Abstract
Background
We assessed the relationship between body mass index and results of rehabilitation in stroke patients.
Material/Methods
The study was carried out at the Clinical Rehabilitation Ward with Early Neurological Rehabilitation Unit at the Clinical Hospital. The examinations were performed 3 times. Based on inclusion and exclusion criteria, 128 subjects were qualified for the first examination, the second examination involved 114 subjects, and 100 stroke patients participated in the third examination. Body mass was examined with an accuracy of 0.1 kg, using a Tanita MC–780 MA body composition analyser. Body mass index (BMI) was calculated for all of the subjects. Effects of rehabilitation were assessed with the Barthel index and Ashworth scale.
Results
Higher functional status in daily life, measured with the Barthel scale, was found in patients with normal body mass, compared to the overweight and obese subjects (examination I, II, and II). Exam I showed that before rehabilitation the overweight patients obtained significantly higher results in assessment of upper limbs, based on the Ashworth scale (mean=0.35±0.54) compared to the obese patients (mean=0.03±0.32) and those with normal body weight (mean=0.24±0.75).
Conclusions
Following hospital-based rehabilitation, patients with normal body mass achieved greater functional efficiency. The findings also show a trend towards normalization of BMI. The positive effect of rehabilitation was sustained for 3 months (Exam III), which may contribute to decreased risk of cardiovascular diseases and complications such as stroke.
MeSH Keywords: Body Mass Index, Rehabilitation, Stroke
Background
According to current data, stroke today is one of the main causes of morbidity, mortality, and long-term disability. It is estimated that the problem annually affects 15 million people worldwide, and 1 in 3 stroke patients die as a result. The worldwide prevalence of stroke was estimated to be 33 million in 2010. Stroke is the third most common cause of mortality, exceeded only by cardiovascular diseases and cancer. Stroke symptoms pose a significant diagnostic problem. Stroke leads to disabilities affecting patients and their families, and to various socioeconomic consequences [1–4]. The major problems include the costs of treatment, long-term care, and rehabilitation [5]. Cerebral complications of cardiovascular disorders may be prevented by significant modifications of the factors affecting people at risk of stroke. It has been emphasised in the literature that susceptibility results from multiple coexisting risk factors in most cases. Primary as well as secondary preventive measures are of extreme importance. Effective prevention is possible only if the causes of stroke are clearly understood, if health symptoms are treated, and if risk factors are eliminated. Stroke itself is not a long process; however, its consequences may accompany patients for the rest of their lives. Therefore, it is necessary to initiate rehabilitation tailored to the specific needs of the patients and designed to improve their performance, and to ensure their adaptation to the environment in which they functioned before the stroke. Obesity is one of the modifiable factors, adversely affecting recovery not only after stroke but also following many other diseases. Excessive weight is recognised as the primary factor contributing to hypertension [6,7]. Furthermore, many researchers emphasise that obesity is associated with the activity of proteins stimulating the nervous system and microcirculation, which generates other coexisting health problems increasing the risk of stroke [8]. Numerous studies confirm the relationship between obesity and stroke incidence, which also correlates with age and other environment-related factors [9,10]. At present, obesity is recognised as a separate disease entity, which in the USA, for example, is responsible for 20% of all deaths [11].
Obesity is one of the potentially modifiable risk factors for stroke, and the related guidelines advocate normal body weight as a way to decrease the risk of stroke [12]. In the literature, there is scarce research investigating the relationship of body mass and rehabilitation outcomes in stroke patients. Available studies focusing on stroke patients assessed the relationship between BMI (body mass index) and functional recovery using only single scales and indexes for activities of daily living [13,14]. The present study was designed to assess the effects of hospital-based rehabilitation administered to stroke patients in relation to their BMI. We designed this study to determine whether the effects of rehabilitation would be sustained in patients’ home environments for up to 3 months following discharge from the Clinic, and to assess whether BMI is associated with the effectiveness of the rehabilitation administered.
Material and Methods
The study was approved by the Local Bioethics Commission (Consent No. 2015/05/10 issued on March 25, 2015). The participants were informed about the research procedure. Written consent was obtained from the director of the Clinic, Head Doctor of the Rehabilitation Clinic, and from the stroke patients.
Participants
During the study (from June 2015 to March 2017), the Clinical Rehabilitation Ward with Early Neurological Rehabilitation Unit at the Clinical Regional Hospital provided treatment to a total of 1143 patients.
All of the stroke patients participated in a comprehensive rehabilitation program lasting 5 weeks at the Clinical Rehabilitation Ward. The patients were examined 3 times. The first examination (Exam I) was performed on admission to the Clinic, before the rehabilitation started. The second examination (Exam II) was performed on discharge, after the 5-week hospital-based rehabilitation. The third examination (Exam III) was carried out 3 months after discharge from the Clinic, during a follow-up visit. It was assumed that Exam I provided control data for Exam II. The third examination was designed to determine whether the effects of rehabilitation and body mass composition identified during Exam II had been sustained.
The following inclusion criteria were used: stroke was experienced, able to stand without assistance, able to walk without aid, no impairments of higher mental functions, and the patient was informed and voluntarily agreed to participate in the study.
Exclusion criteria were: lack of patient consent to participate in the study, lack of ability to stand without assistance, ischemic lesion located in the cerebellum and brain stem, metal or electronic implants, epilepsy, pregnancy or menstruation, and limb injuries incurred following stroke onset prior to the examination.
Outcome measures
The height was measured with an accuracy of 0.1 cm using a PORTSTAND 210 portable stadiometer. Body mass was examined with an accuracy of 0.1 kg using a Tanita MC – 780 MA body composition analyser. The measurements were performed in standard conditions. The subjects, in underwear and with no shoes, were instructed to assume a straight body posture.
Body mass index (BMI) was calculated based on the results of body height and mass measurements. BMI values were analysed by reference to the WHO classification of obesity: BMI ≤18.49 underweight, 18.5–24.99 normal weight, 25–29.99 overweight, ≥30 obesity [15].
Activities of daily living were assessed using the Barthel index, with a maximum possible score of 100 points [16,17]. Muscle tone was assessed with a modified Ashworth scale, which is a 6-point scale modified to include grade 1+ [18].
Rehabilitation program
The subjects participated in exercise 5 days per week for 5 weeks. The comprehensive rehabilitation program administered to all of the patients included morning exercise, individual practice based on neuro-developmental treatment (NDT Bobath) and the PNF method addressing the impaired motor abilities, as well as exercise based on equipment using biological feedback: a Balance Trainer (static and dynamic parapodium) and the Pablo system designed for upper-limb training.
Data analysis
The analyses applied descriptive statistics (mean with 95% confidence interval, standard deviation, standard error, measure of observation location). Differences between quantitative variables and nominal dichotomous independent variables were examined using the Mann-Whitney test. The significance of the differences between quantitative variables and variables of more than 2 categories was assessed using the Kruskal-Wallis test. The tests were selected taking into account normal distributions of the quantitative variables (verified with Kolmogorov-Smirnov and Shapiro-Wilk tests) as well as the equinumerosity of the groups of independent variables (verified with χ2 test). Significance level was assumed when α<0.05. The power of the test was 0.9; therefore, the maximum error was 10%. All of the calculations and the statistical analyses were computed using STATISTICA ver. 10.0 (StatSoft).
Results
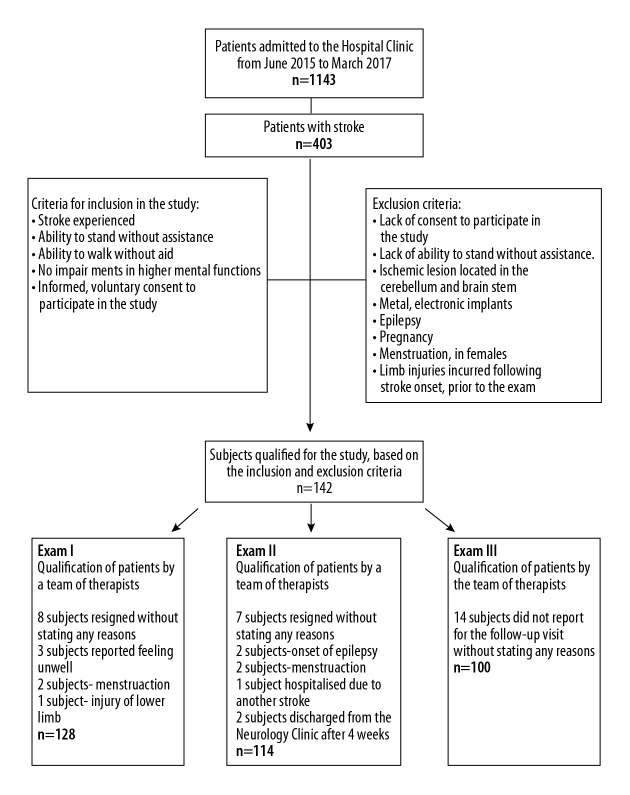
Out of 1143 individuals receiving rehabilitation on the ward during the study, stroke patients constituted 35% (403 individuals). Based on the inclusion criteria, 128 subjects were qualified for the first examination (Exam I). Exam II, again preceded by a qualification procedure, involved 114 patients. Ultimately, 100 patients reported for Exam III, which was performed during a follow-up visit. In the study group, 82% (82 individuals) of patients had experienced ischemic stroke and 18% (18 individuals) had hemorrhagic stroke. The effects of rehabilitation and body mass composition were assessed during the 3 examinations; therefore, analysis of the results took into account the 100 subjects participating in all of the examinations (Exam I, Exam II, and Exam III). After Exam II, each patient received recommendations for comprehensive rehabilitation to be continued after discharge from the hospital. This included therapies provided at home or in outpatient settings, as well as rehabilitation carried out by family members in accordance with instructions received from the team of therapists (Figure 1).
Figure 1.
Study flow diagram.
The subjects’ mean age was 58.34±14.54 years, ranging from 19 to 88 years. The specific age groups, i.e., 19–50 (n=23), 51–65 (n=42), and 66–88 (n=35), accounted for 23%, 42%, and 35% of the group, respectively. Males and females constituted 58% (n=58) and 42% (n=42), respectively. The findings showed that 33% (n=33) of the subjects were normal weight, 37% (n=37) were overweight, and 30% (n=30) were obese.
The study identified no significant correlation between BMI and the subjects’ sex. The findings, however, show that at the end of the hospital-based rehabilitation, in Exam II the values of BMI had decreased (females: Exam I: 27.17±5.05, Exam II: 27.09±5.00; males: Exam I: 27.84±4.54, Exam II: 27.77±4.40) and were sustained 3 months after discharge from the hospital (Exam III: females 27.02±5.02; males 27.81±4.64). With regard to the patients’ age, it was found that in Exam I the older patients presented higher BMI (p=0.003). Following the rehabilitation, the entire group was found to have decreased BMI. Exam III showed that BMI values remained at a similar level 3 months after the end of the rehabilitation (p=0.001) (Table 1).
Table 1.
BMI relative to the subjects’ sex and age.
| BMI | Sex | p | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | |||||||||||||||
| N=42 | N=58 | |||||||||||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | |||||||
| I | 27.17 (25.60–28.75) | 5.05 (0.51) | 23.30 | 25.95 | 30.90 | 27.85 (26.65–29.04) | 4.54 (0,45) | 24.60 | 27.50 | 30.40 | 0.514 | |||||
| II | 27.09 (25.53–28.65) | 5.00 (0,5) | 23.00 | 25.80 | 30.90 | 27.77 (26.62–28.93) | 4.40 (0,44) | 25.10 | 27.45 | 29.80 | 0.398 | |||||
| III | 27.02 (25.45–28.58) | 5.02 (0,5) | 23.10 | 25.90 | 30.90 | 27.81 (26.59–29.03) | 4.64 (0,46) | 24.10 | 27.70 | 29.80 | 0.431 | |||||
| BMI | Age | p | ||||||||||||||
| 19–50 years | 51–65 years | 66–88 years | ||||||||||||||
| N=23 | N=42 | N=35 | ||||||||||||||
| Mean (95%Cl) | SD (SE) | Q1 | Me | Q3 | Mean (95%Cl) | SD (SE) | Q1 | Me | Q3 | Mean (95%Cl) | SD (SE) | Q1 | Me | Q3 | ||
| I | 26.52 (24.57–28.47) | 4.51 (0,45) | 22.60 | 25.50 | 30.70 | 26.44 (24.91–27.97) | 4.91 (0,49) | 23.30 | 25.95 | 29.00 | 29.60 (28.18–31.01) | 4.12 (0.41) | 25.40 | 29.30 | 32.30 | 0.003 |
| II | 26.46 (24.62–28.30) | 4.25 (0,43) | 22.40 | 26.30 | 29.40 | 26.40 (24.89–27.92) | 4.86 (0,49) | 23.00 | 25.80 | 28.80 | 29.46 (28.06–30.86) | 4.07 (0.41) | 25.60 | 29.40 | 32.30 | 0.003 |
| III | 26.30 (24.43–28.18) | 4.33 (0,43) | 22.40 | 26.40 | 29.20 | 26.43 (24.82–28.05) | 5.18 (0.52) | 23.10 | 25.90 | 28.20 | 29.50 (28.13–30.87) | 3.98 (0.4) | 25.80 | 29.40 | 32.30 | 0.001 |
BMI – body mass index; N – number of subjects; CI – confidence interval; SD – standard deviation; SE – standard error; Max – maximum value; Me – median; Min – minimum value, Q1 – quartile I, Q3 – quartile III; Mann-Whitney test for sex, Kruskal-Wallis test for age.
Exam I showed that before rehabilitation the overweight patients obtained significantly higher results in assessment of upper limbs, based on the Ashworth scale (mean=0.35±0.54) compared to the obese patients (mean=0.03±0.32) and those with normal body weight (mean=0.24±0.75). No statistically significant differences were found between the results obtained using the relevant scales in relation to the patients’ body mass category (overweight/obesity) (Table 2). Results of Exam II and Exam III did not show significant differences between the functional condition of overweight and obese patients at the end of the rehabilitation program (Tables 3, 4). Exam III, conducted 3 months after the end of the rehabilitation, in assessment of upper limbs based on the Ashworth scale, showed significantly higher values in overweight patients (mean=0.28±0.55) than in obese patients (mean=0.04±0.34). Despite the lack of statistical significance between the functional condition of overweight and obese patients in Exams II and III, a higher functional status in daily life, measured with the Barthel scale, was found in the patients with normal body mass compared to the overweight and obese subjects (Exams I, II, and III) (Table 4).
Table 2.
The functional status (Barthel index, Ashworth scale) before rehabilitation program (Exam I).
| Exam I | BMI | |||||
|---|---|---|---|---|---|---|
| Normal | p | |||||
| N=33 | ||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | ||
| Effect of rehabilitation (Barthel) | 16.06 (11.59–20.53) | 12.61 (1.3) | 10.00 | 15.00 | 20.00 | 0.9509 |
| Effect of rehabilitation (Ashworth hand) | 0.21 (0.02–0.41) | 0.55 (0.06) | 0.00 | 0.00 | 0.00 | 0.2588 |
| Effect of rehabilitation (Ashworth arm) | 0.24 (−0.02–0.51) | 0.75 (0.08) | 0.00 | 0.00 | 0.00 | 0.0483 |
| Effect of rehabilitation (Ashworth leg) | 0.03 (−0.14–0.20) | 0.47 (0.05) | 0.00 | 0.00 | 0.00 | 0.2917 |
| Exam I | Overweight | p | ||||
| N=37 | ||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | ||
| Effect of rehabilitation (Barthel) | 15.00 (10.77–19.23) | 12.69 (1.3) | 5.00 | 15.00 | 25.00 | 0.9509 |
| Effect of rehabilitation (Ashworth hand) | 0.41 (0.22–0.59) | 0.55 (0.06) | 0.00 | 0.00 | 1.00 | 0.2588 |
| Effect of rehabilitation (Ashworth arm) | 0.35 (0.17–0.53) | 0.54 (0.05) | 0.00 | 0.00 | 1.00 | 0.0483 |
| Effect of rehabilitation (Ashworth leg) | 0.16 (0.04–0.29) | 0.37 (0.04) | 0.00 | 0.00 | 0.00 | 0.2917 |
| Exam I | Obesity | p | ||||
| N=30 | ||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | ||
| Effect of rehabilitation (Barthel) | 14.67 (10.97–18–37) | 9.91 (0.99) | 10.00 | 15.00 | 20.00 | 0.9509 |
| Effect of rehabilitation (Ashworth hand) | 0.23 (−0.02–0.49) | 0.68 (0.07) | 0.00 | 0.00 | 1.00 | 0.2588 |
| Effect of rehabilitation (Ashworth arm) | 0.03 (−0.09–0–15) | 0.32 (0.03) | 0.00 | 0.00 | 0.00 | 0.0483 |
| Effect of rehabilitation (Ashworth leg) | 0.03 (−0.09–0.15) | 0.32 (0.03) | 0.00 | 0.00 | 0.00 | 0.2917 |
BMI – body mass index; N – number of subjects; CI – confidence interval; SD – standard deviation; SE – standard error; Max – maximum value; Me – median; Min – minimum value, Q1 – quartile I, Q3 – quartile III; test Kruskal-Wallis.
Table 3.
The functional status (Barthel index, Ashworth scale) at the end of the hospital-based rehabilitation (Exam II).
| Exam II | BMI | |||||
|---|---|---|---|---|---|---|
| Normal | p | |||||
| N=33 | ||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | ||
| Effect of rehabilitation (Barthel) | 15.65 (11.26–20.03) | 11.95 (1.2) | 10.00 | 15.00 | 25.00 | 0.9514 |
| Effect of rehabilitation (Ashworth hand) | 0.26 (0.05–0.47) | 0.58 (0.06) | 0.00 | 0.00 | 1.00 | 0.8232 |
| Effect of rehabilitation (Ashworth arm) | 0.32 (0.05–0.60) | 0.75 (0.08) | 0.00 | 0.00 | 1.00 | 0.1568 |
| Effect of rehabilitation (Ashworth leg) | 0.10 (−0.08–0.27) | 0.47 (0.05) | 0.00 | 0.00 | 0.00 | 0.7909 |
| Exam II | Overweight | p | ||||
| N=37 | ||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | ||
| Effect of rehabilitation (Barthel) | 15.48 (11.50–19.46) | 12.77 (1.28) | 5.00 | 15.00 | 20.00 | 0.9514 |
| Effect of rehabilitation (Ashworth hand) | 0.33 (0.17–0.50) | 0.53 (0.05) | 0.00 | 0.00 | 1.00 | 0.8232 |
| Effect of rehabilitation (Ashworth arm) | 0.26 (0.09–0.43) | 0.54 (0.05) | 0.00 | 0.00 | 1.00 | 0.1568 |
| Effect of rehabilitation (Ashworth leg) | 0.10 (−0.02–0.21) | 0.37 (0.04) | 0.00 | 0.00 | 0.00 | 0.7909 |
| Exam II | Obesity | p | ||||
| N=30 | ||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | ||
| Effect of rehabilitation (Barthel) | 14.44 (10.36–18.53) | 10.32 (1.03) | 5.00 | 15.00 | 20.00 | 0.9514 |
| Effect of rehabilitation (Ashworth hand) | 0.26 (−0.02–0.54) | 0.71 (0.07) | 0.00 | 0.00 | 1.00 | 0.8232 |
| Effect of rehabilitation (Ashworth arm) | 0.04 (−0.10–0.17) | 0.34 (0.03) | 0.00 | 0.00 | 0.00 | 0.1568 |
| Effect of rehabilitation (Ashworth leg) | 0.04 (−0.10–0.17) | 0.34 (0.03) | 0.00 | 0.00 | 0.00 | 0.7909 |
BMI – body mass index; N – number of subjects; CI – confidence interval; SD – standard deviation; SE – standard error; Max – maximum value; Me – median; Min – minimum value, Q1 – quartile I, Q3 – quartile III; test Kruskal-Wallis.
Table 4.
The functional status (Barthel index, Ashworth scale) at the end of the rehabilitation program (Exam III).
| Exam III | BMI | |||||
|---|---|---|---|---|---|---|
| Normal | p | |||||
| N=33 | ||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | ||
| Effect of rehabilitation (Barthel) | 15.45 (11.34–19.57) | 11.62 (1.16) | 10.00 | 15.00 | 20.00 | 0.9598 |
| Effect of rehabilitation (Ashworth hand) | 0.24 (0.04–0.44) | 0.56 (0.06) | 0.00 | 0.00 | 0.00 | 0.6723 |
| Effect of rehabilitation (Ashworth arm) | 0.30 (0.04–0.56) | 0.73 (0.07) | 0.00 | 0.00 | 1.00 | 0.1559 |
| Effect of rehabilitation (Ashworth leg) | 0.09 (−0.07–0.25) | 0.46 (0.05) | 0.00 | 0.00 | 0.00 | 0.7903 |
| Exam III | Overweight | p | ||||
| N=37 | ||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | ||
| Effect of rehabilitation (Barthel) | 15.63 (11.45–19.80) | 13.07 (1.3) | 5.00 | 15.00 | 22.50 | 0.9598 |
| Effect of rehabilitation (Ashworth hand) | 0.35 (0.18–0.52) | 0.53 (0.05) | 0.00 | 0.00 | 1.00 | 0.6723 |
| Effect of rehabilitation (Ashworth arm) | 0.28 (0.10–0.45) | 0.55 (0.06) | 0.00 | 0.00 | 1.00 | 0.1559 |
| Effect of rehabilitation (Ashworth leg) | 0.10 (−0.02–0.22) | 0.38 (0.04) | 0.00 | 0.00 | 0.00 | 0.7903 |
| Exam III | Obesity | p | ||||
| N=30 | ||||||
| Mean (95% Cl) | SD (SE) | Q1 | Me | Q3 | ||
| Effect of rehabilitation (Barthel) | 14.44 (10.36–18–53) | 10.32 (1.03) | 5.00 | 15.00 | 20.00 | 0.9598 |
| Effect of rehabilitation (Ashworth hand) | 0.26 (−0.02–0.54) | 0.71 (0.07) | 0.00 | 0.00 | 1.00 | 0.6723 |
| Effect of rehabilitation (Ashworth arm) | 0.04 (−0.10–0.17) | 0.34 (0.03) | 0.00 | 0.00 | 0.00 | 0.1559 |
| Effect of rehabilitation (Ashworth leg) | 0.04 (−0.10–0.17) | 0.34 (0.03) | 0.00 | 0.00 | 0.00 | 0.7903 |
BMI – body mass index; N – number of subjects; CI – confidence interval; SD – standard deviation; SE – standard error; Max – maximum value; Me – median; Min – minimum value, Q1 – quartile I, Q3 – quartile III; test Kruskal-Wallis.
Discussion
Rehabilitation administered to patients with circulatory system diseases is to a large extent similar to rehabilitation applied for stroke patients. Many researchers report that comprehensive rehabilitation leads to a 20–25% decrease in the rates of mortality due to cardiovascular and other problems. Rehabilitation also improves physical capacities in overweight and obese patients, reducing the risk of atherosclerosis and ultimately leading to improved quality of life [19].
The likelihood of stroke is 22% higher in overweight people and 64% higher in obese individuals, compared to populations with normal BMI [20]. An increase in this index by only 1 kg/m2 leads to a 4% greater risk of ischemic stroke and a 6% higher risk of hemorrhagic stroke [21]. Following stroke, patients with normal BMI were able to recover their functional efficiency more quickly than obese patients. Furthermore, numerous studies have established that obesity exacerbates the risk of secondary stroke [13,22]. The present study shows that rehabilitation was more effective in patients with normal body mass. The patients with excessive weight and with obesity presented lower gains and these did not differ significantly between the 2 groups. It was also observed that the effects of rehabilitation, achieved by the patients during their stay in the Clinic, were retained for 3 months after discharge from the hospital. These conclusions are consistent with the findings reported by Burke et al., who showed that following stroke, subjects with normal weight presented greater gains from rehabilitation than did overweight and obese patients [13]. Similar effects of excessive weight and obesity were described by Flega et al. Following stroke, patients with BMI >35kg/m2 presented greater risk of suffering another stroke and death [23]. Research conducted at Harvard involving 19 000 subjects also showed that in stroke patients, overweight and obesity were related to greater mortality risk in female patients [24,25]. A study conducted by Heymsfield et al. involving a professional group of nurses, as well as a study by Brown et al. conducted in a group of medical professionals, showed that an increase in BMI coincides with greater risk of another incident of both hemorrhagic and ischemic stroke, and the risk of hemorrhagic stroke increased by 2.25 [26,27].
A study by Andsey et al. conducted in Sweden and involving healthy male subjects aged 47–55 years was continued for 28 years. A total of 7402 subjects were examined and the findings showed that coinciding with growing BMI >30 kg/m2, the risk of ischemic stroke increased by 1.78. On the other hand, no risk of hemorrhagic stroke was recorded [28]. Research conducted by Strazzullo et al. showed that overweight and obesity exacerbate the risk of ischemic stroke, and reported that the risk is unrelated to age, lifestyle, or risk factors for cardiovascular diseases [6].
The effectiveness of rehabilitation is also confirmed by other studies focusing on patients with cardiovascular problems. They investigated exercise tolerance and fatigue, irrespective of the subjects’ sex and body mass, measured with BMI. Based on their, findings it was established that it is more difficult for the bodies of obese patients to adapt to surgical treatment; therefore, recovery and rehabilitation take longer compared to subjects with normal BMI [29].
The present study shows that comprehensive stroke rehabilitation produces a positive effect of normalization of BMI, which is expected to result in long-term reduced risk of cardiovascular diseases, including stroke.
Conclusions
Hospital-based rehabilitation produced greater functional efficiency in the subjects with normal body weight, as well as normalization of BMI. The positive effects of rehabilitation, assessed with the Barthel index and Ashworth scale, was retained for 3 months (Exam III), which may result in reduced risk of cardiovascular diseases and complications such as stroke.
Footnotes
Source of support: Departmental sources
Conflicts of interest
None.
References
- 1.Vafadar AK, Côté JN, Archambault PS. Effectiveness of functional electrical stimulation in improving clinical outcomes in the upper arm following stroke: A systematic review and meta-analysis. Biomed Res Int. 2015;2015 doi: 10.1155/2015/729768. 729768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kitajewska W, Szeląg W, Kopański Z, et al. Civilisation diseases and prevention. J Public Health Nurs Med Rescue. 2014;1:3–7. [Google Scholar]
- 3.Drużbicki M, Przysada G, Guzik A, et al. The efficacy of gait training using a body weight support treadmill and visual biofeedback in patients with subacute stroke: A randomized controlled trial. Biomed Res Int. 2018;2018 doi: 10.1155/2018/3812602. 3812602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mao YR, Lo WL, Lin Q, et al. The effect of body weight support treadmill training on gait recovery, proximal lower limb motor pattern, and balance in patients with subacute stroke. Biomed Res Int. 2015;2015 doi: 10.1155/2015/175719. 175719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knyszewski K, Czapiewska M, Kaźmierczak K, Lebiedzińska A. The impact of modern man lifestyle to the development of cardiovascular disease. Bromat Chem Toksykol. 2016;2:107–13. [Google Scholar]
- 6.Strazzullo P, D’Elia L, Cairella G, et al. Excess body weight and incidence of stroke: Meta-analysis of prospective studies with 2 million participants. Stroke. 2010;5:418–26. doi: 10.1161/STROKEAHA.109.576967. [DOI] [PubMed] [Google Scholar]
- 7.Szpunar P, Mańdziuk M, Kaszuba B, et al. Knowledge of office workers on strike – preliminary. Pol Prz Nauk Zdr. 2017;2:199–206. [Google Scholar]
- 8.Kachur S, Lavie CJ, de Schutter A, et al. Obesity and cardiovascular diseases. Minerva Med. 2017;108:212–28. doi: 10.23736/S0026-4806.17.05022-4. [DOI] [PubMed] [Google Scholar]
- 9.Oesch L, Tatlisumak T, Arnold M, Sarikaya H. Obesity paradox in stroke – Myth or reality? A systematic review. PLoS One. 2017;3:e0171334. doi: 10.1371/journal.pone.0171334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sánchez-Iñigo L, Navarro-González D, Fernández-Montero A, et al. Risk of incident ischemic stroke according to the metabolic health and obesity states in the Vascular-Metabolic CUN cohort. Int J Stroke. 2017;12:187–91. doi: 10.1177/1747493016672083. [DOI] [PubMed] [Google Scholar]
- 11.Masters RK, Reither EN, Powers DA, et al. The impact of obesity on US mortality levels: The importance of age and cohort factors in population estimates. Am J Public Health. 2013;103:1895–901. doi: 10.2105/AJPH.2013.301379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wohlfahrt P, Lopez-Jimenez F, Krajcoviechova, et al. The obesity paradox and survivors of ischemic stroke. J Stroke Cerebrovasc Dis. 2015;24:1443–50. doi: 10.1016/j.jstrokecerebrovasdis.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 13.Burke DT, Al-Adawi S, Bell RB, et al. Effect of body mass index on stroke rehabilitation. Arch Phys Med Rehabil. 2014;95:1055–59. doi: 10.1016/j.apmr.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 14.Nishioka S, Wakabayashi H, Yoshida T, et al. Obese Japanese patients with stroke have higher functional recovery in convalescent rehabilitation wards: A retrospective cohort study. J Stroke Cerebrovasc Dis. 2016;25:26–33. doi: 10.1016/j.jstrokecerebrovasdis.2015.08.029. [DOI] [PubMed] [Google Scholar]
- 15.Chernenko A, Meeks H, Smith KR. Examining validity of body mass index calculated using height and weight data from the US driver license. BMC Public Health. 2019;19:100. doi: 10.1186/s12889-019-6391-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee YC, Chen SS, Koh CL, et al. Development of two Barthel Index-based Supplementary Scales for patients with stroke. PLoS One. 2014;9:e110494. doi: 10.1371/journal.pone.0110494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hong I, Lim Y, Han HS, et al. Application of the Korean version of the Modified Barthel Index: Development of a key form for use in clinical practice. Hong Kong J Occup. 2017;29:39–46. doi: 10.1016/j.hkjot.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pop T, Podgórska J, Przysada G, et al. Analysis of factors and correlation of scales used to evaluate the results of rehabilitation in stroke survivors. In: Madarász Š, Hudáková Z, Pop T, editors. Mechanisms and new markers of occurrence and course of the cerebral circulation disorders and robot-assisted rehabilitation after stroke. Bratislava: STATIS; 2014. pp. 143–54. [Google Scholar]
- 19.Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2016;29:2315–81. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kleinrok A, Głowa B. The obesity and its meaning in cardiovascular diseases Part 1. Obesity as a risk factor. Med Rev. 2015;13:165–72. [Google Scholar]
- 21.Jabłońska R, Sadowska M, Królikowska A, et al. Functional capacity and risk factors and sociodemographic variables of patients after ischemic stroke. Med Health Sci Rev. 2016;2:65–72. [Google Scholar]
- 22.Andersen KK, Olsen TS. Body Mass Index and Stroke: Overweight and obesity less often associated with stroke recurrence. J Stroke Cerebrovasc Dis. 2013;22:e576–81. doi: 10.1016/j.jstrokecerebrovasdis.2013.06.031. [DOI] [PubMed] [Google Scholar]
- 23.Flega KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–97. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 24.Romero-Corral A, Montori VM, Somers VK, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies. Lancet. 2006;368:666–78. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- 25.Azimi A, Charlot MG, Torp-Pedersen C, et al. Moderate overweight is beneficial and severe obesity detrimental for patients with documented atherosclerotic heart disease. Heart. 2013;99:655–60. doi: 10.1136/heartjnl-2012-303066. [DOI] [PubMed] [Google Scholar]
- 26.Heymsfield SB, Cefalu WT. Does body mass index adequately convey a patient’s mortality risk? JAMA. 2013;309:87–88. doi: 10.1001/jama.2012.185445. [DOI] [PubMed] [Google Scholar]
- 27.Brown CV, Neville AL, Rhee P, et al. The impact of obesity on the outcomes of 1,153 critically injured blunt trauma patients. J Trauma. 2005;59:1048–51. doi: 10.1097/01.ta.0000189047.65630.c5. [DOI] [PubMed] [Google Scholar]
- 28.Anstey KJ, Cherbuin N, Budge M, Young J. Body mass index in midlife and late-life as a risk factor for dementia: A meta-analysis of prospective studies. Obes Rev. 2011;12:426–37. doi: 10.1111/j.1467-789X.2010.00825.x. [DOI] [PubMed] [Google Scholar]
- 29.Przysada G, Smerecka D, Rykała J, et al. Analysis of exercise tolerance and fatigue evaluation in patients after coronary artery bypass grafting undergoing cardiac rehabilitation. Med Rev. 2014;12:141–51. [Google Scholar]