Abstract
Purpose
The artery of Adamkiewicz (AKA) provides the major blood supply to the anterior thoracolumbar spinal cord and iatrogenic injury or inadequate reconstruction of this vessel during vascular and endovascular surgery can result in postoperative neurological deficit due to spinal cord ischemia. The aim of this study was to provide comprehensive data on the prevalence and anatomical characteristics of the AKA.
Methods
An extensive search was conducted through the major electronic databases to identify eligible articles. Data extracted included study type, prevalence of the AKA, gender, number of AKA per patient, laterality, origin based on vertebral level, side of origin, morphometric data, and ethnicity subgroups.
Results
A total of 60 studies (n = 5437 subjects) were included in the meta-analysis. Our main findings revealed that the AKA was present in 84.6% of the population, and patients most frequently had a single AKA (87.4%) on the left side (76.6%) originating between T8 and L1 (89%).
Conclusion
As an AKA is present in the majority of the population, caution should be taken during vascular and endovascular surgical procedures to avoid injury or ensure proper reconstruction. All surgeons operating in the thoracolumbar spinal cord should have a thorough understanding of the anatomical characteristics and surgical implications of an AKA.
Electronic supplementary material
The online version of this article (10.1007/s00234-019-02207-y) contains supplementary material, which is available to authorized users.
Keywords: Adamkiewicz artery, Anatomy, Great anterior radiculomedullary artery, Thoracoabdominal aneurysm, Aortic aneurysm
Introduction
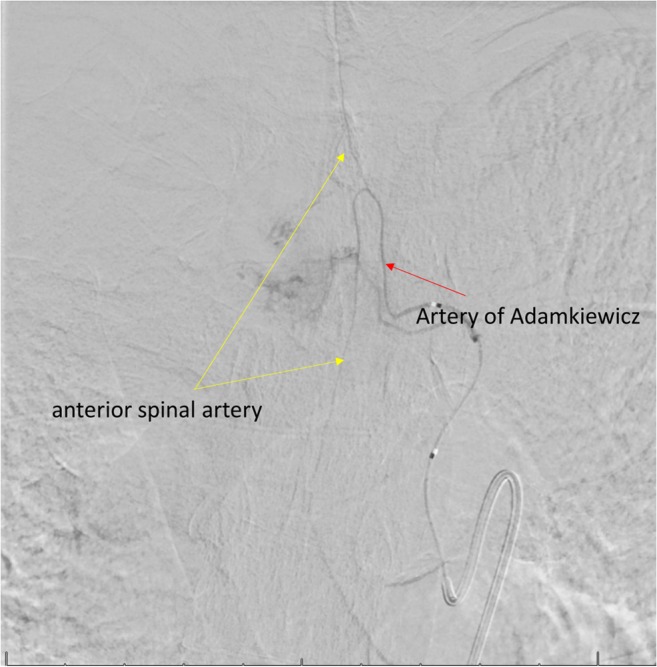
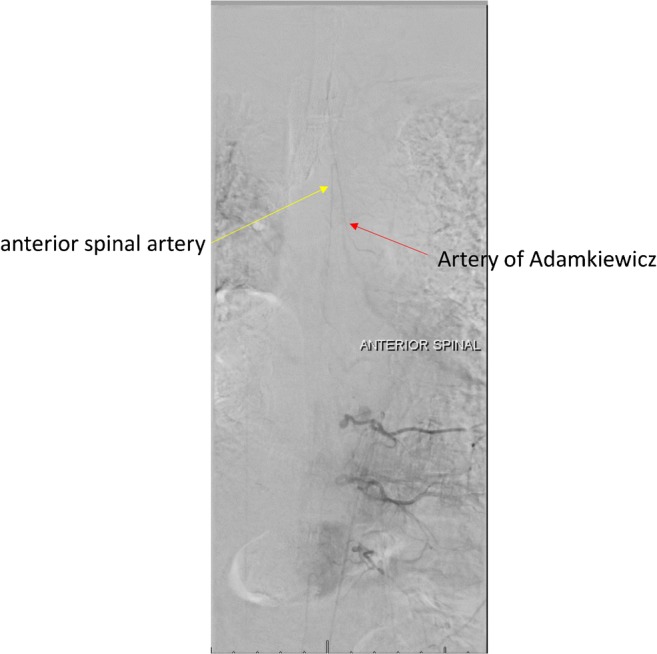
The artery of Adamkiewicz (AKA), also known as the great anterior radiculomedullary artery, is a major artery that joins the anterior spinal artery in the lower one-third of the spinal cord (Fig. 1) [1]. Because of its large role in feeding the spinal cord, many reports have stressed the importance of reattaching the intercostal or lumbar arteries to the AKA in the event of spinal cord ischemia following vascular and endovascular surgery (Fig. 2). Identification of the AKA preoperatively helps surgeons to determine the appropriate range of aortic lesions that require graft replacement [2]. Therefore, accurate localization and detailed anatomical knowledge of the AKA are important when planning surgical and interventional radiological treatments of thoracoabdominal diseases and spinal lesions in order to help reduce the risk of postoperative ischemic spinal complications and paraplegia.
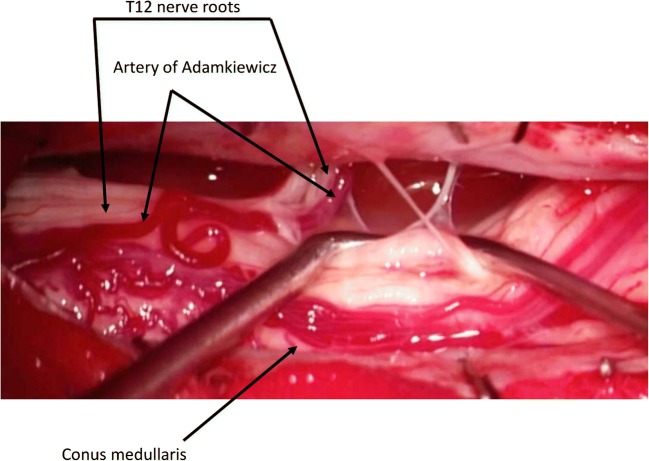
Fig. 1.
Vasculature of the spinal cord—the artery of Adamkiewicz (great radicular a.)
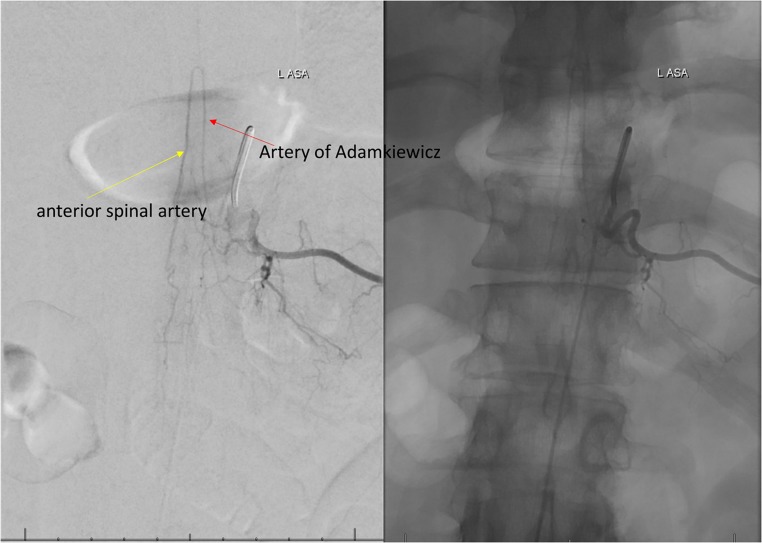
Fig. 2.
Intraoperative image of the artery of Adamkiewicz
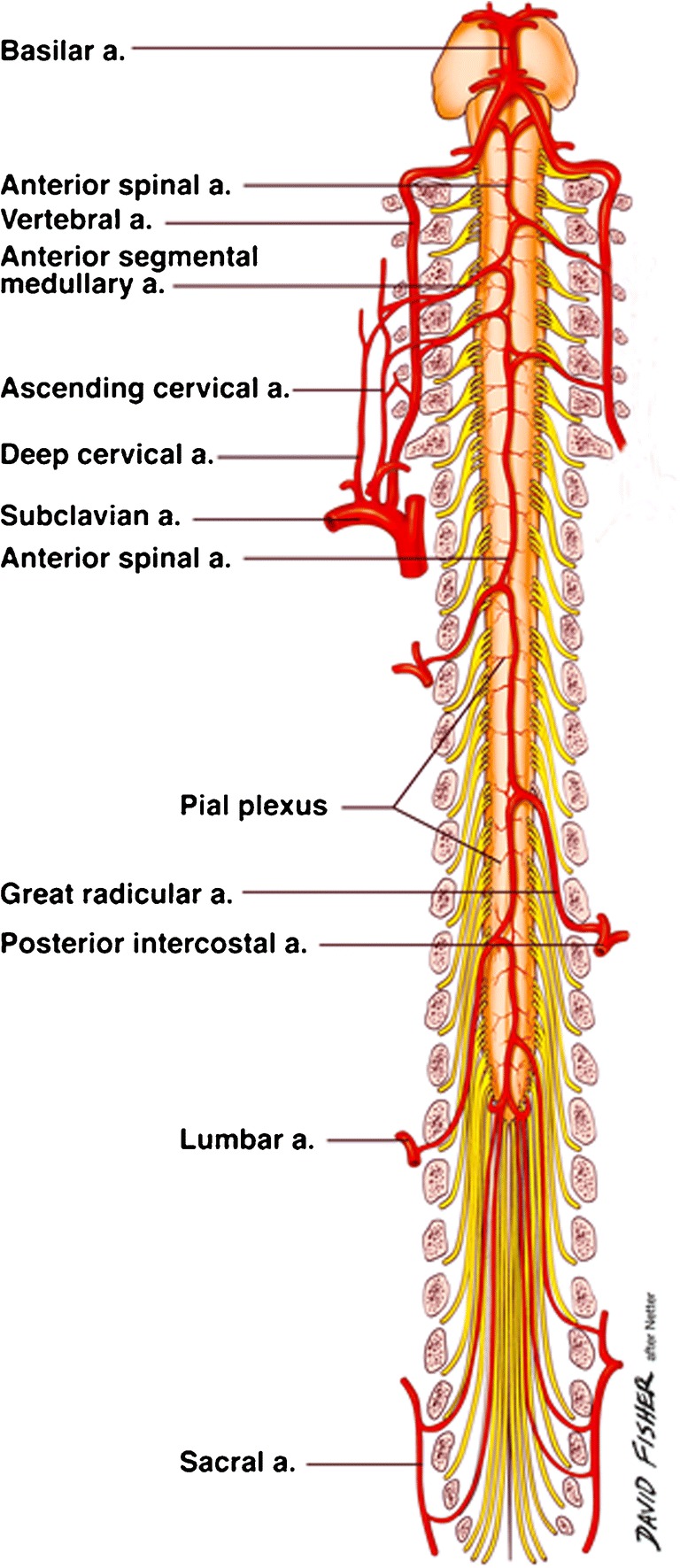
The AKA is the most dominant anterior radiculomedullary artery and is responsible for the arterial blood supply to the spinal cord from T8 to the conus medullaris [3]. Its origin is highly variable and extends from the mid-thoracic level to the lumbar levels, including the bilateral T3-T12 intercostal arteries [4] and L1-L4 lumbar arteries [5]. It typically arises from the T8–L1 neural foramina [6] from the left intercostal or lumbar arteries [7]. The AKA has a diameter of 0.8–1.3 mm, and the distal portion of this artery, together with the anterior spinal artery, forms a characteristic “hairpin” turn [8] (Fig. 3). Various techniques have been devised to preoperatively identify the location and anatomy of this artery. Such techniques include computed tomography angiography (CTA), magnetic resonance angiography (MRA), and digital subtraction angiography (DSA), with the latter considered the gold standard [9].
Fig. 3.
Cadaveric dissection of the artery of Adamkiewicz
The most important cause of injury to the AKA is iatrogenic, and in part, this is a factor of the high degree of variability in the anatomical location of this artery [10]. Preoperative AKA identification and its subsequent reconstruction or preservation may aid in reducing the incidence of postoperative neurological deficits and improving the outcomes of thoracolumbar surgical procedures. To this end, the aim of this study was to provide comprehensive data on the prevalence and anatomical characteristics of the AKA.
Materials and methods
Search strategy
A search of all major electronic databases (PubMed, EMBASE, ScienceDirect, China National Knowledge Infrastructure (CNKI), SciELO, BIOSIS, and Web of Science) was performed in order to identify potential articles. The following search terms were employed: artery of Adamkiewicz, arteria radicularis magna (ARM), radicularis magna, great radicular artery of Adamkiewicz, major anterior segmental medullary artery, great anterior segmental medullary artery, artery of the lumbar enlargement, arteria radicularis anterior magna, and great anterior radiculomedullary artery. A search through the references of the initially selected articles was conducted to identify any potential studies that were omitted. The authors adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines throughout this meta-analysis (Supplement 1).
Eligibility assessment
An eligibility assessment was conducted by two independent reviewers. Studies were included in this meta-analysis if they (1) provided complete data on the prevalence of the AKA or (2) provided data on the anatomy of AKA. The following exclusion criteria were employed: case, case-series, conference abstracts, letters to editors, and studies not published in peer-reviewed journals. Studies that were originally published in languages other than English were translated by medical professionals who are fluent both in English and the original language of the manuscript. All differences of opinion among the reviewers concerning the eligibility of the studies were resolved by consensus through consultation with the author of the respective study.
Data extraction
Two reviewers carried out data extraction independently. The following data was extracted: publication year, country of origin, study type (cadaveric, CTA, MRA, DSA), prevalence data of AKA, number of AKAs per patient, laterality of the AKA, origin of the AKA based on the vertebral level, side of origin, and morphometric data. In cases of incomplete data, the authors of the original articles were contacted for clarification.
Quality assessment
The AQUA tool [11] was used by the reviewers to evaluate quality and reliability of the included studies. In brief, the tool was devised to probe for potential risk of bias. Five domains were evaluated in the analysis: (1) objective(s) and subject characteristics, (2) study design, (3) methodology characterization, (4) descriptive anatomy, and (5) reporting of results; and each domain was categorized as either of “Low,” “High,” or “Unclear” risk of bias. Decision was made that a “No” answer in whichever signaling question within each of the categories arbitrated the domain to be of “High” risk of bias, whereas all answers “Yes” suggested that it presented a “Low” risk of bias. “Unclear” option was chosen when the study with incoherent data did not permit for a clear scrutiny.
Statistical analysis
The prevalence analysis was conducted using MetaXL version 5.8 by EpiGear Pty Ltd. (Wilston, Queensland, Australia). Morphometric analysis using Comprehensive Meta-Analysis version 3.3 yielded the pooled mean diameter of the AKA. Single and multi-categorical pooled prevalence rates were calculated using a random effects model. Heterogeneity was assessed using a chi-squared test and the I2 statistic. For the I2 statistic, the values of 0–40% indicated that heterogeneity might not be important; values of 30–60% could indicate moderate heterogeneity; values of 50–90% could indicate substantial heterogeneity; and values of 75–100% indicated considerable heterogeneity. A p value below 0.10 for Cochran’s Q suggested significant heterogeneity [12].
An analysis of the subgroups was conducted to determine the source of heterogeneity. The difference between the groups was considered to be insignificant if the confidence intervals (CIs) of specific rates overlapped [13]. Subgroups according to study type, gender, and geographical location were analyzed.
Results
Study identification and characteristics of included studies
The study identification process is presented in Fig. 4. An initial search yielded 747 entries. After thorough analysis, 627 entries were excluded. In total, 120 articles were analyzed, and 60 studies were included in this meta-analysis.
Fig. 4.
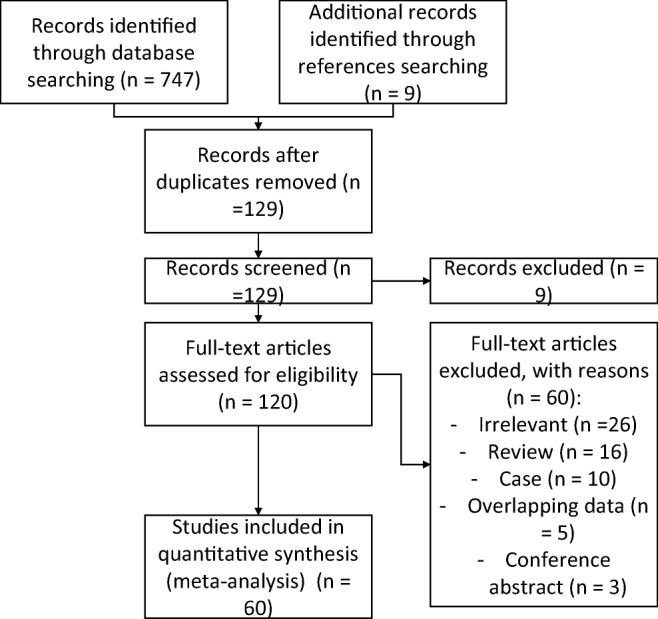
Flow diagram of included studies
The characteristics of the included studies are presented in Table 1. A total of 60 studies (4317 subjects with AKA) published between 1989 [14] and 2017 [15] were included [1–10, 14–62]. The studies originated from North America, Asia and Europe, and from ten different countries.
Table 1.
Characteristics of included studies
| Study | Country | Type of study | Number of subjects | % prevalence of AKA (no. of subjects with AKA) |
|---|---|---|---|---|
| Alleyne 1998 | USA | Cadaveric | 10 | 90.0 (9) |
| Amako 2011 | Japan | CTA | 110 | 100.0 (110) |
| Bachet 1996 | France | CTA | 36 | 77.8 (28) |
| Backes 2008 | Netherlands | MRA | 85 | 100.0 (85) |
| Biglioli 2004 | Italy | Cadaveric | 51 | 100.0 (51) |
| Bley 2010 | Germany | MRA | 68 | 88.2 (60) |
| Boll 2006 | USA | MDCT angiography | 100 | 100.0 (100) |
| Bowen 1996 | USA | MRA | 6 | 100.0 (6) |
| Champlin 1994 | USA | DSA | 61 | 32.8 (20) |
| Charles 2011 | France | DSA | 100 | 96.0 (96) |
| Fanous 2015 | USA | DSA | 34 | 70.6 (24) |
| Fereshetian 1989 | USA | DSA | 12 | 75.0 (9) |
| Furukawa 2010 | Japan | CTA | 37 | 100.0 (37) |
| Gailloud 2013 | USA | DSA | 50 | 92.0 (46) |
| Guzinski 2017 | Poland | MSCT | 200 | 21.5 (43) |
| Heinemann 1998 | Germany | DSA | 46 | 65.2 (30) |
| Hyodoh 2005 | Japan | MRA | 50 | 84.0 (42) |
| Hyodoh 2007 | Japan | MRA (double subtraction maximum intensity projection) | 170 | 82.4 (140) |
| Hyodoh 2009 | Japan | MRA | 82 | 81.7 (67) |
| Jaspers 2007 | Netherlands | MRA | 20 | 100.0 (20) |
| Kawaharada 2002 | Japan | MRA | 40 | 72.5 (29) |
| Kawaharada 2004 | Japan | MRA | 120 | 82.5 (99) |
| Kawaharada 2007 | Japan | MRA | 83 | 85.5 (71) |
| Kieffer 1989 | France | Arteriography | 45 | 88.9 (40) |
| Kieffer 2002 | France | Arteriography | 480 | 87.3 (419) |
| Koshino 1999 | Japan | Cadaveric | 102 | 88.2 (90) |
| Kovacs 2009 | Germany | CT | 51 | 70.6 (36) |
| Kroszczynski 2013 | USA | Cadaveric | 24 | 95.8 (23) |
| Kudo 2003 | Japan | MDCT | 19 | 68.4 (13) |
| Matsuda 2010 | Japan | MRA and CTA | 50 | 94.0 (47) |
| Matsuda 2010a | Japan | MRA and CTA | 60 | 80.0 (48) |
| Melissano 2009 | Italy | MDCT | 67 | 67.2 (45) |
| Mordasini 2012 | Switzerland | MRA | 24 | 83.3 (20) |
| Morishita 2003 | Japan | Cadaveric | 55 | 100.0 (55) |
| Murthy 2010 | USA | Spinal angiography | 248 | 46.4 (115) |
| Nakayama 2008 | Japan | CTA | 80 | 56.3 (45) |
| Nijenhuis 2004 | Netherlands | MRA | 8 | 100.0 (8) |
| Nijenhuis 2007 | Netherlands | MRA and CTA | 39 | 100.0 (39) |
| Nijenhuis 2007a | Netherlands | MRA | 60 | 100.0 (60) |
| Nishida 2014 | Japan | CT | 33 | 75.8 (25) |
| Nishii 2013 | Japan | CTA | 160 | 81.9 (131) |
| Nojiri 2007 | Japan | CTA | 27 | 100.0 (27) |
| Ogino 2006 | Japan | MRA | 92 | 70.7 (65) |
| Ou 2007 | France | CTA | 40 | 95.0 (38) |
| Polaczek 2014 | Poland | Cadaveric | 28 | 100.0 (28) |
| Rodriguez-Baeza 1991 | Spain | Cadaveric | 30 | 100.0 (30) |
| Schurink 2007 | Netherlands | MRA | 9 | 100.0 (9) |
| Sukeeyamonon 2010 | Thailand | MDCT angiography | 73 | 71.2 (52) |
| Takagi 2015 | Japan | MRA and MDCTA | 117 | 89.7 (105) |
| Takase 2002 | Japan | MDCT | 70 | 90.0 (63) |
| Takase 2007 | Japan | MDCT | 10 | 90.0 (9) |
| Tanaka 2016 | Japan | MRA and CTA | 1252 | 87.5 (1096) |
| Uotani 2008 | Japan | CTA | 32 | 78.1 (25) |
| Utsunomiya 2008 | Japan | CTA | 80 | 62.5 (50) |
| Williams 1991 | USA | Retrograde femoral artery catherization | 47 | 55.3 (26) |
| Yamada 2000 | Japan | MRA | 26 | 69.2 (18) |
| Yingbin 2013 | China | MDCT | 217 | 55.8 (121) |
| Yoshioka 2003 | Japan | MRA and CTA | 30 | 90.0 (27) |
| Yoshioka 2006 | Japan | MRA and CTA | 30 | 96.7 (29) |
| Zhao 2009 | China | MDCTA | 51 | 35.3 (18) |
Quality assessment
The majority of studies included in this meta-analysis, evaluated by the AQUA tool, revealed domain one (objective(s) and subject characteristics) and domain three (methodology characterization) to be at “High” risk of bias, owing to missing demographic data of the research group and no information regarding experience of the researchers. All studies had a “Low” risk of bias found in domain two (study design) and domain five (reporting of results), and almost all studies had a “Low” risk of bias found in domain four (descriptive anatomy). The AQUA tool evaluation can be found in Table 2.
Table 2.
The AQUA tool—tabular display
| Study | Risk of bias | ||||
|---|---|---|---|---|---|
| Objective(s) and study characteristics | Study design | Methodology characterization | Descriptive anatomy | Reporting of results | |
| Alleyne 1998 | High | Low | High | Low | Low |
| Amako 2011 | Low | Low | High | Low | Low |
| Bachet 1996 | High | Low | High | High | Low |
| Backes 2008 | High | Low | High | Low | Low |
| Biglioli 2004 | Low | Low | High | High | Low |
| Bley 2010 | Low | Low | High | Low | Low |
| Boll 2006 | High | Low | High | High | Low |
| Bowen 1996 | High | Low | High | Low | Low |
| Champlin 1994 | High | Low | High | Low | Low |
| Charles 2011 | High | Low | High | Low | Low |
| Fanous 2015 | High | Low | High | Low | Low |
| Fereshetian 1989 | High | Low | High | Low | Low |
| Furukawa 2010 | High | Low | High | Low | Low |
| Gailloud 2013 | High | Low | High | Low | Low |
| Guzinski 2017 | High | Low | High | Low | Low |
| Heinemann 1998 | High | Low | High | Low | Low |
| Hyodoh 2005 | High | Low | High | High | Low |
| Hyodoh 2007 | High | Low | High | Low | Low |
| Hyodoh 2009 | High | Low | High | High | Low |
| Jaspers 2007 | High | Low | High | Low | Low |
| Kawaharada 2002 | High | Low | High | Low | Low |
| Kawaharada 2004 | High | Low | High | Low | Low |
| Kawaharada 2007 | High | Low | High | Low | Low |
| Kieffer 1989 | High | Low | High | High | Low |
| Kieffer 2002 | High | Low | High | Low | Low |
| Koshino 1999 | High | Low | High | Low | Low |
| Kovacs 2009 | High | Low | High | Low | Low |
| Kroszczynski 2013 | High | Low | High | Low | Low |
| Kudo 2003 | High | Low | High | Low | Low |
| Matsuda 2010 | High | Low | High | High | Low |
| Matsuda 2010a | High | Low | High | High | Low |
| Melissano 2009 | High | Low | Low | High | Low |
| Mordasini 2012 | High | Low | Low | High | Low |
| Morishita 2003 | High | Low | High | Low | Low |
| Murthy 2010 | Unclear | Low | High | Low | Low |
| Nakayama 2008 | High | Low | Low | Low | Low |
| Nijenhuis 2004 | High | Low | Unclear | Low | Low |
| Nijenhuis 2007 | High | Low | High | Low | Low |
| Nijenhuis 2007a | High | Low | High | Low | Low |
| Nishida 2014 | High | Low | Low | High | Low |
| Nishii 2013 | High | Low | Low | High | Low |
| Nojiri 2007 | High | Low | High | Low | Low |
| Ogino 2006 | High | Low | High | High | Low |
| Ou 2007 | High | Low | Unclear | High | Low |
| Polaczek 2014 | High | Low | High | Low | Low |
| Rodriguez-Baeza 1991 | High | Low | High | Low | Low |
| Schurink 2007 | High | Low | High | Low | Low |
| Sukeeyamonon 2010 | High | Low | Low | High | Low |
| Takagi 2015 | High | Low | Low | Low | Low |
| Takase 2002 | High | Low | High | Low | Low |
| Takase 2007 | High | Low | High | High | Low |
| Tanaka 2016 | High | Low | High | Low | Low |
| Uotani 2008 | High | Low | High | Low | Low |
| Utsunomiya 2008 | High | Low | High | Low | Low |
| Williams 1991 | High | Low | High | Low | Low |
| Yamada 2000 | High | Low | High | Low | Low |
| Yingbin 2013 | High | Low | High | Low | Low |
| Yoshioka 2003 | High | Low | High | Low | Low |
| Yoshioka 2006 | High | Low | High | Low | Low |
| Zhao 2009 | High | Low | High | Low | Low |
Prevalence of the artery of Adamkiewicz
A total of 60 studies (n = 5437 subjects) reported data on the prevalence of the AKA. The pooled prevalence estimate (PPE) of the AKA was 84.6% (95% CI 79.7–89.0) (Table 3).
Table 3.
Overall prevalence of AKA
| Subgroup | Number of studies (number of subjects) | Pooled prevalence of AKA: % (95% CI) | I2 % (95% CI) | Cochran’s Q, p value | |
|---|---|---|---|---|---|
| Overall | 60 (5437) | 84.6 (79.7–89.0) | 95.3 (94.5–95.9) | < 0.001 | |
| Gender | Males | 15 (515) | 93.7 (83.3–100.0) | 94.0 (91.6–95.7) | < 0.001 |
| Females | 14 (345) | 90.4 (68.9–100.0) | 96.4 (95.2–97.4) | < 0.001 | |
| Type of study | Cadaveric | 7 (300) | 97.5 (92.4–100.0) | 72.2 (38.8–87.1) | 0.001 |
| CTA | 9 (602) | 88.1 (74.0–97.6) | 94.4 (91.4–96.4) | < 0.001 | |
| MRA | 16 (943) | 88.3 (81.9–93.4) | 85.1 (77.3–90.3) | < 0.001 | |
| DSA | 6 (303) | 75.4 (49.1–94.9) | 94.9 (91.2–97.0) | < 0.001 | |
| Country of origin | Japan | 27 (3017) | 85.3 (81.0–89.2) | 87.5 (83.0–90.8) | < 0.001 |
| USA | 10 (592) | 79.5 (57.0–95.7) | 96.3 (94.7–97.4) | < 0.001 | |
| France | 5 (701) | 89.8 (83.8–94.6) | 69.0 (20.4–87.9) | 0.012 | |
| Netherlands | 6 (221) | 99.4 (98.2–100.0) | 0.0 (0.0–0.0) | 0.972 | |
The subgroup analysis of gender differences showed that the AKA was slightly more prevalent in males (93.7% [95% CI 83.3–100.0]) than females (90.4% [95% CI 68.9–100.0]), although not significantly.
Seven cadaveric studies (n = 300) yielded the highest PPE of the AKA (97.5% [95% CI 92.4–100.0]) among the different study types. This was followed by MRA, CTA, and DSA studies with PPEs of 88.3%, 88.1%, and 75.4%, respectively (Table 3).
The subgroup analysis of geographical origin showed that the AKA was most prevalent in the Netherlands, with a PPE of 99.4% (95% CI 98.2–100.0); France with a PPE of 89.8% (95% CI 83.8–94.6); and Japan, with a PPE of 85.3 (95% CI 81.0–89.2). It was least prevalent in the USA, with a PPE of 79.5% (95% CI 57.0–95.7).
Number of arteries of Adamkiewicz per patient
An analysis of 20 studies (n = 1329 subjects with AKAs) showed that the majority of patients (87.4% [95% CI 83.4–91.9]) had one AKA. Patients presented with two AKAs in 11.3% (95% CI 7.5–15.8) of cases, three AKAs in 0.8% (95% CI 0.0–2.5) of cases, and four AKAs in 0.5% (95% CI 0.0–1.6) of cases.
In patients with two AKAs, the majority (73.3% [95% CI 47.3–93.4]) presented unilaterally as duplications. A total of 26.7% (95% CI 6.6–52.7; I2 66.2%, 95% CI 12.0–87.0; p = 0.019) of patients with two AKAs had bilateral configuration.
Origin of the artery of Adamkiewicz
A total of 56 studies (n = 3316 patients with AKA) analyzed the side of origin of AKA. The results showed that 76.6% (95% CI 73.2–79.9) of AKAs originated from the left side, while 23.4% (95% CI 20.1–26.8; I2 78.5%, 95% CI 72.5–83.2; p < 0.001) from the right side. The analysis of 43 studies (n = 2834 patients with AKA) showed that 89% of arteries originated between T8 and L1 (Table 4). AKA most frequently originated at the level of T9 with PPE of 22.2% (95% CI 18.9–25.4), followed by T10 and T11 with PPE of 21.7% (95% CI 18.5–25.0) and 18.7% (95% CI 15.6–21.8), respectively.
Table 4.
Origin of AKA (vertebral levels)
| Number of studies (number of subjects with AKA) | T3: % (95% CI) | T4: % (95% CI) | T5: % (95% CI) | T6: % (95% CI) | T7: % (95% CI) | T8: % (95% CI) | T9: % (95% CI) | T10: % (95% CI) | T11: % (95% CI) | T12: % (95% CI) | L1: % (95% CI) | L2: % (95% CI) | L3: % (95% CI) | L4: % (95% CI) | L5: % (95% CI) | I2: % (95% CI) | Cochran’s Q, p value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 43 (2834) | 0.5 (0.1–1.3) | 0.7 (0.2–1.6) | 0.8 (0.2–1.7) | 0.8 (0.2–1.8) | 2.2 (1.2–3.5) | 7.3 (5.3–9.4) | 22.2 (18.9–25.4) | 21.7 (18.5–25.0) | 18.7 (15.6–21.8) | 12.2 (9.7–14.8) | 6.9 (5.0–9.0) | 3.8 (2.4–5.5) | 1.1 (0.4–2.1) | 0.5 (0.1–1.3) | 0.5 (0.1–1.2) | 74.7 (66.0–81.2) | < 0.001 |
Continuity of the artery of Adamkiewicz
A total of seven studies (n = 375 patients with AKAs) were included in an analysis of the continuity of the AKA from the aorta to the anterior spinal artery. The results showed that AKA continued from the aorta to the anterior spinal artery in 71.3% of patients (95% CI 45.8–91.6; I2 95.6%, 95% CI 92.8–97.2; p < 0.001).
Morphometric analysis of the artery of Adamkiewicz
Five studies (n = 324 patients with AKA) analyzed the morphometric data of the AKA. The analysis showed a pooled mean diameter of 1.09 mm (95% CI 0.69–1.50; I2 36.2%; p < 0.001).
Discussion
Because the AKA originates from the lumbar arteries, it may be prudent to preserve the blood flow from the lumbar arteries when a thoracoabdominal aortic repair is planned [5, 63]. Concomitant or previous abdominal aortic repair and extensive thoracic aorta exclusion by means of multiple stent grafts are associated with a significantly higher risk of paraplegia [64]. After the interruption of most of the intercostal and lumbar arteries, the residual collateral blood supply is marginal, and in some cases, the spinal cord may become extremely prone to injury due to arterial hypotension or low cardiac output from any cause [65]. During aortic repair, preservation, reattachment, or reconstruction of the intercostal or lumbar arteries can maintain the blood supply to the spinal cord [66, 67]. Depending on the number of intercostal or lumbar arteries that require reconstruction, the ischemic duration may be prolonged during reconstruction. In our study, in patients with an AKA present, 11.3% had two AKAs, with bilateral AKAs present in 26.7% of these patients. The preoperative identification of the AKA and its anatomical characteristics allows for superior surgical planning, such that the surgical time and postoperative spinal complication risk are decreased [31]. Therefore, AKA identification is of interest for surgeons aiming to reconstruct intercostal or lumbar arteries in order to prevent postoperative spinal ischemic complications [3].
With respect to the continuity between the radicular arteries (including the AKA) and the anterior spinal arteries, the AKA continued from the aorta to the anterior spinal artery in 71.3% of the patients in our study. When this continuity is present, blood may drain away from the spinal cord through the anterior spinal arteries and the radicular arteries, acting as stealing channels by rerouting the blood to be distal to an aortic obstruction [5]. During aortic cross-clamping, back-bleeding from the ostia of the posterior intercostal and lumbar arteries may be a clinical manifestation of such rerouting of blood when continuity between the AKA and the anterior spinal arteries is present. This steal phenomenon may further worsen spinal cord ischemia, causing irreversible neurological injuries if the ischemia time is longer than 20 to 30 min [68].
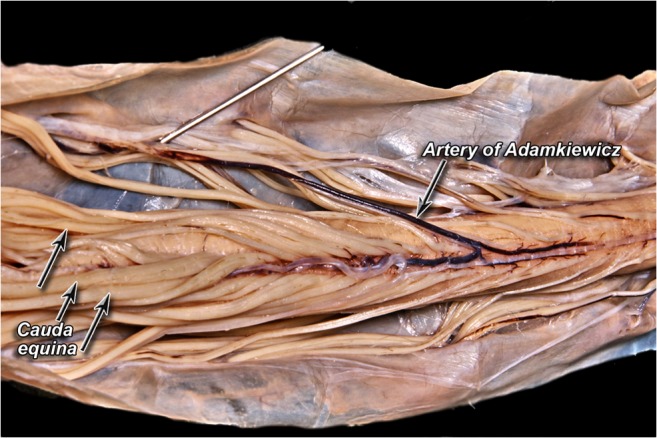
The detection of the AKA can be difficult because of the various possible levels of origins of the artery, its small size, the amount of time needed to obtain the angiogram, and complications that can occur during surgical procedures [14, 26]. In our study, the pooled mean diameter of the AKA was 1.09 mm. Various techniques have been devised to preoperatively identify the location and anatomy of the AKA, such as CTA [55], MRA [7], and DSA [9]. These techniques can be used to identify both the level and the laterality of the artery, which can affect a surgeon’s approach to an aneurysm or spinal lesion. We have included three DSA images with injected contrast into left radicular artery at the level of T4 (Fig. 5), T8 (Fig. 6), and T11 (Fig. 7). In our meta-analysis, cadaveric studies had the highest prevalence of an AKA (97.5%), and among the different imaging modalities, MRA and CTA had the highest prevalence rates (88.3% and 88.1%, respectively), while DSA had the lowest prevalence rate (75.4%). In spite of its apparent success in detecting an AKA, MRA has been shown to be inferior to DSA in terms of evaluating vessel continuity, sharpness, and background homogeneity [7]. Furthermore, compared with CTA, a more limited field of view is a major disadvantage of MRA [61]. As a result, MRA may fail to depict the clinically important collateral vessels to the AKA in some patients, when a collateral source is the internal thoracic artery or the thoracodorsal artery [69]. Despite DSA studies reporting a lower prevalence rate of the AKA than MRA and CTA in our meta-analysis, DSA remains the “gold standard” for identifying spinal cord vasculature as it is both safe and efficient [9]. A possible reason for this discrepancy could be the small number of patients included in our DSA analysis as compared to the number of patients included in our MRA and CTA analyses.
Fig. 5.
Digital subtraction angiography image of the artery of Adamkiewicz from left T4 radicular artery injection
Fig. 6.
Digital subtraction angiography image of the artery of Adamkiewicz from left T8 radicular artery injection
Fig. 7.
Digital subtraction angiography image of the artery of Adamkiewicz from left T11 radicular artery injection
Future studies should examine the blood supply and the collateral circulation of the spinal cord in the presence of degenerative atherosclerotic or dissecting aneurysm, or after a surgical or endovascular aortic procedure. In these patients, the disease and the surgical procedure may occlude several segmental arteries and promote collateral vessels enlargement, significantly altering the normal patterns of blood supply to the spinal cord [5].
Our meta-analysis was limited by the high amount of heterogeneity between the studies. However, the number of included studies and their large sample sizes mitigate this limitation. As cadaveric dissection is the gold standard for anatomical considerations, more cadaveric studies should assess prevalence of AKA, especially performed on subjects poorly represented in our meta-analysis, such as Africa, South America, and Oceania.
Because of the lower prevalence of AKA in radiological studies, surgeons should keep in mind that these results might be false negative. In this case, the risk of iatrogenic injury to the AKA during thoracolumbar surgical procedures is increased. More accurate imaging methods should be developed to assess the true prevalence of AKA.
To ensure spinal cord safety, preoperative AKA identification and its subsequent reconstruction or preservation are effective adjuncts for more secure protection of the spinal cord, along with other adequate management strategies.
Conclusions
Our main findings revealed that the AKA was found to be present in the vast majority of the general population (84.6%), most often as a single vessel (87.4%) originating between T8 and L1 (89%) on the left side (76.6%). Based on our anatomical findings, we recommend that efforts should be made to identify and subsequently reconstruct or preserve the AKA to prevent postoperative neurological deficit due to spinal cord ischemia in vascular and endovascular surgical procedures in the thoracolumbar spinal cord.
Electronic supplementary material
(DOC 64 kb)
Acknowledgements
KAT was supported by the Polish Ministry of Higher Education grant for young scientists.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of meta-analysis study formal consent is not required.
Informed consent
NA
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
DT and BS contributed equally to this work.
References
- 1.Sukeeyamanon W, Siriapisith T, Wasinrat J. Preoperative localization of Adamkiewicz arteries and their origins by using MDCT angiography. J Med Assoc Thail. 2010;93:1430–1436. [PubMed] [Google Scholar]
- 2.Ogino H, Sasaki H, Minatoya K, Matsuda H, Yamada N, Kitamura S. Combined use of Adamkiewicz artery demonstration and motor-evoked potentials in descending and thoracoabdominal repair. Ann Thorac Surg. 2006;82:592–596. doi: 10.1016/j.athoracsur.2006.03.041. [DOI] [PubMed] [Google Scholar]
- 3.Takagi H, Ota H, Natsuaki Y, Komori Y, Ito K, Saiki Y, Takase K. Identifying the Adamkiewicz artery using 3-T time-resolved magnetic resonance angiography: its role in addition to multidetector computed tomography angiography. Jpn J Radiol. 2015;33:749–756. doi: 10.1007/s11604-015-0490-6. [DOI] [PubMed] [Google Scholar]
- 4.Gailloud P. The artery of von Haller: a constant anterior radiculomedullary artery at the upper thoracic level. Neurosurgery. 2013;73:1034–1043. doi: 10.1227/NEU.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 5.Biglioli P, Roberto M, Cannata A, Parolari A, Fumero A, Grillo F, Maggioni M, Coggi G, Spirito R. Upper and lower spinal cord blood supply: the continuity of the anterior spinal artery and the relevance of the lumbar arteries. J Thorac Cardiovasc Surg. 2004;127:1188–1192. doi: 10.1016/j.jtcvs.2003.11.038. [DOI] [PubMed] [Google Scholar]
- 6.Koshino T, Murakami G, Morishita K, Mawatari T, Abe T. Does the Adamkiewicz artery originate from the larger segmental arteries? J Thorac Cardiovasc Surg. 1999;117:898–905. doi: 10.1016/S0022-5223(99)70369-7. [DOI] [PubMed] [Google Scholar]
- 7.Yamada N, Okita Y, Minatoya K, Tagusari O, Ando M, Takamiya M, Kitamura S. Preoperative demonstration of the Adamkiewicz artery by magnetic resonance angiography in patients with descending or thoracoabdominal aortic aneurysms. Eur J Cardiothorac Surg. 2000;18:104–111. doi: 10.1016/S1010-7940(00)00412-7. [DOI] [PubMed] [Google Scholar]
- 8.Yoshioka K, Niinuma H, Ohira A, Nasu K, Kawakami T, Sasaki M, Kawazoe K. MR angiography and CT angiography of the artery of Adamkiewicz: noninvasive preoperative assessment of thoracoabdominal aortic aneurysm. RadioGraphics. 2003;23:1215–1225. doi: 10.1148/rg.235025031. [DOI] [PubMed] [Google Scholar]
- 9.Fanous AA, Lipinski LJ, Krishna C, Roger EP, Siddiqui AH, Levy EI, Leonardo J, Pollina J. The impact of preoperative angiographic identification of the artery of Adamkiewicz on surgical decision making in patients undergoing thoracolumbar corpectomy. Spine (Phila Pa 1976) 2015;40:1194–1199. doi: 10.1097/BRS.0000000000000909. [DOI] [PubMed] [Google Scholar]
- 10.Nijenhuis RJ, Leiner T, Cornips EMJ, Wilmink JT, Jacobs MJ, van Engelshoven JMA, Backes WH. Spinal cord feeding arteries at MR angiography for thoracoscopic spinal surgery: feasibility study and implications for surgical approach. Radiology. 2004;233:541–547. doi: 10.1148/radiol.2331031672. [DOI] [PubMed] [Google Scholar]
- 11.Henry BM, Tomaszewski KA, Ramakrishnan PK, Roy J, Vikse J, Loukas M, Tubbs RS, Walocha JA. Development of the anatomical quality assessment (AQUA) tool for the quality assessment of anatomical studies included in meta-analyses and systematic reviews. Clin Anat. 2017;30:6–13. doi: 10.1002/ca.22799. [DOI] [PubMed] [Google Scholar]
- 12.Higgins J, Green S (eds) (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]
- 13.Henry BM, Tomaszewski KA, Walocha JA. Methods of evidence-based anatomy: a guide to conducting systematic reviews and meta-analysis of anatomical studies. Ann Anat. 2016;205:16–21. doi: 10.1016/j.aanat.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 14.Fereshetian A, Kadir S, Kaufman SL, Mitchell SE, Murray RR, Kinnison ML, Williams GM. Digital subtraction spinal cord angiography in patients undergoing thoracic aneurysm surgery. Cardiovasc Intervent Radiol. 1989;12:7–9. doi: 10.1007/BF02577117. [DOI] [PubMed] [Google Scholar]
- 15.Guziński M, Bryl M, Ziemińska K, Wolny K, Sąsiadek M, Garcarek J. Detection of the Adamkiewiczartery in computed tomography of the thorax and abdomen. Adv Clin Exp Med. 2017;26:31–37. doi: 10.17219/acem/62788. [DOI] [PubMed] [Google Scholar]
- 16.Alleyne CH, Cawley CM, Shengelaia GG, Barrow DL. Microsurgical anatomy of the artery of Adamkiewicz and its segmental artery. J Neurosurg. 1998;89:791–795. doi: 10.3171/jns.1998.89.5.0791. [DOI] [PubMed] [Google Scholar]
- 17.Amako M, Yamamoto Y, Nakamura K, et al. Preoperative visualization of the artery of Adamkiewicz by dual-phase CT angiography in patients with aortic aneurysm. Kurume Med J. 2011;58:117–125. doi: 10.2739/kurumemedj.58.117. [DOI] [PubMed] [Google Scholar]
- 18.Bachet J, Guilmet D, Rosier J, et al. Protection of the spinal cord during surgery of thoraco-abdominal aortic aneurysms. Eur J Cardiothorac Surg. 1996;10:817–825. doi: 10.1016/S1010-7940(96)80305-8. [DOI] [PubMed] [Google Scholar]
- 19.Backes WH, Nijenhuis RJ, Mess WH, Wilmink FA, Schurink GWH, Jacobs MJ. Magnetic resonance angiography of collateral blood supply to spinal cord in thoracic and thoracoabdominal aortic aneurysm patients. J Vasc Surg. 2008;48:261–271. doi: 10.1016/j.jvs.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 20.Bley TA, Duffek CC, François CJ, Schiebler ML, Acher CW, Mell M, Grist TM, Reeder SB. Presurgical localization of the artery of Adamkiewicz with time-resolved 3.0-T MR angiography. Radiology. 2010;255:873–881. doi: 10.1148/radiol.10091304. [DOI] [PubMed] [Google Scholar]
- 21.Boll DT, Bulow H, Blackham KA, Aschoff AJ, Schmitz BL. MDCT angiography of the spinal vasculature and the artery of Adamkiewicz. AJR Am J Roentgenol. 2006;187:1054–1060. doi: 10.2214/AJR.05.0562. [DOI] [PubMed] [Google Scholar]
- 22.Bowen BC, DePrima S, Pattany PM, Marcillo A, Madsen P, Quencer RM. MR angiography of normal intradural vessels of the thoracolumbar spine. AJNR Am J Neuroradiol. 1996;17:483–494. [PMC free article] [PubMed] [Google Scholar]
- 23.Champlin AM, Rael J, Benzel EC, Kesterson L, King JN, Orrison WW, Mirfakhraee M. Preoperative spinal angiography for lateral extracavitary approach to thoracic and lumbar spine. AJNR Am J Neuroradiol. 1994;15:73–77. [PMC free article] [PubMed] [Google Scholar]
- 24.Charles YP, Barbe B, Beaujeux R, Boujan F, Steib JP. Relevance of the anatomical location of the Adamkiewicz artery in spine surgery. Surg Radiol Anat. 2011;33:3–9. doi: 10.1007/s00276-010-0654-0. [DOI] [PubMed] [Google Scholar]
- 25.Furukawa K, Kamohara K, Nojiri J, Egashira Y, Okazaki Y, Kudo S, Morita S. Operative strategy for descending and thoracoabdominal aneurysm repair with preoperative demonstration of the Adamkiewicz artery. Ann Thorac Surg. 2010;90:1840–1846. doi: 10.1016/j.athoracsur.2010.07.056. [DOI] [PubMed] [Google Scholar]
- 26.Heinemann MK, Brassel F, Herzog T, et al. The role of spinal angiography in operations on the thoracic aorta: myth or reality? Ann Thorac Surg. 1998;65:346–351. doi: 10.1016/S0003-4975(97)01239-3. [DOI] [PubMed] [Google Scholar]
- 27.Hyodoh H, Kawaharada N, Akiba H, Tamakawa M, Hyodoh K, Fukada J, Morishita K, Hareyama M. Usefulness of preoperative detection of artery of Adamkiewicz with dynamic contrast-enhanced MR angiography. Radiology. 2005;236:1004–1009. doi: 10.1148/radiol.2363040911. [DOI] [PubMed] [Google Scholar]
- 28.Hyodoh H, Shirase R, Akiba H, Tamakawa M, Hyodoh K, Yama N, Shonai T, Hareyama M. Double-subtraction maximum intensity projection MR angiography for detecting the artery of Adamkiewicz and differentiating it from the drainage vein. J Magn Reson Imaging. 2007;26:359–365. doi: 10.1002/jmri.21024. [DOI] [PubMed] [Google Scholar]
- 29.Hyodoh H, Shirase R, Kawaharada N, et al. MR angiography for detecting the artery of Adamkiewicz and its branching level from the aorta. Magn Reson Med Sci. 2009;8:159–164. doi: 10.2463/mrms.8.159. [DOI] [PubMed] [Google Scholar]
- 30.Jaspers K, Nijenhuis RJ, Backes WH. Differentiation of spinal cord arteries and veins by time-resolved MR angiography. J Magn Reson Imaging. 2007;26:31–40. doi: 10.1002/jmri.20940. [DOI] [PubMed] [Google Scholar]
- 31.Kawaharada N, Morishita K, Fukada J, Yamada A, Muraki S, Hyodoh H, Abe T. Thoracoabdominal or descending aortic aneurysm repair after preoperative demonstration of the Adamkiewicz artery by magnetic resonance angiography. Eur J Cardiothorac Surg. 2002;21:970–974. doi: 10.1016/S1010-7940(02)00097-0. [DOI] [PubMed] [Google Scholar]
- 32.Hachiro Y, Kawaharada N, Morishita K, Fukada J, Fujisawa Y, Kurimoto Y, Abe T. Thoracoabdominal aortic aneurysm repair after detection of the Adamkiewicz artery by magnetic resonance angiography; a way to shorten operating time and improve outcome. Kyobu Geka. 2004;57:280–283. [PubMed] [Google Scholar]
- 33.Kawaharada N, Morishita K, Kurimoto Y, et al. Spinal cord ischemia after elective endovascular stent-graft repair of the thoracic aorta. Eur J Cardiothorac Surg. 2007;31:998–1003. doi: 10.1016/j.ejcts.2007.01.069. [DOI] [PubMed] [Google Scholar]
- 34.Kieffer E, Richard T, Chiras J, Godet G, Cormier E. Preoperative spinal cord arteriography in aneurysmal disease of the descending thoracic and thoracoabdominal aorta: preliminary results in 45 patients. Ann Vasc Surg. 1989;3:34–46. doi: 10.1016/S0890-5096(06)62382-0. [DOI] [PubMed] [Google Scholar]
- 35.Kieffer E, Fukui S, Chiras J, Koskas F, Bahnini A, Cormier E. Spinal cord arteriography: a safe adjunct before descending thoracic or thoracoabdominal aortic aneurysmectomy. J Vasc Surg. 2002;35:262–268. doi: 10.1067/mva.2002.120378. [DOI] [PubMed] [Google Scholar]
- 36.Kovács A, Schiller W, Gerhards HM, Welz A, Willinek W, Schild H, Urbach H, Flacke S. Visualization of the Adamkiewicz artery in patients with acute Stanford A dissections: a prospective 64-row multi-detector CT study. Rofo. 2009;181:870–874. doi: 10.1055/s-0028-1109441. [DOI] [PubMed] [Google Scholar]
- 37.Kroszczynski AC, Kohan K, Kurowski M, Olson TR, Downie SA. Intraforaminal location of thoracolumbar anterior medullary arteries. Pain Med. 2013;14:808–812. doi: 10.1111/pme.12056. [DOI] [PubMed] [Google Scholar]
- 38.Kudo K, Terae S, Asano T, Oka M, Kaneko K, Ushikoshi S, Miyasaka K. Anterior spinal artery and artery of Adamkiewicz detected by using multi-detector row CT. AJNR Am J Neuroradiol. 2003;24:13–17. [PMC free article] [PubMed] [Google Scholar]
- 39.Matsuda H, Fukuda T, Iritani O, Nakazawa T, Tanaka H, Sasaki H, Minatoya K, Ogino H. Spinal cord injury is not negligible after TEVAR for lower descending aorta. Eur J Vasc Endovasc Surg. 2010;39:179–186. doi: 10.1016/j.ejvs.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 40.Matsuda H, Ogino H, Fukuda T, Iritani O, Sato S, Iba Y, Tanaka H, Sasaki H, Minatoya K, Kobayashi J, Yagihara T. Multidisciplinary approach to prevent spinal cord ischemia after thoracic endovascular aneurysm repair for distal descending aorta. Ann Thorac Surg. 2010;90:561–565. doi: 10.1016/j.athoracsur.2010.04.067. [DOI] [PubMed] [Google Scholar]
- 41.Melissano G, Bertoglio L, Civelli V, Moraes Amato AC, Coppi G, Civilini E, Calori G, de Cobelli F, del Maschio A, Chiesa R. Demonstration of the Adamkiewicz artery by multidetector computed tomography angiography analysed with the open-source software OsiriX. Eur J Vasc Endovasc Surg. 2009;37:395–400. doi: 10.1016/j.ejvs.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 42.Mordasini P, El-Koussy M, Schmidli J, et al. Preoperative mapping of arterial spinal supply using 3.0-T MR angiography with an intravasal contrast medium and high-spatial-resolution steady-state. Eur J Radiol. 2012;81:979–984. doi: 10.1016/j.ejrad.2011.02.025. [DOI] [PubMed] [Google Scholar]
- 43.Morishita K, Murakami G, Fujisawa Y, Kawaharada N, Fukada J, Saito T, Abe T. Anatomical study of blood supply to the spinal cord. Ann Thorac Surg. 2003;76:1967–1971. doi: 10.1016/S0003-4975(03)01254-2. [DOI] [PubMed] [Google Scholar]
- 44.Murthy NS, Maus TP, Behrns CL. Intraforaminal location of the great anterior radiculomedullary artery (artery of Adamkiewicz): a retrospective review. Pain Med. 2010;11:1756–1764. doi: 10.1111/j.1526-4637.2010.00948.x. [DOI] [PubMed] [Google Scholar]
- 45.Nakayama Y, Awai K, Yanaga Y, Nakaura T, Funama Y, Hirai T, Yamashita Y. Optimal contrast medium injection protocols for the depiction of the Adamkiewicz artery using 64-detector CT angiography. Clin Radiol. 2008;63:880–887. doi: 10.1016/j.crad.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 46.Nijenhuis RJ, Jacobs MJ, Schurink GW, Kessels AGH, van Engelshoven JMA, Backes WH. Magnetic resonance angiography and neuromonitoring to assess spinal cord blood supply in thoracic and thoracoabdominal aortic aneurysm surgery. J Vasc Surg. 2007;45:71–77. doi: 10.1016/j.jvs.2006.08.085. [DOI] [PubMed] [Google Scholar]
- 47.Nijenhuis RJ, Jacobs MJ, Jaspers K, Reijnders M, van Engelshoven JMA, Leiner T, Backes WH. Comparison of magnetic resonance with computed tomography angiography for preoperative localization of the Adamkiewicz artery in thoracoabdominal aortic aneurysm patients. J Vasc Surg. 2007;45:677–685. doi: 10.1016/j.jvs.2006.11.046. [DOI] [PubMed] [Google Scholar]
- 48.Nishida J, Kitagawa K, Nagata M, Yamazaki A, Nagasawa N, Sakuma H. Model-based iterative reconstruction for multi-detector row CT assessment of the Adamkiewicz artery. Radiology. 2014;270:282–291. doi: 10.1148/radiol.13122019. [DOI] [PubMed] [Google Scholar]
- 49.Nishii T, Kono AK, Negi N, Hashimura H, Uotani K, Okita Y, Sugimura K. The feasibility of a 64-slice MDCT for detection of the Adamkiewicz artery: comparison of the detection rate of intravenous injection CT angiography using a 64-slice MDCT versus intra-arterial and intravenous injection CT angiography using a 16-slice MDCT. Int J Cardiovasc Imaging. 2013;29(Suppl 2):127–133. doi: 10.1007/s10554-013-0301-z. [DOI] [PubMed] [Google Scholar]
- 50.Nojiri J, Matsumoto K, Kato A, Miho T, Furukawa K, Ohtsubo S, Itoh T, Kudo S. The Adamkiewicz artery: demonstration by intra-arterial computed tomographic angiography. Eur J Cardiothorac Surg. 2007;31:249–255. doi: 10.1016/j.ejcts.2006.11.024. [DOI] [PubMed] [Google Scholar]
- 51.Ou P, Schmit P, Layouss W, Sidi D, Bonnet D, Brunelle F. CT angiography of the artery of Adamkiewicz with 64-section technology: first experience in children. AJNR Am J Neuroradiol. 2007;28:216–219. [PMC free article] [PubMed] [Google Scholar]
- 52.Polaczek M, Maslanka M, Skadorwa T, Ciszek B. How does Adamkiewicz artery influence blood supply to the fetal spinal cord? Ital J Anat Embryol. 2014;119:255–262. [PubMed] [Google Scholar]
- 53.Rodriguez-Baeza A, Muset-Lara A, Rodriguez-Pazos M, Domenech-Mateu JM. The arterial supply of the human spinal cord: a new approach to the arteria radicularis magna of Adamkiewicz. Acta Neurochir. 1991;109:57–62. doi: 10.1007/BF01405699. [DOI] [PubMed] [Google Scholar]
- 54.Schurink GWH, Nijenhuis RJ, Backes WH, Mess W, de Haan MW, Mochtar B, Jacobs MJ. Assessment of spinal cord circulation and function in endovascular treatment of thoracic aortic aneurysms. Ann Thorac Surg. 2007;83:S877–S881. doi: 10.1016/j.athoracsur.2006.11.028. [DOI] [PubMed] [Google Scholar]
- 55.Takase K, Sawamura Y, Igarashi K, Chiba Y, Haga K, Saito H, Takahashi S. Demonstration of the artery of Adamkiewicz at multi- detector row helical CT. Radiology. 2002;223:39–45. doi: 10.1148/radiol.2231010513. [DOI] [PubMed] [Google Scholar]
- 56.Takase K, Akasaka J, Sawamura Y. Preoperative MDCT evaluation of the artery of Adamkiewicz and its origin. J Vasc Surg. 2007;45:1086. doi: 10.1016/j.jvs.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 57.Tanaka H, Ogino H, Minatoya K, Matsui Y, Higami T, Okabayashi H, Saiki Y, Aomi S, Shiiya N, Sawa Y, Okita Y, Sueda T, Akashi H, Kuniyoshi Y, Katsumata T. The impact of preoperative identification of the Adamkiewicz artery on descending and thoracoabdominal aortic repair. J Thorac Cardiovasc Surg. 2016;151:122–128. doi: 10.1016/j.jtcvs.2015.07.079. [DOI] [PubMed] [Google Scholar]
- 58.Uotani K, Yamada N, Kono AK, Taniguchi T, Sugimoto K, Fujii M, Kitagawa A, Okita Y, Naito H, Sugimura K. Preoperative visualization of the artery of Adamkiewicz by intra-arterial CT angiography. AJNR Am J Neuroradiol. 2008;29:314–318. doi: 10.3174/ajnr.A0812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Williams GM, Perler BA, Burdick JF, Osterman FA, Jr, Mitchell S, Merine D, Drenger B, Parker SD, Beattie C, Reitz BA. Angiographic localization of spinal cord blood supply and its relationship to postoperative paraplegia. J Vasc Surg. 1991;13:23–33. doi: 10.1016/0741-5214(91)90009-J. [DOI] [PubMed] [Google Scholar]
- 60.Yingbin J, Jiefei M, Jian L, Yonghui S, Haiyan P, Baimeng Z, Weigoo F. Evaluation of the thoracic aortic dissection treated by endografts covering a longer distance of aorta according to the location of the Adamkiewicz artery. Thorac Cardiovasc Surg. 2013;61:569–574. doi: 10.1055/s-0032-1322629. [DOI] [PubMed] [Google Scholar]
- 61.Yoshioka K, Niinuma H, Ehara S, Nakajima T, Nakamura M, Kawazoe K. MR angiography and CT angiography of the artery of Adamkiewicz: state of the art. Radiographics. 2006;26(Suppl 1):S63–S73. doi: 10.1148/rg.26si065506. [DOI] [PubMed] [Google Scholar]
- 62.Zhao S, Logan L, Schraedley P, Rubin GD. Assessment of the anterior spinal artery and the artery of Adamkiewicz using multi-detector CT angiography. Chin Med J. 2009;122:145–149. [PubMed] [Google Scholar]
- 63.Griepp RB, Ergin MA, Galla JD, Lansman S, Khan N, Quintana C, McCollough J, Bodian C. Looking for the artery of Adamkiewicz: a quest to minimize paraplegia after operations for aneurysms of the descending thoracic and thoracoabdominal aorta. J Thorac Cardiovasc Surg. 1996;112:1202–1213. doi: 10.1016/S0022-5223(96)70133-2. [DOI] [PubMed] [Google Scholar]
- 64.Buffolo E, da Fonseca JHP, de Souza JAM, Alves CMR. Revolutionary treatment of aneurysms and dissections of descending aorta: the endovascular approach. Ann Thorac Surg. 2002;74:S1815–S1817. doi: 10.1016/S0003-4975(02)04138-3. [DOI] [PubMed] [Google Scholar]
- 65.Ishimaru S, Kawaguchi S, Koizumi N, Obitsu Y, Ishikawa M. Preliminary report on prediction of spinal cord ischemia in endovascular stent graft repair of thoracic aortic aneurysm by retrievable stent graft. J Thorac Cardiovasc Surg. 1998;115:811–818. doi: 10.1016/S0022-5223(98)70360-5. [DOI] [PubMed] [Google Scholar]
- 66.Safi HJ, Miller CC, Carr C, Iliopoulos DC, Dorsay DA, Baldwin JC. Importance of intercostal artery reattachment during thoracoabdominal aortic aneurysm repair. J Vasc Surg. 1998;27:58–66. doi: 10.1016/S0741-5214(98)70292-7. [DOI] [PubMed] [Google Scholar]
- 67.Wadouh F, Wadouh R, Hartmann M, Crisp-Lindgren N. Prevention of paraplegia during aortic operations. Ann Thorac Surg. 1990;50:543–552. doi: 10.1016/0003-4975(90)90187-B. [DOI] [PubMed] [Google Scholar]
- 68.Taira Y, Marsala M. Effect of proximal arterial perfusion pressure on function, spinal cord blood flow, and histopathologic changes after increasing intervals of aortic occlusion in the rat. Stroke. 1996;27:1850–1858. doi: 10.1161/01.STR.27.10.1850. [DOI] [PubMed] [Google Scholar]
- 69.Yoshioka K, Niinuma H, Kawazoe K, Ehara S. Three-dimensional demonstration of the collateral circulation to the artery of Adamkiewicz via internal thoracic artery with 16-row multi-slice CT. Eur J Cardiothorac Surg. 2005;28:492. doi: 10.1016/j.ejcts.2005.04.043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 64 kb)