Abstract
Background:
Hypertension (HTN) is difficult to diagnose since it is asymptomatic. Most of the patients with HTN are unaware of their disease, and hence a large number of these subjects have target organ damage (TOD) on their first arrival at hospital or clinic. Hence, early detection and treatment of TOD determines the cardiovascular prognosis in hypertensive patient and can retard or prevent further damage.
Methods:
An observational and cross-sectional study was carried out in a tertiary care hospital and clinical profile was collected. Newly detected hypertensive men and women were recruited from outpatient and inpatient departments of medicine based on a set of inclusion and exclusion criteria. The study was carried out over a duration of 18 months from March 2014 to August 2015.
Results:
A total of 150 participants were included in the study with a mean age of 51.64 ± 11.64 years. A total of 91 participants had presence of at least one TOD. In our study, retinopathy (20.67%), macroalbuminuria (MA) (44.67%), electrocardiographic left ventricular hypertrophy (LVH) (20.67%), echocardiographic LVH (29.33%), diastolic dysfunction (21.33%), and systolic dysfunction (3.33%) were particularly notable. Grade 3 retinopathy, microalbuminria, and diastolic dysfunction were associated with severity of HTN.
Conclusion:
We conclude that a strong relationship exists between HTN and TOD. The evidence for TOD was found to be greater than that expected in newly detected hypertensive patients. Hence, a tight control of blood pressure represents the first step in treating essential HTN, which not only keep the blood pressure under control and further steps to be taken to prevent or retard the onset/progression of TOD.
Keywords: Hypertension, microalbuminuria, left venticular hypertrophy, retinopathy
Introduction
Hypertension (HTN) is a chronic medical condition in which the blood pressure (BP) in the arteries is elevated.[1] BP is summarized by two measurements, systolic and diastolic, which depend on whether the heart muscle is contracting (systole) or relaxed between beats (diastole) and equate to a maximum and minimum pressure, respectively. Normal BP at rest is within the range of 100–140 mmHg systolic (top reading) and 60–90 mmHg diastolic (bottom reading). High BP is said to be present if it is persistently at or above 140/90 mmHg [according to Joint National Committee (JNC) 7 hypertensive guidelines].
Worldwide, HTN is the leading risk factor for morbidity and mortality.[2] According to World Health Organization (WHO) global health report 2009, HTN is leading cause for mortality[3] (responsible for 13% of death globally). The prevalence of HTN in India is increasing, and notably it was 25% according to a previous report.[4]
HTN is difficult to diagnose since it is asymptomatic, and BP represents a dynamic measure with inherent minute-to-minute variability and the application of incorrect techniques lead to inaccurate measurements.[5] Furthermore, awareness, treatment, and control of HTN and also techniques available for measurement of BP among healthcare professionals remain suboptimal.[6,7]
Hence, HTN acts as a silent killer for many years before overt target organ damage (TOD) is clinically apparent. Most of the patients with HTN are unaware of their disease, and hence a large number of these subjects have TOD on their first arrival at hospital.[8]
The manifestations of TOD include micro- and macrovasculature pathology such as stroke, coronary artery disease/structural cardiac problems, retinopathy, proteinuria/chronic kidney disease (CKD), and atherosclerotic changes anywhere in the body system. The cost-effectiveness is greater and efficacy is lower for management of BP in patient with TOD.[9]
Methods
Patients
Patients above 18 years of age with newly detected HTN according to JNC-7 both men and women who meet the inclusion criterion were recruited from outpatient and inpatient departments of hospital.
HTN is defined as the systolic BP (SBP) ≥140 mmHg and diastolic BP (DBP) ≥90 mmHg. Stage I HTN is defined as SBP 140–159 mmHg or DBP 90–99 mmHg. Stage II HTN is defined as SBP ≥160 mmHg or DBP ≥100 mmHg as shown in Figure 1.
Figure 1.
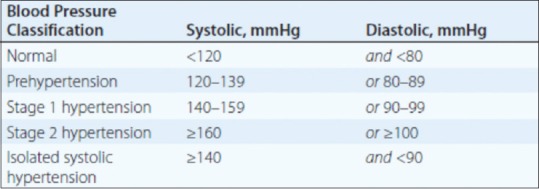
Classification of hypertension
Study design
An observational study and cross-sectional study was carried out, after the receipt of informed consent from the recruited patient and institutional ethical clearance. The study was carried out over a duration of 18 months from March 2014 to August 2015.
A total of 150 patients with newly detected HTN from outpatient and inpatient attending the hospital were included for this study based on a set of inclusion and exclusion criteria out of 395 patients consecutively seen. Patients with comorbid illness were excluded from the study. Of the remaining 164 patients, 14 patients refused to participate in the study as shown in Figure 2.
Figure 2.
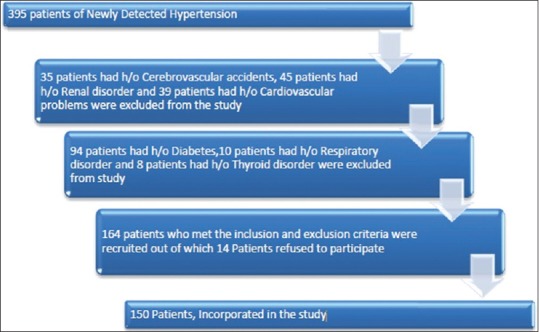
Patients’ recruitment for the study
BP of all patients was measured with dial sphygmomanometers, without coffee or tobacco consumption at least half hour before the procedure, after resting for 5–10 min, in a sitting position and having the arm supported at the level of the heart. Three consecutive measurements were performed and the mean BP was determined.
The target organs examined were as follows:
Retina (eye) – fundus examination with the help of ophthalmoscope.
Kidney – spot urine examination for the presence of microalbumin range of protein (30–300 mg/dL).
Heart – examination with the help of electrocardiogram (ECG) and echocardiography.
Statistical analysis
Baseline characteristics of study patients were expressed as mean and standard deviation. Z-test was performed to analyze the significance of mean and proportion differences observed between dependent variables. A P value ≤0.05 was considered statistically significant.
Results
Among total patients, 58.6% (n = 88) had stage I HTN and 41.4% (n = 62) had stage II HTN as shown in Figure 3 and Table 1.
Figure 3.
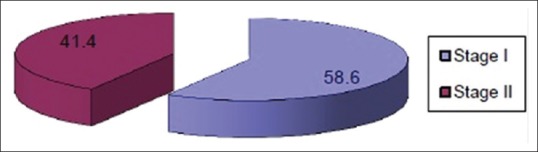
Study groups of patients according to the severity of hypertension
Table 1.
Study groups of patients according to the severity of hypertension
| Groups | Freq | % |
|---|---|---|
| Stage-I | 88 | 58.6 |
| Stage-II | 62 | 41.4 |
| Total | 150 | 100 |
Among 150 patients, 84 (56%) were males and 66 (44%) were females as shown in Table 2 the mean age of study participant was 51.65 11.64 years as shown in Figure 4.
Table 2.
Demographic profile (gender) of study patients
| Sex | Stage-I | Stage-II | ||
|---|---|---|---|---|
| Freq | % | Freq | % | |
| Male | 47 | 53.4 | 37 | 59.6 |
| Female | 41 | 46.6 | 25 | 40.4 |
| Total | 88 | 100 | 62 | 100 |
Figure 4.
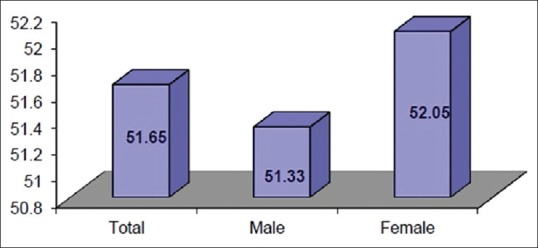
Mean age and gender of study patients
The mean body mass index (BMI) of the total study patients was 28.5 ± 6.26 kg/m2. Among that, the mean BMI of males was 28.5 ± 6.99 kg/m2 and females 28.5 ± 5.2 kg/m2 as shown in Figure 5.
Figure 5.

Number of study patients according to BMI (kg/m2) classification
The mean SBP among the total study participants was 156 ± 22.70 mmHg. The mean DBP among total participants was 93.27 ± 10.57 mmHg.
Retinopathy
The observation of hypertensive retinopathy (HR) grading (according to the Keith–Wagener–Barker classification) of the total study patients reflects the vascular damage to retina due to HTN, with the severity of HTN on Fundus Examination. A total of 31 (20.67%) patients had HR. Ten patients of stage I and seven patients of stage II HTN had grade 1 hypertensive changes. Seven and four patients of stage I and stage II HTN had grade 2 hypertensive changes, respectively. Three patients of stage II HTN had grade 3 hypertensive changes. However, no patients had grade 4 hypertensive changes as shown in Figure 6.
Figure 6.
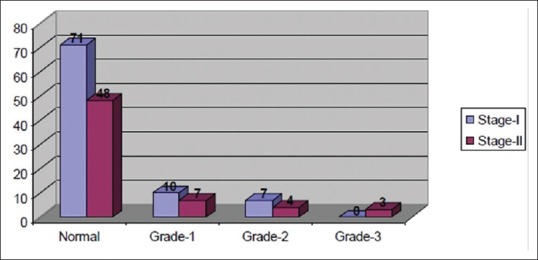
Comparison of study groups with severity of retinopathy
Microalbuminuria
The observation of urine for microalbumin (30–300 mg/day) of the total study patients reflects early damage to kidney due to HTN with the severity of Hypertension. A total of 67 (44.67%) patients had presence of MA; 35 of 88 patients of stage I HTN group and 32 of 62 patients of stage II HTN group had microalbumin range of protein in urine as shown in Figure 7.
Figure 7.
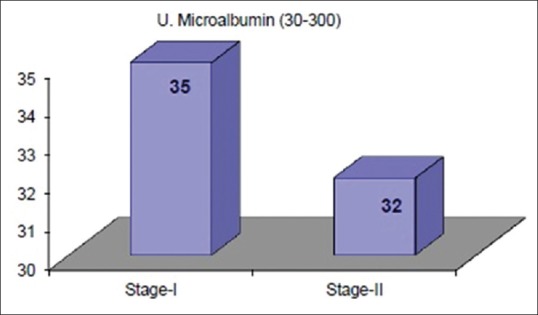
Comparison of study groups with microalbuminuria in patients
ECG findings
The observation of hypertensive changes on ECG (according to Sokolow–Lyon index criteria) of the total study patients reflects the hypertensive changes in heart with the severity of hypertention. A total of 31 (20.67%) patients had left ventricular hypertrophy (LVH) changes on ECG. 14 and 17 patients of stage I and stage II HTN group had LVH on ECG as shown in Figure 8.
Figure 8.
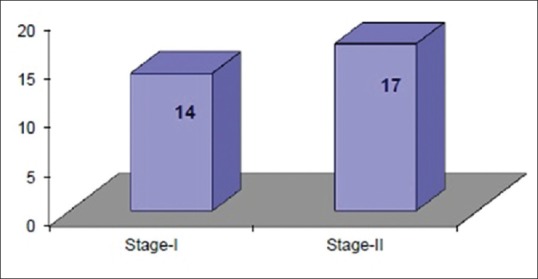
Comparison of study groups with left ventricular hypertrophy in patients on ECG
Echocardiography
The observation of hypertensive changes on echocardiography of the total study patients reflects the hypertensive changes in heart with the severity of HTN in terms of LVH and diastolic dysfunction. A total of 44 (29.33%) patients had increased left ventricular mass. About 22 and 22 patients of stage I and stage II HTN had presence of concentric LVH, respectively as shown in Figure 9, but the P values were not statistically significant. Three patients of stage II HTN had presence of dilated LVH. A total of 32 (21.33%) patients had presence of diastolic dysfunction. 12 and 20 patients of stage I and stage II HTN had diastolic dysfunction as shown in Figure 10.
Figure 9.
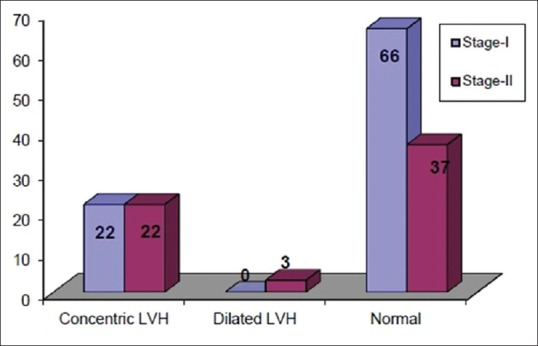
Pattern of LVH in study patients on echocardiography
Figure 10.
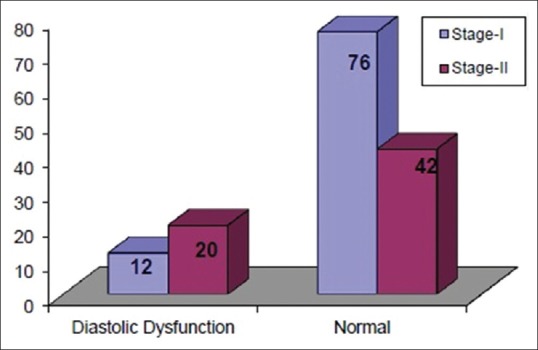
Pattern of diastolic dysfunction in study patients on echocardiography
Pattern of TOD
The TOD in the total 150 study patients shows that 91 (60.66%) patients had at least one target organ involvement. In all, 59 (39.33%) patients did not reveal any of the examined target organ involvement. Single TOD was present in 41 patients (27.33%). Two target organs were involved in 32 patients (21.33%). More than two target organs were involved in 18 patients (12%). Kidney was the most frequent organ involved.
Discussion
The study revealed that 58.6% (n = 88) patients had stage I HTN and 41.4% (n = 62) had stage II HTN, according to JNC-7. The study population in our setting belongs to the urban and semi-urban area. Also, the population in this community is busy in their metro life and as we know HTN is a silent killer, and most of the patients are unaware of their disease and present to their practitioner with relatively high BP values.
Our study revealed the presence of HR in 31 (20.67%) patients, of which 17 patients had grade 1 HR and 11 patients had grade 2 HR. However, only grade 3 HR which was present in stage II hypertensive patient shows association with severity of HTN. Indeed, increased BP may damage the microvasculature and induce retinal arteriolar narrowing.[10]
The presence of MA in 44.67% (n = 67) of patients also shows association with severity of HTN as it was significantly more present in stage II hypertensives. One patient had macroalbumin range of protein in urine. Atherosclerotic, HTN-related vascular lesions in the kidney primarily affect preglomerular arterioles resulting in ischemic changes in the glomeruli and postglomerular structures. Glomerular injury may also be a consequence of direct damage to glomerular capillaries due to glomerular HTN. Clinically, MA (random albumin/creatinine ratio 30–300mg/g) is an early marker of renal injury.[11] Hence, our observations must alert the physician to seek evidence for early CKD in hypertensive subjects and then initiate strategies to prevent MA.
Elecrocardiographic LVH was present in 20.67% of the patients, whereas LVH detected by echocardiography was present in 29.33% of the patients. It has been recognized that the echocardiographic monitoring system is more sensitive and specific than ECG measurements and chest X-ray evaluation for detection of LVH.[12] Our data also suggest more sensitivity of LVH detection by echocardioghaphy than ECG.
Diastolic dysfunction was present in 21.33% (n = 32) of patients. Dysfunction was associated with severity of HTN which was significantly raised in stage II HTN patients. In early stages of HTN, diastolic filling disorder can arise in view of delayed relaxation of left ventricle and subsequently diastolic failure occurs as a consequence of poor left ventricle compliance.[13]
In conclusion, presence of TOD in our study patients on their first arrival at the hospital indicates unawareness among the general population. Our study revealed presence of damage to one or more TOD in 60.66% of study patients. We conclude that a strong relationship exists between HTN and TOD; the evidence of TOD was found to be greater than that expected in newly detected hypertensive patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors 2001: System in analysis of population health data. Lancet. 2006;367:1747–57. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 3.Carretero OA, Oparil S. Essential hypertension. Part I: Definition and etiology. Circulation. 2000;101:329–35. doi: 10.1161/01.cir.101.3.329. [DOI] [PubMed] [Google Scholar]
- 4.Das SK, Sanyal K, Basu A. Study of urban community survey in India: Growing trend of high prevalence of hypertension in developing country. Inst Med Sci. 2005;2:70–8. doi: 10.7150/ijms.2.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rafey M. Beyond office sphygmomanometry: Ways to better assess blood pressure. Cleve Clin J Med. 2009;76:657–62. doi: 10.3949/ccjm.76gr.0409. [DOI] [PubMed] [Google Scholar]
- 6.Wolf Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, et al. Hypertension treatment and control in 5 European countries, Canada and the United States. Hypertension. 2004;43:10–7. doi: 10.1161/01.HYP.0000103630.72812.10. [DOI] [PubMed] [Google Scholar]
- 7.Meenakshisundaram R, Sweni S, Dhanalakshmi G, Sridevi R, Thirumalaikolundusubramanian P. Knowledge attitude, behaviour and practice of interns towards errors in sphygmomanometer and blood pressure measurements. J Clin Hypertens (Greenwich) 2009;11:748–52. doi: 10.1111/j.1751-7176.2009.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guidelines subcommittee. 1999 World Health Organization-International Society of Hypertension guidelines for the management of hypertension. J Hyperten. 1999;17:151–83. [PubMed] [Google Scholar]
- 9.Hitha B, Pappachan JM, Pillai HB, Sujathan P, Ramakrishna CD, Jayaprakash K, et al. Microalbuminuria in patients with essential hypertension and its relationship to target organ damage; an Indian experience. Saudi J Kidney Dis Transpl. 2008;19:411–9. [PubMed] [Google Scholar]
- 10.Leung H, Wang JJ, Rochtchina E, Tan AG, Wong TY, Klein R, et al. Relationships between age, blood pressure, and retinal vessel diameters in an older population. Invest Ophthalmol Vis Sci. 2003;44:2900–4. doi: 10.1167/iovs.02-1114. [DOI] [PubMed] [Google Scholar]
- 11.Kotchen TA. Hypertensive vascular disease. In: Longo DL, Kasper DL, Jameson JL, Fauci AS, Hauser SL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 19th ed. USA: McGraw-Hill Education; 2015. pp. 1611–7. [Google Scholar]
- 12.Lorell BH, Carabello BA. Left ventricular hypertrophy: Pathogenesis, detection, and prognosis. Circulation. 2000;102:470–9. doi: 10.1161/01.cir.102.4.470. [DOI] [PubMed] [Google Scholar]
- 13.Schwab J, Schneider MP, Pauschinger M, Schmieder RE. Hypertension and diastolic dysfunction. MMW Fortschr Med. 2009;151:41–3. doi: 10.1007/BF03365781. [DOI] [PubMed] [Google Scholar]


