Abstract
Objective
To estimate the causal impact of community based blood pressure screening on subsequent blood pressure levels among older adults in China.
Design
Regression discontinuity analysis using data from a national cohort study.
Setting
2011-12 and 2014 waves of the Chinese Longitudinal Healthy Longevity Survey, a national cohort of older adults in China.
Participants
3899 older adults who had previously undiagnosed hypertension.
Intervention
Community based hypertension screening among older adults in 2011-12.
Main outcome measure
Blood pressure two years after initial screening.
Results
The intervention reduced systolic blood pressure: −6.3 mm Hg in the model without covariates (95% confidence interval −11.2 to −1.3) and −8.3 mm Hg (−13.6 to −3.1) in the model that adjusts additionally for demographic, social, and behavioural covariates. The impact on diastolic blood pressure was smaller and non-significant in all models. The results were similar when alternative functional forms were used to estimate the impact and the bandwidths around the intervention threshold were changed. The results did not vary by demographic and social subgroups.
Conclusions
Community based hypertension screening and encouraging people with raised blood pressure to seek care and adopt blood pressure lowering behaviour changes could have important long term impact on systolic blood pressure at the population level. This approach could address the high burden of cardiovascular diseases in China and other countries with large unmet need for hypertension diagnosis and care.
Introduction
Hypertension is an important modifiable risk factor for stroke and cardiovascular disease, and is a major risk factor for mortality globally.1 2 In China,3 nearly half of adults aged 35-75 years have hypertension4 and 24% of deaths have been attributed to the condition,1 which has resulted in major health and economic burdens at the community and national levels.5 Hypertension is easy and inexpensive to diagnose and mortality risk can be substantially reduced through effective low cost off-patent drugs,6 7 8 but China still has large gaps in care for people with the condition. Recent evidence has shown that only 45% of Chinese adults with hypertension were aware of their condition, only 30% were taking antihypertensive drugs, and just 7% had achieved normal blood pressure levels.4 Therefore, reducing blood pressure in adults with hypertension in China has the potential to improve population health.
Awareness of hypertension is a crucial first step for people to seek care and achieve long lasting blood pressure control through lifestyle changes. The finding that more than half of adults with hypertension in China are unaware of their condition4 has led to calls for major investments in hypertension screening at healthcare facilities and in the community, such as through community health worker programmes.9 10 However, an important question is whether community based screening will be effective at improving hypertension at the population level. Screening might not lead to blood pressure improvements if people do not take action after a measurement indicates that they have hypertension.For example, people screened in the community might not act on advice to seek treatment for hypertension at a healthcare facility or to change their diet or exercise habits. Even if people start treatment, they might not adhere to it or routinely seek recommended follow-up care. Therefore, it is important to understand whether and to what extent community based screening causally affects adults’ subsequent blood pressure levels and thus their risk of serious illness such as stroke and cardiovascular disease, and ultimately death.
This study uses a quasi-experimental approach, a non-parametric regression discontinuity design, to estimate the causal impact of community based hypertension screening on blood pressure two years after the initial screening. The design allows causal impact to be estimated in the absence of explicit randomisation. Continuous systolic and diastolic blood pressure measurements are subject to random variability caused by measurement error. This random variability implies that people with a blood pressure measurement just above the standard threshold for hypertension have similar baseline covariates to people with a measurement just below the threshold, just like people in the intervention and control arms of a randomised controlled trial. Therefore, if we compare outcomes in the groups with blood pressure just above and just below the threshold, we can estimate the causal impact of the recommendations made after a screening diagnosis of hypertension, which include to seek care and to make lifestyle changes. We estimated the impact of blood pressure screening on blood pressure after two years, as well as on factors that lie on the pathway from a screening diagnosis of hypertension to future blood pressure levels. We also investigated how the impact of blood pressure screening varies across population subgroups.
Methods
Data source and sampling design
We analysed data from the Chinese Longitudinal Healthy Longevity Survey.11 This national cohort focuses on older people and is the largest cohort of centenarians in the world. The cohort data are high quality and contain individual level information on demographic and socioeconomic characteristics, health indicators, and social and behavioural risk factors. The baseline wave was conducted in 1998, with follow-up waves conducted in 2000, 2002, 2005, 2008-09, 2011-12, and 2014. The sampling for this cohort followed a multistage approach. In the first stage, a random sample was drawn of half the total number of counties and cities in 22 provinces. These cities and counties collectively represent 85% of the total Chinese population. The sample included people from nine eastern provinces (Hebei, Beijing, Tianjing, Shanghai, Jiangsu, Zhejiang, Fujian, Shangdong, and Guangdong), three northeastern provinces (Liaoning, Jilin, and Heilongjiang), six central provinces (Shanxi, Anhui, Jiangxi, Henan, Hubei, and Hunan), and four western provinces (Shaanxi, Guangxi, Sichuan, and Chongqing).
In the second stage, all centenarians living in the sampled counties and cities who were willing to participate were included in the cohort and the response rate was 97.7%. For each participating centenarian, one octogenarian and one nonagenarian living in the same community or institution were randomly sampled. In addition, since 2002, for every three sampled centenarians, four younger elderly people (aged 65-79) living in the same city or county were randomly chosen. Further details on data quality assessment, sampling design, and study procedures can be found elsewhere.12 13 14 In this study, we used data from the latest two waves of the cohort (2011-12 and 2014). Our study is a complete case analysis and is limited to adults who were aged 65 and older in the 2011-12 wave with complete information on all outcomes and covariates.
Blood pressure measurement and treatment encouragement
Field workers from the Chinese Center for Disease Control and Prevention who had previous medical knowledge were trained on how to measure blood pressure. Field workers measured each adult’s blood pressure by using a mercury sphygmomanometer on the right arm while the person was in a seated position. Blood pressure was measured twice with at least one minute between measurements. We have used the average of the two blood pressure measurements in our study.
Our study design uses the fact that field workers encouraged people to seek care and to adopt healthy diet and exercise behaviours when their blood pressure levels were raised. According to the written informed consent, if field workers identify any health issues, they should promptly notify people and provide the necessary advice. All the field workers had been trained in the principles of preventive medicine and understood the Chinese national guidelines for the management of hypertension. Therefore, they could inform people with hypertension about the risks of their condition and how to effectively reduce their blood pressure levels.15
The field workers gave all participants or their relatives the systolic and diastolic blood pressure results after the screening. They verbally encouraged people to seek care for hypertension and to make positive health behaviour changes when their average systolic blood pressure was 140 mm Hg or higher or their average diastolic blood pressure was 90 mm Hg or higher. The field workers’ recommendations were based on the Chinese national guidelines for the management of hypertension. The guidelines include recommendations on the use of antihypertensive drugs; weight management (eg, lower meat consumption and reduced calorie consumption, such as from sugary drinks); stopping smoking; reducing alcohol consumption; lowering salt consumption (eg, consuming fewer salt preserved vegetables and more fresh vegetables and fruits); exercising; and reducing psychological stress.15
The intervention thus consisted of screening, results notification, treatment encouragement, and education on protective lifestyles and behaviours; it did not include educational pamphlets, and the precise times spent on the different components of this intervention were not specified. The intervention is similar to the process carried out during other real-life community based hypertension screening programmes in China. Moreover, the field workers who conducted the study intervention would probably be part of the health worker teams who would perform community based hypertension screening if this intervention were part of routine health policy.15 16
Study design
Regression discontinuity design
The regression discontinuity design can be used when a threshold is applied to a continuous assignment variable to decide whether a person receives an intervention or not; that is, the intervention is assigned deterministically (where everyone on one side of the threshold is treated while no one on the other side is treated, the so-called sharp regression discontinuity design) or probabilistically (where the probability of being treated is higher on one side of the threshold than on the other side, the so-called fuzzy regression discontinuity design).17 18 19 In this study, we used a sharp regression discontinuity design to establish the causal impact of community based hypertension screening in real life. The continuous assignment variable for our regression discontinuity analysis is the blood pressure measurement in the 2011-12 wave. The thresholds used in this analysis are the blood pressure cutoff points: systolic blood pressure of 140 mm Hg or diastolic blood pressure of 90 mm Hg, which are the thresholds for hypertension according to the Chinese national guidelines on hypertension treatment.15 20 The field workers used these thresholds to decide who should receive verbal encouragement or referral to a healthcare facility for a diagnostic workup, and behavioural counselling. Our results thus represent the real-life, or intention-to-treat, impact of community based hypertension screening. Our main outcome measures were the participant’s systolic and diastolic blood pressure in the 2014 wave of the cohort.
The validity of the regression discontinuity design relies on the assumption of continuity in potential outcomes as a function of the assignment variable around the threshold. This implies that people just above the threshold are exchangeable (similar on all factors driving the outcome) with those just below the threshold, except for the probability of receiving the intervention.18 There are generally two major concerns in the application of this design. The first concern is that the assignment variable is manipulated (eg, field workers record a higher blood pressure than measured so that they can offer more people a referral to a healthcare facility). We assessed visually whether assignment was manipulated using a histogram of the continuous assignment variable. We did not find evidence of manipulation such as bunching of observations around the threshold.19 We also tested the hypothesis of no manipulation statistically by using the methods developed by McCrary.21 The second concern is the possibility of other changes that are correlated with both the blood pressure threshold and the outcome. Intuitively, such changes can have effects on the outcome, and these effects would be incorrectly attributed to the treatment. Such other changes are unlikely, however, because the field workers did not use the hypertension threshold to administer any interventions other than those described. We followed the method of Lee and colleagues,22 and Imbens and Lemieux18 to test whether other variables are continuous near the threshold; that is, to evaluate whether there are systematic differences in individual characteristics that are correlated with the threshold. We assessed the balance of participants’ observed characteristics on either side of the threshold by comparing the mean values of important covariates for those just above and below the threshold. For imbalanced variables, we tested whether there is a major jump of these variables at the threshold using placebo tests that treat individual characteristics as the outcome variables.22 We present the results from these tests in the results section.
Covariates
Under the assumptions of the regression discontinuity design, it is not necessary to include covariates for unbiased causal inference. However, adding covariates to the estimation is useful to eliminate small sample imbalances in observed variables that are correlated with the threshold, and to improve the precision of the causal impact estimates.18 23 We thus present models that adjust additionally for demographic characteristics (including age, sex, urban residence, marital status, and number of children); socioeconomic characteristics (including years of education and self reported relative economic status); and health behaviours (including whether people exercised, smoked, drank alcohol, and regularly ate fresh fruits, fresh vegetables, meat, salt preserved vegetables, and sugar). Self reported relative economic status was determined based on a comparison with other local people and measured on a scale ranging from 1 (very rich) to 5 (very poor). Each diet variable was measured on a consumption scale ranging from 1 (rarely or never) to 3 (almost every day).
Statistical methods
We implemented a local linear regression to estimate the impact of blood pressure screening in 2011-12 on blood pressure in 2014, following Imbens and Lemieux.18 Our choice of a local linear specification for our main analysis was guided by recent econometric studies that recommend the use of linear rather than higher order polynomials to prevent overfitting of the data and misleading impact estimation.24 25 The coefficients of the added quadratic terms were also insignificant at the 5% significance level, indicating that higher order polynomials are not adding value to our estimation. However, there was visual evidence of a potential non-linear relation between the assignment variable and the outcome. In a separate analysis, we thus added quadratic terms to our regression equations as a robustness check. We show both the local linear and the local quadratic regression discontinuity design results. In all regressions, we used a triangular kernel function, which gives more weight to observations closer to the threshold.
For the main local linear results we fitted regression models separately for systolic and diastolic blood pressure:
| For systolic blood pressure: |
| Yi = α0 + α1Abovei + α2(SBPi − 140) + α3Abovei(SBPi − 140) + Xiκ + vi |
| For diastolic blood pressure: |
| Zi = β0 + β1Abovei + β2(DBPi − 90) + β3Abovei(DBPi − 90) + Xiϕ + εi |
Yi is a measure of individual i’s systolic blood pressure and Zi is a measure of individual i’s diastolic blood pressure in 2014; Abovei is an indicator variable equal to 1 for people who have systolic blood pressure of at least 140 mm Hg (in the first equation) or have diastolic blood pressure of at least 90 mm Hg (in the second equation) in 2011-12; SBPi is a measure of individual i’s systolic blood pressure in 2011-12 and DBPi is a measure of individual i’s diastolic blood pressure in 2011-12; and Xi is a vector of covariates in 2011-12 predictive of the outcome. In these models, the local average causal impacts of community based screening on blood pressure in 2014 are given by α1 and β1. α2 is the marginal increase in systolic blood pressure in 2014 when systolic blood pressure in 2011-12 is lower than 140 mm Hg (similarly, β2 is the marginal increase in diastolic blood pressure when diastolic blood pressure is lower than 90 mm Hg). α2+α3 is the marginal increase in systolic blood pressure in 2014 when systolic blood pressure in 2011-12 is at least 140 mm Hg (similarly, β2+β3 is the marginal increase in diastolic blood pressure in 2014 when diastolic blood pressure in 2011-12 is at least 90 mm Hg).
We determined the bandwidth around the hypertension threshold using the data driven optimal bandwidth method developed by Imbens and Kalyanaraman.26 The choice of bandwidth is important because estimates using a smaller bandwidth will have lower bias but higher variance, while estimates using a larger bandwidth will have higher bias but lower variance. In additional analyses, we evaluated the sensitivity of our results to the choice of bandwidth by re-estimating the main impact across a range of potential bandwidths. In the baseline analysis, the optimal bandwidth (rounded to the nearest integer) was 6 mm Hg for systolic and diastolic blood pressure. We also explored whether there is important heterogeneity in causal impact by age, sex, urban residence, marital status, number of children, years of education, or self reported economic status.
After estimating the main impact, we conducted additional regression discontinuity analyses to elucidate potential downstream lifestyle changes induced by the intervention, including effects on weight, exercise, smoking, and consumption of alcohol, fresh fruits, fresh vegetables, meat, salt preserved vegetables, and sugar. For these binary outcomes, we used modified Poisson regression to estimate risk ratios.27
We also conducted placebo tests using outcomes that occurred before the intervention and thus could not have been affected by the intervention in 2011-12, to rule out endogenous intervention assignment generated by the 140 and 90 mm Hg blood pressure thresholds. We used Stata version 14.1 to conduct the statistical analyses.
Patient and public involvement
None of the participants was involved in the design of the questionnaire, biological measurements, or outcome measures; they were also not involved in the design, recruitment, and implementation of the study. All participants or their relatives were informed of the systolic and diastolic blood pressure results and use of the data for research in this study. We plan to disseminate our study widely through the media, including in China.
Results
Sample characteristics
The initial sample consisted of 6010 people. We excluded 437 people (7%) because of missing information on blood pressure in 2011-12 or 2014, or because they had not answered the question on whether they had previously been diagnosed as having hypertension. Among the remaining 5573 participants, 3899 (70%) had previously undiagnosed hypertension and thus formed the sample for the analysis.
Table 1 shows the characteristics of the full sample and the within optimal bandwidth samples for systolic blood pressure and diastolic blood pressure. The demographic, socioeconomic, and health behaviour characteristics were similar for all three samples; for example, the mean age was around 85 years, around 45% were married, they had around 2.4 years of education, and around 21% were smokers.
Table 1.
Demographic, socioeconomic, and health behaviour characteristics for overall sample and within bandwidth samples (2011-12 wave, China Longitudinal Healthy Longevity Survey). Data are numbers (%) unless stated otherwise
| Characteristics | Full sample (n=3899) | Samples within optimal bandwidth | |
|---|---|---|---|
| Systolic blood pressure (n=879) | Diastolic blood pressure (n=886) | ||
| Demographic: | |||
| Mean (SD) age (years) | 85.7 (10.6) | 85.4 (10.3) | 85.6 (11.0) |
| Male | 1867 (47.9) | 403 (45.9) | 444 (50.1) |
| Urban residence | 322 (9.0) | 68 (8.5) | 67 (8.5) |
| Married | 1752 (45.2) | 381 (43.6) | 401 (45.5) |
| Mean (SD) no of children | 4.4 (2.1) | 4.5 (2.1) | 4.4 (2.0) |
| Socioeconomic: | |||
| Mean (SD) years of education | 2.4 (3.5) | 2.3 (3.4) | 2.5 (3.4) |
| Mean (SD) self reported relative economic status* | 3.0 (0.7) | 3.0 (0.7) | 3.0 (0.7) |
| Very rich | 51 (1.3) | 9 (1.0) | 14 (1.6) |
| Rich | 674 (17.3) | 158 (18.0) | 147 (16.6) |
| Average | 2551 (65.4) | 581 (66.1) | 593 (66.9) |
| Poor | 475 (12.2) | 96 (10.9) | 106 (12.0) |
| Very poor | 111 (2.9) | 26 (3.0) | 22 (2.5) |
| Don’t know or missing | 37 (1.0) | 9 (1.0) | 4 (0.5) |
| Health behaviour: | |||
| Exercise | 1434 (37.2) | 301 (34.4) | 327 (37.3) |
| Smoke | 819 (21.2) | 177 (20.3) | 177 (20.1) |
| Drink alcohol | 798 (20.7) | 184 (21.3) | 193 (22.0) |
| Mean (SD) consumption of:† | |||
| Fresh fruits | 1.9 (0.6) | 1.9 (0.6) | 1.9 (0.6) |
| Fresh vegetables | 2.6 (0.6) | 2.5 (0.6) | 2.5 (0.6) |
| Meat | 2.3 (0.6) | 2.2 (0.6) | 2.3 (0.6) |
| Salt preserved vegetables | 1.8 (0.7) | 1.8 (0.7) | 1.9 (0.7) |
| Sugar | 1.8 (0.7) | 1.8 (0.7) | 1.8 (0.7) |
SD=standard deviation.
Self reported relative economic status was measured on a scale from 1 (very rich) to 5 (very poor).
Consumption of fresh fruits, fresh vegetables, meat, salt preserved vegetables, and sugar was measured in terms of frequency of consumption ranging from 1 (rarely or never) to 3 (almost every day).
Manipulation of assignment variable
The regression discontinuity design requires that there must be no manipulation of the assignment variable (blood pressure in 2011-12) around the threshold. Figure 1 presents a histogram of the assignment variable to visually check for the presence of manipulation. We found no visual evidence of bunching around the threshold, which would have suggested that the field workers had manipulated the screening results. Based on the formal test developed by McCrary,21 we also failed to reject the null hypothesis of a smooth density across the threshold, which provided further support that there was no manipulation of the assignment variable (see supplementary material A).
Fig 1.
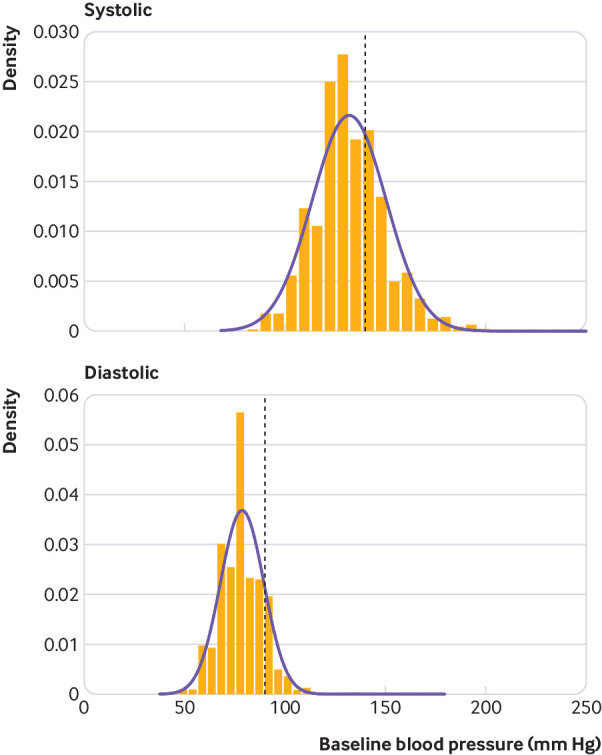
Density of baseline systolic and diastolic blood pressure distribution to test for manipulation of baseline blood pressure at threshold. The dashed line represents the 140 or 90 mm Hg threshold above which field workers encouraged people to seek care and change their lifestyles. Sample size=3899
Continuity of participants’ observed characteristics around threshold
The regression discontinuity design requires that no other interventions or changes that affect the outcome were correlated with the 140 or 90 mm Hg hypertension threshold. Table 2 shows the mean demographic, socioeconomic, and health behaviour characteristics for people just above and just below the thresholds within the optimal bandwidth. Most of the characteristics were balanced around the threshold. For the systolic blood pressure outcome, the exceptions were age, urban residence, exercise, and consumption of salt preserved vegetables. For the diastolic blood pressure outcome, there were slight imbalances in years of education and consumption of sugar. However, the validity of the design still holds because we found that these variables were continuous near the threshold (see supplementary material B), according to the method of Lee and colleagues,22 and Imbens and Lemieux.18 In our regression analysis, we included results controlling for these covariates and found that the results were robust.
Table 2.
Covariate means above and below blood pressure discontinuity thresholds within optimal bandwidths
| Characteristics | Baseline systolic blood pressure | Difference in means (n=879) | Baseline diastolic blood pressure | Difference in means (n=886) | ||
|---|---|---|---|---|---|---|
| <140 mm Hg (n=380) | ≥140 mm Hg (n=499) | <90 mm Hg (n=478) | ≥90 mm Hg (n=408) | |||
| Demographic: | ||||||
| Age (years) | 84.6 | 86.0 | 1.5† | 85.6 | 85.7 | −0.1 |
| Male (%) | 48.9 | 43.5 | −5.4 | 49.8 | 50.5 | 0.7 |
| Urban residence (%) | 10.8 | 6.7 | −4.1† | 8.6 | 8.3 | −0.3 |
| Married (%) | 45.4 | 42.3 | −3.1 | 45.0 | 46.2 | 1.2 |
| No of children | 4.5 | 4.5 | 0.0 | 4.4 | 4.3 | −0.1 |
| Socioeconomic: | ||||||
| Years of education | 2.5 | 2.2 | −0.3 | 2.3 | 2.7 | 0.4* |
| Self reported relative economic status§ | 2.9 | 3.0 | 0.1 | 3.0 | 3.0 | 0.0 |
| Health behaviour: | ||||||
| Exercise (%) | 39.2 | 30.8 | −8.4‡ | 36.6 | 38.1 | 1.4 |
| Smoke (%) | 23.2 | 18.0 | −5.2* | 18.7 | 21.8 | 3.1 |
| Drink alcohol (%) | 21.1 | 21.5 | 0.4 | 23.6 | 20.1 | −3.5 |
| Consumption of:¶ | ||||||
| Fresh fruits | 1.9 | 1.9 | 0.0 | 1.9 | 1.9 | 0.0 |
| Fresh vegetables | 2.1 | 2.1 | 0.0 | 2.1 | 2.1 | 0.0 |
| Meat | 2.3 | 2.2 | −0.1 | 2.3 | 2.2 | −0.1 |
| Salt preserved vegetables | 1.9 | 1.8 | −0.1† | 1.8 | 1.9 | 0.1 |
| Sugar | 1.8 | 1.8 | 0.0 | 1.8 | 1.9 | 0.1* |
Bandwidth is 134-146 mm Hg for systolic blood pressure and 84-96 mm Hg for diastolic blood pressure.
*P<0.1.
†P<0.05.
‡P<0.001.
§Self reported relative economic status was measured on a scale from 1 (very rich) to 5 (very poor).
¶Consumption of fresh fruits, fresh vegetables, meat, salt preserved vegetables, and sugar was measured in terms of frequency of consumption from 1 (rarely or never) to 3 (almost every day).
Impact estimates
Figure 2 shows the main outcome variables (systolic blood pressure and diastolic blood pressure in 2014) across the range of the assignment variable (blood pressure in 2011-12) inside the optimal bandwidths, with the threshold indicated by the dashed line. We observed a sharp downward jump in systolic blood pressure and diastolic blood pressure across the discontinuity, which visually suggests an impact of community blood pressure screening in 2011-12 on blood pressure in 2014.
Fig 2.
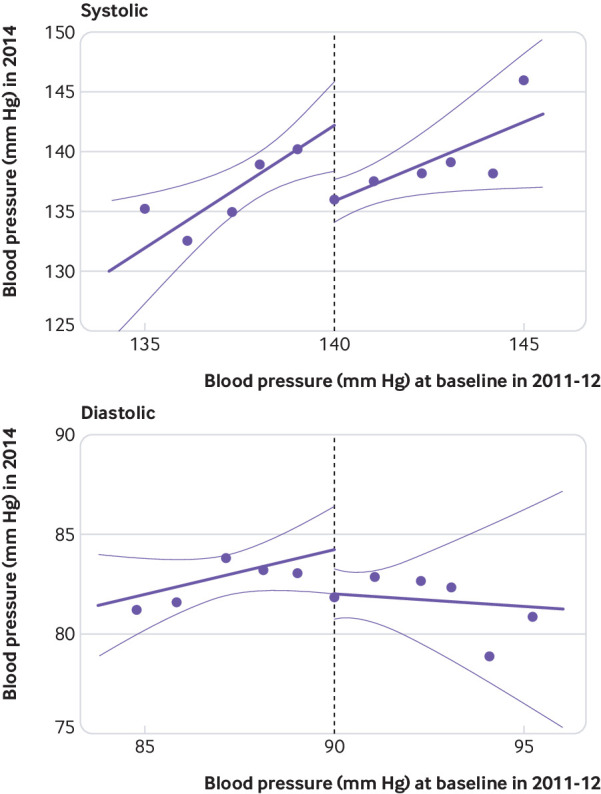
Blood pressure in 2014 across the range of blood pressure in 2011-12 within the optimal bandwidths. The dashed line indicates blood pressure threshold above which field workers encouraged people to seek care and to make lifestyle changes; bold lines correspond to the linear fit; fine lines represent 95% confidence intervals. The total sample size is 3899; the sample size within the optimal bandwidth is 879 for systolic blood pressure and 886 for diastolic blood pressure
Table 3 presents the results from the regression estimates of the local causal impact of community based screening. We found that community based screening in 2011-12 caused a significant reduction in systolic blood pressure in 2014. We estimated that community based screening reduced systolic blood pressure two years later by 6.3 mm Hg (95% confidence interval −11.2 to −1.3, P=0.01). The size of the impact of community based screening on systolic blood pressure increased to a reduction of 8.3 mm Hg when we additionally controlled for the demographic, socioeconomic, and behavioural covariates identified previously (95% confidence interval −13.6 to −3.1, P=0.002). This impact size was larger when estimated using a local quadratic fit (15.9 mm Hg reduction). Our main results did not differ when we adjusted for age using broad age categories (65-79, 80-89, 90-99, and ≥100 years) instead of continuous functional forms to control for age (table S5). The impacts for diastolic blood pressure were in the same direction, but they were smaller and not statistically significant.
Table 3.
Regression discontinuity estimates (95% confidence intervals) of the impact of community based hypertension screening in 2011-12 on blood pressure in 2014 (Chinese Longitudinal Healthy Longevity Survey)
| Impact of screening on blood pressure (mm Hg)* | Without covariates | With demographic covariates | With demographic and social covariates | With demographic, social, and behavioural covariates |
|---|---|---|---|---|
| Systolic blood pressure (local linear) | −6.3 (−11.2 to −1.3) | −7.3 (−12.6 to −2.1) | −7.9 (−13.2 to −2.7) | −8.3 (−13.6 to −3.1) |
| P value | 0.01 | 0.006 | 0.003 | 0.002 |
| Diastolic blood pressure (local linear) | −2.2 (−5.9 to 1.5) | −2.3 (−6.4 to 1.7) | −2.6 (−6.6 to 1.4) | −2.0 (−5.9 to 2.0) |
| P value | 0.24 | 0.26 | 0.21 | 0.33 |
| Systolic blood pressure (local quadratic) | −10.4 (−20.0 to −0.7) | −13.6 (−23.4 to −3.7) | −14.2 (−24.2 to −4.2) | −15.9 (−25.9 to −6.0) |
| P value | 0.04 | 0.007 | 0.005 | 0.002 |
| Diastolic blood pressure (local quadratic) | −0.8 (−8.1 to 6.5) | −1.6 (−9.7 to 6.5) | −2.5 (−10.6 to 5.6) | −2.4 (−10.4 to 5.6) |
| P value | 0.83 | 0.70 | 0.55 | 0.56 |
The sample comprises people within the optimal bandwidth of the threshold of 140 or 90 mm Hg. Each cell represents the coefficient from a separate regression. In all regressions, we used a triangular kernel function, which gives more weight to observations closer to the threshold. Models in the second column do not control for any covariates; models in the third column include demographic covariates (age, sex, urban residence, marital status, and number of children); models in the fourth column additionally include social covariates (education and self reported relative economic status); models in the fifth column additionally include behavioural covariates (such as exercise, smoking, alcohol consumption, and diet).
Baseline systolic blood pressure or diastolic blood pressure used as assignment variable.
We also estimated a set of regressions with interactions to see if the impact of community based screening differed across population subgroups. We found no evidence of heterogeneity in impact by age, sex, urban residence, marital status, number of children, years of education, or self reported economic status (see supplementary material C).
Downstream lifestyle changes as mechanisms of intervention action
Based on additional regression discontinuity analyses, we found evidence that the intervention could have led to substantial weight loss (an average of −1.1 kg, 95% confidence interval −4.5 to 2.4) and large reductions in the likelihood of current smoking (relative risk 0.62, 0.37 to 1.07), current alcohol consumption (0.71, 0.42 to 1.21), and frequent exercise (0.61, 0.41 to 0.91). In contrast, the intervention is unlikely to have had large effects on the daily consumption of salt preserved vegetables (0.99, 0.81 to 1.20), fresh vegetables (1.01, 0.97 to 1.05), fresh fruits (1.03, 0.88 to 1.22), meat (0.98, 0.94 to 1.03), and sugar (1.07, 0.88 to 1.31). Overall, however, our power to estimate downstream lifestyle changes was low and we lacked the data to estimate several potentially important changes, such as receiving drugs to treat hypertension and reducing stress.
Robustness checks and placebo test
We tested the robustness of our findings by examining the magnitude and precision of the impact estimates over multiple blood pressure bandwidths for systolic and diastolic blood pressure. In addition to the optimal bandwidth, we also used bandwidths of 50%, 80%, 120%, and 150% of the optimal bandwidth to see the variation of results with bandwidth. We plotted the impact size against the bandwidth and extrapolated impact size to a bandwidth of zero (fig 3). As the bandwidth shrinks, the impact size becomes larger for systolic blood pressure and approaches zero for diastolic blood pressure. These robustness checks further support our main results of a strong and significant impact of community based screening on systolic blood pressures two years later, and no impact on diastolic blood pressure (see supplementary material D).
Fig 3.
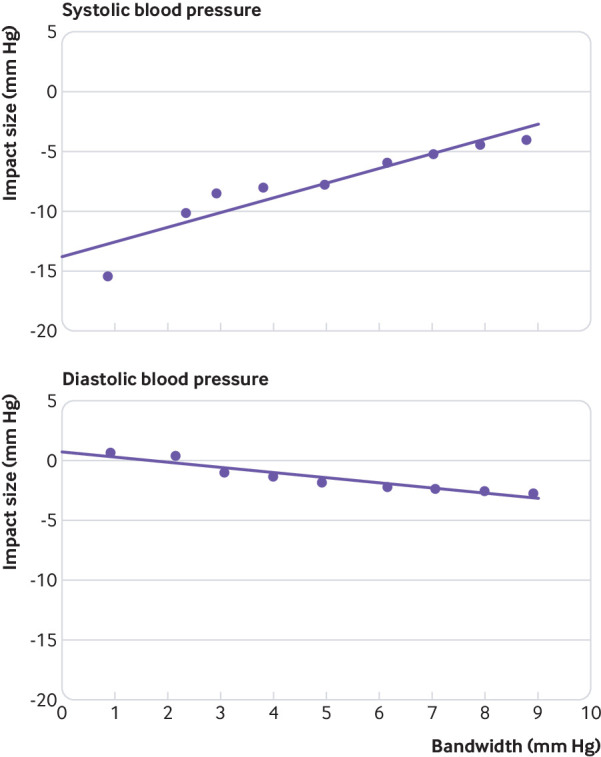
Impact size for systolic and diastolic blood pressure for different bandwidths, smoothing and extrapolating to zero bandwidth
Furthermore, we conducted placebo tests using so-called falsified outcomes that could not have been affected by hypertension screening in 2011-12. Specifically, we analysed the impact of hypertension screening in the 2011-12 wave on systolic and diastolic blood pressure in 2008 instead of in 2014. We found no impacts in these placebo tests, which confirms that intervention assignment was exogenous (see supplementary material E).
Discussion
We found that community based screening for hypertension among adults aged 65 years and older in China resulted in a large and statistically significant reduction in systolic blood pressure two years later. The lowering impact of screening on diastolic blood pressure was smaller and imprecisely estimated. These results were robust when covariates were included, different functional forms were used to estimate the impacts, and the size of the bandwidth around the clinical threshold was changed. The results did not vary by demographic and social subgroups.
Large reduction in systolic blood pressure
Across all main analyses, the reduction in systolic blood pressure ranged from 6 to 16 mm Hg, which is a large reduction in systolic blood pressure for an intervention conducted at the community level. A recent study that also used the Chinese Longitudinal Healthy Longevity Survey as the data source provides a powerful benchmark for our results.28 This study found that a 10 mm Hg reduction in systolic blood pressure corresponded to an 11% decrease in cardiovascular mortality among older people in China. These results highlight the clinical and population health relevance of the impact of community based blood pressure screening.
As has been shown previously, lack of awareness is a major obstacle to successfully reducing hypertension at the population level in China.4 The impact of the intervention on systolic blood pressure could have resulted from several behavioural changes. In analyses of lifestyle changes that are downstream from the intervention but upstream from blood pressure, we found evidence that the intervention might have resulted in substantial weight loss, reduced smoking, and lower alcohol intake. However, the consumption of salt preserved vegetables, fresh vegetables, fresh fruits, meat, and sugar appear to have been largely unaffected by the intervention. Against our initial expectations, we found that the intervention might have resulted in less, rather than more, exercise. One possible explanation for this finding is that the media in China often recommends against high intensity exercise for older people with hypertension.29 30 31 32 Overall, our analyses of mechanisms lacked the power to firmly establish the significance of intervention effects on individual lifestyles and behaviours. Moreover, our data did not contain information on several potentially important mechanisms of action, including uptake of antihypertensive treatment and stress reduction.
Insignificant reduction in diastolic blood pressure
Community based blood pressure screening had only small and insignificant impact on diastolic blood pressure. One possible reason for this finding is that field workers might have provided less encouragement for people with raised diastolic blood pressure to seek care and change behaviours compared with those with raised systolic blood pressure. Based on the evidence of a stronger link between systolic blood pressure and cardiovascular disease endpoints,33 the Chinese guidelines for management of hypertension place greater emphasis on systolic blood pressure. For example, the guidelines state that systolic blood pressure is more tightly associated with cardiovascular diseases than diastolic blood pressure and that systolic blood pressure is a more powerful predictor of coronary heart disease among older adults than diastolic blood pressure.15 Furthermore, recommendations for adults older than 65 years only specify targets for systolic blood pressure. It is thus plausible that the field workers provided greater encouragement for treatment uptake and behaviour change to address raised systolic blood pressure compared with raised diastolic blood pressure.
Comparison with published evidence
Our results suggest that in China, a large proportion of older adults who had high blood pressure during community based screening adhered to advice to seek antihypertensive care and modify lifestyles. In contrast, many other studies in low and middle income countrieshave found low rates of linkage and adherence to care after household or community based screening. For example, Bovet and colleagues estimated that only 34% of people with hypertension in Tanzania who were advised to seek care actually sought care, and at the end of one year, only 3% were taking antihypertensive drugs.34 Low levels of care seeking and treatment compliance among people with hypertension screened at home and encouraged to seek further care have also been found in Burkina Faso,35 Kenya,36 and the Seychelles.37 However, these studies focused on populations that were younger. Our study focuses on older adults and our results suggest that behaviour change played a part in reducing systolic blood pressure in this population.
Health policy implications
According to our results, community based screening should be routinely offered to older adults in China because it could substantially reduce hypertension at the population level. This recommendation does not imply, however, that the impact of community based screening could not be further improved. Evidence from China and previous studies in other low and middle income countries show a large potential to enhance the effectiveness of community based screening interventions on blood pressure outcomes. One study in China found that only 67% of people who were aware of their hypertension reported regularly receiving treatment and only 16% had successfully controlled their hypertension.4 Possible avenues for intervention improvement include intensified training of healthcare workers who conduct screening interventions, increased standardisation of recommendations on behaviour change, and additional tools to communicate the need for treatment and behaviour change at the population level (such as interactive eHealth applications38 39 or health promotion videos40). In addition, interventions dealing with gaps at higher levels of the health system might also contribute to the effectiveness of community based hypertension screening programmes. These interventions include structured physician education programmes focused on hypertension, and encouragement of systematic and frequent blood pressure screening in patients who visit clinics for unrelated reasons.3 4 Intervention studies that combine community based screening with health system changes that improve linkage and retention in primary care might result in greater impacts than those shown in this study.41 Further research to identify how to maximise the impact of community and household based screening will be important for translating these interventions into sustained population level health improvements.42 43 44 Policy makers should consider piloting, evaluating, and scaling up interventions that strengthen community based blood pressure screening and the downstream hypertension care continuum.
Limitations
Our study has several limitations. We only had data on adults aged 65 years and older; therefore we could not conclude that the intervention would also have been effective in younger adults. Because our data were limited to two waves of a national cohort, we were unable to estimate the timelines of impact or to determine impact beyond the two year time horizon of our analysis. Additionally, the success of community based hypertension screening could depend on other factors, such as use of healthcare and adherence to antihypertensive drugs. We did not have data on antihypertensive treatment uptake and were thus unable to analyse the extent to which treatment contributed to our findings.
The Chinese Longitudinal Healthy Longevity Survey randomly samples people aged 65 years and older in China. However, different age, sex, and urban versus rural location groups are sampled with different probabilities. In our regression with covariates, we take into account this differential weighting across subpopulations by controlling for the three variables that define the groups. In general, our impact size results are thus generalisable to the population aged 65 years and older in China. However, this study provides impact estimates only for those within the analysed bandwidths around the threshold for the regression discontinuity analyses. This external validity constraint is a general limitation of the regression discontinuity design. Nevertheless, the hypertension threshold was arbitrary (it did not correspond to an underlying jump in cardiovascular disease risk or any physiological event that occurs at this threshold) and blood pressure was measured with random variation over time and random measurement error from the blood pressure monitor. Our results remained robust to changes in the regression discontinuity bandwidth. Therefore, our results will probably be transferable to population groups further away from the threshold.17 19 45 46
Conclusions
Community based hypertension screening and encouraging people with raised blood pressure to seek care and adopt blood pressure lowering behaviour changes could have important long term impact on systolic blood pressure at the population level. Policy makers should consider implementing routine community based hypertension screening programmes for older adults in China and other countries with an unmet need for hypertension diagnosis and care.
What is already known on this topic
Studies have found low levels of healthcare use after community based blood pressure screening
Evidence is lacking about the causal impact of community based blood pressure screening on subsequent blood pressure in China and other low and middle income countries
What this study adds
This study found that community based hypertension screening reduced systolic blood pressure two years later among older adults in China
Measuring blood pressure during home visits and encouraging people with raised blood pressure to seek care and adopt blood pressure lowering behaviour changes could have important long term impact on systolic blood pressure at the population level
This approach could address the high burden of cardiovascular diseases in China and other countries with an unmet need for hypertension diagnosis and care
Acknowledgments
We thank staff at the provincial and county Centres for Disease Control and Prevention for giving us detailed information on the survey and fieldwork.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary material
Contributors: SC and NS are first authors. PG and TB are senior authors. SC, TB, and PG contributed to the study concept and design. SC conducted data analysis and wrote the first draft of the manuscript. SC, NS, PG, and TB contributed to literature review and the interpretation of the data. NS, FH, YL, PG, and TB critically revised the manuscript for important intellectual content. All authors approved the final version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. SC and TB are the guarantors.
Funding: This study received no specific funding.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; TB is supported by the Alexander von Humboldt Foundation through the Alexander von Humboldt Professor award, funded by the German Federal Ministry of Education and Research; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study used only publicly available, deidentified data. The underlying national cohort study was approved by the biomedical ethics committee of Peking University (IRB00001052-13074), and all participants or their proxy respondents provided written informed consent.
Data sharing: No additional data available.
The lead author (SC) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1. Institute for Health Metrics and Evaluation Global burden of disease study 2016 (GBD 2016) Results. Institute for Health Metrics and Evaluation, 2016. [Google Scholar]
- 2. Lacey B, Lewington S, Clarke R, et al. China Kadoorie Biobank collaborative group Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0·5 million adults in China: a prospective cohort study. Lancet Glob Health 2018;6:e641-9. 10.1016/S2214-109X(18)30217-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Li Y, Yang L, Wang L, et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol 2017;227:516-23. 10.1016/j.ijcard.2016.10.110 [DOI] [PubMed] [Google Scholar]
- 4. Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 2017;390:2549-58. 10.1016/S0140-6736(17)32478-9 [DOI] [PubMed] [Google Scholar]
- 5. Bloom DE, Chen S, Kuhn M, et al. The economic burden of chronic diseases: estimates and projections for China, Japan, and South Korea. J Econ Ageing 2018. 10.1016/j.jeoa.2018.09.002. [DOI] [Google Scholar]
- 6. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957-67. 10.1016/S0140-6736(15)01225-8 [DOI] [PubMed] [Google Scholar]
- 7. Bundy JD, Li C, Stuchlik P, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol 2017;2:775-81. 10.1001/jamacardio.2017.1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gu D, He J, Coxson PG, et al. The cost-effectiveness of low-cost essential antihypertensive medicines for hypertension control in China: a modelling study. PLoS Med 2015;12:e1001860. 10.1371/journal.pmed.1001860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhang L, Zuo L, Xu G, et al. Community-based screening for chronic kidney disease among populations older than 40 years in Beijing. Nephrol Dial Transplant 2007;22:1093-9. 10.1093/ndt/gfl763 [DOI] [PubMed] [Google Scholar]
- 10. Gong Y, Peng P, Bao P, et al. The implementation and first-round results of a community-based colorectal cancer screening program in Shanghai, China. Oncologist 2018;23:928-35. 10.1634/theoncologist.2017-0451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yi Z. Introduction to the Chinese Longitudinal Healthy Longevity Survey (CLHLS). Healthy longevity in China. Springer, 2008: 23-38. [Google Scholar]
- 12. Gu D. General data quality assessment of the CLHLS. Healthy longevity in China. Springer, 2008: 39-60 10.1007/978-1-4020-6752-5_3. [DOI] [Google Scholar]
- 13. Yi Z, Vaupel JW, Zhenyu X, et al. Sociodemographic and health profiles of the oldest old in China. Popul Dev Rev 2002;28:251-73 10.1111/j.1728-4457.2002.00251.x. [DOI] [Google Scholar]
- 14.Duke University The Center for the Study of Aging and Human Development. Chinese Longitudinal Healthy Longevity Survey (CLHLS) 2018. https://sites.duke.edu/centerforaging/programs/chinese-longitudinal-healthy-longevity-survey-clhls/.
- 15. Liu LS, Writing Group of 2010 Chinese Guidelines for the Management of Hypertension [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi 2011;39:579-615. [PubMed] [Google Scholar]
- 16. Zeng Y, Feng Q, Hesketh T, Christensen K, Vaupel JW. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet 2017;389:1619-29. 10.1016/S0140-6736(17)30548-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bor J, Moscoe E, Mutevedzi P, Newell ML, Bärnighausen T. Regression discontinuity designs in epidemiology: causal inference without randomized trials. Epidemiology 2014;25:729-37. 10.1097/EDE.0000000000000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Imbens GW, Lemieux T. Regression discontinuity designs: A guide to practice. J Econom 2008;142:615-35. 10.1016/j.jeconom.2007.05.001. [DOI] [Google Scholar]
- 19. Moscoe E, Bor J, Bärnighausen T. Regression discontinuity designs are underutilized in medicine, epidemiology, and public health: a review of current and best practice. J Clin Epidemiol 2015;68:122-33. 10.1016/j.jclinepi.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 20. Wang J-G. Chinese hypertension guidelines. Pulse (Basel) 2015;3:14-20. 10.1159/000382025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McCrary J. Manipulation of the running variable in the regression discontinuity design: A density test. J Econom 2008;142:698-714 10.1016/j.jeconom.2007.05.005. [DOI] [Google Scholar]
- 22. Lee DS, Moretti E, Butler MJ. Do voters affect or elect policies? Evidence from the US House. Q J Econ 2004;119:807-59 10.1162/0033553041502153. [DOI] [Google Scholar]
- 23. Lee DS, Lemieux T. Regression discontinuity designs in economics. J Econ Lit 2010;48:281-355 10.1257/jel.48.2.281. [DOI] [Google Scholar]
- 24.Imbens G, Wooldridge J. “What’s New in Econometrics” Lecture 3: NBER 2007. http://www.nber.org/WNE/slides_3_rd7-30-07.pdf
- 25. Gelman A, Imbens G. Why high-order polynomials should not be used in regression discontinuity designs. J Bus Econ Stat 2018. 10.1080/07350015.2017.1366909. [DOI] [Google Scholar]
- 26. Imbens G, Kalyanaraman K. Optimal bandwidth choice for the regression discontinuity estimator. Rev Econ Stud 2012;79:933-59 10.1093/restud/rdr043. [DOI] [Google Scholar]
- 27. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702-6. 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 28. Lv Y-B, Gao X, Yin Z-X, et al. Revisiting the association of blood pressure with mortality in oldest old people in China: community based, longitudinal prospective study. BMJ 2018;361:k2158. 10.1136/bmj.k2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.CCTV.com. [Elderly exercising, you need to know these fatal risks] 2016. http://jiankang.cctv.com/2016/12/14/ARTIUeIHMHCLqaRuz2B5zwcc161214.shtml accessed 7 March 2019.
- 30.health.people.cn. [Don’t overexert yourself when exercising! Middle-aged and the elderly need to know these fatal risks] 2016. http://health.people.com.cn/n1/2016/1213/c14739-28944620.html accessed 7 March 2019.
- 31.Familydoctor.com. [What kind of exercise is suitable for elderly people with hypertension?] 2013 http://ksjk.familydoctor.com.cn/a/201310/530067.html.
- 32.Sohu Health. [Exercise therapy for high blood pressure, eight issues to be aware of]. 2007 http://health.sohu.com/20070917/n252200129.shtml accessed 7 March 2019.
- 33. Izzo JL, Jr, Levy D, Black HR. Clinical Advisory Statement. Importance of systolic blood pressure in older Americans. Hypertension 2000;35:1021-4. 10.1161/01.HYP.35.5.1021 [DOI] [PubMed] [Google Scholar]
- 34. Bovet P, Gervasoni J-P, Mkamba M, Balampama M, Lengeler C, Paccaud F. Low utilization of health care services following screening for hypertension in Dar es Salaam (Tanzania): a prospective population-based study. BMC Public Health 2008;8:407. 10.1186/1471-2458-8-407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Doulougou B, Kouanda S, Ouédraogo GH, Meda BI, Bado A, Zunzunegui MV. Awareness, treatment, control of hypertension and utilization of health care services following screening in the North-central region of Burkina Faso. Pan Afr Med J 2014;19:259. 10.11604/pamj.2014.19.259.4707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Oti SO, van de Vijver S, Gomez GB, et al. Outcomes and costs of implementing a community-based intervention for hypertension in an urban slum in Kenya. Bull World Health Organ 2016;94:501-9. 10.2471/BLT.15.156513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bovet P, Burnier M, Madeleine G, Waeber B, Paccaud F. Monitoring one-year compliance to antihypertension medication in the Seychelles. Bull World Health Organ 2002;80:33-9. [PMC free article] [PubMed] [Google Scholar]
- 38. Norman GJ, Zabinski MF, Adams MA, et al. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med 2007;33:336-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Jacobs RJ, Lou JQ, Ownby RL, Caballero J. A systematic review of eHealth interventions to improve health literacy. Health Informatics J 2016;22:81-98. 10.1177/1460458214534092 [DOI] [PubMed] [Google Scholar]
- 40. Tuong W, Larsen ER, Armstrong AW. Videos to influence: a systematic review of effectiveness of video-based education in modifying health behaviors. J Behav Med 2014;37:218-33. 10.1007/s10865-012-9480-7 [DOI] [PubMed] [Google Scholar]
- 41. Bovet P, Chiolero A, Paccaud F, Banatvala N. Screening for cardiovascular disease risk and subsequent management in low and middle income countries: challenges and opportunities. Public Health Rev 2015;36:13. 10.1186/s40985-015-0013-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kotwani P, Balzer L, Kwarisiima D, et al. SEARCH Collaboration Evaluating linkage to care for hypertension after community-based screening in rural Uganda. Trop Med Int Health 2014;19:459-68. 10.1111/tmi.12273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. van de Vijver S, Oti SO, Gomez GB, et al. Impact evaluation of a community-based intervention for prevention of cardiovascular diseases in the slums of Nairobi: the SCALE-UP study. Glob Health Action 2016;9:30922. 10.3402/gha.v9.30922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pennant M, Davenport C, Bayliss S, Greenheld W, Marshall T, Hyde C. Community programs for the prevention of cardiovascular disease: a systematic review. Am J Epidemiol 2010;172:501-16. 10.1093/aje/kwq171 [DOI] [PubMed] [Google Scholar]
- 45. Cook TD, Shadish WR, Wong VC. Three conditions under which experiments and observational studies produce comparable causal estimates: New findings from within-study comparisons. J Policy Anal Manage 2008;27:724-50. 10.1002/pam.20375. [DOI] [Google Scholar]
- 46. Green DP, Leong TY, Kern HL, et al. Testing the accuracy of regression discontinuity analysis using experimental benchmarks. Polit Anal 2009;17:400-17 10.1093/pan/mpp018. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary material


