Abstract
Childhood maltreatment is associated with increased risk for most forms of psychopathology. We examine emotion dysregulation as a transdiagnostic mechanism linking maltreatment with general psychopathology. A sample of 262 children and adolescents participated; 162 (61.8%) experienced abuse or exposure to domestic violence. We assessed four emotion regulation processes (cognitive reappraisal, attention bias to threat, expressive suppression, and rumination) and emotional reactivity. Psychopathology symptoms were assessed concurrently and at a 2-year longitudinal follow-up. A general psychopathology factor (p factor), representing co-occurrence of psychopathology symptoms across multiple internalizing and externalizing domains, was estimated using confirmatory factor analysis. Maltreatment was associated with heightened emotional reactivity and greater use of expressive suppression and rumination. The association of maltreatment with attention bias varied across development, with maltreated children exhibiting a bias toward threat and adolescents a bias away from threat. Greater emotional reactivity and engagement in rumination mediated the longitudinal association between maltreatment and increased general psychopathology over time. Emotion dysregulation following childhood maltreatment occurs at multiple stages of the emotion generation process, in some cases varies across development, and serves as a transdiagnostic mechanism linking child maltreatment with general psychopathology.
Keywords: adversity, attention bias, p factor, rumination, threat
Exposure to maltreatment in childhood is a potent risk factor for psychopathology that accounts for a substantial proportion of mental disorders in the population (Green et al., 2010; Kessler et al., 2010; McLaughlin et al., 2012). US population-based studies estimate that approximately between 1 in 10 and 1 in 4 children will experience physical, sexual, or emotional abuse or exposure to some other form of violence within the family by the time they reach adulthood (Finkelhor, Shattuck, Turner, & Hamby, 2014; Finkelhor, Turner, Shattuck, & Hamby, 2013; McLaughlin et al., 2012). Exposure to child maltreatment is associated with elevated risk for virtually all forms of psychopathology, including mood, anxiety, disruptive behavior, substance abuse, and psychotic disorders (Cicchetti & Toth, 2005; Green et al., 2010; Kessler et al., 2010; McGrath et al., 2017; McLaughlin et al., 2012; Schaefer et al., 2018). Identifying mechanisms linking child maltreatment to the onset of psychopathology is critical for developing more effective early interventions. In this paper, we examine relationships between maltreatment and emotion regulation strategies within the framework of a leading conceptual model of emotion regulation. We additionally evaluate whether the associations between maltreatment and emotion regulation strategies vary across development, and test whether emotion dysregulation serves as a mechanism linking maltreatment with transdiagnostic risk for psychopathology.
Emotion Regulation and the Process Model
Emotion regulation has been defined as the “processes responsible for monitoring evaluating and modifying emotional reactions, especially their intensive and temporal features, to accomplish one’s goals” (Thompson, 1994). Emotion regulation encompasses a wide range of specific component processes that can occur at different points in the emotion generation process. The process model of emotion regulation (Gross, 1998b, 2014; Gross & Thompson, 2007) is a leading conceptual framework for organizing emotion regulation strategies. This model outlines four temporal stages involved in the generation and expression of an emotional response: (a) an emotional response is triggered by an internal or external situation; (b) attention is allocated to that situation; and (c) an appraisal is generated. An emotional response occurs when a situation is appraised as being relevant to one’s goals, and a wide range of (d) responses can occur following that emotional experience.
Emotion regulation can occur at every stage of this process (Gross, 1998b, 2014; Gross & Thompson, 2007). Individual strategies for emotion regulation can be either adaptive or maladaptive (Aldao & Nolen-Hoeksema, 2010, 2012b) and vary in their efficacy at influencing emotional reactions (Gross, 1998a; Gross & John, 2003; Webb, Miles, & Sheeran, 2012). These strategies generally fall into one of two categories: “antecedent focused” or “response focused.” Antecedent-focused strategies occur before or during the first three stages of the emotion process (situation, attention, and appraisal) and have been shown be effective at modulating the intensity and duration of emotional responses (Gross, 1998a; Gross & John, 2003; Webb et al., 2012). Response-focused strategies, in contrast, occur during the response phase of the emotion regulation model and, paradoxically, may actually increase emotion intensity (Gross, 1998a; Gross & Levenson, 1997; John & Gross, 2004). For that reason, response-focused strategies are generally considered to be maladaptive (Gross & John, 2003; Nolen-Hoeksema & Aldao, 2011).
Two common antecedent-focused emotion regulation strategies include cognitive reappraisal and attention deployment. Cognitive reappraisal involves thinking about an emotional situation in a different way in order to alter one’s emotional response, and is considered an effective and adaptive form of emotion regulation in most situations (Aldao & Nolen-Hoeksema, 2010, 2012a, 2012b; Gross & John, 2003; Nolen-Hoeksema & Aldao, 2011; Webb et al., 2012). Attention deployment involves the manipulation of attention either toward or away from an emotional stimulus. Habitual biases toward particular types of emotion-generating stimuli can be considered a rapid, unconscious form of attention deployment (Todd, Cunningham, Anderson, & Thompson, 2012).
Response-focused strategies include expressive suppression and rumination. Expressive suppression involves modulation of the outward expression of emotion. Its efficacy at modulating emotional responses is limited to their expression, however, and both the physiological and subjective experience of emotions is intensified by use of this strategy (Gross, 1998a; Gross & Levenson, 1997). Rumination involves passive, repetitive self-focused thinking about the causes and consequences of distress, while failing to engage in problem solving to alleviate the source of distress (Nolen-Hoeksema & Morrow, 1991; Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008). Experimental evidence suggests that rumination increases negative affect (McLaughlin, Borkovec, & Sibrava, 2007), leads to other forms of negative, maladaptive thinking (Lyubomirsky, Caldwell, & Nolen-Hoeksema, 1998), and reduces engagement in more effective strategies to alleviate negative mood (Lyubomirsky & Nolen-Hoeksema, 1993).
Development of Emotion Regulation and Reactivity
The utilization of specific emotion regulation strategies and the effectiveness of particular strategies at modulating emotional responses varies from middle childhood through adolescence (Gresham & Gullone, 2012; Gullone, Hughes, King, & Tonge, 2010; Silvers et al., 2012, 2017b). Attention biases toward threat are detectable as early as infancy (Lobue & Deloache, 2010) and tend to decrease with age from childhood through adolescence (Lonigan & Vasey, 2009; Reinholdt-Dunne, Mogg, Esbjorn, & Bradley, 2012). This developmental shift may indicate an increasing capacity to effortfully direct attention away from threat as an emotion regulation strategy (Morales, Fu, & Pérez-Edgar, 2016). The strength of the association between anxiety and attention biases toward threat increases with age (Dudeney, Sharpe, & Hunt, 2015), suggesting that a failure to develop this emotion regulatory strategy may contribute to psychopathology. The use of cognitive reappraisal has been found to remain relatively consistent across development (Gresham & Gullone, 2012; Gullone et al., 2010), but the effectiveness of cognitive reappraisal use at reducing negative affect increases from middle childhood through adolescence (McRae et al., 2012; Silvers et al., 2012, 2017a). Use of expressive suppression decreases from childhood to middle adolescence, then remains at the same level into adulthood (Gresham & Gullone, 2012; Gullone et al., 2010). The observed developmental trajectories of rumination across middle childhood and adolescence are inconsistent across studies (Abela, Hankin, Sheshko, Fishman, & Stolow, 2012; Hankin, 2008; Jose & Brown, 2008), but individual differences in the tendency to engage in rumination are quite stable (Ziegert & Kistner, 2002), bolstered by reciprocal relations between rumination and psychopathology over time (Nolen-Hoeksema, Stice, Wade, & Bohon, 2007).
The continued development of emotion regulation tendencies and competency across adolescence corresponds with a concurrent peak in emotional reactivity, as indicated by greater emotional volatility and intensity compared to childhood and adulthood (Gunnar, Wewerka, Frenn, Long, & Griggs, 2009; Guyer, Silk, & Nelson, 2016; Larson, Moneta, Richards, & Wilson, 2002; Stroud et al., 2009). This peak in emotional reactivity in adolescence, while systems of cognitive control and emotion regulation are still developing, is the basis of influential models explaining the rise in risk-taking behaviors and the emergence of psychopathology in adolescence (Ernst, Pine, & Hardin, 2006; Shulman et al., 2016; Somerville, Jones, & Casey, 2010).
Maltreatment and Emotion Dysregulation
Emotion dysregulation has been conceptualized as a key mechanism linking child maltreatment with multiple forms of psychopathology (Beauchaine, 2015; Heleniak, Jenness, Vander Stoep, McCauley, & McLaughlin, 2016; Kim & Cicchetti, 2010; Maughan & Cicchetti, 2002; McLaughlin & Lambert, 2017). Emotion dysregulation is a pattern of emotion regulation that interferes with an individual’s goals (Beauchaine, 2015; Cole, Hall, & Hajal, 2017), either because of more habitual use of maladaptive emotion regulation strategies or because of failure to effectively implement adaptive emotion regulation strategies. Because emotion dysregulation involves the presence instead of the absence of problematic behavior or experiences, it may be easier to identify and observe than effective emotion regulation (Beauchaine, 2015). Maltreated children may lack adaptive emotion regulation skills because rather than scaffolding these skills, caregivers may model maladaptive strategies and punish emotional expressions (Cicchetti, Ackerman, & Izard, 1995; Kim & Cicchetti, 2010). Further, in an environment characterized by high levels of threat, regulatory patterns that promote vigilance to potential threats may contribute to immediate self-preservation, with trade-offs for adaptive functioning in other contexts (Frankenhuis & Del Giudice, 2012).
Child maltreatment has been associated with emotion dysregulation, as indicated by parent reports (Kim & Cicchetti, 2010) and behavioral observations (Maughan & Cicchetti, 2002; Shields & Cicchetti, 1997) in prior research. Moreover, child maltreatment has been linked to differences in many specific forms of emotion regulation (Heleniak et al., 2016; McLaughlin & Lambert, 2017). Critically, although the use and efficacy of emotion regulatory strategies varies across development (Dudeney et al., 2015; Gullone et al., 2010; Silvers et al., 2012), few studies have examined whether the association of child maltreatment with specific types of emotion regulation strategies varies by age.
Child maltreatment, particularly exposure to abuse, is associated with abnormal attention deployment to threatening stimuli (e.g., angry faces). Children who have experienced abuse are more perceptually sensitive to detecting anger in faces (Pollak, Cicchetti, Hornung, & Reed, 2000; Pollak & Kistler, 2002; Pollak & Sinha, 2002) and demonstrate patterns of neural activity that suggest greater attentional engagement toward and difficulty disengaging attention from angry faces (Pollak, 2003; Pollak & Tolley-Schell, 2003; Shackman, Shackman, & Pollak, 2007). Consistent with this increased sensitivity and attention to threat, children, adolescents, and young adults exposed to abuse and other forms of violence exhibit greater attention bias toward angry faces than those without a history of violence exposure (Briggs-Gowan et al., 2015; Miller, 2015; Pollak & Tolley-Schell, 2003; Swartz, Graham-Bermann, Mogg, Bradley, & Monk, 2011). However, several studies have also documented associations between maltreatment and attention biases away from threat in middle childhood and early adolescence (Kelly et al., 2015; Pine et al., 2005), suggesting avoidance of threat cues among maltreated children in this age range. This may be indicative of age-specific engagement of attentional avoidance as an emotion regulation strategy among maltreated youth during the transition to adolescence.
To our knowledge, no published studies have investigated the relation between child maltreatment and habitual use of cognitive reappraisal. However, in a neuroimaging study in which participants were trained to use reappraisal to downregulate emotional reactivity to emotional stimuli, reappraisal efficacy based on self-reported affect did not differ between maltreated and control participants. However, maltreated participants engaged prefrontal cortex regions associated with cognitive control to a greater degree than controls during cognitive reappraisal, perhaps indicating greater regulatory effort required to decrease negative affect (McLaughlin, Peverill, Gold, Alves, & Sheridan, 2015).
Greater effort might be required to effectively modulate negative emotions among maltreated children, in part, because they experience emotions more intensely than their nonmaltreated peers. Maltreatment has been consistently associated with heightened emotional reactivity, as indicated by self-reported reactivity to stress among adolescents and adults exposed to child maltreatment (Glaser, van Os, Portegijs, & Myin-Germeys, 2006; Heleniak et al., 2016; McLaughlin et al., 2010). In addition, maltreatment is associated with greater reactivity to negative stimuli in brain regions known to respond to emotional salience, including the amygdala (Hein & Monk, 2017; McCrory et al., 2011; McLaughlin et al., 2015; Viding et al., 2012). Thus, maltreated children and adolescents experiencing more intense emotions may both contribute to and result from difficulties with emotion regulation.
Response-focused emotion regulation strategies have also been associated with child maltreatment. Parenting practices characterized by low monitoring, inconsistent discipline, and corporal punishment are associated with greater use of expressive suppression in children (Balan, Dobrean, Roman, & Balazsi, 2017). Exposure to multiple types of stressors in development, including maltreatment, is associated with greater propensity to engage in rumination (Conway, Mendelson, Giannopoulos, Csank, & Holm, 2004; Heleniak et al., 2016; LeMoult et al., 2018; McLaughlin & Hatzenbuehler, 2009; Michl, McLaughlin, Shepherd, & Nolen-Hoeksema, 2013). Children and adolescents exposed to maltreatment may attempt to suppress intrusive and intense negative emotions, and, when unsuccessful, dwell on those feelings, thereby increasing their duration. Taken together, these findings suggest that maltreatment exposure may interfere with children and adolescents’ ability to employ adaptive, antecedent-focused emotion regulation strategies, while increasing their emotional reactivity and tendency to utilize maladaptive, response-focused strategies. These specific manifestations of emotion dysregulation are likely to be a key pathway explaining increased risk for psychopathology following child maltreatment.
Emotion Dysregulation and Psychopathology
Emotion dysregulation is a transdiagnostic mechanism contributing to virtually all common types of psychopathology in adults and adolescents (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Burns, Jackson, & Harding, 2010; O’Mahen, Karl, Moberly, & Fedock, 2015) as well as comorbidity across different forms of psychopathology (McLaughlin, Aldao, Wisco, & Hilt, 2014; McLaughlin & Nolen-Hoeksema, 2011; Messman-Moore & Bhuptani, 2017). Emotion dysregulation resulting from early adversity is thought to exacerbate traitlike vulnerabilities, such as impulsivity or behavioral inhibition, leading to more severe manifestations of psychopathology symptoms transdiagnostically (Beauchaine, 2015). Emotion dysregulation has been found to mediate associations between maltreatment and several specific types of psychopathology, including depression (O’Mahen et al., 2015), self-harm (Peh et al., 2017), posttraumatic stress disorder (PTSD; Burns et al., 2010), and comorbid substance use, eating disorders, and borderline personality disorder among those with PTSD (Messman-Moore & Bhuptani, 2017). Given these associations, it is likely that emotion dysregulation represents a transdiagnostic mechanism that contributes to elevated risk for many forms of psychopathology following exposure to child maltreatment (Beauchaine & Zisner, 2017; Carver, Johnson, & Timpano, 2017).
One approach to capturing the nonspecific relationship between emotion dysregulation and psychopathology involves the use of a hierarchical measure of general psychopathology labeled the “p factor.” Conceptually similar to the “g factor” of general intelligence, “p” captures shared liability to common mental disorders across the internalizing and externalizing psychiatric spectra and predicts general life impairment, including educational attainment, employment, social service use, and criminal activity (Caspi et al., 2014; Lahey et al., 2012; Lahey, Krueger, Rathouz, Waldman, & Zald, 2017; Patalay et al., 2015). Since its first presentation in initial reports, “p” has been computed with similar structure and correlates in studies of children, adolescents, and adults; across studies from many different parts of the world; and across studies that assess psychiatric symptoms using different measures, including self-reports, parent reports, and teacher reports (Caspi et al., 2014; Castellanos-Ryan et al., 2016; Gomez, Stavropoulos, Vance, & Griffiths, 2018; Laceulle, Vollebergh, & Ormel, 2015; Martel et al., 2017; Murray, Eisner, & Ribeaud, 2016; Neumann et al., 2016; Patalay et al., 2015; Schaefer et al., 2018; Snyder, Young, & Hankin, 2017). Critically, several studies have shown that child maltreatment increases this transdiagnostic psychopathology with no residual associations with specific symptoms types after accounting for the links with this latent factor (Caspi et al., 2014; Keyes et al., 2012). The p factor is therefore a useful tool for quantifying, in a single variable, co-occurrence of multiple types of psychopathology symptoms associated with childhood maltreatment. Emotion dysregulation may be a key mechanism through which maltreatment increases risk for general psychopathology (Beauchaine & Zisner, 2017; Carver et al., 2017).
The Current Study
The current study investigated the role of emotion dysregulation as a transdiagnostic mechanism linking childhood maltreatment to the development of psychopathology. First, we hypothesized that child maltreatment would be associated with lower levels of adaptive, antecedent-focused emotion regulation strategies (i.e., attention deployment and cognitive reappraisal) and greater use of maladaptive, response-focused emotion regulation strategies (i.e., expressive suppression and rumination). We also expected to replicate the well-established finding of heightened emotional reactivity in children who had been maltreated. Second, we expected that maltreatment would interact with age in relation to attention biases toward threat, such that younger participants exposed to maltreatment would show larger attentional biases toward threat than older participants exposed to maltreatment, who might be more capable of effortfully regulating their attention. Third, we predicted that lower use of adaptive antecedent-focused emotion regulation strategies, greater use of maladaptive response-focused emotion regulation strategies, and heightened emotional reactivity would each be associated with higher scores on our measure of general psychopathology, and would mediate the association between child maltreatment and this outcome.
Method
Sample
Youth aged 8–16 years and a parent or guardian were recruited to participate in a study examining child trauma exposure, emotion regulation, and psychopathology. A total of 262 youth aged 8–16 years were enrolled into the study. Exposure to maltreatment and other inclusion and exclusion criteria were assessed during the first study visit, along with several behavioral and self-report measures of emotion regulation. Youth and caregivers were recruited for participation at schools, after-school and prevention programs, adoption programs, food banks, shelters, parenting programs, medical clinics, and the general community in Seattle, Washington, between January 2015 and June 2017. Recruitment efforts were targeted at recruiting a sample with variation in exposure to maltreatment-related trauma. To do so, we recruited from neighborhoods with high levels of violent crime, from clinics that served a predominantly low-socioeconomic status catchment area, and agencies that work with families who have been victims of violence (e.g., domestic violence shelters and programs for parents mandated to receive intervention by Child Protective Services). Inclusion criteria for the maltreated group included exposure to physical or sexual abuse or direct witnessing of domestic violence. Children in the control group were matched to children in the maltreated group on age, sex, and handedness; inclusion criteria required an absence of exposure to maltreatment or other forms of significant interpersonal violence. Exclusion criteria included IQ < 80, presence of pervasive developmental disorder, active psychotic symptoms or mania, active substance abuse, and presence of safety concerns. IQ was measured with the Wechsler Abbreviated Intelligence Scale (Wechsler, 2011) in the first study visit. Pervasive developmental disorders were assessed via parent report. Of the 262 children enrolled in the first study visit, 3 were excluded from all analysis due to low IQ (n = 1), presence of pervasive developmental disorder (n = 1), and presence of psychotic symptoms and drug abuse (n = 1). The total sample size for the present analysis was 259 children and adolescents. A longitudinal follow-up assessment was conducted approximately 2 years following the baseline assessments (M = 21.96 months, SD = 7.88 months) to assess symptoms of psychopathology. A total of 198 children and adolescents (76.4%) completed a follow-up visit. Of the 65 children who dropped out, 44 were maltreated (28% attrition) and 21 were not (20% attrition; χ2 = 2.38, p = .123).
All procedures were approved by the institutional review board at the University of Washington. Written informed consent was obtained from legal guardians; children provided written assent. Maltreatment not previously reported to the relevant authorities was reported to Child Protective Services using standard clinical procedures. Children with active safety concerns were not enrolled in the study. See Table 1 for sociodemographic characteristics of the sample.
Table 1.
Descriptive statistics and intercorrelations
| Maltreated | Control | Cohen’s d | |||||
|---|---|---|---|---|---|---|---|
| N | M | SD | N | M | SD | ||
| 1. Age | 156 | 12.78 | 2.57 | 106 | 12.33 | 2.59 | 0.18 |
| 2. Maltreatment severity | 156 | 7.19 | 2.94 | 106 | 2.01 | 1.87 | 2.02 |
| 3. Threat bias (ms) | 153 | −4.55 | 35.12 | 105 | −8.55 | 38.65 | 0.11 |
| 4. Reappraisal | 145 | 27.05 | 7.93 | 101 | 27.94 | 6.86 | −0.12 |
| 5. Emotional reactivity | 153 | 18.80 | 16.65 | 104 | 6.77 | 8.60 | 0.86 |
| 6. Suppression | 145 | 15.41 | 5.91 | 101 | 14.11 | 5.32 | 0.23 |
| 7. Rumination | 154 | 12.51 | 8.85 | 106 | 8.83 | 7.61 | 0.44 |
| 8. P-factor (baseline) | 156 | 0.440 | 0.75 | 106 | −0.66 | 0.66 | 1.54 |
| 9. P-factor (follow-up) | 112 | 0.32 | 0.88 | 85 | −0.41 | 0.70 | 0.90 |
| Intercorrelations (full sample) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| 1 | – | ||||||||
| 2 | .19* | – | |||||||
| 3 | .11 | .06 | – | ||||||
| 4 | .04 | −.06 | .00 | – | |||||
| 5 | .16* | .40* | .04 | −.04 | – | ||||
| 6 | .11 | .13* | .01 | .10 | .09 | – | |||
| 7 | .35* | .25* | .08 | .01 | .63* | .21* | – | ||
| 8 | .15* | .66* | .05 | −.08 | .55* | .22* | .45* | – | |
| 9 | .30* | .52* | .12 | −.06 | .46* | .18* | .43* | .67* | – |
M, mean. SD, standard deviation. All pairwise, Pearson correlations
p < .05.
Measures
For younger children in the study (8–10 year olds) and those who had difficulty reading, all questionnaires were read out loud by a study team member to ensure comprehension of all items.
Child maltreatment
For the purposes of this study, child maltreatment was defined as exposure to traumatic violence or abuse within the family, including physical, sexual, and emotional abuse, and chronic exposure to domestic violence. We used a multi-informant, multimethod approach for assessing exposure to child maltreatment. Children completed two interviews with a trained member of our research team assessing child maltreatment experiences and exposure to interpersonal violence: the Childhood Experiences of Care and Abuse (CECA) Interview (Bifulco, Brown, & Harris, 1994) and the Violence Exposure Scale for Children—Revised (VEX-R; Raviv et al., 2001; Raviv, Raviv, Shimoni, Fox, & Leavitt, 1999). The CECA assesses caregiving experiences, including physical, sexual, and emotional abuse. We modified the interview to ask parallel questions about witnessing domestic violence (i.e., directly observing violence directed at a caregiver). Interrater reliability for maltreatment reports is excellent, and validation studies suggest high agreement between siblings on maltreatment reports (Bifulco, Brown, Lillie, & Jarvis, 1997). The VEX-R assesses the frequency of exposure to different forms of violence. Children are presented with a cartoon and caption depicting a child of the same sex witnessing a type of violence (e.g., “Chris sees a person slap another person really hard”) and experiencing that same type of violence (e.g., “A person slaps Chris really hard”). Children are then asked to report how frequently they have witnessed or experienced that type of violence (e.g., “How many times have you seen a person slap another person really hard?” or “How many times has a person slapped you really hard?”) on a Likert scale ranging from 0 (never) to 3 (lots of times). We added follow-up questions for each item that was endorsed to gather additional information (e.g., the perpetrator or age of onset). The VEX-R demonstrates good reliability and has been validated with children as young as second grade (Raviv et al., 1999, 2001).
Children also completed two self-report measures: the Childhood Trauma Questionnaire (CTQ; Bernstein, Ahluvalia, Pogge, & Handelsman, 1997) and the UCLA PTSD Reaction Index (PTSD-RI; Steinberg, Brymer, Decker, & Pynoos, 2004). The CTQ is a 28-item scale that assesses the frequency of maltreatment during childhood, including physical and sexual abuse. Validated thresholds for exposure to physical and sexual abuse (Walker et al., 1999) were applied here in evaluating abuse exposure based on the CTQ. The CTQ has excellent psychometric properties including internal consistency, test–retest reliability, and convergent and discriminant validity with interviews and clinician reports of maltreatment (Bernstein et al., 1994, 1997). The PTSD-RI includes a trauma screen that assesses exposure to numerous traumatic events, including physical abuse, sexual abuse, and domestic violence, and additionally assesses PTSD symptoms. The PTSD-RI has good internal consistency and convergent validity (Steinberg et al., 2013).
Caregivers completed three self-report measures: the Conflict Tactics Scale—Parent Child Version (CTS; Straus, Hamby, Finkelhor, Moore, & Runyan, 1998), the Juvenile Victimization Questionnaire (JVQ) lifetime caregiver report (Finkelhor, Hamby, Ormrod, & Turner, 2005), and the caregiver version of the PTSD-RI. The CTS includes 22 items assessing caregiver responses to child disobedience or misbehavior in the past year. Caregivers indicate how frequently they have used each strategy (e.g., shook him/her) on a Likert scale ranging from 0 (this has never happened) to 6 (more than 20 times in the past year) and can also indicate if they have used the strategy in the past but not in the last year. The CTS has adequate reliability and good discriminant and construct validity (Straus et al., 1998). The JVQ includes 34 items assessing exposure to crime, child maltreatment, peer and sibling victimization, sexual victimization, and witnessing and indirect victimization and has excellent psychometric properties, including test–retest reliability and construct validity (Finkelhor et al., 2005). Caregivers endorsed whether their child had experienced each event in his/her lifetime. Caregivers also completed the trauma screen included in the PTSD-RI, described above. A trained interviewer followed up with the caregiver if he/she endorsed any form of abuse or domestic violence to gather additional information about the experience.
Children were classified as experiencing physical or sexual abuse if abuse was endorsed by the child (on the CECA interview, PTSD-RI trauma screen, or above the validated CTQ threshold) or parent (on the CTS, JVQ, or PTSD-RI trauma screen). A total of 100 children (38.6%) experienced physical or sexual abuse. Interrater reliability was fair to good for child and caregiver reports (82.0% agreement; κ = .62). Exposure to emotional abuse (above the validated threshold on either the CECA or the CTQ) and domestic violence (on the VEX-R interview or the PTSD-RI trauma screen) was determined based on child report only. A total of 82 children (31.7%) reported experiencing emotional abuse, and 99 children (38.2%) reported witnessing domestic violence.
A maltreatment severity score was created by summing the total number of types of maltreatment and violence exposure experienced by the child, including physical abuse, sexual abuse, emotional abuse, domestic violence, and exposure to violence in the broader community. Each type of maltreatment or violence exposure was coded as present or absent, and these indicators were summed to create a severity score.
Emotional reactivity and regulation
Attention bias to threat.
A visual dot-probe task using affective faces was administered to assess attention bias to threat. This task has been widely used as a measure of attention bias to threat in children and adolescents (Briggs-Gowan et al., 2015; Pérez-Edgar et al., 2010; Waters, Henry, Mogg, Bradley, & Pine, 2010). Task stimuli consisted of face pairs with one angry face and one neutral face from the same actor, selected from the NimStim stimulus set (Tottenham, Borscheid, Ellertsen, Marcus, & Nelson, 2002). The task included 16 practice trials followed by two experimental blocks of 80 trials each. Participants were randomly assigned to one of three pseudorandom orders of stimulus presentation. Each trial began with a central fixation cross presented for 500 ms, followed by an angry–neutral face pair presented for 500 ms, followed immediately by a small white arrow, pointing either left or right, displayed for 500 ms. The arrow appeared in the space previously occupied by the center of one of the two face pictures. Angry faces were presented with equal frequency on either the right or the left side of the screen. Left and right arrows appeared with equal frequency in the location of the angry or neutral face. Participants were instructed to press the arrow key on the keyboard corresponding to the arrow on the screen, as quickly as possible, avoiding mistakes. Accuracy and response times were recorded. A measure of attention bias toward threat was obtained by subtracting the mean response time on correct trials when the arrow appeared behind the angry face, from mean response time on correct trials when the arrow appeared behind the neutral face. Positive scores indicate an attention bias toward threat; negative scores indicate attention away from threat.
Rumination.
The Children’s Response Styles Questionnaire (Abela, Brozina, & Haigh, 2002) is a 25-item scale that assesses the extent to which children respond to sad feelings with rumination, defined as self-focused thought concerning the causes and consequences of depressed mood, distraction, or problem solving. The measure is modeled after the Response Styles Questionnaire (Nolen-Hoeksema & Morrow, 1991) that was developed for adults. For each item, youth are asked to rate how often they respond in that way when they feel sad on a 4-point Likert scale ranging from almost never (1) to almost always (4). The rumination subscale includes 13 items that are summed, with higher scores indicating greater habitual engagement of rumination. Sample items include: “Think about a recent situation wishing it had gone better” and “Think why can’t I handle things better?” The Children’s Response Styles Questionnaire has demonstrated good psychometric properties (Abela et al., 2002) and had good internal consistency in this sample (α = 0.91).
Reappraisal and suppression.
The Emotion Regulation Questionnaire (ERQ; Gross & John, 2003) is a 10-item self-report questionnaire assessing the tendency to use cognitive reappraisal and expressive suppression. Six items pertain to cognitive reappraisal (e.g., “I control my emotions by changing the way I think about the situation I’m in”), and 4 pertain to expressive suppression (e.g., “I control my emotions by not expressing them”). Responses are provided on a 7-point Likert scale ranging from strongly disagree (1) to strongly agree (7). Separate sum scores are calculated for cognitive reappraisal and expressive suppression. Higher scores indicate a greater tendency to use that strategy. Both the reappraisal (α = 0.84) and the expressive suppression subscales (α = 0.75) demonstrated adequate internal consistency in this sample.
Emotional reactivity.
The Emotion Reactivity Scale (ERS) is a 21-item scale that assesses stable patterns of emotional reactivity (Nock, Wedig, Holmberg, & Hooley, 2008). The ERS asks participants to think about how they experience emotions on a regular basis, such as anger, sadness, excitement, or other emotions. The ERS items assess emotional sensitivity (8 items; e.g., “I tend to get emotional very easily”), arousal/intensity of emotional experiences (10 items; e.g., “When I experience emotions, I feel them very strongly/intensely”), and persistence of emotions (3 items; e.g., “When I am angry/upset, it takes me much longer than most people to calm down”), which are summed to create an overall emotion reactivity score. Participants rate each item on a 5-point Likert scale ranging from not at all like me (0) to completely like me (4), with a total possible score ranging from 0 to 84. The ERS has demonstrated excellent reliability and validity among adolescents (Nock et al., 2008), and demonstrated excellent internal consistency in this study (α = 0.92).
Income-to-needs ratio
Income-to-needs ratio was calculated by dividing the parent-reported family income by the poverty threshold for a family of that size as indicated by the US Census Bureau (www.census.gov/hhes/www/poverty/data/threshld/). Family income was not reported for 17 participants (12 maltreated). Multiple imputation with 100 imputations was conducted using the mice package in R (Van Buuren & Groothuis-Oudshoorn, 2011) to estimate income in all regression analyses. For mediation analyses, the mean income of all other maltreated children was imputed for all maltreated children missing income data, and the mean income of all other nonmaltreated children was imputed for all nonmaltreated children with missing income data.
Symptoms of psychopathology
Depression symptoms were assessed with the Children’s Depression Inventory—Second edition (CDI-2), a recently revised version of the widely used self-report measure of depressive symptoms in children and adolescents (Kovacs, 1992, 2011). The CDI has demonstrated good reliability and validity among children and adolescents (Craighead, Smucker, Craighead, & Ilardi, 1998). The CDI demonstrated excellent internal consistency in our sample (α = 0.89). Anxiety symptoms were assessed with the Screen for Child Anxiety Related Emotional Disorders (SCARED), which measures anxiety disorder symptoms across five domains: panic/somatic, generalized anxiety, separation anxiety, social phobia, and school phobia (Birmaher et al., 1997). The SCARED has sound psychometric properties (Birmaher et al., 1997, 1999) and excellent internal consistency in our sample (α = 0.94). Externalizing symptoms were assessed using both child and caregiver reports on the Youth Self-Report (YSR) and Child Behavior Checklist (CBCL; Achenbach, 1991). The YSR/CBCL scales are among the most widely used measures of youth emotional and behavioral problems. The higher raw score between the CBCL and YSR was used from the attention problems, rule-breaking behaviors, and aggressive behavior subscales. Symptoms of PTSD were assessed using child- and parent-report versions of the PTSD-RI (Steinberg et al., 2004). The PTSD-RI assesses PTSD reexperiencing, avoidance/numbing, and hyper-arousal symptoms according to DSM-IV criteria. A total symptom severity score is generated by summing all items. The PTSD-RI has sound psychometric properties (Steinberg et al., 2013), and had excellent internal consistency in our sample (α = 0.92). The higher of the parent- and child-reported PTSD symptom severity score was used. Given that half our sample was recruited for exposure to maltreatment, these psychopathology indicators were positively skewed and kurtotic (skewness values above 1 ranged from 1.1 to 2.27; kurtosis values above 1 ranged from 1.1 to 6.94). We used each of these indicators to define “p.”
Defining p factor
Following Caspi et al. (2014) and recent replications (Laceulle et al., 2015; Schaefer et al., 2018), we performed confirmatory factor analysis (CFA) to test two standard models: a correlated-factors model specifying internalizing and externalizing latent factors and a bifactor model specifying both a general psychopathology latent factor (“p”) and residual internalizing and externalizing factors (Figure 1). In order to ensure that our latent factors were not being driven by one or more indicators simply because of measurement differences across psychopathology instruments (i.e., different number of items, scoring, etc.), we binned scores on each indicator into deciles prior to CFA analyses. All CFA analyses were performed in MPlus version 8.1 (Muthén & Muthén, 2012). Given that our observed indicator variables were slightly skewed and kurtotic, we used the robust maximum likelihood estimator, which employs a sandwich estimator to arrive at standard errors robust to nonnormality of observations. The robust maximum likelihood estimator performs well in modest sample sizes with skewed data, as in the present study (Li, 2016). We assessed the relative fit of each model using the Akaike information criterion (AIC), Bayesian information criterion (BIC), and the sample adjusted BIC. Fit indices for the correlated-factors model were AIC = 6056.31, BIC = 6249.00, sample adjusted BIC = 6077.79. Standardized factor loadings for the internalizing (CDI, SCARED, PTSD) latent factor ranged from 0.65 to 0.73, all ps < .001. Standardized factor loadings for the externalizing (aggressive behaviors, rule-breaking behaviors, and attention problem) latent factor ranged from 0.76 to 0.87, all ps < .001. Fit indices for the bifactor model were AIC = 6018.23, BIC = 6228.77, sample adjusted BIC = 6041.71. Standardized factor loadings for the latent p factor (CDI, SCARED, PTSD, aggressive behaviors, rule-breaking behaviors, and attention problems) ranged from 0.44 to 0.80, all ps < .001. Fit indices for the correlated factors model at follow-up were AIC = 4507.81, BIC = 4682.09, sample adjusted BIC = 4514.19. Standardized factor loadings for the internalizing factor ranged from 0.48 to 0.95, all ps < .001. Standardized factor loadings for the externalizing factor ranged from 0.76 to 0.84, all ps < .001. Fit indices for the bifactor model at the longitudinal follow-up were AIC = 4481.00, BIC = 4665.15, sample adjusted BIC = 4487.74. Standardized factor loadings for the latent p factor ranged from 0.46 to 0.81, all ps < .001. As assessed by relative fit indices and factor loadings, both models fit the data similarly well at the baseline assessment, with a relatively better fit for the bifactor model. In the present analyses, we used the bifactor model because it is the most commonly reported general factor model of psychopathology in the existing literature (Caspi et al., 2014; Greene & Eaton, 2017; Laceulle et al., 2015; Lahey et al., 2012; Martel et al., 2017; Murray et al., 2016; Olino, Dougherty, Bufferd, Carlson, & Klein, 2014; Patalay et al., 2015; Schaefer et al., 2018; Snyder et al., 2017), including in studies comparing the p factor in children with and without exposure to adversity.
Figure 1.
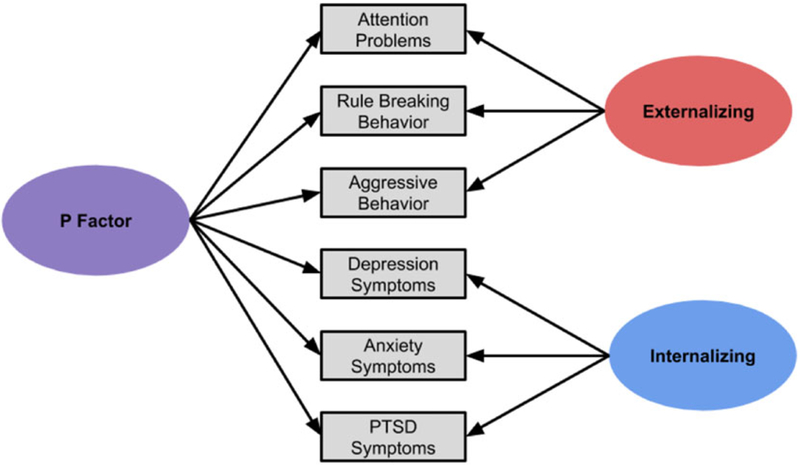
Factor structure of the bifactor model used to generate p factor scores from transdiagnostic symptom counts.
Our aim in estimating “p” in this sample was to condense an array of disparate psychiatric measures into a single transdiagnostic measure of psychopathology using a well-validated approach, not to characterize the latent structure of psychopathology in the general population. To ensure that our recruitment strategy did not unduly influence the latent structure of “p” in our sample, we fit the bifactor model separately in our maltreated participants and nonmaltreated controls. Because fit indices are sensitive to sample size and we had more maltreated cases than controls, we were not able to directly compare model fit indices. However, we examined standardized factor loadings to ensure that the models fit the data similarly in each group (see online-only Supplementary Materials for details). With the exception of rule-breaking behavior (.65 in maltreated youth, .37 in control youth) and PTSD (.73 in maltreated youth, .50 in control youth), factor loadings were very similar, and all standardized factor loadings were significant at p < .001 in both groups.
Analysis methods
Linear regression analyses were conducted in R (R Core Team, 2018) to examine each of our hypotheses. We examined the association of maltreatment exposure and maltreatment severity with threat bias, emotional reactivity, cognitive reappraisal, expressive suppression, and rumination. To evaluate whether these associations varied by age, we computed interactions of maltreatment exposure and severity with age and examined their association with threat bias, cognitive reappraisal, emotional reactivity, expressive suppression, and rumination. Significant interactions were visualized using the interActive data visualization tool (McCabe, Kim, & King, 2018). To determine how emotion regulation was related to psychopathology, we examined associations of threat bias, cognitive reappraisal, emotional reactivity, expressive suppression, and rumination with “p,” both at baseline and at the longitudinal follow-up controlling for “p” at baseline; these analyses controlled for maltreatment exposure. All analyses included covariates for racial/ethnic minority status and family income-to-needs ratio, as the maltreated and control groups differed on these variables. Regression analyses and mediation models predicting “p” at follow-up were conducted only among the 198 adolescents with follow-up data.
Mediation models with bootstrapped confidence intervals (10,000 iterations) were tested using version 2.13 of the process macro in SPSS (Hayes, 2013) for emotion regulation indices that were significantly related to both maltreatment exposure or severity and “p” at follow-up, controlling for “p” at baseline and maltreatment exposure or severity. We evaluated whether difficulties with emotion regulation mediated the association between maltreatment exposure and severity and “p” at the longitudinal follow-up, controlling for the effects of baseline “p,” racial/ethnic minority status, and income-to-needs ratio on “p.” Indices of maltreatment, emotional reactivity, and all control variables were collected concurrently. However, indices of maltreatment were retrospective. Data used to calculate “p” at follow-up was collected 2 years later.
Results
Descriptive statistics
Descriptive statistics for maltreated and control youth and intercorrelations of study variables are summarized in Table 1. Average reaction time during the dot-probe task was significantly faster for trials when the target was behind the neutral face than when it was behind the angry face, suggesting an attention bias away from threat in the total sample (M = –6.18, SD = 36.58, t = –2.71, p = .007). Cognitive reappraisal (M = 27.41, SD = 7.51) and expressive suppression (M = 14.88, SD = 5.70) were used at moderate levels in this sample, with mean totals over half of the maximum possible scores of 42 and 28, respectively. Rumination was somewhat less commonly used, with a mean score of 24.01 (SD = 8.64) out of a possible 52. Age was positively correlated with rumination (r = .35, p < .001) and emotional reactivity (r = .16, p = .009), but not threat bias (r = .11, p = .074), cognitive reappraisal (r = .04, p = .513), or expressive suppression (r = .11, p = .088). Indices of emotion regulation and emotional reactivity were mostly uncorrelated, with the exceptions that youth who reported greater rumination also reported greater expressive suppression (r = .21, p = .001) and emotional reactivity (r = .63, p < .001).
Maltreatment and antecedent-focused emotion regulation
Results of regression analyses relating maltreatment exposure and severity to emotion regulation are summarized in Tables 2 and 3. Neither maltreatment exposure (Table 2, Model 1) nor maltreatment severity (Table 2, Model 3) were associated with attention bias toward or away from threat. However, both maltreatment exposure (β = −.133, p = .038; Table 2, Model 2) and maltreatment severity (β = −.142, p = .030; Table 2, Model 4) interacted with age in predicting threat bias. In both cases, maltreatment exposure and greater maltreatment severity were associated with greater attention bias toward threat cues in children that disappeared during early adolescence and shifted to a significant attention bias away from threat in older adolescents (Figure 2). Neither maltreatment exposure nor severity was associated with cognitive reappraisal (Table 3). These associations did not vary with age.
Table 2.
Regression table of effects of maltreatment, age, and their interaction on attention bias to threat
| Model 1: Effect of maltreatment | Model 2: Age × Maltreatment | Model 3: Effect of maltreatment severity | Model 4: Age × Maltreatment Severity | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | p | B | SE | β | p | B | SE | β | p | B | SE | β | p | ||
| Income-to-needs | 0.946 | 1.08 | .070 | .382 | 0.705 | 1.07 | .052 | .511 | Income-to-needs | 0.493 | 1.01 | .036 | .626 | 0.287 | 1.00 | .021 | .775 |
| Race/ethnicity | 7.85 | 5.17 | .105 | .131 | 6.77 | 5.12 | .090 | .188 | Race/ethnicity | 8.37 | 5.19 | .112 | .109 | 7.40 | 5.13 | .099 | .151 |
| Maltreatment | 6.00 | 5.85 | .080 | .306 | 4.28 | 5.81 | .057 | .462 | Maltreatment Severity | 0.197 | 0.728 | .019 | .787 | 0.069 | 0.743 | .007 | .926 |
| Age | 4.13 | 1.46 | .122 | .005 | Age | 1.93 | 0.923 | .137 | .037 | ||||||||
| Age × Maltreatment | −3.86 | 1.85 | −.133 | .038 | Age × Maltreatment Severity | −0.557 | 0.255 | −.142 | .030 | ||||||||
| Model Summary | R2 = .02, p = .249 | R2 = .05, p = .010 | Model Summary | R2 = .01, p = .406 | R2 = .05. p = .045 | ||||||||||||
Note: Significant effects are in bold. B, unstandardized coefficient; β, standardized coefficient.
Table 3.
Regression tables of main effects of maltreatment and maltreatment severity on emotion reactivity and regulation
| Cognitive reappraisal | Emotion reactivity | Expressive suppression | Rumination | p | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | p | B | SE | β | P | B | SE | β | p | B | SE | β | ||
| Income-to-needs | 0.150 | 0.227 | .054 | .510 | 0.184 | 0.411 | .033 | .654 | −0.147 | 0.170 | −.069 | .389 | 0.199 | 0.248 | .063 | .423 |
| Race/ethnicity | 1.03 | 1.20 | .067 | .350 | 2.49 | 1.94 | .080 | .201 | −0.381 | 0.823 | −.033 | .643 | −0.21 | 1.19 | −.012 | .859 |
| Maltreatment Exposure | −0.030 | 1.23 | −.062 | .705 | 11.92 | 2.20 | .383 | <.001 | 1.44 | 0.926 | .123 | .120 | 5.29 | 1.34 | .301 | <.001 |
| Model Summary | R2 = .01, p = .692 | R2 = .16, p < .001 | R2 = .03, p = .335 | R2 = .07, p = .001 | ||||||||||||
| Cognitive reappraisal | Emotion reactivity | Expressive suppression | Rumination | p | ||||||||||||
| B | SE | β | p | B | SE | β | P | B | SE | β | p | B | SE | β | ||
| Income-to-needs | 0.114 | 0.213 | .041 | .593 | 0.085 | 0.357 | .015 | .812 | −0.121 | 0.158 | ‒.057 | .446 | 0.250 | 0.220 | .079 | .256 |
| Race/ethnicity | 1.14 | 1.10 | .074 | .302 | 1.62 | 1.83 | .052 | .378 | −0.533 | 0.816 | −.045 | .515 | −0.805 | 1.13 | −.046 | .479 |
| Maltreatment severity | −0.153 | 0.157 | −.074 | .329 | 2.02 | 0.255 | .482 | <.001 | 0.307 | 0.117 | .194 | .009 | 1.06 | 0.159 | .447 | <.001 |
| Model summary | R2 = .01, p = .510 | R2 = .26, p < .001 | R2 = .05, p = .047 | R2 = .17, p < .001 | ||||||||||||
Note: Significant effects are in bold. B, unstandardized coefficient. β, standardized coefficient.
Figure 2.
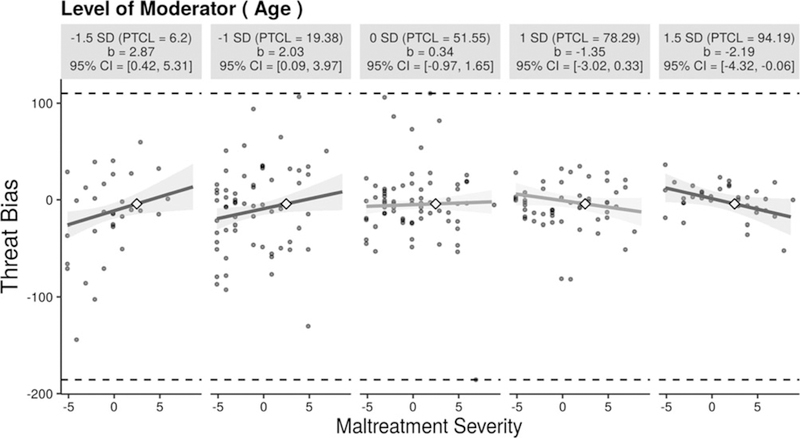
Attention bias toward threat increases significantly with increasing maltreatment severity for younger (1.5 SD below the mean = 8.7 and 1 SD below the mean = 10.0 year old) participants and decreases significantly with increasing maltreatment for the oldest (1.5 SD above the mean = 16.5 year old) participants. Figure produced using the interActive data visualization tool (McCabe, Kim, & King, 2018).
Maltreatment and emotional reactivity
Maltreatment exposure and severity were both positively associated with emotional reactivity (β = .383, p < .001), such that participants who experienced maltreatment and greater maltreatment severity reported greater emotional reactivity (Table 3). Age did not interact with maltreatment exposure or severity in predicting emotional reactivity.
Maltreatment and response-focused emotion regulation
Maltreatment exposure was unrelated to expressive suppression. However, maltreatment severity was positively associated with expressive suppression (β = .194, p = .009), such that participants who experienced more severe maltreatment reported using expressive suppression more frequently (Table 3). Age did not interact with maltreatment exposure or severity in predicting expressive suppression.
Rumination was positively associated with both maltreatment exposure (β = .301, p < .001) and maltreatment severity (β = .447, p < .001). Children who experienced maltreatment were more likely to ruminate than those who had never been maltreated, and greater maltreatment severity was associated with greater engagement in rumination (Table 3). Age did not interact with maltreatment exposure or severity in predicting rumination.
Emotion regulation and psychopathology
Associations of emotion regulation strategies and emotional reactivity with “p” scores at baseline and at the longitudinal follow-up, controlling for baseline, are summarized in Table 4. Coefficients and test statistics of the full models are available in the online-only Supplementary Materials. First, we examined antecedent-focused emotion regulation strategies. Biased attention to threat was not associated with “p” at baseline, but did significantly predict higher “p” scores at the follow-up (β = .134, p = .021), indicating that youth with greater attention biases toward threat demonstrated greater increases in psychopathology over time. Cognitive reappraisal was not associated with “p” at either baseline or follow-up. Second, youth with higher emotional reactivity had higher “p” at baseline (β = .379, p < .001), and marginally greater increases in “p” at follow-up (β = .128, p = .072). Finally, we examined response-focused strategies. Youth who used expressive suppression more had higher “p” at baseline (β = .167, p < .001), but not at follow-up, (β = .063, p = .299). Youth who engaged in rumination more frequently had higher “p” at baseline (β = .301, p < .001), and greater increases in “p” at the follow-up (β = .175, p = .004).
Table 4.
Associations of emotion regulation and reactivity with psychopathology
| P factor at baseline | P factor at follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | β | p | B | SE | β | p | |
| Threat bias | −.00094 | .00122 | −.038 | .439 | .00323 | .00139 | .134 | .021 |
| Cognitive reappraisal | −.00612 | .00600 | −.051 | .309 | .00228 | .00704 | .019 | .747 |
| Emotional reactivity | .0223 | .0029 | .379 | <.001 | .00740 | .00410 | .128 | .072 |
| Expressive suppression | .0262 | .0078 | .167 | <.001 | .00985 | .00945 | .063 | .299 |
| Rumination | .0316 | .0048 | .301 | <.001 | .0180 | .0062 | .175 | .004 |
Note: Significant effects are in bold. B, unstandardized coefficient. β, standardized coefficient. All models controlled for race/ethnicity and income-to-needs ratio. Results of full models are in online-only Supplemental Materials.
Indirect effects of maltreatment on psychopathology through emotion dysregulation
Because the component paths were at least marginally significant, we examined whether emotional reactivity and rumination at baseline mediated the association between maltreatment exposure and severity and “p” at the longitudinal follow-up, controlling for “p” at baseline (Figure 3a). The total effect of maltreatment on “p” at follow-up when controlling for “p” at baseline was not significant (c = −.017, p = .901), but it is well established that a significant c path is not required to test for indirect effects (Hayes, 2013; MacKinnon, Fairchild, & Fritz, 2007). We found a significant indirect effect of maltreatment exposure on “p” at follow-up through baseline emotional reactivity and rumination in parallel (95% confidence interval [.015, .210]). In contrast to maltreatment exposure, maltreatment severity was significantly associated with “p” at follow-up when controlling for “p” at baseline (c = .044, p = .016). The indirect effect of maltreatment severity on “p” at follow-up through baseline emotional reactivity and rumination in parallel was statistically significant (95% confidence interval [.002, .037]).
Figure 3.

Models used to test the indirect effects of maltreatment and maltreatment severity on psychopathology (p factor) at follow-up, via emotional reactivity and rumination, controlling for baseline psychopathology. Income-to-needs ratio and racial minority status were also included as covariates in both models. Independent variables (maltreatment exposure and severity), mediators (emotional reactivity and rumination), and covariates (p factor at baseline, race/ethnicity, and income-to-needs) were collected concurrently, but independent variables were retrospective. Dependent variable (p factor at follow-up) was collected 2 years later. Standardized coefficients are shown. Solid lines indicate significant paths. Dotted lines indicate nonsignificant paths.
Discussion
We investigated the role of emotion regulation processes occurring at multiple stages of the emotion generation process as transdiagnostic mechanisms linking childhood maltreatment with psychopathology across childhood and adolescence. Maltreatment was associated with emotion dysregulation, as indicated by increased engagement in maladaptive response-focused emotion regulation strategies and heightened emotional reactivity, which in turn were associated with greater general psychopathology both concurrently and longitudinally. The associations between maltreatment and emotion regulation were largely age-invariant, with the exception of attention biases toward or away from threat. Specifically, maltreated children had greater attention biases toward threat that shifted to an attention bias away from threat in older adolescents. Further, youth with preferential attention to threat had increased psychopathology over time, conversely demonstrating that attention away from threat was associated with decreased psychopathology over time. Thus, the age-specific shift in bias direction found in the current study may reflect an adaptive strategy that buffers against risk for psychopathology among maltreated adolescents.
Childhood maltreatment is associated with multiple forms of emotion dysregulation. Specifically, children and adolescents who were maltreated and who experienced more severe maltreatment exhibited a greater tendency to engage in maladaptive, response-focused strategies like expressive suppression and rumination and also had increased emotional reactivity relative to children who had never been maltreated. These findings are consistent with a growing body of research using multiple methods and modalities demonstrating that childhood maltreatment, particularly forms of maltreatment that involve abuse and interpersonal violence, are associated with heightened emotional reactivity, as measured by self-report (Glaser et al., 2006; Heleniak et al., 2016; McLaughlin et al., 2010). The self-reported heightened emotional reactivity is corroborated by studies that find increased reactivity in neurobiological systems involved in emotional responding in maltreated youth, including the amygdala (Hein & Monk, 2017; McCrory et al., 2011; McLaughlin et al., 2015; Viding et al., 2012). This suggests that maltreated children and adolescents may experience more intense emotions, perhaps contributing to, but also resulting from, emotion dysregulation.
To our knowledge, this is the first study to investigate the association between childhood maltreatment and engagement in expressive suppression. The positive association between expressive suppression and maltreatment severity is consistent with previous findings that harsh and inconsistent discipline is associated with increased use of this strategy in children (Balan et al., 2017). When engagement in expressive suppression fails to prevent intrusive and intense negative thoughts and feelings, maltreated youth may dwell or ruminate on these distressing emotions. Consistent with past studies of maltreatment and other forms of early life stress (Conway et al., 2004; Heleniak et al., 2016; LeMoult et al., 2018; McLaughlin & Hatzenbuehler, 2009), we found that maltreated children and adolescents engage in greater habitual use of rumination than children who have not experienced maltreatment. Building on control theory, (Carver & Scheier, 1982; Martin & Tesser, 1996), we have previously argued that chronic and uncontrollable stressors might increase engagement in rumination because they either create or accentuate discrepancies between goals or desired states and one’s actual situation (Michl et al., 2013). Experiences of maltreatment are inherently uncontrollable and often chronic, and thus may be particularly likely to generate discrepancies between one’s current situation and desired states that cannot be resolved. Overall, our findings indicate that maltreatment can trigger a pattern of emotion dysregulation characterized by heightened emotional reactivity, which is unaided or exacerbated by greater engagement in maladaptive emotion regulation strategies, which may actually increase the intensity and duration of negative emotions.
Tendencies to engage in cognitive reappraisal were not associated with child maltreatment. This is consistent with the view that greater engagement in maladaptive emotion regulation is a more consistent mechanism conveying risk for psychopathology than decreased engagement in adaptive emotion regulation (Aldao & Nolen-Hoeksema, 2012a, 2012b; Aldao et al., 2010). It may be that while the tendency to engage in cognitive reappraisal is unrelated to childhood maltreatment, the capacity to utilize this strategy effectively may be nonetheless diminished in children and adolescents exposed to maltreatment. For example, maltreated adolescents have been found to engage prefrontal cortex more than nonmaltreated adolescents during a cognitive reappraisal task in which their self-reported change in negative affect did not differ (McLaughlin et al., 2015), suggesting they may need to employ more regulatory effort to achieve the same emotional outcome.
Most of the associations between maltreatment and emotion regulation observed in this study were age invariant. However, age did interact with maltreatment exposure and maltreatment severity in relation to attention bias to threat. In children, maltreatment severity was associated with larger attention bias toward threat; in early adolescence, no association was observed between maltreatment severity and attention bias to threat, and among older adolescents, greater maltreatment severity was associated with attention bias away from threat. Attention bias away from threat was in turn associated with lower psychopathology at follow-up, consistent with past findings linking attention biases to threat-related cues with psychopathology, in particular anxiety (Hankin, Gibb, Abela, & Flory, 2010; Lau & Waters, 2017; Waters et al., 2010). The association between abuse and attention bias toward threatening stimuli is consistent with prior work (Briggs-Gowan et al., 2015; Cicchetti & Curtis, 2005; Pollak & Tolley-Schell, 2003; Shackman et al., 2007). The variability of this association with age is consistent with the interpretation that with increasing age comes an increasing capacity to regulate attention away from distressing emotional stimuli, overriding pre-potent tendencies to orient toward potential threats (Morales et al., 2016) that may arise as a result of being raised in a dangerous environment (McLaughlin & Lambert, 2017). The maturation of attentional control with age interacts with maltreatment experiences, which make potential threats in the environment both more salient, drawing attention (Pollak, 2003), and potentially more distressing, which might motivate attentional avoidance (Kelly et al., 2015).
A greater tendency to engage in maladaptive emotion regulation strategies is associated with a higher “p” both concurrently and prospectively, indicating greater transdiagnostic risk for psychopathology. Prior evidence suggesting that emotion dysregulation is a transdiagnostic factor in psychopathology comes largely from meta-analyses and reviews of many studies (Aldao & Nolen-Hoeksema, 2012a, 2012b; Aldao et al., 2010) or studies that have examined emotion regulation difficulties as mechanisms underlying comorbidity or transitions between different forms of psychopathology (McLaughlin et al., 2014; McLaughlin & Nolen-Hoeksema, 2011; Messman-Moore & Bhuptani, 2017). Here, we demonstrate that emotion regulation strategies contribute directly to general psychopathology, as captured by the p factor (Caspi et al., 2014).
The association between maladaptive emotion regulation strategies and “p” is also consistent with evidence that greater engagement in maladaptive strategies like expressive suppression and rumination is more strongly associated with multiple psychiatric disorders than lesser engagement in adaptive strategies like cognitive reappraisal (Aldao et al., 2010). As conceptual models of emotion regulation consider it to be so intertwined with the emotion process itself that it is difficult to distinguish between emotions and their regulation (Cole et al., 2017; Gross, 2014; Gross & Thompson, 2007; Thompson, 1994), it is perhaps unsurprising that emotion dysregulation would be associated with global disruptions to emotion functioning, increasing risk for psychopathology transdiagnostically. Moreover, greater tendencies to engage in expressive suppression and rumination and greater emotional reactivity were strongly interrelated, suggesting multiple interrelated manifestations of emotion dysregulation that together contribute to greater risk for psychopathology. It may be that because increased emotional reactivity, expressive suppression, and rumination tend to reinforce one another, that their impact and potential to spiral into psychopathology are more pronounced then adaptive strategies like cognitive reappraisal. Rumination and emotional reactivity also predict “p” longitudinally, as does attention bias to threat. As suggested by the age-related patterns in the relation between attention bias and childhood maltreatment, a greater attention bias away from threat may indicate a greater capacity to utilize attentional avoidance, an antecedent-focused strategy to direct attention away from negative or distressing emotional stimuli, which may be protective against developing psychopathology.
Childhood maltreatment was associated with a higher “p.” This is unsurprising and consistent with past findings that (a) childhood maltreatment explains a substantial proportion of all mental disorders in the population (Green et al., 2010; Kessler, Mickelson, & Williams, 1999; McLaughlin et al., 2012) and (b) that maltreatment in childhood and adolescence predicts higher “p” in adulthood in longitudinal studies (Caspi et al., 2014; Schaefer et al., 2018). In the present study, however, greater engagement in rumination and heightened emotional reactivity emerged as key mechanisms linking maltreatment with general psychopathology. Even though childhood maltreatment was not associated with changes in “p” over time, it indirectly influenced increases in “p” through the combined effect of increased emotional reactivity and rumination. A similar pattern was observed for maltreatment severity, which did predict increases in “p” over time. Thus, while maltreatment exposure was associated with increased psychopathology, this risk may be highly stable over time. Nonetheless, the maladaptive emotion regulation processes engendered by maltreatment exposure continue to maintain and worsen psychopathology across development.
This study had several strengths, including a large sample, which was recruited to ensure sufficient variability in both age and maltreatment exposure to evaluate their independent effects and interactions, integration of multiple measures of maltreatment from both youth and parents, and longitudinal measures of psychopathology from both youth and parents. However, some limitations constrain interpretation and suggest directions for future research. While maltreated and nonmaltreated youth were matched on both age and gender, maltreated youth had significantly lower income and a higher proportion of racial/ethnic minority youth. These factors frequently co-occur, and all analyses controlled for income-to-needs ratio and racial minority status. However, potential confounds from this collinearity cannot be entirely ruled out. Future work in samples recruited specifically to examine interactions among violence exposure, race/ethnicity, and socioeconomic status could help distinguish the unique and shared influence of these variables on emotion regulation and psychopathology. Next, this study relies on youth self-reported emotion regulation. While the use of multiple reporters for quantifying both maltreatment and psychopathology symptoms allays some concerns about associations being attributable to shared method variance, work utilizing behavioral and ecological measures of emotion regulation would provide necessary additional support to our findings. In addition, the meaning of “p” is still a subject of considerable debate, with hypotheses ranging from poor impulse control over emotions to deficits in intellectual functioning to a simple tendency to report on oneself in a negative way (Caspi & Moffitt, 2018). However, there is robust evidence supporting the utility of “p” as a correlate of both theoretically and practically important risk factors and outcomes, suggesting that identification of the specific emotion regulation mechanisms that contribute to “p” may significantly advance clinical science (Caspi & Moffitt, 2018; Snyder & Hankin, 2017).
Although questionnaires were read out loud for younger children in the study (8- to 10-year-olds) and those who had difficulty reading, the ERS and ERQ have not been validated for children under 12 (Nock et al., 2008), and at the time the study started, we were not aware of the child and adolescent version of the ERQ with slightly simplified language (Gullone & Taffe, 2012). Finally, while associations between attention bias and psychopathology, especially anxiety, are quite consistent across studies (Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & Van IJzendoorn, 2007; Dudeney et al., 2015), attention biases as measured by the dot-probe task demonstrate low test–retest reliability (Brown et al., 2014; Chapman, Devue, & Grimshaw, 2017; Waechter, Nelson, Wright, Hyatt, & Oakman, 2014), calling into question its utility as a between-subjects measure of emotion regulation. Further validation by other indices of attention like eye tracking and event-related potentials would therefore provide necessary support to our findings related to attention biases and their implications.
Greater emotional reactivity and greater engagement in maladaptive emotion regulation strategies, in particular rumination, are transdiagnostic mechanisms linking childhood maltreatment with psychopathology in middle childhood and adolescence, and which maintain and exacerbate psychopathology symptoms over time. Attention biases away from threat predict decreased psychopathology over time. Maltreatment contributes to maladaptive patterns of emotion regulation in the form of attention biases toward threat in children and younger adolescents, but with more adaptive patterns in older adolescents, who may have a greater capacity to redirect their attention away from threatening and distressing emotional cues. These results suggest that therapies and interventions aimed at disrupting patterns of rumination in youth exposed to childhood maltreatment have the potential to reduce risk for multiple forms of psychopathology in adolescence, and that attention bias modification may also reduce risk for psychopathology, but its efficacy might be restricted to older adolescence and young adults who may have a greater capacity for regulating their attention.
Supplementary Material
Acknowledgments
Financial support. This research was funded by the National Institute of Mental Health Grant R01-MH103291 (awarded to K.A.M.) and Grant K01MH116325 (awarded to A.B.M.), an Early Career Research Fellowship from the Jacobs Foundation (to K.A.M.), and a OneMind Institute Rising Star Award (to K.A.M.).
References
- Abela JRZ, Brozina K, & Haigh EP (2002). An examination of the response styles theory of depression in third- and seventh-grade children: A short-term longitudinal study. Journal of Abnormal Child Psychology, 30, 515–527. doi: 10.1023/A:1019873015594 [DOI] [PubMed] [Google Scholar]
- Abela JRZ, Hankin BL, Sheshko DM, Fishman MB, & Stolow D (2012). Multi-wave prospective examination of the stress-reactivity extension of response styles theory of depression in high-risk children and early adolescents. Journal of Abnormal Child Psychology, 40, 277–287. doi: 10.1007/s10802-011-9563-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achenbach TM (1991). Manual for the Child Behavior Checklist/4–18 and 1991 profile Burlington, VT: University of Vermont, Department of Psychiatry. [Google Scholar]
- Aldao A, & Nolen-Hoeksema S (2010). Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research and Therapy, 48, 947–983. doi: 10.1016/j.brat.2010.06.002 [DOI] [PubMed] [Google Scholar]
- Aldao A, & Nolen-Hoeksema S (2012a). The influence of context on the implementation of adaptive emotion regulation strategies. Behaviour Research and Therapy, 50, 493–501. doi: 10.1016/j.brat.2012.04.004 [DOI] [PubMed] [Google Scholar]
- Aldao A, & Nolen-Hoeksema S (2012b). When are adaptive strategies most predictive of psychopathology? Journal of Abnormal Psychology, 121, 276–281. doi: 10.1037/a0023598 [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30, 217–237. doi: 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Balan R, Dobrean A, Roman GD, & Balazsi R (2017). Indirect effects of parenting practices on internalizing problems among adolescents: The role of expressive suppression. Journal of Child and Family Studies, 26, 40–47. doi: 10.1007/s10826-016-0532-4 [DOI] [Google Scholar]
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, & Van Ijzendoorn MH (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin, 133, 1–24. doi: 10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP (2015). Future directions in emotion dysregulation and youth psychopathology. Journal of Clinical Child and Adolescent Psychology, 133, 1–24. doi: 10.1080/15374416.2015.1038827 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, & Zisner A (2017). Motivation, emotion regulation, and the latent structure of psychopathology: An integrative and convergent historical perspective. International Journal of Psychophysiology, 119, 108–118. doi: 10.1016/j.ijpsycho.2016.12.014 [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, & Handelsman L (1997). Validity of the childhood trauma questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 340–348. doi: 10.1097/00004583-199703000-00012 [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, … Ruggiero J (1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry, 151, 1231–1236. doi: 10.1176/ajp.151.8.1132 [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, & Harris TO (1994). Childhood Experience of Care and Abuse (CECA): A retrospective interview measure. Journal of Child Psychology and Psychiatry, 35, 1419–1435. doi: 10.1111/j.1469-7610.1994.tb01284.x [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, Lillie A, & Jarvis J (1997). Memories of childhood neglect and abuse: Corroboration in a series of sisters. Journal of Child Psychology and Psychiatry and Allied Disciplines, 38, 364–375. doi: 10.1111/j.1469-7610.1997.tb01520.x [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M (1999). Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child & Adolescent Psychiatry, 38, 1230–1236. doi: 10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SMK (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 545–553. doi: 10.1097/00004583-199704000-00018 [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Pollak SD, Grasso D, Voss J, Mian ND, Zobel E, … Pine DS (2015). Attention bias and anxiety in young children exposed to family violence. Journal of Child Psychology and Psychiatry and Allied Disciplines, 56, 1194–1201. doi: 10.1111/jcpp.12397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown HM, Eley TC, Broeren S, MacLeod C, Rinck M, Hadwin JA, & Lester KJ (2014). Psychometric properties of reaction time based experimental paradigms measuring anxiety-related information-processing biases in children. Journal of Anxiety Disorders, 28, 97–107. doi: 10.1016/j.janxdis.2013.11.004 [DOI] [PubMed] [Google Scholar]
- Burns EE, Jackson JL, & Harding HG (2010). Child maltreatment, emotion regulation, and posttraumatic stress: The impact of emotional abuse. Journal of Aggression, Maltreatment and Trauma, 19, 801–819. doi: 10.1080/10926771.2010.522947 [DOI] [Google Scholar]
- Carver CS, Johnson SL, & Timpano KR (2017). Toward a functional view of the p factor in psychopathology. Clinical Psychological Science Advance online publication. doi: 10.1177/2167702617710037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, & Scheier MF (1982). Control theory: A useful conceptual framework for personality-social, clinical, and health psychology. Psychological Bulletin, 92, 111–135. doi: 10.1037/0033-2909.92.1.111 [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, … Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2, 119–137. doi: 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, & Moffitt TE (2018). All for one and one for all: Mental disorders in one dimension. American Journal of Psychiatry, 175, 831–844. doi: 10.1176/appi.ajp.2018.17121383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos-Ryan N, Briere FN, O’Leary-Barrett M, Banaschewski T, Bokde A, Bromberg U, … IMAGEN Consortium. (2016). The structure of psychopathology in adolescence and its common personality and cognitive correlates. Journal of Abnormal Psychology, 125, 1039–1052. doi: 10.1037/abn0000193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman A, Devue C, & Grimshaw GM (2017). Fleeting reliability in the dot-probe task. Psychological Research Advance online publication. doi: 10.1007/s00426-017-0947-6 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Ackerman BP, & Izard CE (1995). Emotions and emotion regulation in developmental psychopathology. Development and Psychopathology, 7, 1. doi: 10.1017/S0954579400006301 [DOI] [Google Scholar]
- Cicchetti D, & Curtis WJ (2005). An event-related potential study of the processing of affective facial expressions in young children who experienced maltreatment during the first year of life. Development and Psychopathology, 17, 641–677. doi: 10.1017/S0954579405050315 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2005). Child maltreatment. Annual Review of Clinical Psychology, 1, 409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029 [DOI] [PubMed] [Google Scholar]
- Cole PM, Hall SE, & Hajal NJ (2017). Emotion dysregulation as a vulnerability to psychopathology. In Beauchaine TP & Hinshaw SP (Eds.), Child and adolescent psychopathology (pp. 346–386). Hoboken, NJ: Wiley. [Google Scholar]
- Conway M, Mendelson M, Giannopoulos C, Csank PAR, & Holm SL (2004). Childhood and adult sexual abuse, rumination on sadness, and dysphoria. Child Abuse and Neglect, 28, 393–410. doi: 10.1016/j.chiabu.2003.05.004 [DOI] [PubMed] [Google Scholar]
- Craighead WE, Smucker MR, Craighead LW, & Ilardi SS (1998). Factor analysis of the Children’s Depression Inventory in a community sample. Psychological Assessment, 10, 156–165. doi: 10.1037/1040-3590.10.2.156 [DOI] [Google Scholar]
- Dudeney J, Sharpe L, & Hunt C (2015). Attentional bias towards threatening stimuli in children with anxiety: A meta-analysis. Clinical Psychology Review, 40, 66–75. doi: 10.1016/j.cpr.2015.05.007 [DOI] [PubMed] [Google Scholar]
- Ernst M, Pine DS, & Hardin M (2006). Triadic model of the neurobiology of motivated behavior in adolescence. Psychological Medicine, 36, 299–312. doi: 10.1017/S0033291705005891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Hamby SL, Ormrod R, & Turner H (2005). The Juvenile Victimization Questionnaire: Reliability, validity, and national norms. Child Abuse and Neglect, 29, 393–412. doi: 10.1016/j.chiabu.2004.11.001 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Shattuck A, Turner HA, & Hamby SL (2014). The lifetime prevalence of child sexual abuse and sexual assault assessed in late adolescence. Journal of Adolescent Health, 55, 329–333. doi: 10.1016/j.jadohealth.2013.12.026 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2013). Violence, crime, and abuse exposure in a national sample of children and youth an update. JAMA Pediatrics, 167, 614–621. doi: 10.1001/jamapediatrics.2013.42 [DOI] [PubMed] [Google Scholar]
- Frankenhuis WE, & Del Giudice M (2012). When do adaptive developmental mechanisms yield maladaptive outcomes? Developmental Psychology, 48, 643–646. doi: 10.1037/a0025629 [DOI] [PubMed] [Google Scholar]
- Glaser JP, van Os J, Portegijs PJM, & Myin-Germeys I (2006). Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. Journal of Psychosomatic Research, 61, 229–236. doi: 10.1016/j.jpsychores.2006.04.014 [DOI] [PubMed] [Google Scholar]
- Gomez R, Stavropoulos V, Vance A, & Griffiths MD (2018). Reevaluation of the latent structure of common childhood disorders: Is there a general psychopathology factor (p-factor)? International Journal of Mental Health and Addiction Advance online publication. doi: 10.1007/s11469-018-0017-3 [DOI] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication: I. Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67, 113–123. doi: 10.1001/archgenpsychiatry.2009.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene AL, & Eaton NR (2017). The temporal stability of the bifactor model of comorbidity: An examination of moderated continuity pathways. Comprehensive Psychiatry, 72, 74–82. doi: 10.1016/j.comppsych.2016.09.010 [DOI] [PubMed] [Google Scholar]
- Gresham D, & Gullone E (2012). Emotion regulation strategy use in children and adolescents: The explanatory roles of personality and attachment. Personality and Individual Differences, 52, 616–621. doi: 10.1016/j.paid.2011.12.016 [DOI] [Google Scholar]
- Gross JJ (1998a). Antecedent- and response-focused emotion regulation: Divergent consequences for experience, expression, and physiology. Journal of Personality and Social Psychology, 74, 224–237. doi: 10.1037/0022-3514.74.1.224 [DOI] [PubMed] [Google Scholar]
- Gross JJ (1998b). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2, 271–299. doi: 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- Gross JJ (2014). Emotion regulation: Conceptual and empirical foundations. In Gross JJ (Ed.). Handbook of emotion regulation (2nd ed., pp. 3–20). New York: Guilford Press. [Google Scholar]
- Gross JJ, & John OP (2003). Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85, 348–362. doi: 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- Gross JJ, & Levenson RW (1997). Hiding feelings: The acute effects of inhibiting negative and positive emotion. Journal of Abnormal Psychology, 106, 95–103. doi: 10.1037/0021-843X.106.1.95 [DOI] [PubMed] [Google Scholar]
- Gross JJ, & Thompson R (2007). Emotion regulation: Conceptual foundations. In Gross JJ (Ed.), Handbook of emotion regulation New York: Guilford Press. [Google Scholar]
- Gullone E, Hughes EK, King NJ, & Tonge B (2010). The normative development of emotion regulation strategy use in children and adolescents: A 2-year follow-up study. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51, 567–574. doi: 10.1111/j.1469-7610.2009.02183.x [DOI] [PubMed] [Google Scholar]
- Gullone E, & Taffe J (2012). The Emotion Regulation Questionnaire for Children and Adolescents (ERQ-CA): A psychometric evaluation. Psychological Assessment, 24, 409–417. doi: 10.1037/a0025777 [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Wewerka S, Frenn K, Long JD, & Griggs C (2009). Developmental changes in hypothalamus-pituitary-adrenal activity over the transition to adolescence: Normative changes and associations with puberty. Development and Psychopathology, 21, 69–85. doi: 10.1017/S0954579409000054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyer AE, Silk JS, & Nelson EE (2016). The neurobiology of the emotional adolescent: From the inside out. Neuroscience & Biobehavioral Reviews, 70, 74–85. doi: 10.1016/j.neubiorev.2016.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2008). Stability of cognitive vulnerabilities to depression: A short-term prospective multiwave study. Journal of Abnormal Psychology, 117, 324–333. doi: 10.1037/0021-843X.117.2.324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Gibb BE, Abela JRZ, & Flory K (2010). Selective attention to affective stimuli and clinical depression among youths: Role of anxiety and specificity of emotion. Journal of Abnormal Psychology, 119, 491–501. doi: 10.1037/a0019609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis New York: Guildford Press. [Google Scholar]
- Hein TC, & Monk CS (2017). Research Review: Neural response to threat in children, adolescents, and adults after child maltreatment—A quantitative meta-analysis. Journal of Child Psychology and Psychiatry and Allied Disciplines, 58, 222–230. doi: 10.1111/jcpp.12651 [DOI] [PubMed] [Google Scholar]
- Heleniak C, Jenness JL, Vander Stoep A, McCauley E, & McLaughlin KA (2016). Childhood maltreatment exposure and disruptions in emotion regulation: A transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognitive Therapy and Research, 40, 394–415. doi: 10.1007/s10608-015-9735-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- John OP, & Gross JJ (2004). Healthy and unhealthy emotion regulation: Personality processes, individual differences, and life span development. Journal of Personality, 72, 1301–1333. doi: 10.1111/j.1467-6494.2004.00298.x [DOI] [PubMed] [Google Scholar]
- Jose PE, & Brown I (2008). When does the gender difference in rumination begin? Gender and age differences in the use of rumination by adolescents. Journal of Youth and Adolescence, 37, 180–192. doi: 10.1007/s10964-006-9166-y [DOI] [Google Scholar]
- Kelly PA, Viding E, Puetz VB, Palmer AL, Mechelli A, Pingault JB, … McCrory EJ (2015). Sex differences in socioemotional functioning, attentional bias, and gray matter volume in maltreated children: A multilevel investigation. Development and Psychopathology, 27, 1591–1601. doi: 10.1017/S0954579415000966 [DOI] [PubMed] [Google Scholar]
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, … Williams DR (2010). Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. British Journal of Psychiatry, 197, 378–385. doi: 10.1192/bjp.bp.110.080499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, & Williams DR (1999). The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior, 40, 208. doi: 10.2307/2676349 [DOI] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, & Hasin DS (2012). Childhood maltreatment and the structure of common psychiatric disorders. British Journal of Psychiatry, 200, 107–115. doi: 10.1192/bjp.bp.111.093062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51, 706–716. doi: 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M (1992). Children’s Depression Inventory CDI manual North Tonawanda, NY: Multi-Health Systems. [Google Scholar]
- Kovacs M (2011). Children’s Depression Inventory (CDI2) North Tonawanda NY: Multi-Health Systems. [Google Scholar]
- Laceulle OM, Vollebergh WAM, & Ormel J (2015). The structure of psychopathology in adolescence: Replication of a general psychopathology factor in the TRAILS study. Clinical Psychological Science, 3, 850–860. doi: 10.1177/2167702614560750 [DOI] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, & Rathouz PJ (2012). Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology, 121, 971–977. doi: 10.1037/a0028355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143, 142–186. doi: 10.1037/bul0000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson RW, Moneta G, Richards MH, & Wilson S (2002). Continuity, stability, and change in daily emotional experience across adolescence. Child Development, 73, 1151–1165. doi: 10.1111/1467-8624.00464 [DOI] [PubMed] [Google Scholar]
- Lau JYF, & Waters AM (2017). Annual Research Review: An expanded account of information-processing mechanisms in risk for child and adolescent anxiety and depression. Journal of Child Psychology and Psychiatry and Allied Disciplines, 58, 387–407. doi: 10.1111/jcpp.12653 [DOI] [PubMed] [Google Scholar]
- LeMoult J, Humphreys KL, King LS, Colich NL, Price AN, Ordaz SJ, & Gotlib IH (2018). Associations among early life stress, rumination, symptoms of psychopathology, and sex in youth in the early stages of puberty: A moderated mediation analysis. Journal of Abnormal Child Psychology Advance online publication. doi: 10.1007/s10802-018-0430-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li CH (2016). Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behavior Research Methods, 48, 936–949. doi: 10.3758/s13428-015-0619-7 [DOI] [PubMed] [Google Scholar]
- Lobue V, & Deloache JS (2010). Superior detection of threat-relevant stimuli in infancy. Developmental Science, 13, 221–228. doi: 10.1111/j.1467-7687.2009.00872.x [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, & Vasey MW (2009). Negative affectivity, effortful control, and attention to threat-relevant stimuli. Journal of Abnormal Child Psychology, 37, 387–399. doi: 10.1007/s10802-008-9284-y [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Caldwell ND, & Nolen-Hoeksema S (1998). Effects of ruminative and distracting responses to depressed mood on retrieval of autobiographical memories. Journal of Personality and Social Psychology, 75, 166–177. doi: 10.1037/0022-3514.75.1.166 [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, & Nolen-Hoeksema S (1993). Self-perpetuating properties of dysphoric rumination. Journal of Personality and Social Psychology, 65, 239–249. doi: 10.1037/0022-3514.65.2.339 [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation analysis. Annual Review of Psychology, 58, 593. doi: 10.1146/annurev.psych.58.110405.085542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Pan PM, Hoffmann MS, Gadelha A, do Rosário MC, Mari JJ, … Salum GA (2017). A general psychopathology factor (P factor) in children: Structural model analysis and external validation through familial risk and child global executive function. Journal of Abnormal Psychology, 126, 137–148. doi: 10.1037/abn0000205 [DOI] [PubMed] [Google Scholar]
- Martin LL, & Tesser A (1996). Some ruminative thoughts. In Wyer RS Jr. (Ed.), Ruminative thoughts: Vol. 9. Advances in social cognition (pp. 1–48). Mahwah, NJ: Erlbaum. [Google Scholar]
- Maughan A, & Cicchetti D (2002). Impact of child maltreatment and inter-adult violence on children’s emotion regulation abilities and socioemotional adjustment. Child Development, 73, 1525–1542. doi: 10.1111/1467-8624.00488 [DOI] [PubMed] [Google Scholar]
- McCabe CJ, Kim DS, & King KM (2018). Improving present practices in the visual display of interactions. Advances in Methods and Practices in Psychological Science Advance online publication. doi: 10.1177/2515245917746792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrory EJ, De Brito SA, Sebastian CL, Mechelli A, Bird G, Kelly PA, & Viding E (2011). Heightened neural reactivity to threat in child victims of family violence. Current Biology, 21, R947–R948. doi: 10.1016/j.cub.2011.10.015 [DOI] [PubMed] [Google Scholar]
- McGrath JJ, Saha S, Lim CCW, Aguilar-Gaxiola S, Alonso J, Andrade LH, … Wojtyniak B (2017). Trauma and psychotic experiences: Transnational data from the World Mental Health survey. British Journal of Psychiatry, 211, 373–380. doi: 10.1192/bjp.bp.117.205955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Aldao A, Wisco BE, & Hilt LM (2014). Rumination as a transdiagnostic factor underlying transitions between internalizing symptoms and aggressive behavior in early adolescents. Journal of Abnormal Psychology, 123, 13–23. doi: 10.1037/a0035358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Borkovec TD, & Sibrava NJ (2007). The effects of worry and rumination on affect states and cognitive activity. Behavior Therapy, 38, 23–38. doi: 10.1016/j.beth.2006.03.003 [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2012). Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Archives of General Psychiatry, 69, 1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Hatzenbuehler ML (2009). Mechanisms linking stressful life events and mental health problems in a prospective, community-based sample of adolescents. Journal of Adolescent Health, 144, 153–160. doi: 10.1016/j.jadohealth.2008.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Kubzansky LD, Dunn EC, Waldinger R, Vaillant G, & Koenen KC (2010). Childhood social environment, emotional reactivity to stress, and mood and anxiety disorders across the life course. Depression and Anxiety, 27, 1087–1094. doi: 10.1002/da.20762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Lambert HK (2017). Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Current Opinion in Psychology, 14, 29–34. doi: 10.1016/j.copsyc.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Nolen-Hoeksema S (2011). Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy, 49, 186–193. doi: 10.1016/j.brat.2010.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Peverill M, Gold AL, Alves S, & Sheridan MA (2015). Child maltreatment and neural systems underlying emotion regulation. Journal of the American Academy of Child & Adolescent Psychiatry, 54, 753–762. doi: 10.1016/j.jaac.2015.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRae K, Gross JJ, Weber J, Robertson ER, Sokol-Hessner P, Ray RD, … Ochsner KN (2012). The development of emotion regulation: An fMRI study of cognitive reappraisal in children, adolescents and young adults. Social Cognitive and Affective Neuroscience, 7, 11–22. doi: 10.1093/scan/nsr093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, & Bhuptani PH (2017). A review of the long-term impact of child maltreatment on posttraumatic stress disorder and its comorbidities: An emotion dysregulation perspective. Clinical Psychology: Science and Practice, 24, 154–169. doi: 10.1111/cpsp.12193 [DOI] [Google Scholar]
- Michl LC, McLaughlin KA, Shepherd K, & Nolen-Hoeksema S (2013). Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: Longitudinal evidence in early adolescents and adults. Journal of Abnormal Psychology, 1222, 339–352. doi: 10.1037/a0031994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LE (2015). Perceived threat in childhood: A review of research and implications for children living in violent households. Trauma, Violence, and Abuse, 16, 153–168. doi: 10.1177/1524838013517563 [DOI] [PubMed] [Google Scholar]
- Morales S, Fu X, & Pérez-Edgar KE (2016). A developmental neuroscience perspective on affect-biased attention. Developmental Cognitive Neuroscience, 21, 26–41. doi: 10.1016/j.dcn.2016.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray AL, Eisner M, & Ribeaud D (2016). The development of the general factor of psychopathology “p factor„ through childhood and adolescence. Journal of Abnormal Child Psychology, 44, 1573–1586. doi: 10.1007/s10802-016-0132-1 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus user’s guide (7th ed.). Los Angeles: Author. [Google Scholar]
- Neumann A, Pappa I, Lahey BB, Verhulst FC, Medina-Gomez C, Jaddoe VW, … Tiemeier H (2016). Single nucleotide polymorphism heritability of a general psychopathology factor in children. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 1038–1045. doi: 10.1016/j.jaac.2016.09.498 [DOI] [PubMed] [Google Scholar]
- Nock MK, Wedig MM, Holmberg EB, & Hooley JM (2008). The Emotion Reactivity Scale: Development, evaluation, and relation to self-injurious thoughts and behaviors. Behavior Therapy, 39, 107–116. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, & Aldao A (2011). Gender and age differences in emotion regulation strategies and their relationship to depressive symptoms. Personality and Individual Differences, 51, 704–708. doi: 10.1016/j.paid.2011.06.012 [DOI] [Google Scholar]
- Nolen-Hoeksema S, & Morrow J (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology, 61, 115–121. doi: 10.1037/0022-3514.61.1.115 [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Stice E, Wade E, & Bohon C (2007). Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. Journal of Abnormal Psychology, 116, 198–207. doi: 10.1037/0021-843X.116.1.198 [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, & Lyubomirsky S (2008). Rethinking rumination. Perspectives on Psychological Science, 3, 400–424. doi: 10.1111/j.1745-6924.2008.00088.x [DOI] [PubMed] [Google Scholar]
- Olino TM, Dougherty LR, Bufferd SJ, Carlson GA, & Klein DN (2014). Testing models of psychopathology in preschool-aged children using a structured interview-based assessment. Journal of Abnormal Child Psychology, 42, 1201–1211. doi: 10.1007/s10802-014-9865-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Mahen HA, Karl A, Moberly N, & Fedock G (2015). The association between childhood maltreatment and emotion regulation: Two different mechanisms contributing to depression? Journal of Affective Disorders, 174, 287–295. doi: 10.1016/J.JAD.2014.11.028 [DOI] [PubMed] [Google Scholar]
- Patalay P, Fonagy P, Deighton J, Belsky J, Vostanis P, & Wolpert M (2015). A general psychopathology factor in early adolescence. British Journal of Psychiatry, 207, 15–22. doi: 10.1192/bjp.bp.114.149591 [DOI] [PubMed] [Google Scholar]
- Peh CX, Shahwan S, Fauziana R, Mahesh MV, Sambasivam R, Zhang Y, … Subramaniam M (2017). Emotion dysregulation as a mechanism linking child maltreatment exposure and self-harm behaviors in adolescents. Child Abuse & Neglect, 67, 383–390. doi: 10.1016/J.CHIABU.2017.03.013 [DOI] [PubMed] [Google Scholar]
- Pérez-Edgar K, Bar-Haim Y, McDermott JM, Chronis-Tuscano A, Pine DS, & Fox NA (2010). Attention biases to threat and behavioral inhibition in early childhood shape adolescent social withdrawal. Emotion, 10, 349–357. doi: 10.1037/a0018486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pine DS, Mogg K, Bradley BP, Montgomery LA, Monk CS, McClure E, … Kaufman J (2005). Attention bias to threat in maltreated children: Implications for vulnerability to stress-related psychopathology. American Journal of Psychiatry, 162, 291–298. doi: 10.1176/appi.ajp.162.2.291 [DOI] [PubMed] [Google Scholar]
- Pollak SD (2003). Experience-dependent affective learning and risk for psychopathology in children. Annals of the New York Academy of Sciences, 1008, 102–111. doi: 10.1196/annals.1301.011 [DOI] [PubMed] [Google Scholar]
- Pollak SD, Cicchetti D, Hornung K, & Reed A (2000). Recognizing emotion in faces: Developmental effects of child abuse and neglect. Developmental Psychology, 36, 679–688. doi: 10.1037/0012-1649.36.5.679 [DOI] [PubMed] [Google Scholar]
- Pollak SD, & Kistler DJ (2002). Early experience is associated with the development of categorical representations for facial expressions of emotion. Proceedings of the National Academy of Sciences, 99, 9072–9076. doi: 10.1073/pnas.142165999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak SD, & Sinha P (2002). Effects of early experience on children’s recognition of facial displays of emotion. Developmental Psychology, 38, 784–791. doi: 10.1037/0012-1649.38.5.784 [DOI] [PubMed] [Google Scholar]
- Pollak SD, & Tolley-Schell SA (2003). Selective attention to facial emotion in physically abused children. Journal of Abnormal Psychology, 112, 323–338. doi: 10.1037/0021-843X.112.3.323 [DOI] [PubMed] [Google Scholar]
- Raviv A, Erel O, Fox NA, Leavitt LA, Raviv A, Dar I, … Greenbaum CW (2001). Individual measurement of exposure to everyday violence among elementary schoolchildren across various settings. Journal of Community Psychology, 29, 117–140. doi: [DOI] [Google Scholar]
- Raviv A, Raviv A, Shimoni H, Fox NA, & Leavitt LA (1999). Children’s self-report of exposure to violence and its relation to emotional distress. Journal of Applied Developmental Psychology, 20, 337–353. doi: 10.1016/S0193-3973(99)00020-9 [DOI] [Google Scholar]
- R Core Team. (2018). R: A language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria: https://www.R-project.org/ [Google Scholar]
- Reinholdt-Dunne ML, Mogg K, Esbjorn BH, & Bradley BP (2012). Effects of age and anxiety on processing threat cues in healthy children. Journal of Experimental Psychopathology, 3, 30–41. doi: 10.5127/jep.019611 [DOI] [Google Scholar]
- Schaefer JD, Moffitt TE, Arseneault L, Danese A, Fisher HL, Houts R, … Caspi A (2018). Adolescent victimization and early-adult psychopathology: Approaching causal inference using a longitudinal twin study to rule out noncausal explanations. Clinical Psychological Science, 6, 352–371. doi: 10.1177/2167702617741381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shackman JE, Shackman AJ, & Pollak SD (2007). Physical abuse amplifies attention to threat and increases anxiety in children. Emotion, 7, 838–852. doi: 10.1037/1528-3542.7.4.838 [DOI] [PubMed] [Google Scholar]
- Shields A, & Cicchetti D (1997). Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology, 33, 906–916. doi: 10.1037/0012-1649.33.6.906 [DOI] [PubMed] [Google Scholar]
- Shulman EP, Smith AR, Silva K, Icenogle G, Duell N, Chein J, & Steinberg L (2016). The dual systems model: Review, reappraisal, and reaffirmation. Developmental Cognitive Neuroscience, 17, 103–117. doi: 10.1016/j.dcn.2015.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvers JA, Insel C, Powers A, Franz P, Helion C, Martin RE, … Ochsner KN (2017a). VlPFC-vmPFC-amygdala interactions underlie age-related differences in cognitive regulation of emotion. Cerebral Cortex, 27, 3502–3514. doi: 10.1093/cercor/bhw073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvers JA, Insel C, Powers A, Franz P, Helion C, Martin RE, … Ochsner KN (2017b). The transition from childhood to adolescence is marked by a general decrease in amygdala reactivity and an affect-specific ventral-to-dorsal shift in medial prefrontal recruitment. Developmental Cognitive Neuroscience, 25, 128–137. doi: 10.1016/j.dcn.2016.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvers JA, McRae K, Gabrieli JDE, Gross JJ, Remy KA, & Ochsner KN (2012). Age-related differences in emotional reactivity, regulation, and rejection sensitivity in adolescence. Emotion, 12, 1235–1247. doi: 10.1037/a0028297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, & Hankin BL (2017). All models are wrong, but the p factor modelis useful: Reply to Widiger and Oltmanns (2017) and Bonifay, Lane, and Reise (2017). Clinical Psychological Science, 5, 187–189. doi: 10.1177/2167702616659389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017). Strong homotypic continuity in common psychopathology-, internalizing-, and externalizing-specific factors over yime in adolescents. Clinical Psychological Science, 5, 98–110. doi: 10.1177/2167702616651076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville LH, Jones RM, & Casey BJ (2010). A time of change: Behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain and Cognition, 72, 124–133. doi: 10.1016/j.bandc.2009.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, & Pynoos RS (2004). The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index. Current Psychiatry Reports, 6. doi: 10.1007/s11920-004-0048-2 [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Kim S, Briggs EC, Ippen CG, Ostrowski SA, … Pynoos RS (2013). Psychometric properties of the UCLA PTSD Reaction Index: Part I. Journal of Traumatic Stress, 26, 1–9. doi: 10.1002/jts.21780 [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, & Runyan D (1998). Identification of child maltreatment with the parent-child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse and Neglect, 22, 249–270. doi: 10.1016/S0145-2134(97)00174-9 [DOI] [PubMed] [Google Scholar]
- Stroud LR, Foster E, Papandonatos GD, Handwerger K, Granger DA, Kivlighan KT, & Niaura R (2009). Stress response and the adolescent transition: Performance versus peer rejection stressors. Development and Psychopathology, 21, 47–68. doi: 10.1017/S0954579409000042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz JR, Graham-Bermann SA, Mogg K, Bradley BP, & Monk CS (2011). Journal of Child and Adolescent Trauma, 4, 109–122. doi: 10.1080/19361521.2011.573525 [DOI] [Google Scholar]
- Thompson RA (1994). Emotion regulation: A theme in search of definition. Monographs of the Society for Research in Child Development, 59, 25–52. doi: 10.1111/j.1540-5834.1994.tb01276.x [DOI] [PubMed] [Google Scholar]
- Todd RM, Cunningham WA, Anderson AK, & Thompson E (2012). Affect-biased attention as emotion regulation. Trends in Cognitive Sciences, 16, 365–372. doi: 10.1016/j.tics.2012.06.003 [DOI] [PubMed] [Google Scholar]
- Tottenham N, Borscheid A, Ellertsen K, Marcus DJ, & Nelson CA (2002). Categorization of facial expressions in children and adults: Establishing a larger stimulus set. Journal of Cognitive Neuroscience, 14, S74. [Google Scholar]
- Van Buuren S, & Groothuis-Oudshoorn K (2011). mice : Multivariate Imputation by Chained Equations in R. Journal of Statistical Software, 45. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- Viding E, Sebastian CL, Dadds MR, Lockwood PL, Cecil CAM, De Brito SA, & McCrory EJ (2012). Amygdala response to preattentive masked fear in children with conduct problems: The role of callous-unemotional traits. American Journal of Psychiatry, 169, 1109–1116. doi: 10.1176/appi.ajp.2012.12020191 [DOI] [PubMed] [Google Scholar]
- Waechter S, Nelson AL, Wright C, Hyatt A, & Oakman J (2014). Measuring attentional bias to threat: Reliability of dot probe and eye movement indices. Cognitive Therapy and Research, 38, 313–333. doi: 10.1007/s10608-013-9588-2 [DOI] [Google Scholar]
- Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, … Katon W (1999). Costs of health care use by women HMO members with a history of childhood abuse and neglect. Archives of General Psychiatry, 56, 809–813. doi: 10.1001/archpsyc.56.7.609 [DOI] [PubMed] [Google Scholar]
- Waters AM, Henry J, Mogg K, Bradley BP, & Pine DS (2010). Attentional bias towards angry faces in childhood anxiety disorders. Journal of Behavior Therapy and Experimental Psychiatry, 41, 158–164. doi: 10.1016/j.jbtep.2009.12.001 [DOI] [PubMed] [Google Scholar]
- Webb TL, Miles E, & Sheeran P (2012). Dealing with feeling: A meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychological Bulletin, 138, 775–808. doi: 10.1037/a0027600 [DOI] [PubMed] [Google Scholar]
- Wechsler D (2011). Wechsler Abbreviated Scale of Intelligence—Second edition (WASI-II) San Antonio, TX: Pearson. [Google Scholar]
- Ziegert DI, & Kistner JA (2002). Response styles Theory: Downward extension to children. Journal of Clinical Child and Adolescent Psychology, 31, 325–334. doi: 10.1207/S15374424JCCP3103_04 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


