Abstract
Background
Although studies have shown improved pain, function, and patient satisfaction after total shoulder arthroplasty (TSA), preoperative factors predicting poor outcomes are unexplored. Comparison of postoperative complications between osteoarthritis (OA), cuff arthropathy (CA), and fracture patients is important for identifying at-risk patients.
Methods
Primary TSAs from 2014 to 2016 with preoperative OA, CA, and proximal humerus fractures as indications were queried from the National Surgical Quality Improvement Program database. Short-interval postoperative complications were compared using multivariate binary logistic regression, and postoperative time to discharge between groups was analyzed using univariate analysis of variance with Tukey comparison. Statistical significance was defined as P < .05 using SPSS software version 23.0 (IBM Corp., Armonk, NY, USA).
Results
Of 9684 TSA cases, the primary indication was OA in 6571 patients, CA in 725 patients, and fractures in 646 patients. Compared with fractures, OA patients had statistically significant lower risk of dislocation, readmission, return to operating room, nonhome discharge, surgical site infection, perioperative bleeding requiring transfusion, and pulmonary embolism (all P < .05). Statistically significant lower risk of dislocation, nonhome discharge, and transfusion was also found between CA and fracture patients (all P < .03). However, in comparing CA vs. OA as preoperative indications, only postoperative venous thromboembolism (odds ratio, 4.5; P = .01) and surgical site infection (odds ratio, 3.7; P = .007) were significant. Mean differences in discharge time were significant between both OA and CA groups compared with fractures (P < .001), but there was no significance between OA and CA (P = .116).
Conclusion
Proximal humerus fracture is a risk factor for increased postoperative complications compared with OA and CA. With new outcomes-based reimbursement models, nonroutine discharge and increased discharge time should be considered in arthroplasty planning.
Keywords: Shoulder arthroplasty, osteoarthritis, cuff arthropathy, humerus fracture, readmission, postoperative complications, discharge
Total shoulder arthroplasty (TSA) has been shown to reduce pain and to improve function and patient satisfaction. However, preoperative factors predicting poor outcomes remain relatively unexplored. With the increasing popularity of shoulder arthroplasty and a growing aging population that desires to remain active, the volume of TSAs increased by 534% from 2000 to 2010 in the United States.24 As surgeons' experience with both anatomic TSA and reverse TSA (RTSA) expands to include predictable improvements in range of motion and overall quality of life, surgical indications for shoulder arthroplasty have shifted from primarily glenohumeral osteoarthritis (OA) to now include rotator cuff arthropathy (CA), irreparable rotator cuff tears, and proximal humerus fractures.35 These expanded surgical indications along with an increased number of insured patients since the advent of the Affordable Care Act have contributed to a higher prevalence of arthroplasty patients with preoperative risk factors for costly care under hospital quality metrics.27 With the shift toward delivery of cost-efficient care through bundled payments and outcomes-based reimbursements, it is important for health care providers to consider risk factors that predict readmissions and postoperative complications.
The expanding surgical indications for TSA point to the growing diverse population of patients, pathologic processes, and comorbidities that uniquely affect recovery. For example, patients requiring TSA for revision as opposed to OA or CA have significant differences in inpatient hospital outcomes and risks for surgical site infection (SSI).32 Prior studies have suggested that complication rates are higher in patients undergoing revision compared with primary TSA as previous soft tissue disruption may be linked to poor arthroplasty outcomes, such as instability, infection, and nonunion after fracture.3, 32 Even in comparing patients presenting for revision TSA, the cause of revision, whether component loosening or pain, may predict better outcomes than in revisions performed for infection. The increasing rate of shoulder arthroplasty procedures will increase the need for revision surgery, and thus it is even more important to understand factors that contribute to poor outcomes.
Health care economics prioritizes patient satisfaction with cost-effective care. The literature is still unclear about the role of rotator cuff disease as it compares with arthroplasty outcomes for OA and proximal humerus fractures. In assessing preoperative risk factors and hospital course, the role of primary OA, CA, and fracture as modifiers to the postoperative TSA rehabilitation protocol is unclear.26 Studies have shown that readmission rates for pulmonary embolism (PE) after discharge for TSA are comparable to those after hip arthroplasty.9, 31, 38 Comparison of length of stay, discharge destination, readmission, infection, and postoperative thrombosis and transfusion rates between patients is important, especially for elderly patients who may benefit from early active rehabilitation and restoration of autonomy as quickly as possible. Moreover, identifying differences in outcomes between surgical indications may minimize the potential for future revision surgery in patients who may benefit from nonoperative treatment.
With the Centers for Medicare and Medicaid Services and Hospital Readmissions Reduction Program creating penalties for postoperative readmission, providers should be aware of patient comorbidities and indications that predict adverse outcomes. Many patients with newly acquired access to health care have increased risk factors for poor outcomes because of the relatively high rates of smoking status, pulmonary disease, and vascular disease.8 By understanding the role of surgical indications in postoperative outcomes, providers can better stratify and plan for the preoperative management and prevention of complications in at-risk patients that would fall outside a bundled payment model. In identifying OA, CA, fracture, and revision surgery as independent risk factors for increased hospital stay and short-interval postoperative complications, providers can better educate and inform patients on expectations of outcomes and time to discharge according to the primary diagnosis.
Methods
All TSAs from 2014 to 2016 were queried from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database. The NSQIP database includes deidentified perioperative data and patient information from >600 hospitals nationwide ranging from small community hospitals to large tertiary academic centers. Clinical information is gathered by trained data reviewers prospectively collecting perioperative information on site through outpatient clinic visits, inpatient provider notes, and direct interviews.16 During the years 2014-2016, there were 274 collected variables identified for surgical patients; these included demographics, elective status, discharge destination, preoperative laboratory values, operative time, intraoperative complications, and 30-day postoperative complication and readmission rates.
All surgical patients who underwent primary TSAs from 2014 to 2016 with preoperative OA, CA, and proximal humerus fractures as indications for operation were identified and selected with International Classification of Diseases codes and Current Procedural Terminology (CPT) code 23472, which included both anatomic TSAs and RTSAs. Revision TSA cases involving either the humeral or glenoid component were identified with CPT codes 23473 and 23474. Etiologic factors for revision TSA were identified through International Classification of Diseases codes and included dislocation, loosening, infection, fractures, stiffness, rotator cuff disease, and pain. Age, sex, body mass index (BMI), diabetes status, smoking status, steroid use, American Society of Anesthesiologists (ASA) class, operation time, and elective surgery status were compared to assess baseline characteristics.20, 22 Patients with routine intake of oral or parenteral corticosteroids or immunosuppressant medications within 30 days before surgery were categorized into the steroid group, whereas patients who smoked only cigarettes at any point within the past year before surgery were part of the smoking cohort.
Short-interval postoperative complications, including dislocation, readmission rate, nonroutine discharge, return to the operating room (OR), SSI, PE, deep venous thrombosis (DVT), bleeding requiring red blood cell transfusion, pneumonia, renal insufficiency, cardiac arrest, myocardial infarction, and urinary tract infection, were compared using bivariate and multivariate binary logistic regression. Discharge destination was dichotomized to routine (home) or nonroutine, which included rehabilitation and other care facilities. Reasons for readmission within 30 days of surgery included dislocation, infection, bleeding, pain, thrombosis, pneumonia, urinary tract infection, and cardiac complications. In the cohort of patients who were readmitted, bivariate logistic regression analysis was used to compare surgical indication and reason for readmission.
Multivariate binary logistic regression analyses were conducted to determine whether surgical indications of OA, CA, fracture, and revision were independent risk factors for postoperative complications. Regressions were adjusted for age, sex, elective status, BMI, diabetes status, smoking status, and steroid use and reported as odds ratios in relation to the 95% confidence interval. Postoperative time to discharge between surgical groups was analyzed by univariate analysis of variance with Tukey test for multiple comparisons. Statistical significance was defined as P < .05 using SPSS software version 23.0 (IBM Corp., Armonk, NY, USA).
Results
From 2014 to 2016, a total of 8614 patients undergoing TSAs were included in the study, including OA in 76% (n = 6570), CA in 8.40% (n = 725), fracture in 7.50% (n = 646), and revision in 7.80% (n = 673; Table I). Compared with OA, CA patients were more likely to be older (70.60 vs. 68.60 years), to be ASA class ≥3, to undergo shorter operative times, and to be diabetic (all P values < .004; Table II). Compared with both OA and CA, fracture patients were more likely to be older and female, to be smokers, to be ASA class ≥3, to undergo longer operative times, to be diabetic, and not to have elective surgery (all P < .024). Patients undergoing revision TSA were more likely to be younger, to have lower average BMI, to be smokers, to be ASA class ≥3, to have longer operative times, to be diabetic, and not to have elective surgery (all P < .013) compared with patients undergoing primary TSA for OA and CA. Patients undergoing primary TSA for fracture were more likely to be older, female, ASA class ≥3, and diabetic and not to have elective surgery (all P < .05) compared with revision patients. There was no difference in steroid use between the various surgical indication groups.
Table I.
Patients' demographic characteristics and comorbidity burden
| Baseline characteristics | OA (n = 6570) | CA (n = 725) | Fracture (n = 646) | Revision (n = 673) |
|---|---|---|---|---|
| Patients | 76 | 8.40 | 7.50 | 7.80 |
| Average age (yr) | 68.60 | 70.60 | 72.40 | 67.10 |
| Female sex | 53 | 55 | 81 | 56 |
| Average BMI, kg/m2 | 31.20 | 31.10 | 31.40 | 30.60 |
| Smoking | 9.80 | 11.90 | 12.80 | 16.60 |
| Steroid or immunosuppressant use | 4.40 | 5.90 | 4.30 | 4.90 |
| ASA class | 2.50 | 2.60 | 2.70 | 2.60 |
| Operation time (min) | 110 | 95.50 | 129 | 128 |
| Diabetes status | 16.60 | 19.70 | 25.20 | 20.60 |
| Not elective | 0.70 | 1.30 | 27.20 | 4.70 |
OA, osteoarthritis; CA, cuff arthropathy; BMI, body mass index; ASA, American Society of Anesthesiologists.
Categorical variables are presented as percentage.
Table II.
Comparison of baseline characteristics between all surgical groups and associated P values
| Baseline characteristics | Comparison of surgical indication |
|||||
|---|---|---|---|---|---|---|
| OA vs. fracture |
CA vs. fracture |
CA vs. OA |
OA/CA vs. revision |
Fracture vs. revision |
Fracture vs. OA/CA |
|
| P value | ||||||
| Average age | <.001 | .002 | <.001 | <.001 | <.001 | <.001 |
| Female sex | <.001 | <.001 | .276 | .148 | <.001 | <.001 |
| Average BMI | .070 | .929 | .159 | .006 | .755 | .100 |
| Smoking | .015 | .579 | .082 | <.001 | .053 | .024 |
| Steroid or immunosuppressant use | .925 | .185 | .064 | .688 | .623 | .788 |
| ASA class ≥3 | <.001 | <.001 | .004 | <.001 | .002 | <.001 |
| Operation time (min) | <.001 | <.001 | <.001 | <.001 | .629 | <.001 |
| Diabetes status | <.001 | .015 | .032 | .013 | .048 | <.001 |
| Not elective | <.001 | <.001 | .085 | <.001 | <.001 | <.001 |
OA, osteoarthritis; CA, cuff arthropathy; BMI, body mass index; ASA, American Society of Anesthesiologists.
Significant differences (P < .05) are indicated with bold text.
After controlling for age, sex, BMI, smoking, steroid use, ASA class, diabetes, and elective status in adjusted multivariate logistic regression analysis, CA patients were more likely to have postoperative SSI and DVT compared with OA patients (P = .007, .001; Table III). Compared with OA and CA patients, fracture patients were at a greater risk for readmission, postoperative dislocation, nonroutine discharge, return to the OR, SSI, PE, and postoperative bleeding requiring transfusion (P < .022; Table IV, Table V, Table VI). Patients undergoing revision TSA were at a greater risk for readmission, postoperative dislocation, return to the OR, SSI, DVT, and postoperative bleeding requiring transfusion compared with primary OA and CA patients (P < .013; Table VII). Compared with revision, fracture patients were at a greater risk for nonroutine discharge and postoperative bleeding requiring transfusion, but no statistically significant difference was seen in readmission, dislocation, SSI, or DVT rates (Table VIII).
Table III.
Bivariate and multivariate analysis of postoperative complications between CA and OA
| CA |
OA |
Bivariate analysis |
Multivariate analysis |
|||
|---|---|---|---|---|---|---|
| (n = 725), % | (n = 6570), % | Odds ratio | P value | Odds ratio | P value | |
| Readmission | 3.59 | 2.36 | 1.538 (1.008-2.346) | .046 | 1.420 (0.929-2.172) | .106 |
| Postoperative dislocation | 0.55 | 0.46 | 1.209 (0.425-3.443) | .722 | 1.283 (0.448-3.670) | .642 |
| Nonroutine discharge | 11.31 | 9.19 | 1.239 (0.967-1.586) | .090 | 1.042 (0.802-1.353) | .758 |
| Return to OR | 1.38 | 1.05 | 1.357 (0.695-2.650) | .371 | 1.373 (0.700-2.693) | .356 |
| Postoperative SSI | 0.83 | 0.26 | 3.217 (1.264-8.185) | .014 | 3.696 (1.432-9.541) | .007 |
| Postoperative PE | 0.55 | 0.27 | 2.019 (0.682-5.983) | .205 | 1.891 (0.635-5.630) | .253 |
| Postoperative DVT | 0.97 | 0.21 | 4.565 (1.837-11.348) | .001 | 4.533 (1.812-11.342) | .001 |
| Postoperative bleeding requiring transfusion | 2.34 | 1.60 | 1.478 (0.880-2.482) | .139 | 1.288 (0.763-2.173) | .343 |
| Postoperative pneumonia | 0.55 | 0.41 | 1.344 (0.469-3.853) | .582 | 1.252 (0.433-3.618) | .678 |
| Postoperative renal insufficiency | 0.14 | 0.08 | 1.814 (0.212-15.544) | .587 | 1.441 (0.165-12.570) | .741 |
| Postoperative cardiac arrest | 0.14 | 0.06 | N/A | .992 | N/A | .992 |
| Postoperative myocardial infarction | 0.41 | 0.17 | 2.478 (0.690-8.901) | .164 | 2.035 (0.561-7.387) | .280 |
| Postoperative urinary tract infection | 0.55 | 0.52 | 1.066 (0.377-3.014) | .903 | 0.940 (0.331-2.667) | .907 |
OA, osteoarthritis; CA, cuff arthropathy; OR, operating room; SSI, surgical site infection; PE, pulmonary embolism; DVT, deep venous thrombosis; N/A, not applicable.
Significant differences (P < .05) are indicated with bold text.
Table IV.
Bivariate and multivariate analysis of postoperative complications between fracture and OA/CA
| Fracture |
OA/CA |
Bivariate analysis |
Multivariate analysis |
|||
|---|---|---|---|---|---|---|
| (n = 646), % | (n = 7295), % | Odds ratio | P value | Odds ratio | P value | |
| Readmission | 6.81 | 2.48 | 2.871 (2.044-4.033) | <.001 | 2.335 (1.569-3.475) | <.001 |
| Postoperative dislocation | 2.01 | 0.47 | 4.386 (2.303-8.353) | <.001 | 4.991 (2.398-10.386) | <.001 |
| Nonroutine discharge | 35.45 | 9.40 | 5.360 (4.479-6.414) | <.001 | 2.494 (1.991-3.124) | <.001 |
| Return to OR | 2.79 | 1.06 | 2.687 (1.598-4.517) | <.001 | 2.571 (1.409-4.692) | .002 |
| Postoperative SSI | 0.62 | 0.32 | 1.970 (0.679-5.714) | .212 | 3.736 (1.246-11.201) | .019 |
| Postoperative PE | 0.93 | 0.30 | 3.099 (1.252-7.671) | .014 | 3.135 (1.180-8.328) | .022 |
| Postoperative DVT | 0.62 | 0.29 | 2.158 (0.739-6.306) | .160 | 1.636 (0.435-6.154) | .467 |
| Postoperative bleeding requiring transfusion | 14.55 | 1.67 | 10.012 (7.548-13.282) | <.001 | 4.847 (3.437-6.835) | <.001 |
| Postoperative pneumonia | 0.93 | 0.42 | 2.197 (0.913-5.285) | .079 | 0.716 (0.219-2.334) | .579 |
| Postoperative renal insufficiency | 0.31 | 0.08 | 3.773 (0.760-18.730) | .104 | 2.103 (0.286-15.484) | .466 |
| Postoperative cardiac arrest | 0.31 | 0.05 | 2.826 (0.315-25.321) | .353 | 0.618 (0.025-15.454) | .770 |
| Postoperative myocardial infarction | 0.62 | 0.19 | 3.240 (1.063-9.873) | .039 | 1.224 (0.276-5.418) | .790 |
| Postoperative urinary tract infection | 1.86 | 0.52 | 3.615 (1.879-6.952) | <.001 | 1.564 (0.664-3.681) | .306 |
OA, osteoarthritis; CA, cuff arthropathy; OR, operating room; SSI, surgical site infection; PE, pulmonary embolism; DVT, deep venous thrombosis.
Significant differences (P < .05) are indicated with bold text.
Table V.
Bivariate and multivariate analysis of postoperative complications between OA and fracture
| OA |
Fracture |
Bivariate analysis |
Multivariate analysis |
|||
|---|---|---|---|---|---|---|
| (n = 6570), % | (n = 646), % | Odds ratio | P value | Odds ratio | P value | |
| Readmission | 2.36 | 6.81 | 0.331 (0.234-0.467) | <.001 | 0.433 (0.286-0.657) | <.001 |
| Postoperative dislocation | 0.46 | 2.01 | 0.223 (0.116-0.430) | <.001 | 0.202 (0.091-0.445) | <.001 |
| Nonroutine discharge | 9.19 | 35.45 | 0.182 (0.152-0.219) | <.001 | 0.378 (0.300-0.476) | <.001 |
| Return to OR | 1.05 | 2.79 | 0.359 (0.212-0.609) | <.001 | 0.357 (0.191-0.667) | .001 |
| Postoperative SSI | 0.26 | 0.62 | 0.416 (0.140-1.241) | .116 | 0.225 (0.071-0.714) | .011 |
| Postoperative PE | 0.27 | 0.93 | 0.293 (0.116-0.741) | .009 | 0.280 (0.102-0.769) | .014 |
| Postoperative DVT | 0.21 | 0.62 | 0.343 (0.112-1.044) | .060 | 0.348 (0.096-1.264) | .109 |
| Postoperative bleeding requiring transfusion | 1.60 | 14.55 | 0.095 (0.071-0.128) | <.001 | 0.197 (0.137-0.282) | <.001 |
| Postoperative pneumonia | 0.41 | 0.93 | 0.440 (0.181-1.070) | .070 | 1.257 (0.366-4.312) | .717 |
| Postoperative renal insufficiency | 0.08 | 0.31 | 0.245 (0.047-1.267) | .093 | 0.449 (0.059-3.427) | .440 |
| Postoperative cardiac arrest | 0.06 | 0.31 | 0.393 (0.044-3.521) | .404 | 1.898 (0.072-50.024) | .701 |
| Postoperative myocardial infarction | 0.17 | 0.62 | 0.269 (0.085-0.848) | .025 | 0.732 (0.151-3.545) | .698 |
| Postoperative urinary tract infection | 0.52 | 1.86 | 0.275 (0.142-0.533) | <.001 | 0.764 (0.299-1.954) | .575 |
OA, osteoarthritis; OR, operating room; SSI, surgical site infection; PE, pulmonary embolism; DVT, deep venous thrombosis.
Significant differences (P < .05) are indicated with bold text.
Table VI.
Bivariate and multivariate analysis of postoperative complications between CA and fracture
| CA |
Fracture |
Bivariate analysis |
Multivariate analysis |
|||
|---|---|---|---|---|---|---|
| (n = 725), % | (n = 646), % | Odds ratio | P value | Odds ratio | P value | |
| Readmission | 3.59 | 6.81 | 0.509 (0.309-0.836) | .008 | 0.615 (0.357-1.061) | .081 |
| Postoperative dislocation | 0.55 | 2.01 | 0.270 (0.088-0.833) | .023 | 0.259 (0.078-0.857) | .027 |
| Nonroutine discharge | 11.31 | 35.45 | 0.226 (0.170-0.300) | <.001 | 0.394 (0.285-0.544) | <.001 |
| Return to OR | 1.38 | 2.79 | 0.488 (0.224-1.065) | .072 | 0.490 (0.211-1.137) | .097 |
| Postoperative SSI | 0.83 | 0.62 | 1.339 (0.376-4.767) | .652 | 0.832 (0.224-3.086) | .783 |
| Postoperative PE | 0.55 | 0.93 | 0.592 (0.166-2.106) | .418 | 0.529 (0.141-1.987) | .345 |
| Postoperative DVT | 0.97 | 0.62 | 1.565 (0.456-5.370) | .477 | 1.576 (0.396-6.272) | .519 |
| Postoperative bleeding requiring transfusion | 2.34 | 14.55 | 0.141 (0.083-0.239) | <.001 | 0.253 (0.144-0.447) | <.001 |
| Postoperative pneumonia | 0.55 | 0.93 | 0.592 (0.166-2.106) | .418 | 1.573 (0.348-7.112) | .556 |
| Postoperative renal insufficiency | 0.14 | 0.31 | 0.445 (0.040-4.916) | .509 | 0.647 (0.045-9.330) | .647 |
| Postoperative cardiac arrest | 0.14 | 0.31 | N/A | .992 | N/A | .992 |
| Postoperative myocardial infarction | 0.41 | 0.62 | 0.667 (0.149-2.991) | .597 | 1.490 (0.238-9.309) | .670 |
| Postoperative urinary tract infection | 0.55 | 1.86 | 0.293 (0.094-0.913) | .034 | 0.718 (0.195-2.642) | .619 |
CA, cuff arthropathy; OR, operating room; SSI, surgical site infection; PE, pulmonary embolism; DVT, deep venous thrombosis; N/A, not applicable.
Significant differences (P < .05) are indicated with bold text.
Table VII.
Bivariate and multivariate analysis of postoperative complications between OA/CA and revision
| OA/CA |
Revision |
Bivariate analysis |
Multivariate analysis |
|||
|---|---|---|---|---|---|---|
| (n = 7295), % | (n = 673), % | Odds ratio | P value | Odds ratio | P value | |
| Readmission | 2.48 | 5.05 | 0.480 (0.330-0.699) | <.001 | 0.512 (0.347-0.756) | .001 |
| Postoperative dislocation | 0.47 | 2.53 | 0.181 (0.100-0.325) | <.001 | 0.188 (0.103-0.342) | <.001 |
| Nonroutine discharge | 9.40 | 10.40 | 0.883 (0.681-1.145) | .346 | 0.943 (0.712-1.249) | .682 |
| Return to OR | 1.06 | 3.71 | 0.277 (0.175-0.437) | <.001 | 0.306 (0.190-0.492) | <.001 |
| Postoperative SSI | 0.32 | 2.53 | 0.122 (0.065-0.230) | <.001 | 0.132 (0.068-0.255) | <.001 |
| Postoperative PE | 0.30 | 0.59 | 0.506 (0.174-1.472) | .211 | 0.438 (0.149-1.283) | .132 |
| Postoperative DVT | 0.29 | 1.04 | 0.321 (0.129-0.798) | .014 | 0.311 (0.124-0.783) | .013 |
| Postoperative bleeding requiring transfusion | 1.67 | 5.50 | 0.292 (0.201-0.426) | <.001 | 0.318 (0.216-0.469) | <.001 |
| Postoperative pneumonia | 0.42 | 0.45 | 0.953 (0.291-3.126) | .937 | 1.051 (0.310-3.563) | .936 |
| Postoperative renal insufficiency | 0.08 | 0.00 | N/A | .992 | N/A | .992 |
| Postoperative cardiac arrest | 0.05 | 0.00 | N/A | .992 | N/A | .992 |
| Postoperative myocardial infarction | 0.19 | 0.15 | 1.292 (0.170-9.841) | .805 | 1.460 (0.187-11.386) | .718 |
| Postoperative urinary tract infection | 0.52 | 1.04 | N/A | .992 | N/A | .992 |
OA, osteoarthritis; CA, cuff arthropathy; OR, operating room; SSI, surgical site infection; PE, pulmonary embolism; DVT, deep venous thrombosis; N/A, not applicable.
Significant differences (P < .05) are indicated with bold text.
Table VIII.
Bivariate and multivariate analysis of postoperative complications between fracture and revision
| Fracture |
Revision |
Bivariate analysis |
Multivariate analysis |
|||
|---|---|---|---|---|---|---|
| (n = 646), % | (n = 673), % | Odds ratio | P value | Odds ratio | P value | |
| Readmission | 6.81 | 5.05 | 1.378 (0.869-2.186) | .173 | 1.196 (0.723-1.979) | .486 |
| Postoperative dislocation | 2.01 | 2.53 | 0.792 (0.382-1.645) | .533 | 0.936 (0.423-2.071) | .871 |
| Nonroutine discharge | 35.45 | 10.40 | 4.731 (3.521-6.356) | <.001 | 2.351 (1.687-3.278) | <.001 |
| Return to OR | 2.79 | 3.71 | 0.743 (0.401-1.375) | .344 | 0.787 (0.400-1.548) | .488 |
| Postoperative SSI | 0.62 | 2.53 | 0.240 (0.080-0.718) | .011 | 0.492 (0.159-1.523) | .218 |
| Postoperative PE | 0.93 | 0.59 | 1.568 (0.440-5.582) | .488 | 1.371 (0.369-5.091) | .637 |
| Postoperative DVT | 0.62 | 1.04 | 0.693 (0.195-2.466) | .571 | 0.510 (0.118-2.207) | .367 |
| Postoperative bleeding requiring transfusion | 14.55 | 5.50 | 2.927 (1.968-4.353) | <.001 | 1.542 (1.150-2.380) | .045 |
| Postoperative pneumonia | 0.93 | 0.45 | 2.094 (0.521-8.407) | .297 | 0.752 (0.166-3.410) | .712 |
| Postoperative renal insufficiency | 0.31 | 0.00 | N/A | .992 | N/A | .992 |
| Postoperative cardiac arrest | 0.31 | 0.00 | N/A | .992 | N/A | .992 |
| Postoperative myocardial infarction | 0.62 | 0.15 | 4.187 (0.467-37.560) | .201 | 1.787 (0.175-18.210) | .624 |
| Postoperative urinary tract infection | 1.86 | 1.04 | N/A | .992 | N/A | .992 |
OR, operating room; SSI, surgical site infection; PE, pulmonary embolism; DVT, deep venous thrombosis; N/A, not applicable.
Significant differences (P < .05) are indicated with bold text.
Among patients undergoing revision TSA, the most common reason for revision was prosthetic loosening (31.95%), followed by dislocation (12.78%) and infection, fracture, and rotator cuff disease (5.94%). Patients who underwent revision TSA for a primary diagnosis of infection were more likely to experience postoperative SSI (P < .001), whereas those undergoing revision with a primary diagnosis of dislocation were at a greater risk for postoperative DVT (P = .018; Table IX).
Table IX.
Comparison of etiologic factors for revision as independent risk factors for adverse outcomes
| Only revision surgery patients |
Independent risk factors for adverse outcomes |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Readmission |
Postoperative dislocation |
Postoperative SSI |
Postoperative DVT |
Nonhome discharge |
||||||
| Etiologic factor for revision (n = 673) | Odds ratio | P value | Odds ratio | P value | Odds ratio | P value | Odds ratio | P value | Odds ratio | P value |
| Dislocation (12.78%) | 0.648 (0.194-2.168) | .482 | 0.908 (0.204-4.041) | .899 | 0.908 (0.204-4.041) | .899 | 7.036 (1.397-35.438) | .018 | 1.479 (0.759-2.883) | .250 |
| Loosening (31.95%) | 1.020 (0.488-2.132) | .958 | 0.449 (0.128-1.578) | .212 | 0.885 (0.308-2.544) | .821 | 0.423 (0.049-3.646) | .434 | 0.837 (0.485-1.445) | .523 |
| Infection (5.94%) | 2.233 (0.746-6.683) | .151 | 0.000 | .998 | 7.393 (2.467-22.152) | <.001 | 0.000 | .998 | 0.955 (0.329-2.766) | .932 |
| Fracture (5.94%) | 0.988 (0.228-4.281) | .988 | 0.989 (0.128-7.650) | .991 | 0.000 | .998 | 3.221 (0.367-28.242) | .291 | 1.919 (0.815-4.518) | .136 |
| Stiffness (0.59%) | 0.000 | .999 | 0.000 | .999 | 0.000 | .999 | 0.000 | .999 | 0.000 | .999 |
| Rotator cuff disease (5.94%) | 1.575 (0.460-5.391) | .470 | 0.989 (0.128-7.650) | .991 | 0.000 | .998 | 0.000 | .999 | 1.248 (0.472-3.298) | .655 |
| Pain (5.05%) | 1.186 (0.272-5.167) | .821 | 1.180 (0.152-9.169) | .874 | 0.000 | .998 | 0.000 | .998 | 0.525 (0.123-2.239) | .384 |
| Other (31.79%) | ||||||||||
SSI, surgical site infection; DVT, deep venous thrombosis.
Significant differences (P < .05) are indicated with bold text.
In comparing only patients who were unexpectedly readmitted within 30 days of surgery, revision patients were at a greater risk for readmission for infection compared with OA and CA (P = .012) and fracture patients (P = .008; Table X). Among readmissions, CA patients were more likely to experience readmission for cardiac complications compared with OA patients (P = .028).
Table X.
Bivariate analysis and associated P values of reason for readmission among surgical groups
| Reason for readmission | OA |
Fracture |
Bivariate analysis |
|
|---|---|---|---|---|
| (n = 155), % | (n = 44), % | Odds ratio | P value | |
| Dislocation | 19.35 | 29.55 | 0.572 (0.268-1.224) | .150 |
| Infection | 10.97 | 4.55 | 2.587 (0.574-11.656) | .216 |
| Bleeding | 3.23 | 2.27 | 1.433 (0.163-12.599) | .745 |
| Pain | 2.58 | 4.55 | 0.556 (0.098-3.142) | .507 |
| PE or thrombosis | 7.10 | 9.09 | 0.764 (0.231-2.528) | .659 |
| Pneumonia | 10.97 | 6.82 | 1.684 (0.470-6.031) | .424 |
| Urinary tract infection | 4.52 | 2.27 | 2.034 (0.243-16.988) | .512 |
| Cardiac complications | 3.87 | 6.82 | 0.550 (0.132-2.296) | .412 |
| CA |
Fracture |
|||
|---|---|---|---|---|
| (n = 26), % | (n = 44), % | |||
| Dislocation | 15.38 | 29.55 | 0.434 (0.125-1.508) | .189 |
| Infection | 19.23 | 4.55 | 5.000 (0.894-27.693) | .067 |
| Bleeding | 11.54 | 2.27 | 5.609 (0.552-57.022) | .145 |
| Pain | 3.85 | 4.55 | 0.840 (0.072-9.744) | .889 |
| PE or thrombosis | 7.69 | 9.09 | 0.833 (0.142-4.898) | .840 |
| Pneumonia | 11.54 | 6.82 | 1.783 (0.332-9.563) | .500 |
| Urinary tract infection | 0.00 | 2.27 | N/A | .998 |
| Cardiac complications | 15.38 | 6.82 | 2.485 (0.510-12.113) | .260 |
| CA |
OA |
|||
|---|---|---|---|---|
| (n = 26), % | (n = 155), % | |||
| Dislocation | 15.38 | 19.35 | 0.758 (0.243-2.363) | .632 |
| Infection | 19.23 | 10.97 | 1.933 (0.645-5.793) | .239 |
| Bleeding | 11.54 | 3.23 | 3.913 (0.876-17.487) | .074 |
| Pain | 3.85 | 2.58 | 1.510 (0.162-14.068) | .717 |
| PE or thrombosis | 7.69 | 7.10 | 1.091 (0.228-5.230) | .913 |
| Pneumonia | 11.54 | 10.97 | 1.059 (0.287-3.902) | .932 |
| Urinary tract infection | 0.00 | 4.52 | N/A | .998 |
| Cardiac complications | 15.38 | 3.87 | 4.515 (1.180-17.278) | .028 |
| OA/CA |
Revision |
|||
|---|---|---|---|---|
| (n = 181), % | (n = 28), % | |||
| Dislocation | 18.78 | 25.00 | 0.642 (0.275-1.501) | .307 |
| Infection | 12.15 | 32.14 | 0.332 (0.140-0.786) | .012 |
| Bleeding | 4.42 | 0.00 | N/A | .998 |
| Pain | 2.76 | 0.00 | N/A | .998 |
| PE or thrombosis | 7.18 | 3.57 | 2.554 (0.323-20.194) | .374 |
| Pneumonia | 11.05 | 3.57 | 4.099 (0.531-31.621) | .176 |
| Urinary tract infection | 3.87 | 0.00 | N/A | .998 |
| Cardiac complications | 5.52 | 10.71 | 0.604 (0.157-2.321) | .463 |
| Fracture |
Revision |
|||
|---|---|---|---|---|
| (n = 44), % | (n = 28), % | |||
| Dislocation | 29.55 | 25.00 | 1.165 (0.429-3.166) | .765 |
| Infection | 4.55 | 32.14 | 0.114 (0.023-0.565) | .008 |
| Bleeding | 2.27 | 0.00 | N/A | .998 |
| Pain | 4.55 | 0.00 | N/A | .998 |
| PE or thrombosis | 9.09 | 3.57 | 3.300 (0.352-30.975) | .296 |
| Pneumonia | 6.82 | 3.57 | 2.415 (0.240-24.305) | .454 |
| Urinary tract infection | 2.27 | 0.00 | N/A | .998 |
| Cardiac complications | 6.82 | 10.71 | 0.756 (0.143-4.004) | .742 |
| Fracture |
OA/CA |
|||
|---|---|---|---|---|
| (n = 44), % | (n = 181), % | |||
| Dislocation | 29.55 | 18.78 | 1.813 (0.859-3.828) | .119 |
| Infection | 4.55 | 12.15 | 0.344 (0.078-1.522) | .160 |
| Bleeding | 2.27 | 4.42 | 0.503 (0.061-4.130) | .522 |
| Pain | 4.55 | 2.76 | 1.676 (0.314-8.940) | .545 |
| PE or thrombosis | 9.09 | 7.18 | 1.292 (0.400-4.174) | .668 |
| Pneumonia | 6.82 | 11.05 | 0.589 (0.167-2.079) | .411 |
| Urinary tract infection | 2.27 | 3.87 | 0.578 (0.069-4.824) | .613 |
| Cardiac complications | 6.82 | 5.52 | 1.251 (0.329-4.752) | .742 |
OA, osteoarthritis; PE, pulmonary embolism; CA, cuff arthropathy; N/A, not applicable.
Significant differences (P < .05) are indicated with bold text.
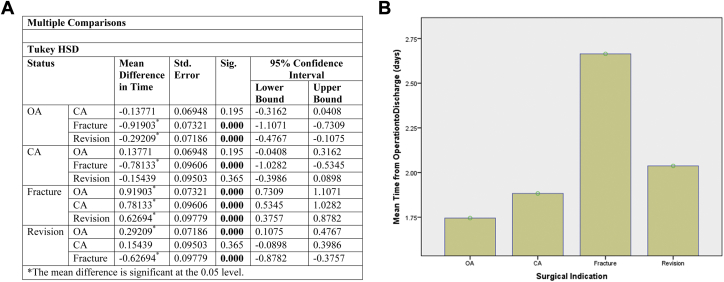
Time from operation to discharge was 1.75 days in OA, 1.88 days in CA, 2.66 days in fracture, and 2.04 days in revision (Fig. 1). Mean differences in discharge time were statistically significant between fracture and all other surgical indications (P < .001). Revision patients had a longer time to discharge compared with OA patients (P < .001).
Figure 1.
(A) Comparison of time from operation to discharge among surgical groups using univariate analysis of variance with Tukey test. (B) Comparison of mean time from operation to discharge among surgical indication groups. OA, osteoarthritis; CA, cuff arthropathy.
Discussion
As the landscape of health care economics shifts toward bundled outcomes-based reimbursements, providers must be aware of the differences in TSA postoperative outcomes to be expected between various evolving surgical indications. Patient demographics and associated risk factors are unique to each surgical indication group and affect the recovery process differently.5 Understanding the risks of adverse outcomes, such as DVT and SSI, is important in our population of aging patients with multiple comorbidities and is the initial step in being able to achieve cost-effectiveness and better use of resources.25
In comparing baseline characteristics between OA, CA, fracture, and revision, surgeons can better inform patients in the consent process and plan for interdisciplinary medical optimization of fracture patients, who are typically older, have a higher ASA class, and are more likely to have diabetes compared with OA and CA patients. The higher percentage of female patients in the fracture group and longer average operative times compared with OA and CA are characteristics that are likely to reflect poor bone stock and surgical technical difficulties of which the surgeon should be aware in predicting future clinical outcomes.37 Whereas there is limited and conflicting literature comparing hemiarthroplasty, internal fixation, and TSA for proximal humerus fractures, our findings of high percentages of ASA class ≥3, diabetics, and long operative times indicate the importance of counseling fracture patients that short-term TSA complications may reflect comorbidity rather than procedural outcomes.7 The high rates of smoking and younger age of revision patients must be considered in planning for postoperative rehabilitation protocols as smoking has been linked to prosthetic loosening, wound infections, and increased risk for further revision.34, 36 The younger age of revision patients in this study is consistent with other studies that found increased risk of revision and primary arthroplasty failure in younger patients.12, 14, 34, 36 Although the etiology is still unclear, the increased activity level and complex pathologic process, such as inflammatory arthritis, post-traumatic arthropathy, or capsulorrhaphy arthropathy, seen in younger patients are thought to contribute to increased implant failure rates compared with the elderly.12, 34 Previous reports have found revision arthroplasty outcomes inferior to outcomes after primary shoulder arthroplasty due to soft tissue injury, and this study warrants further discussion and education between the surgeon and young arthroplasty patients about careful postoperative rehabilitation and medical optimization.3, 4, 32
Whereas the long-term functional improvements and reoperation rates in CA patients after RTSA remain unclear, there have been no comparisons of short-term complications between OA and CA patients despite the fact that OA and CA represent a majority of arthroplasty indications.19 Previous reports have found CA associated with pseudoparalysis, anterosuperior escape, and comorbid conditions such as cervical radiculopathy to correlate with poor functional improvements.21 The greater risk of DVT and SSI in CA patients compared with OA patients should be considered for modifications to the postoperative rehabilitation protocol as patients are more likely to report index procedure dissatisfaction with unexpected inability to return to daily functioning.30 Although studies have shown CA to be a risk factor for revision surgery and failure to achieve American Shoulder and Elbow Surgeons minimal clinically important difference compared with OA, this study further expands the need to consider DVT and SSI in evaluating outcomes-based care. Guidelines for perioperative mechanical or chemical prophylaxis for thrombosis after shoulder arthroplasty have not been established but are important in preventing unexpected prolonged hospital stays and revisions.1 These unexpected outcomes are especially important to consider in fracture patients, who require extensive interdisciplinary postoperative care because of increased risk for readmission, postoperative dislocation, nonroutine discharge, return to the OR, SSI, PE, and postoperative bleeding requiring transfusion. Increased risk of nonroutine discharge, blood loss, and return to the OR compared with OA and CA suggest poorer return to independent mobility and activities of daily living with increased hospitalization costs.17
Previous studies have found revision arthroplasty groups to have worse functional outcomes and greater risk for postoperative complications compared with primary arthroplasty.3, 6, 10, 11, 32 In our study, revision patients were at a greater risk for readmission, postoperative dislocation, return to the OR, SSI, DVT, and postoperative bleeding requiring transfusion compared with primary OA and CA patients. Prior soft tissue mobilization and rotator cuff manipulation are thought to affect prosthetic implant stabilization and may play a role in the increased dislocation, infection, and bleeding rates seen in revision patients.28 Among revision patients, TSA for prior dislocation is a risk factor for postoperative DVT as implant stabilization must be carefully balanced with early return to activity. Dislocation, loosening, instability, and infection are common revision causes that may be due to the increased rate of Cutibacterium (formerly Propionibacterium) acnes colonization of the shoulder and implant.29 Among revision patients, infection as an etiologic factor was significantly associated with increased postoperative SSI, highlighting the importance of careful intraoperative and postoperative measures to prevent reoperation and site bleeding.
RTSA has become an increasingly popular option for treating proximal humerus fractures in the elderly as the need for cuff integrity and anatomic tuberosity healing is minimized.18 However, short-term adverse outcomes are important to consider in this older, female population with inherent risks of anesthesia because compromised vascularity and poor bone quality may necessitate revision surgery.13 Whereas treatment of proximal humerus fractures varies between conservative management, hemiarthroplasty, and TSA, the increased risk of nonroutine discharge compared with revision patients predicts poorer return to independent mobility and increased costs that should be balanced with lifestyle considerations. In this study, fracture patients are at an increased risk of postoperative bleeding requiring transfusion, which is consistent with prior reports of hematoma and instability after arthroplasty.2 Time from operation to discharge in fracture patients is significantly longer compared with the other surgical groups, and these associated increased hospitalization costs should be recognized and made clear to patients during preoperative planning.
There are limitations to be considered in using the NSQIP database despite the large number of patients and variables included. Complication rates are limited to 30-day outcomes, and although the use of RTSA is becoming more prevalent, CPT code 23472 was not able to separate reverse from anatomic arthroplasty. However, previous studies have found both anatomic TSA and RTSA to have similar complication rates, revision rates, and patient-reported outcomes, and this study focuses on short 30-day hospital quality metrics.15, 23, 33
Conclusions
Overall, this study provides evidence that surgical indication is an independent risk predictor for postoperative readmission, dislocation, nonroutine discharge, postoperative outcomes, and increased time to discharge. Understanding of surgical risk factors is important not only for managing patients' expectations but also for identifying indications that predict costly complications and adverse outcomes. With new outcomes-based reimbursement models, nonroutine discharge and increased discharge time in proximal humerus fracture patients should be considered in arthroplasty planning.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional Review Board approval is not required for this retrospective cohort study.
References
- 1.American Academy of Orthopaedic Surgeons . 2009. The treatment of glenohumeral joint osteoarthritis: guideline and evidence report.http://www.aaos.org/research/guidelines/glosummary.pdf Available at: accessed August 25, 2018. [DOI] [PubMed] [Google Scholar]; American Academy of Orthopaedic Surgeons. The treatment of glenohumeral joint osteoarthritis: guideline and evidence report; 2009. Available at: http://www.aaos.org/research/guidelines/glosummary.pdf. [DOI] [PubMed]
- 2.Anakwenze O.A., Zoller S., Ahmad C.S., Levine W.N. Reverse shoulder arthroplasty for acute proximal humerus fractures: a systematic review. J Shoulder Elbow Surg. 2014;23:e73–e80. doi: 10.1016/j.jse.2013.09.012. [DOI] [PubMed] [Google Scholar]; Anakwenze OA, Zoller S, Ahmad CS, Levine WN. Reverse shoulder arthroplasty for acute proximal humerus fractures: a systematic review. J Shoulder Elbow Surg 2014;23:e73-e80. doi: 10.1016/j.jse.2013.09.012. [DOI] [PubMed]
- 3.Boddapati V., Fu M.C., Schairer W.W., Gulotta L.V., Dines D.M., Dines J.S. Revision total shoulder arthroplasty is associated with increased thirty-day postoperative complications and wound infections relative to primary total shoulder arthroplasty. HSS J. 2018;14:23–28. doi: 10.1007/s11420-017-9573-5. [DOI] [PMC free article] [PubMed] [Google Scholar]; Boddapati V, Fu MC, Schairer WW, Gulotta LV, Dines DM, Dines JS. Revision Total Shoulder Arthroplasty is Associated with Increased Thirty-Day Postoperative Complications and Wound Infections Relative to Primary Total Shoulder Arthroplasty. HSS J. 2018 Feb;14(1):23-28. doi: 10.1007/s11420-017-9573-5. [DOI] [PMC free article] [PubMed]
- 4.Carroll R.M., Izquierdo R., Vazquez M., Blaine T.A., Levine W.N., Bigliani L.U. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: long-term results. J Shoulder Elbow Surg. 2004;13:599–603. doi: 10.1016/j.jse.2004.03.016. [DOI] [PubMed] [Google Scholar]; Carroll RM, Izquierdo R, Vazquez M, Blaine TA, Levine WN, Bigliani LU. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: long-term results. J Shoulder Elbow Surg 2004;13:599-603. doi: 10.1016/j.jse.2004.03.016. [DOI] [PubMed]
- 5.Chalmers P.N., Keener J.D. Expanding roles for reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2016;9:40–48. doi: 10.1007/s12178-016-9316-0. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chalmers PN, Keener JD. Expanding roles for reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2016 Mar;9(1):40-48. doi: 10.1007/s12178-016-9316-0. [DOI] [PMC free article] [PubMed]
- 6.Cheung E.V., Sperling J.W., Cofield R.H. Revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg. 2008;17:371–375. doi: 10.1016/j.jse.2007.09.003. [DOI] [PubMed] [Google Scholar]; Cheung EV, Sperling JW, Cofield RH. Revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg. 2008 May-Jun;17(3):371-375. doi: 10.1016/j.jse.2007.09.003. [DOI] [PubMed]
- 7.Cvetanovich G.L., Chalmers P.N., Verma N.N., Nicholson G.P., Romeo A.A. Open reduction internal fixation has fewer short-term complications than shoulder arthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2016;25:624–631. doi: 10.1016/j.jse.2015.09.011. [DOI] [PubMed] [Google Scholar]; Cvetanovich GL, Chalmers PN, Verma NN, Nicholson GP, Romeo AA. Open reduction internal fixation has fewer short-term complications than shoulder arthroplasty for proximal humeral fractures. J Shoulder Elbow Surg. 2016 Apr;25(4):624-631. doi: 10.1016/j.jse.2015.09.011. [DOI] [PubMed]
- 8.Dailey E.A., Cizik A., Kasten J., Chapman J.R., Lee M.J. Risk factors for readmission of orthopaedic surgical patients. J Bone Joint Surg Am. 2013;95:1012–1019. doi: 10.2106/JBJS.K.01569. [DOI] [PubMed] [Google Scholar]; Dailey EA, Cizik A, Kasten J, Chapman JR, Lee MJ. Risk factors for readmission of orthopaedic surgical patients. J Bone Joint Surg Am. 2013 Jun 5;95(11):1012-1019. doi: 10.2106/JBJS.K.01569. [DOI] [PubMed]
- 9.Day J.S., Ramsey M.L., Lau E., Williams G.R. Risk of venous thromboembolism after shoulder arthroplasty in the Medicare population. J Shoulder Elbow Surg. 2015;24:98–105. doi: 10.1016/j.jse.2014.09.025. [DOI] [PubMed] [Google Scholar]; Day JS, Ramsey ML, Lau E, Williams GR. Risk of venous thromboembolism after shoulder arthroplasty in the Medicare population. J Shoulder Elbow Surg. 2015 Jan;24(1):98-105. doi: 10.1016/j.jse.2014.09.025. [DOI] [PubMed]
- 10.Deutsch A., Abboud J.A., Kelly J., Mody M., Norris T., Ramsey M.L. Clinical results of revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg. 2007;16:706–716. doi: 10.1016/j.jse.2007.01.007. [DOI] [PubMed] [Google Scholar]; Deutsch A, Abboud JA, Kelly J, Mody M, Norris T, Ramsey ML, et al. Clinical results of revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg. 2007 Nov-Dec;16(6):706-716. doi: 10.1016/j.jse.2007.01.007. [DOI] [PubMed]
- 11.Dines J.S., Fealy S., Strauss E.J., Allen A., Craig E.V., Warren R.F. Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am. 2006;88:1494–1500. doi: 10.2106/JBJS.D.02946. [DOI] [PubMed] [Google Scholar]; Dines JS, Fealy S, Strauss EJ, Allen A, Craig EV, Warren RF, Dines DM. Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am. J Bone Joint Surg Am. 2006 Jul;88(7):1494-1500. doi: 10.2106/JBJS.D.02946. [DOI] [PubMed]
- 12.Farng E., Zingmond D., Krenek L., Soohoo N.F. Factors predicting complication rates after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20:557–563. doi: 10.1016/j.jse.2010.11.005. [DOI] [PubMed] [Google Scholar]; Farng E, Zingmond D, Krenek L, Soohoo NF. Factors predicting complication rates after primary shoulder arthroplasty. J Shoulder Elbow Surg 2011;20:557-563. https://doi.org/10.1016/j.jse.2010.11.005 [DOI] [PubMed]
- 13.Ferrel J.R., Trinh T.Q., Fischer R.A. Reverse total shoulder arthroplasty versus hemiarthroplasty for proximal humeral fractures: a systematic review. J Orthop Trauma. 2015;29:60–68. doi: 10.1097/BOT.0000000000000224. [DOI] [PubMed] [Google Scholar]; Ferrel JR, Trinh TQ, Fischer RA. Reverse total shoulder arthroplasty versus hemiarthroplasty for proximal humeral fractures: a systematic review. J Orthop Trauma. 2015 Jan;29(1):60-68. doi: 10.1097/BOT.0000000000000224. [DOI] [PubMed]
- 14.Fevang B.T., Lie S.A., Havelin L.I., Skredderstuen A., Furnes O. Risk factors for revision after shoulder arthroplasty: 1,825 shoulder arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop. 2009;80:83–91. doi: 10.1080/17453670902805098. [DOI] [PMC free article] [PubMed] [Google Scholar]; Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Risk factors for revision after shoulder arthroplasty: 1,825 shoulder arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop 2009;80:83-91. No doi [DOI] [PMC free article] [PubMed]
- 15.Flurin P.H., Roche C.P., Wright T.W., Marczuk Y., Zuckerman J.D. A comparison and correlation of clinical outcome metrics in anatomic and reverse total shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2015;73(Suppl 1):S118–S123. [PubMed] [Google Scholar]; Flurin PH, Roche CP, Wright TW, Marczuk Y, Zuckerman JD. A Comparison and Correlation of Clinical Outcome Metrics in Anatomic and Reverse Total Shoulder Arthroplasty. Bull Hosp Jt Dis (2013). 2015 Dec;73 Suppl 1:S118-S123.No doi [PubMed]
- 16.Fu M.C., Boddapati V., Dines D.M., Warren R.F., Dines J.S., Gulotta L.V. The impact of insulin dependence on short-term postoperative complications in diabetic patients undergoing total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:2091–2096. doi: 10.1016/j.jse.2017.05.027. [DOI] [PubMed] [Google Scholar]; Fu MC, Boddapati V, Dines DM, Warren RF, Dines JS, Gulotta LV. The impact of insulin dependence on short-term postoperative complications in diabetic patients undergoing total shoulder arthroplasty. J Shoulder Elbow Surg. 2017 Dec;26(12):2091-2096. doi: 10.1016/j.jse.2017.05.027. [DOI] [PubMed]
- 17.Gallinet D., Clappaz P., Garbuio P., Tropet Y., Obert L. Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Surg Res. 2009;95:48–55. doi: 10.1016/j.otsr.2008.09.002. [DOI] [PubMed] [Google Scholar]; Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L. Three or four parts complex proximal humerus fractures: Hemiarthroplasty versus reverse prosthesis: A comparative study of 40 cases. Orthop Traumatol Surg Res. 2009 Feb;95(1):48-55. doi: 10.1016/j.otsr.2008.09.002. [DOI] [PubMed]
- 18.Garofalo R., Brody F., Castagna A., Ceccarelli E., Krishnan S.G. Reverse shoulder arthroplasty with glenoid bone grafting for anterior glenoid rim fracture associated with glenohumeral dislocation and proximal humerus fracture. Orthop Traumatol Surg Res. 2016;102:989–994. doi: 10.1016/j.otsr.2016.09.009. [DOI] [PubMed] [Google Scholar]; Garofalo R, Brody F, Castagna A, Ceccarelli E, Krishnan SG. Reverse shoulder arthroplasty with glenoid bone grafting for anterior glenoid rim fracture associated with glenohumeral dislocation and proximal humerus fracture. Orthop Traumatol Surg Res. 2016 Dec;102(8):989-994. doi: 10.1016/j.otsr.2016.09.009. [DOI] [PubMed]
- 19.Gerber C., Canonica S., Catanzaro S., Ernstbrunner L. Longitudinal observational study of reverse total shoulder arthroplasty for irreparable rotator cuff dysfunction: results after 15 years. J Shoulder Elbow Surg. 2018;27:831–838. doi: 10.1016/j.jse.2017.10.037. [DOI] [PubMed] [Google Scholar]; Gerber C, Canonica S, Catanzaro S, Ernstbrunner L. Longitudinal observational study of reverse total shoulder arthroplasty for irreparable rotator cuff dysfunction: results after 15 years. J Shoulder Elbow Surg. 2018 May;27(5):831-838. doi: 10.1016/j.jse.2017.10.037. [DOI] [PubMed]
- 20.Hackett N.J., De Oliveira G.S., Jain U.K., Kim J.Y. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015;18:184–190. doi: 10.1016/j.ijsu.2015.04.079. [DOI] [PubMed] [Google Scholar]; Hackett NJ, De Oliveira GS, Jain UK, Kim JY. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015 Jun;18:184-190. doi: 10.1016/j.ijsu.2015.04.079. [DOI] [PubMed]
- 21.Hartzler R.U., Steen B.M., Hussey M.M., Cusick M.C., Cottrell B.J., Clark R.E. Reverse shoulder arthroplasty for massive rotator cuff tear: risk factors for poor functional improvement. J Shoulder Elbow Surg. 2015;24:1698–1706. doi: 10.1016/j.jse.2015.04.015. [DOI] [PubMed] [Google Scholar]; Hartzler RU, Steen BM, Hussey MM, Cusick MC, Cottrell BJ, Clark RE, et al. Reverse shoulder arthroplasty for massive rotator cuff tear: risk factors for poor functional improvement. J Shoulder Elbow Surg. 2015 Nov;24(11):1698-1706. doi: 10.1016/j.jse.2015.04.015. [DOI] [PubMed]
- 22.Kay H.F., Sathiyakumar V., Yoneda Z.T., Lee Y.M., Jahangir A.A., Ehrenfeld J.M. The effects of American Society of Anesthesiologists physical status on length of stay and inpatient cost in the surgical treatment of isolated orthopaedic fractures. J Orthop Trauma. 2014;28:e153–e159. doi: 10.1097/01.bot.0000437568.84322.cd. [DOI] [PubMed] [Google Scholar]; Kay HF, Sathiyakumar V, Yoneda ZT, Lee YM, Jahangir AA, Ehrenfeld JM, Obremskey WT, Apfeld JC, Sethi MK. The effects of American Society of Anesthesiologists physical status on length of stay and inpatient cost in the surgical treatment of isolated orthopaedic fractures. J Orthop Trauma. 2014 Jul;28(7):e153-e159. doi: 10.1097/01.bot.0000437568.84322.cd. [DOI] [PubMed]
- 23.Kiet T.K., Feeley B.T., Naimark M., Gajiu T., Hall S.L., Chung T.T. Outcomes after shoulder replacement: comparison between reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:179–185. doi: 10.1016/j.jse.2014.06.039. [DOI] [PubMed] [Google Scholar]; Kiet TK, Feeley BT, Naimark M, Gajiu T, Hall SL, Chung TT, et al. Outcomes after shoulder replacement: comparison between reverse and anatomic total shoulder arthroplasty. Journal of Shoulder and Elbow Surgery.2015;24:179-185. doi: 10.1016/j.jse.2014.06.039. [DOI] [PubMed]
- 24.Kim S.H., Wise B.L., Zhang Y., Szabo R.M. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93:2249–2254. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed] [Google Scholar]; Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93:2249-2254. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed]
- 25.Madhusudhan T.R., Sinha A., Widdowson D. Deep vein thrombosis in shoulder arthroplasty—a prospective study. BMC Musculoskelet Disord. 2013;14:139. doi: 10.1186/1471-2474-14-139. [DOI] [PMC free article] [PubMed] [Google Scholar]; Madhusudhan TR, Sinha A, Widdowson D. Deep vein thrombosis in shoulder arthroplasty - a prospective study. BMC Musculoskelet Disord. 2013 Apr 18;14:139. doi: 10.1186/1471-2474-14-139. [DOI] [PMC free article] [PubMed]
- 26.Mahony G.T., Werner B.C., Chang B., Grawe B.M., Taylor S.A., Craig E.V. Risk factors for failing to achieve improvement after anatomic total shoulder arthroplasty for glenohumeral osteoarthritis. J Shoulder Elbow Surg. 2018;27:968–975. doi: 10.1016/j.jse.2017.12.018. [DOI] [PubMed] [Google Scholar]; Mahony GT, Werner BC, Chang B, Grawe BM, Taylor SA, Craig EV, et al. Risk factors for failing to achieve improvement after anatomic total shoulder arthroplasty for glenohumeral osteoarthritis. J Shoulder Elbow Surg. 2018 Jun;27(6):968-975. doi: 10.1016/j.jse.2017.12.018. [DOI] [PubMed]
- 27.Matsen F.A., 3rd, Li N., Gao H., Yuan S., Russ S.M., Sampson P.D. Factors affecting length of stay, readmission, and revision after shoulder arthroplasty: a population-based study. J Bone Joint Surg Am. 2015;97:1255–1263. doi: 10.2106/JBJS.N.01107. [DOI] [PubMed] [Google Scholar]; Matsen FA 3rd, Li N, Gao H, Yuan S, Russ SM, Sampson PD. Factors Affecting Length of Stay, Readmission, and Revision After Shoulder Arthroplasty: A Population-Based Study. J Bone Joint Surg Am. 2015 Aug 5;97(15):1255-1263. doi: 10.2106/JBJS.N.01107. [DOI] [PubMed]
- 28.Norris T.R., Iannotti J.P. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Shoulder Elbow Surg. 2002;11:130–135. doi: 10.1067/mse.2002.121146. [DOI] [PubMed] [Google Scholar]; Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Shoulder Elbow Surg 2002;11:130-135. doi: 10.1067/mse.2002.121146. [DOI] [PubMed]
- 29.Patel A., Calfee R.P., Plante M., Fischer S.A., Green A. Propionibacterium acnes colonization of the human shoulder. J Shoulder Elbow Surg. 2009;18:897–902. doi: 10.1016/j.jse.2009.01.023. [DOI] [PubMed] [Google Scholar]; Patel A, Calfee RP, Plante M, Fischer SA, Green A. Propionibacterium acnes colonization of the human shoulder. J Shoulder Elbow Surg.2009;18:897-902. doi: 10.1016/j.jse.2009.01.023. [DOI] [PubMed]
- 30.Petri M., Euler S.A., Dornan G.J., Greenspoon J.A., Horan M.P., Katthagen J.C. Predictors for satisfaction after anatomic total shoulder arthroplasty for idiopathic glenohumeral osteoarthritis. Arch Orthop Trauma Surg. 2016;136:755–762. doi: 10.1007/s00402-016-2452-6. [DOI] [PubMed] [Google Scholar]; Petri M, Euler SA, Dornan GJ, Greenspoon JA, Horan MP, Katthagen JC, et al. Predictors for satisfaction after anatomic total shoulder arthroplasty for idiopathic glenohumeral osteoarthritis. Arch Orthop Trauma Surg 2016;136:755-762. doi: 10.1007/s00402-016-2452-6. [DOI] [PubMed]
- 31.Phillips C.B., Barrett J.A., Losina E., Mahomed N.N., Lingard E.A., Guadagnoli E. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am. 2003;85-A:20–26. doi: 10.2106/00004623-200301000-00004. [DOI] [PubMed] [Google Scholar]; Phillips C.B., Barrett J.A., Losina E., Mahomed N.N., Lingard E.A., Guadagnoli E., et al: Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am. 2003 Jan;85-A(1):20-26.No doi [DOI] [PubMed]
- 32.Sajadi K.R., Kwon Y.W., Zuckerman J.D. Revision shoulder arthroplasty: an analysis of indications and outcomes. J Shoulder Elbow Surg. 2010;19:308–313. doi: 10.1016/j.jse.2009.05.016. [DOI] [PubMed] [Google Scholar]; Sajadi KR, Kwon YW, Zuckerman JD. Revision shoulder arthroplasty: an analysis of indications and outcomes. J Shoulder Elbow Surg. 2010 Mar;19(2):308-313. doi: 10.1016/j.jse.2009.05.016. [DOI] [PubMed]
- 33.Triplet J.J., Everding N.G., Levy J.C., Formaini N.T., O'Donnell K.P., Moor M.A. Anatomic and reverse total shoulder arthroplasty in patients older than 80 years. Orthopedics. 2015;38:e904–e910. doi: 10.3928/01477447-20151002-58. [DOI] [PubMed] [Google Scholar]; Triplet JJ, Everding NG, Levy JC, Formaini NT, O'Donnell KP, Moor MA, Virraroel LD. Anatomic and Reverse Total Shoulder Arthroplasty in Patients Older Than 80 Years. Orthopedics. 2015 Oct;38(10):e904-e910. doi: 10.3928/01477447-20151002-58. [DOI] [PubMed]
- 34.Wagner E.R., Houdek M.T., Schleck C.D., Harmsen W.S., Sánchez-Sotelo J., Cofield R. The role age plays in the outcomes and complications of shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1573–1580. doi: 10.1016/j.jse.2017.01.020. [DOI] [PubMed] [Google Scholar]; Wagner ER, Houdek MT, Schleck CD, Harmsen WS, Sanchez-Sotelo J, Cofield R, Elhassan BT, Sperling JW. The role age plays in the outcomes and complications of shoulder arthroplasty. J Shoulder Elbow Surg. 2017 Sep;26(9):1573-1580. doi: 10.1016/j.jse.2017.01.020. [DOI] [PubMed]
- 35.Wall B., Nové-Josserand L., O'Connor D.P., Edwards T.B., Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]; Wall B, Nove-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007 Jul;89(7):1476-1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed]
- 36.Werner B.C., Burrus M.T., Begho I., Gwathmey F.W., Brockmeier S.F. Early revision within 1 year after shoulder arthroplasty: patient factors and etiology. J Shoulder Elbow Surg. 2015;24:e323–e330. doi: 10.1016/j.jse.2015.05.035. [DOI] [PubMed] [Google Scholar]; Werner BC, Burrus MT, Begho I, Gwathmey FW, Brockmeier SF. Early revision within 1 year after shoulder arthroplasty: patient factors and etiology. J Shoulder Elbow Surg. 2015 Dec;24(12):e323-e330. doi: 10.1016/j.jse.2015.05.035. [DOI] [PubMed]
- 37.Werner B.C., Wong A.C., Mahony G.T., Craig E.V., Dines D.M., Warren R.F. Causes of poor postoperative improvement after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25:e217–e222. doi: 10.1016/j.jse.2016.01.002. [DOI] [PubMed] [Google Scholar]; Werner BC, Wong AC, Mahony GT, Craig EV, Dines DM, Warren RF, et al. Causes of poor postoperative improvement after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2016 Aug;25(8):e217-e222. doi: 10.1016/j.jse.2016.01.002. [DOI] [PubMed]
- 38.White R.H., Zhou H., Romano P.S. Incidence of symptomatic venous thromboembolism after different elective or urgent surgical procedures. Thromb Haemost. 2003;90:446–455. doi: 10.1160/TH03-03-0152. [DOI] [PubMed] [Google Scholar]; White R.H., Zhou H., and Romano P.S.: Incidence of symptomatic venous thromboembolism after different elective or urgent surgical procedures. Thromb Haemost. 2003 Sep;90(3):446-455. doi: 10.1160/TH03-03-0152. [DOI] [PubMed]