Abstract
Objectives:
Reduction in the amount of information (storage capacity) retained in working memory (WM) has been associated with sleep loss. The present study examined whether reduced WM capacity was also related to poor everyday sleep quality, and more importantly, whether the effects of sleep quality could be dissociated from the effects of depressed mood and age on WM.
Methods:
In two studies, WM was assessed using a short-term recall task, producing behavioral measures for both the amount of retained WM information (capacity) and how precise the retained WM representations were (precision). Self-report measures of sleep quality and depressed mood were obtained using questionnaires.
Results:
In a college-student sample, Study 1 found that poor sleep quality and depressed mood could independently predict reduced WM capacity, but not WM precision. Study 2 generalized these sleep and mood related WM capacity effects to a community sample (aged 21 to 77 years old), and further showed that age was associated with reduced WM precision.
Conclusions:
Together, these findings have demonstrated dissociable effects of three health-related factors (sleep, mood, and age) on WM representations and highlighted the importance of assessing different aspects of WM representations (e.g., capacity and precision) in future neuropsychological research.
Keywords: working memory, capacity, precision, sleep, depressed mood, age
Working memory (WM) stores task-relevant information over a few seconds at the service of other ongoing mental activities (Cowan, 2001; Luck & Vogel, 1997). As a core aspect of cognition (Cowan, 2001), WM is highly limited in the amount of information that can be simultaneously maintained over a short period of time (Cowan, 2001; Luck & Vogel, 2013; Zhang & Luck, 2008; 2011). This sets a major constraint on a wide range of cognitive and affective processes, such as attention (Kane, Poole, Tuholski, & Engle, 2006), fluid intelligence (Conway, Cowan, Bunting, Therriault, & Minkoff, 2002), processing of affective information (Lynn et al., 2016; Xie et al., 2017), and emotional regulation (Schmeichel, Volokhov, & Demaree, 2008). In addition, compromised WM is also frequently associated with declines in various health-related factors, such as poor sleep quality (e.g., Wee, Asplund, & Chee, 2013), depressed mood (e.g., Xie et al., 2018a), and age (e.g., Peich, Husain, & Bays, 2013), suggesting the importance of WM assessment in translational research.
For example, naturally-occurring and experimentally-induced sleep loss can significantly impair WM (Chee & Chuah, 2007; Smith, McEvoy, & Gevins, 2002; F. Waters & Bucks, 2011; Wee et al., 2013). Although these impairments have been taken as evidence for reduced WM capacity (i.e., the amount of information maintained in WM), a reduction in memory quality might also account for these findings (see Xie & Zhang, 2016; 2017a; 2017b; Zhang & Luck, 2009; 2011 for some discussions). To clarify this issue, Wee and colleagues (2013) recently distinguished the effects of sleep deprivation on the quantitative (e.g., the number of remembered stimuli) and qualitative (e.g., precision, how precisely a given memory representation corresponds to the original to-be-remembered physical stimulus) aspects of visual WM using a procedure and a mathematical model developed by Zhang and Luck (2008). They found that sleep deprivation had a detrimental effect on the number, instead of the precision, of retained WM representations.
However, disrupted sleep is often coupled with other factors, such as depressed mood (Banthia, Malcarne, Ko, Varni, & Sadler, 2009; Zawadzki, Graham, & Gerin, 2013) and age (Maglione et al., 2014; but see Ohayon, Zulley, Guilleminault, Smirne, & Priest, 2001; Ohayon, Carskadon, Guilleminault, & Vitiello, 2004), which are also associated with reduced WM functions (Adams, Stanczak, Leutzinger, Waters, & Brown, 2001; Arnett, Higginson, Voss, Bender, et al., 1999a; Hubbard et al., 2015; Park et al., 2002). It is thus unclear whether reduced WM capacity under experimentally-induced sleep deprivation as shown in Wee et al. (2013) is a direct result of disrupted sleep or a secondary effect of factors associated with sleep loss (e.g., a transient change in depressed mood, Zawadzki et al., 2013), and whether these effects can be generalized to poor sleep quality in everyday life.
The present study thus examines how self-report measure for sleep quality in everyday life and two related factors (depressed mood and age) are associated with WM capacity and precision using an individual-differences approach. In brief, Study 1 assesses contributions of sleep quality and depressed mood to reduced WM capacity in a college sample. Study 2 further evaluates these adverse effects of poor sleep quality and depressed mood on WM in a community sample with a wider age range. We hypothesize that poor everyday sleep quality is mostly associated with reduced WM capacity, but less so with WM precision (Wee et al., 2013), and this effect can be dissociated from the contributions of depressed mood and age on WM.
Study 1
Method
Participants
One hundred and ten college students (19.50 ± 1.51 years old, 68 female) from the University of California, Riverside, participated in this study. This sample size was determined based on a power analysis using G*Power (Faul, Erdfelder, Buchner, & Lang, 2009) for 80% power using a r-based effect size at a medium level (.20 to .30), considering that the present study focused on individual differences manifested as correlational patterns across participants. All participants reported normal (or corrected-to-normal) visual acuity and normal color vision. Three additional participants scored above 20 in the depressed mood scale (see Method section; classified as “major depression, severe”) were excluded from data analysis. Nonetheless, inclusion of these three participants did not substantially influence the results. The University of California, Riverside Institutional Review Board approved this study. All the participants gave their written informed consent prior to the study, and received course credits for their participation.
Procedure
Participants performed a computer-based WM task for independent estimates of the number and precision of retained WM representations (Zhang & Luck, 2008). Subsequently, they completed a packet of questionnaires capturing sleep quality and depressed mood.
WM task.
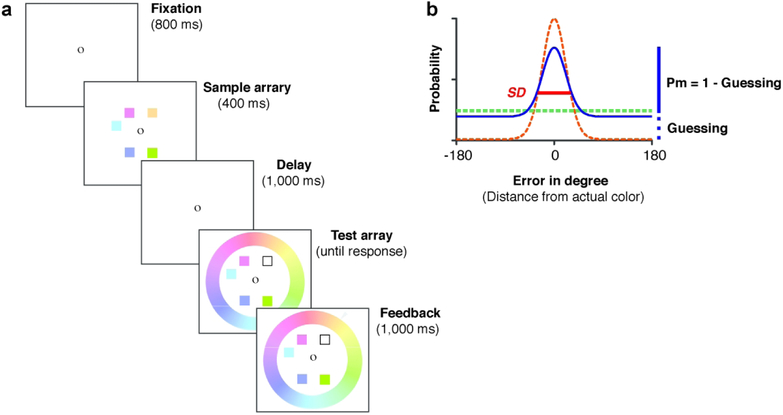
In this task (Figure 1a), participants were instructed to remember an array of four color squares that were simultaneously presented on the screen for 400 ms. Locations of the color squares were randomly selected from a set of eight possible locations that were equally spaced on an invisible circle (4.5° radius). Colors on each trial were randomly chosen from 180 colors that were evenly distributed on a circle in the Commission Internationale de l’Eclairage Lab color space (see Zhang & Luck, 2008 for details). All colors had comparable luminance and varied mainly in hue and slightly in saturation. After a short delay of 1000 ms, the test array appeared. It contained all but one color from the memory array, in addition to a continuous color wheel (radius = 8.2°; thickness = 2.2°) with all 180 colors in the chosen color space. The missing color (indicated by the empty square) was randomly chosen from the presented color squares in the previous sample array. Participants were required to report the color of this probed item – based on their memory – as precisely as possible by using a computer mouse to click a matching color on the wheel. Performance on each trial was measured as the error in degrees between the color chosen by the participant and actual color shown in the sample array. All observers completed 5 blocks of 30 trials, yielding 150 trials in total.
Figure 1.
A sample trial of the color recall working memory task. a). Immediately after an 800-ms fixation, a sample array of five colored squares was presented for 400 ms, followed by a 1,000-ms delay interval. A test array appeared after the delay and stayed on screen until participants’ recall responses. The test array consisted of all but one colored square from the sample array and a continuous color wheel of 180 equally spaced colors. The missing color (marked by an outline square) was randomly chosen from the sample array, indicating the probed color for recall. That is, participants tried to reproduce its color from memory by clicking on the best matching color on the color wheel. Immediately following the recall response, the actual color presented in the sample array was marked on the color wheel by an arrow as online feedback. The difference between the actual color presented in the memory array and the reported color (i.e., recall error) was aggregated across trials and fitted with the MLE model fitting procedure. b). A hypothetical distribution of recall errors (solid line) could be decomposed into a uniform distribution (bolded dashed line) representing guesses and a von Mises distribution (light dashed line) representing noisy memory representations. The probability of remembering (Pm) is one minus the probability of guessing, manifested as the height of the uniform distribution. The number of retained WM representations (K) is thus Pm × memory set size. SD of the von Mises distribution (in degrees) is inversely related to the precision of retained WM representation.
Sleep quality.
Pittsburgh Sleep Quality Index (PSQI) was used to assess participants’ sleep quality over last month (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989). It consists of 10 multi-component questions. The full index is a summation of seven sub-scores, including Duration of Sleep, Sleep Disturbance, Sleep Latency, Day Dysfunction Due to Sleepiness, Sleep Efficiency, Overall Sleep Quality, and Need of Medication to Sleep (see Supplementary Table S1 for correlations among these sub-scores and other measures of interest). Each sub-score ranges from 0 to 3, and therefore the full index ranges from 0 to 21. Higher scores indicate poorer sleep quality.
Depressed mood.
Patient Health Questionnaire-9 (PHQ-9) is a self-report measure of depressive symptoms over the previous two weeks (Kroenke & Spitzer, 2001). Participants respond to 9 symptom questions by indicating how often in the past two weeks they have been bothered by that symptom using a 4-point scale (from “Not at all = 0” to “Nearly Every Day = 3”). Possible scores range from 0-27, with 0 indicating no experience of depression and 27 reflecting severe depression.
Data analysis
WM Task.
Participants’ recall errors in the WM task were fitted with Zhang & Luck’s (2008) standard mixture model using a Maximum Likelihood Estimation (MLE) procedure. With this procedure, recall errors (solid line in Figure 1b) can be decomposed into a weighted summation of two components as shown in Figure 1b, one representing a graded and noisy memory representation for the probed item when it was encoded in memory (light dashed line in Figure 1b) and the other representing random guesses when the probed item was absent from memory (bolded dashed line in Figure 1b). The proportion of retained noisy memory representations, Pm (i.e., probability of remembering), is inversely related to the proportion of random guesses (1-Pm), which can be captured as the height of the tails in the recall error distribution (see Figure 1b). The number of stimuli that can be retained in WM (denoted as K) is therefore the product of memory set size (the number of to-be-membered items) and Pm. WM precision is further defined as the standard deviation (SD) of the distribution for retained noisy memory representations. Note, a smaller SD is associate with higher WM precision.
Analysis of Individual Differences.
Multicollinearity is an issue when assessing independent contributions of multiple predictors to an outcome variable (e.g., Alvaro, Roberts, & Harris, 2014). Without removing the conceptually overlapping items in measurement that can lead to the multicollinearity, the effects of sleep quality and depressed mood on WM could be confounded by the inflated correlation between the two variables. To assess the independent effects of sleep quality and depressed mood on WM, we therefore eliminated these overlapping items. Specifically, the PHQ-9 scale contained an item conceptually similar to sleep quality (Item 3 on the PHQ-9), and the PSQI had a sub-score measuring daily dysfunction due to sleepiness, which was highly related with depressed symptoms (Item 8 and 9 on the PSQI). Correlational analyses were conducted and reported for both the original and the non-overlapping versions of the PSQI and PHQ-9 scores. To examine their potentially independent effects on WM capacity, we further performed a path analysis for the effects of sleep quality and depressed mood on WM measures based on the non-overlapping scores of PSQI and PHQ-9 using the R package (R Core Team, 2014).
Results and Discussion
Correlational Analyses
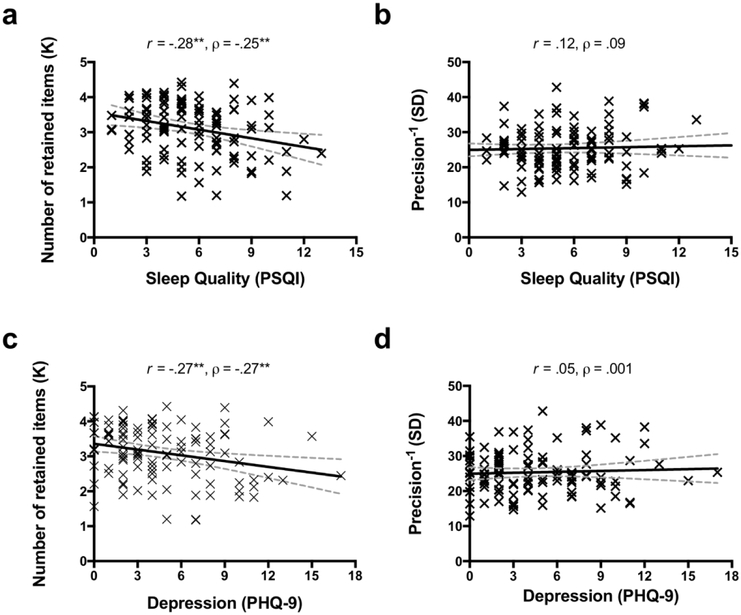
Sleep problems and depressed mood were highly correlated with each other (based on non-overlapping items: r = .38 [.21, .53], p < .001; with overlapping items: r = .54 [.40, .66], p < .001; see Table 1), and they were both associated with decreased WM capacity (see Figure 2). Specifically, the number of retained WM representations (K) was negatively correlated with both poor sleep quality as measured by PSQI scores (r = −.28 [−.44, −.10], p = .003, Figure 2a) and depressed mood as measured by PHQ-9 scores (r = −.27 [−.43, −.08], p = .005, Figure 2c). In contrast, SD (precision−1) was not significantly correlated with either PHQ-9 (Figure 2b) or PSQI (Figure 2d) scores, regardless of the original or non-overlapping versions of the scales (all ps > .05, see Table 1). Critically, the correlation between K and depressed mood was significant larger than the correlation between SD and depressed mood (z = 2.58, p < .01), using the one-tailed test on correlated correlations (Meng, Rosenthal, & Rubin, 1992). Likewise, the correlation between K and sleep quality was significantly greater than the correlation between SD and sleep quality (z = 3.21, p < .001). These correlations remained robust when the overlapping items in PHQ-9 and PSQI were removed (non-overlapping PHQ-9: r = −.27 [−.43, −.09], p = .005; non-overlapping PSQI: r = −.27 [−.44, −.09, p = .004), as summarized in Table 1. Overall, these findings suggested that both poor sleep quality and depressed mood could reduce the amount of information that can be maintained in WM.
Table 1.
Correlations of WM measurements, age, depressed mood, and sleep quality in Study 1
| 1 | 2 | 3 | 4 | 5 | Mean (SD) | |
|---|---|---|---|---|---|---|
| 1. Capacity (K) | - | 3.11(0.76) | ||||
| 2. Precision−1 (SD) | .17 | - | 25.34(6.11) | |||
| 3. Depressed mood-Ia | −.27** | .05 | - | 4.52(3.68) | ||
| 4. Sleep quality-Ia | −.28** | .12 | .54** | - | 5.58(2.58) | |
| 5. Depressed mood-IIb | −.27** | .05 | .98** | .49** | - | 3.68(3.10) |
| 6. Sleep quality-IIb | −.27** | .11 | .45** | .96** | .38** | 4.71(2.30) |
Note: Mean (SD) for each variable is presented in the last column. Depressed mood was assessed with Patient Health Questionnaire-9 (PHQ-9). Sleep quality was measured with Pittsburgh Sleep Quality Index (PSQI) questionnaire.
Scores from full scales of PHQ-9 and PSQI;
Scores from the conceptually non-overlapping versions of PHQ-9 and PSQI.
p < .05;
p < .01.
Figure 2.
The effects of depressed mood and sleep quality on WM capacity in Study 1. Sleep quality (score from the full scale of PSQI) was significantly correlated with WM capacity (a), but not with precision (b). Depressed mood (score from the full scale of PHQ-9) was significantly correlated with WM capacity (c), but not with precision (d). The solid lines represent the linear regression prediction. The broken lines represent 95% confidence intervals (CI) for the linear regression prediction. Pearson correlation coefficient (r) and Spearman rank-order correlation coefficient (ρ) are presented in the figure. *. p < .05, **. p < .01.
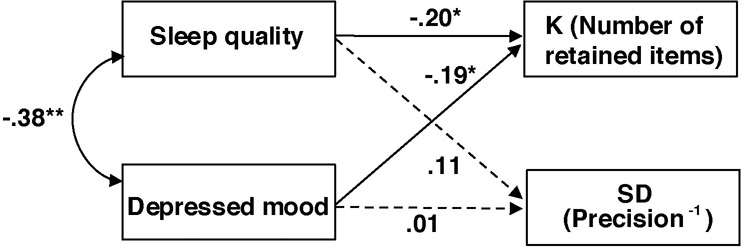
Path Analysis
We then conducted a path analysis on the non-overlapping version of PSQI and PHQ-9 to further test the independent influences of sleep quality and depressed mood on WM capacity and precision simultaneously (also see Online Supplementary for the path analysis based on the full version of the scales and additional analysis based on group means, Supplementary Table S2). As shown in Figure 3, the non-overlapping versions of PSQI (β = −.20 [−.39, −.01], SE = 0.098, p = .042) and PHQ-9 (β = −.19 [−.38, −.01], SE= .098, p = .048) scores were independently predictive of individual difference in the number of retained WM representations (K). In contrast, neither sleep quality (β = .11 [−.09, .31], SE = .102, p = .29) nor depressed mood (β = .01 [−.19, .21], SE = .102, p = .94) significantly predicted individual difference in WM precision (SD).
Figure 3.
Correlated predictive model of sleep quality, depressed mood, and WM. K denotes the number of retained WM representations, as an estimate of capacity; SD denotes variability of retained WM recall errors, which is inversely related to precision. The broken lines indicate insignificant relationships. Note, the scores from the non-overlapping versions of PSQI and PHQ-9 that removed conceptually overlapping items were used in this multiple regression analysis *. p < .05.
Conclusion
In summary, these findings demonstrated that both depressed mood and poor sleep quality could reduce WM capacity. More importantly, the detrimental effect of sleep disturbance on WM could not entirely result from the depressed mood that was associated with poor sleep quality.
Study 2
Study 1 showed that depressed mood and poor sleep quality primarily reduced WM capacity with a minimal impact on WM precision. It is important to demonstrate that the lack of precision effects was not due to insensitive measurement of WM precision in the current paradigm. Study 2 thus tested an additional health-related factor, age, which was previously associated with reductions in WM precision (e.g., Noack, Lövdén, & Lindenberger, 2012; Peich et al., 2013; Pertzov, Heider, Liang, & Husain, 2015). Note, some previous reports attributed declines in WM function over age to reduced storage capacity (e.g., Park et al., 2002). However, these previous studies did not separately estimate WM capacity and precision, leaving open the possibility that these previous effects could result from decreases in WM precision. Study 2 also isolated the effects of sleep disturbance on WM from the effects of age on WM, given that both sleep problems (e.g., Mellor, Waters, Olaithe, McGowan, & Bucks, 2014) and depression-related psychological conditions (e.g., Sözeri-Varma, 2012) may change with age.
To achieve these two goals, Study 2 tested a community sample (n = 31) with larger variability in age (from 21 to 77 years old). Given the potential increased variability in perceptual and motor abilities in community participants, overall effects on WM, especially effects on WM precision (inversely related to variability), could potentially result from effects on perceptual and motor processing (Gold et al., 2010). Study 2 thus included a motor control task and a perception control task (for details, see Method and Gold et al., 2010), to test whether compromised WM, if any, could be attributed to problems in motor functions or perception.
Method
Participants
Participants were recruited from the greater Ann Arbor community as part of a large-scale genetics research project (see Berry et al., 2014 for details) examining the relationship between cognitive functions and a polymorphism limiting cholinergic capacity (Ile89Val variant [rs1013940] of the choline transporter gene SLC5A7). Participants with this polymorphism may exhibit different susceptibility to external distraction (Berry et al., 2014) as compared to participants without the polymorphism. However, they did not significantly differ in the qualitative or quantitative estimates of WM in the present study (the number of retained items, K: t(29) = 0.20 , p = .84; precision−1, SD: t(29) = 0.58 , p = .57). The two groups of subjects were therefore combined for present analyses to increase statistical power. Analyses included a total of 31 participants (17 female) who completed the present WM task and met the following criteria: 1) participants were free from current psychopharmacological medication (e.g., selective serotonin reuptake inhibitors, SSRI); 2) they reported normal (or corrected normal) visual acuity and color vision; and 3) they were currently not suffering from severe depressive symptoms (all scoring lower than 9 on the Patient Health Questionaire-9; Kroenke & Spitzer, 2001). Participants’ age ranged from 21 to 77 years old (M = 46.32, SD =16.91), and years of education ranged from 12 to 20 (M = 15.87, SD = 2.35). The sample size of this study was determined by the actual number of eligible participants meeting these mentioned criteria. Based on G*Power (Faul et al., 2009), this sample size is sensitive to detect – with 80% power – a statistically significant effect size r as small as 0.42. As estimated by Peich et al. (2013), the size of correlation between age and reduced WM precision is about 0.51, which is larger than 0.42. Thus, the current sample size would have sufficient statistical power to demonstrate a significant effect using the current measure of WM precision.
The University of Michigan Institutional Review Board approved the current study. All the participants gave their written informed consent at the beginning of the study, and received monetary compensation ($10) for their participation.
Procedure
The procedure was the same as that in Study 1 with the exception on the two control tasks. The two control tasks were modeled from Gold et al. (2010) and run at the beginning of the test session. In the motor control task, observers used the computer mouse to click on specified points on the color wheel. In the subsequent color perception control task, the target color and color wheel were shown simultaneously and the observer was instructed to click on the matching color on the color wheel. The motor and perceptual control tasks were included to estimate errors in motor responses and perception, respectively, both of which are presumably independent of errors resulting from noisy representations in WM. The motor control task and the subsequent perceptual control task contained 30 trials each.
Data Analysis
The data analysis routines were the same as those in Study 1 with the following exceptions. First, the small number of trials in the two control tasks also made it practically impossible to obtain reliable mixture model fits (30 trials per task in the present study, as opposed to 150 trials as suggested in Zhang & Luck, 2008). Instead, overall circular SD were analyzed and reported for the two control tasks. Mathematically the overall circular SD approaches to the SD of the mixture model as Pm approaches to 1, which is the case in the control tasks where the perception of and motor responses for a single item are not limited by capacity. Therefore, the overall circular SD for the two control tasks can be used to measure precision of perception and motor responses, respectively, in a way that is equivalent to the SD of the mixture model in the WM task. Second, path analysis was not conducted due to the small sample size in Study 2. Last, in addition to correlational analyses for the relationships between age and WM, as a complementary test, participants were categorized into two age groups based on median split of age (younger adult group: age < 50, M = 31.60, SD = 6.71; older adult group: age >= 50, M = 62.06, SD = 7.17), considering that the age distribution showed more younger and older participants with fewer middle-aged participants (40-55 years old). Subsequently, t tests were conducted to assess differences in WM across the two age groups. The two groups of participant differed significantly in age (t(29) = 12.20 , p < .0001), but not in gender ratio, sleep quality, or depressed mood (all ps > .10), as shown in Table 2.
Table 2.
Age group differences in demographic information and measures of interest.
| Older Adults (50 to 77 years old) |
Younger Adults (21 to 43 years old) |
χ2/t | p | |||
|---|---|---|---|---|---|---|
| Gender | 10 males 6 females |
7 males 8 females |
0.78 | .38 | ||
| M | SD | M | SD | |||
| Age | 62.06 | 7.17 | 31.60 | 6.71 | 12.20 | <.001 |
| Years of Education | 15.50 | 2.45 | 16.27 | 2.60 | 0.84 | .41 |
| Depressed Mooda | 1.56 | 1.67 | 2.33 | 2.41 | 1.04 | .31 |
| Sleep Qualitya | 4.31 | 2.96 | 4.33 | 3.09 | 0.02 | .98 |
| Motor Control | ||||||
| Circular Mean | −0.06 | 0.10 | −0.01 | 0.12 | 1.24 | .22 |
| Circular SD | 0.06 | 0.05 | 0.03 | 0.04 | 1.58 | .13 |
| Perceptual Control | ||||||
| Circular Mean | 0.80 | 2.94 | 0.79 | 2.23 | 0.01 | .98 |
| Circular SD | 1.53 | 0.66 | 1.32 | 0.51 | 0.95 | .35 |
| WM Task | ||||||
| Capacity (K) | 2.74 | 0.54 | 2.80 | 0.78 | 0.26 | .80 |
| Precision−1 (SD) | 29.06 | 3.99 | 25.39 | 5.42 | 2.16 | .039 |
Note: Scores from full scales of PHQ-9 (Patient Health Questionnaire-9) and PSQI (Pittsburgh Sleep Quality Index).
Results and Discussion
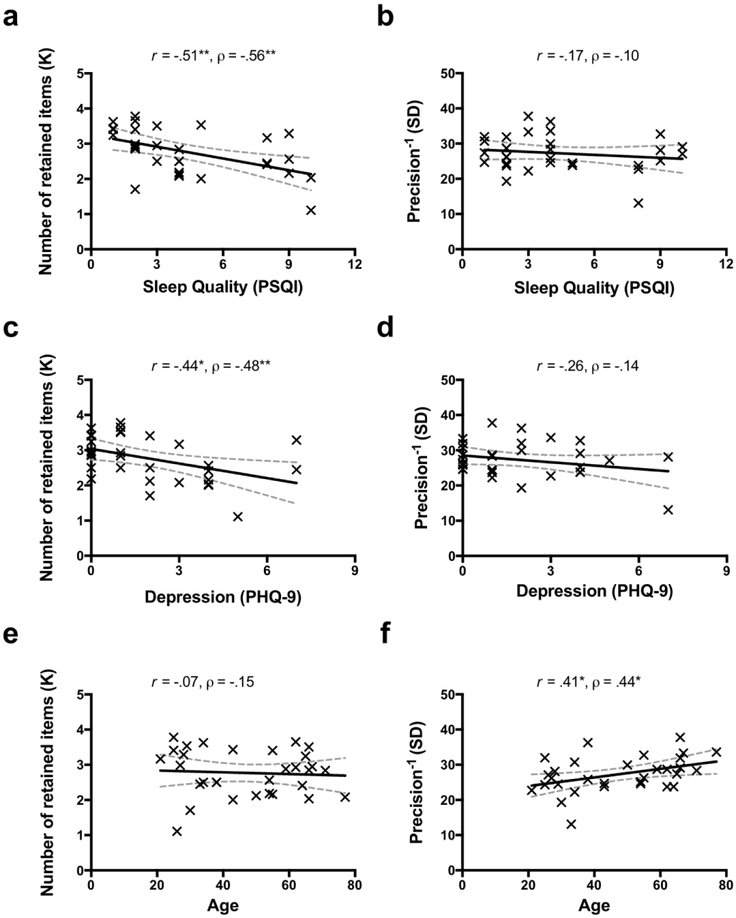
WM Capacity, Sleep Quality, and Depressed Mood
Consistent with the observations in Study 1, poor sleep quality and depressed mood were also highly correlated in the community sample (based on non-overlapping items: r = .77 [.57, .88], p < .001; with overlapping items: r = .83 [.67, .92], p < .001; see Table 3). Furthermore, the number of retained WM representations (K) decreased as sleep quality decreased (i.e., increasing PSQI score, see Figure 4a) and as depressed mood scores increased (see Figure 4c). These observations were supported by significant negative correlations between K and self-reported sleep problems as indexed by PSQI scores (r = −.51 [−.73, −.19], p = .003), and between K and self-reported depressed mood as indexed by PHQ-9 scores (r = −.44 [−.69, −.10], p = .013). Correlations between capacity and depressed mood/sleep quality remained robust for the non-overlapping PSQI scores (r = −.50 [−.72, −.17], p = .004) and PHQ-9 (r = −.42 [−.67, −.08], p = .018), as summarized in Table 3. In contrast, SD (inversely related to precision) was not significantly correlated with sleep quality or depressed mood, regardless of the full or non-overlapping versions of the scales (allps > .05; see Table 3). Overall, these findings from a community sample were consistent with the results in Study 1.
Table 3.
Correlations of WM measurements, depressed mood, and sleep quality in Study 2
| 1 | 2 | 3 | 4 | 5 | 6 | Mean (SD) | |
|---|---|---|---|---|---|---|---|
| 1. Capacity (K) | - | 2.77(0.65) | |||||
| 2. Precision−1 (SD) | .12 | - | 27.28(5.02) | ||||
| 3. Age | −.07 | .41* | - | 47.32(16.92) | |||
| 4. Depressed mood-Ia | −.44* | −.26 | −.22 | - | 1.94(2.06) | ||
| 5. Sleep quality-Ia | −.51** | −.17 | −.09 | .83** | - | 4.32(2.97) | |
| 6. Depressed mood-IIb | −.42* | −.34 | −.28 | .97** | .78** | - | 1.42(1.61) |
| 7. Sleep quality-IIb | −.50** | −.18 | −.11 | .83** | .98** | .77** | 3.94(2.69) |
Note: Mean (SD) for each variable is presented in the last column. Depressed mood was assessed with Patient Health Questionnaire-9 (PHQ-9). Sleep quality was measured with Pittsburgh Sleep Quality Index (PSQI) questionnaire.
Scores from full scales of PHQ-9 and PSQI;
Scores from the conceptually non-overlapping versions of PHQ-9 and PSQI.
p < .05
p < .01.
Figure 4.
The dissociable effects on working memory (WM) capacity and precision in Study 2. Sleep quality (score from the full scale of PSQI) was significantly correlated with WM capacity (a), but not with precision (b). Depressed mood (score from the full scale of PHQ-9) was significantly correlated with WM capacity (c), but not with precision (d). Age was significantly correlated with WM precision (f), but not with capacity (e). The solid lines represent the linear regression prediction. The broken lines represent 95% confidence intervals (CI) for the linear regression prediction. Pearson correlation coefficient (r) and Spearman rank-order correlation coefficient (ρ) are presented in the figure. *. p < .05, **. p < .01.
Age-related Precision Effects
In contrast to the capacity effects of poor sleep quality and depressed mood, age had detrimental effects on WM precision. First, using an individual-differences approach, age was positively correlated with SD of memory recall errors across participants (r = .41 [.07, .67], p = .022; see Figure 4f), but not significantly correlated with K (r = −.07 [−.41, .29], p = .71, see Figure 4e). Critically, using the same one-tailed test on correlated correlations (Meng et al., 1992), the difference between the correlation between K and age and the correlation between WM precision and age was significant (z = 1.96, p = .025, one-tailed). Second, in a complementary between-group test, older adults had substantially worse precision for retained WM representations (i.e., larger SD) as compared to younger adults (t(29) = 2.16, p = .039, Cohen’s d = 0.80). In contrast, WM capacity was comparable between the two age groups (t(29) = 0.26, p = .80, Cohen’s d = 0.09).
Motor and Perceptual Control Tasks
Participants’ performances in the motor control task (absolute circular mean = 0.08 ± 0.11 degrees; circular SD = 0.04 ± 0.04 degrees) and the perceptual color matching task (absolute circular mean = 1.99 ± 1.79 degrees; circular SD = 1.43 ± 0.59 degrees) were highly accurate. Both the circular mean and SD were close to zero. The circular SD in the motor control tasks and the circular SD in the perceptual control tasks were both substantially smaller than the SD in the WM task (27.27 ± 5.01 degrees), indicating that internal noise in perceptual processing and motor response had a negligible contribution to the overall SD in the WM task. More importantly, the circular SD in the motor and perceptual tasks was not significantly correlated with any measures (K, SD, depressed mood, sleep quality, and age; all ps >.05; see Supplementary Table S3). These results suggested that the significant effects in Study 2 were unlikely to be confounded by individual differences in motor performance or perceptual discriminability in the community sample.
Conclusion
In sum, Study 2 demonstrated dissociable effects of sleep quality and age on the number and quality of WM representations, respectively, replicating the previous effects of sleep on WM quantity (e.g., Wee et al., 2013) and the effects of age on WM quality (e.g., Noack et al., 2012; Peich et al., 2013; Pertzov et al., 2015). The two effects were unlikely to be confounded by each other, given that they were opposite to each other.
General Discussion
The present study demonstrated that poor sleep quality was primarily associated with reduced WM capacity, even after the effects of depressed mood were considered. Specifically, by controlling for statistical and measurement covariance between depressed mood and poor sleep quality, Study 1 showed that the two measures were independently correlated with reductions in the number, but not the precision, of remembered colors in WM in college students. Study 2 generalized the detrimental effects of poor sleep quality and depressed mood on WM capacity to a community sample and further demonstrated an opposite effect of age on WM (i.e., reduced WM precision with intact WM capacity). Overall, these results demonstrated the dissociable effects of the three health-related factors on WM representations.
The current study replicated some previously reported adverse relationships between sleep disturbance and WM capacity (Chee & Chuah, 2007; Wee et al., 2013), between depressed mood and WM capacity (Arnett, Higginson, Voss, Bender, et al., 1999a; Arnett, Higginson, Voss, Wright, et al., 1999b), and between ageing and WM precision (e.g., Bermudez & Souza, 2017; Noack et al., 2012; Peich et al., 2013; Pertzov et al., 2015; Souza, 2016) in the same study. This is not a trivial contribution for three reasons. First, previous investigations on these relationships mostly used a piecemeal approach by looking at the relationship between one of these health-related factors and WM at a time (e.g., Peich et al., 2013; Wee et al., 2013). This approach leaves open the possibility that an observed effect may be influenced by other factors. Without controlling for these confounding factors, it would be difficult to isolate the effects of health-related factors on WM. By statistically controlling the covariance of sleep quality and depressed mood, Study 1 demonstrated the independently predictive power of sleep quality and depressed mood on WM capacity. Thus, previously observed adverse effect of poor sleep quality on WM capacity (Chee & Choo, 2004; Chee & Chuah, 2007; Smith et al., 2002; Wee et al., 2013) would be unlikely to be confounded by depressed mood associated with sleep loss. Similarly, the adverse effects of poor sleep quality on WM capacity would be unlikely to be confounded by age in Study 2, given age was more associated with decreases in WM precision.
Second, the impacts of the three health-related factors on WM were examined in some of the previous studies using experimental methods that, on the one hand, controlled low-level experimental confounds, and on the other hand, limited the generalizability of the findings. For example, the experimental manipulation of sleep (e.g., sleep deprivation, Wee et al., 2013) could induce some changes in subjects’ emotional states, even though it allowed tests of the effects of sleep on WM using within-subject design (thus minimizing effects of individual differences). The comparisons between dichotomized clinical subject groups (e.g., depression group versus control group, Arnett, Higginson, Voss, Bender, et al., 1999a) are mainly informative for understanding the differences in WM between pathological stage and the general healthy population. In contrast, the present study (also see Klein & Boals, 2001 with a similar approach) assessed how individual differences in self-report measures of daily-life sleep quality and depressed mood in a more general population (with some subclinical symptoms, in comparison to pathological cases) were related with individual differences in WM representations. These self-report measures of sleep quality and depressed mood in a general population are critical for generalizing the previous findings from highly controlled laboratory settings to applied settings. This applied approach promotes the research on the cognitive effects of health-related factors in broader contexts (e.g., Klein & Boals, 2001; Korten, Sliwinski, Comijs, & Smyth, 2014) and potentially facilitate the development of specific and sensitive neuropsychology tests to identify intermediate cognitive risk factors associated with common health-related factors, paving the way for early diagnosis and intervention (Cuijpers et al., 2014).
Last, traditional measures of performance such as accuracy and response time often confound the quantitative and qualitative aspects of WM representations. This approach is problematic because effects on these compound measures are often interpreted as effects on WM capacity, even though these behavioral measures could reflect effects on WM capacity, precision, or both (see Xie & Zhang, 2016; 2017a; 2017b; Zhang & Luck, 2009; 2011 for some discussions). Using a novel experimental paradigm (Zhang & Luck, 2008), the current study obtained simultaneous assessments of quantity and quality for retained WM representations, making it possible to assess the dissociable effects of the three health-related factors on WM representations. Furthermore, the present study also provides insights into the current debate on the nature of WM storage limits. The center of this debate is whether capacity and precision are both necessary as independent factors for WM storage limitation as proposed by capacity-limit theories (Zhang & Luck, 2008), or whether precision alone is sufficient to account for WM storage limitation as proposed by precision-limit theories (Bays & Husain, 2008). While precision-limit theories (e.g., Bays & Husain, 2008) predicts an omnibus reduction of WM precision under poor sleep quality, depressed mood, and age, the dissociable patterns of WM impairments in the present study provide some evidence that both capacity and precision are necessary to account for the effects of health-related factors on WM, as predicted by the capacity-limit theories (Zhang & Luck, 2008).
Several mechanisms could potentially account for the current observations of the dissociable associations among the three health-related factors (sleep quality, depressed mood, and age) and compromised WM representations. First, increased attentional lapses due to disrupted sleep may account for reduced WM capacity (Verstraeten, Cluydts, Pevernagie, & Hoffmann, 2004), considering the close association between attention and WM (Engle, 2002). This can manifest as alteration of the functional network for attention/WM following disrupted sleep (Chee & Chuah, 2007; Chee et al., 2011). Second, depressed mood may deplete the overall cognitive resource (Mathews & MacLeod, 1994), leading to compromised cognitive functions (Hertel & Hardin, 1990; Hertel & Rude, 1991). Third, age is often associated with increased intra-individual variabilities (Hultsch & MacDonald, 2004), potentially resulting from noisier mental representations (Jagust, 2013; Leal & Yassa, 2015) and/or decreased prefrontal functions including distractor inhibition (Fabiani, Zimmerman, & Gratton, 2015; Hasher & Zacks, 1988; Lustig & Jantz, 2015; Lustig, Hasher, & Zacks, 2007). Future research needs to explore these potential neurocognitive mechanisms.
There are several cautious notes for the present study. First, it is important to note that WM is viewed here as the central cognitive resource and the decline in this resource is viewed as the cause of WM deficits (e.g., Craik & Byrd, 1982). This is different from theories that describe WM deficits as the outcome of inefficient processing (Fabiani et al., 2015; Hasher & Zacks, 1988; Lustig et al., 2007; Lustig & Jantz, 2015). For example, sleep loss related WM deficits may result from inefficient processing of relevant information when distracted by irrelevant information (e.g., executive function, Rana et al., 2018). Future research is needed to test whether these deficits in the processing modules of WM in relation to deficits in WM storage (e.g., Park et al., 2002). Second, the age effect in the present study was obtained in a crosssectional design (e.g., Peich et al., 2013), a longitudinal approach will be needed (e.g., Blackwell et al., 2014; Nebes, Buysse, Halligan, Houck, & Monk, 2009) to reveal how and why WM precision declines over age. Third, the current study did not find a significant association between age and the self-report measure of sleep quality, which is not necessarily at odds with the literature given the mixed findings on this relationship (Mellor et al., 2014; Ohayon et al., 2001; 2004; Unruh et al., 2008). Future research is needed to evaluate how more objective measures of sleep characteristics (e.g., slow-wave sleep) may interact with the effect of age on WM. Last, the current study relies exclusively on non-clinical samples with a focus on relative transient changes in mood states. Future investigation should also examine how the alterations in different aspects of WM representations are related to prolonged negative thoughts and depressed feelings in clinically depressed individuals (Xie, Li, Zou, Sun, & Shi, 2018b).
Conclusion
The present study refines our understandings of the relationships among sleep quality, depressed mood, age, and WM 1) by specifying the effects of sleep quality, depressed mood, and age on WM capacity and precision, and 2) by looking at their individual/independent effects on memory via path analysis (for sleep quality and depressed mood). These findings add to the growing literature on dissociating effects of health-related factors on different aspects of WM, and facilitate the development of specific and sensitive neuropsychology tests to evaluate WM deficits associated with common health-related factors.
Supplementary Material
Acknowledgement
This work was made possible by funding support from the National Institute of Mental Health (R01MH117132 to WZ) and the Public Health Service (R01MH086530 to CL). AB was supported by a National Science Foundation Graduate Research Fellowship.
Footnotes
Declaration of Conflicting Interests
The authors declared that they had no conflicts of interest with respect to their authorship or the publication of this article.
References
- Adams RA, Stanczak DE, Leutzinger MR, Waters MD, & Brown T (2001). The impact of psychological disturbances on immediate memory. Archives of Clinical Neuropsychology, 16(6), 605–618. 10.1016/S0887-6177(00)00072-X [DOI] [PubMed] [Google Scholar]
- Alvaro PK, Roberts RM, & Harris JK (2014). The independent relationships between insomnia, depression, subtypes of anxiety, and chronotype during adolescence. Sleep Medicine, 15(8), 934–941. 10.1016/j.sleep.2014.03.019 [DOI] [PubMed] [Google Scholar]
- Arnett PA, Higginson CI, Voss WD, Bender WI, Wurst JM, & Tippin JM (1999a). Depression in multiple sclerosis: Relationship to working memory capacity. Neuropsychology, 13(4), 546–556. [DOI] [PubMed] [Google Scholar]
- Arnett PA, Higginson CI, Voss WD, Wright B, Bender WI, Wurst JM, & Tippin JP (1999b). Depressed mood in multiple sclerosis: Relationship to capacity-demanding memory and attentional functioning. Neuropsychology, 13(3), 434–446. 10.1037/0894-4105.13.3.434 [DOI] [PubMed] [Google Scholar]
- Banthia R, Malcarne VL, Ko CM, Varni JW, & Sadler GR (2009). Fatigued breast cancer survivors: The role of sleep quality, depressed mood, stage and age. Psychology & Health, 24(8), 965–980. 10.1080/08870440802110831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bays PM, & Husain M (2008). Dynamic shifts of limited working memory resources in human vision. Science, 321(5890), 851–854. 10.1126/science.1158023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bermudez T, & Souza AS (2017). Can emotional content reduce the age gap in visual working memory? Evidence from two tasks. Cognition and Emotion, 31(8), 1676–1683. 10.1080/02699931.2016.1240066 [DOI] [PubMed] [Google Scholar]
- Berry AS, Demeter E, Sabhapathy S, English BA, Blakely RD, Sarter M, & Lustig C (2014). Disposed to distraction: Genetic variation in the cholinergic system influences distractibility but not time-on-task effects. Journal of Cognitive Neuroscience, 26(9), 1981–1991. 10.1162/jocn_a_00607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell T, Yaffe K, Laffan A, Ancoli-Israel S, Redline S, Ensrud KE, … & Stone KL (2014). Associations of objectively and subjectively measured sleep quality with subsequent cognitive decline in older community-dwelling men: the MrOS sleep study. Sleep, 37(4), 655–663. 10.5665/sleep.3562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Chee MWL, & Choo WC (2004). Functional imaging of working memory after 24 hr of total sleep deprivation. Journal of Neuroscience, 24(19), 4560–4567. 10.1523/JNEUROSCI.0007-04.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chee MWL, & Chuah YML (2007). Functional neuroimaging and behavioral correlates of capacity decline in visual short-term memory after sleep deprivation. Proceedings of the National Academy of Sciences of the United States of American, 104(22), 9487–9492. 10.1073/pnas.0610712104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chee MWL, Goh CSF, Namburi P, Parimal S, Seidl KN, & Kastner S (2011). Effects of sleep deprivation on cortical activation during directed attention in the absence and presence of visual stimuli. NeuroImage, 58(2), 595–604. 10.1016/j.neuroimage.2011.06.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway AR, Cowan N, Bunting MF, Therriault DJ, & Minkoff SR (2002). A latent variable analysis of working memory capacity, short-term memory capacity, processing speed, and general fluid intelligence. Intelligence, 30(2), 163–183. [Google Scholar]
- Cowan N (2001). The magical number 4 in short-term memory: A reconsideration of mental storage capacity. Behavioral and Brain Sciences, 24(1), 87–185. 10.1177/0963721409359277 [DOI] [PubMed] [Google Scholar]
- Craik FIM, & Byrd M (1982). Aging and cognitive deficits: The role of attentional resources In Craik FIM & Trehub S (Eds.), Aging and Cognitive Processes (pp. 191–211). New York, NY: Springer Science & Business Media; 10.1007/978-1-4684-4178-9 [DOI] [Google Scholar]
- Cuijpers P, Koole SL, van Dijke A, Roca M, Li J, & Reynolds CF (2014). Psychotherapy for subclinical depression: Meta-analysis. The British Journal of Psychiatry, 205(4), 268–274. 10.1192/bjp.bp.113.138784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engle RW (2002). Working memory capacity as executive attention. Current Directions in Psychological Science, 11(1), 19–23. 10.1111/1467-8721.00160 [DOI] [Google Scholar]
- Fabiani M, Zimmerman B, & Gratton G (2015). Working memory and aging: A review In Jolicoeur P, Lefebvre C, & Martinez-Trujillo J (Eds.), Mechanisms of Sensory Working Memory Attention and Performance XXV (pp. 131–148). Amsterdam, Netherlands: Elsevier; 10.1016/b978-0-12-801371-7.00011-9 [DOI] [Google Scholar]
- Faul F, Erdfelder E, Buchner A, & Lang A-G (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- Gold JM, Hahn B, Zhang W, Robinson BM, Kappenman ES, Beck VM, & Luck SJ (2010). Reduced capacity but spared precision and maintenance of working memory representations in schizophrenia. Archives of General Psychiatry, 67(6), 570–577. 10.1001/archgenpsychiatry.2010.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasher L, & Zacks RT (1988). Working memory, comprehension, and aging: A review and a new view. Psychology of Learning and Motivation, 22, 193–225. [Google Scholar]
- Hertel PT, & Hardin TS (1990). Remembering with and without awareness in a depressed mood: evidence of deficits in initiative. Journal of Experimental Psychology: General, 119(1), 45–59. [DOI] [PubMed] [Google Scholar]
- Hertel PT, & Rude SS (1991). Depressive deficits in memory: Focusing attention improves subsequent recall. Journal of Experimental Psychology: General, 120(3), 301–309. 10.1037//0096-3445.120.3.301 [DOI] [PubMed] [Google Scholar]
- Hubbard NA, Hutchison JL, Turner M, Montroy J, Bowles RP, & Rypma B (2015). Depressive thoughts limit working memory capacity in dysphoria. Cognition and Emotion, 30(2), 193–209. 10.1080/02699931.2014.991694 [DOI] [PubMed] [Google Scholar]
- Hultsch DF, & MacDonald SWS (2004). Intraindividual variability in performance as a theoretical window onto cognitive aging In Dixon RA, Bäckman L, & Nilsson LG (Eds.), New Frontiers in Cognitive Aging (pp. 65–88). New York, NY. [Google Scholar]
- Jagust W (2013). Vulnerable Neural Systems and the Borderland of Brain Aging and Neurodegeneration. Neuron, 77(2), 219–234. 10.1016/j.neuron.2013.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane MJ, Poole BJ, Tuholski SW, & Engle RW (2006). Working memory capacity and the top-down control of visual search: Exploring the boundaries of "executive attention". Journal of Experimental Psychology: Learning, Memory, and Cognition, 32(4), 749–777. 10.1037/0278-7393.32.4.749 [DOI] [PubMed] [Google Scholar]
- Klein K, & Boals A (2001). The relationship of life event stress and working memory capacity. Applied Cognitive Psychology, 15(5), 565–579. 10.1002/acp.727 [DOI] [Google Scholar]
- Korten NCM, Sliwinski MJ, Comijs HC, & Smyth JM (2014). Mediators of the Relationship Between Life Events and Memory Functioning in a Community Sample of Adults. Applied Cognitive Psychology, 28(5), 626–633. 10.1002/acp.3043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leal SL, & Yassa MA (2015). Neurocognitive aging and the hippocampus across species. Trends in Neurosciences, 38(12), 800–812. 10.1016/j.tins.2015.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luck SJ, & Vogel EK (1997). The capacity of visual working memory for features and conjunctions. Nature, 390(6657), 279–281. 10.1038/36846 [DOI] [PubMed] [Google Scholar]
- Luck SJ, & Vogel EK (2013). Visual working memory capacity: from psychophysics and neurobiology to individual differences. Trends in Cognitive Sciences, 17(8), 391–400. 10.1016/j.tics.2013.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustig C, & Jantz T (2015). Questions of age differences in interference control: When and how, not if? Brain Research, 1612, 59–69. 10.1016/j.brainres.2014.10.024 [DOI] [PubMed] [Google Scholar]
- Lustig C, Hasher L, & Zacks RT (2007). Inhibitory deficit theory: Recent developments in a “new view.” In Gorfein DS & MacLeod CM (Eds.), Inhibition in Cognition (Vol. 17, pp. 145–162). Washington, DC: Inhibition in cognition; 10.1037/11587-008 [DOI] [Google Scholar]
- Lynn SK, Ibagon C, Bui E, Palitz SA, Simon NM, & Barrett LF (2016). Working memory capacity is associated with optimal adaptation of response bias to perceptual sensitivity in emotion perception. Emotion, 16(2), 155–163. 10.1037/emo0000111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maglione JE, Ancoli-Israel S, Peters KW, Paudel ML, Yaffe K, Ensrud KE, & Stone KL (2014). Subjective and objective sleep disturbance and longitudinal risk of depression in a cohort of older women. Sleep, 37(7), 1179–1187. 10.5665/sleep.3834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews A, & MacLeod C (1994). Cognitive approaches to emotion and emotional disorders. Annual Review of Psychology, 45(1), 25–50. 10.1146/annurev.ps.45.020194.000325 [DOI] [PubMed] [Google Scholar]
- Mellor A, Waters F, Olaithe M, McGowan H, & Bucks RS (2014). Sleep and aging: Examining the effect of psychological symptoms and risk of sleep-disordered breathing. Behavioral Sleep Medicine, 12(3), 222–234. 10.1080/15402002.2013.801343 [DOI] [PubMed] [Google Scholar]
- Meng XL, Rosenthal R, & Rubin DB (1992). Comparing correlated correlation coefficients. Psychological Bulletin, 111(1), 172–175. 10.1037/0033-2909.111.1.172 [DOI] [Google Scholar]
- Nebes RD, Buysse DJ, Halligan EM, Houck PR, & Monk TH (2009). Self-reported sleep quality predicts poor cognitive performance in healthy older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 64(2), 180–187. 10.1093/geronb/gbn037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noack H, Lövdén M, & Lindenberger U (2012). Normal aging increases discriminal dispersion in visuospatial short-term memory. Psychology and Aging, 27(3), 627–637. 10.1037/a0027251 [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Carskadon MA, Guilleminault C, & Vitiello MV (2004). Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep, 27(7), 1255–1273. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Zulley J, Guilleminault C, Smirne S, & Priest RG (2001). How age and daytime activities are related to insomnia in the general population: consequences for older people. Journal of the American Geriatrics Society, 49(4), 360–366. [DOI] [PubMed] [Google Scholar]
- Park DC, Lautenschlager G, Hedden T, Davidson NS, Smith AD, & Smith PK (2002). Models of visuospatial and verbal memory across the adult life span. Psychology and Aging, 17(2), 299–320. 10.1037/0882-7974.17.2.299 [DOI] [PubMed] [Google Scholar]
- Peich M-C, Husain M, & Bays PM (2013). Age-related decline of precision and binding in visual working memory. Psychology and Aging, 28(3), 729–743. 10.1037/a0033236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertzov Y, Heider M, Liang Y, & Husain M (2015). Effects of healthy ageing on precision and binding of object location in visual short term memory. Psychology and Aging, 30(1), 26–35. 10.1037/a0038396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2014). R: A language and environment for statistical computing. Retrieved August 15, 2014, from http://www.R-project.org/
- Rana BK, Panizzon MS, Franz CE, Spoon KM, Jacobson KC, Xian H, … & Kremen WS (2018). Association of Sleep Quality on Memory-Related Executive Functions in Middle Age. Journal of the International Neuropsychological Society, 24(1), 67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmeichel BJ, Volokhov RN, & Demaree HA (2008). Working memory capacity and the self-regulation of emotional expression and experience. Journal of Personality and Social Psychology, 95(6), 1526–1540. 10.1037/a0013345 [DOI] [PubMed] [Google Scholar]
- Smith ME, McEvoy LK, & Gevins A (2002). The impact of moderate sleep loss on neurophysiologic signals during working-memory task performance. Sleep, 25(7), 784–794. [PMC free article] [PubMed] [Google Scholar]
- Souza AS (2016). No age deficits in the ability to use attention to improve visual working memory. Psychology and Aging, 31(5), 456–470. 10.1037/pag0000107 [DOI] [PubMed] [Google Scholar]
- Sözeri-Varma G (2012). Depression in the elderly: clinical features and risk factors. Aging and Disease, 3(6), 465–471. [PMC free article] [PubMed] [Google Scholar]
- Unruh ML, Redline S, An M-W, Buysse DJ, Nieto FJ, Yeh J-L, & Newman AB (2008). Subjective and Objective Sleep Quality and Aging in the Sleep Heart Health Study. Journal of the American Geriatrics Society, 56(7), 1218–1227. 10.1111/j.1532-5415.2008.01755.x [DOI] [PubMed] [Google Scholar]
- Verstraeten E, Cluydts R, Pevernagie D, & Hoffmann G (2004). Executive function in sleep apnea: controlling for attentional capacity in assessing executive attention. Sleep, 27(4), 685–693. [PubMed] [Google Scholar]
- Waters F, & Bucks RS (2011). Neuropsychological effects of sleep loss: Implication for neuropsychologists. Journal of the International Neuropsychological Society, 17(4), 571–586. 10.1017/S1355617711000610 [DOI] [PubMed] [Google Scholar]
- Wee N, Asplund CL, & Chee MWL (2013). Sleep deprivation accelerates delay-related loss of visual short-term memories without affecting precision. Sleep, 36(6), 849–856. 10.5665/sleep.2710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie W, & Zhang W (2016). Negative emotion boosts quality of visual working memory representation. Emotion, 16(5), 760–774. 10.1037/emo0000159 [DOI] [PubMed] [Google Scholar]
- Xie W, & Zhang W (2017a). Dissociations of the number and precision of visual short-term memory representations in change detection. Memory & Cognition, 45(8), 1423–1437. 10.3758/s13421-017-0739-7 [DOI] [PubMed] [Google Scholar]
- Xie W, & Zhang W (2017b). Familiarity increases the number of remembered Pokémon in visual short-term memory. Memory & Cognition, 45(4), 677–689. 10.3758/s13421-016-0679-7 [DOI] [PubMed] [Google Scholar]
- Xie W, Li H, Ying X, Zhu S, Fu R, Zou Y, & Cui Y (2017). Affective bias in visual working memory is associated with capacity. Cognition and Emotion, 31(7), 1345–1360. 10.1080/02699931.2016.1223020 [DOI] [PubMed] [Google Scholar]
- Xie W, Cappiello M, Park H-B, Deldin P, Chan RCK, & Zhang W (2018a). Schizotypy is associated with reduced mnemonic precision in visual working memory. Schizophrenia Research, 193, 91–97. 10.1016/j.schres.2017.07.046 [DOI] [PubMed] [Google Scholar]
- Xie W, Li H, Zou Y, Sun X, & Shi C (2018b). A suicidal mind tends to maintain less negative information in visual working memory. Psychiatry Research, 262, 549–557. 10.1016/j.psychres.2017.09.043 [DOI] [PubMed] [Google Scholar]
- Zawadzki MJ, Graham JE, & Gerin W (2013). Rumination and anxiety mediate the effect of loneliness on depressed mood and sleep quality in college students. Health Psychology, 32(2), 212–222. 10.1037/a0029007 [DOI] [PubMed] [Google Scholar]
- Zhang W, & Luck SJ (2008). Discrete fixed-resolution representations in visual working memory. Nature, 453(7192), 233–235. 10.1038/nature06860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, & Luck SJ (2009). Sudden death and gradual decay in visual working memory. Psychological Science, 20(4), 423–428. 10.1111/j.1467-9280.2009.02322.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, & Luck SJ (2011). The number and quality of representations in working memory. Psychological Science, 22(11), 1434–1441. 10.1177/0956797611417006 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.