ABSTRACT
Physiological responses to work in cold water have been well studied but little is known about the effects of exercise in warm water; an overlooked but critical issue for certain military, scientific, recreational, and professional diving operations. This investigation examined core temperature responses to fatiguing, fully-immersed exercise in extremely warm waters. Twenty-one male U.S. Navy divers (body mass, 87.3 ± 12.3 kg) were monitored during rest and fatiguing exercise while fully-immersed in four different water temperatures (Tw): 34.4, 35.8, 37.2, and 38.6°C (Tw34.4, Tw35.8, Tw37.2, and Tw38.6 respectively). Participants exercised on an underwater cycle ergometer until volitional fatigue or core temperature limits were reached. Core body temperature and heart rate were monitored continuously. Trial performance time decreased significantly as water temperature increased (Tw34.4, 174 ± 12 min; Tw35.8, 115 ± 13 min; Tw37.2, 50 ± 13 min; Tw38.6, 34 ± 14 min). Peak core body temperature during work was significantly lower in Tw34.4 water (38.31 ± 0.49°C) than in warmer temperatures (Tw35.8, 38.60 ± 0.55°C; Tw37.2, 38.82 ± 0.76°C; Tw38.6, 38.97 ± 0.65°C). Core body temperature rate of change increased significantly with warmer water temperature (Tw34.4, 0.39 ± 0.28°C·h−1; Tw35.8, 0.80 ± 0.19°C·h−1; Tw37.2, 2.02 ± 0.31°C·h−1; Tw38.6, 3.54 ± 0.41°C·h−1). Physically active divers risk severe hyperthermia in warmer waters. Increases in water temperature drastically increase the rate of core body temperature rise during work in warm water. New predictive models for core temperature based on workload and duration of warm water exposure are needed to ensure warm water diving safety.
KEYWORDS: Core body temperature, clothing, thermal limits, physiology, biophysics
Introduction
Exercise in the heat is challenging for soldiers [1], athletes [2], and manual laborers [3,4] alike. Humans overcome heat stress in many environments primarily through evaporative cooling. However, humidity can limit the potential for evaporative heat loss through sweating. There is no evaporative underwater cooling and heat transfer from the body occurs via conduction, provided that the skin-water temperature gradient favors heat loss. The skin-water gradient narrows and eventually reverses when water temperature (Tw) increases. At the same time, increased hydrostatic pressure causes changes in circulation, renal functioning, breathing ability (on-air), and fluid shifts and fluid losses (i.e., diuresis) [5]. The addition of exercise during warm water immersion provides an opportunity to further challenge the limits of human thermoregulatory capacity.
Strenuous exercise in very warm waters is uncommon but necessary for certain military, scientific, recreational, and professional purposes. Military operations may task divers to work in the warm waters of the Persian Gulf; where sea surface temperatures typically reach 35°C but have increased by nearly 0.6°C since 1990 [6]. Microbiological research on thermophilic bacteria has involved scuba diving expeditions to shallow hydrothermal fissures venting water at temperatures between 30–95°C [7]. Tourists scuba dive in natural hot springs such as the Homestead Crater in Utah where water temperature is approximately 35°C [8]. The Dead Sea is frequently visited by both researchers [9] and tourists [10] and has sea surface temperatures that have historically ranged between 33–36°C during the summer months [11]. Furthermore, daytime sea surface temperatures in the Dead Sea were shown to have increased by 0.6°C·decade−1 over the period of 2000–2016 [12]. Thermoregulatory responses to warm water exercise must be better understood for the safety of current divers and future generations that face rising global water temperatures.
The effects of cold water immersion have been extensively researched [13–16] but fewer studies have examined the physiological and thermoregulatory responses to warm immersion exercise. Previous studies have examined exercise with either mid-chest [17] or heads out [18] immersion, following pre-exercise immersion [19], or while wearing a water-perfusion jacket [20]. The level of water immersion (e.g. knee, hip, chest) results in varying responses in physiological measures such as heart rate and oxygen uptake [21]. However, the physiological responses to full warm water immersion have not been fully elucidated. This study examined core temperature (Tc) and cardiovascular responses to fatiguing, fully-immersed exercise in extremely warm waters in order to better understand human thermoregulatory limits. We hypothesized that the rate of change in Tc (ROC.Tc) would increase significantly with warmer Tw.
Methods
Participants
Twenty-one male Navy-trained divers (body mass, 87.3 ± 12.3 kg) from the Navy Experimental Diving Unit (NEDU) and the Navy Diving and Salvage Training Center volunteered for this investigation. All participants provided voluntary informed consent before performing any experimental procedures. The study was approved by the review committee for the protection of human subjects at NEDU and the Institutional Review Board at the U.S. Army Research Institute of Environmental Medicine (USARIEM; Natick, MA).
Procedures
Prior to data collection, all participants completed a five week periodized cycle ergometer conditioning program in the NEDU Environmental Chamber (room temperature, 34.4°C; relative humidity, 50%) and an initial 4 h familiarization exercise dive with a water temperature (Tw) of 25.6°C. The familiarization dive followed the same protocol as the test exercise dives and was designed to expose participants to testing procedures, reduce learning effects, and ensure divers could tolerate the physical workload of the exercise test in the absence of thermal strain from the warmer water conditions. Subsequently, participants completed both a resting dive (≤ 8 h) and an exercise dive (≤ 4 h) at four different Tw in ascending order: 34.4, 35.8, 37.2, and 38.6°C (Tw34.4, Tw35.8, Tw37.2, and Tw38.6 respectively). Treatment order was not randomized due to diver safety concerns based on studies completed at the Naval Medical Research Center (NRMC) [22]. Familiarization, resting, and exercise dives were separated by at least 3 days of recovery.
Participants consumed one Meal, Ready-to-Eat (MRE) and at least 1 L of water the evening before scheduled dives and refrained from consuming either alcohol (> 48 h) and caffeine (> 24 h). On the morning of each dive, participants reported to the Physiology Lab two hours prior to their scheduled start times and were provided another MRE and 0.3 L of water. Diver dress consisted of a cotton T-shirt, swim trunks, and diver booties. Participants were weighed immediately before and after they entered the water for each dive to determine body mass changes (Post – Pre) for rehydration purposes. Body mass changes are reported for descriptive purposes but should not be interpreted as solely indicative of sweat loss since divers were permitted to urinate during the test dives and urine volume measurements were not available for analysis.
Core temperature (Tc) was recorded every 30-sec using an YSI 700 series thermistor probe (YSI, Inc.; Yellow Springs, OH). This probe was inserted 15 cm past the anal verge and retained there by a 6.4 mm diameter button. Water temperature was monitored using another YSI 700 series thermistor probe positioned at the participants’ depth and remained within ± 0.28°C of the designated Tw. Core temperature and Tw were recorded every 30 seconds with LabVIEW (National Instruments; Austin, TX) software on an NEDU data acquisition system (DAS) computer on the test pool medical deck. Heart rate was continuously monitored with Quinton Q-Tel Rehab ECG telemetry (Quinton Cardiology Systems, Inc.; Bothell, WA) and manually logged every five minutes. Two trolling motors (MotorGuide, WI; Minn Kota, MN) stirred the water column in the test pool to ensure a more homogeneous Tw. Oxygen pressure gauges and thermistors were calibrated at the beginning of each day.
Participants donned the underwater breathing apparatus (OXY-LUNG UBA; Aqua Lung America, Inc.; Vista, CA) and entered the test pool after all instrumentation checks were completed. Each participant then boarded a Modified Collins Pedal-Mate cycle ergometer (Collins Medical; Braintree, MA) set at zero inclination on a platform approximately three feet deep. Participants remained approximately 1–2 feet below the water surface in a slightly upward prone position with shoulders pressed against restraints, each hand gripping a handle, and feet strapped to the cycle ergometer for the entire dive. An Extrel Mass Spectrometer Model GS (ABB Extrel; Pittsburgh, PA) monitored inspired gas concentrations during all dives to ensure participant safety. Participants were asked to pedal at 60 rpm at a level of resistance that produced a work rate equal to a standard combat swim (50 watts) [23]. Trials were terminated when (a) the participant was unable to sustain the work rate; (b) Tc exceeded 40°C for 5 min; (c) Tc exceeded 40.5°C at any time; (d) if the participant requested termination for any reason; or (e) after 4 hours.
Data analysis
All data were analyzed using analyzed using R (Version 3.3.1; R Foundation for Statistical Computing; Vienna, Austria) [24]. Data are displayed as mean ± SD unless specifically noted otherwise. Rate of change in core temperature (ROC.Tc) was calculated as the average rate of change in core temperature over time. Pairwise least-squares mean comparisons were conducted using mixed effects models with random intercepts if a significant main effect was detected by analysis of variance. The level of statistical significance was set at p < 0.05.
Results
There was a significant main effect of Tw on trial endurance time (p < 0.001) (Figure 1). Trial time was significantly longer for Tw34.4 versus the Tw35.8, Tw37.2, and Tw38.6 conditions (p < 0.001 for each). Similarly, trial time was significantly higher for Tw35.8 versus Tw37.2 (p = 0.001) and Tw38.6 (p < 0.001). However, there was no significant difference between Tw37.2 and Tw38.6 (p = 0.409). Four participants reached the 4-hour time limit for Tw34.4 while only one finished for Tw35.8. Two trials were halted due to Tc limits for the Tw37.2 and Tw38.6 conditions with none of the participants reaching the 4-hour time limit in either condition. There was no significant main effect of Tw on body mass change (p = 0.061). Body mass changes were negative; indicating body mass was lost during test dives (Tw34.4, −1.8 ± 0.9%; Tw35.8, −2.5 ± 1.3%; Tw37.2, −2.0 ± 1.2%; Tw38.6, −1.4 ± 0.9%).
Figure 1.
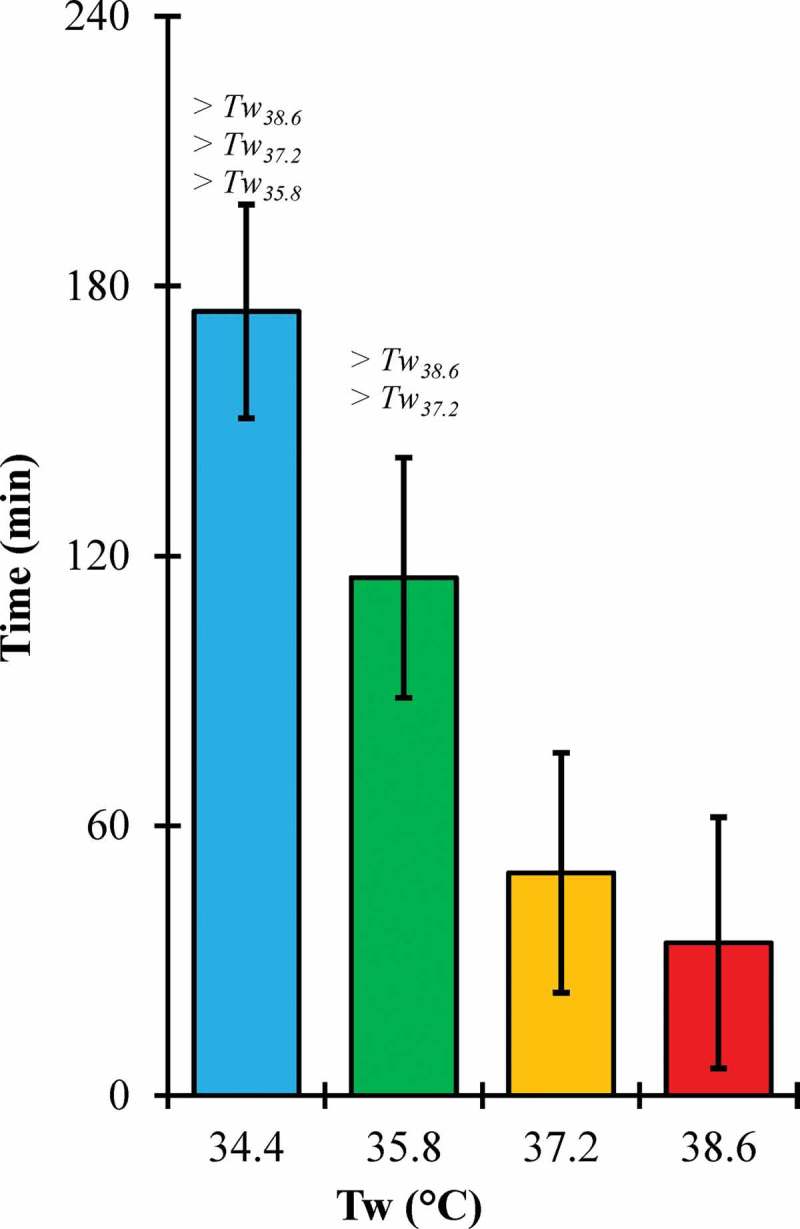
Endurance time across water temperature (Tw) conditions.
Error bars, 95% confidence intervals; > #, significantly greater than #°C water condition.
There was a significant main effect of Tw on peak HR (p = 0.002) (Figure 2). Peak HR for Tw34.4 was not significantly different from Tw35.8 (p = 0.107) but was significantly lower than Tw37.2 (p = 0.007) and Tw38.6 (p < 0.001). Similarly, peak HR for Tw35.8 was not significantly different than Tw37.2 (p = 0.231) but was significantly lower than Tw38.6 (p = 0.016). However, peak HR for Tw37.2 was not significantly different than Tw38.6 (p = 0.165).
Figure 2.
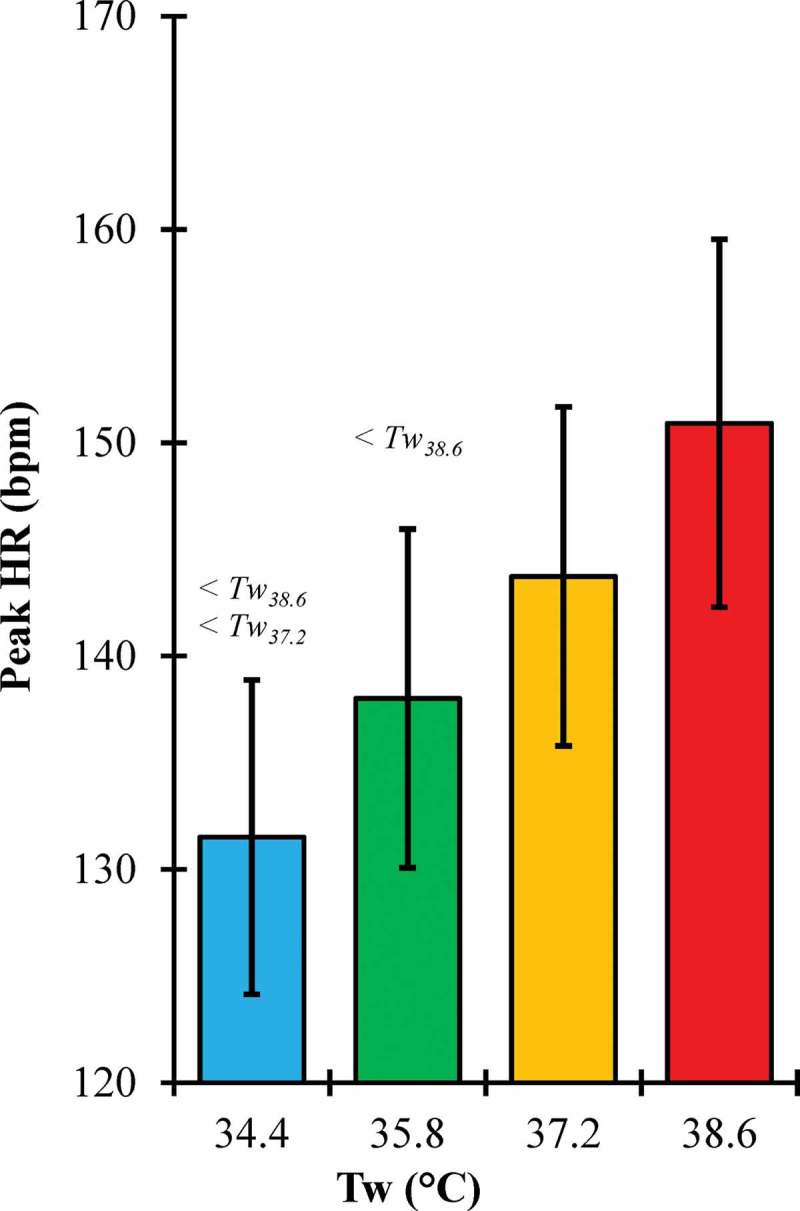
Peak heart rate (HR) across water temperature (Tw) conditions.
Error bars, 95% confidence intervals; < #, significantly lower than #°C water condition.
There was a significant main effect of Tw on peak Tc (p = 0.038) but not initial Tc (p = 0.329) (Figure 3). Peak Tc for Tw34.4 was not significantly different from Tw35.8 (p = 0.203) but was significantly lower than Tw37.2 (p = 0.032) and Tw38.6 (p = 0.008). In contrast, peak Tc for Tw35.8 was not significantly different than Tw37.2 (p = 0.361) or Tw38.6 (p = 0.145). Peak Tc for Tw37.2 was not significantly different than Tw38.6 (p = 0.547).
Figure 3.
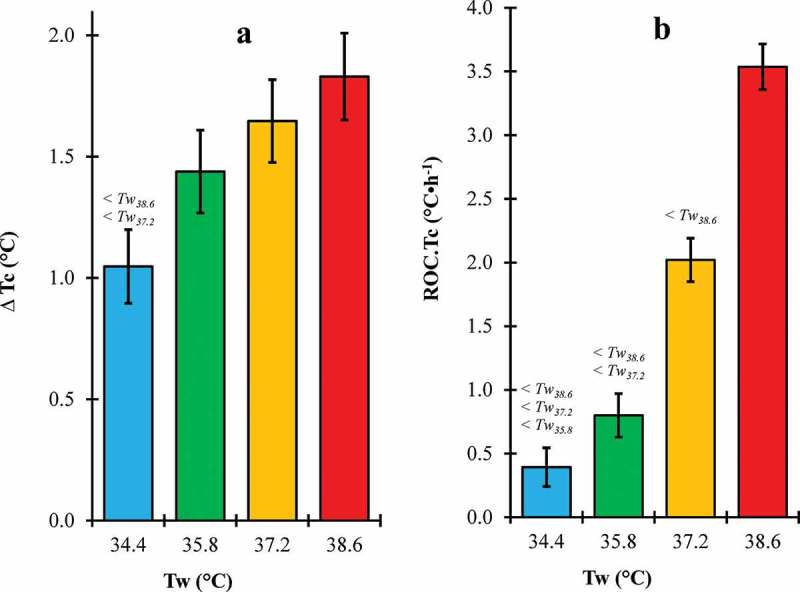
∆Tc (a) and ROC.Tc (b) across water temperature (Tw) conditions.
Tc, core temperature (°C); ROC.Tc, rate of change in core temperature (°C·h−1); Error bars, 95% confidence intervals; < #, significantly lower than #°C water condition.
There was a significant main effect of Tw on ∆Tc (p = 0.003) and ROC.Tc (p < 0.05 for each) (Figure 4). ∆Tc for Tw34.4 was significantly lower than Tw37.2 (p = 0.004) and Tw38.6 (p < 0.001) but not Tw35.8 (p = 0.064). ∆Tc for Tw35.8 was not significantly different than Tw37.2 (p = 0.342) or Tw38.6 (p = 0.097). ∆Tc for Tw37.2 was not significantly different than Tw38.6 (p = 0.435). ROC.Tc for Tw34.4 was significantly lower than Tw35.8, Tw37.2, and Tw38.6 (p < 0.001 for each). Similarly, ROC.Tc for Tw35.8 was significantly lower than Tw37.2 and Tw38.6 (p < 0.001 for each). Furthermore, ROC.Tc for Tw37.2 was also significantly lower than Tw38.6 (p < 0.001). Figures 4 and 5 display Tc and heart rate respectively over trial endurance time for each Tw condition.
Figure 4.
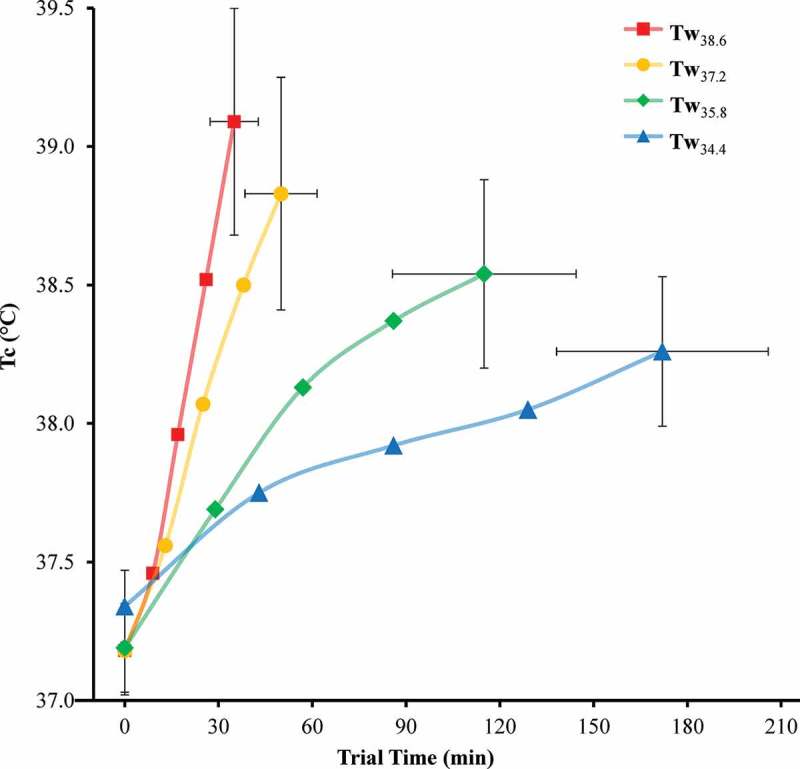
Trial endurance time and core temperature (Tc) at 0, 25, 50, 75, and 100% trial time.
Error bars, 95% confidence intervals.
Figure 5.
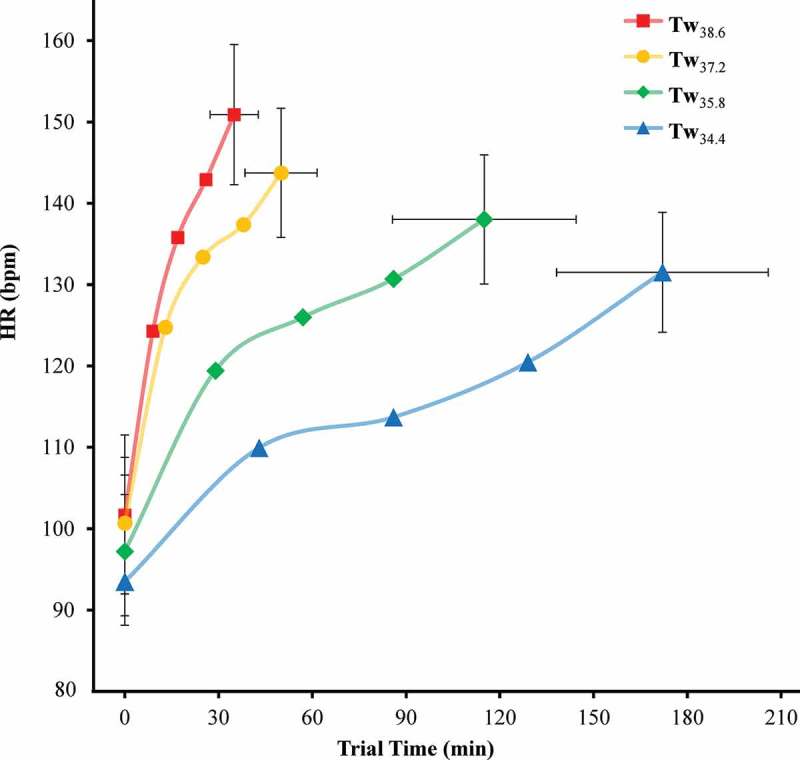
Trial endurance time and heart rate (HR) at 0, 25, 50, 75, and 100% trial time.
Error bars, 95% confidence intervals.
Discussion
Warm water immersion results in increasingly rapid rises in Tc and onset of fatigue during exhaustive exercise. Rate of change in Tc increased significantly with warmer Tw indicating an unsustainable level of thermal-work strain. Additionally, there was a drastic reduction in trial endurance time in the warmer Tw conditions. Although all participants were required to complete a 4 h exercise dive in 25.6°C water before testing, the same work rate was only sustained for 34 ± 14 min in the Tw38.6 condition. These findings highlight the dangers of warm water diving expeditions and enhance understanding of human thermoregulatory limits.
Prior investigations have noted reduced aerobic endurance capacity with warm water immersion [25,26]. Nybo et al. [27] reviewed a combination of different cardiovascular, psychological, neurobiological, respiratory, and muscular factors that explain the accelerated fatigue during exertional heat stress [27]. Temperature-related reductions in time trial performance have been attributed to impaired nerve conduction and force development [28]. Exertional hyperthermia decreases skeletal muscle activation [29] while increasing perceived exertion [30]. Watson et al. [19] noted significantly greater perceived exertion in addition to elevated heart rate, blood glucose, and lactate concentrations during exercise in 39°C water versus 35°C. In the current study, participants were likely unable to regulate Tc in the warmer Tw conditions due to the loss of sweat evaporation capabilities and heat gained from the water.
The results in Figure 4 show that heat stress during warm water immersion dramatically accelerates ROC.Tc during exercise. Few studies have observed such extreme rates of Tc rise as the present study (3.54°C·h−1 for Tw38.6) during strenuous exercise in warm water environments where the body gains heat from the water. Gonzalez-Alonso et al. [20] noted a rate of change in esophageal temperature of 6.31°C·h−1 in trained cyclists during an endurance trial (258 ± 20 W; 87 ± 2 rpm; 66 ± 3% VO2 max) while wearing a 42°C water-perfusion jacket in a 40°C environmental chamber. Rhind et al. [17] observed an average ROC.Tc of 3.15°C·h−1 after 40 min of cycle ergometer exercise (65% VO2 peak) while immersed to mid-chest in 39°C water. In contrast, Macaluso et al. [31] recorded an average ROC.Tc of only 0.87°C·h−1 in competitive masters swimmers following a 5-km simulated race in 32°C water.
One limitation of this investigation is that treatment order was not randomized. Trials were scheduled in ascending order of Tw and were scheduled at least 3 days after a resting trial at the designated Tw to best ensure diver safety and minimize heatstroke risk. Acclimatization status is a prominent moderator of the effect of environmental heat stress on endurance exercise performance [32]. Consequently, the treatment order may have blunted the thermoregulatory responses observed in the higher Tw conditions. Another limitation for this investigation is the lack of skin temperature data which is essential for tracking the time course of the inversion of the skin-water temperature gradient. High skin temperatures are associated with earlier exhaustion during submaximal exercise in the heat [33–35]. This performance decrement has been attributed to reductions in cardiac output and peak oxygen uptake resulting from increased peripheral blood flow [33].
This study examined Tw conditions that are greater or equal to the most extreme warm water environments where diving occurs outside of the laboratory. The divers faced a level of exertional heat stress that is unrealistic for the majority of everyday scenarios. The highest Tw conditions (Tw37.2 and Tw38.6) exceed nearly all current warm water diving environments outside of the laboratory. However, climate change poses major heat illness risks [36] and rising global Tw trends [6,12,37] suggest divers may be exposed to greater thermal stress over time. These health risks may be exacerbated in the aging workforce due to the reduced ability of older adults to compensate for heat gain [38]. This study provides insight on the excessive thermal-work strain experienced during fatiguing warm water exercise that is of relevance to military, recreational, and professional divers who will endure similar conditions in the near or distant future.
Conclusion
Divers risk severe predictable hyperthermia in warmer waters. Physical performance degrades sharply at warmer temperature extremes. Incremental increases in water temperature drastically increase the rate of core temperature rise. Precise core temperature monitoring strategies and/or predictive models are needed to ensure warm water diving safety.
Acknowledgments
The authors would like to thank all human subject volunteers for this study and special thanks to the men and women who have and continue to serve our Armed Services.
Disclosure statement
No potential conflict of interest was reported by the authors.
Disclaimer
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Army, Department of the Navy, or the Department of Defense. Citations of commercial organizations and trade names in this report do not constitute an official endorsement or approval of the products or services of these organizations.
References
- [1].Hunt AP, Billing DC, Patterson MJ, et al. Heat strain during military training activities: the dilemma of balancing force protection and operational capability. Temperature. 2016;3(2):307–317.doi: 10.1080/23328940.2016.1156801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Pryor JL, Johnson EC, Roberts WO, et al. Application of evidence-based recommendations for heat acclimation: individual and team sport perspectives. Temperature. 2018;6:1–13.doi: 10.1080/23328940.2018.1516537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Jay O, Brotherhood JR.. Occupational heat stress in Australian workplaces. Temperature. 2016;3(3):394–411. doi: 10.1080/23328940.2016.1216256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Notley SR, Meade RD, D’Souza AW, et al. Cumulative effects of successive workdays in the heat on thermoregulatory function in the aging worker. Temperature. 2018;5(4):293–295. doi: 10.1080/23328940.2018.1512830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Pendergast DR, Lundgren CE. The underwater environment: cardiopulmonary, thermal, and energetic demands. J Appl Physiol. 2009;106(1):276–283. [DOI] [PubMed] [Google Scholar]
- [6].Shirvani A, Nazemosadat S, Kahya E. Analyses of the Persian Gulf sea surface temperature: prediction and detection of climate change signals. Arabian J Geosci. 2015;8(4):2121–2130. [Google Scholar]
- [7].Lentini V, Gugliandolo C, Maugeri TL. Identification of enzyme-producing thermophilic bacilli isolated from marine vents of Aeolian Islands (Italy). Ann Microbiol. 2007;57(3):355–361. [Google Scholar]
- [8].Blackett R, Lund JW. Midway area, Wasatch County. Geo-Heat Cen Quarterly Bulletin. 2004;25(4):48–49. [Google Scholar]
- [9].Ionescu D, Siebert C, Polerecky L, et al. Microbial and chemical characterization of underwater fresh water springs in the Dead Sea. PloS one. 2012;7(6):e38319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Wendt JA. Tourism development challenges on the Dead Sea shore. Limnol Review. 2016;16(2):105–112. [Google Scholar]
- [11].Nehorai R, Lensky I, Lensky N, et al. Remote sensing of the Dead Sea surface temperature. J Geophys Res Oceans. 2009;114:C5. doi: 10.1029/2008JC005196 [DOI] [Google Scholar]
- [12].Kishcha P, Pinker RT, Gertman I, et al. Observations of positive sea surface temperature trends in the steadily shrinking Dead Sea. Nat Hazards Earth Sys Sci. 2018;18(11):3007–3018. [Google Scholar]
- [13].Xu X, Tikuisis P. Thermoregulatory modeling for cold stress. Compr Physiol. 2014. July;4(3):1057‐1081. [DOI] [PubMed] [Google Scholar]
- [14].Toner MM, McArdle WD. Human thermoregulatory responses to acute cold stress with special reference to water immersion In: Pollock DM, editor. Comprehensive physiology. Hoboken, NJ: John Wiley & Sons, Inc; 2011. p. 379–397. [Google Scholar]
- [15].Riera F, Hoyt R, Xu X, et al. Thermal and metabolic responses of military divers during a 6-hour static dive in cold water. Aviat Space Environ Med. 2014;85(5):509–517. [DOI] [PubMed] [Google Scholar]
- [16].Pakanen L, Pääkkönen T, Ikäheimo TM, et al. Urinary thrombomodulin and catecholamine levels are interrelated in healthy volunteers immersed in cold and warm water. Temperature. 2016;3(1):161–166. doi: 10.1080/23328940.2015.1033589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Rhind SG, Gannon GA, Shek PN, et al. Contribution of exertional hyperthermia to sympathoadrenal-mediated lymphocyte subset redistribution. J Appl Physiol. 1999;87(3):1178–1185. [DOI] [PubMed] [Google Scholar]
- [18].Craig A, Dvorak M. Thermal regulation during water immersion. J Appl Physiol. 1966;21(5):1577–1585. [DOI] [PubMed] [Google Scholar]
- [19].Watson P, Shirreffs SM, Maughan RJ. Blood-brain barrier integrity may be threatened by exercise in a warm environment. Am J Physiol Regul Integr Comp Physiol. 2005;288(6):R1689–R1694. [DOI] [PubMed] [Google Scholar]
- [20].González-Alonso J, Teller C, Andersen SL, et al. Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol. 1999;86(3):1032–1039. [DOI] [PubMed] [Google Scholar]
- [21].Barbosa TM, Marinho DA, Reis VM, et al. Physiological assessment of head-out aquatic exercises in healthy subjects: a qualitative review. J Sports Sci Med. 2009;8(2):179. [PMC free article] [PubMed] [Google Scholar]
- [22].Hyde D, Weinberg R, Stevens D, et al. Pyridostigmine and warm water diving Protocol 90-05: 2. Thermal balance. Bethesda, MD: Naval Medical Research Institute; 1990. [Google Scholar]
- [23].Knafelc M. Oxygen consumption rate of operational underwater swimmers. Panama City, FL: Navy Experimental Diving Unit (NEDU); 1989. [Google Scholar]
- [24].R Core Team R: A language and environment for statistical computing. Vienna, Austria: R Foundation Stat Comp. 2014. p.1–16 [Google Scholar]
- [25].Bonde-Petersen F, Schultz-Pedersen L, Dragsted N. Peripheral and central blood flow in man during cold, thermoneutral, and hot water immersion. Aviat Space Environ Med. 1992;63(5):346–350. [PubMed] [Google Scholar]
- [26].Galloway S, Maughan RJ. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Med Sci Sports Exerc. 1997;29(9):1240–1249. [DOI] [PubMed] [Google Scholar]
- [27].Nybo L, Rasmussen P, Sawka MN. Performance in the heat-physiological factors of importance for hyperthermia-induced fatigue. Compr Physiol. 2014;4(2):657–689. [DOI] [PubMed] [Google Scholar]
- [28].Tucker R, Rauch L, Harley YX, et al. Impaired exercise performance in the heat is associated with an anticipatory reduction in skeletal muscle recruitment. Eur J Appl Physiol. 2004;448(4):422–430. [DOI] [PubMed] [Google Scholar]
- [29].Nybo L, Nielsen B. Hyperthermia and central fatigue during prolonged exercise in humans. J Appl Physiol. 2001;91(3):1055–1060. [DOI] [PubMed] [Google Scholar]
- [30].Nybo L, Nielsen B. Perceived exertion is associated with an altered brain activity during exercise with progressive hyperthermia. J Appl Physiol. 2001;91(5):2017–2023. [DOI] [PubMed] [Google Scholar]
- [31].Macaluso F, Di Felice V, Boscaino G, et al. Effects of three different water temperatures on dehydration in competitive swimmers. Sci Sports. 2011;26(5):265–271. [Google Scholar]
- [32].Junge N, Jørgensen R, Flouris AD, et al. Prolonged self-paced exercise in the heat–environmental factors affecting performance. Temperature. 2016;3(4):539–548. doi: 10.1080/23328940.2016.1216257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Cheuvront SN, Kenefick RW, Montain SJ, et al. Mechanisms of aerobic performance impairment with heat stress and dehydration. J Appl Physiol. 2010;109(6):1989–1995. [DOI] [PubMed] [Google Scholar]
- [34].Sawka MN, Cheuvront SN, Kenefick RW. High skin temperature and hypohydration impair aerobic performance. Exp Physiol. 2012;97(3):327–332. [DOI] [PubMed] [Google Scholar]
- [35].Kenefick RW, Cheuvront SN, Palombo LJ, et al. Skin temperature modifies the impact of hypohydration on aerobic performance. J Appl Physiol. 2010;109(1):79–86. [DOI] [PubMed] [Google Scholar]
- [36].Kenny GP, Flouris AD, Yagouti A, et al. Towards establishing evidence-based guidelines on maximum indoor temperatures during hot weather in temperate continental climates. Temperature. 2019; 6(1): 11–36. doi: 10.1080/23328940.2018.1456257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Xie S-P, Deser C, Vecchi GA, et al. Global warming pattern formation: sea surface temperature and rainfall. J Clim. 2010;23(4):966–986. [Google Scholar]
- [38].Kenny GP, Poirier MP, Metsios GS, et al. Hyperthermia and cardiovascular strain during an extreme heat exposure in young versus older adults. Temperature. 2017;4(1):79–88. doi: 10.1080/23328940.2016.1230171 [DOI] [PMC free article] [PubMed] [Google Scholar]


