Abstract
Background.
This study evaluated in a rigorous 18-month randomized controlled trial the efficacy of an enhanced vocational intervention for helping individuals with a recent first schizophrenia episode to return to and remain in competitive work or regular schooling.
Methods.
Individual Placement and Support (IPS) was adapted to meet the goals of individuals whose goals might involve either employment or schooling. IPS was combined with a Workplace Fundamentals Module (WFM) for an enhanced, outpatient, vocational intervention. Random assignment to the enhanced integrated rehabilitation program (N = 46) was contrasted with equally intensive clinical treatment at UCLA, including social skills training groups, and conventional vocational rehabilitation by state agencies (N = 23). All patients were provided case management and psychiatric services by the same clinical team and received oral atypical antipsychotic medication.
Results.
The IPS-WFM combination led to 83% of patients participating in competitive employment or school in the first 6 months of intensive treatment, compared with 41% in the comparison group (p < 0.005). During the subsequent year, IPS-WFM continued to yield higher rates of schooling/employment (92% v. 60%, p < 0.03). Cumulative number of weeks of schooling and/or employment was also substantially greater with the IPS-WFM intervention (45 v. 26 weeks, p < 0.004).
Conclusions.
The results clearly support the efficacy of an enhanced intervention focused on recovery of participation in normative work and school settings in the initial phase of schizophrenia, suggesting potential for prevention of disability.
Keywords: first-episode schizophrenia, functional outcome, randomized controlled trial, supported education, supported employment, work recovery
Introduction
After the initial onset of schizophrenia, individuals with the illness are focused on resuming a normal life and often specifically on returning to work or school (Roe, 2001; Judge et al., 2008; Lam et al., 2011). First-episode schizophrenia patients associate earning an income with better quality of life (Gioia and Brekke, 2003). Individuals with a first hospitalization for non-affective psychosis spontaneously report as a life goal finding a job in 53% of cases and going back to school in 38% of cases (with unknown overlap), and endorse related services as desirable in 80% and 75% of cases (Ramsay et al., 2011). Thus, while a subgroup does not spontaneously list work or schooling as a life goal, these are the most frequently listed. The goal of returning to work or school after onset of schizophrenia may unfortunately be the aspect of recovery that is least often achieved (Ventura et al., 2011).
In long-term severe mental disorders, supported employment has been the most successful approach to facilitating return to competitive jobs (Bond, 2004; Bond et al., 2008; Modini et alx., 2016). The Individual Placement and Support (IPS) approach (Becker and Drake, 2003) significantly increases the rate of competitive employment for individuals with long-term severe mental illness as compared with conventional vocational rehabilitation services (Drake et al., 1999; Becker and Drake, 2003; Bond et al., 2008; Drake et al., 2012; Drake et al., 2013). IPS emphasizes rapid search for a competitive job, integration of vocational services into mental health teams, attending to client job preferences, community outreach, and ongoing employment support (Becker and Drake, 2003; Bond, 2004).
IPS has only begun to be examined in randomized controlled trials (RCTs) in the initial period of schizophrenia, despite the fact that high symptomatic remission rates, short interruptions of education or employment, and high motivation to return to school or work might lead to even greater success during this period (Nuechterlein et al., 2006; Killackey et al., 2008; Nuechterlein et al., 2008; Rinaldi et al., 2010). IPS was first introduced in first- episode psychosis by Rinaldi et al. in a naturalistic study in London with promising results (Rinaldi et al., 2004). However, results of only one RCT that isolates the impact of IPS in first-episode psychosis have been published (Killackey et al., 2008). That pioneering 6-month study by Killackey et al. with 41 first-episode psychosis patients found that IPS resulted in competitive work or school participation in 85% of participants, compared with 29% of participants in a treatment-as-usual comparison group. Return to school was not differentially affected, but competitive employment rates clearly were. Furthermore, the mean number of weeks worked was significantly greater for IPS participants (8.6 weeks) compared with the treatment-as-usual group (3.8 weeks).
The Killackey et al. RCT left several critical questions unanswered. First, it was unclear whether the advantage of IPS for first-episode patients lasted beyond the initial 6 months. The mean duration of employment/schooling created by IPS was quite brief (about 9 weeks). Second, given that first-episode schizophrenia patients often initially choose to return to school rather than employment (Nuechterlein et al., 2008), further adaptation of IPS was desirable to determine whether this approach could successfully enhance return to schooling as well as employment. Third, a related issue was whether the timing of return to school would be the same as return to employment for first-episode patients when both options were offered. Fourth, the study used a treatment-as-usual comparison group, not matched for treatment intensity, so a RCT with a more closely matched comparison group was desirable. Finally, it was unclear whether the results, completed in Australia where mental health services are characterized by universal treatment access, would generalize to our more fractionated psychiatric care system in the USA.
The RAISE Early Treatment Program (RAISE-ETP) study is another important step in demonstrating the promise of IPS in early psychosis (Kane et al., 2016). Although this large RCT involved a comprehensive early intervention program in community clinics and did not randomly assign IPS, a mediation analysis suggested that the increase in work/school participation was associated with patients’ use of supported education/employment (Rosenheck et al., 2017). The RAISE Connection Program study also showed that supported education/employment could be successfully applied in first-episode schizophrenia, but did not include a comparison group (Dixon et al., 2015; Humensky et al., 2017).
While IPS has a focus on return to work or school, we recognized that young people are prone to change career goals in school as well as jobs before they find their niches. Thus, we hypothesized that improving generic work/school skills would help young patients to maintain school/work attendance and also to change schools and jobs when appropriate. The Workplace Fundamentals Module (WFM) is a group skills training approach that is focused on general skills to support work/school performance over time (Wallace and Tauber, 2004). Thus, we combined IPS and WFM to maximize the impact on work recovery after a first psychotic episode.
We describe here the results of an 18-month RCT of IPSWFM in the initial course of schizophrenia. Participants were randomly assigned to an 18-month IPS-WFM intervention or to conventional vocational rehabilitation [Brokered Vocational Rehabilitation (BVR)] plus a social skills group not focused on the workplace. We adapted supported education (Egnew, 1993, 1997; Unger, 1998) such that the program met the standards for IPS fidelity (Nuechterlein et al., 2008). We hypothesized that IPS-WFM would: (1) increase the likelihood that individuals with a recent first episode of schizophrenia would return to school or competitive jobs during the initial 6 months of treatment, (2) continue to show a higher level of participation in school and competitive employment in a following year of less intensive treatment, and (3) lead to greater cumulative duration of schooling or employment during the 18-month RCT.
Method
Participants
The 69 recent-onset schizophrenia patients were recruited from Los Angeles public and private psychiatric hospitals and clinics. Project staff visited over 25 hospitals and clinics to introduce the UCLA first-episode schizophrenia clinic and to encourage referral of all potentially eligible patients. All participants received their outpatient psychiatric treatment at the UCLA Aftercare Research Program to allow a common clinical treatment base.
Inclusion criteria were: (1) a recent first psychotic episode, beginning within the last 2 years (with psychotic symptoms lasting at least 2 weeks); (2) a diagnosis by Research Diagnostic Criteria (RDC) (Spitzer et al., 1978) of schizophrenia or schizoaffective disorder, mainly schizophrenic subtype; (3) 18–45 years old; (4) sufficient English fluency to avoid invalidating research measures; (5) residence within commuting distance of UCLA; and (6) possible interest in trying to resume work or school. Potential participants were excluded if they showed evidence of (1) a neurological disorder; (2) significant habitual substance use disorder in the 6 months prior to hospitalization or substance use that accounted for the psychotic symptoms; (3) mental retardation; or (4) contra-indication for risperidone treatment (risperidone was the first-line antipsychotic medication). As approved by the UCLA IRB, all participants received oral and written information about research procedures and provided written informed consent. All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The sample included 58 individuals with RDC schizophrenia (84%), 10 with schizoaffective disorder, depressed type, mainly schizophrenic (14%), and one with schizoaffective disorder, manic type, mainly schizophrenic (2%), based on the Structured Clinical Interview for DSM-IV (SCID) (First et al., 2001) and informant and medical record information. Mean age at randomization was 24.5 years (s.d. = 4.1, range 18–38), mean education was 13.2 years (S.D. = 1.9, range 10–17), 67% were male, and 93% were single. At entry, the sample had a mean of 1.2 psychiatric hospitalizations (S.D. = 0.9) and a mean lifetime duration of psychosis of 8.3 months (S.D. = 7.7). Racial distribution was 26% White, 22% African American, 12% Asian, 3% Pacific Islander, and 38% more than one race. Twenty-six percent were of Hispanic/Latino ethnicity. None were homeless.
Procedures
The UCLA Aftercare Research Program provided high diagnostic inter-rater reliability (Ventura et al., 1998) and a common therapeutic base (Nuechterlein et al., 1992). All participants were provided with atypical antipsychotic medication, weekly psychiatrist visits and individual case management, and family psychoeducation, thereby equating these aspects of their psychiatric care. Oral risperidone was prescribed as the initial medication to standardize this treatment component, with switching to another atypical antipsychotic as needed due to lack of efficacy or intolerable side effects. Medication adherence was not required to continue in the study. Details of medication procedures and medication non-adherence effects in this sample were the focus of a prior publication (Subotnik et al., 2011). A medication stabilization period, typically about 3 months, was used to reduce acute psychotic symptoms, given that patients usually entered the study immediately following hospital discharge. No symptom remission requirement was used, and no patients were excluded due to continued symptoms. While most prior IPS studies have not used initial stabilization periods, those studies focused on long-term outpatients rather than patients entering in an acute psychotic state (Bond et al., 2008). Participants were then randomly assigned to either the combination of IPS and WFM training or to an equally intensive BVR condition (vocational rehabilitation through conventional outside agencies plus social skills training). A 2/3 v. 1/3 ratio (Ns of 46 for IPS-WFM and 23 for BVR) was used to allow examination of outcome predictors within IPSWFM. Data were collected from 2000 to 2006.
Individual Placement and Support
IPS followed the principles of this form of supported employment (Becker and Drake, 2003; Drake et al., 2012), but was adapted to a first-episode sample by providing supported education for participants whose preferences and situations made resuming education more appropriate than returning to employment (Nuechterlein et al., 2008). The common principles are: (1) the goal is competitive employment or schooling in typical community settings, (2) IPS services integrated into the mental health treatment team, (3) rapid search for schooling or employment, (4) eligibility based on participant choice, (5) attention to the individual’s job/school preferences, (6) continuous individualized support, (7) community outreach, and (8) disability benefits counseling. The IPS specialist (L.R.T.) was a member of the clinical team of psychiatrists, psychologists, and social workers, coordinated treatments with them to optimize work recovery, and met with the participants at the clinic, their homes, and their school or work settings, as appropriate for each individual. IPS fidelity was good (score of 101 on IPS-25) (Becker et al., 2008), with the major limitations being use of research-based exclusion criteria, an initial medication stabilization period, and only one IPS specialist. Participants varied widely in initial willingness to allow the IPS specialist to interact directly with potential employers or instructors, but they typically developed greater openness to this direct support over time. By study completion, 74% (34 of 46) approved and received direct IPS help with employers or instructors in the community (Nuechterlein et al., 2008). The remaining 26% received IPS help behind the scenes. Initially 54% (25 of 46) prohibited disclosure of their disability or psychiatric condition. However, disclosure of disability was found to be needed for only 26% (12 of 46) of patients, so this was not a major factor inhibiting IPS intervention (Nuechterlein et al., 2008).
Workplace Fundamentals Module
The WFM uses a group-based skills training approach emphasizing social and problem-solving skills necessary for keeping a job (Wallace and Tauber, 2004). Skill areas included: (1) how work/school changes your life; (2) learning about your place of work or school; (3) identifying stressors; (4) solving problems; (5) managing symptoms and medications; (6) managing health; (7) improving job/school performance; (8) socializing with fellow workers/students; and (9) finding motivation. Each involved showing videotaped scenarios, role played practice, generation and evaluation of solutions to individually relevant school/work problems, and individualized homework assignments. For WFM materials, see https://www.psychrehab.com/modules/module_workplace.html. Participants used the WFM Job Organizing Book during the group sessions, led by the case managers. To adapt the WFM to school settings, additional scenarios involving school situations were generated. Participants had 75 min groups weekly for 6 months, followed by booster groups of fading frequency over 6 months. Booster sessions occurred every other week in weeks 27–42 and monthly in weeks 43–52. Because clinic attendance was only 1 day a week, it did not interfere with work/school attendance. Participants attended a mean of 19.4 sessions.
BVR plus social skills training
For participants randomly assigned to the BVR condition, case managers made referrals to vocational rehabilitation services at separate agencies, similar to the RCT of Drake et al. with chronic patients (Drake et al., 1999). The case manager discussed the Department of Vocational Rehabilitation and other options and actively assisted in connections to these agencies. The vocational rehabilitation at local state agencies emphasized initial assessment of vocational abilities and interests, referrals to job openings and school opportunities, and arrangements to pay for schooling or job training, but not in-person, active outreach in the community. All patients were eligible for BVR services and were scheduled with their local vocational rehabilitation center immediately upon randomization. These centers were generally closer to the patients’ homes than UCLA. The study case managers ensured that all BVR patients had an initial appointment and served as the communications link with the VR center. To further equate the intensity of treatment to the IPS-WFM group, these individuals also participated in clinic-based skills training groups, matched in time to WFM. Skills training included medication management and communication skills training (Kopelowicz et al., 2006), but did not focus on workplace skills. The clinic-based treatments were delivered by the same staff members for both conditions, separated by day of the week to minimize contact between participants in the two conditions. The UCLA clinic team also had separate weekly case conferences for the two treatment conditions, with the IPS specialist attending only the IPSWFM case conference. Manualized materials for WFM and for the comparison social skills training maximized the fidelity of these treatments.
Assessments
A modified interview-based version of the work section of the Social Adjustment Scale (Weissman and Bothwell, 1976) was used to assess school and employment activities (Subotnik et al., 2008), completed by the case managers based on their ongoing interactions with the patients, family members, and employers or teachers. Mean inter-rater agreement for judging presence at competitive work or regular schooling was κ = 0.84. Completers of the Social Adjustment Scale were not blind to treatment condition, but presence/absence of work/school return is minimally subject to rater bias.
Antipsychotic medication adherence was rated on a 1 (complete adherence) to 5 (complete nonadherence) scale based on a combination of pill counts, plasma assays, psychiatrist ratings, and patient reports (Subotnik et al., 2011). Symptom severity was rated every 3 months on the Schedule for Assessment of Positive Symptoms (Andreasen, 1984b) and the Schedule for Assessment of Negative Symptoms (Andreasen, 1984a).
Analyses
Following the grant protocol, the primary analysis of treatment effects (IPS-WFM v. BVR) used data gathered at the end of the intensive treatment period (6-month point) and at the 18-month point. We hypothesized that differential participation in work or school would be apparent at the 6-month point, with months 7–18 being used primarily to examine duration of effects. Separate outcome analyses were completed for the 6- and 18-month points. The primary dichotomous outcome, participation in competitive work or school, was analyzed with χ2 and logistic regression. Group differences in duration of work/school were examined via t test.
Results
A CONSORT diagram is given in Fig. 1. Only one patient declined to participate due to disinterest in pursuing work or schooling, possibly due to the low threshold we used (possible interest in work or school) and because study entry in 75% of cases occurred before beginning federal Social Security disability benefits. The 69 randomized patients did not differ significantly in demographic, symptom severity, or illness history variables from 18 patients who met inclusion criteria but dropped out prior to randomization (Nuechterlein et al., 2008). As shown in Table 1, the groups randomized to IPS-WFM v. BVR did not differ significantly in demographic variables, illness history, symptom severity, intellectual functioning, or antipsychotic medication. The socioeconomic status of the two groups was comparable and ranged widely within groups [Revised Duncan Socioeconomic Index (Stevens and Featherman, 1981): IPSWFM: M =51.3, s.d. = 22.4, range = 17.4–88.4; BVR: M = 47.2, S.D. = 24.2, range = 15.7–88.4]. The vast majority of patients were recruited from public hospitals and clinics (85% of IPSWFM and 83% of BVR patients). Family psychoeducation was attended by 18 of 46 IPS-WFM families (39%) and nine of 23 BVR families (39%). Thus, randomization produced well-matched groups.
Fig. 1.
Participant flow in a randomized controlled trial of Individual Placement and Support (IPS) and the Workplace Fundamentals Module (WFM) in individuals with a recent first episode of schizophrenia.
Table 1.
Demographic and clinical data and antipsychotic medication for individuals with schizophrenia in Individual Placement and Support Plus Workplace Fundamentals Module Intervention (IPS-WFM) v. Conventional Brokered Vocational Rehabilitation plus social skills training intervention (BVR)
| IPS-WFM condition (n = 46) | Brokered vocational rehabilitation condition (n = 23) | |||
|---|---|---|---|---|
| Variable | M (S.D.) | M (S.D.) | T | p |
| Age at randomization | 24.2 (4.2) | 25.1 (3.8) | 0.87 | NS |
| Education (years) | 13.1 (1.8) | 13.5 (2.1) | 0.76 | NS |
| Highest parental education (years) | 14.7 (3.6) | 14.7 (4.0) | −0.01 | NS |
| Revised Duncan Socioeconomic lndexa | 51.3 (22.4) | 47.2 (24.2) | 0.67 | NS |
| Lifetime psychosis duration (months) | 8.7 (8.3) | 7.5 (6.6) | −0.59 | NS |
| Hospitalizations (number) | 1.3 (1.0) | 1.1 (0.9) | −0.64 | NS |
| Total hospitalization duration (weeks) | 1.9 (1.7) | 1.8 (2.9) | −0.18 | NS |
| BPRS mean of 24 items (1–7 scale)b | 1.7 (0.5) | 1.6 (0.5) | 0.08 | NS |
| BPRS mean of positive symptoms | 1.9 (1.1) | 1.8 (1.1) | 0.48 | NS |
| BPRS mean of negative symptoms | 2.3 (1.1) | 2.1 (1.1) | 0.90 | NS |
| BPRS mean of depr-anx symptoms | 1.9 (1.1) | 2.2 (1.1) | −1.05 | NS |
| WAIS Vocabulary Scaled Score | 8.7 (2.4) | 8.9 (3.1) | −0.31 | NS |
| WAIS Block Design Scaled Score | 9.7 (2.9) | 8.7 (2.9) | 1.39 | NS |
| N (%) | N (%) | x2 | P | |
| Gender (male) | 32 (70) | 14 (61) | 0.52 | NS |
| Marital status (single) | 34 (94) | 17 (90) | 0.44 | NS |
| Race | ||||
| White | 11 (24) | 7 (30) | 1.07 | NS |
| African American | 11 (24) | 4 (17) | ||
| Asian | 6 (13) | 2 (9) | ||
| Pacific Islander | 1 (2) | 1 (4) | ||
| More than one race | 17 (37) | 9 (39) | ||
| Hispanic ethnicity | 11 (24) | 7 (30) | 0.53 | NS |
| Public health system sourcec | 35 (85) | 15 (83) | 0.40 | NS |
| Antipsychotic medication at end of participationd | ||||
| Risperidone | 37 (80) | 19 (83) | 1.26 | NS |
| Aripiprizole | 5 (11) | 1 (4) | ||
| Olanzapine | 1 (2) | 1(4) | ||
| Quetiapine | 1 (2) | 1 (4) | ||
| Ziprazidone | 2 (4) | 1 (4) |
Based on highest status parental occupation.
Brief Psychiatric Rating Scale ratings at baseline.
Hospital source unspecified for nine patients.
All participants started on oral risperidone at baseline. They were switched to another antipsychotic medication if inadequate symptomatic response or intolerable side effects occurred.
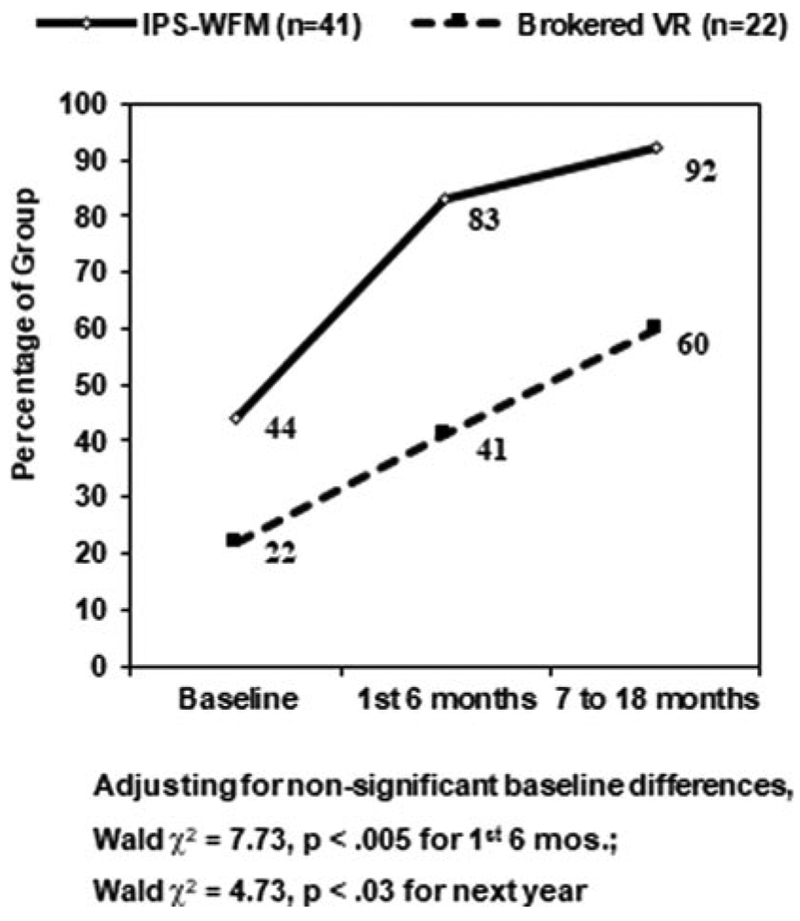
The first hypothesis concerned the likelihood of participating in school or a competitive job during the first 6 months of intensive treatment, defined as school courses relevant to a degree or vocational interest or paid jobs available to any applicant and at regular wages. By the end of the first 6 months, 83% (34 of 41) of IPS-WFM participants were in school or competitive employment, compared with 41% (nine of 22) of BVR participants, χ2 =11.67, df= 1, p < 0.001. Although all participants had a period of no work or school during and immediately after hospitalization, some participants (44% of IPS-WFM, 22% of BVR) started school or competitive employment within the initial medication stabilization period before entry into the randomized interventions. Thus, although this early return to school or work did not differ significantly between groups, we used logistic regression that entered baseline status on the dependent variable and group assignment as predictor variables. The 6-month outcome difference attributable to IPS-WFM treatment remained highly significant (Wald χ2 = 7.73, df = 1, p < 0.005).
The second hypothesis involved whether a higher likelihood of participation in school or competitive employment continued in the following year, during which treatment intensity was decreased. School/employment outcome data were available for 36 (88%) of the 41 IPS-WFM patients and 15 (68%) of the 22 BVR patients during months 7–18 [dropouts involved refusing treatment (IPS-WFM = 3, BVR = 5), moving out of region (IPS-WFM = 1, BVR = 2), or developing a serious medical condition (IPS-WFM = 1)]. Dropout frequency did not differ significantly between groups (χ2=1.35, df = 1, p = 0.25). We found that 92% (33 of 36) of IPS-WFM patients with 7–18 month data were in school or competitive employment during at least part of this period, compared with 60% (nine of 15) of BVR patients, χ2 = 7.31, df = 1, p < 0.007. Logistic regression correcting for non-significant group differences in baseline school/job status revealed that this difference continued to be significant (Wald χ2 = 4.73, df = 1, p < 0.03). School/work participation rates are summarized for the key study points in Fig. 2. Considering the entire 18-month period, 90% of the IPS-WFM group, compared with 59% of the comparison group, participated in competitive work or school (correcting for baseline, Wald χ2 = 5.82, df = 1, p < 0.02).
Fig. 2.
Percentage of first-episode schizophrenia patients in school or competitive employment at study baseline, during initial 6 months, and during following 1-year period.
The third hypothesis concerned whether IPS-WFM could increase the total amount of time in schooling or employment during the study. The 41 IPS-WFM patients had significantly longer mean time in schooling/employment than the 22 BVR patients [45.1 weeks (s.d. = 34.0) v. 26.3 weeks (s.d. = 42.2), unequal variance t = 3.06, df=32.9, p <0.004], considering all periods of education and competitive employment during the 18-month period. Thus, the IPS-WFM patients were in work/school 58% of the 78-week RCT period, compared with 34% for the BVR patients.
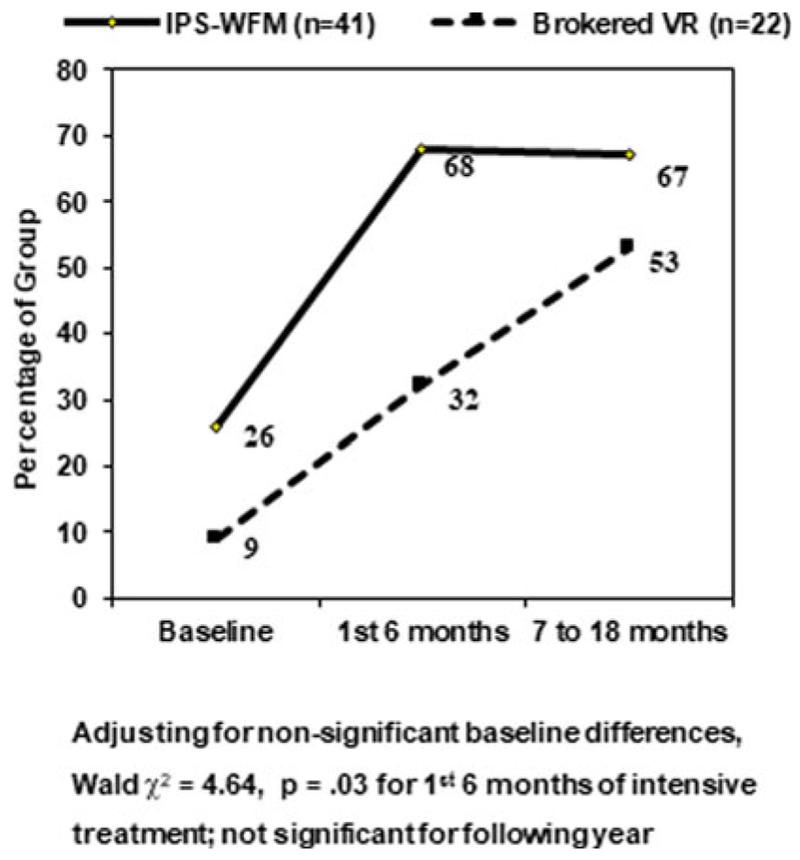
Supplemental analyses considered educational and job outcomes separately. As shown in Fig. 3, IPS-WFM patients had a substantially greater likelihood of returning to school during the initial 6 months than BVR patients [68% (28 of 41) v. 32% (seven of 22), logistic regression correcting for non-significant group differences in school status at baseline, Wald χ2 = 4.64, df = 1, p = 0.03]. The percentage of BVR patients returning to school continued to increase during the following year, resulting in absence of significant group differences during that period. Mean total number of weeks in schooling across the entire 18 months for all study participants was also significantly greater for IPS-WFM (25.7 weeks, s.d. = 22.9) compared with BVR (14.7 weeks, s.d. = 21.0), t = 2.09, df = 61, p = 0.04. For those who did attend school during the trial, the mean duration of individual periods of schooling was similar for IPS-WFM (17.8 weeks, s.d. = 17.6) and BVR groups (14.8 weeks, s.d. = 9.2), but the IPS-WFM group had more school periods than the BVR group (1.7 v. 1.0, s.d. = 1.7 and 1.2, t = 2.06, df = 57.1, p < 0.05). Thus, IPS-WFM may have aided patient persistence in pursuing further education as well as increasing the chances that they would attend at all.
Fig. 3.
Percentage of first-episode schizophrenia patients in school at study baseline, during initial six months, and during following 1-year period.
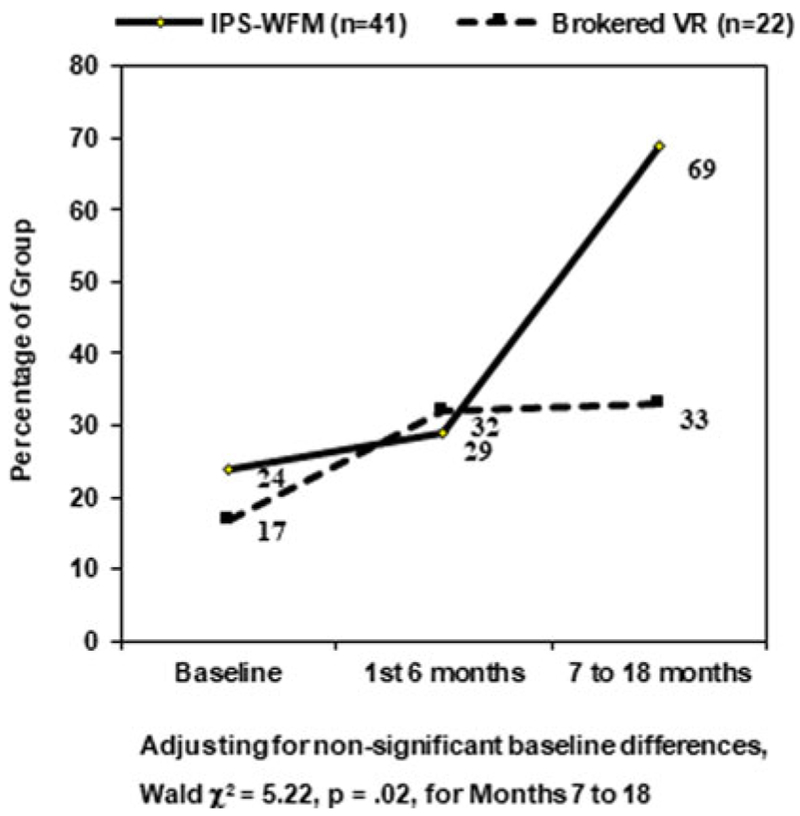
In contrast, return to competitive employment did not show group differences in the first 6 months (Fig. 4), but the IPSWFM group showed notable advantages for the following 1-year period [69% (25 of 36) v. 33% (five of 15), logistic regression correcting for non-significant group differences in baseline work status, Wald χ2 = 5.22, df = 1, p = 0.02]. Mean weeks in competitive employment for all study participants was also significantly greater for IPS-WFM (19.4 weeks, S.D. = 25.4) than for BVR (11.7, s.d. = 25.6), t = 2.07, df = 61, p = 0.04. Individual periods of employment tended to be longer for IPS-WFM than BVR (means of 20.4 v. 14.9 weeks, s.d. = 20.3 and 13.0) and the number of jobs held was somewhat greater (1.4 v. 1.0, s.d. = 1.1 and 1.3), but these differences were not statistically significant.
Fig. 4.
Percentage of first-episode schizophrenia patients in competitive employment at study baseline, during initial 6 months, and during following 1-year period.
IPS-WFM patients also tended to participate in both school and work more frequently than those in BVR, but this only approached statistical significance [29 of 46 (63%) v. nine of 23 (39%), χ2 = 3.54, df = 1, p = 0.06]. Most of these individuals had overlapping periods of school and work (68%).
Exploratory analyses examined medication adherence, symptom severity, and WFM attendance effects. Treatment group assignment did not impact medication adherence during the study (means of 2.30 for IPS-WFM and 2.34 for BVR). Better medication adherence during the first 6 months of intensive vocational treatment was significantly associated with being at work or school during this period (p < 0.035). Logistic regression showed that this tendency continued when treatment group and medication adherence were jointly considered as predictors of return to work or school during this period, but IPS-WFM treatment assignment was a stronger predictor (Wald χ2 = 7.35, p < 0.007, for group assignment; Wald χ2 = 2.87, p < 0.09, for medication adherence).
Severity of positive symptoms (SAPS) and negative symptoms (SANS) decreased significantly across groups during the first 6 months (p <0.03) but not during the next year. IPS-WFM v. BVR assignment did not differentially impact these changes. Baseline SAPS and SANS did not differ between groups, nor did they significantly predict return to work or school.
Number of WFM sessions attended was not significantly associated with the number of weeks worked or in school, although correlations were in the expected direction (r = 0.09–0.23). Furthermore, when number of attended skills training sessions was added to treatment group assignment as a predictor in logistic regression analyses, only IPS-WFM assignment significantly predicted return to work or school.
Discussion
This 18-month RCT demonstrates that the IPS-WFM enhanced vocational rehabilitation doubles the percentage of patients with a recent first episode of schizophrenia who are in competitive jobs or school within 6 months (83% v. 41%). Considered relative to non-significant baseline differences in work/school status, IPSWFM led to a 39% increase while conventional vocational rehabilitation led to a 19% increase. Furthermore, this RCT demonstrates for the first time that the advantage of IPS-WFM continues during a subsequent year of less intensive treatment, with a very high proportion of the IPS-WFM patients (92%, 33 of 36 for whom outcome data were available during this period) engaged in competitive work or school during at least part of this year. The total number of weeks of employment or schooling across all participants was also significantly and meaningfully longer with IPS-WFM compared with BVR (45 v. 26 of the 78 weeks).
The percentage of patients participating in competitive work or school within 6 months is very comparable to that obtained in the only published RCT that isolates IPS effects after a first psychotic episode (83% v. 85% in Killackey et al., 2008). These results confirm the efficacy of IPS in this early phase of psychosis, its applicability across the Australian and US mental health systems, and its superiority even in relationship to a comparison treatment of similar intensity. High rates of participation in work or school were also observed with first-episode patients in the RAISE Connection Program, which included IPS (68% by 6 months and 82% by 2 years) (Humensky et al., 2017).
Our evaluation of IPS-WFM over a period three times as long as the Killackey et al. (2008) first-episode psychosis RCT allowed the impact on the ability to hold a job or stay in school to be more clearly demonstrated, with the proportion of the RCT period actively engaged in work or school being substantially higher in the current study (58%) than in the prior one (33%). The extent to which the addition of WFM to IPS contributed to the greater proportion of time at work/school cannot be directly determined but might have played a role (Wallace and Tauber, 2004; Mueser et al., 2005; Tsang et al., 2009). Two RCTs with patients with long-established schizophrenia that added WFM to supported employment did not detect a significant impact on employment outcomes (Mueser et al., 2005; Glynn et al., 2017), but one that added similar work-related social skills training to IPS did find significant employment advantages (Tsang et al., 2010).
In the current RCT, IPS-WFM led to significantly higher rates of participation in school as well as to employment, whereas in the Killackey et al. (2008) RCT, the advantage was for employment alone. This difference in the two RCTs may be due to the greater proportion of first-episode psychosis patients who preferred return to school in the current study as compared with in Australia (Allott et al., 2013) and to the expanded supported education approach developed within the current study (Nuechterlein et al., 2008). It is noteworthy that the rate of return to school was immediately improved by IPS-WPM in the current study, while the advantages for employment were evident in the 7–18-month period. We observed school entry to be easier to arrange and less dependent on job availability, which may explain the faster school re-entry. The tendency for over half of our IPSWFM patients to return to both school and work during the study may also contribute, as in these instances school return often preceded employment.
The type of education and employment pursued was quite variable. Education involved General Educational Development (GED) credentialing programs or vocational schools (20%), community colleges (60%), or 4-year colleges (20%). Employment examples include movie usher, janitor, restaurant cook, research assistant, laboratory technician, and engineer.
Comparison of the present study sample with that of Killackey et al. (2008) would also initially suggest that the exclusion of individuals with prominent substance misuse and the use of a 3-month clinical stabilization period in the present study led to a more select sample than in the Killackey et al. study. However, the Killackey et al. study (personal communication, March 2017) drew its participants from the Early Psychosis Prevention and Intervention Centre, which also screened out individuals with possible substance-induced psychosis and which had clinically stabilized patients for about 9 months prior to IPS study entry.
Limitations of this study include sample size, use of a single IPS specialist, lack of separate evaluation of IPS and WFM effects, frequent psychiatrist and case manager contacts, use of an initial stabilization period, and restriction of sampling to patients with well-diagnosed schizophrenia or schizoaffective disorder who did not have extensive drug use comorbidity or neurological disorder. A larger sample size would allow multiple IPS specialists. Recruitment of large first-episode samples at a single site is difficult in the USA, as no centralized early psychosis intervention system exists. The combination of IPS and WFM was desirable for an initial RCT to determine their joint impact, but a research design allowing delineation of their separate effects would be a useful addition. Weekly clinic visits, while provided to both treatment groups, might have increased overall retention in this study. The frequent clinic visits may not be possible in a typical community clinic. However, the recent RAISE-ETP and RAISE Connection Program studies do demonstrate that IPS can be successfully implemented in early psychosis programs in US community clinics (Dixon et al., 2015; Kane et al., 2016). The use of an initial stabilization period seemed wise because patients typically entered the program in an acute psychotic state, but this aspect is a departure from the ‘rapid job search’ approach used in IPS studies of more chronically ill patients. Similarly, while sampling of patients without substantial substance misuse or neurological disorder was appropriate for a tightly controlled efficacy study, RCTs with a broader range of first-episode psychosis patients should evaluate the boundaries of the advantages of enhanced work rehabilitation.
In summary, this study demonstrates the substantial benefits of the combined IPS-WFM treatment for helping first-episode psychosis patients return to competitive work or school and to extend work/school participation over time. Combined with other RCT studies of IPS applied with first-episode patients (Killackey et al., 2008; Kane et al., 2016), these results support the broader application of supported education/employment approaches at the beginning of psychotic illnesses.
Acknowledgements.
We gratefully acknowledge the very able assistance of UCLA Aftercare Research Program treating psychiatrists Martha Love, M.D., and Benjamin Siegel, M.D., and therapists Kimberly Baldwin, M.F.T., Rosemary Collier, M.A., Sally Friedlob, M.S.W., Deborah Gioia, Ph.D., and Tasha Nienow, Ph.D. We thank the patients for their participation in this research. Dr Wallace passed away before this manuscript version was completed.
Financial support. This research was supported by the National Institute of Mental Health research grants MH37705 and MH066286 to K. Nuechterlein and by supplemental support from Janssen Scientific Affairs, LLC. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health, the National Institutes of Health, or Janssen Scientific Affairs, LLC.
Footnotes
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S0033291718003860.
Conflict of interest. Dr Nuechterlein has received research grants for other research from Janssen Scientific Affairs, LLC, Posit Science, Inc., and Genentech, Inc., and has been a consultant to Astellas, Genentech, Janssen, Medincell, Otsuka, Takeda, and Teva. Dr Subotnik has received income from research grants from Janssen Scientific Affairs, LLC, and Genentech, Inc., and has been a consultant to Genentech, Medincell, and Otsuka. Dr Ventura has received research grants from Pfizer, Inc., Genentech, Inc., and Posit Science, Inc., income from research grants from Janssen Scientific Affairs, LLC, and Genentech, Inc., and has been a consultant to Boehringer-Ingelheim Pharmaceuticals, Inc. Dr Michael Gitlin has received honoraria and has been on the Speaker’s Bureau of Bristol Myers Squibb and Otsuka. Dr Drake and Ms Becker do not receive any funding directly from corporations, but The Geisel Medical School at Dartmouth received gifts from the Johnson & Johnson Office of Corporate Contributions to help states to implement supported employment. Dr Drake and Dr Becker are now affiliated with Westat. Dr Liberman received a research grant from the Nathan Cummings Foundation and has been a consultant to Janssen Pharmaceutica and F. Hoffmann-La Roche Pharmaceutical Corporation. Dr Turner, Dr Gretchen-Doorly, and Dr Wallace report no financial relationships with commercial interests.
References
- Allott KA, Turner LR, Chinnery GL, Killackey EJ and Nuechterlein KH (2013) Managing disclosure following recent-onset psychosis: utilizing the individual placement and support model. Early Intervention in Psychiatry 7, 338–344. [DOI] [PubMed] [Google Scholar]
- Andreasen NC (1984a) The Scale for the Assessment of Negative Symptoms (SANS). Iowa City, IA: The University of Iowa. [Google Scholar]
- Andreasen NC (1984b) The Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, IA: The University of Iowa. [Google Scholar]
- Becker D and Drake R (2003). A Working Life for People with Severe Mental Illness. New York: Oxford Press. [Google Scholar]
- Becker DR, Swanson S, Bond GR and Merrens MR (2008) Evidence-based Supported Employment Fidelity Review Manual. Lebanon, NH: Dartmouth Psychiatric Research Center. [Google Scholar]
- Bond GR (2004) Supported employment: evidence for an evidence-based practice. Psychiatric Rehabilitation Journal 27, 345–359. [DOI] [PubMed] [Google Scholar]
- Bond GR, Drake RE and Becker DR (2008) An update on randomized controlled trials of evidence-based supported employment. Psychiatric Rehabilitation Journal 31, 280–290. [DOI] [PubMed] [Google Scholar]
- Dixon LB, Goldman HH, Bennett ME, Wang Y, McNamara KA, Mendon SJ, Goldstein AB, Choi CW, Lee RJ, Lieberman JA and Essock SM (2015) Implementing coordinated specialty care for early psychosis: the RAISE connection program. Psychiatric Services 66, 691–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake RE, McHugo GJ, Bebout RR, Becker DR, Harris M, Bond GR and Quimby E (1999) A randomized clinical trial of supported employment for inner-city patients with severe mental illness. Archives of General Psychiatry 56, 627–633. [DOI] [PubMed] [Google Scholar]
- Drake RE, Bond GR and Becker DR (2012) Individual Placement and Support: An Evidence-Based Approach to Supported Employment. New York: Oxford University Press. [Google Scholar]
- Drake RE, Frey W, Bond GR, Goldman HH, Salkever D, Miller A, Moore TA, Riley J, Karakus M and Milfort R (2013) Assisting social security disability insurance beneficiaries with schizophrenia, bipolar disorder, or major depression in returning to work. American Journal of Psychiatry 170, 1433–1441. [DOI] [PubMed] [Google Scholar]
- Egnew R (1993) Supported education and employment: an integrated approach Psychosocial Rehabilitation Journal. Special Issue: Supported education; 17, 121–127. [Google Scholar]
- Egnew R (1997) Integrating supported education and supported employment. Journal of the California Alliance for the Mentally Ill. 8, 33–35. [Google Scholar]
- First M, Spitzer R, Gibbon M and Williams J (2001) Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition (SCID-I/P). New York: Biometrics Research Department, New York State Psychiatric Institute. [Google Scholar]
- Gioia D and Brekke JS (2003) Rehab rounds: use of the Americans with disabilities Act by young adults with schizophrenia. Psychiatric Services 54, 302–304. [DOI] [PubMed] [Google Scholar]
- Glynn SM, Marder SR, Noordsy DL, O’Keefe C, Becker DR, Drake RE and Sugar CA (2017) An RCT evaluating the effects of skills training and medication type on work outcomes among patients with schizophrenia. Psychiatric Services 68, 271–277. [DOI] [PubMed] [Google Scholar]
- Humensky JL, Essock SM and Dixon LB (2017) Characteristics associated with the pursuit of work and school among participants in a treatment program for first episode of psychosis. Psychiatric Rehabiliation Journal 40, 108–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judge AM, Estroff SE, Perkins DO and Penn DL (2008) Recognizing and responding to early psychosis: a qualitative analysis of individual narratives. Psychiatric Services 59, 96–99. [DOI] [PubMed] [Google Scholar]
- Kane JM, Robinson DG, Schooler NR, Mueser KT, Penn DL,Rosenheck RA, Addington J, Brunette MF, Correll CU, Estroff SE, Marcy P, Robinson J, Meyer-Kalos PS, Gottlieb JD, Glynn SM, Lynde DW, Pipes R, Kurian BT, Miller AL, Azrin ST, Goldstein AB, Severe JB, Lin H, Sint KJ, John M and Heinssen RK (2016) Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. American Journal of Psychiatry 173, 362–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killackey EJ, Jackson HJ and McGorry PD (2008) Vocational intervention in first-episode psychosis: Individual Placement and Support versus treatment as usual. British Journal of Psychiatry 193, 114–120. [DOI] [PubMed] [Google Scholar]
- Kopelowicz A, Liberman RP and Zarate R (2006). Recent advances in social skills training for schizophrenia. Schizophrenia Bulletin 32(suppl. 1), S12–S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam MM, Pearson V, Ng RM, Chiu CP, Law CW and Chen EY (2011) What does recovery from psychosis mean? Perceptions of young first-episode patients. International Journal of Social Psychiatry 57, 580–587. [DOI] [PubMed] [Google Scholar]
- Modini M, Tan L, Brinchmann B, Wang MJ, Killackey E, Glozier N, Mykletun A and Harvey SB (2016) Supported employment for people with severe mental illness: systematic review and meta-analysis of the international evidence. British Journal of Psychiatry 209, 14–22. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Aalto S, Becker DR, Ogden JS, Wolfe RS, Schiavo D, Wallace CJ and Xie H (2005) The effectiveness of skills training for improving outcomes in supported employment. Psychiatric Services 56, 1254–1260. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Dawson ME, Gitlin MJ, Ventura J, Goldstein MJ, Snyder KS, Yee CM and Mintz J (1992) Developmental processes in schizophrenic disorders: longitudinal studies of vulnerability and stress. Schizophrenia Bulletin 18, 387–425. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Miklowitz DJ, Ventura J, Gitlin MJ, Stoddard M and Lukoff D (2006) Classifying episodes in schizophrenia and bipolar disorder: criteria for relapse and remission applied to recent-onset samples. Psychiatry Research 144, 153–166. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Subotnik KL, Turner LR, Ventura J, Becker DR and Drake RE (2008) Individual Placement and Support for individuals with recent-onset schizophrenia: integrating supported education and supported employment. Psychiatric Rehabilitation Journal 31, 340–349. [DOI] [PubMed] [Google Scholar]
- Ramsay CE, Broussard B, Goulding SM, Cristofaro S, Hall D, Kaslow NJ, Killackey E, Penn D and Compton MT (2011) Life and treatment goals of individuals hospitalized for first-episode nonaffective psychosis. Psychiatry Research 189, 344–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinaldi M, McNeil K, Firn M, Koletsi M, Perkins R and Singh SP (2004) What are the benefits of evidence-based supported employment for patients with first-episode psychosis? Psychiatric Bulletin 28, 281–284. [Google Scholar]
- Rinaldi M, Killackey E, Smith J, Shepherd G, Singh SP and Craig T (2010) First episode psychosis and employment: a review. International Review of Psychiatry 22, 148–162. [DOI] [PubMed] [Google Scholar]
- Roe D (2001) Progressing from patienthood to personhood across the multidimensional outcomes in schizophrenia and related disorders. Journal of Nervous and Mental Disease 189, 691–699. [DOI] [PubMed] [Google Scholar]
- Rosenheck R, Mueser KT, Sint K, Lin H, Lynde DW, Glynn SM, Robinson DG, Schooler NR, Marcy P, Mohamed S and Kane JM (2017) Supported employment and education in comprehensive, integrated care for first episode psychosis: effects on work, school, and disability income. Schizophrenia Research 182, 120–128. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J and Robins E (1978) Research diagnostic criteria: rationale and reliability. Archives of General Psychiatry 35, 773–782. [DOI] [PubMed] [Google Scholar]
- Stevens G and Featherman DL (1981) A revised socioeconomic index of occupational status. Social Science Research 10, 364–395. [Google Scholar]
- Subotnik KL, Nuechterlein KH, Kelly KA, Kupic AL, Brosemer M and Turner LR (2008) Modified Version of the Social Adjustment Scale -Work Outcome (originally by M. Weisman & S. Bothwell, 1976). University of California, Los Angeles: Los Angeles, CA. [Google Scholar]
- Subotnik KL, Nuechterlein KH, Ventura J, Gitlin MJ, Marder S, Mintz J, Hellemann GS, Thornton LA and Singh IR (2011) Risperidone nonadherence and return of positive symptoms in the early course of schizophrenia. American Journal of Psychiatry 168, 286–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang HW, Chan A, Wong A and Liberman RP (2009) Vocational outcomes of an integrated supported employment program for individuals with persistent and severe mental illness. Journal of Behavior Therapy and Experimental Psychiatry 40, 292–305. [DOI] [PubMed] [Google Scholar]
- Tsang HW, Fung KM, Leung AY, Li SM and Cheung WM (2010) Three year follow-up study of an integrated supported employment for individuals with severe mental illness. Australian and New Zealand Journal of Psychiatry 44, 49–58. [DOI] [PubMed] [Google Scholar]
- Unger KV (1998) Handbook on Supported Education: Providing Services for Students with Psychiatric Disabilities. Baltimore, MD: Paul H. Brooks Publishing Co. [Google Scholar]
- Ventura J, Liberman RP, Green MF, Shaner A and Mintz J (1998) Training and quality assurance with the structured clinical interview for DSM-IV (SCID-I/P). Psychiatry Research 79, 163–173. [DOI] [PubMed] [Google Scholar]
- Ventura J, Subotnik KL, Guzik LH, Hellemann GS, Gitlin MJ, Wood RC and Nuechterlein KH (2011) Remission and recovery during the first out-patient year of the early course of schizophrenia. Schizophrenia Research 132, 18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace CJ and Tauber R (2004) Supplementing supported employment with workplace skills training. Psychiatric Services 55, 513–515. [DOI] [PubMed] [Google Scholar]
- Weissman MM and Bothwell S (1976) Assessment of social adjustment by patient self-report. Archives of General Psychiatry 33, 1111–1115. [DOI] [PubMed] [Google Scholar]