Abstract
Introduction
When women with a previous cesarean section and an unfavorable cervix have an indication for delivery, the choice is to induce labor or to perform a cesarean section. This study aims to assess the effectiveness and safety of a balloon catheter as a method of induction of labor in women with one previous cesarean section and an unfavorable cervix compared with an elective repeat cesarean section.
Material and methods
We performed a prospective cohort study in 51 hospitals in the Netherlands on term women with one previous cesarean section, a live singleton fetus in cephalic position, an unfavorable cervix and an indication for delivery. We recorded obstetric, maternal and neonatal characteristics. We compared the outcome of women who were induced with a balloon catheter with the outcome of women who delivered by elective repeat cesarean section. Main outcomes were maternal and neonatal morbidity. Mode of delivery was a secondary outcome for women who were induced. Adjusted odds ratios (aOR) were calculated using logistic regression, adjusted for potential confounders.
Results
Analysis was performed on 993 women who were induced and 321 women who had a repeat cesarean section (August 2011 until September 2012). Among the women who were induced, 560 (56.4%) delivered vaginally and 11 (1.1%) sustained a uterine rupture. Composite adverse maternal outcome (uterine rupture, severe postpartum hemorrhage or postpartum infection) occurred in 73 (7.4%) in the balloon and 14 (4.5%) women in the repeat cesarean section group (aOR 1.58, 95% confidence interval [CI] 0.85‐2.96). Composite adverse neonatal outcome (Apgar score <7 at 5 minutes or umbilical pH <7.10) occurred in 57 (5.7%) and 10 (3.2%) neonates, respectively (aOR 1.40, 95% CI 0.87‐3.48). Women who were induced had a shorter postpartum admission time (2.0 vs 3.0 days (P < 0.0001)).
Conclusions
In women with a previous cesarean section and a need for delivery, induction of labor with a balloon catheter does not result in a significant increase in adverse maternal and neonatal outcomes as compared with planned cesarean section.
Keywords: balloon catheter, cervical ripening, induction of labor, repeat cesarean, vaginal birth after cesarean
Abbreviations
- aOR
adjusted odds ratios
- BMI
body mass index
- CI
confidence interval
- RR
relative risk
- VBAC
vaginal birth after cesarean
Key message.
In women with a previous cesarean section and a need for delivery, induction of labor with a balloon catheter does not result in a significant increase in adverse maternal and neonatal outcomes as compared with planned cesarean section.
1. INTRODUCTION
Among women attempting vaginal birth after a previous cesarean section, labor is induced in 18%‐27%.1, 2, 3 Previous studies have shown that 60%‐80% of women with one previous cesarean section will deliver vaginally if a trial of labor is allowed, even when induced.3, 4, 5 When delivery is indicated, a decision must be made whether to induce labor or perform primary cesarean section, and the risks and benefits of this choice must be weighed carefully.
Various publications suggest that induction of labor in women after previous cesarean section increases the risk of uterine rupture, especially after induction with prostaglandins.3, 6, 7 In women with a previous cesarean section, balloon catheters have also been proven effective and safe, with vaginal delivery rates of 55.7%‐71% and uterine rupture rates of 0.3%‐1.6%.3, 8, 9, 10 Guidelines now discourage the use of prostaglandins but suggest use of the balloon catheter for cervical ripening.11, 12, 13
With rising cesarean rates worldwide, repeat cesarean section with corresponding maternal and neonatal morbidity are increasing as well.14 The national cesarean section rate in the Netherlands was 16% (28 713/176 155) in 2012.15 In a national study including 4569 women with a previous cesarean section, 72% (3274/4569) attempted a trial of labor.1 Although prostaglandins are still used for cervical ripening, the use of mechanical methods in this population is increasing.16
When an indication for delivery arises, the decision between induction of labor or a repeat cesarean section may be a difficult one, and one that many clinicians face daily. However, so far, a comparison between the two in terms of effectiveness and safety of the method has not been reported.
The objective of this study is to assess the effectiveness and safety of the balloon catheter in women with one previous cesarean section and an unfavorable cervix compared with an elective repeat cesarean section.
2. MATERIAL AND METHODS
We performed a prospective cohort study in 51 hospitals in the Netherlands. We included term, pregnant women (between 37 and 42 weeks’ gestational age) with one previous cesarean section, a live singleton pregnancy in cephalic presentation, an unfavorable cervix and an indication for delivery. The cervix was considered unfavorable if amniotomy was not possible and induction by a cervical priming method such as a balloon catheter was necessary. Women with contraindications for vaginal delivery, such as placenta previa, previous classical uterine incision or obstructing cervical fibroids were not included.
We compared women undergoing an induction of labor by a balloon catheter (with subsequent amniotomy and/or oxytocin augmentation if necessary) with women who had an elective repeat cesarean section performed for one or more reasons. Because of rapid recruitment of women in the elective repeat cesarean section group, with the previous cesarean section as a single reason, recruitment in this group was stopped a few months into the study period. We considered this a homogeneous group and further recruitment was not possible due to lack of resources. Recruitment in the induction of labor group continued until the target number of 1000 women was reached. Some women were excluded because they were preterm, resulting in a cohort of 993 women induced by balloon catheter.
In women undergoing induction of labor, indications for induction of labor were hypertensive disorders, threatening post‐term pregnancy (before 42 weeks), insulin‐dependent diabetes, intrauterine growth restriction or oligohydramnion, suspected fetal compromise of a non‐acute nature (decreased fetal movement and/or suboptimal fetal heart rate tracing) or other maternal or neonatal reasons (ie, elective, intrahepatic cholestasis of pregnancy, pelvic instability, social or psychological reasons, gestational diabetes, obstetric history or suspected macrosomia).
Insertion of the balloon catheter was performed according to local protocol in the participating hospitals. Generally, the catheter was placed transcervically either manually or using a speculum, followed by fetal heart rate tracing. A single balloon (Foley) catheter (16F or 18F, n = 847), a double balloon (Cook) catheter (n = 125) or a prostatectomy catheter (20F) (n = 21) was used. After passing the internal os, the single balloon and prostatectomy catheters were most commonly filled with 30‐50 mL of sterile saline and the double balloon catheters with 60‐80 mL. Evaluation of cervical ripeness was done as per hospital protocol, generally after 12‐24 hours. When the balloon catheter was expelled or removed, and the cervix was judged to be “ripe”, amniotomy was performed and continuous fetal monitoring was started. If uterine activity was insufficient (<3 contractions per 10 minutes), intravenous oxytocin was infused until three to four contractions per 10 minutes or adequate progression occurred.
Primary maternal outcome was a composite maternal morbidity that consisted of uterine rupture (defined as clinical symptoms such as abdominal pain, abnormal fetal heart rate pattern, acute loss of contractions or vaginal blood loss that led to an emergency cesarean section, at which the presumed diagnosis of uterine rupture (with complete rupture of the uterine wall and serosa) was confirmed; or peripartum hysterectomy or laparotomy for uterine rupture after vaginal birth), severe postpartum hemorrhage (≥2 L blood loss, blood transfusion, hysterectomy or re‐laparotomy for bleeding) or postpartum infection (defined as treated urinary tract infection, endometritis, pneumonia, wound infection or any other unspecified suspected maternal infection requiring treatment).17 The components of composite adverse maternal outcome were also assessed separately.
Secondary outcomes included suspected maternal intrapartum infection (defined as fever of ≥38°C during labor or fetal tachycardia (a persistent fetal heart rate of more than 150 bpm) and start of broad‐spectrum intravenous antibiotics for suspected infection during labor), the amount of postpartum hemorrhage (mL) and postpartum blood transfusion. We also noted the length of maternal postpartum admission, as it is common practice in the Netherlands to be discharged within 4 hours after labor in case of an uneventful delivery. We also collected data on silent uterine ruptures noted during cesarean section (defined as a complete separation of the uterine wall and serosa without clinical symptoms), uterine scar dehiscence (separation of a preexisting scar but with an intact uterine serosa, as seen during cesarean section, with or without clinical symptoms) and uterine hyperstimulation (more than six contractions in 10 minutes over a minimal period of two periods of 10 minutes, or a contraction lasting more than 3 minutes with fetal heart rate changes). For the induction group, secondary outcomes were the use of epidural analgesia, oxytocin augmentation, mode of delivery, indications for operative delivery and time from start of induction to delivery.
Primary neonatal outcome was an adverse neonatal composite outcome of an Apgar score <7 at 5 minutes or an umbilical arterial pH <7.10. Secondary neonatal outcomes were birthweight, neonatal death, indications for and length of neonatal admissions to the ward, medium and intensive care.
Trained research nurses identified eligible women. From their charts we collected demographics, obstetric history, reasons for induction of labor or cesarean section, intrapartum and postpartum information. Neonatal data until discharge from the hospital were extracted from the corresponding neonatal files. All data were collected in a web‐based case‐record form using consistency checks (Oracle Clinical version 4.5.3, www.oracle.com). We reviewed all operative reports of all cases with uterine rupture or scar dehiscense to ensure the accuracy of the diagnosis and reclassified if necessary.
2.1. Statistical analyses
Women were analyzed according to the treatment that was planned, meaning that women who started induction but had to have a (emergency) cesarean, were analyzed in the induction group. For maternal outcome, adjusted odds ratios (aOR) with 95% confidence intervals (CI) were calculated after correction for the potential confounding variables maternal age >35, body mass index (BMI) >30, prior vaginal delivery, (un)planned previous cesarean section, reasons for labor induction and prolonged rupture of membranes. For neonatal outcome, aORs with 95% CI were calculated after correction for the potential confounders gestational age, maternal age >35, reasons for labor induction, known fetal (congenital) disease and prolonged rupture of membranes. P values of less than 0.05 and confidence intervals of relative risks and aORs that do not include 1 were considered to be statistically significant. All analyses were done with SPSS version 23 (Statistical Package for Social Sciences, Chicago, IL, USA).
2.2. Ethical approval
The protocol was approved by the Medical Ethical Committee of Leiden University Medical Center and the board of directors of each of the participating hospitals approved local execution of the study (reference number p11.023; 11 March 2011).
3. RESULTS
From 1 August 2011 until 30 September 2012, we enrolled 1305 women in the study, of whom 993 were induced with a balloon catheter and 312 women underwent an elective repeat cesarean section (see Figure 1, flow diagram).
Figure 1.
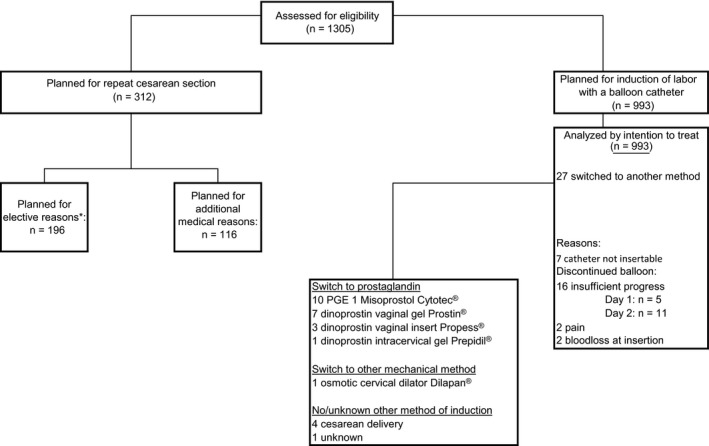
Flow chart. A total of 1305 women were included in the study, of whom 993 were planned for induction of labor by balloon catheter and 312 for repeat cesarean section. *The previous cesarean section was the sole reason to opt for a repeat cesarean section
Table 1 shows the baseline characteristics of the two groups. Women in the elective repeat cesarean section group were slightly older: 34.0 vs 33.2 mean years of age (P = 0.006). Women in the balloon catheter group had a higher gestational age: 40.0 vs 39.0 weeks (P < 0.0001). Hypertension and threatening post‐term pregnancy as an indication for delivery were more common in the induction group: 21.3% vs 10.9%, (relative risk [RR] 1.90, 95% CI 1.37‐2.64, P < 0.0001) and 35.9% vs 9.6%, (RR 3.95, 95% CI 2.76‐5.64, P < 0.0001), respectively. Of the women planned for induction of labor by balloon catheter, 27 switched to another method for various reasons (Figure 1).
Table 1.
Baseline characteristics for method of induction/delivery
| Balloon catheter (n = 993) (%) | Repeat CS (n = 312) (%) | RR (95% CI) | P value | |
|---|---|---|---|---|
| Maternal age mean, SD | 33.2 (4.5) | 34.0 (4.5) | NA | 0.006 |
| <25 y | 48 (4.8) | 7 (2.2) | 1.92 (0.95‐3.86) | 0.05 |
| 25‐35 y | 589 (59.3) | 174 (55.8) | 1.12 (0.92‐1.36) | 0.27 |
| >35 y | 356 (35.9) | 131 (42.0) | 0.82 (0.68‐1.00) | 0.05 |
| SES | ||||
| Low | 337 (33.9) | 95 (30.4) | 1.13 (0.92‐1.40) | 0.25 |
| Middle | 372 (37.5) | 131 (42.0) | 0.87 (0.71‐1.05) | 0.15 |
| High | 253 (25.5) | 78 (25.0) | 1.02 (0.82‐1.28) | 0.87 |
| Unknown | 31 (3.1) | 8 (2.6) | 1.17 (0.63‐2.19) | 0.61 |
| Caucasian | 715 (72.0) | 235 (75.3) | 0.96 (0.90‐1.03) | 0.25 |
| BMI, kg/m2; median (IQR) | 25.9 (23.0 ‐ 30.0)a | 26.7 (23.0 ‐31.2)b | NA | 0.22 |
| BMI >30 | 216 (21.8) | 78 (25.0) | 0.87 (0.70‐1.09) | 0.23 |
| Parity | ||||
| 1 | 801 (80.7) | 258 (82.7) | ||
| ≥2 | 192 (19.3) | 54 (17.3) | 1.11 (0.86‐1.44) | 0.42 |
| Previous vaginal births before CS | ||||
| 0 | 880 (88.6) | 270 (86.5) | 1.05 (0.95‐1.16) | 0.32 |
| 1 | 88 (8.9) | 35 (11.2) | 0.82 (0.61‐1.11) | 0.21 |
| ≥2 | 25 (2.5) | 7 (2.2) | 1.10 (0.57‐2.12) | 0.79 |
| Previous vaginal births after CS | ||||
| 0 | 882 (88.8) | 287 (92.0) | 0.92 (0.85‐1.01) | 0.11 |
| 1 | 90 (9.1) | 21 (6.7) | 1.29 (0.86‐1.92) | 0.20 |
| ≥2 | 21 (2.1) | 4 (1.3) | 1.50 (0.61‐3.71) | 0.35 |
| Previous unplanned CS | 608 (61.7) | 215 (69.6) | 0.76 (0.62‐0.95) | 0.01 |
| Gestational age wk; median, IQR | 40.0 (38.6‐41.1) | 39.0 (38.4‐39.7) | NA | <0.0001d |
| Indications for induction of labor | ||||
| Hypertensive disorders | 212 (21.3) | 34 (10.9) | 1.90 (1.37‐2.64) | <0.0001 |
| Threatening post‐term pregnancy | 356 (35.9) | 30 (9.6) | 3.95 (2.76‐5.64) | <0.0001 |
| Insulin‐dependent diabetes | 70 (7.0) | 32 (10.3) | 0.74 (0.55‐1.01) | 0.07 |
| Intrauterine growth restriction or oligohydramnion | 81 (8.2) | 17 (5.4) | 1.41 (0.90‐2.20) | 0.11 |
| Fetal distress | 96 (9.7) | 27 (8.7) | 1.10 (0.78‐1.56) | 0.59 |
| Otherc | 367 (37.0) | 224 (71.8) | 0.51 (0.46‐0.57) | <0.0001 |
BC, balloon catheter; CS, cesarean section; IQR, interquartile range; NA, not applicable; RCS, repeat cesarean section; SES, socioeconomic status; RR, relative risk.
13% missing.
17% missing.
Other reasons for induction: other maternal/neonatal disease not mentioned in any of the above options.
Mann‐Whitney U test.
Composite adverse maternal outcome (uterine rupture, severe postpartum hemorrhage or suspected postpartum infection) occurred in 7.4% and 4.5% in the balloon catheter group and the repeat cesarean section group, respectively (aOR 1.58, 95% CI 0.85‐2.96, P = 0.15).
Uterine rupture occurred 11 times in the balloon catheter group and once in the elective repeat cesarean section group. The latter was a silent rupture without clinical signs. Two of the women with a uterine rupture had severe postpartum hemorrhage and one woman also had bladder injury during cesarean section. Uterine dehiscence occurred seven times in the balloon catheter group and three times in the elective repeat cesarean section group.
Table 2 shows maternal and neonatal outcomes. Although maternal temperature of ≥38°C during labor occurred more often in the balloon catheter group (8.4% vs 1.6%; aOR 7.00, 95% CI 2.73‐17.95, P < 0.0001), maternal suspected intrapartum infection and postpartum infection was comparable between the two groups. The higher occurrence rate of pyrexia is most likely due to the use of epidural analgesia: 15.9% (73/459) women with epidural analgesia developed pyrexia, accounting for 88% (73/83) of all women with pyrexia.
Table 2.
Maternal and neonatal outcome
| Balloon catheter (n = 993) (%) | Repeat CS (n = 312) (%) | adjusted OR (95% CI) | adjusted P value | |
|---|---|---|---|---|
| Maternal outcome | ||||
| Composite maternal morbiditya | 73 (7.4) | 14 (4.5) | 1.58 (0.85‐2.96) | 0.15 |
| Suspected intrapartum infectionb | 25 (2.5) | 4 (1.3) | 2.04 (0.66‐6.34) | 0.22 |
| Postpartum hemorrhage c | 30 (3.0) | 5 (1.6) | 1.34 (0.49‐3.68) | 0.57 |
| Postpartum infectiond | 37 (3.7) | 8 (2.6) | 1.66 (0.73‐3.81) | 0.23 |
| Uterine rupture | 11 (1.1) | 1 (0.3)e | 3.01 (0.36‐25.03) | 0.31 |
| Maternal length of admission days; median (IQR) | 2.0 (1.0‐3.0) | 3.0 (2.25‐3.0) | Beta: ‐1.09 | <0.0001 |
| Neonatal outcome | ||||
| Composite neonatal morbidity | 57 (5.7) | 10 (3.2) | 1.40 (0.67‐2.93) | 0.38 |
| Apgar score <7 | ||||
| 1 min | 68 (6.9) | 11 (3.5) | 1.74 (0.87‐3.48) | 0.12 |
| 5 min | 21 (2.1) | 4 (1.3) | 1.31 (0.41‐4.17) | 0.65 |
| pH <7·10 | 40 (5.9)f | 8 (3.7)g | 1.08 (0.46‐2.55) | 0.86 |
| Neonatal birthweight, g; mean (SD) | 3515 (527) | 3627 (558) | NA | <0.0001 |
| Neonatal admission | ||||
| Ward | 252 (25.4) | 72 (23.1) | 1.24 (0.89‐1.73) | 0.20 |
| Medium care | 85 (8.6) | 26 (8.3) | 1.13 (0.69‐1.85) | 1.13 |
| Intensive care | 26 (2.6) | 2 (0.6) | 6.20 (1.31‐29.38) | 0.02 |
| Reason for admission | ||||
| Suspected infection | 42 (4.2) | 9 (2.9) | 1.35 (0.62‐2.94) | 0.45 |
| Asphyxia | 10 (1.0) | 2 (0.6) | 1.32 (0.27‐6.54) | 0.73 |
| Dysmaturity | 40 (4.0) | 11 (3.5) | 1.08 (0.50‐2.33) | 0.84 |
| Hypoglycemia | 16 (1.6) | 10 (3.2) | 0.46 (0.19‐1.10) | 0.08 |
| Glucose protocol | 160 (16.1) | 60 (19.2) | 0.99 (0.67‐1.46) | 0.95 |
| IRDS | 1 (0.1) | 2 (0.6) | 0.05 (0.00‐0.62) | 0.02 |
| Meconium aspiration | 4 (0.4) | 0 | NA | 0.99 |
| Pneumothorax | 2 (0.2) | 0 | NA | 0.99 |
| Apnea | 6 (0.6) | 0 | NA | 0.99 |
| Other or unknownh | 174 (17.5) | 33 (10.6) | 2.18 (1.39‐3.42) | 0.001 |
| Neonatal length of admission (d) | 2.0 (1.0‐4.0) | 3.0 (3.0‐5.0) | NA | <0.0001 |
CS, cesarean section; NA, not applicable. RR, relative risk.
Suspected postpartum infection or severe postpartum hemorrhage or uterine rupture.
Body temperature during labor ≥38˚C or fetal tachychardia (a persistent fetal heart rate of >150 bpm) and start of broad‐spectrum antibiotics due to suspected infection.
>2000 mL or blood transfusion.
Defined as treated urinary tract infection, endometritis, pneumonia, wound infection or other unspecified suspected maternal infection.
Silent rupture.
31% missing values.
34% missing values.
Other reasons including: lung disease, pneumothorax, apnea, intraventricular hemorrhage, periventricular leucomalacia.
Serious adverse events in the balloon catheter group were umbilical cord prolapse (n = 1), partial placental abruption (n = 1, several hours after removing the balloon catheter), bladder injury (n = 4, during cesarean section), uterine inversion after vaginal birth (n = 1) and relaparotomy (n = 1). In two women, cesarean section was performed due to abnormal blood loss after catheter placement. One woman had an unknown amount of blood loss directly after trans‐cervical balloon catheter insertion and, after removal, immediate cesarean section was performed. Another woman suddenly had approximately 1000 mL of blood loss 10 hours after insertion, after which emergency cesarean section was performed. In both cases neonatal outcome was good. The woman undergoing relaparotomy suffered from severe postpartum hemorrhage after an emergency cesarean section. Total blood loss was 7.5 L, for which she received 11 units of blood and was admitted to the intensive care unit. There were no other women with massive transfusion (defined as 10 units of red cells in 24 hours), no women with hysterectomy or organ failure and no maternal deaths. Three women were admitted to the intensive care unit, all due to severe hemorrhage (7.5, 2.8 and 2.6 L, respectively). Hyperstimulation occurred in 14 women who were induced by a balloon catheter, leading to a uterine rupture once and postpartum hemorrhage twice. Neonatal outcomes were not affected. In the repeat cesarean section group, there was one maternal adverse event: a uterine inversion during cesarean section. There were no women with massive blood transfusion, hysterectomy, organ failure and no maternal deaths. One woman was admitted to a maternal intensive care unit due to spinal muscular atrophy, for which she was observed post‐cesarean.
In the balloon catheter group, 21.6% of women were not admitted (adjusted P < 0.0001) during the postpartum period (ie, discharged within 4 hours after delivery) and those admitted had a shorter median maternal postpartum admission in the hospital (2.0 days vs 3.0 days, adjusted P < 0.0001) (Table 2). However, median total admission time was 3.0 days for both groups.
The cesarean section rate was 43.6% (433 women) in the balloon catheter group. Further delivery characteristics for women induced by balloon catheter can be seen in Table 3.
Table 3.
Delivery characteristics for women induced by balloon catheter
| n = 993 (%) | |
|---|---|
| Intrapartum information | |
| Epidural analgesia | 457 (46.2) |
| Oxytocin augmentation (Y/N) | 770 (77.5) |
| Hyperstimulation | 14 (1.4) |
| Time from start of induction to birth (median, IQR) | 30.8 (21.9‐39.0) |
| Mode of delivery | |
| Spontaneous | 469 (47.2) |
| Vaginal instrumental | 91 (9.2) |
| Cesarean delivery | 433 (43.6) |
| Indication for cesarean delivery | |
| Failure to progress in first stage | 221 (50.8) |
| Failure to progress in second stage | 24 (5.5) |
| Fetal distress | 127(29.2) |
| Maternal reason | 13 (3.0) |
| Other or Unknown | 50 (11.5) |
| Indication for vaginal instrumental delivery | |
| Failure to progress in second stage | 38 (38.8) |
| Fetal distress | 44 (44.9) |
| Failure to progress in second stage AND fetal distress | 13 (13.3) |
| Maternal complication | 3 (3.1) |
| Operative deliveries for fetal distressa | 182 (18.3) |
Two women had a cesarean delivery for fetal distress after failed ventouse extraction.
Composite adverse neonatal outcome of an Apgar score <7 at 5 minutes or an umbilical arterial pH <7.10 was not significantly different between the groups, it occurred in 5.7% and 3.2% (aOR 1.40, 95% CI 0.67‐2.93, P = 0.38) after induction by balloon catheter and repeat cesarean section, respectively. Specific neonatal outcomes can be seen in Table 2. There was one case of neonatal death in the balloon catheter group due to a prenatally detected congenital heart disease. Of the 11 women with a uterine scar rupture, there were two neonates with low Apgar scores (1/2/5 and 0/3/4 after 1, 5 and 10 minutes) and an umbilical artery pH below 7.0; they were admitted to the neonatal intensive care unit. One neonate was cooled for 72 hours with good cerebral function monitoring at discharge after 8 days; the (neurological) outcome of other neonate is unknown, discharge was after 20 days.
4. DISCUSSION
The results of this prospective cohort study show that in women with one previous cesarean section and an unfavorable cervix, induction of labor with a balloon catheter is a safe method to induce delivery compared with women who deliver by means of an elective repeat cesarean section. Between the two groups, there was no significant difference in maternal morbidity such as uterine scar rupture or dehiscence, postpartum hemorrhage or infection. Postpartum admission time was shorter in the induction of labor group. Neonatal morbidity with regard to umbilical cord pH and Apgar scores was similar in both groups.
In the induction of labor group, the cesarean section rate was 43.6%, which is comparable to other studies such as the systematic review and meta‐analysis by Kehl et al (n = 144, cesarean section rate 43.6%)18 but higher than a recent study by Kruit et al (n = 361, cesarean section rate 38%)9 and the study by Jozwiak et al (n = 208, cesarean section rate 28.8%).10 All of these studies specifically looked at balloon catheter for induction of labor at term after previous cesarean section.
We found a uterine rupture rate after induction of labor of 1.1%, which is comparable to the incidence quoted in the literature of 0.3%‐1.2%.9, 18 Notable in our study is the relative good neonatal outcome after uterine rupture. The uterine rupture rate is high when compared with rates of 0.7%‐0.8% seen in spontaneous vaginal birth after cesarean section (VBAC).9, 18 This percentage must be included in counseling women who may be opting for an induced trial of labor. It is unclear whether there is a selection bias in the population or it is the balloon catheter that increases the risk of uterine rupture. Since most uterine ruptures occur in the active phase of labor, it is unlikely that the balloon catheter itself, used for cervical ripening, explains this increased risk.
Oxytocin for augmentation of labor was used in 77.5% of women, in keeping with rates quoted in the literature (68.4‐85.3%).9, 18 The rate of intra‐ and postpartum infection after induction of labor of 2.5% and 3.7%, respectively, is comparable to that found by Kruit et al (2.8% and 2.2%, respectively).
Of all cesarean sections after induction of labor, 50.8% were because of failure to progress in the first stage. Unfortunately, we were not able to record cervical dilation at the time of cesarean section. It is possible that many women in whom failure to progress in first stage was diagnosed, had not yet entered the accelerative phase, as commonly used standards to evaluate adequate progress of labor may not apply in women who are induced.19, 20
The strength of our study is that it is the largest cohort of inductions by balloon catheter to date, including almost 1000 women. By collecting information prospectively, and not relying on ICD 10 codes, all outcomes were studied specifically.
Limitations are the short follow‐up period (until discharge), so long‐term effects of possible consecutive cesarean sections were not included. Another weakness is the lack of randomization. Confounding by indication—which occurs when the clinical indication for selecting a particular treatment also affects the outcome—probably meant that the groups were not comparable at baseline for important prognostic factors. Although we have corrected for numerous possible confounders, there may still be some residual confounders that we could not correct for, such as hospital induction protocols and expected fetal weight. No randomized controlled trials, however, have been performed which compare induction of labor and planned repeat cesarean sections in women with a prior cesarean section.21 We considered randomization also to be unfeasible, after a randomized controlled trial on this subject in another country was stopped due to low participation rates. A large cohort study is then the best alternative.22
While cerebral palsy is thought to occur more often at an arterial umbilical cord pH <7.00, we chose to use the cut‐off of pH <7.10 for the adverse neonatal composite outcome. If we had chosen for a pH value of <7.00 or 7.05, it would mean that the incidence of adverse neonatal composite outcome would be even lower.
Another limitation is the difference in group size. The balloon catheter group is more than three times as large as the cesarean section group, partly because recruitment of women undergoing a repeat cesarean with the previous cesarean section as a single reason, was stopped after a few months.
With an unknown denominator of potentially eligible women meeting the inclusion criteria for the study in either the induction group or the repeat cesarean group, there is risk of selection bias or risk identification. For example, despite the fact that the median gestational age in the cesarean section group was shorter, mean neonatal birthweight was higher. This could possibly be the result of risk identification, where women carrying large‐for‐gestational‐age babies were not offered induction of labor.
We consider our findings to have value for low‐ and middle‐income settings. Although a more expectant management instead of induction may be preferred, regarding the higher rate of uterine rupture after induction compared with spontaneous vaginal birth after cesarean section, induction should still be considered if adequate fetal and maternal monitoring can be provided and emergency cesarean sections can be performed. If there is a medical indication for delivery, and there is enough time to start induction, this group of women will profit from the opportunity to have a vaginal birth instead of another cesarean, with high risks of abnormal invasive placentation in following pregnancies. Although not focused on in this manuscript, induction with balloon catheter compared with prostaglandins is cheaper and is associated with fewer abnormalities of contraction pattern, and fewer maternal side effects, and is thus well suited in resource‐poor settings.
With this large cohort study, more evidence is provided that induction of labor after cesarean section is an effective and safe option when an indication for delivery arises. Labor should be closely monitored for signs of uterine rupture, and facilities for emergency cesarean section are imperative. The rates of uterine rupture, emergency cesarean section and complications are useful for clinicians and pregnant women in the shared decision‐making process when facing this dilemma. Individual previous experiences, possible long‐term effects and future family planning have to be discussed. Individualized management in women with a previous cesarean section and an indication for delivery need to be considered. Both women's preferences and the a priori chance of vaginal delivery in case of induction can be helpful. Decision aids combined with a prediction model that includes induction as a variable can be considered.23, 24
5. CONCLUSION
In women with a previous cesarean section and a need for delivery, induction of labor with a balloon catheter does not result in a significant increase in adverse maternal and neonatal outcome as compared with planned cesarean section.
CONFLICT OF INTEREST
B.W.M. is supported by a NHMRC Practitioner Fellowship (GNT1082548). B.W.M. is a consultant for ObsEva, Merck and Guerbet.
Huisman CMA, ten Eikelder MLG, Mast K, et al. The PROBAAT‐S project group . Balloon catheter for induction of labor in women with one previous cesarean and an unfavorable cervix. Acta Obstet Gynecol Scand. 2019;98:920‐928. 10.1111/aogs.13558
Funding Information
Financial support of €25,000 was given by the Perinatology and Maternal Disease workgroup of the Dutch Society of Obstetrics and Gynecology NVOG and €25,000 by the Dutch Obstetric Consortium.
REFERENCES
- 1. Kwee A, Bots ML, Visser GH, Bruinse HW. Obstetric management and outcome of pregnancy in women with a history of caesarean section in the Netherlands. Eur J Obstet Gynecol Reprod Biol. 2007;132:171‐176. [DOI] [PubMed] [Google Scholar]
- 2. Locatelli A, Regalia AL, Ghidini A, Ciriello E, Biffi A, Pezzullo JC. Risks of induction of labour in women with a uterine scar from previous low transverse caesarean section. BJOG. 2004;111:1394‐1399. [DOI] [PubMed] [Google Scholar]
- 3. Ravasia DJ, Wood SL, Pollard JK. Uterine rupture during induced trial of labor among women with previous cesarean delivery. Am J Obstet Gynecol. 2000;183:1176‐1179. [DOI] [PubMed] [Google Scholar]
- 4. Durnwald C, Rouse DJ, Leveno KJ, et al. The maternal‐fetal medicine units cesarean registry: safety and efficacy of a trial of labor in preterm pregnancy after a prior cesarean delivery. Am J Obstet Gynecol. 2006;195:1119‐1126. [DOI] [PubMed] [Google Scholar]
- 5. Dekker G, Chan A, Luke CG, et al. Risk of uterine rupture in Australian women attempting vaginal birth after one prior caesarean section: a retrospective population‐based cohort study. BJOG. 2010;117:1358‐1365. [DOI] [PubMed] [Google Scholar]
- 6. Kayani SI, Alfirevic Z. Induction of labour with previous caesarean delivery: where do we stand? Curr Opin Obstet Gynecol. 2006;18:636‐641. [DOI] [PubMed] [Google Scholar]
- 7. Ophir E, Odeh M, Hirsch Y, Bornstein J. Uterine rupture during trial of labor: controversy of induction's methods. Obstet Gynecol Surv. 2012;67:734‐745. [DOI] [PubMed] [Google Scholar]
- 8. Bujold E, Blackwell SC, Gauthier RJ. Cervical ripening with transcervical foley catheter and the risk of uterine rupture. Obstet Gynecol. 2004;103:18‐23. [DOI] [PubMed] [Google Scholar]
- 9. Kruit H, Wilkman H, Tekay A, Rahkonen L. Induction of labor by Foley catheter compared with spontaneous onset of labor after previous cesarean section: a cohort study. J Perinatol. 2017;37:787‐792. [DOI] [PubMed] [Google Scholar]
- 10. Jozwiak M, van de Lest HA, Burger NB, Dijksterhuis MG, De Leeuw JW. Cervical ripening with Foley catheter for induction of labor after cesarean section: a cohort study. Acta Obstet Gynecol Scand. 2014;93:296‐301. [DOI] [PubMed] [Google Scholar]
- 11. American College of Obstetricians and Gynecologists . ACOG Practice Bulletin no. 115: Vaginal birth after previous cesarean delivery. Obstet Gynecol. 2010;116:450‐463. [DOI] [PubMed] [Google Scholar]
- 12. Birth after Previous Caesarean Birth (Green‐top Guideline No. 45). 2015. https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg45/.)
- 13. Zwangerschap en Bevalling na een Voorgaande Sectio Caesarea. 2010. https://www.nvog.nl/wp-content/uploads/2017/12/Zwangerschap-en-bevalling-na-een-voorgaande-sectio-caesarea-1.0-04-06-2010.pdf. Accessed 7 May 2018.
- 14. Betran AP, Ye J, Moller AB, Zhang J, Gulmezoglu AM, Torloni MR. The Increasing Trend in Caesarean Section Rates: Global, Regional and National Estimates: 1990‐2014. PLoS ONE. 2016;11:e0148343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. The Netherlands Perinatal Registry . Trends 1999–2012. Utrecht: The Netherlands Perinatal Registry; 2013. [Google Scholar]
- 16. Huisman CM, Jozwiak M, de Leeuw JW, Mol BW, Bloemenkamp KW. Cervical ripening in the Netherlands: a survey. Obstet Gynecol Int. 2013;2013:745159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zwart JJ, Richters JM, Ory F, de Vries JI, Bloemenkamp KW, van Roosmalen J. Uterine rupture in The Netherlands: a nationwide population‐based cohort study. BJOG. 2009;116:1069‐1078; discussion 78‐80. [DOI] [PubMed] [Google Scholar]
- 18. Kehl S, Weiss C, Rath W. Balloon catheters for induction of labor at term after previous cesarean section: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2016;204:44‐50. [DOI] [PubMed] [Google Scholar]
- 19. Harper LM, Caughey AB, Odibo AO, Roehl KA, Zhao Q, Cahill AG. Normal progress of induced labor. Obstet Gynecol. 2012;119:1113‐1118. [DOI] [PubMed] [Google Scholar]
- 20. Rinehart BK, Terrone DA, Hudson C, Isler CM, Larmon JE, Perry KG Jr. Lack of utility of standard labor curves in the prediction of progression during labor induction. Am J Obstet Gynecol. 2000;182:1520‐1526. [DOI] [PubMed] [Google Scholar]
- 21. Dodd JM, Crowther CA, Grivell RM, Deussen AR. Elective repeat caesarean section versus induction of labour for women with a previous caesarean birth. Cochrane Database Syst Rev. 2017;(7):CD004906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Crowther CA, Dodd JM, Hiller JE, Haslam RR, Robinson JS, Birth After Caesarean Study Group . Planned vaginal birth or elective repeat caesarean: patient preference restricted cohort with nested randomised trial. PLoS Med. 2012;9:e1001192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schoorel EN, van Kuijk SM, Melman S, et al. Vaginal birth after a caesarean section: the development of a Western European population‐based prediction model for deliveries at term. BJOG. 2014;121:194‐201; discussion. [DOI] [PubMed] [Google Scholar]
- 24. Schoorel EN, Vankan E, Scheepers HC, et al. Involving women in personalised decision‐making on mode of delivery after caesarean section: the development and pilot testing of a patient decision aid. BJOG. 2014;121:202‐209. [DOI] [PubMed] [Google Scholar]


