Abstract
Antimicrobial resistance (AMR) is now a global public health issue and is projected to affect the longevity of people and increase health expenditure of countries. Its impact is going to be higher in low-middle income countries as the healthcare systems are suboptimal and ill-equipped to deal with the issue. As antibiotic misuse is the primary driver for AMR, there is an acute need to create awareness among general public regarding antibiotic misuse. This calls for a comprehensive communication strategy, which takes into account the various drivers of AMR and the solutions associated with it. In the short term, the focus of communication strategies can be on raising awareness in specific interest groups. It can help in channeling limited resources to achieve specific objectives for raising awareness among these groups, thereby improving the chances of behavior change. The general public can be targeted at a later stage or as a second phase with definite strategies and messages. But, it is erroneous to assume that a higher level of awareness will translate into a positive change in behavior. We propose that behavior change is the final fruit of a long and dynamic process. This process should rest on four pillars: adequate awareness, robust regulatory environment, emotional or material incentives, and an enabling social structure. Unless all these domains are satisfactorily addressed, the communication strategy will not be able to bring about a discernible change in behavior in terms of antibiotic use.
Keywords: Antibiotics, antimicrobial resistance, behavioral change, communication, health system
Antibiotic Resistance as a Global Health Issue
Antimicrobial resistance (AMR) has emerged as one of the most difficult public health issues of the 21st century and is threatening to offset all our achievements in controlling communicable diseases. An accurate quantification of the impact of the problem may be difficult due to its complex nature and effect on diverse domains.[1] There are studies that demonstrate the impact of AMR on hospitalized patients showing a significant increase in hospital mortality, healthcare expenditure, and length of hospital stay.[2,3] The impact of AMR in low and middle income countries (LMIC) may become much higher than high income countries. Some studies have indicated that drug-resistant infections cause around 19,000 additional deaths in Thailand alone.[4] Some other projections have hypothesized that 58,000 deaths in India may be a result of drug-resistant organisms, which produce Extended Spectrum Beta Lactamase enzymes.[5] Antibiotic resistance, conservatively calculated, causes >500,000 deaths every year.[6] The healthcare costs associated with AMR are also difficult to estimate, but there has been report that currently it results in a total economic burden of USD 55 Billion in United States alone - USD 20 Billion in direct healthcare costs and USD 35 Billion in lost productivity.[7] All these factors make it essential that we invest time and resources to the study the drivers and impact of AMR and also devise sustainable solutions to the issue.
Misuse of Antibiotics as the Primary Driver of AMR
The misuse of antibiotics is documented from multiple sectors, and this is one of the main drivers of AMR. The excessive and often irrational use of antibiotics provides a selection pressure for the emergence of drug resistant strains of a micro-organism.[8] Antibiotics are often prescribed for trivial infections such as viral upper respiratory tract infection or uncomplicated diarrhea. In many developing countries, antibiotics are freely sold over the counter, without any medical advice or prescriptions.[9] Also, the right choice of antibiotics may not be prescribed to the patients, in the absence of effective diagnostic and culture facilities in many LMIC contexts.[10] Another dimension of this problem is the heavy use of antibiotics in food animal production. It has been reported that there is significant antibiotic use as growth promoters or for disease prophylaxis, in poultry and aquaculture sectors.[11] Antibiotics increase the “feed conversion efficiency” and negate the need to have robust biosecurity measures in farms, and therefore, its use may result in significant direct savings to the farmers.[12] Antibiotics, therefore, continue to be used in the absence of awareness among general public or significant pressure from consumer groups.[12] The misuse of antibiotics in the community may be a direct indicator of the poor regulatory framework and the level of awareness among the general public. Many doctors and veterinarians say that the pressure to prescribe antibiotics actually comes from their clients, as there is an erroneous perception among the general public about the utility of antibiotics in faster relief of health issues. Apart from having a more responsive regulatory system, there is an acute need to create awareness among general public regarding antibiotic misuse and AMR.
Designing Communication Strategies for AMR
Public awareness messaging is a resource intensive process if we have to engage all the stakeholders. Even if we create an adequate level of awareness, there is no guarantee that it will result in any change in behavior among the stakeholders. In the short and medium term therefore, focusing on raising awareness in specific interest groups may be a potential high impact activity. It can help in channeling limited resources to achieve specific objectives for raising awareness among these groups, thereby improving the chances of behavior change.[13] The general public can be targeted at a later stage or as a second phase with definite strategies and messages. When targeting the general public in any region/country, a baseline level of awareness should be measured using standardized tools such as Eurobarometer 445 or the tool developed by World Health Organization.[14] This is needed since a number of public awareness campaigns have not got sustainable funding in developing countries, as they were not able to show a demonstrable increase in the level of awareness.[13]
The messaging should be clear and unambiguous. Communication professionals with previous experience in health issues should ideally be leading the activity and there should be an attempt to tailor it to the sociocultural sensitivities of each region/country. The focus should be on three to four key messages relevant to the country setting, rather than bombarding the recipients with huge volume of information.[15] The messaging can possibly be directed at areas such as use of antibiotics for simple ailments like upper respiratory tract infections, diarrhea, and simple wounds; antibiotic use in food animal production; and environmental contamination from hospitals and pharmaceutical factories.[15]
Deciding Target Groups for Messaging
Users of antibiotics such as informal healthcare providers, nurse-practitioners, and small-scale farmers are often ignored in various campaigns to increase awareness about antibiotic misuse and AMR.[16] This can be a problem particularly in LMICs, as these groups generally outnumber the qualified medical practitioners or large-scale farmers. Raising awareness among school and college students can be a priority in all regions/countries. This can help in maximizing the impact of efforts/resources spends on the exercise of raising awareness. Basic modules on the human microbiome, issues regarding antibiotic use, rational drug use, and AMR can be incorporated into the curriculum of students, as well as the template of environmental stewardship and climate change taught to most students across the world.[17] The expertise and networks of civil society groups are often overlooked in the campaigns on antibiotic misuse and AMR. There should be an attempt to involve these groups in any activity/campaign aimed at improving awareness on AMR. Civil society groups may have a better reach and experience in advocacy-related domains and may help to complement the efforts of governmental agencies. There should also be an institutional mechanism to involve civil society at the region/country level.[18] Consumer groups and associations can play a pivotal role in increasing the awareness about antibiotic use in food animal production too. This will help to increase the demand for “antibiotic-smart” food and for farmers to adopt antibiotic-free farming especially in LMICs. Consumers willing to pay a premium for “antibiotic-smart” food can incentivise the farmers to adopt these sustainable practices in food production and thereby widen the net to other consumers too.[19]
Leadership in Communication and Raising Awareness
Leadership and responsibilities in awareness activities should be clearly defined before initiation. Health ministries or departments should take the lead in this activity as antibiotics are still perceived by the general public to be a domain related to human health. This can continue till a more robust interministerial agency or group is established in the country. A multi stakeholder approach is the best possible method in dealing with the issue.[20] Financing of activities related to raising awareness should be entirely financed by the government through budgetary provisions. Development funding or international aid should be looked at as a supplementary source of funds only and not the primary source.[21] Larger countries should look at establishing standalone interministerial agencies for implementation of the activities related to increasing awareness on antibiotic use and AMR. This can be the coordinating agency for operationalization of the respective national action plans. Smaller countries can have interministerial coordination group jointly funded by all the ministries involved for overseeing the implementation.[20] There should be civil society participation in the implementation process and also transparency in the decision-making process. The decision-making process should be based on clearly defined conventions or frameworks and possible conflicts of interest should be avoided.[22] The progress of activities involved in raising awareness and their impact should be monitored and evaluated by intergovernmental agencies mandated to do so. This is needed as AMR is an issue which can easily cross national boundaries. Care should be taken however to ensure that these evaluations do not compromise the principles of sovereignty of nations.[22] Agencies of UN such as UNESCO and UNICEF should be encouraged to be active partners and should assist WHO, FAO, and OIE in effectively designing messages regarding awareness on an international stage. The mandate for this partnership should come from the highest possible level; and the message should be transmitted at all levels of these agencies. A Global Health Partnership approach is best suited for a complex, global issue, such as AMR.[23]
Designing the Messaging Approach
When approaching specific interest groups with the aim of increasing awareness, a targeted approach should be taken rather than using general media tools. The existing communication channels between the government and these groups should be explored and utilized to its full potential rather than investing in new communication channels.[13] The issue of antibiotics residues in food served by quick service restaurant chains and varying standards followed by them regarding procurement of meat products in LMIC should be highlighted. This can possibly induce policy changes in the procurement practices of restaurant chains and also increase the demand for “antibiotic-smart” food among consumers.[24] The awareness on Human Immunodeficiency Virus (HIV) infection and its modes of transmission is high in most parts of the world. There should be an attempt to learn from the successes of how awareness was created for HIV and adapt it to the issue of AMR.[25]
There is a risk of groups with commercial interests (such as pharmaceutical companies or organisations funded by them) taking over the campaign and orienting it to ways which can benefit them or their interests. There should be an institutional mechanism, therefore, to evaluate potential partners regarding their commercial interests and funding channels.
Engaging Professional and Industry Groups
Raising the level of awareness among professional and occupational groups (who use or prescribe antibiotics) can lead to behavior change. It should, therefore, receive priority, while national action plans are operationalized.[13] Professional associations and trade unions can be effective tools to engage professional groups. Governments should take active interest in engaging these groups, directly or through civil society organisations. Besides a policy for engaging these groups, there should be a framework for engagement. Associations of medical/nursing practitioners, pharmacists, farmers, and other groups, such as teachers, provide a window of opportunity to improve awareness even among the general population.[26] International professional organizations/associations can also play an important role in raising awareness and bringing about behavior change. Since the mandate of these organizations is transnational, engagement can be done through specialized UN agencies. Industry groups and trade bodies should be engaged when operationalizing national action plans. The import of Active Pharmaceutical Ingredients and their distribution in the market can potentially be monitored with the help of trade bodies.[27] International and national bodies representing pharmaceutical industry should initiate stewardship conversations with different local companies engaged in manufacture/marketing of antimicrobial products.[28] Wherever possible, professional associations and industry groups should be encouraged to communicate their position statements and “code-of-conduct” for its members regarding antibiotic use, marketing, and AMR. The position statements and “code-of-conducts” can be tools to induce behavior change in the members, though these are in no way enforceable.[29] Specific training modules could be developed for engaging professional groups, and efforts should be made to increase awareness through short training sessions. There should be a clear action plan in place regarding development of these modules and administering them.[30] The mandate for engaging professional groups should be given to interministerial agency or coordination group (whichever is applicable). However, in large countries the regional health authorities can also help in effective engagement.
Stakeholders of the Messaging Strategy
Being a complex and multisectoral issue, AMR requires a broader approach in terms of building a consensus on the messages and the potential target audience. Large campaigns are sometimes effective in building awareness among general public and professional groups, but the efforts involved may be disproportional to the impact of the strategy.[31] Any such campaign also needs to identify the potential barriers at the level of individuals, communities, and health systems, which is possible only through a bottoms-up strategy. The primary care physicians, family physicians, local veterinarians, and local administrators are pivotal in ensuring the success of such campaigns. The role of family physicians in effective leadership of healthcare campaigns has been highlighted in multiple platforms.[32] For any messaging strategy or intervention to succeed in healthcare sector, it needs to be integrated into the routines of primary care, which is possible only through the support of primary care practitioners, family physicians, and the local health system administrators.[33] A similar level of support may also be required from the grass-roots leadership of those non-human sectors, which are big users of antimicrobial products. It has been demonstrated that such campaigns are effective in the domain of AMR, if there is a right messaging strategy, support from all the stakeholder groups, and an effective follow-up mechanism.[34] Therefore, a preliminary understanding of communication strategies for healthcare campaigns is a necessity among professional groups, which are stakeholders in the process of tackling AMR.
Awareness and Behaviour Change
Raising awareness on the misuse of antibiotics in various sectors is one of the most important steps in bringing about a sustainable change in behavior. Many healthcare planners and policymakers assume that increasing awareness will result in a change in behavior. However, this is mostly a very simplistic view of human decision-making processes.[35] We propose that behavior change is the final fruit of a long and hopefully dynamic process. This process should rest on four pillars: adequate awareness, robust regulatory environment, emotional or material incentives, and an enabling social structure. Along with the process of building adequate awareness on AMR, there should be efforts to address the other three areas mentioned above. We need a responsive and comprehensive regulatory system that can look at antibiotic use more holistically. There should be some kind of incentives for physicians, pharmacists, or farmers to rationalize antibiotic use. The society should start frowning upon the practice of using antibiotics irrationally. All these are essential for translating increase in awareness to a change in human behavior [Figure 1].
Figure 1.
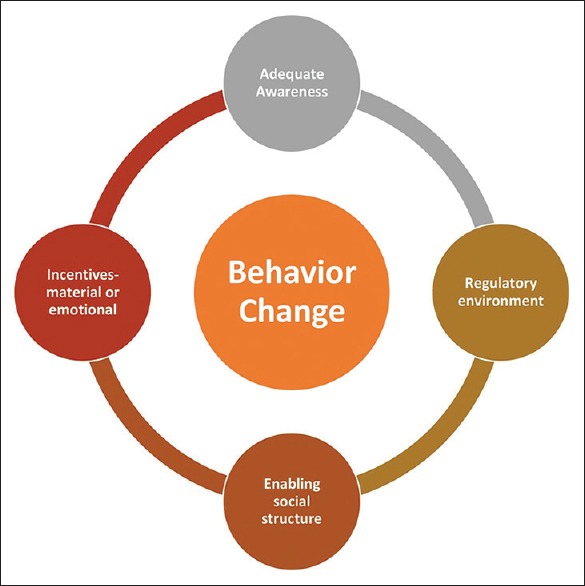
Behaviour change in public health
Conclusion
Effective communication plays a remarkable role in improving the level of community awareness about important healthcare issues. But increasing awareness alone does not result in significant behavior change, unless the issues are addressed holistically. The messaging should be culturally relevant and adapted to the preferences of the target population. Even though a multi-stakeholder approach is preferred, clear leadership responsibilities should be assigned in the whole communication processes. The role of champions and social influencers are very important in deciding the success of messaging, as their presence adds a layer of credibility to the whole exercise. In the case of AMR, it is pertinent that the messaging strategy should not be high jacked by commercial entities, who have conflicting interests in the sector. Even though professional and industry groups can be allies in a potential communication campaign on AMR, care should be taken to ensure that the process is free of any conflicts of interest. More importantly, it is pertinent to accept that awareness is just one part of the entire behavior change process and the targets for the communication campaign should not be restricted to raising of awareness.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.de Kraker MEA, Stewardson AJ, Harbarth S. Will 10 million people die a year due to antimicrobial resistance by 2050? PLoS Med. [Last accessed on 2019 Apr 05]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5127510/ [DOI] [PMC free article] [PubMed]
- 2.Lob SH, Biedenbach DJ, Badal RE, Kazmierczak KM, Sahm DF. Antimicrobial resistance and resistance mechanisms of Enterobacteriaceae in ICU and non-ICU wards in Europe and North America: SMART 2011-2013. J Glob Antimicrob Resist. 2015;3:190–7. doi: 10.1016/j.jgar.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Stewardson AJ, Allignol A, Beyersmann J, Graves N, Schumacher M, Meyer R, et al. The health and economic burden of bloodstream infections caused by antimicrobial-susceptible and non-susceptible Enterobacteriaceae and Staphylococcus aureus in European hospitals, 2010 and 2011: A multicentre retrospective cohort study. Euro Surveill. 2016;18:21. doi: 10.2807/1560-7917.ES.2016.21.33.30319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lim C, Takahashi E, Hongsuwan M, Wuthiekanun V, Thamlikitkul V, Hinjoy S, et al. Epidemiologyand burden of multidrug-resistant bacterial infection in a developing country. eLife [Internet] [cited 2019 Apr 05]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5030096/ [DOI] [PMC free article] [PubMed]
- 5.Laxminarayan R, Duse A, Wattal C, Zaidi AKM, Wertheim HFL, Sumpradit N, et al. Antibiotic resistance-the need for global solutions. Lancet Infect Dis. 2013;13:1057–98. doi: 10.1016/S1473-3099(13)70318-9. [DOI] [PubMed] [Google Scholar]
- 6.Fact sheet on ‘Antibiotic use, resistance and the link to nutrition. 2018. [Last accessed on 2019 Mar 04]. ReAct. Available from: https://www.reactgroup.org/wp-content/uploads/2018/02/ReAct-Factsheet_AntibioticResistance-Nutriton-and-Children-Feb-2018.pdf .
- 7.Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: A global multifaceted phenomenon. Pathog Glob Health. 2015;109:309–18. doi: 10.1179/2047773215Y.0000000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsueh P-R, Chen W-H, Luh K-T. Relationships between antimicrobial use and antimicrobial resistance in Gram-negative bacteria causing nosocomial infections from 1991-2003 at a university hospital in Taiwan. Int J Antimicrob Agents. 2005;26:463–72. doi: 10.1016/j.ijantimicag.2005.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li J, Song X, Yang T, Chen Y, Gong Y, Yin X, et al. A systematic review of antibiotic prescription associated with upper respiratory tract infections in China. Medicine (Baltimore) 2016;95:e3587. doi: 10.1097/MD.0000000000003587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuehn BM. IDSA: Better, faster diagnostics for infectious diseases needed to curb overtreatment, antibiotic resistance. JAMA. 2013;310:2385–6. doi: 10.1001/jama.2013.283828. [DOI] [PubMed] [Google Scholar]
- 11.Landers TF, Cohen B, Wittum TE, Larson EL. A review of antibiotic use in food animals: Perspective, policy, and potential. Public Health Rep. 2012;127:4–22. doi: 10.1177/003335491212700103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Economou V, Gousia P. Agriculture and food animals as a source of antimicrobial-resistant bacteria. Infect Drug Resist. 2015;8:49–61. doi: 10.2147/IDR.S55778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith RA, Quesnell M, Glick L, Hackman N, M’ikanatha NM. Preparing for antibiotic resistance campaigns: A person-centered approach to audience segmentation. J Health Commun. 2015;20:1433–40. doi: 10.1080/10810730.2015.1018652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mazińska B, Strużycka I, Hryniewicz W. Surveys of public knowledge and attitudes with regard to antibiotics in Poland: Did the European antibiotic awareness day campaigns change attitudes. Gupta V, ed? PLoS One. 2017;12:e0172146. doi: 10.1371/journal.pone.0172146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Godinho N, Bezbaruah S, Nayyar S, Gautam J, Sachdeva S, Behara I, Vong S. Antimicrobial resistance communication activities in South East Asia. BMJ. 2017;358:j2742. doi: 10.1136/bmj.j2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Founou LL, Founou RC, Essack SY. Antibiotic resistance in the food Chain: A developing country-perspective. Front Microbiol. 2016;7:1881. doi: 10.3389/fmicb.2016.01881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azevedo M-M, Pinheiro C, Yaphe J, Baltazar F. Assessing the impact of a school intervention to promote students’ knowledge and practices on correct antibiotic use. Int J Environ Res Public Health. 2013;10:2920–31. doi: 10.3390/ijerph10072920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nweneka CV, Tapha-Sosseh N, Sosa A. Curbing the menace of antimicrobial resistance in developing countries. Harm Reduct J. 2009;6:31. doi: 10.1186/1477-7517-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vanden Eng J, Marcus R, Hadler JL, Imhoff B, Vugia DJ, Cieslak PR, et al. Consumer attitudes and use of antibiotics. Emer Infect Dis. 2003;9:1128–35. doi: 10.3201/eid0909.020591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Birgand G, Castro-Sánchez E, Hansen S, Gastmeier P, Lucet JC, Ferlie E, et al. Comparison of governance approaches for the control of antimicrobial resistance: Analysis of three European countries. Antimicrob Resist Infect Control. 2018;7:28. doi: 10.1186/s13756-018-0321-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. Worldwide country situation analysis: Response to antimicrobial resistance. 2015. [Last accessed on 2019 Apr 05]. Available from: http://www.who.int/drugresistance/en/
- 22.Hoffman SJ, Ottersen T. Addressing antibiotic resistance requires robust international accountability mechanisms. J Law Med Ethics. 2015;43(Suppl 3):53–64. doi: 10.1111/jlme.12275. [DOI] [PubMed] [Google Scholar]
- 23.Ngoasong MZ. Transcalar networks for policy transfer and implementation: The case of global health policies for malaria and HIV/AIDS in Cameroon. Health Policy Plann. 2011;26:63–72. doi: 10.1093/heapol/czq018. [DOI] [PubMed] [Google Scholar]
- 24.Bhusan C, Khurana A, Tewari A. New Delhi: 2017. Double Standards, Antibiotic Misuse by Fast Food Companies, Centre for Science and Environment. [Google Scholar]
- 25.Peltzer K, Parker W, Mabaso M, Makonko E, Zuma K, Ramlagan S. Impact of national HIV and AIDS communication campaigns in South Africa to reduce HIV risk behaviour. ScientificWorldJournal. 2012;2012:384608. doi: 10.1100/2012/384608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Enani MA. Antimicrobial resistance: Insights from the declaration of world alliance against antibiotic resistance. Saudi Med J. 2015;36:11–2. doi: 10.15537/smj.2015.1.10362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.George A. Antimicrobial resistance, trade, food safety and security. One Health. 2018;5:6–8. doi: 10.1016/j.onehlt.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Declaration by the Pharmaceutical, Biotechnology and Diagnostics Industries on Combating Antimicrobial Resistance. [Last accessed on 2019 Apr 05]. Available from: https://www.ifpma.org/resource-centre/declaration-by-the-pharmaceutical-biotechnology-anddiagnostics-industries-on-combating-antimicrobialresistance/
- 29.Edwards R, Drumright L, Kiernan M, Holmes A. Covering more territory to fight resistance: Considering nurses’ role in antimicrobial stewardship. J Infect Prev. 2011;12:6–10. doi: 10.1177/1757177410389627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rogers VKS S, Jones SL, Hoffman SJ. Mapping educational opportunities for healthcare workers on antimicrobial resistance and stewardship around the world. Hum Resour Health. 2018;16:9. doi: 10.1186/s12960-018-0270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seymour J. The impact of public health awareness campaigns on the awareness and quality of palliative care. J Palliat Med. 2018;21:S30–6. doi: 10.1089/jpm.2017.0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.‘Health is primary’ launches to much fanfare at AAFP assembly. Ann Fam Med. 2015;13:87–8. doi: 10.1370/afm.1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen DJ, Tallia AF, Crabtree BF, Young DM. Implementing health behaviour change in primary care: Lessons from prescription for health. Ann Fam Med. 2005;3(Suppl 2):S12–9. doi: 10.1370/afm.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chaintarli K, Ingle SM, Bhattacharya A, Ashiru-Oredope D, Oliver I, Gobin M. Impact of a United Kingdom-wide campaign to tackle antimicrobial resistance on self-reported knowledge and behaviour change. BMC Public Health. 2016;16:393. doi: 10.1186/s12889-016-3057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Datta S, Mullainathan S. Behavioral design: A new approach to development policy. Review of Income and Wealth Series. 2014;60:7–35. [Google Scholar]


