Abstract
Objective
Benign fibroepithelial lesions (BFL) lesions of the breast are various and predominantly benign, although a few can be locally aggressive. Definitive diagnosis of some BFL can be challenging from core needle biopsy (CNB). Radiological findings can help guide the management of the lesions. The aim of this study was to investigate the accuracy rate of CNB results and evaluate the radiological findings of the most common BFL according to the final excision pathology results. The secondary aim was to assess the contribution of the imaging findings to CNB results.
Materials and Methods
A retrospective review was made of 266 patients diagnosed with suspicious BFL, conventional fibroadenoma, complex fibroadenoma, cellular fibroadenoma and benign phyllodes tumor (PT). The study included 132 patients who underwent surgical excision. The radiological and histopathological findings were evaluated.
Results
While 66 patients were diagnosed with more descriptive results on CNB, the other 66 patients were diagnosed with suspicious BFL. Agreement between CNB and excisional pathology was good, when CNB provided a definite diagnosis. While conventional and complex fibroadenoma were observed to have hypo or normal vascularity, cellular fibroadenoma and PT showed hypervascularity. Oval shaped and homogeneous internal echo pattern were significantly associated with conventional fibroadenoma. A heterogeneous internal echo pattern was seen in complex fibroadenomas and PT.
Conclusion
CNB often reaches the correct diagnosis alone when it gives a definite diagnosis. The radiological findings which help in the differentiation of BFL are hypervascularity, oval shape and internal heterogeneity. More accurate results can be obtained when histopathological and radiological findings are evaluated together.
Keywords: Benign fibroepithelial lesions, fibroadenoma, phyllodes tumor, histopathological findings, radiological findings
Introduction
Benign fibroepithelial lesions (BFL) of the breast are characterized by proliferation of both epithelial and stromal components. BFL are various and predominantly benign, although a small percentage can be locally aggressive (1). Fibroadenoma is the most common benign neoplasm among BFL. Fibroadenomas have variants including cellular and complex fibroadenoma. Complex fibroadenoma is a variant of the fibroadenoma harboring at least 1 of the following features: sclerosing adenosis, cysts, papillary apocrine metaplasia and epithelial calcifications. Cellular fibroadenoma is another variant of fibroadenoma with remarkable cellularity. These different characteristics of fibroadenoma can cause misdiagnosis histopathologically (2–4).
To distinguish between fibroadenoma and phyllodes tumor (PT) is clinically important due to different clinical management. While fibroadenomas can be followed up safely with conservative methods, surgical excision is recommended for PT. Definitive diagnosis of some of the BFL can be challenging from core needle biopsy (CNB) due to increased cellularity and complex structures. They can be upstaged to phyllodes tumor on excision pathology (5). If there is histopathological uncertainty, the World Health Organization working group proposes using the term of benign fibroepithelial neoplasm in order to avoid overtreatment (6, 7). On the other hand, National Comprehensive Cancer Network guidelines suggest excisional biopsy for palpable, large (>3 cm) and rapid growing lesions which are diagnosed as fibroadenoma or are indeterminate on CNB (8).
There can also be overlapping findings in the radiological diagnosis of BFL (9). However, more accurate results can be obtained when histopathological and radiological findings are evaluated together. The main aim of this study was to investigate the accuracy rate of CNB results and to evaluate the radiological findings of the most common BFL according to the final excision pathology results. The secondary aim of the study was to assess the contribution of the imaging findings to CNB results.
Material and Methods
Approval for the study was granted by the Hacettepe University Ethics Commission. Informed consent was not taken due to the retrospective nature of the study.
Patients
A retrospective review was made of 266 patients diagnosed with BFL on CNB between January 2014 and June 2018. The study included 132 patients who underwent surgical excision with a diagnosis of conventional fibroadenoma, complex fibroadenoma, cellular fibroadenoma and benign PT. As the excisional pathology results are gold standard in the diagnosis of the BFL, we excluded the 121 patients who did not undergo surgical excision. There were only 5 patients diagnosed with borderline and malignant PT. We excluded the borderline and malignant PT, because of the limited number and more aggressive nature of these lesions. Uncommon BFL including pseudoangiomatous stromal hyperplasia, lactating adenoma, adenomyoepithelioma and tubular adenoma were also excluded due to lower numbers. The total number of these patients was 8.
The patients diagnosed with suspicious fibroepithelial lesion and PT in CNB and the patients categorized as BIRADS 4B and 4C underwent surgical excision. 26 patients underwent excisional surgery due to positive family history or their own request.
Imaging
All patients underwent ultrasonography (US), 45 patients had mammography and only 8 patients had magnetic resonance imaging (MRI).
The US images were obtained using a 12 MHz linear probe on a Toshiba Aplio 400 device (Toshiba Medical Systems Corporation, Otawara, Japan). For the mammograms, standard mediolateral oblique and craniocaudal images were obtained using Seno essential mammography systems (General Electric, USA). The MRI scans were acquired with the patient in the prone position in a 1.5-Tesla MRI scanner (Signa HD, GE Medical Systems, USA) using a four-channel phased array breast coil. The imaging protocol included the following sequences: axial T2-weighted fat saturated (TR/TE 5100/90 ms, slice thickness=2 mm, flip angle 90°, matrix 256×256), axial echo-planar DWI (TR/TE 2500/72, slice thickness=3 mm, matrix 256 × 256, diffusion gradient with b values of 0 and 500 s/mm2), and axial T1-weighted fast spin echo pre-contrast MR images (TR/TE 4.3/2.1 ms, slice thickness=2 mm, flip angle 90°, matrix 512×512). Dynamic breast examination was performed after the injection of intravenous contrast material (Magnevist, Bayer Schering Pharma AG, Berlin, Germany) through the antecubital vein at a dose of 0.1 mmol/kg using a power injector (Medrad, Bayer HealthCare, Netherlands). After pre-contrast T1-weighted images, the following 5 axial T1-weighted post-contrast dynamic sequences (TR/TE 4.5/2.1 ms, slice thickness=2 mm, flip angle 10°, matrix 512×512) were obtained at intervals of 90 seconds.
Pathological examination
The patients with suspicious histopathological or radiological findings underwent surgical excision. Some patients underwent surgery due to family history and their own request for surgery, although the CNB pathology results and radiological findings were benign.
All CNBs were performed under US guidance using a 14-gauge cutting needle. All needle biopsies were performed using an automated biopsy gun and at least 4 core specimens were obtained from each lesion.
The pathological reports were reviewed. The lesions with a final pathological diagnosis of conventional fibroadenoma, complex fibroadenoma, cellular fibroadenoma and benign PT were assessed.
Statistical Analysis
Mean and standard deviation were presented for continuous variables; number and proportion were presented for categorical variables. Yates’ Chi-square test or Fisher Exact tests were used to examine the relationship between two categorical variables. The Kappa coefficient was obtained to assess the agreement between CNB and excisional pathology results.
A p value of 0.05 was accepted as statistically significant. Data analysis was performed by Statistical Package for the Social Sciences version 23.0 (IBM Corp., Armonk, NY, USA) software package.
Results
Clinical and histopathological data
The mean age of patients was 41±10 years and the mean size of the lesions was 19±11mm.
While 66 patients were diagnosed with more descriptive results as conventional fibroadenoma, complex fibroadenoma, cellular fibroadenoma, benign phyllodes on CNB, the other 66 patients were diagnosed with suspicious BFL and excision was recommended. According to the excisional pathological results, the numbers of conventional fibroadenoma, complex fibroadenoma, cellular fibroadenoma and benign PT were 64 (48.5%), 24 (18.2%), 12 (9%) and 32 (24.3%), respectively.
Although all patients diagnosed with cellular fibroadenoma were under 35 years of age, there was no statistical significance between the types of BFL and age (p=0.5) Lesion size was larger in PT than in the other BFL, but not at a level of statistical significance (p=0.3).
Radiological findings
The radiological characteristics of the lesions are shown in Table 1. Most lesions had an oval shape (75%), circumscribed margin (53%), homogeneous internal echo pattern (62.1%), hypo or normal vascularity (75.8%) and were BI-RADS 4A (85.6%) category. There was no statistically significant difference between types of BFL and the features of the margins (p=0.6), size increase (p=0.4) and BI-RADS category (p=0.3). There was no relationship between the types of BFL and MRI, and mammography findings (p>0.05 for all findings).
Table 1.
Imaging characteristics of lesions
| Radiological Findings | n (%) |
|---|---|
| Ultrasound Features | |
| Shape | |
| Oval | 99 (75.0) |
| Round | 24 (18.1) |
| Irregular | 9 (6.8) |
| Margins | |
| Circumscribed | 70 (53.0) |
| Microlobulated | 48 (36.4) |
| Indistinct | 14 (10.6) |
| Internal echo pattern | |
| Homogeneous | 82 (62.1) |
| Heterogenous | 50 (37.9) |
| Vascularity | |
| Hypovascular and normal vascularity | 100 (75.8) |
| Hypervascular | 32 (24.2) |
| Size increase | 33 (25) |
| Mammography Features | |
| Patients underwent mammography | 45 (34) |
| No features on mammography | 15 (33.3) |
| Asymmetric density | 5 (11.1) |
| Mass | 25 (55.5) |
| Calcification within the lesion | 2 (4.4) |
| MRI Features | |
| Patients underwent MRI | 8 (6.0) |
| Type 1 dynamic curve | 5 (62.5) |
| Type 2 and type 3 dynamic curve | 3 (37.5) |
| Homogeneous contrast enhancement | 6 (75) |
| Heterogenous contrast enhancement | 2(25) |
| BI-RADS | |
| BI-RADS 4A | 113 (85.6) |
| BI-RADS 4B | 17 (12.9) |
| BI-RADS 4C | 2 (1.5) |
MRI: magnetic resonance imaging; BI-RADS: breast imaging reporting and data system
We analysed BIRADS category and pathology results. From 113 lesions reported as BIRADS 4A category, 58 lesions diagnosed with suspicious fibroepithelial lesion and 29 lesions diagnosed with PT in CNB. The other 26 patients underwent to the excisional surgery due to positive family history or their own request. From 17 lesions reported as BIRADS 4B category, 7 lesions diagnosed with suspicious fibroepithelial lesion and 4 lesions diagnosed with PT on core needle biopsy. There were only 2 patients categorized as BIRADS 4C. And from these two patients, one was reported as suspicious fibroepithelial lesion while the other one was reported as complex fibroadenoma.
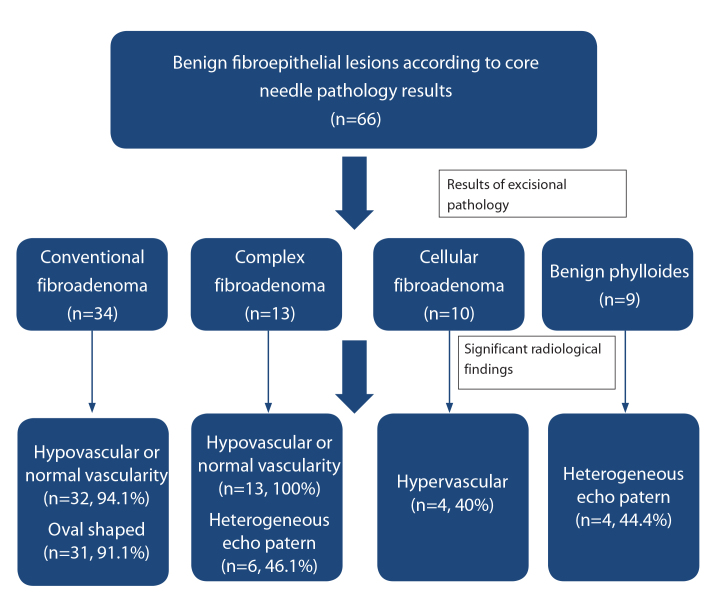
While conventional and complex fibroadenoma have hypo or normal vascularity, cellular fibroadenoma and PT show hypervascularity on Doppler ultrasonography (p=0.0001). An oval shape (85.9%) and homogeneous internal echo pattern (57%) are significantly associated with conventional fibroadenoma (p=0.002 for shape, p=0.001 for internal echo pattern). A heterogeneous internal echo pattern is seen in complex fibroadenomas (62.5%) and PT (68.8%) (p=0.001). The significant radiological findings of BFL are shown in Table 2 and Figure 1.
Table 2.
The significant ultrasonography findings of benign fibroepithelial lesions are given with their percentages
| Shape/(%)/p | Internal echo patern/(%)/p | Vascularity/(%)/p | |
|---|---|---|---|
| Conventional fibroadenoma (n=64) | Oval/(85.9)/0.002 | Homogeneous/(57)/0.001 | Hypovascular or normal/(9.8)/0.0001 |
| Complex fibroadenoma(n=24) | Oval/(62.5)/0.1 | Heterogeneous/(62.5)/0.001 | Hypovascular or normal/(95.8)/0.0001 |
| Cellular fibroadenoma(n=12) | Oval/(75)/0.1 | Homogeneous/(50)/0.3 | Hypervascularity/(75)/0.0001 |
| Benign phyllodes(n=32) | Oval/(62.5)/0.1 | Heterogenous/(68.8)/0.001 | Hypervascularity/(56.3)/0.0001 |
Figure 1. a–d.
Oval shaped and homogeneous internal echo pattern benign fibroepithelial lesions diagnosed with conventional fibroadenoma is shown in US (a). US shows small solid lesion with heterogeneous internal echo pattern due to the millimetric cyst. It was diagnosed as complex fibroadenoma histopathologically (b). Doppler US demonstrates hypervascularity within the cellular fibroadenoma (c). Heterogenous solid lesion diagnosed with phyllodes tumor is shown in US (d).
Agreement between CNB and excisional biopsy
Agreement between CNB and excisional pathology was good (kappa=0.641 p<0.001). Agreement was evaluated in 66 patients who got a definite diagnosis in CNB and underwent surgical excision. Table 3 shows the agreement in detail.
Table 3.
Agreement between core needle biopsy and excisional pathology
| Excisional Pathology Results | Benign phyllodesn (%) | ||||
|---|---|---|---|---|---|
| Conventional fibroadenoma n (%) |
Complex fibroadenoma n (%) |
Cellular fibroadenoma n (%) |
|||
| Core Needle | Conventional fibroadenoma (%) | 19 (63.3) | 1 (9.1) | 0 (0) | 1 (4.3) |
| Biopsy Results | Complex fibroadenoma (%) | 1 (3.3) | 9 (81.8) | 0 (0) | 0 (0) |
| Cellular fibroadenoma (%) | 0 (0) | 0 (0) | 1 (50) | 1 (4.3) | |
| Benign phyllodes (%) | 10 (30.4) | 1 (9.1) | 1 (50) | 21 (91.4) | |
| Total n (%) | 30 (100) | 11 (100) | 2 (100) | 23 (100) | |
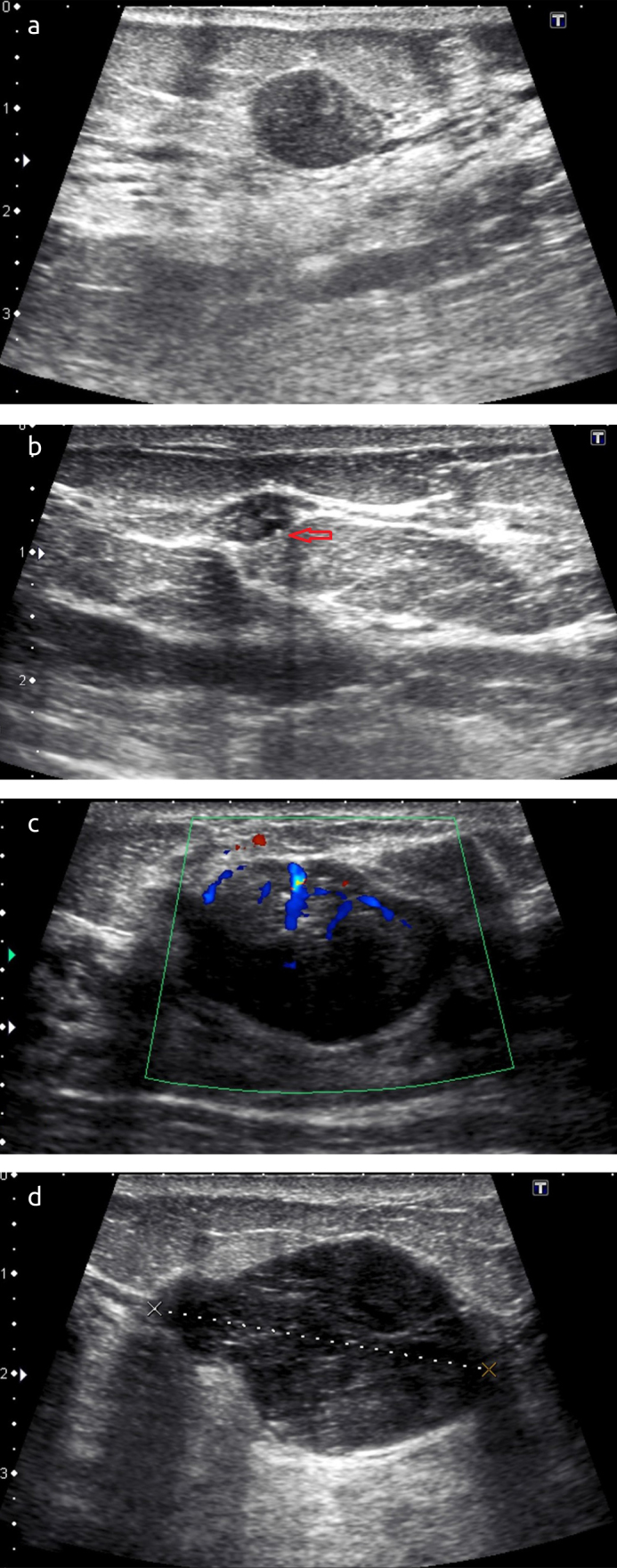
Evaluation of core needle biopsy results with radiological findings
From 32 patients with diagnosed with PT accordingly to excisional pathology result, 21 patients got correct diagnosis in CNB at the rate of 65.6%. When statistically significant radiological findings including hypervascularity and heterogeneous internal echo pattern were added to CNB findings, additional 7 patients got accurate diagnosis although CNB could not give exact correct diagnosis. So, accuracy rate of diagnosis PT increased to 87.5% (Figure 2).
Figure 2.
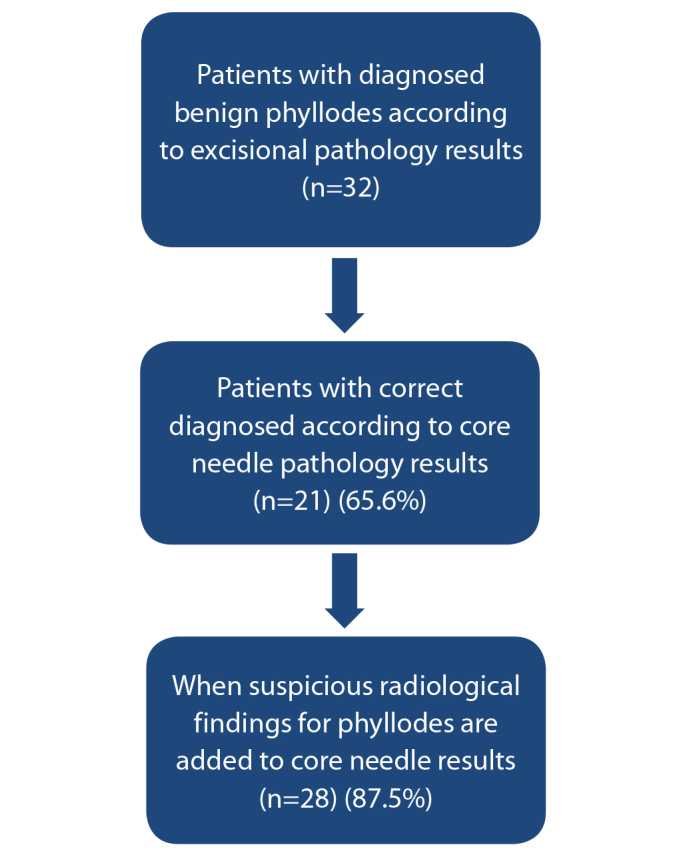
The diagram shows evaluation of core needle biopsy results with radiological findings in phyllodes tumors
Half of the patients were diagnosed with a suspicious BFL on CNB. Figure 3 shows the excisional pathology results and the percentages of significant radiology features of the patients who could not be definitively diagnosed from CNB.
Figure 3.
The diagram demonstrates the excisional pathology results and the percentages of significant radiology features of the patients who could not get definite diagnosis on CNB
Discussion and Conclusion
The major findings of the current study are that first, CNB often reaches the correct diagnosis alone, when it gives a definite diagnosis. Second, radiological findings including oval shape, presence of vascularity and internal echogenicity of the lesions can help in the diagnosis of BFL (p<0.05). Finally, when the radiological findings and CNB are evaluated together, more accurate results can be provided than by separate evaluation.
Benign fibroepithelial lesions encompass a heterogeneous group of neoplasms exhibiting epithelial and stromal proliferation. Although most BFL are conventional fibroadenoma, PT and subtypes of fibroadenoma including cellular fibroadenoma, complex fibroadenoma are other common BFL (1, 2). Awareness of the different BFL is important because of the requirement for different management. However, the evaluation of BFL in CNB is challenging because of their heterogeneous nature. In PT, areas with marked overgrowth and stromal cellularity with leaflike stromal fronds may be present only as minor foci within a seemingly fibroadenoma. And insufficient samples including torn-cracked samples prevent the accurate diagnosis in CNB. So, adequate samples with additional sampling of the areas showing heterogeneous internal echo on US may help in diagnosis of BFL in CNB. In the current study, the agreement between CNB and excisional pathology was good, if CNB provided a definite diagnosis (kappa=0.641 p<0.001) but the CNB diagnosis was of a suspicious BFL without a definitive diagnosis in half of the patients. And, also according to the results of current study, the core biopsy showed an overestimation. Because only 2 benign phyllodes tumor were reported as fibroadenoma, while 12 fibroadenomas were reported as benign phyllodes in core needle biopsy.
In CNB, the lesion most frequently misdiagnosed as PT is cellular fibroadenoma due to its increased stromal cellularity. Cellular fibroadenoma is usually seen in young women and surgical excision is recommended because of the larger size (10). In the current study, all the patients diagnosed with cellular fibroadenoma were younger than 35 years old. Nevertheless, no statistical relationship was determined between age and cellular fibroadenoma, which could be attributed to an insufficient number of patients. Furthermore, the accuracy of the CNB results could not be optimally evaluated due to surgical excision of most of the cellular fibroadenomas without preoperative CNB.
Complex fibroadenoma is another variant of fibroadenoma harboring one or more complex features. Previous studies have shown that complex fibroadenomas are usually smaller than other BFL and are seen in older patients (3, 4). However, in this study, no statistical significance could be determined between subtypes of BFL and age, or size. PT is usually seen in older patients than simple fibroadenomas such as complex fibroadenoma (11, 12). According to the current study results, CNB often gives the diagnosis of complex fibroadenoma and PT correctly. Evaluation of the age, size and radiological findings together may help in the diagnosis of suspicious BFL in CNB. And when there is a radio-pathological discordance, second look US and re-biopsy can be performed.
Most of the lesions in this study were categorized as BI-RADS 4A. There was no significant finding among BFL on mammography and MRI. This was probably due to the limited number of patients applied with mammography and MRI. Some previous studies have shown that high density and absence of intratumoral calcification were associated with PT on mammography (9, 13, 14) and other studies have reported that PT and other fibroadenomas could not be precisely differentiated on breast MRI (15, 16). In the current study, the features of margins and size increase could not differentiate benign fibroepithelial lesions from each other, whereas hypervascularity (p=0.0001), internal echo pattern (p=0.001) and shape (p=0.002) were able to help differentiate the different types of BFL. While conventional and complex fibroadenoma have hypo or normal vascularity, cellular fibroadenoma and PT show hypervascularity on Doppler ultrasonography. An oval shape and homogeneous internal echo pattern are significantly associated with conventional fibroadenoma. Moreover, a heterogeneous internal echo pattern is seen in complex fibroadenomas and PT. Similar to the current study results, Duman et al. (16) found hypervascularity to be associated with PT. Increased cellularity in PT and cellular fibroadenoma may be the cause of the hypervascularity seen on Doppler US. The reason for the heterogeneous internal echo pattern in complex fibroadenoma may be the complex pathological nature of it including calcification and cystic changes. Wiratkapun et al. (14) reported that PTs often showed sonographic heterogeneity, similar to the observations of the current study. This can be explained by the presence of cystic changes representing areas of focal necrosis and dilated glands (1).
Although CNB often reaches the correct diagnosis alone, it could not provide a definitive diagnosis in half the patients. When CNB gives a diagnosis of suspicious BFL, close follow-up may be selected in cases of benign radiological findings. Furthermore, when suspicious radiological findings for PT including hypervascularity and internal heterogeneity were added to the results of CNB in the current study, the diagnostic accuracy rate increased from 65.6% to 87.5%.
There are some limitations to this study. First, it was a retrospective study and the radiological findings were only assessed from the recorded images. The retrospective nature of the study limited the determination of US and Doppler US characteristics. Second, the small number of cellular fibroadenoma and the small number of masses evaluated by mammography and MRI limited the statistically significance of the results. Finally, due to the very small number of borderline, malignant PTs and uncommon benign fibroepithelial tumors including pseudoangiomatous stromal hyperplasia, lactating adenoma, adenomyoepithelioma and tubular adenoma, these were not included in the study. Therefore, the range of BFL for which the radiological and histopathological features were evaluated, was limited.
In conclusion, CNB often reaches the correct diagnosis alone when it gives a definite diagnosis (kappa= 0.641 and p<0.001). The radiological findings which can help in the differentiation of BFL are hypervascularity, oval shape and internal heterogeneity. More accurate results can be obtained when histopathological and radiological findings are evaluated together. When the suspicious radiological findings were added to the results of the CNB, the diagnostic accuracy of rate increased from 65.6 % to 87.5 %. The presence of suspicious radiological findings can predict PT, even if CNB results show fibroadenoma or suspicious BFL. Nevertheless, close follow-up may be preferred for cases with benign radiological findings in BFL.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Hacettepe University School of Medicine.
Informed Consent: Informed consent was not received due to the retrospective nature of the study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - G.D., Ö.Ö.; Design - G.D., Ö.Ö.; Supervision - M.G.A., F.D.; Resources - A.A., Ö.Ö.; Materials - K.K., A.A.; Data Collection and/or Processing - J.K., K.K.; Analysis and/or Interpretation - J.K., A.A.; Literature Search - G.D., A.A.; Writing Manuscript - G.D., Ö.Ö.; Critical Review - M.G.A., F.D.; Other - G.D., Ö.Ö.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Lerwill MF. Biphasic lesions of the breast. Semin Diagn Pathol. 2004;21:48–56. doi: 10.1053/j.semdp.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Tan BY, Tan PH. A Diagnostic Approach to Fibroepithelial Breast Lesions. Surg Pathol Clin. 2018;11:17–42. doi: 10.1016/j.path.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 3.Sklair-Levy M, Sella T, Alweiss T, Craciun I, Libson E, Mally B. Incidence and management of complex fibroadenomas. AJR Am J Roentgenol. 2008;190:214–218. doi: 10.2214/AJR.07.2330. [DOI] [PubMed] [Google Scholar]
- 4.Kuijper A, Mommers EC, van der Wall E, van Diest PJ. Histopathology of fibroadenoma of the breast. Am J Clin Pathol. 2001;115:736–742. doi: 10.1309/F523-FMJV-W886-3J38. [DOI] [PubMed] [Google Scholar]
- 5.Marcil G, Wong S, Trabulsi N, Allard-Coutu A, Parsyan A, Omeroglu A, Atinel G, Mesurolle B, Meterissian S. Fibroepithelial breast lesions diagnosed by core needle biopsy demonstrate a moderate rate of upstaging to phyllodes tumors. Am J Surg. 2017;214:318–322. doi: 10.1016/j.amjsurg.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 6.Safayi S, Korn N, Bertram A, Akers RM, Capuco AV, Pratt SL, Ellis S. Myoepithelial cell differentiation markers in prepubertal bovine mammary gland: effect of ovariectomy. J Dairy Sci. 2012;95:2965–2976. doi: 10.3168/jds.2011-4690. [DOI] [PubMed] [Google Scholar]
- 7.Tan BY, Acs G, Apple SK, Badve S, Bleiweiss IJ, Brogi E, Calvo JP, Dabbs DJ, Ellis IO, Eusebi V, Farshid G, Fox SB, Ichihara S, Lakhani SR, Rakha EA, Reis-Filho JS, Richardson AL, Sahin A, Schmitt FC, Schnitt SJ, Siziopikou KP, Soares FA, Tse GM, Vincent-Salomon A, Tan PH. Phyllodes tumours of the breast: a consensus review. Histopathology. 68:5–21. doi: 10.1111/his.12876. 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Comprehensive Cancer Network Guidelines Phyllodes Tumor (Version 2.2017) Available from: URL: https://irp-cdn.multiscreensite.com/85275e7e/files/uploaded/phyllodes%20NCCN-richtlijn%202017_JuYqkeH1QC5mFLITnYCE.pdf.
- 9.Yilmaz E, Sal S, Lebe B. Differentiation of phyllodes tumors versus fibroadenomas. Acta Radiol. 2002;43:34–39. doi: 10.1080/028418502127347619. [DOI] [PubMed] [Google Scholar]
- 10.Edwards T, Jaffer S, Szabo JR, Sonnenblick EB, Margolies LR. Cellular fibroadenoma on Core needle biopsy: management recommendations for the radiologist. Clin Imaging. 2016;40:587–590. doi: 10.1016/j.clinimag.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Guillot E, Couturaud B, Reyal F, Curnier A, Ravinet J, Laé M, Bollet M, Pierga JY, Salmon R, Fitoussi A. Management of phyllodes breast tumors. Breast J. 2011;17:129–137. doi: 10.1111/j.1524-4741.2010.01045.x. [DOI] [PubMed] [Google Scholar]
- 12.Komenaka IK, El-Tamer M, Pile-Spellman E, Hibshoosh H. Core needle biopsy as a diagnostic tool to differentiate phyllodes tumor from fibroadenoma. Arch Surg. 2003;138:987–990. doi: 10.1001/archsurg.138.9.987. [DOI] [PubMed] [Google Scholar]
- 13.Chao TC, Lo YF, Chen SC, Chen MF. Sonographic features of phyllodes tumors of the breast. Ultrasound Obstet Gynecol. 2002;20:64–71. doi: 10.1046/j.1469-0705.2002.00736.x. [DOI] [PubMed] [Google Scholar]
- 14.Wiratkapun C, Piyapan P, Lertsithichai P, Larbcharoensub N. Fibroadenoma versus phyllodes tumor: distinguishing factors in patients diagnosed with fibroepithelial lesions after a core needle biopsy. Diagn Interv Radiol. 2014;20:27–33. doi: 10.5152/dir.2013.13133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wurdinger S, Herzog AB, Fischer DR, Marx C, Raabe G, Schneider A, Kaiser WA. Differentiation of phyllodes breast tumors from fibroadenomas on MRI. AJR Am J Roentgenol. 2005;185:1317–1321. doi: 10.2214/AJR.04.1620. [DOI] [PubMed] [Google Scholar]
- 16.Duman L, Gezer NS, Balci P, Altay C, Basara I, Durak MG, Sevinç AI. Differentiation between Phyllodes Tumors and Fibroadenomas Based on Mammographic Sonographic and MRI Features. Breast Care (Basel) 2016;11:123–127. doi: 10.1159/000444377. [DOI] [PMC free article] [PubMed] [Google Scholar]