ABSTRACT
A 27-year-old male was presented with a decrease in vision in the left eye. Best-corrected visual acuity was 10/10 in the right eye and counting fingers at 2 m in the left eye. On fundus examination, the left optic disc was oedematous and there was a wide yellowish, well-defined placoid lesion between the temporal vascular arcades with mild vitreous inflammation. However, a small yellowish well-defined placoid lesion was detected in the inferior temporal region of the macula in the right eye. He was diagnosed with posterior placoid chorioretinopathy (PPC), papillitis, and neurosyphilis after performing fundus fluorescein angiography, fundus autofluorescence imaging, optical coherence tomography, serology for human immunodeficiency virus (HIV) and syphilis, and cerebrospinal fluid examination. Intravenous penicillin treatment was commenced as soon as the diagnosis was established. Seven days after treatment initiation, lesions were partially regressed. PPC and papillitis are rare manifestations of ocular syphilis. In addition, neurosyphilis may also accompany these manifestations. Therefore, syphilis should be considered in the differential diagnosis of patients who have PPC or papillitis and all patients should be tested for HIV coinfection and neurosyphilis.
KEYWORDS: Human immunodeficiency virus, papillitis, posterior placoid chorioretinopathy, syphilis, uveitis
Introduction
Syphilis is a multisystem chronic infection caused by a spirochete known as Treponema pallidum which is still among the important causes of the sexually transmitted infections.1 Epidemiologic studies indicate that human immunodeficiency virus (HIV) and syphilis can be transmitted together synergistically.2,3 Syphilis is a great mimicker together with the tuberculosis and intraocular lymphoma and may present with a wide variety of ocular symptoms and findings. Syphilis can affect any structure of the eye including sclera-episclera (episcleritis-scleritis)4, cornea (interstitial keratitis)5, iris-ciliary body (iridocyclitis)6, pars plana (intermediate uveitis)7, vitreous (vitritis)8, retinal vasculature (vasculitis)9, retina-choroidea (chorioretinitis)10, optic disc-retina (neuroretinitis)11, and optic disc (papillitis).12 Different studies have reported on fundus examination either PPC or papillitis secondary to syphilis. To our knowledge, this rare combination has not been reported with further imaging modalities such as fundus autofluorescence (FAF), fundus fluorescein angiogram (FA), and optical coherence tomography (OCT). Herein, we reported a rare coexistence of posterior placoid chorioretinopathy (PPC) and papillitis secondary to syphilis-HIV coinfection.
Case report
A 27-year-old male was presented with a visual decline of 5 days’ duration in his left eye. His family and past medical histories were unremarkable and he was not on any medication. He was heterosexual and had multiple casual partners. On examination, the blood pressure and heart rate were 135/75 mmHg and 76 beats/per minute, respectively. External physical and neurological examinations were normal. The pupils were reactive to light and there was a relative afferent pupillary defect in OS. Colour vision with Ishihara pseudoisochromatic plate test was 15/15 in OD and 1/15 in OS. Best-corrected visual acuity was 10/10 in OD and counting fingers at 2 m in OS. While the right anterior segment was normal, there was mild vitritis in OS on slit-lamp examination. Intraocular pressure measured was 11 mmHg OU. On fundus examination, a small yellowish well-defined placoid lesion was detected in the inferior temporal region of the macula in OD (Figure 1(a)). However, there was optic disc oedema and a large yellowish well-defined placoid lesion covering the macula between the temporal vascular arcades with mild vitreous inflammation in OS (Figure 1(b)). FAF revealed spotting hypoautofluorescent and hyperautofluorescent areas corresponding to the retinal lesions (Figure 1(c) and (d)). FA showed optic disc leakage in OS and late staining in the affected area in OU (Figure 1(e) and (f)). The OCT revealed hyperreflective dots, thickening of the outer retinal and retinal pigment epithelial (RPE) layer, loss of the photoreceptor inner segment/outer segment (IS/OS) bands, disruption of the external limiting membrane (ELM) at the macular region and optic disc swelling in OS (Figure 2(a) and (b)). However, there were only hyperreflective dots in OD (Figure 2(c) and (d)). Routine investigations including a full blood count, C-reactive protein level, erythrocyte sedimentation rate, angiotensin-converting enzyme level, and purified protein derivative skin test were within normal limits. Chest X-ray was unremarkable. Autoantibody tests were performed for differential diagnosis of connective tissue and vasculitic diseases [antinuclear antibodies, anti-double-stranded DNA, rheumatoid factor, antineutrophil cytoplasmic antibody, etc.] were all negative. Serologic tests for syphilis [Venereal disease research laboratory, fluorescent treponemal antibody absorption, and treponema pallidum microhemagglutination assay] and HIV [enzyme-linked immunosorbent assays] were positive. Papillitis and PPC were diagnosed secondary to syphilis–HIV coinfection. A consultation was requested from the department of infectious diseases. The patient was diagnosed as neurosyphilis after cerebrospinal fluid examination following the lumbar puncture. Treatment was begun with intravenous penicillin G (24 million units per day for 14 days). He was followed up at regular intervals over the next 2 weeks. Two weeks later, vitreous inflammation and optic disc oedema were partially regressed and the visual acuity in OS was 1/10.
Figure 1.
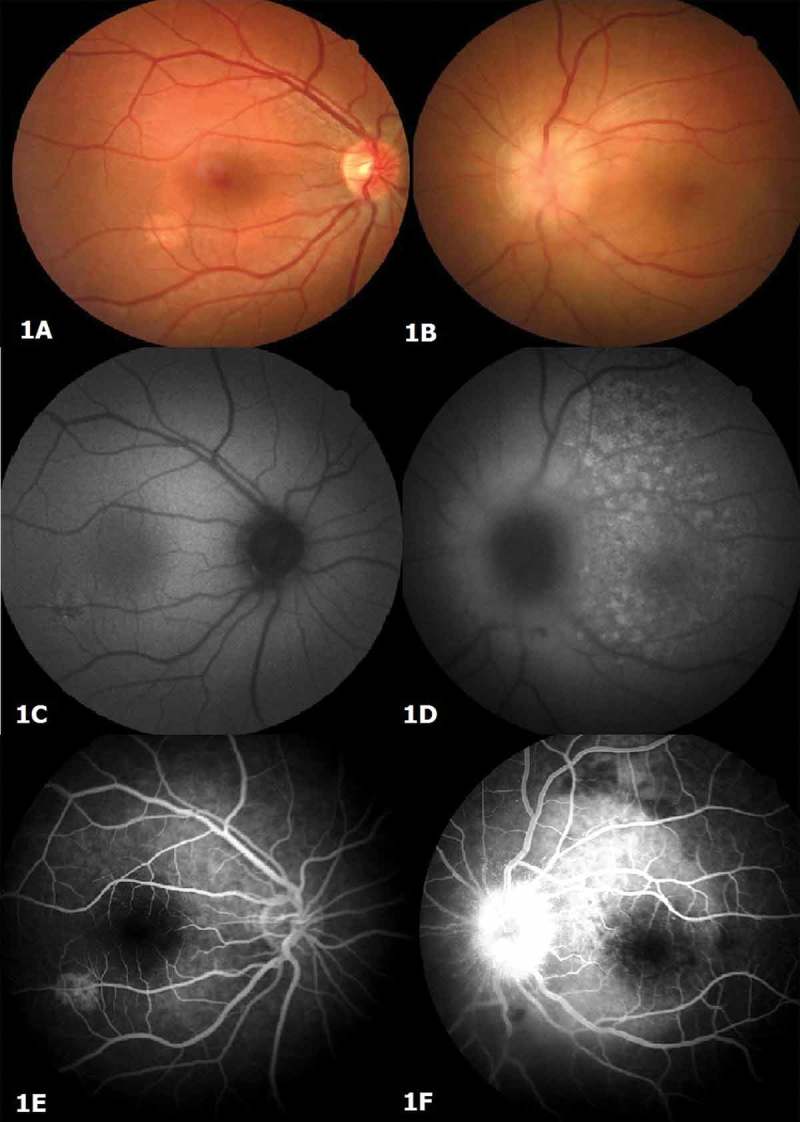
Colour fundus photograph depicting a small, yellowish placoid lesion in the right eye (A), and papillitis and a wide, yellowish placoid lesion between the superotemporal and inferotemporal arcades in the left eye (B). Fundus autofluoresence (hypoautofluorescence and hyperautofluorescence spotting) corresponding to the lesion locations (C, D). Fundus fluorescein angiogram showing left optic disc leakage and bilateral late diffuse staining in the affected area (E, F).
Figure 2.
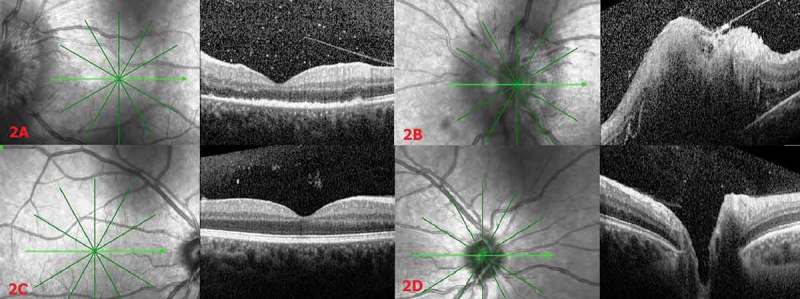
Optical coherence tomography (OCT) scan of the left eye depicting hyperreflective dots, thickening of the outer retinal and the retinal pigment epithelial layer, disruption of the external limiting membrane, and loss of the photoreceptor inner segment/outer segment band at the macular region (A) and optic disc oedema (B). Right OCT scan depicting hyperreflective dots in the macula (C), and a normal OCT scan of the right optic disc (D).
Discussion
Syphilis is considered to have four disease stages: primary, secondary, latent, and tertiary stages. Ocular syphilis, a rare manifestation of syphilis, usually occurs in the secondary or latent stages. It is more common in males and often affects both eyes.13,14 Uveitis is the most common ocular manifestation of syphilis that may affect both the anterior and posterior segments of the eye.15 While anterior uveitis is more common in immunocompetent patients, posterior uveitis is more common in HIV-infected patients. Shalaby et al.16 reported that the rate of posterior uveitis was 38%, and that of anterior uveitis was 31%, in patients with ocular syphilis and HIV coinfection. Anterior uveitis can be nongranulomatous or granulomatous, mimicking ocular sarcoidosis and tuberculosis. Posterior uveitis most often presents as a chorioretinitis but can also occur with retinitis alone. Acute syphilitic posterior placoid chorioretinitis (ASPPC) refers to the presence of one or more placoid, yellowish, outer retinal lesions, typically in the macula, and was first used by Gass et al.10 Besides typical lesions, cases of ASPPC may also be characterized by focal, yellow, and deep retinal lesions. FAF, FA, indocyanine green angiography (ICGA), and OCT provide additional useful information about pathological processes. FAF patterns of ASPPC have been described in detail and the active placoid lesion is hyperautofluorescent. This may suggest lipofuscin accumulation at the level of the RPE-photoreceptor complex and is the most typical presentation of placoid syphilis.17 Unlike most previous studies, our case was presented with mottling hypoautofluorescence and hyperautofluorescence. This pattern is uncommon in ASPPC, but has been described previously.17 Early phase FA exhibits either hypofluorescence or faint hyperfluorescence. Scattered hypofluorescent spots are often observed in the area corresponding to the yellowish opacification; this pattern is sometimes called “leopard spotting.” However, progressive hyperfluorescence is observed in the mid- and late-phase FA. ICGA characteristics of ASPPC reveal early phase hypofluorescent areas corresponding to lesions that persist into later phases of angiography. 10,18–20 In some patients, late-phase ICGA hyperfluorescence in affected areas has also been described.20,21 Burkholder et al.22 reported OCT findings including thickening and hyperreflective nodularity of the choroid-RPE complex, with disruption of the overlying photoreceptor IS/OS bands and ELM in the areas corresponding to retinal lesions in patients with ASPPC. Optic nerve involvement, one of the causes of vision loss in syphilis, usually occurs in secondary and tertiary stages of syphilis. Optic nerve involvement may occur as neuroretinitis, gumma of the optic disc, papillitis, optic disc cupping, optic atrophy, perineuritis or chiasmal syndrome.23–29
In conclusion, present case exhibits an uncommon combination of unilateral papillitis and bilateral PPC in a patient with syphilis–HIV coinfection. Syphilis should therefore be considered in the differential diagnosis of patients with PPC or papillitis, and also all patients should be tested for HIV coinfection and neurosyphilis.
Funding Statement
None.
Acknowledgements
None.
Author contributions
All authors contributed significantly to the creation of this manuscript; each fulfilled criteria as established by the ICMJE.
Declaration of interests
The authors declare that they have no conflict of interest.
Consent
Authors obtained consent from the patients for publishing the photo.
References
- 1.French P. Syphilis. BMJ. 2007;334(7585):143–147. doi: 10.1136/bmj.39085.518148.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruan Y, Li D, Li X, et al. Relationship between syphilis and HIV infections among men who have sex with men in Beijing, China. Sex Transm Dis. 2007;34:592–597. [DOI] [PubMed] [Google Scholar]
- 3.Rottingen JA, Cameron DW, Garnett GP. A systematic review of the epidemiologic interactions between classic sexually transmitted diseases and HIV: how much really is known? Sex Transm Dis. 2001;28(10):579–597. doi: 10.1097/00007435-200110000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Wilhelmus KR, Yokoyama CM. Syphilitic episcleritis and scleritis. Am J Ophthalmol. 1987;104:595–597. [DOI] [PubMed] [Google Scholar]
- 5.Orsoni JG, Zavota L, Manzotti F, Gonzales S. Syphilitic interstitial keratitis: treatment with immunosuppressive drug combination therapy. Cornea. 2004;23:530–532. [DOI] [PubMed] [Google Scholar]
- 6.Schulman JA, Peyman GA. Syphilitic gummatous iridocyclitis. Ann Ophthalmol. 1989;21:333–336. [PubMed] [Google Scholar]
- 7.Babu BM, Rathinam SR. Intermediate uveitis. Indian J Ophthalmol. 2010;58(1):21–27. doi: 10.4103/0301-4738.58469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuo IC, Kapusta MA, Rao NA. Vitritis as the primary manifestation of ocular syphilis in patients with HIV infection. Am J Ophthalmol. 1998;125:306–311. [DOI] [PubMed] [Google Scholar]
- 9.Yokoi M, Kase M. Retinal vasculitis due to secondary syphilis. Jpn J Ophthalmol. 2004;48(1):65–67. doi: 10.1007/s10384-003-0011-5. [DOI] [PubMed] [Google Scholar]
- 10.Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97:1288–1297. [DOI] [PubMed] [Google Scholar]
- 11.Katarzyna P, Jerzy N, Zofia M. Syphilitic bilateral neuroretinitis–a case report. Klin Oczna. 2012;114:50–52. [PubMed] [Google Scholar]
- 12.Benson CE, Soliman MK, Knezevic A, Xu DD, Nguyen QD, Do DV. Bilateral papillitis and unilateral focal chorioretinitis as the presenting features of syphilis. J Ophthalmic Inflamm Infect. 2015;5:16. doi: 10.1186/s12348-015-0045-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chao JR, Khurana RN, Fawzi AA, Reddy HS, Rao NA. Syphilis: reemergence of an old adversary. Ophthalmology. 2006;113(11):2074–2079. doi: 10.1016/j.ophtha.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 14.Tran TH, Cassoux N, Bodaghi B, Fardeau C, Caumes E, Lehoang P. Syphilitic uveitis in patients infected with human immunodeficiency virus. Graefes Arch Clin Exp Ophthalmol. 2005;243(9):863–869. doi: 10.1007/s00417-005-1137-6. [DOI] [PubMed] [Google Scholar]
- 15.Kiss S, Damico FM, Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol. 2005;20(3):161–167. doi: 10.1080/08820530500232092. [DOI] [PubMed] [Google Scholar]
- 16.Shalaby IA. Syphilitic uveitis in human immunodeficiency virus-infected patients. Arch Ophthalmol. 1997;115(4):469–473. doi: 10.1001/archopht.1997.01100150471003. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto Y, Spaide RF. Autofluorescence imaging of acute syphilitic posterior placoid chorioretinitis. Retin Cases Brief Rep. 2007;1(3):123–127. doi: 10.1097/01.iae.0000242759.80833.39. [DOI] [PubMed] [Google Scholar]
- 18.Meira-Freitas D, Farah ME, Hofling-Lima AL, Aggio FB. Optical coherence tomography and indocyanine green angiography findings in acute syphilitic posterior placoid choroidopathy: case report. Arq Bras Oftalmol. 2009;72(6):832–835. doi: 10.1590/S0004-27492009000600019. [DOI] [PubMed] [Google Scholar]
- 19.Pichi F, Ciardella AP, Cunningham ET Jr, et al. Spectral domain optical coherence tomography findings in patients with acute syphilitic posterior placoid chorioretinopathy. Retina. 2014;34(2):373–384. doi: 10.1097/IAE.0b013e3182993f11. [DOI] [PubMed] [Google Scholar]
- 20.Baglivo E, Kapetanios A, Safran AB. Fluorescein and indocyanine green angiographic features in acute syphilitic macular placoid chorioretinitis. Can J Ophthalmol. 2003;38(5):401–405. doi: 10.1016/S0008-4182(03)80053-4. [DOI] [PubMed] [Google Scholar]
- 21.Joseph A, Rogers S, Browning A, et al. Syphilitic acute posterior placoid chorioretinitis in non immuno-compromised patients. Eye (Lond). 2007;21(8):1114–1119. doi: 10.1038/sj.eye.6702504. [DOI] [PubMed] [Google Scholar]
- 22.Burkholder BM, Leung TG, Ostheimer TA, Butler NJ, Thorne JE, Dunn JP. Spectral domain optical coherence tomography findings in acute syphilitic posterior placoid chorioretinitis. J Ophthalmic Inflamm Infect. 2014;4(1):2. doi: 10.1186/1869-5760-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith GT, Goldmeier D, Migdal C. Neurosyphilis with optic neuritis: an update. Postgrad Med J. 2006;82(963):36–39. doi: 10.1136/pgmj.2006.047001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meehan K, Rodman J. Ocular perineuritis secondary to neurosyphilis. Optom Vis Sci. 2010;87(10):790–796. doi: 10.1097/OPX.0b013e3181f361b0. [DOI] [PubMed] [Google Scholar]
- 25.Sacks JG, Osher RH, Elconin H. Progressive visual loss in syphilitic optic atrophy. J Clin Neuroophthalmol. 1983;3:5–8. [PubMed] [Google Scholar]
- 26.Arruga J, Valentines J, Mauri F, Roca G, Salom R, Rufi G. Neuroretinitis in acquired syphilis. Ophthalmology. 1985;92(2):262–270. doi: 10.1016/S0161-6420(85)34045-9. [DOI] [PubMed] [Google Scholar]
- 27.Smith JL, Byrne SF, Cambron CR. Syphiloma/gumma of the optic nerve and human immunodeficiency virus seropositivity. J Clin Neuroophthalmol. 1990;10:175–184. [PubMed] [Google Scholar]
- 28.Perry ME, Cooper S, Corry S. Neurosyphilis presenting with papillitis. EJCRIM. 2017;4. doi: 10.12890/2017_000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mansberger SL, MacKenzie PJ, Falardeau J. Optic disc cupping associated with neurosyphilis. J Glaucoma. 2013;22(2):80–83. doi: 10.1097/IJG.0b013e3182311eb2. [DOI] [PubMed] [Google Scholar]


