Abstract
Background
The aim of this study was to investigate the effect of active shoulder exercise with a sling suspension system on shoulder subluxation, proprioception, and upper extremity function in patients with acute stroke.
Material/Methods
Thirty-six patients with acute stroke and shoulder subluxation were randomly assigned into two groups. The study group (n=18) received active shoulder exercise with a sling suspension system, and the control group (n=18) received bilateral arm training for 40 minutes, for five days a week, for four weeks. The outcome measures before and after the intervention included measurement of shoulder subluxation distance, shoulder proprioception, the Fugl-Meyer assessment (FMA) scale, and the manual function test (MFT).
Results
Comparison of the study group with the control group showed significant differences in all outcome scores post-intervention (p<0.05). The study group had significant improvement in shoulder subluxation distance, shoulder proprioception, the FMA score, and the MFT compared with the control group. There was a significant difference in shoulder subluxation (p=0.001), shoulder proprioception (p=0.046), the FMA score (p=0.002), and the MFT (p=0.007) between the two groups, which favored the study group.
Conclusions
Active shoulder exercise with a sling suspension system may be effective in reducing shoulder subluxation, improving proprioception, and upper extremity function in patients following acute stroke.
MeSH Keywords: Proprioception, Shoulder Dislocation, Stroke
Background
Shoulder subluxation is a frequent complication of post-stroke hemiplegia [1]. The incidence of shoulder subluxation in patients following a stroke varies from 7–81%, and 73% occur in the acute stage [2]. In a 10-month follow-up study, shoulder subluxation was shown to be further aggravated in 67% of patients over time [3]. Shoulder subluxation in patients with hemiplegia increases the distance between the acromion and the humeral head, which may delay the recovery of upper extremity function and may reduce proprioception [1,4]. Shoulder subluxation can cause adhesive capsulitis which can cause shoulder pain that increases over time [5]. Therefore, active management and rehabilitation of shoulder subluxation to recover upper extremity function in patients with acute stroke should begin immediately after the onset of stroke [6,7].
Previous studies attempted to reduce shoulder subluxation in patients with hemiplegia and have reported the use of shoulder subluxation therapy with an arm sling [8], electrical stimulation therapy [9], upper limb taping [10], and the use of robot-assisted upper limb rehabilitation [11]. However, the use of an arm sling can result in difficulty in walking due to the limitation of symmetrical movement of both arms while walking, and prevention of normal sensory input due to a fixed shoulder joint and increased flexor synergy [7,12]. The use of taping can cause trauma to the skin at the sites where the skin is attached [1]. Robot-assisted therapy is not universally used due to problems caused by installation and the unclear effects on upper limb function. Therefore, general rehabilitation treatment should be performed concurrently with any assisted rehabilitation methods [13].
Recently, a sling suspension-based exercise method has been used that can compensate for gravity by hanging part of the body on a string or to minimize resistance to movement by reducing friction on contact with the floor [14]. Because the upper limb of the stroke patient is more sensitive to gravity than the lower extremity, sling suspension can induce selective active muscle contraction in the muscles around the shoulder joint by adjusting the gravity applied to the upper limb [13]. Fill et al. [15] reported that muscle strengthening through the active contraction of the muscles around the shoulder joint is crucial for reducing shoulder subluxation.
However, few studies have investigated active exercises for the muscles around the shoulder joint in hemiplegic patients following acute stroke. Also, no exercise program can induce active muscle contraction at the initial stage, although shoulder subluxation usually occurs at this stage. Therefore, the purpose of this study was to investigate the effect of active shoulder exercise using a sling suspension system on shoulder subluxation, shoulder proprioception, and upper extremity function in patients with acute stroke.
Material and Methods
Study participants
The study included 36 post-stroke patients admitted to a university hospital in the Republic of Korea. The study inclusion criteria were a stroke within less than four weeks before the study, and a diagnosis based on the World Health Organization (WHO) guidelines and confirmed by clinical examination and magnetic resonance imaging (MRI), and shoulder subluxation of 9.5 mm or more [16]. Study inclusion criteria also required adequate cognitive function to participate in the training, as determined by the Mini-Mental State Examination (MMSE) score (range, 0–30) with a score of 24 or more, and shoulder flexor and abductor manual function test (MFT) score between fair to poor and no excessive spasticity, as defined by a modified Ashworth Scale score of 2 or more.
The study exclusion criteria were any accompanying diseases or disorders, other than stroke, that could interfere with upper extremity training, and uncontrolled health conditions for which exercise was contraindicated. The study was approved by the Wonkwang University Hospital Institutional Review Board (IRB No. WKUH 201510-HR-094) and was conducted following the criteria established by the Helsinki Declaration.
Study design
This study used a single-blind, randomized and controlled design. The 36 study participants were randomly assigned to a study group (n=18) and a control group (n=18). The randomization method was performed using closed, sealed envelopes for each study participant that contained the group assignment, and the assessor was blinded to the patient group assignments. All participants were informed of how their test results would be used, and they signed written informed consent to participate in the study
All study participant underwent general physical therapy and occupational therapy. Active shoulder exercise using the sling suspension system was performed by the study group (n=18) and bilateral arm training was performed by the control group (n=18), for 40 minutes, for five days a week, and for four weeks. The sling suspension system used in this study was a Redcord™ sling exercise therapy device (Redcord AS, Staubo, Norway).
The sling suspension exercise program (study group)
The sling suspension exercise program is a method designed to strengthen muscles around the shoulder joint [17,18]. First, horizontal a shoulder abduction-adduction exercise was performed in the sitting position with the elbow in full extension. Second, an internal-external shoulder rotation exercise was performed in the sitting position with the elbow flexed at 90°. Third, the shoulder flexion-extension exercise was performed while positioned on the side with the elbow in full extension. Fourth, the shoulder abduction-adduction exercise was performed in the supine position with full elbow extension. The exercises were performed in the active range of motion. The position of the hanging point and the sandbag (weight, 1–3 kg) determined the intensity of the exercise.
The bilateral arm training program (control group)
The bilateral arm training program consisted of four components [18,19]. All the exercises were performed with both hands clasped together. First, a shoulder flexion-extension exercise was performed in the sitting position. Second, an elbow joint flexion-extension exercise was performed with 90º shoulder joint flexion. Third, a forward-reaching exercise was performed in the supine position. Fourth, a pull into the body was performed at 90° shoulder joint flexion and 180° elbow joint extension. A sandbag (weight, 1–3 kg) was used to determine exercise intensity.
In the exercise programs, each set of exercises was performed 20 times, and a total of five sets of exercises were included in each session. A physiotherapist with five or more years of experience was present to monitor the exact method of exercise, number of exercises, and the physical status of each patient (Figure 1).
Figure 1.
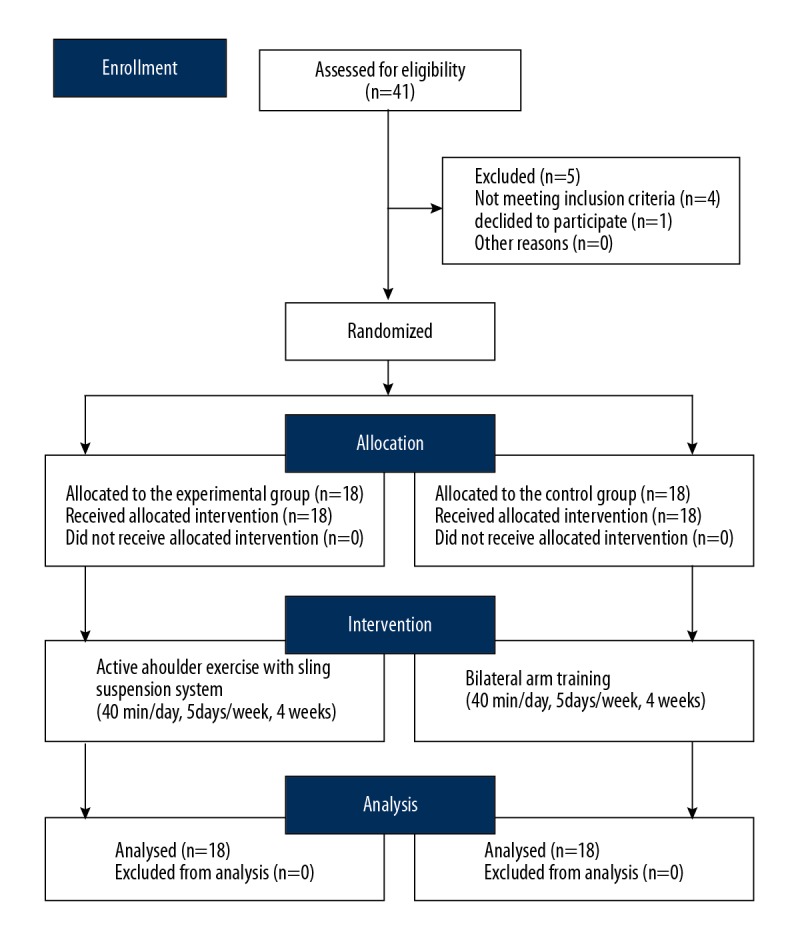
Flowchart of the study design.
Outcome measures
The shoulder subluxation distance was evaluated using an L-shaped thermoplastic rod (or jig) containing an embedded tape measure that was able to move [20]. The rod was placed on the acromion, and the end of the movement was measured at a point drawn by a pen to allow the length of movement to be measured. Subsequently, the degree of subluxation was re-measured to compare the difference between pre-exercise and post-exercise shoulder subluxation. This method of measurement was chosen due to its reliability, reproducibility, and accuracy [20].
The assessment of shoulder proprioception was performed using a repositioning test of shoulder flexion position sense, using five specified angles (30°, 60°, 90 °, 120°, 150°), determined using boards. The patients underwent measurements of shoulder joint flexion through the paralyzed upper limb by hanging the limb from the sling in while on their side in a lying position. The paralyzed shoulder joint was manually positioned twice at each angle to allow recognition of the position at each angle. The study participants performed two repositioning tests in random order from each angle with their eyes closed. The error angle was measured and the mean value was calculated and recorded [21].
The Fugl-Meyer assessment (FMA) tool was used for quantitative assessment of the functional recovery of the hemiplegic stroke patients. This tool assessed motor function, sensory function, balance, the range of motion, and joint pain, and was divided into 66 points for evaluation of the upper extremity. Examination of the upper extremity only was performed and the shoulder, wrist joint, hand reflex, voluntary movement, and coordination were examined. The Fugl-Meyer assessment method was chosen because of its high reliability, reproducibility, and validity [22].
The manual function test (MFT) is a rapid method of measuring upper limb function and movement ability in patients with stroke. One point was recorded for each item performed, and zero points were given when performance was impossible, with the highest total number of points being 32 [23].
Statistical analysis
All data were analyzed using SPSS Win version 22.0. The baseline characteristics of the subjects were analyzed using descriptive statistics. Pearson’s chi-squared (χ2) test and the Mann-Whitney U test were performed to determine the differences between the study and control groups. The Shapiro-Wilk test was used to assess the normality of data distribution. Data were presented as mean and standard deviation (SD). Within-group differences from pre-test to post-test measurements were evaluated using paired t-tests. Between-group differences at the time points of measurement and mean score changes were evaluated using independent t-tests. A p-value <0.05 was considered to be statistically significant.
Results
There were no significant differences in the affected side, type of lesion, and age between the study group and the control group (Table 1) (p>0.05). Table 2 shows the results of the study group and the control group that were recorded pre-treatment and post-treatment. Baseline findings showed no significant differences between the two groups. Patients in the study group significantly improved compared with the control group for all outcome measures.
Table 1.
Pre-treatment baseline characteristics of the study group (n=18) and the control group (n=18).
| Variable | Pre-treatment | P-value | |
|---|---|---|---|
| Study group (n=18) | Control group (n=18) | ||
| Gender (Male/Female) | 10/8 | 9/9 | 0.94 |
| Affected side (left/right) | 7/11 | 10/8 | 0.88 |
| Type of stroke (ischemic/hemorrhagic) | 10/8 | 9/9 | 0.94 |
| Age, mean years ±SD | 60.30±7.56 | 57.18±8.41 | 0.37 |
| Onset duration, mean days ±SD | 18.60±5.76 | 20.10±4.84 | 0.54 |
| *MMSE ±SD | 25.86±2.77 | 26.48±1.67 | 0.75 |
Values are presented as the mean ± standard deviation (SD). MMSE – Mini-Mental State Examination.
Range of scores, from 0–30.
Table 2.
Comparison of shoulder function within the study and control groups and between the study and control groups.
| Variables | Study group (n=18) | Control group (n=18) | Between-group P-values (95% CI) | Mean change | |||
|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | Study group | Control group | ||
| SSD (mm) | 10.86±0.64a | 6.21±1.64*# | 10.88±0.9 | 8.81±1.44* | 0.001 (−3.635–1.542) | 4.71±1.72# | 2.86±2.16 |
| SP (degree) | 15.33±3.95 | 11.5±3.33*# | 14.01±3.49 | 12.44±3.39* | 0.046 (−3.224–1.335) | 3.83±1.72# | 1.56±0.61 |
| FMA (scores) | 7.28±4.02 | 19.5±8.43*# | 6.67±5.32 | 10.5±7.77* | 0.002 (3.505–14.495) | 12.22±6.31# | 3.83±2.87 |
| MFT (scores) | 4.01±1.87 | 10.39±4.04*# | 3.83±3.24 | 6.22±4.61* | 0.007 (1.229–7.104) | 6.39±3.05# | 2.39±1.50 |
Mean ± standard deviation (SD).
Significance of the difference within groups;
significance of the difference between groups.
Pre-test was performed before the intervention, and post-test was performed after four weeks. In the pre-test comparison between the study and control groups, there was no significant difference (P>0.05). The significance level was set at P<0.05 for differences between the two groups. CI – confidence interval; SSD – shoulder subluxation distance; SP – shoulder proprioception; FMA – Fugl-Meyer assessment; MFT – manual function test.
The change in distance measured in shoulder subluxation was significantly greater in the study group than in the control group (4.71±1.72 vs. 2.86±2.16 mm; p=0.008). The change in the degree of shoulder proprioception measured by the assessment board was significantly greater in the study group compared with the control group (3.83°±1.72° vs. 1.56°±0.61°; p=0.006). The change in the score for the upper extremity manual function measured by the Fugl-Meyer assessment (FMA) tool was significantly greater in the study group compared with the control group (12.22±6.31 vs. 3.83±2.87 points; p=0.002). The change in the score for upper extremity function measured by the manual function test (MFT) was significantly greater in the study group than in the control group (6.39±3.05 vs. 2.39±1.50 points; p=0.004) (Table 2).
Discussion
This study was conducted to investigate the effects of active shoulder exercise using a sling suspension system on shoulder subluxation, shoulder proprioception, and upper extremity function in patients with shoulder subluxation following acute stroke. The results showed that in the study group, active shoulder exercise with the sling suspension system resulted in significant improvement when compared with the control group in which patients underwent bilateral arm training, in terms of shoulder subluxation distance, shoulder proprioception, the Fugl-Meyer assessment (FMA), and the manual function test (MFT).
In the active shoulder exercise with sling suspension system protocol, when the paralyzed upper limb with subluxation was hung on the sling suspension system, the influence of gravity on the upper limb was minimized. This protocol allowed the patients to facilitate selective movements of the muscles involved in stabilization of the shoulder joint [14]. Also, this suspension system allowed intensive training of the upper extremity of the affected side and reduced the occurrence of involuntary flexor synergy that can interfere with upper limb movements [24]. Previous studies have shown that active muscle contraction of the shoulder joint is the most important method for reducing shoulder subluxation [15]. However, no previous studies have been undertaken on the use of active shoulder joint exercises in the acute stage within four weeks following stroke although subluxation is most likely to occur at this stage.
Kim et al. [25] reported that 25 patients with hemiplegia with shoulder subluxation in their study group showed significantly reduced subluxation as a result of applying shoulder joint isometric contraction with a sling suspension system to the upper extremities when compared with a control group. Fil et al. [15] reported that 48 patients with acute stroke with subluxation of less than 9.5 mm underwent selective muscle strengthening exercises of the rotator cuff and the deltoid muscle by correct alignment of the shoulder complex, resulting in decreased subluxation in the study group. The results of these previous studies support the findings of the present study, which included patients in the acute stage following stroke with the aim to reduce subluxation assisted by gravitational compensation to promote selective movement of the shoulder joint.
The possible mechanisms responsible for reducing the shoulder subluxation distance in patients with acute stroke after a short period of training may be identified from previously published studies [15,24,26]. Although the therapeutic intervention method is also important for the reduction of subluxation in patients with stroke, the timing of treatment initiation is a more important factor [26]. Patients in the acute stage of stroke, of less than one month in duration, showed clinically significant differences between the study group and the control group including in shoulder subluxation distance because the upper limb weight was supported by the sling suspension system, gravity was compensated for, and the flexor synergy was reduced. Using active shoulder exercise with a sling suspension system, selective muscle strengthening occurred following exercise of the muscles involved in the stabilization of the shoulder joint.
Participants in the active shoulder exercise with sling suspension system showed significantly improved shoulder proprioception, as measured by the repositioning error test, compared with the control group in which patients underwent bilateral arm training. Movement disorders due to the instability of the shoulder joint in patients with stroke lead to reduced shoulder position sense and abnormal movement patterns [21]. A vicious cycle occurs in which the position sense is further decreased when the range of motion is limited and contractures increase over time [27]. Position sense is strongly promoted by activation of the muscle spindle and Golgi organelles in cells of the joint tendons, and muscle spindles cause the activation of position sense and kinesthetic sensation [28]. In patients with stroke, there is a correlation between the degree of restoration of upper extremity function and the sense of joint position, associated with muscle spindles [28]. Shoulder position sense is important for shoulder joint stability [29]. The findings of the present study suggested that sensory information generated by muscles, joints, and skin during active shoulder exercise with a sling suspension system was projected and integrated into the brain to increase position sense.
The study group that underwent active shoulder exercise with the sling suspension system showed significant improvement in upper extremity function compared with the control group in which patients underwent bilateral arm training. Paci et al. [30] reported a direct correlation between shoulder joint subluxation and upper extremity function. Jonsson et al. [31] reported a significant improvement in shoulder function scores in ten patients with shoulder joint instability due to shoulder joint impingement syndrome after undergoing 12 weeks of sling therapy exercise. According to Zorowitz [32], upper extremity function improves with decreasing shoulder subluxation distance. These findings suggest that active shoulder joint exercise with a sling suspension system may be more helpful in improving shoulder subluxation distance, shoulder proprioception, and upper extremity function patients with acute stroke with shoulder subluxation compared with bilateral arm training.
However, this study had several limitations. The study included a small study population from a single center, which limits the interpretation of the findings. Therefore, the results of the present study should be verified by additional studies with larger sample sizes. Persistent long-term effects were not evaluated because there were was no follow-up after the four-week therapeutic intervention was completed. Long-term follow-up studies should be conducted to confirm the effect of active shoulder joint exercises with the sling suspension system. Also, further studies should be performed to compare the baseline data of the control group without upper limb movement because bilateral upper extremity exercises in the control group led to active assisted movement of the shoulder joint in the paralyzed arm.
Conclusions
There is no exercise program that can induce active muscle contraction at the in the acute stage following stroke, although subluxation most commonly occurs in the acute stage. The findings of this study showed that active shoulder exercise with the sling suspension system reduced shoulder subluxation, and improved proprioception, and upper extremity function in patients with acute stroke with subluxation of the shoulder. Therefore, to reduce shoulder subluxation in patients with acute stroke, active rehabilitation treatment and management should commence immediately after the onset of stroke.
Footnotes
Source of support: Departmental sources
References
- 1.Paci M, Nannetti L, Rinaldi LA. Glenohumeral subluxation in hemiplegia: An overview. J Rehabil Res Dev. 2005;42:557–68. doi: 10.1682/jrrd.2004.08.0112. [DOI] [PubMed] [Google Scholar]
- 2.Hurd MM, Farrell KH, Waylonis GW. Shoulder sling for hemiplegia: Friend or foe? Arch Phys Med Rehabil. 1974;55:519–22. [PubMed] [Google Scholar]
- 3.Smith RG, Cruikshank JG, Dunbar S, et al. Malalignment of the shoulder after stroke. Br Med J. 1982;284:1224–26. doi: 10.1136/bmj.284.6324.1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ikai T, Tei K, Yoshida K, et al. Evaluation and treatment of shoulder subluxation in hemiplegia: relationship between subluxation and pain. Am J Phys Med Rehabil. 1998;77:421–26. doi: 10.1097/00002060-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Hanger HC, Whitewood P, Brown G, et al. A randomized controlled trial of strapping to prevent post-stroke shoulder pain. Clin Rehab. 2000;14:370–80. doi: 10.1191/0269215500cr339oa. [DOI] [PubMed] [Google Scholar]
- 6.Vafadar AK, Côté JN, Archambault PS. Effectiveness of functional electrical stimulation in improving clinical outcomes in the upper arm following stroke: A systematic review and meta-analysis. Biomed Res Int. 2015;2015 doi: 10.1155/2015/729768. 729768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang RY, Chan RC, Tsai MW. Functional electrical stimulation on chronic and acute hemiplegic shoulder subluxation. Am J Phys Med Rehab. 2000;79:385–90. doi: 10.1097/00002060-200007000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Stolzenberg D, Siu G, Cruz E. Current and future interventions for glenohumeral subluxation in hemiplegia secondary to stroke. Top Stroke Rehab. 2012;19:444–56. doi: 10.1310/tsr1905-444. [DOI] [PubMed] [Google Scholar]
- 9.Ada L, Foongchomcheay A. Efficacy of electrical stimulation in preventing or reducing subluxation of the shoulder after stroke: A meta-analysis. Aust J Physiother. 2002;48:257–67. doi: 10.1016/s0004-9514(14)60165-3. [DOI] [PubMed] [Google Scholar]
- 10.Chatterjee S, Hayner KA, Arumugam N, et al. The California tri-pull taping method in the treatment of shoulder subluxation after stroke: a randomized clinical trial. N Am J Med Sci. 2016;8:175–82. doi: 10.4103/1947-2714.179933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dohle CI, Rykman A, Chang J, et al. Pilot study of a robotic protocol to treat shoulder subluxation in patients with chronic stroke. J Neuroeng Rehabil. 2013;10:88. doi: 10.1186/1743-0003-10-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brooke MM, de Lateur BJ, Diana-Rigby GC, et al. Shoulder subluxation in hemiplegia: effects of three different supports. Arch Phys Med Rehabil. 1991;72:582–86. [PubMed] [Google Scholar]
- 13.Prange GB, Jannink MJ, Stienen AH, et al. Influence of gravity compensation on muscle activation patterns during different temporal phases of arm movements of stroke patients. Neurorehabil Neural Repair. 2009;23:478–85. doi: 10.1177/1545968308328720. [DOI] [PubMed] [Google Scholar]
- 14.Chen L, Chen J, Peng Q, et al. Effect of sling exercise training on balance in patients with stroke: A meta-analysis. PLoS One. 2016;11:e0163351. doi: 10.1371/journal.pone.0163351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fil A, Armutlu K, Atay AO, et al. The effect of electrical stimulation in combination with Bobath techniques in the prevention of shoulder subluxation in acute stroke patients. Clin Rehabil. 2011;25:51–59. doi: 10.1177/0269215510375919. [DOI] [PubMed] [Google Scholar]
- 16.Hall J, Dudgeon B, Guthrie M. Validity of clinical measures of shoulder subluxation in adults with poststroke hemiplegia. Am J Occup Ther. 1995;49:526–33. doi: 10.5014/ajot.49.6.526. [DOI] [PubMed] [Google Scholar]
- 17.Ekstrom RA, Donatelli RA, Soderberg GL. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2003;33:247–58. doi: 10.2519/jospt.2003.33.5.247. [DOI] [PubMed] [Google Scholar]
- 18.Reed D, Cathers I, Halaki M, et al. Does supraspinatus initiate shoulder abduction? J Electromyogr Kinesiol. 2013;23:425–29. doi: 10.1016/j.jelekin.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 19.Majsak MJ. Application of motor learning principles to the stroke population. Top Stroke Rehabil. 1996;3:37–59. doi: 10.1080/10749357.1996.11754113. [DOI] [PubMed] [Google Scholar]
- 20.Hayes KW, Sullivan JE. Reliability of a new device used to measure shoulder subluxation. Phys Ther. 1989;69:762–67. doi: 10.1093/ptj/69.9.762. [DOI] [PubMed] [Google Scholar]
- 21.Baek JH, Kim JW, Kim SY, et al. Acute effect of repeated passive motion exercise on shoulder position sense in patients with hemiplegia: A pilot study. Neurorehabilitation. 2009;25:101–6. doi: 10.3233/NRE-2009-0504. [DOI] [PubMed] [Google Scholar]
- 22.Gladstone DJ, Danells CJ, Black SE. The Fugl-Meyer assessment of motor recovery after stroke: A critical review of its measurement properties. Neurorehabil Neural Repair. 2002;16:232–40. doi: 10.1177/154596802401105171. [DOI] [PubMed] [Google Scholar]
- 23.Miyamoto S, Kondo T, Suzukamo Y, et al. Reliability and validity of the Manual Function Test in patients with stroke. Am J Phys Med Rehabil. 2009;88:247–55. doi: 10.1097/PHM.0b013e3181951133. [DOI] [PubMed] [Google Scholar]
- 24.Faul F, Erdfelder E, Lang A, et al. G*Power 3: A flexible statistical power analysis program for the social, behavior, and biomedical science. Behav Res Methods. 2007;39:175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 25.Kung PC, Lin CC, Ju MS. Neuro-rehabilitation robot-assisted assessments of synergy patterns of the forearm, elbow and shoulder joints in chronic stroke patients. Clin Biomech. 2010;25:647–54. doi: 10.1016/j.clinbiomech.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 26.Kim MK, Jung JM, Chang JS, et al. Radiographic imaging analysis after sling exercises for hemiplegic shoulder subluxation. J Phys Ther Sci. 2012;24:1099–101. [Google Scholar]
- 27.Lee JH, Baker LL, Johnson RE, et al. Effectiveness of neuromuscular electrical stimulation for management of shoulder subluxation post-stroke: A systematic review with meta-analysis. Clin Rehabil. 2017;31:1431–44. doi: 10.1177/0269215517700696. [DOI] [PubMed] [Google Scholar]
- 28.Niessen MH, Veeger DH, Koppe PA, et al. Proprioception of the shoulder after stroke. Arch Phys Med Rehabil. 2008;89:333–38. doi: 10.1016/j.apmr.2007.08.157. [DOI] [PubMed] [Google Scholar]
- 29.Niessen MH, Veeger DH, Meskers CG, et al. Relationship among shoulder proprioception, kinematics, and pain after stroke. Arch Phys Med Rehabil. 2009;90:1557–64. doi: 10.1016/j.apmr.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Paci M, Nannetti L, Taiti P, et al. Shoulder subluxation after stroke: Relationships with pain and motor recovery. Physiother Res Int. 2007;12:95–104. doi: 10.1002/pri.349. [DOI] [PubMed] [Google Scholar]
- 31.Jonsson P, Wahlström P, Ohberg L, et al. Eccentric training in chronic painful impingement syndrome of the shoulder: Results of a pilot study. Knee Surg Sports Traumatol Arthrosc. 2006;14:76–81. doi: 10.1007/s00167-004-0611-8. [DOI] [PubMed] [Google Scholar]
- 32.Zorowitz RD. Recovery patterns of shoulder subluxation after stroke: A six-month follow-up study. Top Stroke Rehabil. 2001;8:1–9. doi: 10.1310/LADU-8LJY-KTQ0-L5DJ. [DOI] [PubMed] [Google Scholar]


