterica | Undetected |
| 52 | Shigella | Undetected |
| 53 | Klebsiella pneumonia | Undetected |
| 54 | Yersinia psttis | Undetected |
| 55 | Yersinia enterocolitica | Undetected |
| 56 | Citrobacter freundii | Undetected |
| 57 | Proteus mirabilis | Undetected |
| 58 | Morganella morganii | Undetected |
| 59 | Providencia | Undetected |
| 60 | Mycoplasma pneumoniae | Undetected |
| 61 | Fusobacterium nucleatum | Undetected |
| 62 | Leptospira interrogans | Undetected |
| 63 | Chlamydia psittaci | Undetected |
| 64 | Chlamydia trachomatis | Undetected |
| 65 | Chlamydia pneumoniae | Undetected |
| 66 | Aspergillus fumigatus | Undetected |
| 67 | Aspergillus nigar | Undetected |
| 68 | Aspergillus flavus | Undetected |
| 69 | Cryptococcus | Undetected |
| 70 | Histoplasma | Undetected |
| 71 | Trichosporon | Undetected |
| 72 | Mucor | Undetected |
| 73 | Coccidioides | Undetected |
| 74 | Propionibacterium acnes | Detected (not significant) |
| 75 | Stenotrophomonas maltophilia | Detected (not significant) |
| 76 | Candida albicans | Detected (not significant) |
Abbreviations: TBB Transbronchial biopsy, PCR Polymerase chain reaction
Fig. 5.

Gross and microscopic pathology of lung specimens obtained by surgery a Gross pathology showed pus inside the lung abscess (arrow), b Microscopic pathology showed granuloma formation by epithelioid histiocytes and Langhans giant cells (arrow), in addition to necrosis (arrow-head). Original Magnification X100. Hematoxylin and eosin (HE) staining
Discussion and conclusions
This is a rare case of a lung abscess caused by secondary syphilis, that was diagnosed by PCR techniques in TBB. The abscess was not improved by antibiotics and required surgery.
Coleman showed the criteria for the clinical diagnosis of secondary syphilis with pulmonary involvement in 1983 [5], and several dozen cases have been reported [6–16]. In some of them, PCR was used for the diagnosis of pulmonary involvement (Table 3) [13–16]. PCR is useful for the diagnosis of the infection of Treponema pallidum [18, 19], because it is difficult to directly visualize Treponema pallidum. In those reports, PCR was used in samples from TBB, bronchoalveolar lavage (BAL), bronchial aspirate, or computed tomography-guided percutaneous needle aspiration (CTNA) [13–16]. Thus far, only one case has been reported on lung abscess caused by secondary syphilis, that was diagnosed by PCR in CTNA [15]. In our case, the results of PCR in samples from TBB, but not BAL, was positive. For the detection of some infectious diseases, TBB or the combination of BAL and TBB was reported to be useful [20, 21]. Thus, it could be important to perform TBB to detect the pulmonary involvement by Treponema pallidum.
Table 3.
Reported cases of secondary syphilis with pulmonary involvement which was diagnosed by PCR techniques
| Case no. | Age | Gender | Respiratory symptoms | Extrapulmonary symptoms | Chest imaging | Sample collection method | Reporting year | Reference |
|---|---|---|---|---|---|---|---|---|
| 1 | 34 | Male | Chest pain | Progressive weakening, anorexia, weight loss, and night sweats | Several bilateral, round, excavated opacities and subtracheal adenopathy | BAL | 2006 | [13] |
| 2 | 49 | Female | Dry cough | Disabling cervical pain, fever, and night sweats | Lung lobe parenchymal lesion | BAL and bronchial aspirate | 2015 | [14] |
| 3 | 30 | Male | Hemoptysis, chest pain, dyspnea | Fever and rash | a 3 cm, irregularly-shaped, well-defined consolidation and a 1 cm hilar node | CTNA | 2018 | [15] |
| 4 | 62 | Male | No respiratory symptoms | epigastric pain | Multiple nodular bibasilar subpleural nodules | TBB | 2018 | [16] |
Abbreviation: PCR Polymerase chain reaction, BAL Bronchoalveolar lavage, CTNA Computed tomography-guided percutaneous needle aspiration, TBB Transbronchial biopsy
The lung abscess was not improved by 2 weeks of oral antibiotics. It may be because penetration of antibiotics into the abscess was impaired. We treated the present case with amoxicillin and probenecid, because there is no insurance coverage for intramuscular penicillin for syphilis in Japan. Administration of intravenous penicillin G was considered as a more potent antibiotic treatment. However, as in this case, it is necessary to consider surgical resection as the treatment for uncontrolled infection and in order to exclude other diseases, including malignancy, when the lung involvement is poorly improved by antibiotics.
Lung lesions associated with syphilis are still rare, but the reported cases have been increasing as the number of patients with syphilis increases [5–16]. Thus, we should consider chest X-ray in the cases of the patients with syphilis who have pulmonary symptoms.
In conclusion, to our knowledge, this is the first surgically treated case of a lung abscess caused by syphilis, which was diagnosed by PCR techniques in TBB. This report could propose a useful diagnostic method for the pulmonary involvement of syphilis.
Acknowledgments
The authors thank Shu-Ichi Nakayama, Makoto Ohnishi (Department of Bacteriology I), and Harutaka Katano (Department of Pathology, National Institute of Infectious Diseases, Tokyo, Japan), for their assistance with the PCR techniques. The authors obtained patient permission to publish this information.
Abbreviations
- BAL
Bronchoalveolar lavage
- CTNA
Computed tomography-guided percutaneous needle aspiration
- PCR
Polymerase chain reaction
- RPR
Rapid plasma reagin test
- TBB
Transbronchial biopsy
- TPHA
Treponema pallidum hemagglutination test
Authors’ contributions
SF and TT drafted the manuscript. SF, TT and FN were responsible for the clinical care of the patient. SS, MH, MK and KM contributed to the acquisition of the TBB specimen. SK, KI, HH and IN analyzed and interpreted the patient’s data, including the microbiology data. YT, HK and AK critically revised the manuscript. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shinji Futami, Email: s-futami@imed3.med.osaka-u.ac.jp.
Takayuki Takimoto, Email: takimoto@imed3.med.osaka-u.ac.jp.
Futoshi Nakagami, Email: fnakagami@hp-gm.med.osaka-u.ac.jp.
Shingo Satoh, Email: s.satoh@imed3.med.osaka-u.ac.jp.
Masanari Hamaguchi, Email: masanari_hamaguchi@yahoo.co.jp.
Muneyoshi Kuroyama, Email: kuroyama18@outlook.jp.
Kotaro Miyake, Email: kotaromiyake@imed3.med.osaka-u.ac.jp.
Shohei Koyama, Email: koyama@imed3.med.osaka-u.ac.jp.
Kota Iwahori, Email: iwahori@climm.med.osaka-u.ac.jp.
Haruhiko Hirata, Email: charhirata@imed3.med.osaka-u.ac.jp.
Izumi Nagatomo, Email: iznagatomo@imed3.med.osaka-u.ac.jp.
Yoshito Takeda, Email: yoshito@imed3.med.osaka-u.ac.jp.
Hiroshi Kida, Email: hiroshi.kida@imed3.med.osaka-u.ac.jp.
Atsushi Kumanogoh, Email: kumanogo@imed3.med.osaka-u.ac.jp.
References
- 1.Ho EL, Lukehart SA. Syphilis: using modern approaches to understand an old disease. J Clin Invest. 2011;121(12):4584–4592. doi: 10.1172/JCI57173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sugishita Y, Yamagishi T, Arima Y, Hori N, Seki N. Increase in primary and secondary syphilis notifications in men in Tokyo, 2007-2013. Jpn J Infect Dis. 2016;69(2):154–157. doi: 10.7883/yoken.JJID.2015.312. [DOI] [PubMed] [Google Scholar]
- 3.Patton ME, Su JR, Nelson R, Weinstock H. Centers for Disease Control and Prevention (CDC). Primary and secondary syphilis--United States, 2005-2013. Morb Mortal Wkly Rep. 2014;63(18):402–406. [PMC free article] [PubMed] [Google Scholar]
- 4.Bremer V, Marcus U, Hamouda O. Syphilis on the rise again in Germany - results from surveillance data for 2011. Euro Surveill. 2012;17(29). [PubMed]
- 5.Coleman DL, McPhee SJ, Ross TF, Naughton JL. Secondary syphilis with pulmonary involvement. West J Med. 1983;138(6):875–878. [PMC free article] [PubMed] [Google Scholar]
- 6.Dooley DP, Tomski S. Syphilitic pneumonitis in an HIV-infected patient. Chest. 1994;105(2):629–631. doi: 10.1378/chest.105.2.629. [DOI] [PubMed] [Google Scholar]
- 7.Zaharopoulos P, Wong J. Cytologic diagnosis of syphilitic pleuritis: a case report. Diagn Cytopathol. 1997;16(1):35–38. doi: 10.1002/(SICI)1097-0339(199701)16:1<35::AID-DC8>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 8.Olson AL, Gutman JA, Welsh CH. A 50-year-old man with skin lesions and multiple pulmonary nodules. Chest. 2004;125(6):2322–2327. doi: 10.1378/chest.125.6.2322. [DOI] [PubMed] [Google Scholar]
- 9.Alrajab S, Payne K, Areno J, Holladay R, Smith T, Zhang S. A 40-year-old man with a nodular lung disease and skin rash. Chest. 2012;141(6):1611–1617. doi: 10.1378/chest.11-1100. [DOI] [PubMed] [Google Scholar]
- 10.Jeny F, Fargelat A, Laurent-Roussel S, et al. Pulmonary consolidations due to secondary syphilis with positive bronchial washing immunohistochemistry. Am J Respir Crit Care Med. 2016;193(9):1061–1062. doi: 10.1164/rccm.201511-2296IM. [DOI] [PubMed] [Google Scholar]
- 11.Ohta A, Furusyo N, Kishihara Y, et al. Secondary syphilis with pulmonary involvement. Intern Med. 2018;57(1):121–126. doi: 10.2169/internalmedicine.8439-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freitas DMM, Azevedo A, Pinheiro G, Ribeiro R. Psoriasiform papules, condyloma lata, lung nodules and hepatitis: the enormous variability of secondary syphilis manifestations. BMJ Case Rep. 10.1136/bcr-2017-219408. [DOI] [PMC free article] [PubMed]
- 13.David G, Perpoint T, Boibieux A, et al. Secondary pulmonary syphilis: report of a likely case and literature review. Clin Infect Dis. 2006;42(3):e11–e15. doi: 10.1086/499104. [DOI] [PubMed] [Google Scholar]
- 14.Crouzy F, Alvarez V, Gex G, Troillet N. Unusual presentations and pitfalls of secondary syphilis: osteitis, pneumonia and malignancy. BMJ Case Rep. 2015. 10.1136/bcr-2015-210618. [DOI] [PMC free article] [PubMed]
- 15.Visuttichaikit S, Suwantarat N, Apisarnthanarak A, Damronglerd P. A case of secondary syphilis with pulmonary involvement and review of the literature. Int J STD AIDS. 2018;29(10):1027–1032. doi: 10.1177/0956462418765834. [DOI] [PubMed] [Google Scholar]
- 16.Ogawa Y, Imai Y, Yoshihara S, et al. Pulmonary involvement of secondary syphilis. Int J STD AIDS. 2018;29(1):89–91. doi: 10.1177/0956462417717653. [DOI] [PubMed] [Google Scholar]
- 17.Fukumoto H, Sato Y, Hasegawa H, Saeki H, Katano H. Development of a new real-time PCR system for simultaneous detection of bacteria and fungi in pathological samples. Int J Clin Exp Pathol. 2015;8(11):15479–15488. [PMC free article] [PubMed] [Google Scholar]
- 18.Liu H, Rodes B, Chen CY, Steiner B. New tests for syphilis: rational design of a PCR method for detection of Treponema pallidum in clinical specimens using unique regions of the DNA polymerase I gene. J Clin Microbiol. 2001;39(5):1941–1946. doi: 10.1128/JCM.39.5.1941-1946.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orle KA, Gates CA, Martin DH, Body BA, Weiss JB. Simultaneous PCR detection of Haemophilus ducreyi, Treponema pallidum, and herpes simplex virus types 1 and 2 from genital ulcers. J Clin Microbiol. 1996;34(1):49–54. doi: 10.1128/jcm.34.1.49-54.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sánchez-Cabral O, Martínez-Mendoza D, Flores-Bello ÁP, et al. Diagnostic discrepancy between bronchoalveolar lavage and transbronchial biopsy from bronchoscopies of HIV patients with pneumonia: toward an integral diagnosis. HIV AIDS (Auckl) 2018;10:115–123. doi: 10.2147/HIV.S161899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Broaddus C, Dake MD, Stulbarg MS, et al. Bronchoalveolar lavage and transbronchial biopsy for the diagnosis of pulmonary infections in the acquired immunodeficiency syndrome. Ann Intern Med. 1985;102(6):747–752. doi: 10.7326/0003-4819-102-6-747. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


