Abstract
Objective:
In commercial direct-to-consumer (DTC) telemedicine, physicians outside of the medical home treat common, acute complaints through real-time, audio-visual conferencing using telephones and personal computers. There has been little examination of the use of DTC telemedicine by children. We described trends in DTC telemedicine use and DTC telemedicine visit characteristics.
Methods:
Using 2011-2016 claims from a large national health plan, we identified pediatric acute visits to DTC telemedicine and to primary care providers (PCPs). We examined DTC telemedicine visits trends, and compared DTC telemedicine and acute PCP visit diagnoses and patient characteristics.
Results:
From 2011 to 2016, pediatric DTC telemedicine visits increased from 38 to 24,409 visits annually. In 2015-2016, the most common primary diagnoses for DTC telemedicine visits (n=42,072) were infections of the nose/sinuses (24%), mouth/throat (16%), and ear (9%), which were also the most common diagnoses for acute PCP visits (n=6,917,976). Odds of DTC telemedicine use were higher for children in non-metropolitan communities (OR=1.45, 95% CI 1.40-1.51) and children without preventive visits (OR=1.08, 95% CI 1.06-1.11). Compared to children receiving acute PCP care, children with DTC telemedicine visits were also more likely to have had urgent care (17% vs. 10%, p<0.001) and emergency department visits (21% vs. 19%, p<0.001) during the study period.
Conclusion:
There is rapid growth of commercial DTC telemedicine visits for children, primarily for acute respiratory infections. Compared to children who did not use DTC telemedicine for acute care, children using DTC telemedicine were also more likely to use other venues for acute care outside of the medical home.
Keywords: telemedicine, telehealth, pediatric, direct-to-consumer, utilization
Introduction
In the commercial direct-to-consumer (DTC) telemedicine model of many national companies, physicians outside of the medical home treat common, acute complaints on-demand through audio-only or audio-video conferencing via personal devices.1 While some primary care practices have integrated acute care telemedicine within the medical home,2–4 national commercial DTC telemedicine companies (e.g., Doctor on Demand, Amwell, Teladoc) currently provide the majority of telemedicine visits for acute primary care complaints, either directly or through platforms re-branded by hospitals or health plans as their own.5
The American Academy of Pediatrics cautioned against DTC telemedicine outside of the medical home,6 given concerns about fragmentation and quality of care. Specifically, DTC telemedicine outside of the medical home may decrease informational continuity, relational continuity, and management continuity.7 Quality concerns include the limited exam that can be performed via smartphone and personal computer, as well as potential inconsistency of camera and connection quality.6,8 Despite such concerns, 96% of large employers now provide coverage through their health plans for telemedicine services for employees and dependents,9 providing millions of children with access to DTC telemedicine.
While access to DTC telemedicine expands, data on pediatric DTC telemedicine are limited. One health system recently described their first thousand DTC telemedicine visits for children, and reported high parent satisfaction; two-third of parents stated that the DTC telemedicine visit allowed them to avoid a urgent care, retail-based clinic, or emergency visit.10 Studies on commercial DTC telemedicine quality outcomes are limited to adults. These studies report that DTC telemedicine can increase access to care,1,11,12 but that visit quality may be lower for specific quality measures,11,13 and that the ease of accessing DTC telemedicine may generate increased utilization and spending.1
To fill the knowledge gap on pediatric DTC telemedicine use, we analyzed claims from a large national health plan. We examined trends in DTC telemedicine use over time and compared DTC telemedicine and acute PCP visit diagnoses, patient characteristics, and patient health care use.
Methods
We used 2011-2016 claims for children ≤17 years old from a national commercial health plan which contracts with a large national DTC telemedicine vendor and covers approximately 4 million children enrolled per year across all 9 census divisions of the US. All professional, pharmaceutical, and facility claims were available.
We identified DTC telemedicine, emergency department (ED), and urgent care visits using a combination of Current Procedural Terminology (CPT) codes, place of service codes, national provider identifiers, and tax identification numbers using previously published methods.14 We identified PCP visits using CPT codes and provider specialty codes. We defined acute PCP visits as PCP visits where the billing or primary diagnosis code did not indicate a health supervision or immunization visit.
In visit-level analyses, we examined volume of DTC telemedicine visits from 2011-2016, including absolute number of visits as well as number of visits per pediatric member-year nationally and within census regions. Focusing on 2015-2016 DTC telemedicine visits to assess the most recent use patterns, we then compared primary diagnosis subgroups and diagnosis severity determined using a published diagnosis grouping system designed for categorizing pediatric acute care visits.15 This diagnosis grouping system identifies 21 major groups (e.g., respiratory diseases; neurologic disease; trauma) and 77 subgroups of diagnoses (e.g., asthma; headache; strains & sprains). This diagnosis grouping system also categorizes visit diagnoses into five severity levels, from least severe (1) to most severe (5). We compared visit diagnosis subgroups and diagnosis severity for DTC telemedicine versus acute PCP visits using chi-square tests. After examining diagnoses in most recent years, we examined trends in DTC telemedicine visit diagnosis subgroups across all years (2011-2016).
In patient-level analyses, we assessed patient characteristics among children with ≥1 DTC telemedicine visits in 2015-2016 (“DTC telemedicine users”). We compared these children to children with no DTC telemedicine visits but ≥1 acute PCP visit in 2015-2016 (“DTC telemedicine non-users”). Patients with no use of either DTC telemedicine or acute PCP visits were excluded from analysis. Patients with missing state or gender were also excluded from analysis (n=36 DTC telemedicine users [0.1%] and n=5321 telemedicine non-users [0.2%]). Additional patient-level variables examined included child age, gender, chronic medical complexity, rural/urban status, ZIP code median income, receipt of preventive care, and high deductible health plan status. Level of chronic illness was determined by applying the Pediatric Medical Complexity Algorithm to patient data, which we applied to 2014-2016 claims data to be consistent with prior algorithm use.16 Rural/urban status was determined by using the US Department of Agriculture rural-urban commuting area (RUCA) codes.17 ZIP code median income was determined by using 2015 US census data, categorized by the 2015 federal poverty level (FPL) for a family of 4. Preventive care receipt was determined by identifying any preventive care CPT codes (99381-99387, 99391-99397, 99401-99412, 99429) during 2015-2016.
To understand patient factors associated with use of DTC telemedicine, we compared patient characteristics for DTC telemedicine users and non-users first using chi-square tests and then in adjusted analysis using logistic regression. In the logistic regression model, we included patient characteristics with significance of p<0.1 in unadjusted analysis, with final model including patient age, gender, medical complexity, rural-urban commuting area (RUCA), ZIP code median income, high deductible health plan status, and receipt of preventive care.
Finally, to understand whether use of DTC telemedicine is associated with use of other venues of acute care, we used chi-square tests to compare use of urgent care and emergency care during 2015-2016 among DTC telemedicine users and non-users.
This analysis was reviewed by the Harvard Medical School Institutional Review Board and determined to be exempt. Analyses were conducted in SAS version 9.4 (SAS Institute, INC., Cary, North Carolina).
Results
From 2011 to 2016, total pediatric DTC telemedicine visits per year increased from 38 to 24,409 visits. DTC telemedicine use in 2016 was highest among children in the South with 1,231 visits per 100,000 member-years (Figure 1). Growth in DTC telemedicine use in the most recent year was highest in the Midwest (79% increase from 2015 to 2016), followed by the Northeast (66% increase from 2015 to 2016). Overall in 2016, there were 7 DTC telemedicine visits for every 1000 acute PCP visits (n=3,403,930).
Figure 1: Pediatric DTC Telemedicine Visits Nationally and by Region, 2011-2016.
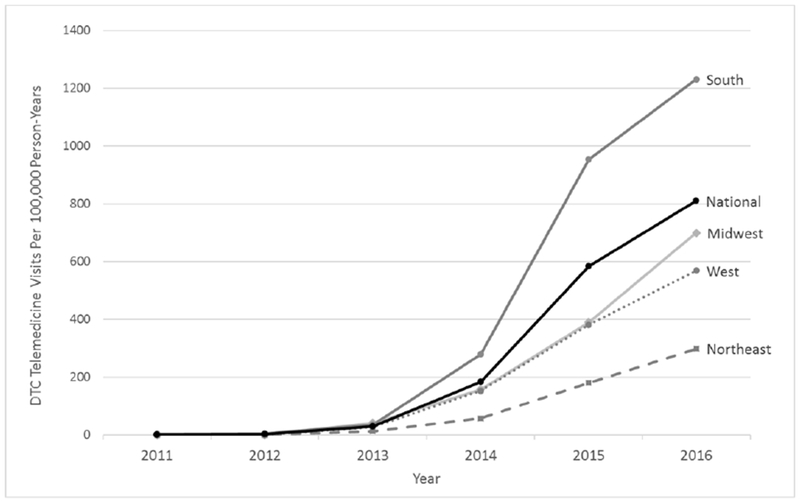
Number of DTC telemedicine visits per 100,000 pediatric member-years within each census region within a large commercial health plan, 2011-2016.
In 2015-16, the three most common diagnosis subgroups for both DTC telemedicine and acute PCP visits were infections of nose/sinuses, mouth/throat, and ears (Figure 2). Compared to acute PCP visits, proportionately more DTC telemedicine visits addressed eye complaints (6% DTC telemedicine vs. 2% acute PCP, p<0.001) and proportionately fewer received a diagnosis of an unspecified viral illness (1.7% DTC telemedicine vs. 4.1% acute PCP, p<0.001). Compared to acute PCP visits, a smaller proportion of DTC telemedicine visits addressed psychiatric/behavioral concerns (0.1% vs. 4.5%, p<0.001) The diagnoses detailed in Figure 2 accounted for 83% of DTC telemedicine visits, and 71% of acute PCP visits.
Figure 2: Primary Diagnosis Subgroup for Direct to Consumer (DTC) Telemedicine versus Acute Primary Care Provider (PCP) Visit, 2015-2016.
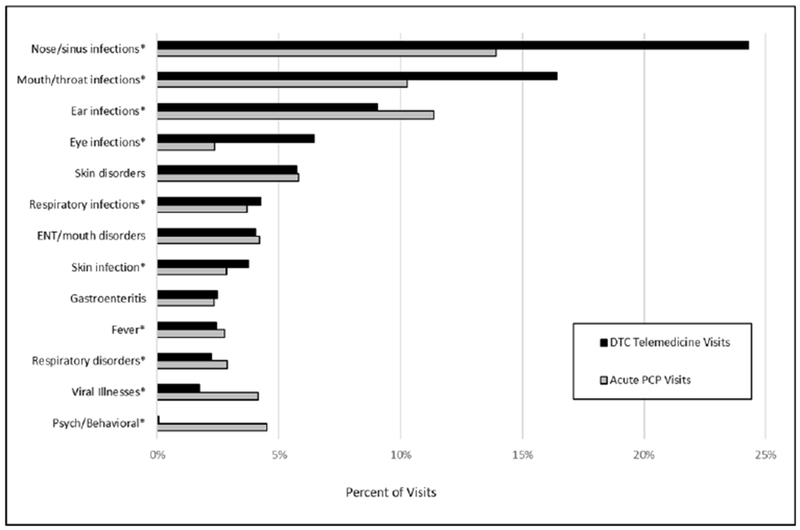
Diagnosis subgroups were determined through use of a published diagnosis grouping system designed for categorization of acute pediatric visits,15 which was applied to the primary diagnosis for each visit. The diagnosis grouping system identifies 21 major groups and 77 subgroups. The 10 most common diagnosis subgroups (out of 77 total subgroups) for either DTC telemedicine and acute PCP visits are listed (totaling 13 diagnosis subgroups, due to overlap). Abbreviations: DTC, direct to consumer; ENT, ear, nose, throat; PCP, primary care provider. *=p<0.001.
Diagnosis severity was statistically different but clinically similar across settings. Compared to PCP visits, the fraction of DTC telemedicine visits categorized as least severe differed by one percentage point (5% of DTC telemedicine visits vs. 6% of acute PCP visits, p<0.001) as did the fraction categorized in the two highest severity categories (0.3% of DTC telemedicine visits versus 1.3% of acute PCP visits, p<0.001).
Across all six years, nose/sinus infection, ear infections, and mouth/throat infections were the three most common diagnosis subgroups for DTC telemedicine visits, together comprising 46-61% of visits within each year. However, over time the proportion of DTC telemedicine visits receiving a diagnosis of nose/sinus infection has increased from 5% to 23%, while the percent receiving a diagnosis of mouth/throat infections decreased from 36% to 17% and the percent receiving a diagnosis of ear infection decreased from 18% to 10%.
In 2015-2016, odds of DTC telemedicine use were higher for older children, children in non-metropolitan and lower median income communities, and children without preventive visits (Table 1). Odds of DTC telemedicine use were lower for children with complex chronic diseases.
Table 1:
Characteristics of Children Using DTC Telemedicine, 2015-2016
| Children, No. (%) |
|||||
|---|---|---|---|---|---|
| Characteristics | DTC Telemedicine Users | DTC Telemedicine Non-Users | P | OR | 95% CI |
| Overall | 30,171 | 2,316,611 | |||
| Age | <0.001 | ||||
| 0-1 years old | 1751 (6) | 285,119 (12) | 1 | Ref | |
| 2-5 years old | 7801 (26) | 560,852 (24) | 2.27 | 2.16-2.40 | |
| 6-11 years old | 10,665 (35) | 735,605 (32) | 2.37 | 2.25-2.49 | |
| 12-17 years old | 9954 (33) | 735,035 (32) | 2.23 | 2.12-2.35 | |
| Gender | <0.001 | ||||
| Female | 15,399 (51) | 1,137,160 (49) | 1.07 | 1.04-1.09 | |
| Male | 14,772 (49) | 1,179,451 (51) | 1 | Ref | |
| Chronic Medical Complexity | <0.001 | ||||
| No Chronic Disease | 21,649 (72) | 1,607,713 (69) | 1 | Ref | |
| Non-complex Chronic Disease | 5998 (20) | 464,121 (20) | 0.92 | 0.89-0.94 | |
| Complex Chronic Disease | 2524 (8) | 244,777 (11) | 0.74 | 0.71-0.78 | |
| Metropolitan/Non-Metropolitan | <0.001 | ||||
| Metropolitan | 26,388 (87) | 2,118,881 (91) | 1 | Ref | |
| Non-Metropolitan | 3541 (12) | 173,292 (7) | 1.45 | 1.40-1.51 | |
| Missing | 242 (0.8) | 24,438 (1) | 0.74 | 0.65-0.84 | |
| ZIP Code Median Income | <0.001 | ||||
| 0-200% FPL | 6578 (22) | 438,544 (19) | 1.52 | 1.46-1.58 | |
| 201-300% FPL | 11,368 (38) | 786,394 (34) | 1.57 | 1.51-1.62 | |
| 301-400% FPL | 7871 (26) | 602,915 (26) | 1.46 | 1.41-1.52 | |
| 401%+ FPL | 4354 (14) | 488,758 (21) | 1 | Ref | |
| Preventative PCP visits | <0.001 | ||||
| 0 visits | 9763 (32) | 639,173 (28) | 1.08 | 1.06-1.11 | |
| 1 + visits | 20,408 (68) | 1,677,438 (72) | 1 | Ref | |
| High Deductible Health Plan (HDHP) | 0.030 | ||||
| Yes | 2877 (10) | 212,477 (9) | 1.00 | 0.96-1.04 | |
| No | 27,294 (90) | 2,104,134 (91) | 1 | Ref | |
Abbreviations: CI, confidence interval; DTC, direct-to-consumer; FPL, federal poverty level; HDHP, high deductible health plan; OR, odds ratio; PCP, primary care provider; RUCA, rural urban commuting areas.
Unadjusted and adjusted analysis comparing DTC telemedicine users (pediatric patients with ≥1 DTC telemedicine visit, with or without associated acute PCP visits) versus DTC telemedicine non-users (pediatric patients with ≥1 acute PCP visits, but no DTC telemedicine visits) in 2015-2016. We compared patient characteristics among telemedicine users and non-users first using chi-squared tests and then in adjusted analysis using logistic regression, adjusting for patient age, gender, medical complexity, rural-urban commuting area (RUCA), ZIP code median income, high deductible health plan status, and receipt of preventive care.
Most DTC telemedicine users also visited a PCP for acute concerns (70%) at least once during the two-year study period. DTC telemedicine users were more likely than non-users to have had any urgent care visit (17% vs. 10% of non-users, p<0.001) and any emergency department (ED) visits (21% vs. 19% of non-users, p<0.001) during the study period.
Discussion
Commercial DTC telemedicine visits by children grew substantially from 2011 to 2016, but still accounted for only a small percentage of acute pediatric care. While some variation was observed, the most common diagnoses and diagnosis severity were relatively similar for DTC telemedicine and acute PCP visits. This is surprising because the care in DTC telemedicine is delivered via personal devices that are not equipped with peripheral exam devices (i.e., tele-otoscopy),18 such that there may be limited ability to perform specific components of the physical exam. While commercial DTC telemedicine companies often provide online lists of diagnoses they do or do not treat, our analysis suggests that families are seeking care through DTC telemedicine for a wide spectrum of pediatric acute care needs.
Pediatric DTC telemedicine use appears to be driven by relative convenience rather than absolute lack of availability. While children from non-metropolitan and lower income areas had modestly increased odds of DTC telemedicine use, the vast majority of DTC telemedicine users lived in metropolitan areas. Over two-thirds of DTC telemedicine users also had preventive and acute PCP visits, suggesting these children are connected with alternative options for in-person care.
DTC telemedicine users were also more likely than DTC telemedicine non-users to have urgent care and ED visits, suggesting a cohort turning to multiple venues for acute care outside of the medical home. This could occur if these children have PCPs who do not have appointment options that fit parents’ expectations during acute illness. Alternatively, these children may have higher real or perceived need for acute medical care, resulting in increased use of multiple acute care venues.
Among DTC telemedicine users, 6% were less than 2 years old, despite the American Telemedicine Association advice that children less than 2 should not use commercial DTC telemedicine outside of the medical home.8 Additionally 8% of DTC telemedicine users were identified as having complex chronic conditions (i.e., chronic disease involving multiple body systems, progressive disease with decreased life expectancy, malignancy, technology dependence16). While children with this level of chronic medical complexity may realize benefits from the use of telemedicine (e.g., reduced travel burden, reduced exposure to infections),19 the lack of informational continuity and care management continuity in DTC telemedicine may be of particular concern for this population, warranting focused evaluation on the risks and benefits among children with medical complexity.
Key limitations of this claims analysis are that we cannot account for patient preferences or details of plan product coverage. We also focused in this analysis on examining DTC telemedicine use, and did not examine quality or care or clinical outcomes. Additionally, this analysis focuses on the DTC telemedicine use by children within one national health plan and may not generalize to other populations.
In conclusion, our findings highlight increasing use of commercial DTC telemedicine by children, predominantly for acute respiratory infections, and primarily by children who also had PCP visits. Given this rapid increase in use, there is a need to examine the quality of pediatric care at DTC telemedicine visits, to assess the impact of DTC telemedicine on child health outcomes and utilization, and to consider strategies integrate acute telemedicine into the medical home.
What’s New.
Pediatric direct-to-consumer telemedicine use is rapidly growing, primarily for acute respiratory infections. Compared to children not using commercial DTC telemedicine for acute care, children using DTC telemedicine were more likely to also use emergency departments and urgent care facilities.
Acknowledgements.
Funding: Supported in part by grants from the NICHD (K23HD088642, Dr. Ray) and gifts from Melvin Hall. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Abbreviations:
- CI
confidence interval
- DTC
direct-to-consumer
- ENT
ear, nose, throat
- FPL
federal poverty level
- HDHP
high deductible health plan
- OR
odds ratio
- PCP
primary care provider
- RUCA
rural urban commuting areas
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosures/Conflicts of Interest: The authors have no conflicts of interest to disclose.
Authors note: These findings were presented in part at the Pediatric Academic Societies meeting in Toronto, ON, on May 6, 2018. Dr. Poon’s affiliation is now with Vanderbilt University.
References
- 1.Ashwood JS, Mehrotra A, Cowling D, Uscher-Pines L. Direct-To-Consumer Telehealth May Increase Access To Care But Does Not Decrease Spending. Health Aff (Millwood). 2017;36(3):485–491. [DOI] [PubMed] [Google Scholar]
- 2.McConnochie KM, Wood NE, Herendeen NE, et al. Acute illness care patterns change with use of telemedicine. Pediatrics. 2009;123(6):e989–995. [DOI] [PubMed] [Google Scholar]
- 3.Pearl RM. Engaging Physicians in Telehealth. NEJM Catalyst 2017; https://catalyst.nejm.org/engaging-physicians-in-telehealth/. Accessed August 7, 2018. [Google Scholar]
- 4.North SW, McElligot J, Douglas G, Martin A. Improving access to care through the patient-centered medical home. Pediatr Ann. 2014;43(2):e33–38. [DOI] [PubMed] [Google Scholar]
- 5.Raja P, Mehrotra A. The Nuts and Bolts of Convenient Care Partnerships. NEJM Catalyst 2016; https://catalyst.nejm.org/the-nuts-and-bolts-of-convenient-care-partnerships/. Accessed August 9, 2018. [Google Scholar]
- 6.Conners GP, Kressly SJ, Perrin JM, et al. Nonemergency Acute Care: When It’s Not the Medical Home. Pediatrics. 2017;139(5). [DOI] [PubMed] [Google Scholar]
- 7.Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McSwain SD, Bernard J, Burke BL, Jr., et al. American Telemedicine Association Operating Procedures for Pediatric Telehealth. Telemed J E Health. 2017;23(9):699–706. [DOI] [PubMed] [Google Scholar]
- 9.Large US employers project health care benefit costs to surpass $14000 per employee in 2018, National Business Group on Health survey finds [press release]. August 8, 2017. Accessed from https://www.businessgrouphealth.org/news/nbgh-news/press-releases/press-release-details/?ID=334. .
- 10.Vyas S, Murren-Boezem J, Solo-Josephson P. Analysis of a Pediatric Telemedicine Program. Telemed J E Health. 2018. [DOI] [PubMed] [Google Scholar]
- 11.Uscher-Pines L, Mulcahy A, Cowling D, Hunter G, Burns R, Mehrotra A. Access and Quality of Care in Direct-to-Consumer Telemedicine. Telemed J E Health. 2016;22(4):282–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uscher-Pines L, Mehrotra A. Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Aff (Millwood). 2014;33(2):258–264. [DOI] [PubMed] [Google Scholar]
- 13.Uscher-Pines L, Mulcahy A, Cowling D, Hunter G, Burns R, Mehrotra A. Antibiotic Prescribing for Acute Respiratory Infections in Direct-to-Consumer Telemedicine Visits. JAMA Intern Med. 2015;175(7):1234–1235. [DOI] [PubMed] [Google Scholar]
- 14.Poon SJ, Schuur JD, Mehrotra A. Trends in Low-Acuity Visits to Acute Care Venues in the United States From 2008 to 2015. JAMA Intern Med. 2018;178(10):1342–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alessandrini EA, Alpern ER, Chamberlain JM, Shea JA, Gorelick MH. A new diagnosis grouping system for child emergency department visits. Acad Emerg Med. 2010;17(2):204–213. [DOI] [PubMed] [Google Scholar]
- 16.Simon TD, Cawthon ML, Popalisky J, Mangione-Smith R, Center of Excellence on Quality of Care Measures for Children with Complex N. Development and Validation of the Pediatric Medical Complexity Algorithm (PMCA) Version 2.0. Hosp Pediatr. 2017;7(7):373–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United States Department of Agriculture. 2010. Rural-Urban Commuting Area Codes. Available at: https://wwwersusdagov/data-products/rural-urban-commuting-area-codes/ Accessed April 2, 2018.
- 18.Weinstein RS, Krupinski EA, Doarn CR. Clinical Examination Component of Telemedicine, Telehealth, mHealth, and Connected Health Medical Practices. Med Clin North Am. 2018;102(3):533–544. [DOI] [PubMed] [Google Scholar]
- 19.Ray KN, Ashcraft LE, Mehrotra A, Miller E, Kahn JM. Family Perspectives on Telemedicine for Pediatric Subspecialty Care. Telemed J E Health. 2017;23(10):852–862. [DOI] [PMC free article] [PubMed] [Google Scholar]


