Key Points
Question
What are the expected financial and reproductive health implications for the Veterans Affairs health care system of implementing a 12-month dispensing option for oral contraceptive pills?
Findings
In this economic decision model built from the Veterans Affairs health system payer perspective using a cohort of 24 309 women, adoption of a 12-month dispensing option for oral contraceptive pills is expected to produce substantial cost savings for the payer compared with standard 3-month dispensing, while reducing unintended pregnancies among women veterans.
Meaning
A 12-month dispensing option for oral contraceptive pills is economically feasible for the Veterans Affairs health system while better supporting women veterans’ reproductive goals and autonomy.
This economic decision model estimates the financial and reproductive health implications for implementation of a 12-month option for dispensing oral contraceptive pills in the Veterans Affairs health care system.
Abstract
Importance
The Veterans Affairs (VA) health care system is the largest integrated health care system in the United States. Like most US health plans, the VA currently stipulates a 3-month maximum dispensing limit for all medications, including oral contraceptive pills (OCPs). However, 12-month OCP dispensing has been shown to improve continuation of use, decrease coverage gaps, and reduce unintended pregnancy in other practice settings.
Objective
To estimate the financial and reproductive health implications for the VA of implementing a 12-month OCP dispensing option, with the goal of informing policy change.
Design, Setting, and Participants
A decision model from the VA payer perspective was developed to estimate incremental costs to the health care system of allowing the option to receive a 12-month supply of OCPs up front, compared with the standard 3-month maximum, during a 1-year time horizon. A model cohort of 24 309 reproductive-aged, heterosexually active, female VA enrollees who wish to avoid pregnancy for at least 1 year was assumed. Probabilities of continuation of OCP use, coverage gaps, pregnancy, and pregnancy outcomes were drawn from published data. Costs of OCP provision and pregnancy-related care and the number of women using OCPs were drawn from VA administrative data. One-way and probabilistic sensitivity analyses were performed to assess model robustness.
Main Outcomes and Measures
Incremental per-woman and total costs to the VA of allowing for 12-month dispensing of OCPs compared with standard 3-month dispensing.
Results
The 12-month OCP dispensing option, modeled from the VA health system perspective using a cohort of 24 309 women, resulted in anticipated VA annual cost savings of $87.12 per woman compared with the cost of 3-month dispensing, or an estimated total savings of $2 117 800 annually. Cost savings resulted from an absolute reduction of 24 unintended pregnancies per 1000 women per year with 12-month dispensing, or 583 unintended pregnancies averted annually. Expected cost savings with 12-month dispensing were sensitive to changes in the probability of OCP coverage gaps with 3-month dispensing, the probability of pregnancy during coverage gaps, and the proportion of pregnancies paid for by the VA. When simultaneously varying all variables across plausible ranges, the 12-month strategy was cost saving in 95.4% of model iterations.
Conclusions and Relevance
Adoption of a 12-month OCP dispensing option is expected to produce substantial cost savings for the VA while better supporting reproductive autonomy and reducing unintended pregnancy among women veterans.
Introduction
The Veterans Affairs (VA) health care system is the largest integrated health care system in the United States1 and provides care to a growing population of reproductive-aged women veterans, including provision of all contraceptive methods approved by the US Food and Drug Administration.2,3 Similar to within the general US population, oral contraceptive pills (OCPs) are among the most commonly used methods of contraception among women veterans.4 To be most effective at preventing pregnancy, OCPs require adherence to daily use, timely medication refills, and prescription renewals. Missing more than 2 consecutive pills can increase a woman’s chance of contraceptive failure and thus the potential for unintended pregnancy.5 The effects of this user dependence are evidenced by dramatic differences between perfect and typical use failure rates for OCPs (0.3% and 9.0% in the first year of use, respectively).6
Although OCP prescriptions can be written for a full year, pill pack quantity per fill is primarily determined by the patient’s insurance. In the United States, medication dispensing is typically limited to 30-, 60-, or 90-day supplies, as a mechanism to control costs.7,8 Three-month supplies are increasingly common among commercial and public insurers owing to associations with improved adherence and cost savings for patients and payers.9,10,11,12 Nevertheless, 90-day limits still necessitate multiple refills annually. Gaps in OCP coverage due to prescription refill delays are an established barrier to perfect contraceptive use among US women.13,14
Like most US health plans, the VA stipulates a 3-month dispensing limit for all prescription medications, including OCPs. However, VA data indicate that 43% of women dispensed 3-month contraceptive supplies experience at least 1 gap of at least 7 days between refills during the course of a year of use.15 Conversely, US women dispensed 12-month contraceptive supplies experience fewer gaps and improved method continuation compared with women receiving fewer pills up front,16,17,18 which in turn leads to reductions in unintended pregnancy and abortion.19 Citing this research, international and US guidelines now recommend routine initial dispensing of up to 1-year supplies of hormonal contraception.5,20
Despite mounting evidence favoring 12-month dispensing strategies for improving contraceptive access and reproductive outcomes, the financial consequences for the VA are unclear and will likely shape policy decisions. We used decision modeling to estimate financial and reproductive health implications to the VA of a revised policy allowing for 12-month dispensing of OCPs. Based on existing data, we hypothesized that 12-month dispensing would reduce VA costs while decreasing unintended pregnancies among women veterans.
Methods
Model Design and Cohort
The institutional review board of VA Pittsburgh Health Care System determined this study, which used retrospective administrative data, to be exempt from human subjects review. Additional approval was obtained from the VA Pharmacy Benefits Management Service to use administrative data. This study followed the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) reporting guideline for economic evaluation.
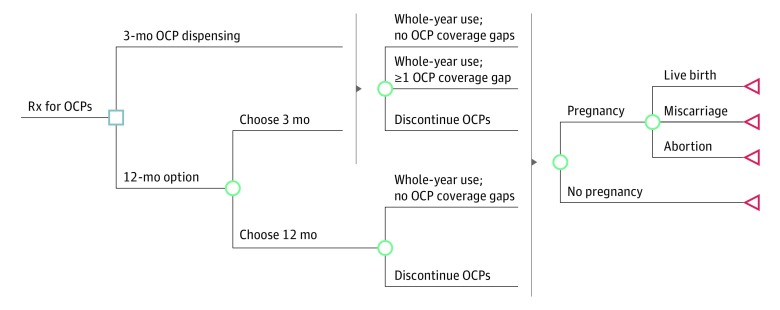
We developed a decision analysis model from the VA payer perspective to estimate incremental costs of a 12-month OCP supply option (twelve 28-day pill packs) compared with conventional 3-month dispensing (three 28-day packs dispensed 4 times). Figure 1 shows a simplified model schematic. The 12-month strategy is modeled as an option to account for personal preference (eg, trialing a new pill type) and because some VA enrollees are subject to copayments for contraceptive medications,21 which may disincentivize some women from accepting a 12-month supply. The model was run over a time horizon of twelve 28-day periods (approximately 1 year).
Figure 1. Decision Model Schematic.
Decision analysis model of 3- vs 12-month dispensing strategies for oral contraceptive pills (OCPs). Rx indicates prescription.
Our model assumes a cohort of reproductive-aged, heterosexually active female VA enrollees who wish to avoid pregnancy for at least 1 year. Pregnancy outcomes include abortion, miscarriage (pregnancy loss before gestational age of 20 weeks), and live birth. Stillbirths (fetal death after gestational age of 20 weeks) and ectopic pregnancies were excluded for model parsimony because these outcomes represent less than 2% of pregnancies, and because pregnancy outcome probabilities are not expected to differ between strategies.22,23 Model outcomes were per-woman mean costs for 3-month and 12-month dispensing, the incremental cost difference between strategies, and total incremental annual cost difference among all women using OCPs. A cohort of 24 309 women was used to calculate total annual costs, based on the number of VA enrollees who filled an OCP prescription during fiscal year 2017 (FY2017). Model construction and analyses were performed using TreeAge Pro 2018 and 2019, version R1 software (TreeAge Software). Independent coding of model components and review of model accuracy by two of us (C.P.J.-G. and K.J.S.) was used to reduce risk of model errors or programming bugs (internal validity).24
Key Assumptions
Base case analyses assume that 50% of OCP users opt to receive a 12-month supply of OCPs, and this value was varied from 0% to 100% in sensitivity analyses; cohorts choosing 12- vs 3-month supplies are assumed to be identical in demographic factors and unintended pregnancy risk. Based on a cohort wishing to avoid pregnancy for at least 1 year, all pregnancies in the model are unintended (ie, occurring sooner than desired or when no future pregnancies were desired, per standard definitions).25 This assumption informs the base case proportion of pregnancies that result in abortion (42%).26 Although empirical evidence indicates that continuation of OCP use is improved among women dispensed greater numbers of pills,15,16 discontinuation rates are equivalent between the 3- and 12-month strategies and treated as a single variable in the model, biasing against the 12-month strategy. The model assumes an equal probability of daily contraceptive adherence between 3- and 12-month cohorts (ie, if women have no gaps in pill coverage, they are equally likely to take them consistently). Typical use failure rates account for imperfect daily adherence.6 Finally, mean pregnancy risk is assumed to be constant over time, allowing for pregnancy risk prorating based on time covered by OCPs.
Model Variables
Model variables are listed in Table 1. Probabilities of contraceptive continuation, coverage gaps, pregnancy, and pregnancy outcomes were drawn from published literature.4,6,15,21,26,27,28,29,30 Our model does not allow for switching from OCPs to other prescription contraceptive methods during the 1-year time horizon. However, prior work indicates that prescription contraceptive method switching is low among VA enrollees using hormonal contraception (4.8% switched to another short-acting method during 1 year)15 and among non-VA women using OCPs (mean of 0.11 OCP cycles wasted annually owing to method switching).19 Women discontinuing use of OCPs are assumed to use nonprescription methods or no method for the remainder of the time horizon. The base case pregnancy risk among those who discontinue OCP use is a weighted mean of annual typical use failure rates for condoms, withdrawal, fertility awareness methods, spermicides, and no contraceptive use, based on the distribution of use of these methods among a nationally representative sample of women veterans who use the VA for primary care.4,6 Women with gaps between OCP refills are assumed to use no contraception during gaps, with an 85% annual pregnancy risk.6 Pregnancy probabilities are prorated based on OCP coverage time vs gap or discontinuation. All annual pregnancy probabilities were additionally prorated to account for a model time horizon of twelve 28-day cycles (336 days) rather than 365 days.
Table 1. Variables for Base Case and Sensitivity Analyses.
| Variable | Base Case | One-way Sensitivity Analysisa | Probabilistic Sensitivity Analysisb | Source | |||
|---|---|---|---|---|---|---|---|
| Low Value | High Value | SD | Distribution | ||||
| Costs | |||||||
| Intermediate costs, 2017 US $c | |||||||
| 3-mo OCP supply | 38.48 | 0.01 | 5000.00 | 100.68 | Gamma | VA data | |
| Dispensing for 3-mo OCP supply | 8.58 | 0.01 | 110.00 | 6.70 | Gamma | VA data | |
| Copayment for 3-mo OCP supply | −24.00 | NA | NA | NA | NA | US Department of VA,21 2018 | |
| Outcome costs, $ | |||||||
| Live birth | |||||||
| Prenatal cared | 2968.79 | 100.00 | 15 000.00 | 3789.39 | Gamma | National Partnership for Women and Families27 2013 | |
| Intrapartum/delivery care | 7933.67 | 1000.00 | 100 000.00 | 6827.42 | Gamma | VA data | |
| Newborn care (7 d) | 6480.85 | 300.00 | 100 000.00 | 6000.00 | Gamma | VA data | |
| Miscarriage | 1186.41 | 100.00 | 5000.00 | 1452.71 | Gamma | VA data | |
| Abortion | 0 | NA | NA | NA | NA | US Department of VA28 | |
| Probabilities | |||||||
| Choose 12-mo supply | 0.50 | 0 | 1.00 | 0.20 | Beta | Assumption | |
| Have copayments for OCPs | 0.35 | 0 | 1.00 | 0.10 | Beta | VA data | |
| OCP use probabilities | |||||||
| Discontinue OCP use given 3 or 12 mo | 0.35 | 0 | 0.07 | 0.10 | Beta | Borrero et al,152013; assumption | |
| ≥1 gap in coverage given 3 mo | 0.43 | 0 | 0.70 | 0.15 | Beta | Borrero et al,15 2013 | |
| Annual pregnancy probabilitiese | |||||||
| Pregnancy given continuous OCP use | 0.09 | 0 | 0.20 | 0.05 | Beta | Trussell,6 2011 | |
| Pregnancy given discontinued OCPsf | 0.47 | 0 | 1.00 | 0.15 | Beta | Borrero et al,4 2017; Trussell,6 2011 | |
| Pregnancy during OCP coverage gap(s) | 0.85 | 0 | 1.00 | 0.08 | Beta | Trussell,6 2011; assumption | |
| Pregnancy outcome probabilities | |||||||
| Miscarriage | 0.10 | 0 | 0.40 | 0.07 | Beta | American College of Obstetricians and Gynecologists,29 2018 | |
| Abortion | 0.42 | 0 | 0.70 | 0.05 | Beta | Finer and Zolna,26 2016 | |
| Live birth | 0.48 | NA | NA | NA | NA | NA | |
| Pregnancy paid for by VA | 0.52 | 0 | 1.00 | 0.20 | Beta | Borrero et al,4 2017; assumption | |
| Newborn care paid for by VAg | 0.58 | 0 | 1.00 | 0.20 | Beta | VA data | |
| Durations | |||||||
| OCP use given ≥1 coverage gap, mo | 10 | 3 | 11.75h | 1.00 | Beta | Borrero et al,15 2013 | |
| OCP use given discontinuation of OCPs, mo | 8 | 0 | 12.00 | 1.5.0 | Beta | Borrero et al,15 2013 | |
Abbreviations: NA, not applicable; OCP, oral contraceptive pill; VA, Veterans Affairs.
Cost ranges for 1-way sensitivity analysis are based on extremes of empirical VA data. All other ranges are based on published literature and are intentionally broad to reflect parameter uncertainty and allow for extreme value analysis.30
Distribution means are equal to the base case. Distributions were chosen based on established best practices.30
Intermediate costs are scaled directly based on the minimum number of 3-month supplies necessary to account for time covered by OCPs or multiplied by 4 for 12-month supplies.
Prenatal care costs are based on mean costs paid by commercial insurers for prenatal care in 2010 ($2641), adjusted to 2017 US dollars.
Based on 1 full year of use and prorated in the model to account for the proportion of time in a given state (covered by OCPs, OCP use gap, or discontinuation of OCP use), and for a time horizon of twelve 28-day periods (336 days) instead of a full calendar year.
The base case probability is a weighted mean of annual typical use failure rates for nonprescription contraceptive methods (male condoms, withdrawal, fertility awareness–based methods, and spermicides) and no method use, based on the distribution of current use of these methods observed among women veterans at risk for unintended pregnancy in the Examining Contraceptive Use and Unmet Need Among Women Veterans (ECUUN) study.4,6
Indicates the probability that newborn care is paid for by the VA among women whose pregnancy care is covered by the VA.
Indicates the maximum amount of time that can be covered by OCPs if a woman misses at least 7 days between refills in a time horizon of twelve 28-day time periods (336 days).
Costs were drawn from VA administrative data. Intermediate costs include the mean cost of pills (including fixed and variable supply costs and overhead) and mean dispensing costs (including labor and, for mail-order prescriptions, supplies and overhead) for each 3-month OCP supply; mean costs include prescriptions filled at pharmacy windows and via the VA’s mail-order pharmacy in FY2017. Intermediate costs were multiplied by 4 in 12-month dispensing arms and scaled in 3-month dispensing arms based on the minimum number of 3-month supplies required to account for mean OCP coverage time in that arm (eg, multiplied by 3 for discontinuers in the base case to account for a mean of 8 months of OCP coverage). Our assumption of direct scalability for pill and dispensing costs from 3- to 12-month supplies biases against the 12-month option, because dispensing of larger quantities may be associated with reduced per-unit costs and thus lower relative intermediate costs.
Veteran copayments represent negative intermediate costs (ie, profit) to the VA and were fixed in the model at −$24 per 3-month supply or −$96 for a 12-month supply, based on copayment rates for 2017.21 Copayments were scaled as above in 3-month arms based on OCP coverage time. Whether a veteran is subject to copayments for medications, including contraceptive methods, is based on a variety of factors, including income level, military service time frame, and service-connected disability level.21 The proportion of women subject to OCP copayments (34.5%) was determined using FY2017 administrative data. Copayment amounts were multiplied by the proportion of veterans with copayments.
Outcome costs include the mean costs incurred by the VA for live births and miscarriages. Abortion cost is set at $0, because the VA does not cover pregnancy termination under any circumstances.28 Live birth costs include prenatal care, intrapartum and delivery care, and newborn care, which the VA covers for a maximum of 7 days. The VA does not provide pregnancy or newborn care directly, but contracts with non-VA entities to reimburse this care using VA benefits.2 Costs of intrapartum care, newborn care, and miscarriage management represent VA mean payments in FY2015, the latest available data from which we could derive reliable estimates. All costs associated with prenatal care are drawn from mean costs paid by commercial insurers for prenatal care in 2010.27 All costs are presented in 2017 US dollars, with costs from prior years inflated using the US Consumer Price Index.
A proportion of VA enrollees use non-VA insurance benefits (eg, private insurance or Medicaid) to cover pregnancy care. Our base case of 52% of pregnancies paid for by VA was derived from unpublished data from the Examining Contraceptive Use and Unmet Need Among Women Veterans (ECUUN) study,4 where 52% of veterans currently receiving OCPs from the VA have no additional, non-VA insurance coverage. Administrative data indicate that the VA paid for newborn care for approximately 58% of infants born to women whose maternity care was covered by the VA in FY2015.
Estimating the Number of Unintended Pregnancies Associated With Each Dispensing Strategy
Unintended pregnancy frequency per 1000 women per year associated with each strategy was calculated based on the proportion of the cohort experiencing a pregnancy outcome (live birth, miscarriage, or abortion) during the model time horizon. We estimated the expected total unintended pregnancy frequency by multiplying the frequency per 1000 women per year by the number of VA enrollees using OCPs (n = 24 309).
Sensitivity Analyses
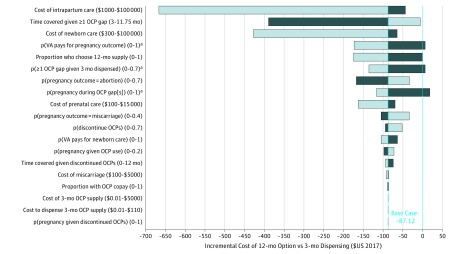
We performed 1-way sensitivity analyses, independently varying model variables across the ranges shown in Table 1, to identify variables with the greatest effect on base case results. Cost ranges are based on empirical VA data; ranges for probabilities and other variables are based on the literature and are intentionally broad to reflect uncertainty and allow consideration of potentially extreme values.30 A tornado diagram was generated to graphically represent 1-way sensitivity analyses, and threshold values (ie, variable values at which favored strategies change) were determined.
To assess overall model robustness and further estimate the effects of variable uncertainty, probabilistic sensitivity analysis with 5000 iterations was performed, simultaneously varying all model variables across plausible distributions.30 Per established guidelines, beta and gamma distributions were chosen to approximate probability distributions and right-skewed cost data, respectively.30 Table 1 shows distribution means and SDs. Standard deviations for cost variables are from VA data; resulting distributions were compared with empirical data to ensure reasonable approximation. Standard deviations for other variables were selected to approximate broad but plausible ranges similar to those used in 1-way sensitivity analyses. We calculated the likelihood that the 12-month option resulted in lower per-woman costs compared with the 3-month strategy, and the 95% probability range of incremental cost differences between strategies.
Results
Base Case Analyses
Mean annual cost per woman was $700.60 for the 12-month dispensing option, compared with $787.72 for the 3-month dispensing strategy, resulting in incremental VA cost savings of $87.12 per woman per year with the 12-month option. Among the 24 309 women receiving OCPs in the VA, the 12-month dispensing option is expected to save $2 117 800 annually.
Cost savings with 12-month dispensing result primarily from reductions in unintended pregnancies. Annually, 149 unintended pregnancies per 1000 women were expected with the 12-month option, compared with 173 per 1000 women in the 3-month strategy, for an absolute reduction of 24 unintended pregnancies per 1000 women per year. This reduction translates to 583 unintended pregnancies averted annually among women receiving OCPs in the VA with adoption of a 12-month dispensing option.
Sensitivity Analyses
One-way sensitivity analyses are shown in Figure 2. Cost savings with 12-month dispensing were sensitive to changes at the extremes of plausible ranges for probability of OCP coverage gaps with 3-month dispensing, pregnancy risk during gaps, and the proportion of pregnancies paid for by the VA. Threshold values for these variables are shown in Table 2.
Figure 2. One-way Sensitivity Analyses.
Bar colors denote the directionality of the variable range associated with the resultant incremental cost (ie, dark blue bars represent decreasing and light blue bars indicate increasing values). Threshold values are reported in Table 2. OCP indicates oral contraceptive pill; p, probability; VA, Veterans Affairs.
aVariation can result in the 3-month strategy being favored over the 12-month option.
Table 2. Threshold Values From One-way Sensitivity Analyses.
| Variable | Threshold Valuea |
|---|---|
| Probability VA pays for pregnancy outcome | 0.037 |
| Probability of ≥1 OCP coverage gap given 3 mo of OCPs dispensed | 0.031 |
| Probability of pregnancy during OCP coverage gap(s)b | 0.133 |
Abbreviations: OCP, oral contraceptive pill; VA, Veterans Affairs.
3-month dispensing is less costly than 12-month dispensing at the indicated variable range.
Annual probability of pregnancy given no contraceptive use, which is assumed during OCP coverage gaps (base case, 0.85). The overall probability of pregnancy over the model time horizon is prorated according to time using OCPs vs coverage gaps. Annual pregnancy probabilities are also prorated in the model to account for a time horizon of twelve 28-day periods (336 days) instead of a full calendar year.
In probabilistic sensitivity analyses simultaneously varying each variable across a plausible distribution, the 12-month strategy was cost saving in 95.4% of model iterations. The 95% probability range of the incremental cost difference ranged from annual cost savings of $389.79 per woman to additional costs of $13.34 per woman with the 12-month option compared with 3-month dispensing.
Discussion
Adoption of a 12-month OCP dispensing option is expected to produce substantial cost savings for the VA health care system while reducing unintended pregnancies experienced by women veterans. Model results are robust to variations across broad but plausible variable ranges, suggesting that 12-month OCP dispensing is economically feasible for the VA while better meeting the reproductive needs of the women the VA serves.
The potential consequences of an adverse event (ie, unintended pregnancy) resulting from short gaps in contraceptive coverage are arguably greater than for other prescription medications, and pregnancy is a costly outcome for both women and insurers. Although the VA uses innovative strategies such as a centralized mail-order pharmacy used for nearly 80% of prescriptions, refills are not automatic or instantaneous, and potential coverage gaps remain; this is evidenced by the 43% of women veterans who experience at least 1 gap between contraceptive refills,15 similar to patterns observed in US populations.13,14,16 In this model, sensitivity analyses indicate that only 3% of women can incur a coverage gap for 3-month dispensing to be favored, an implausibly low value based on empirical evidence. In contrast, robust evidence now highlights the potential for reduced contraceptive gaps and improved reproductive outcomes with dispensing of greater quantities of contraceptives,16,17,18,19 while additional health care system contacts have little effect on continuation of contraceptive use or patient safety.31,32 In addition to influencing national and international medical guidelines,5,20 these data have spurred recent US state-level legislative efforts, with 17 states and the District of Columbia requiring coverage of 12-month contraceptive supplies as of January 2019.33 As the largest US integrated health care system, and with its centralized pharmacy, the VA is uniquely positioned to implement similar evidence-based policy change on a national scale.
The substantial incremental cost savings predicted by our model with a 12-month OCP dispensing option are in alignment with existing empirical evidence and other models of contraceptive cost-effectiveness16,34,35 and, in fact, are intentionally conservative due to multiple assumptions biasing against the 12-month strategy. Our model’s projected 14% reduction in unintended pregnancy for 12-month vs 3-month dispensing is notably less than the empirically observed 30% reduced odds of pregnancy among California family planning program clients,19 suggesting that real-world implications of this policy change may have a greater effect than our model estimates. Despite our conservative assumptions, probabilistic sensitivity analysis indicates that 12-month dispensing is nearly always cost saving, and that additional costs per woman are minimal in rare iterations in which 3-month dispensing is favored. This robustness of model results to variations across generous ranges suggests that the projected cost savings with 12-month dispensing may translate to other US health care contexts, despite potential differences in baseline costs or population characteristics.
Allowing for 12-month OCP dispensing is one mechanism to enhance contraceptive access for US women and women veterans; however, other policies also limit veterans’ receipt of optimal reproductive health care. First, unlike most insured US women, who have zero cost sharing for contraception under the Affordable Care Act,36 some VA enrollees incur copayments for contraception, including 35% of women who filled VA OCP prescriptions in 2017. Copayments are associated with reduced adherence to contraceptive use among women veterans across all income levels37 and may be a barrier to use. In addition, VA policy excludes all abortion coverage. Although veterans seek abortion at rates similar to women in the general population,38 VA policy is more restrictive than many public insurance programs and the Department of Defense, which allow for coverage in cases of rape, incest, or life endangerment.39 Although our model defines abortion as a $0 cost to the VA, it clearly represents a nonzero cost to veterans seeking termination of unintended pregnancies.
Although our results suggest financial benefits to the VA of a 12-month OCP dispensing policy, it is vital that contraceptive policies serve first and foremost to augment women’s reproductive outcomes and autonomy. Economic arguments in family planning have historically been used to promote racist and classist policies by positing that limiting the reproduction of poor women and women of color can curb societal poverty.40,41 Such poverty amelioration arguments have led to coercive sterilization programs targeting socially marginalized populations and proposals conditioning receipt of welfare benefits on Norplant provision, among other injustices.40,41 Thus, although the favorable bottom line suggested by our results may be helpful in influencing policy change in the VA and other settings, we highlight these potential financial gains as a secondary benefit to the more important and evidence-based goal of improving contraceptive access and facilitating women veterans’ individual abilities to manage their reproductive lives as they see fit.
Limitations
Our model does not allow for switching to additional contraception methods during the 1-year time horizon or account for resultant pill wastage, which is a common counterargument against extended medication dispensing. However, prescription method switching and pill wastage were low in 2 large-scale studies in veteran and nonveteran populations.15,16 In addition, intermediate costs of additional methods would likely be negligible compared with cost savings due to reduced unintended pregnancies, as seen in empirical data.16 Second, our model may overestimate pregnancy risk by assuming use of only nonprescription methods or no contraception among women who discontinue OCPs, and no contraception use during OCP coverage gaps. We account for this limitation by broadly varying pregnancy probabilities in sensitivity analyses. Results were not sensitive to variations in pregnancy probability after discontinuation of OCP use, and annual pregnancy risk given no contraceptive use (assumed during OCP gaps) would have to be less than 13.3% for 3-month dispensing to be favored. This value is notably lower than the established annual pregnancy risk with no contraception (85%), as well as failure rates for all nonprescription contraceptive methods (range, 18%-28%) that women might use during coverage gaps. Third, our model does not account for the possibility that groups of women veterans choosing 12- vs 3-month OCP supplies may differ according to characteristics associated with OCP use, adherence, or risk of unintended pregnancy, including medical and mental health comorbidities. Finally, our work is subject to inherent limitations of model-based approaches, wherein applicability to real-world situations is bounded by assumptions, input data quality, and combined variable uncertainty. To mitigate these limitations and produce policy-relevant results, we made structural and parameter assumptions to bias against the 12-month dispensing option wherever possible and varied all variables individually and simultaneously over generous bounds.
Conclusions
Based on the outcomes of this model, adoption of a 12-month dispensing option for oral contraceptive pills may support reproductive autonomy and improve reproductive outcomes among women veterans and is expected to produce cost savings for the VA due to reductions in unintended pregnancies. Thus, the proposed policy is expected to be economically feasible for the VA while better supporting women veterans in meeting their reproductive goals.
References
- 1.Kizer KW, Dudley RA. Extreme makeover: transformation of the veterans health care system. Annu Rev Public Health. 2009;30:313-339. doi: 10.1146/annurev.publhealth.29.020907.090940 [DOI] [PubMed] [Google Scholar]
- 2.Frayne S, Phibbs C, Saechao F, et al. Sociodemographics, Utilization, Costs of Care, and Health Profile. Washington, DC: Women’s Health Evaluation Initiative, Women’s Health Services, Veterans Health Administration, Department of Veterans Affairs; 2014. Sourcebook: Women Veterans in the Veterans Health Administration, Volume 3. [Google Scholar]
- 3.Department of Veterans Affairs, Veterans Health Administration. VHA DIRECTIVE 1330.01(1). https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=5332. Amended July 24, 2018. Accessed Sept 29, 2017.
- 4.Borrero S, Callegari LS, Zhao X, et al. Unintended pregnancy and contraceptive use among women veterans: the ECUUN study. J Gen Intern Med. 2017;32(8):900-908. doi: 10.1007/s11606-017-4049-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Curtis KM, Jatlaoui TC, Tepper NK, et al. US selected practice recommendations for contraceptive use, 2016. MMWR Recomm Rep. 2016;65(4):1-66. doi: 10.15585/mmwr.rr6504a1 [DOI] [PubMed] [Google Scholar]
- 6.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397-404. doi: 10.1016/j.contraception.2011.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schneiter E. States and prescription drugs: an overview of state programs to rein in costs. National Academy for State Health Policy. https://nashp.org/wp-content/uploads/2016/04/Drug-Brief1.pdf. Published April 2016. Accessed March 18, 2019.
- 8.Guttmacher Institute Insurance coverage of contraception. https://www.guttmacher.org/evidence-you-can-use/insurance-coverage-contraception. Published August 2018. Accessed March 18, 2019.
- 9.Liang S-Y, Grossman D, Phillips KA. Women’s out-of-pocket expenditures and dispensing patterns for oral contraceptive pills between 1996 and 2006. Contraception. 2011;83(6):528-536. doi: 10.1016/j.contraception.2010.09.013 [DOI] [PubMed] [Google Scholar]
- 10.Rabbani A, Alexander GC. Cost savings associated with filling a 3-month supply of prescription medicines. Appl Health Econ Health Policy. 2009;7(4):255-264. doi: 10.1007/BF03256159 [DOI] [PubMed] [Google Scholar]
- 11.Taitel M, Fensterheim L, Kirkham H, Sekula R, Duncan I. Medication days’ supply, adherence, wastage, and cost among chronic patients in Medicaid. Medicare Medicaid Res Rev. 2012;2(3):mmrr.002.03.a04. doi: 10.5600/mmrr.002.03.A04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kazerooni R, Takizawa A, Vu K. Predictors of adherence to hormonal contraceptives in a female veteran population. Contraception. 2014;89(4):292-298. doi: 10.1016/j.contraception.2013.12.009 [DOI] [PubMed] [Google Scholar]
- 13.Nelson AL, Westhoff C, Schnare SM. Real-world patterns of prescription refills for branded hormonal contraceptives: a reflection of contraceptive discontinuation. Obstet Gynecol. 2008;112(4):782-787. doi: 10.1097/AOG.0b013e3181875ec5 [DOI] [PubMed] [Google Scholar]
- 14.Pittman ME, Secura GM, Allsworth JE, Homco JB, Madden T, Peipert JF. Understanding prescription adherence: pharmacy claims data from the Contraceptive CHOICE Project. Contraception. 2011;83(4):340-345. doi: 10.1016/j.contraception.2010.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borrero S, Zhao X, Mor MK, Schwarz EB, Good CB, Gellad WF. Adherence to hormonal contraception among women veterans: differences by race/ethnicity and contraceptive supply. Am J Obstet Gynecol. 2013;209(2):103.e1-103.e11. doi: 10.1016/j.ajog.2013.03.024 [DOI] [PubMed] [Google Scholar]
- 16.Foster DG, Parvataneni R, de Bocanegra HT, Lewis C, Bradsberry M, Darney P. Number of oral contraceptive pill packages dispensed, method continuation, and costs. Obstet Gynecol. 2006;108(5):1107-1114. doi: 10.1097/01.AOG.0000239122.98508.39 [DOI] [PubMed] [Google Scholar]
- 17.White KO, Westhoff C. The effect of pack supply on oral contraceptive pill continuation: a randomized controlled trial. Obstet Gynecol. 2011;118(3):615-622. doi: 10.1097/AOG.0b013e3182289eab [DOI] [PubMed] [Google Scholar]
- 18.Steenland MW, Rodriguez MI, Marchbanks PA, Curtis KM. How does the number of oral contraceptive pill packs dispensed or prescribed affect continuation and other measures of consistent and correct use? a systematic review. Contraception. 2013;87(5):605-610. doi: 10.1016/j.contraception.2012.08.004 [DOI] [PubMed] [Google Scholar]
- 19.Foster DG, Hulett D, Bradsberry M, Darney P, Policar M. Number of oral contraceptive pill packages dispensed and subsequent unintended pregnancies. Obstet Gynecol. 2011;117(3):566-572. doi: 10.1097/AOG.0b013e3182056309 [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. Selected Practice Recommendations for Contraceptive Use. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
- 21.US Department of Veterans Affairs Medication Copayments. https://www.va.gov/healthbenefits/resources/publications/hbco/hbco_copayments.asp. Updated April 2, 2018. Accessed March 13, 2019.
- 22.MacDorman MF, Gregory EC. Fetal and perinatal mortality: United States, 2013. Natl Vital Stat Rep. 2015;64(8):1-24. [PubMed] [Google Scholar]
- 23.American College of Obstetricians and Gynecologists ACOG Practice Bulletin No. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018;131(3):e91-e103. doi: 10.1097/AOG.0000000000002560 [DOI] [PubMed] [Google Scholar]
- 24.Eddy DM, Hollingworth W, Caro JJ, Tsevat J, McDonald KM, Wong JB; ISPOR−SMDM Modeling Good Research Practices Task Force . Model transparency and validation: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force–7. Value Health. 2012;15(6):843-850. doi: 10.1016/j.jval.2012.04.012 [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. 2011-2013 NSFG: public use data files, codebooks, and documentation. https://www.cdc.gov/nchs/nsfg/nsfg_2011_2013_puf.htm. Reviewed May 29, 2019. Accessed January 3, 2019.
- 26.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008-2011. N Engl J Med. 2016;374(9):843-852. doi: 10.1056/NEJMsa1506575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Partnership for Women and Families. Transforming Maternity Care blog. The cost of having a baby in the United States. Ann Arbor, MI: Truven Health Analytics. http://transform.childbirthconnection.org/reports/cost/. Published January 2013. Accessed January 24, 2019.
- 28.US Department of Veterans Affairs. Electronic Code of Federal Regulations. Medical benefits package. 38 CFR § 17.38(c)(1). https://ecfr.io/Title-38/pt38.1.17#se38.1.17_138. Reviewed May 29, 2019. Accessed January 3, 2019.
- 29.American College of Obstetricians and Gynecologists ACOG Practice Bulletin No. 200: early pregnancy loss. Obstet Gynecol. 2018;132(5):e197-e207. doi: 10.1097/AOG.0000000000002899 [DOI] [PubMed] [Google Scholar]
- 30.Briggs AH, Weinstein MC, Fenwick EAL, Karnon J, Sculpher MJ, Paltiel AD; ISPOR-SMDM Modeling Good Research Practices Task Force . Model parameter estimation and uncertainty analysis: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force Working Group–6. Med Decis Making. 2012;32(5):722-732. doi: 10.1177/0272989X12458348 [DOI] [PubMed] [Google Scholar]
- 31.Steenland MW, Zapata LB, Brahmi D, Marchbanks PA, Curtis KM. Appropriate follow up to detect potential adverse events after initiation of select contraceptive methods: a systematic review. Contraception. 2013;87(5):611-624. doi: 10.1016/j.contraception.2012.09.017 [DOI] [PubMed] [Google Scholar]
- 32.Steenland MW, Zapata LB, Brahmi D, Marchbanks PA, Curtis KM. The effect of follow-up visits or contacts after contraceptive initiation on method continuation and correct use. Contraception. 2013;87(5):625-630. doi: 10.1016/j.contraception.2012.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guttmacher Institute Insurance coverage of contraceptives. State laws and policies. http://www.guttmacher.org/state-policy/explore/insurance-coverage-contraceptives. Updated May 1, 2019. Accessed January 9, 2019.
- 34.McMenamin SB, Charles SA, Tabatabaeepour N, Shigekawa E, Corbett G. Implications of dispensing self-administered hormonal contraceptives in a 1-year supply: a California case study. Contraception. 2017;95(5):449-451. doi: 10.1016/j.contraception.2016.12.008 [DOI] [PubMed] [Google Scholar]
- 35.Trussell J, Lalla AM, Doan QV, Reyes E, Pinto L, Gricar J. Cost effectiveness of contraceptives in the United States. Contraception. 2009;79(1):5-14. doi: 10.1016/j.contraception.2008.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bearak JM, Finer LB, Jerman J, Kavanaugh ML. Changes in out-of-pocket costs for hormonal IUDs after implementation of the Affordable Care Act: an analysis of insurance benefit inquiries. Contraception. 2016;93(2):139-144. doi: 10.1016/j.contraception.2015.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kazerooni R, Vu K, Takizawa A, Broadhead C, Morreale AP. Association of copayment and socioeconomic status with hormonal contraceptive adherence in a female veteran population. Womens Health Issues. 2014;24(2):e237-e241. doi: 10.1016/j.whi.2013.12.002 [DOI] [PubMed] [Google Scholar]
- 38.Schwarz EB, Sileanu FE, Zhao X, Mor MK, Callegari LS, Borrero S. Induced abortion among women veterans: data from the ECUUN study. Contraception. 2018;97(1):41-47. doi: 10.1016/j.contraception.2017.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Legal Information Institute. US Code § 1093. Performance of abortions: restrictions. https://www.law.cornell.edu/uscode/text/10/1093. Last amended January 2, 2013. Accessed January 15, 2019.
- 40.Burrell DE. The Norplant Solution: Norplant and the control of African-American motherhood. UCLA Womens Law J. 1995;5(2):401-444. [Google Scholar]
- 41.Harris LH, Wolfe T. Stratified reproduction, family planning care and the double edge of history. Curr Opin Obstet Gynecol. 2014;26(6):539-544. doi: 10.1097/GCO.0000000000000121 [DOI] [PubMed] [Google Scholar]