Abstract
Poisoning is a leading cause of morbidity and mortality in India and also a major health problem worldwide. Majority of the studies shows that insecticides and pesticides compounds are the most widely used agents for poisoning.
Materials and Methods:
A retrospective study was conducted to explore the hospital records of patients with acute poisoning cases. A structured proforma used to collect data regarding patients’ demographic information, incidence of poisoning, cause and type of poisoning, clinical presentation of patient, treatment, and prognosis. Data were analyzed with descriptive and inferential statistics.
Results:
A total 505 patient files with poisoning cases were admitted at emergency department. The mean age of the patients was 28.43 ± 14 years (range 1–84 years). In gender-wise ratio, male patients (59%) were higher than the females (39%). The occurrence of poisoning was high 209 (41.38%) in young adult with age of 21–30 years. The causes of poisoning were suicide in 63.96% of cases. In majority, 310 (61.38%) patients consumed insecticides or pesticides. About 51.1% patients were treated at locally available medical facilities and 48.9% cases were brought to tertiary care center directly for the treatment. About 258 (51.08%) patients treated with gastric lavage, and for 9 (1.8%) patients endotracheal intubation was performed. The average stay in the hospital was 12.53 ± 7.53 days and mortality was 42 (8.31%).
Conclusion:
This study highlights that the incidence of poisoning and its morbidity and mortality can be reduced by development and implementation of effective intervention at primary level by health care providers and strategies on preventive aspect.
Keywords: Poisoning, primary care, tertiary care teaching hospital, treatment and prognosis
Introduction
Acute poisoning is one of the commonest causes of hospitalization to the emergency department.[1,2] Acute poisoning is a result of deliberate or accidental or homicidal ingestion of harmful chemical substance into the body. Death due to poisoning has been known since time immemorial. Poisoning is a major problem all over the world, as it is a silent weapon, which is used without any violence. An individual swallow poisoning substance and have a peaceful death instead of dying by hanging or physical harm to self.
Morbidity and mortality among poisoning cases depends on type of poisoning agent and country to country. In India, death due to poisoning is recorded as unnatural death along with registration in medicolegal case.[3,4] Many times due to lack of information accidental poisoning occurs. In general, among young adult suicidal poisoning and in children accidental poisoning is more common.[5] Industrialization and progress in agriculture has made a number of insecticides easily available to all, exposure to these products causes a severe toxicity.[1,5,6,7]
The purpose of studying poisoning cases is primarily determination of the occurrence of use of various toxic substances (poison), the corresponding area-wise distribution of type of poisoning in the demographic area, effectively received and duration of treatment received, proportional mortality (if any) - where several sociodemographic variation serves the purpose of the retrospective study conducted. The resulting evaluation is instrumental in prevention and management of future cases, along with providing proper education of children and guidelines to the parents or guardians to curb future possibilities of the incidents.
Materials and Methods
This was a retrospective study carried out in a tertiary care teaching hospital in Uttarakhand, India. All the cases admitted in the hospital from 2010 to 2014 were reviewed from data base of hospital information system and 505 poisoning cases were retrieved. These poisoning case files were screened and data were collected in May 2015 by self-prepared structured questionnaire. The structured questionnaire consist of patients’ age, gender, occupation, type and cause of poisoning, type of substance consumed, time of incidence, primary treatment, time duration to arrive to the tertiary care centre, clinical presentation of patients, treatment, prognosis, and duration of hospitalization. Data were entered in excel sheet, frequency, distribution, mean, standard deviation were computed. Administrative approval was taken to review patient's files.
Results
The incidence of poisoning was high which constitute about 6.2% of all cases registered during the study period of 2010–2014. The proportion of male patients was higher 298 (59%) than the females 207 (41%). The mean age was 28.43 ± 14 years (range 1–84 years), whereas, the incidence was highest among male and females in the age range from 21–30 years [Figure 1]. The reason of poisoning cases was committing suicide (63.96%), accidental (24.55%), homicide (3.76%), and unknown (7.72%). In majority of poisoning cases, 310 (61.38%) patients consumed organophosphorus compound (OPC), whereas other cases used medicinal (4.14%), corrosive (4.14%), phenol (3.16%), chemicals (1.98%), kerosene (1.58%), alcohol (1.38%), plants (1.38%). There were 59 (11.68%) cases with snake/scorpion/insect bites and 67 (13.26%) unknown [Figure 2].
Figure 1.
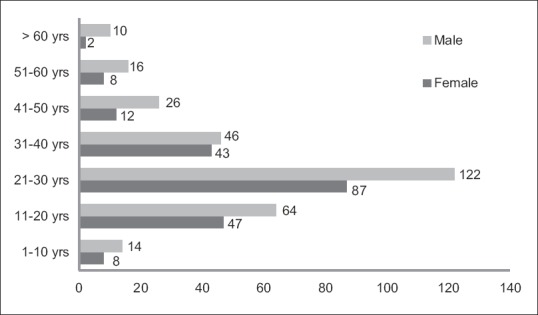
Age- and gender-wise distribution of poison cases
Figure 2.
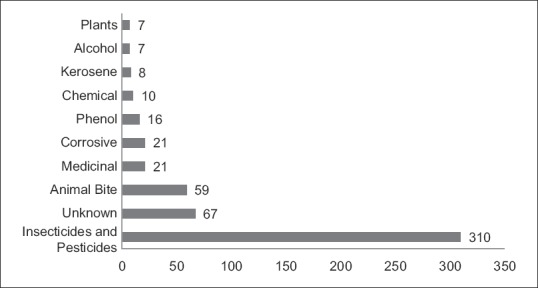
Poisoning agent among patients
Majority (49.1%), incidences occurred in day time (7 am to 7 pm) and almost one third (34.85%) in the night time (after 7 pm to before 7 am), in remaining (16.01%) cases, time of incidence was unavailable. Most common place of poisoning was at home (84.55%), remaining were in agriculture field/forest (2.97%), outdoor (2.17%), and unknown (10.29%).
About 51.1% patients were treated at locally available medical facilities, such as community health center (3.48%), district hospital (38.75%), and private clinic/nursing home (57.75%) and referred to tertiary care center. Remaining 48.9% cases were brought to tertiary care center directly for the treatment within the mean time duration of 3.3 hours. Whereas, those who were treated locally and then brought to tertiary care center took 6.9 hours of mean time [Figure 3]. More than half 280 (55.44) of cases had complaint of vomiting, 85 (16.83) had altered sensorium and 36 (7.12) had complaint of difficulty in breathing.
Figure 3.
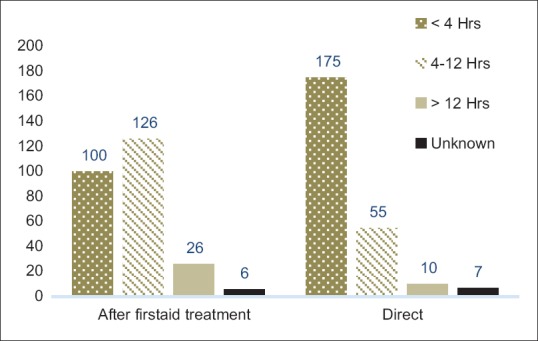
Time duration to reach at tertiary care center
In most of the cases, the body temperature was normal 451 (89.30%), while in few cases 20 (3.96%), 34 (6.73%) hyperthermia and hypothermia was recorded, respectively. Majority 401 (79.40%) patients were conscious, while 60 (11.88%) unconscious and 38 (7.52%) were semiconscious. A total of 8 patients developed seizures and 99 (19.60%) patient's oxygen saturation was below 95%.
About 258 (51.08%) patients treated with gastric lavage and for 9 (1.8%) patients endotracheal intubation was performed. Based on clinical presentation patients were treated with PAN 115 (22.77%), sodium bicarbonate 35 (6.93%), atropine 168 (33.26%), MgSO4 81 (16.03%), dopamine 28 (10.85%), Norad 8 (1.58%), Tab. Pantocid 365 (72.27%) and other symptomatic treatment was initiated in emergency department. Majority 426 (84.35%), patients required admission in different intensive care units. The average stay in the hospital was 12.53 ± 7.53 days and mortality was 42 (8.31%); while 8 (1.58%) patients got readmission. Furthermore, financial burden was estimated, an average hospital expenditure on medical care was Rs. 14,434.95.
Discussion
In the present study, ratio of male cases was higher (59%) than females (41%). Studies from India have reported with the similar proportions of male and female cases with poison.[4] In other studies, the male ratio was higher (3:1) than the present study results.[8,9] Study from Nepal[10] has shown M: F = 1:2, Albania[11] M: F = 0.09:1 and in Turkey and Ethiopia[12,13] M: F about 1:1.47.
Most of the poisoning cases were from the age group 21 to 30 years. Similar age group of poisoning cases was reported by various studies.[1,8,11,14,15] The age group between 21 and 30 is a productive period of life where individual get higher education and start earning for family and children. At the same time individual faces many challenges of life such as new jobs, settlement in marriage, and other social responsibilities.[1] Many times due to inability to cope up with life's stress and personality factors, the person commits suicide.
In the present study, the reason of poisoning for committing suicide was more (63.96%) than accidental (24.55%), homicidal (3.76%), and unknown (7.72%). The findings from other studies[1,9,10,12,16,17] have supported present study results where most of the poisoning cases were with committing suicide.
The most common substance for poisoning case was organophosphorus (61.38%), followed by snake/scorpion/insect bite, medicinal, corrosive, phenol, chemicals, kerosene, alcohol, plants, and 13.26% unknown substances. Studies[8,18] have reported that poisoning with organophosphorus compound was higher in proportion then other poisoning substances, whereas in other studies[1,4,15,19,20] reported of lower percentage of poisoning cases with organophosphorus than the present study results. It might be possible that insecticides and pesticides are readily available and easily accessible in Indian markets, including rural and urban areas to commit suicide.[21] These results shows an alarming sign where government need to make policies for strict and rationalized usage of such products. At the same time, primary health care provider at peripheral level should be trained enough to manage these kind of specific poisoning case.
It was observed that most of the cases of poisoning occurred in daytime (49.1%), whereas 34.85% incidences in the night-time, remaining 7.72% cases details were not available in records. Almost similar findings were observed in other studies.[1,22,23] In addition to that the most of poisoning cases occurred at home 427 (84.55%). Home was the most common place where 82% of incident reported by a study.[11]
Among all, about 258 (51.1%) cases reported that they were taken first aid/primary treatment at locally available medical facilities, such as community health center, district hospital, and private clinic/nursing homes and referred to higher center for further treatment and the average time was 6.9 hours to arrive at tertiary health care center from the place of incidence. Whereas 247 (48.9%) of poisoning cases reached to tertiary health care center directly within 3.3 hours of average time duration. Findings from other studies[17,22,24] reported of less time duration to arrive at tertiary care center than present study results. It may be due to geographical difference in Uttarakhand state and other part of study setting.
Surprisingly, mortality rate was low (3.16%) among patients who arrive directly to the tertiary care health center than who came after primary treatment (5.14%). Similar pattern was observed from other studies[19,25] of high mortality rate with larger time duration to initiate advance treatment with poisoning cases. It shows that patients who arrived to the tertiary health care center received advance medical care and timely treatment.
Clinical presentation of poisoning patients depends on various factors, type, quantity, and duration of exposure to poisoning substance. In present study, the most common symptoms were vomiting, nausea, altered sensorium, dyspnea, diarrhea hyper and hypothermia. Similar findings were observed in other studies.[10,17,26] High percentage (25–30%) was observed in other studies[12] where poisoning patients lost consciousness than the present study (11.88%). Hence, it is important for primary health care personals to identify the early signs of specific poisoning agent, start intervention appropriately, and refer them to higher center for advance treatment.
In poisoning cases, treatment plan determined by the type of poisoning agent and duration of ingestion. The most common treatment included gastric lavage, PAM, sodium bicarbonate, atropine, MgSO4, dopamine, mechanical ventilator, and other supportive therapy.[8,9,15,27,28] In most of the cases (84.35%), patients were admitted in different intensive care units initially, based on their clinical condition and then shifted to general wards.
The average stay in the hospital (12.53 ± 7.52 days) and financial expenditure was substantially high.[9] Mortality rate was found in accordance with other studies,[9,15,29] while a study[19] from Karnataka reported of high rate of mortality.
Poisoning act, intentionally or unintentionally both are dangerous. Once it occurs, it has to be identified, evaluated by poisoning severity score and intervene rapidly where the primary care physician, nurses, or other health care provider need to render first aid care and insist family/friend for rapid transport to the tertiary care center where poisoning cases can be managed with advanced health care facilities.
Conclusion
Acute poisoning is a medical emergency which require quick diagnosis and fast treatment. Early identification of type of poisoning, close observation, and standard management can reduce the complication and mortality rate. In present study, a high proportion of male and young adults was found. In the majority of patients, OPC was ingested deliberately for committing suicide. Timely initiation of medical management at primary level can save the life in acute poisoning cases, which was lacking among present study cases and resulted higher mortality and morbidity rate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank the administration of Himalayan Hospital, Dehradun for the granting permission for this study. The authors also like to thank Anil Negi, Ankit George, Mili Bhatia, Nargis, Mona Mathew, Neelam, Negi, Monika Rawat for their contribution in this study.
References
- 1.Dash SK, Raju AS, Mohanty MK, Patnaik KK, Mohanty S. Sociodemographic profile of poisoning cases. J Indian Acad Forensic Med. 2005;27:133–8. [Google Scholar]
- 2.Bamathy B, Punnagai K, Amritha CA, Chellathai DD. Incidence and patterns of acute poisoning cases in an emergency department of a tertiary care hospital in Chennai. Biomed Pharmacol J. 2017;10:1285–91. [Google Scholar]
- 3.Islam MN, Islam N. Retrospective study of 273 deaths due to poisoning at Sir Salimullah Medical College from 1988 to 1997. Leg Med. 2003;5:S129–31. doi: 10.1016/s1344-6223(02)00128-1. [DOI] [PubMed] [Google Scholar]
- 4.Singh RR, Singh RR, Kumar A, Uraiya D, Dhaon P. Retrospective analysis of poisoning cases admitted in a tertiary care hospital in North Eastern UP, India. [Last cited on 2019 Apr 22];Int J Med Res Rev [Internet] 2016 4:1172–7. Available from: http://medresearch.in/index.php/IJMRR/article/view/871 . [Google Scholar]
- 5.Das RK. Epidemiology of Insecticide poisoining at AIIMS Emergency Services and role of its detection by gas liquid chromatography in diagnosis. Medico-Legal Updat Int J. 2007;7:49–60. [Google Scholar]
- 6.Unnikrishnan B, Singh B, Rajeev A. Trends of acute poisoning in south Karnataka. Kathmandu Univ Med J. 2005;3:149–54. [PubMed] [Google Scholar]
- 7.Srivastava A, Peshin SS, Kaleekal T, Gupta SK. An epidemiological study of poisoning cases reported to the national poisons information centre, All India Institute of Medical Sciences, New Delhi. Hum Exp Toxicol. 2005;24:279–85. doi: 10.1191/0960327105ht527oa. [DOI] [PubMed] [Google Scholar]
- 8.Saxena V, Atal DK, Das S. Retrospective analysis of pattern of poisoning in Uttarakhand. J Indian Acad Forensic Med. 2014;36:230–3. [Google Scholar]
- 9.Kumar MR, Kumar GPV, Babu PR, Kumar SS, Subrahmanyam B V, Veeraprasad M, et al. A retrospective analysis of acute organophosphorus poisoning cases admitted to the tertiary care teaching hospital in South India. Ann Afr Med. 2014;13:71–5. doi: 10.4103/1596-3519.129876. [DOI] [PubMed] [Google Scholar]
- 10.Rehiman S, Lohani SP, Bhattarai MC. Correlation of serum cholinesterase level, clinical score at presentation and severity of organophosphorous poisoning. J Nepal Med Assoc. 2018;47:47–52. [PubMed] [Google Scholar]
- 11.Sulaj Z, Prifti E, Demiraj A, Strakosha A. Early clinical outcome of acute poisoning cases treated in intensive care unit. Med Arch. 2015;69:400–4. doi: 10.5455/medarh.2015.69.400-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yurumez Y, Durukan P, Yavuz Y, Ikizceli I, Avsarogullari L, Ozkan S, et al. Acute organophosphate poisoning in university hospital emergency room patients. Intern Med. 2007;46:965–9. doi: 10.2169/internalmedicine.46.6304. [DOI] [PubMed] [Google Scholar]
- 13.Adinew GM, Woredekal AT, DeVos EL, Birru EM, Abdulwahib MB. Poisoning cases and their management in emergency centres of government hospitals in northwest Ethiopia. African J Emerg Med. 2017;7:74–8. doi: 10.1016/j.afjem.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta BD, Vaghela PC. Profile of fatal poisoning in and around Jamnagar. J Indian Acad Forensic Med. 2005;27:145–8. [Google Scholar]
- 15.Dhanya SP, Dhanva TH, Latha RNB, Hema CG. A retrospective analysis of the pattern of poisoning in patients admitted to Medical College hospital. Calicut Med J. 2009;7:e3. [Google Scholar]
- 16.Thomas M, Anandan S, Kuruvilla PJ, Singh PR, David S. Profile of hospital admissions following acute poisoning--experiences from a major teaching hospital in south India. Adverse Drug React Toxicol Rev. 2000;19:313–7. [PubMed] [Google Scholar]
- 17.Patel DJ, Tekade PR. Profile of organophosphorus poisoning at maharani hospital, Jagdalpur, Chhattisgarh: A three years study. J Indian Acad Forensic Med. 2011;33:102–5. [Google Scholar]
- 18.Gupta P, Kumar A, Singh SP, Prakash M, Gupta M, Kumar P. Pattern of cases of acute poisoning in a rural tertiary care center in Northern India. Community Med. 2016;7:307–10. [Google Scholar]
- 19.Ramesha KN, Rao KBH, Kumar GS. Pattern and outcome of acute poisoning cases in a tertiary care hospital in Karnataka, India. Indian Soc Crit Care Med. 2009;13:152. doi: 10.4103/0972-5229.58541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gupta A, Kumar A, Joshi A. Socio-demographic profile of poisoning cases in a tertiary care teaching hospital of Uttarakhand. Ann Int Med Dent Res. 2017;3:1–3. [Google Scholar]
- 21.Gururaj G, Isaac MK. Epidemiology of Suicides in Bangalore [Internet] Bangalore: 2001. [cited 2019 Apr 03]. Available from: http://www.nimhans.ac.in/sites/default/files/Suicides Beyond Numbers.pdf . [Google Scholar]
- 22.Kora SA, Doddamani GB, Halagali GR, Vijayamahantesh SN, Boke U. Sociodemographic profile of the organophosphorus poisoning cases in Southern India. J Clin Diag Res. 2011;5:953–6. [Google Scholar]
- 23.Peranantham S, Shaha KK, Sahai A, Das S, Manigandan G, Shanmugam K. A hospital based epidemiological study of deaths due to organophosphorus compound poisoning. Indo Am J Pharm Res. 2014;4:3773–9. [Google Scholar]
- 24.Mishra A, Shukla SK, Yadav MK, Gupta AK. Epidemiological study of medicolegal organophosphorus poisoning in central region of Nepal. J Forensic Res. 2012;3:167. [Google Scholar]
- 25.Kumar SV, Venkateswarlu B, Sasikala M, Kumar GV. A study on poisoning cases in a tertiary care hospital. J Nat Sci Biol Med. 2010;1:35–9. doi: 10.4103/0976-9668.71671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Banerjee I, Tripathi SK, Roy AS. Clinico-epidemiological characteristics of patients presenting with organophosphorus poisoning. N Am J Med Sci. 2012;4:147–50. doi: 10.4103/1947-2714.93884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eddleston M, Buckley NA, Eyer P, Dawson AH. Management of acute organophosphorus pesticide poisoning. Lancet. 2008;371:597–607. doi: 10.1016/S0140-6736(07)61202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eddleston M, Singh S, Buckley N. Organophosphorus poisoning (acute) Clin Evid (Online) 2005;13:1744–55. [PubMed] [Google Scholar]
- 29.Eddleston M. Patterns and problems of deliberate self-poisoning in the developing world. QJM. 2000;93:715–31. doi: 10.1093/qjmed/93.11.715. [DOI] [PubMed] [Google Scholar]


