Abstract
Background
Several new treatment options have become available for pancreatic ductal adenocarcinoma (PDAC), but the support for their use for resectable, borderline resectable and locally advanced PDAC is unclear.
Methods
A survey was distributed to the members of the European-African Hepato-Pancreato Biliary Association (E-AHPBA) and the pancreas group of the European Organization for Research and Treatment of Cancer (EORTC) regarding 1) definitions of local resectability, 2) indications for neoadjuvant therapy and 3) case-vignettes regarding the resectability and treatment of PDAC.
Results
In total, 114 participants from 37 countries were registered. About 35% of respondents, each, were of the opinion that borderline resectability is defined by any venous tumor contact and venous involvement < 180° or > 180°, respectively. The majority (75.4%) of participants believed that borderline resectable PDAC has a high risk for R1 resection and that neoadjuvant therapy might increase the R0-resection rate (79.8%) and improve oncological patient selection (84.2%). Chemotherapy was regarded useful to convert locally advanced to resectable PDAC by 55.7% of respondents. In the cases with resectable, borderline resectable, and locally advanced PDAC, 10 (8.8%), 78 (68.4%), 55 (48.2%) of participants would start with chemotherapy, respectively.
Conclusions
Although definitions for borderline resectability differ among European surgeons, there seems to be a rather strong support for preoperative chemotherapy in PDAC aiming at minimizing R1 resections while increasing resection rates.
Electronic supplementary material
The online version of this article (10.1186/s12885-019-5889-5) contains supplementary material, which is available to authorized users.
Keywords: Pancreatic cancer, PDAC, Neoadjuvant therapy, Defintions, Resectability, Survey
Background
The treatment of pancreatic ductal adenocarcinoma (PDAC) has seen large changes during recent years. While surgery was only an option for resectable and non-metastatic PDAC in the past [1], modern poly-chemotherapeutic regimens (e.g. FOLFIRINOX or gemcitabine/nab-paclitaxel) with increased efficacy have changed the attitude to the management of PDAC: multimodality regimens are increasingly used to improve survival after curative resection, and increase resectability in both metastatic and non-metastatic disease [2–4]. In addition, the surgical understanding of a curative resection is changing: recent literature suggests that the long term outcome is markedly improved if the circumferential tumor free margins is at least 1 mm (R0 wide) [5].
Several expert panels and associations have established criteria for resectability of PDAC [6]. These definitions contain a subgroup of (borderline resectable) tumors, which may be considered resectable or unresectable based on the available surgical expertise. Most centers liberally offer venous resections despite an impaired long-term survival in deep venous infiltration (portal/superior mesenteric vein, pv/smv) and are highly restrictive with arterial resections in PDAC [7–9] because the limited oncological outcome adds to the risk for surgical morbidity. Consequently, the assessment of resectability of PDAC and the management of this subgroup varies widely based on the (surgical) expertise and the oncological practice of a center, but this heterogeneity complicates the interpretation of the current literature [2].
In parallel, neoadjuvant therapy is gaining popularity, but again indications may vary. Current literature suggests that a significant proportion of locally unresectable PDAC (=locally advanced PDAC, LAPC) may undergo radical resection with favourable outcome after adequate treatment response [10]. Recently, a randomized phase II-trial has reported a longer recurrence-free survival and R0-resection rate after neoadjuvant chemoradiation therapy for borderline resectable PDAC [11]. Even in primarily resectable tumors, resection margins appear wider, the proportion of lymph node metastases smaller, and survival superior following neoadjuvant chemotherapy. Since the definition and preoperative prediction of an R0 resection is difficult, any treatment with the potential aim of curative resection is considered neoadjuvant resulting in significant heterogeneity in the literature [2].
The aim of this survey was to analyze the current understanding of experts in the field regarding treatment aims and attitudes in the (neoadjuvant) management of pancreatic cancer.
Methods
A web-based survey was distributed through the administrative offices of the European-African Hepato-Pancreato Biliary Association (E-AHPBA) and the pancreas group of the European Organization for Research and Treatment of Cancer (EORTC) to the respective members using Surveymonkey™. In addition to questions regarding the individual experience in the treatment of pancreatic cancer, the survey was designed to evaluate the attitude of European experts regarding the definition of local resectability and the indications for neoadjuvant therapy of PDAC of the pancreatic head.
Since participation to this European survey was anonymous and participation was voluntary and only offered to experts in the field, an approval of an ethical review board was not considered necessary.
Survey
The SurveyMonkey™ platform was used. The survey contained 21 questions, of which 9 questions served to assess the individual experience of each participant in the management of PDAC, the understanding of definitions of resectability, and effects of neoadjuvant therapy on resectable, borderline resectable and unresectable PDAC (see Additional file 1).
Case vignettes
Four case vignettes were presented at the end of the survey by computed tomography images in order to assess the attitude of the participants regarding resectability and choice of treatment (see Additional file 2). Case 1 was a resectable, case 2 borderline and case 3 unresectable (locally advanced) PDAC. Lastly, case 4 was locally resectable with a solitary resectable liver metastasis. For each case, the participant had to assess resectability and to propose the optimal treatment. Furthermore, we asked about a potential aim of a neoadjuvant treatment in the particular case (3 questions per case).
Statistics
All Analyses were performed using IBM SPSS 23 software. Categorial data between the groups were compared using the χ2-test. Differences were considered significant at a level of 0.05.
Results
Participants
In total, 114 participants were registered from 37 countries. Most of them originated from Europe, with most participants coming from Spain (n = 15), The Netherlands (n = 10), Great Britain (n = 9), Germany (n = 9) and Italy (n = 9). The vast majority of participants was hepato-pancreato-biliary (HPB) surgeons, and most of the participants reported an experience of more than 10 years in the management of patients with PDAC (Table 1). Amongst HPB and general surgeons, 52/84 (62%) and 9/15 (60%) reported an experience of more than 10 years in the management of PDAC, while only 8/84 (9.5%) and 3/15 (20%) had less than 5 years of experience, respectively. Similarly, 9/13 (69.2%) Gastrointestinal (GI) oncologists and all Radiation Oncologists had more than 10 years, while only 2 Medical Oncologists had less than 5 years of experience in managing PDAC patients.
Table 1.
Participants characteristics
| Participants | 114 |
|---|---|
| Experience in Treatment of PDAC | |
| < 5 years | 13 (11.4%) |
| 5–10 years | 29 (25.4%) |
| > 10 years | 72 (63.2%) |
| Scope of practice | |
| Surgery | 99 (86.8%) |
| General surgery | 84 (73.7%) |
| HPB surgery | 15 (13.2%) |
| Oncology | 15 (13.2%) |
| Medical oncology | 12 (10.5%) |
| Radiation oncology | 2 (1.8%) |
| Gastroenterology | 1 (0.9%) |
| Origin of participants | |
| Europe | 99 (86.8%) |
| Africa | 8 (7%) |
| Middle East | 5 (4.4%) |
| South America | 2 (1.8%) |
| Countries | 37 |
Resectability
The participants had a high agreement (75.4%) that borderline resectability is associated with a high risk of R1 resections. In addition, a significant proportion of surgeons felt that borderline resectability inherits a higher surgical morbidity and requires a particular technical expertise (Table 2).
Table 2.
Value of borderline resectability
| surgeons | oncologists | |
|---|---|---|
| What does borderline resectable mean to you? | ||
| The primary tumor can only be resected by surgeons with particular expertise | 26/99 (26.3%) | 2/15 (13.3%) |
| The resection of the primary tumor inherits a high risk for (incomplete) R1 resection | 73/99 (73.7%) | 13/15 (86.7%) |
| The tumor can be resected R0, but the oncological outcome after surgery is questionable | 16/99 (16.9%) | 1/15 (6.7%) |
| The morbidity of a resection of the primary tumor exceeds the normal morbidity by far | 9/99 (9.1%) | – |
| Is not important – either a tumor is resectable or not | 2/99 (2%) | – |
| What defines borderline resectability? | ||
| Tumor contact to the portal (PV)/superior mesenteric (SMV) veins on imaging – likelihood of a PV/SMV resection | 29/99 (29.3%) | 8/15 (53.3%) |
| Tumor contact to the hepatic or mesenteric arteries on imaging | 35/99 (35.4%) | 4/15 (26.7%) |
| Tumor contact to the PV/SMV up to 180° on imaging | 31/99 (31.3%) | 6/15 (40%) |
| Tumor contact to celiac, hepatic or mesenteric arteries up to 180° on imaging | 43/99 (43.4%) | 5/15 (33.3%) |
| Tumor contact to the PV/SMV of more than 180° on preoperative imaging | 40/99 (40.4%) | 5/15 (33.3%) |
| Tumor contact to the celiac/hepatic or superior mesenteric arteries of more than 180° on imaging | 19/99 (19.2%) | – |
| Tumor related portal vein thrombosis on imaging | 16/99 (16.2%) | – |
| Resectability cannot be assessed on imaging only | 12/99 (12.1%) | 1/15 (6.7%) |
| others | 9/99 9.1%) | – |
While 39.5% of participants believed that any tumor contact > 180° defines borderline resectability, 32.5% each considered a venous contact up to 180° or any venous involvement as criteria for borderline resectability. Moreover, 42% of participants considered an arterial involvement up to 180°, and 34.2% any tumor contact to the superior mesenteric (sma) or hepatic artery as borderline resectable disease (Table 2).
The majority of participants (n = 74; 64.9%) considered locally unresectable tumors without metastases as locally advanced disease. Six participants did not fully agree with the offered definitions (Table 3).
Table 3.
Definition of locally advanced disease
| Experience (years) | ||||
|---|---|---|---|---|
| < 5 (n = 13) |
5–10 (n = 29) |
> 10 (n = 72) |
total | |
| Locally advanced disease describes a locally unresectable disease without evidence of metastases | 11 (84.6%) | 19 (65.6%) | 44 (61.1%) | 74 (64.9%) |
| Locally advanced disease is equvivalent to borderline resectability | – | 5 (4.3%) | 7 (6.1%) | 12 (10.5%) |
| Locally advanced disease means a locally resectable disease with infiltration of mesenteric vascular structures | 1 (7.7%) | 3 (10.3%) | 11 (15.3%) | 15 (13.2%) |
| other | – | 1 (8.8%) | 5 (4.4%) | 6 (5.3%) |
Treatment aims in cancer treatment
Being asked, which treatment aims are associated with palliative and adjuvant therapies in pancreatic cancer, 23 (20.2%) participants considered any postoperative treatment as adjuvant, all of which were surgeons - except one participant. Only eight participants believed that palliative treatment has a potential for patient cure, and about a third of participants (n = 37; 32.5%) was of the opinion that palliative therapy is associated with a prolongation of survival. Interestingly, the 80% of oncologists (12/15) associated a palliative treatment with a prolongation of survival, while on a 25.3% of surgeons (25/99) had the same association. Moreover, (86.7%) of oncologists (13/15) and 63.6% of surgeons (63/99) were of the opinion that the aim of a palliative therapy is to relief symptoms. The vast majority of participants, however, was of the opinion that the aim of adjuvant therapy is to reduce the recurrence risk after complete tumor resection (92/114; 80.7%), while palliative treatments should relief symptoms (75/114; 65.8%).
Considering neoadjuvant therapy, 91 participants (79.8%) replied that neoadjuvant therapy has the aim to increase the R0-resection rate in borderline resectable cancer. Also, 45 (39.5%) respondents considered the treatment of micrometastases and 33 (28.9%) a decreased risk of metastases in resectable cancer as treatment aims of neoadjuvant therapy. Moreover, 31 (27.2%) participants believed that the aim of neoadjuvant therapy is to increase the size of the resection margin in resectable as well as borderline resectable cancer (Table 4). On the other hand, 64 (55.3%) respondents were of the opinion that the aim of neoadjuvant therapy can be the convertion of LAPC to resectable disease or even to stabilize oligo-metastatic disease with the aim of a secondary surgical treatment (n = 17; 14.9%).
Table 4.
Treatment aims/advantages of neoadjuvant therapy
| surgeons | oncologists | |
|---|---|---|
| Which treatment aims do you associate with neoadjuvant therapy for PDAC? | ||
| increasing the size of the resection margin (in resectable or borderline resectable cancer) | 27/99 (27.3%) | 4/15 (26.7%) |
| decreasing the risk of distant metastases after an apparently curative resection by a preoperative treatment | 27/99 (27.3%) | 6/15 (40%) |
| increasing the R0 resection rate (e.g. in borderline resectable cancer) | 77/99 (77.8%) | 14/15 (93.3%) |
| achieving resectability/disease stabilization in oligometastasized disease with the aim of surgical treatment | 16/99 (16.2%) | 2/15 (13.3%) |
| achieving secondary resectability in locally unresectable disease | 54/99 (54.5%) | 9/15 (60%) |
| Preoperative treatment of micrometastases | 35/99 (35.4%) | 10/15 (66.7%) |
| What are the theoretical advantages of neoadjuvant over adjuvant treatment? | ||
| better treatment tolerability of neoadjuvant treatment | 41/99 (41.4%) | 12/15 (80%) |
| higher dosage possible during neoadjuvant treatment | 26/99 (26.3%) | 7/15 (46.7%) |
| lower surgical complication rate after neoadjuvant treatment | 11/99 (11.1%) | 3/15 (20%) |
| better oncological patient selection by neoadjuvant treatment | 83/99 (83.8%) | 13/15 (86.7%) |
| better vascular supply of the tumor for neoadjuvant treatment | 24/99 (24.2%) | 6/15 (40%) |
In summary, 39.5% of the respondents associated neoadjuvant therapy with the treatment of micrometastases. Moreover, more participants (79.8%) considered neoadjuvant treatment to increase the R0-resection rate of borderline resectable PDAC than to convert unresectable to resectable PDAC (55.3%). We also found a tendency that oncologists more often believe that the treatment of micrometastases is the primary aim of neoadjuvant therapy. Since multiple answers were allowed to this question, we found a large overlap between the replies.
Neoadjuvant vs adjuvant therapy
The majority of participants (96/114, 84.2%) considered the oncological patient selection as the strongest advantage of neoadjuvant therapy over adjuvant therapy, meaning that surgery would be avoided in patients with progressive disease. A quarter of respondents believed that the blood supply to the tumor is better during neoadjuvant than adjuvant therapy. Only 12.3% (n = 14) of respondents were of the opinion that the surgical morbidity is lower after neoadjuvant therapy. Nearly half of the participants felt that neoadjuvant therapy was better tolerated than adjuvant therapy. However, these differences did not reach statistical significance.
Case vignettes
Resectability
The assessment of resectability of the resectable, borderline resectable and locally unresectable tumors matched with the intention of the survey and findings on the CT images in the majority of cases. Most of the participants (84.2%) considered the resectable tumor as resectable, while three were not sure and five participants were of the opinion that the tumor was borderline resectable.
Similarly, most participants judged the borderline resectable tumor as true borderline resectable (n = 79; 69.3%), 11 respondents considered the tumor as upfront resectable, and 10 as unresectable. Only two were not sure.
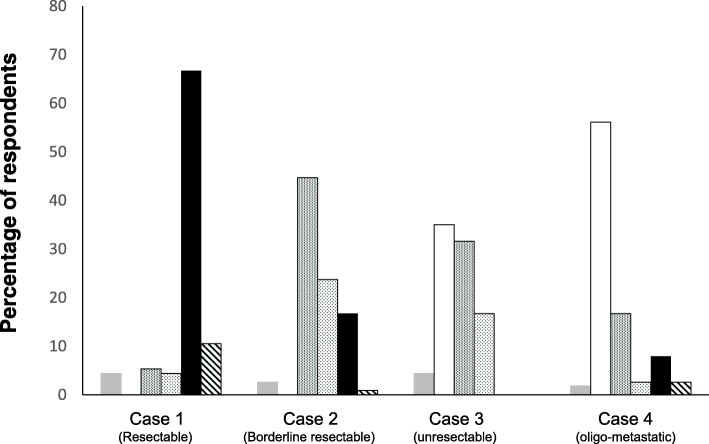
The unresectable tumor was considered unresectable by 72% of the participants, while 16% had the impression the tumor was borderline resectable. None of the participants thought this was a resectable tumor, and one was not sure (Fig. 1).
Fig. 1.
Assessment of the clinical cases regarding resectability of the disease ( not sure,
not sure,  unresectable,
unresectable,  borderline resectable,
borderline resectable,  resectable)
resectable)
Treatment including neoadjuvant therapy
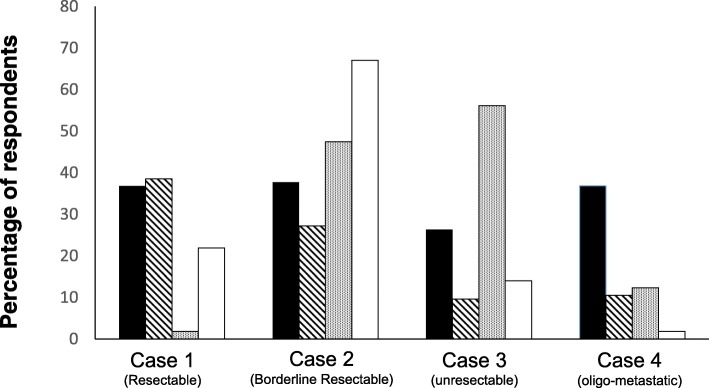
The majority of participants would treat primarily resectable PDAC (case 1) with upfront surgery followed by adjuvant chemotherapy (65%). However, 11% recommended surgery-only (without adjuvant therapy), and 9% would start with a neoadjuvant therapy (6 chemotherapy, 4 chemo-radiotherapy) (Fig. 2). In this case, 45 participants (39.5%) defined a potential aim of neoadjuvant therapy as a decreased risk of tumor recurrence (metastases) and 42 (36.8%) to improve long-term survival. In addition, 25 (21.9%) participants would apply neoadjuvant therapy to increase the probability of R0 resection, while only two would apply it to achieve (secondary) resectability (Fig. 3).
Fig. 2.
Proposition of the treatment for the different clinical scenarios ( others,
others,  neoadjuvant chemo-radiotherapy,
neoadjuvant chemo-radiotherapy,  neoadjuvant chemotherapy,
neoadjuvant chemotherapy,  palliative chemotherapy,
palliative chemotherapy,  Surgery + adj. Chemotherapy,
Surgery + adj. Chemotherapy,  surgery only)
surgery only)
Fig. 3.
Treatment aims for the four clinical cases suggested by the respondents ( improving the long-term survival,
improving the long-term survival,  decrease risk of metastasis,
decrease risk of metastasis,  achieve resectability,
achieve resectability,  increase the probability of R0 resection)
increase the probability of R0 resection)
In the borderline resectable tumor (case 2), about half of the respondents (48%) would start with a neoadjuvant treatment, of which 15 (13.2%) would treat the patient with chemotherapy, and 27 (23.7%) with chemoradiotherapy. Only 20 participants (17.5%) would primarily explore the patient with the aim of a primary resection, and 19 of them would also give adjuvant therapy after an apparently curative resection (Fig. 2). The rationale for a neoadjuvant therapy in such borderline resectable tumors was to achieve resectability by 54 (47%) and to increase the rate of R0-resections by 72 (63%) participants. Again, 27% participants considered a decreased risk of metastasis and 38% an improvement of long-term survival as potential aims of neoadjuvant therapy in borderline resectable cancer (Fig. 3).
In the locally unresectable tumor (case 3), about half of participants (n = 55, 48%) would start with a neoadjuvant therapy with consequent surgery in case of adequate tumor response, while 41 (36%) would apply palliative chemotherapy. As neoadjuvant treatment, chemotherapy was preferred (n = 36, 31.6%) over chemo-radiotherapy (n = 19, 16.7%), and five participants would use other treatments (Fig. 2). The majority of respondents (55%) was of the opinion that the aim of neoadjuvant therapy in unresectable cancer is to achieve resectability, and a fourth of participants considered an improvement in long-term survival as the primary treatment aim. Only 16 and 11 participants, respectively, considered an increase in the R0-resection rate and a decreased risk of metastases as treatment aims in this particular situation (Fig. 3).
Lastly, 54% of the participants considered a locally resectable pancreatic cancer with a solitary (resectable) liver metastasis (case 4) as unresectable (≈non-surgical) disease. In contrast, 26 respondants (22.8%) considered this clinical scenario as primarily resectable, and 12 as borderline resectable disease. Only two participants were not sure (Fig. 1). Consequently, 56% recommended palliative chemotherapy, while 17% would apply a neoadjuvant chemotherapy. Twelve participants (10.5%) proposed upfront surgery, of whom 9 would apply adjuvant chemotherapy thereafter. Three participants would start with neoadjuvant chemoradiotherapy and two with another treatment (Fig. 2). The majority (38%) proposed a neoadjuvant therapy in order to increase long-term survival (Fig. 3).
Discussion
This first pan-European survey performed by E-AHPBA and EORTC on neoadjuvant treatment in pancreatic cancer found that the definition of borderline resectability (and unresectability) varies among European experts. These different definitions often do not affect the clinical management of patients with PDAC. This study confirms a paradigm shift in the understanding and treatment of patients with locally advanced and oligo-metastatic cancer, but also a broad heterogeneity in the management of such patients. For resectable PDAC, primary resection followed by adjuvant chemotherapy was the preferred concept, and a neoadjuvant approach was only recommended by a few participants. About half of the respondents would initiate neoadjuvant therapy in borderline resectable and in LAPC. Finally, neoadjuvant therapy was only recommended by a minority of participants for metastatic PDAC.
Following most classifications, a resectable tumor has a maximal tumor contact to the pv/smv of less than 180° without any contact to the celiac or superior mesenteric artery. Borderline resectability includes tumors which have more than 180° contact to the pv/smv and up to 180° contact to the celiac/superior mesenteric arteries. Tumor infiltration of the celiac/superior mesenteric arteries beyond 180° defines unresectable disease [6]. Although differences in the assessment of resectability are generally attributed to the surgical expertise of centers in the literature, this survey demonstrates that such differences are more likely related to different perceptions of PDAC disease and different oncological attitudes considering the experience in this field of most participating surgeons: while some may primarily consider the technical success of surgery, others predominantly see the questionable oncological benefit of an R1 resection. Accordingly, resectability rates in series on neoadjuvant therapy depend on the inclusion policy in addition to the surgical expertise and the applied treatment.
The heterogeneity in treatment concepts for unresectable or oligo-metastatic cancer is even more pronounced and mainly reflects the controversial literature: a few recent publications suggest favorable long-term outcome of patients with unresectable or even oligo-metastatic disease after response to FOLFIRINOX [10, 12, 13]. Although these are retrospective studies, some centers have already adopted these concepts for selected patients. Thus, a large proportion of participants considered both scenarios as potentially curable in a multimodality concept.
In contrast to well established definitions of adjuvant and palliative treatment aims, a clear definition of treatment aims for a neoadjuvant treatment has not been established, yet. Accordingly, about half of the recipients considered the conversion from an unresectable to a resectable disease as aim of neoadjuvant therapy, while ¾ of them considered the increase in the R0-resection rate as aim of neoadjuvant therapy. Considering the aim of an adjuvant treatment (reduction of tumor recurrence) and the homology of the terms “adjuvant” and “neoadjuvant”, the primary aim of a neoadjuvant treatment should be to decrease the recurrence risk after a curative resection, which may be attributed to fewer lymph node metastases as well as the treatment of micrometastases and circulating tumor cells as indicated by most participants. Further beneficial effects may be larger resection margins, a lower R1 resection rate and smaller tumors. In locally unresectable tumors or whenever the risk of an R1 (wide) resection is high, the primary treatment aim of a preoperative therapy is to shrink the tumor and convert a (potentially) unresectable to a resectable disease. In this scenario, the treatment should be considered a down-sizing or conversion therapy [2]. If secondary resectability is not attempted (or unprobable), a palliative therapy is indicated. Similarly, neoadjuvant therapy for other tumors such as breast or upper GI cancer implies the preoperative therapy of technically resectable tumors with the aim of a reduction of tumor recurrence [14–16]. Also for colorectal liver metastases, many authors differentiate a “conversion” and a “neoadjuvant” chemotherapy [17–19].
Such differentiation in the terminology of treatment concepts would particularly increase the comparability of results in the borderline resectable group: a borderline resectable tumor (e.g. infiltration of the smv) according to current definitions could be treated by a neoadjuvant therapy with an expected high resectability rate – since it is most probably primarily resectable and would be resected upfront in many experienced centers. Since a deep infiltration may be associated with impaired outcome [9], a real neoadjuvant therapy could be given with the aim of an improvement of recurrence-free and overall survival in this scenario. The same idea is the basis of neoadjuvant therapy in resectable tumors [6]. A primarily unresectable disease, however, would undergo conversion therapy with an estimated lower secondary resection rate (depending on the tumor response rate). The same would be true for a borderline resectable tumor with tumor contact to the superior mesenteric artery – a scenario with a high risk of R1- or even un-resectability. Moreover, in the case of a resectable primary tumor with resectable liver metastases, the aim of a neoadjuvant therapy would be to decrease recurrence rate (e.g. new metastases) after the resection of both the primary tumor and metastases (e.g. case 4).
These two separate definitions of “neoadjuvant” treatment would not necessarily change the management of the patient, since the same treatment is often applied in both situations. However, they might help to better define inclusion criteria for clinical studies and the reading of the literature. If a high response rate is required for a locally unresectable tumor, the conversion therapy should be a maximally potent local treatment (including chemo-radiation), while a systemic treatment could be more suitable to prevent metastatic recurrence in some borderline resectable tumors (e.g. portal vein infiltration).
Conclusions
In conclusion, this first E-AHPBA/EORTC pan-European survey documents a shift in attitudes regarding the management of advanced PDAC among HPB surgeons and oncologists with fairly large support for neoadjuvant treatment. Moreover, this survey depicts different understandings of borderline resectability and neoadjuvant therapy which should trigger a discussion on an adaption of definitions in the setting of PDAC.
Additional files
Questions of the survery (number of potential answers indicated). (PDF 323 kb)
Case vignettes (provided including CT scans). (PDF 362 kb)
Acknowledgements
None.
Abbreviations
- E-AHPBA
European-African Hepato-Pancreato Biliary Association
- EORTC
European Organization for Research and Treatment of Cancer
- GI
Gastrointestinal
- HPB
Hepato-pancreato-biliary
- LAPC
Locally advanced pancreatic cancer
- PDAC
Pancreatic ductal adenocarcinoma
- pv
Portal vein
- sma
Superior mesenteric artery
- smv
Superior mesenteric vein
Authors’ contributions
This study was designed by ML2, SH, MB, JLvL, MD. The questionnaire was reated by PG, SH and JM. The manuscript was prepared by ML1, MB and SH and intensively reviewed and adjusted by MM, JLvL, MD, MP and HL. In addition, all authors have read and approved the manuscript.
Funding
This survey was not funded
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Does not apply.
Consent for publication
Does not apply
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Stefan Heinrich, Phone: +49 6131 17 2738, Email: stefan.heinrich@unimedizin-mainz.de.
Marc Besselink, Email: m.g.besselink@amc.uva.nl.
Markus Moehler, Email: markus.moehler@unimedizin-mainz.de.
Jean-Luc van Laethem, Email: JL.vanlaethem@erasme.ulb.ac.de.
Michel Ducreux, Email: michel.durcreux@gustaveroussy.fr.
Peter Grimminger, Email: peter.grimminger@unimedizin-mainz.de.
Jens Mittler, Email: jens.mittler@unimedizin-mainz.de.
Hauke Lang, Email: hauke.lang@unimedizin-mainz.de.
Manfred P. Lutz, Email: m.lutz@caritasklinikum.de
Mickael Lesurtel, Email: mickael.lesurtel@chu-lyon.fr.
References
- 1.Li D, Xie K, Wolff R, Abbruzzese JL. Pancreatic cancer. Lancet. 2004;363(9414):1049–1057. doi: 10.1016/S0140-6736(04)15841-8. [DOI] [PubMed] [Google Scholar]
- 2.Puleo F, Marechal R, Demetter P, Bali MA, Calomme A, Closset J, et al. New challenges in perioperative management of pancreatic cancer. World J Gastroenterol. 2015;21(8):2281–2293. doi: 10.3748/wjg.v21.i8.2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310(14):1473–1481. doi: 10.1001/jama.2013.279201. [DOI] [PubMed] [Google Scholar]
- 4.Klaiber Ulla, Leonhardt Carl-Stephan, Strobel Oliver, Tjaden Christine, Hackert Thilo, Neoptolemos John P. Neoadjuvant and adjuvant chemotherapy in pancreatic cancer. Langenbeck's Archives of Surgery. 2018;403(8):917–932. doi: 10.1007/s00423-018-1724-8. [DOI] [PubMed] [Google Scholar]
- 5.Hank T, Hinz U, Tarantino I, Kaiser J, Niesen W, Bergmann F, et al. Validation of at least 1 mm as cut-off for resection margins for pancreatic adenocarcinoma of the body and tail. Br J Surg. 2018;105(9):1171–1181. doi: 10.1002/bjs.10842. [DOI] [PubMed] [Google Scholar]
- 6.Heinrich S, Lang H. Neoadjuvant therapy of pancreatic Cancer: definitions and benefits. Int J Mol Sci. 2017;18(8). 10.3390/ijms18081622. [DOI] [PMC free article] [PubMed]
- 7.Fukuda S, Oussoultzoglou E, Bachellier P, Rosso E, Nakano H, Audet M, et al. Significance of the depth of portal vein wall invasion after curative resection for pancreatic adenocarcinoma. Arch Surg. 2007;142(2):172–179. doi: 10.1001/archsurg.142.2.172. [DOI] [PubMed] [Google Scholar]
- 8.Mollberg N, Rahbari NN, Koch M, Hartwig W, Hoeger Y, Buchler MW, et al. Arterial resection during pancreatectomy for pancreatic cancer: a systematic review and meta-analysis. Ann Surg. 2011;254(6):882–893. doi: 10.1097/SLA.0b013e31823ac299. [DOI] [PubMed] [Google Scholar]
- 9.Giovinazzo F, Turri G, Katz MH, Heaton N, Ahmed I. Meta-analysis of benefits of portal-superior mesenteric vein resection in pancreatic resection for ductal adenocarcinoma. Br J Surg. 2016;103(3):179–191. doi: 10.1002/bjs.9969. [DOI] [PubMed] [Google Scholar]
- 10.Crippa S, Bittoni A, Sebastiani E, Partelli S, Zanon S, Lanese A, et al. Is there a role for surgical resection in patients with pancreatic cancer with liver metastases responding to chemotherapy? Eur J Surg Oncol. 2016;42(10):1533–1539. doi: 10.1016/j.ejso.2016.06.398. [DOI] [PubMed] [Google Scholar]
- 11.Jang JY, Han Y, Lee H, Kim SW, Kwon W, Lee KH, et al. Oncological benefits of neoadjuvant Chemoradiation with gemcitabine versus upfront surgery in patients with borderline Resectable pancreatic Cancer: a prospective, randomized, open-label, multicenter phase 2/3 trial. Ann Surg. 2018;268(2):215–222. doi: 10.1097/SLA.0000000000002705. [DOI] [PubMed] [Google Scholar]
- 12.Gemenetzis G, Groot VP, Blair AB, Laheru DA, Zheng L, Narang AK, et al. Survival in locally advanced pancreatic Cancer after neoadjuvant therapy and surgical resection. Ann Surg. 2018. 10.1097/SLA.0000000000002753. [DOI] [PMC free article] [PubMed]
- 13.Suker M, Beumer BR, Sadot E, Marthey L, Faris JE, Mellon EA, et al. FOLFIRINOX for locally advanced pancreatic cancer: a systematic review and patient-level meta-analysis. Lancet Oncol. 2016;17(6):801–810. doi: 10.1016/S1470-2045(16)00172-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shapiro J, van Lanschot JJB, Hulshof M, van Hagen P, van Berge Henegouwen MI, Wijnhoven BPL, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16(9):1090–1098. doi: 10.1016/S1470-2045(15)00040-6. [DOI] [PubMed] [Google Scholar]
- 15.Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20. doi: 10.1056/NEJMoa055531. [DOI] [PubMed] [Google Scholar]
- 16.Bear HD, Tang G, Rastogi P, Geyer CE, Jr, Robidoux A, Atkins JN, et al. Bevacizumab added to neoadjuvant chemotherapy for breast cancer. N Engl J Med. 2012;366(4):310–320. doi: 10.1056/NEJMoa1111097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nozawa H, Ishihara S, Kawai K, Hata K, Kiyomatsu T, Tanaka T, et al. Conversion to resection in patients receiving systemic chemotherapy for Unresectable and/or metastatic colorectal Cancer-predictive factors and prognosis. Clin Colorectal Cancer. 2018;17(1):e91–ee7. doi: 10.1016/j.clcc.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Kataoka K, Kanazawa A, Iwamoto S, Kato T, Nakajima A, Arimoto A. Does "conversion chemotherapy" really improve survival in metastatic colorectal cancer patients with liver-limited disease? World J Surg. 2014;38(4):936–946. doi: 10.1007/s00268-013-2305-1. [DOI] [PubMed] [Google Scholar]
- 19.Poston G, Adam R, Xu J, Byrne B, Esser R, Malik H, et al. The role of cetuximab in converting initially unresectable colorectal cancer liver metastases for resection. Eur J Surg Oncol. 2017;43(11):2001–11. doi: 10.1016/j.ejso.2017.07.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Questions of the survery (number of potential answers indicated). (PDF 323 kb)
Case vignettes (provided including CT scans). (PDF 362 kb)
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.