Abstract
Background:
Primary dysmenorrhea is the most common complaint of women. Imbalance secretion of prostaglandin from the endometrium during menstruation cycle is effective in primary dysmenorrhea and menstrual bleeding. The aim of this study was to compare rosemary capsule and mefenamic acid on menstrual bleeding and primary dysmenorrhea.
Materials and Methods:
This randomized double-blinded study was conducted on 82 students with primary dysmenorrhea in the Islamic Azad University of Mashhad in 2016. Participants had moderate dysmenorrhea and normal menstrual bleeding. No intervention was carried out at the two cycles. During the next two cycles, participants were randomly divided into two groups (rosemary and mefenamic acid(. Participants in the intervention group received 250 mg rosemary capsules and the control group received 250 mg mefenamic acid capsules in the first 3 days of menstruation. The visual analogue scale (VAS) was used to determine the severity of pain and Hingham chart to determine the amount of bleeding in menstruation. Independent t-tests, Mann--Whitney were used for statistical analysis. p < 0.05 was considered statistically significant.
Results:
Pain intensity score standard deviation (SD) before and after intervention for rosemary group were 40.39 (11.41) and 23.57 (12.78) (t41 = 9.90, p < 0.001). For the control group, they were 46.75 (13.32) and 28.29 (17.21) (t39 = 9.10, p < 0.001). Menstrual bleeding score (SD) before and after intervention for rosemary group were 55.21 (21.32) and 46.30 (24.16) (t41 = 2.60, p = 0.01). For the control group, they were 51.05 (23.87) and 43.43 (29.47) (t39 = 2.10, p = 0.01). There was no statistically significant difference between the pain severity and menstrual bleeding score SD in these two groups.
Conclusions:
Rosemary capsules reduce the menstrual bleeding and primary dysmenorrhea the same as mefenamic acid capsules.
Keywords: Dysmenorrhea, mefenamic acid, menstruation, rosmarinus
Introduction
Dysmenorrhea is divided into two types: primary and secondary. Primary dysmenorrhea is described as painful menses in women with normal pelvic anatomy without any pathology.[1] These conditions come into existence at the time of first menstruation or shortly thereafter and last for 48--72 h.[2,3] Mood changes, fatigue, headache, nausea, and edema during menstruation are reported with dysmenorrhea. Negative consequences of dysmenorrhoea may include impaired quality of personal and social life, mood disorders, sleep disturbance, and limitation of usual daily activities. In the entire world, from 2010 to 2015, the prevalence of dysmenorrhea varied greatly from 94% (Oman), 59.80% (Bangladesh), 34% (Egypt), and to 0.90% (Korea).[4] Kharaghani and Damghanian in a systematic review study indicated that the total prevalence of primary dysmenorrhea in Iranian women was estimated to be 71%.[5] Primary dysmenorrhea is resulting from excess or imbalance secretion of prostaglandin from the endometrium during menstruation cycle. In women whose prostaglandin concentrations reach their highest level, most severe menstrual pain is experienced.[6]
The amount of bleeding also affects the synthesis of endometrial prostaglandins so that at the end of the secretory phase and until the first 48 h of menstruation cycle, the prostaglandin E2 and prostacyclin, which causes vasodilation and prevents topical accumulation platelets, increases in the uterus, while prostaglandin F2α, which causes vascular contraction, decreases.[7,8,9] Menstrual bleeding refers to the average loss of blood in a normal menstrual cycle.[10] The normal cycle of menstrual bleeding is 4--6 days, and the normal volume of menstrual bleeding is 30 ml.[11]
Various types of treatments have been recommended for the treatment of dysmenorrhea, including antiprostaglandin synthases, oral contraceptives, and a kind of narcotic drugs.[12] Today, due to the effects of chemical drugs, the high economic cost of importing raw materials, and lack of desire of young girls to use hormonal drugs to reduce pain, use of medicinal plants is a step toward self-sufficiency and has attracted the attention of researchers.[13] In the study of Davari et al. (2014), aromatherapy effect of rosemary and lavender on primary dysmenorrhea indicates that the rosemary and lavender and their combination reduce both the severity and duration of pain but there are not many clinical studies about these plants.[14] In the study of Jafarnejad et al. (2014), it was indicated that the use of Nigella sativa can increase the amount of menstrual bleeding, but this increase was not significantly different from mefenamic acid.[15]
Rosemary (Rosmarinus officials L.) from Lamiaceae family is an evergreen plant and is aromatic.[16] Rosemary aerial parts can be prepared the ethanol and aqueous extract.[17] In the study of Mengoni et al. (2011), which was done in vivo, it was indicated that the amount of Carnosic Acid (CA) and Carnosol (CS) in ethanol extract is higher than the aqueous extract. The ethanol extract of this plant has been able to reduce inflammation of the ear and foot of the mice.[18] Rosemary extract can reduce the production of prostaglandins by reducing the IL β, TNF-α (tumor necrosis factor α), and cyclooxygenase-2.[19] Inhibitors of Cyclooxygenase-2 (cox2) enzyme can reduce the production of prostaglandin which causes vasodilation and prevents the topical accumulation of platelets.[11] The recommended amount of rosemary based on antispasmodic effect is 3--5 g/day and no complication is observed from the use of the recommended amount.[17] Therefore, according to the antiprostaglandin properties of rosemary alcoholic extract, this study was conducted to compare the effect of rosemary and mefenamic acid capsules on menstrual bleeding and primary dysmenorrhea.
Materials and Methods
This study was a randomized clinical trial (IRCT2016062228586N1). A double-blind technique was used that neither the participants nor the researchers knew which participants belonged to the control group and which to the test group.
The sample size (n = 90) was calculated using different proportions method with confidence interval 95%, and s test's power of 80%, effect size 60%. This study was carried out on 82 female students of Mashhad Medical School in 2016, with primary dysmenorrheal assayed by VAS method.
The inclusion criteria consisted of being 18-25 years old, being single, having regular menstrual periods (a menstruation duration of 3--8 days with a 21-35 day interval between two menstrual cycles), obtaining a moderate pain intensity score of 40--70 according to VAS (0-100), having the score of menstrual bleeding according to Hingham chart less than 100.
The exclusion criteria consisted of having genital disease, coagulation disorders, using Oral Contraceptive Pills (OCP), using less than 6 doses of considered drugs in any types of intervention cycle.
Data collection tool consisted of three parts: the first part was demographic information. The second part was VAS for pain, in which the pain intensity was measured with a 100 VAS. Severity of pain was classified as: 0-40 mm as mild, 40-70 mm as moderate, and 80--100 mm as severe.[20] Due to the validity of VAS, there is no need for revalidation of this tool in determining the severity of pain. Phumdoung in his study in Thailand calculated the reliability coefficient of the instrument to measure pain intensity as 0.95.[21] To determine the reliability of this instrument, the test-retest method was used (r = 0.86). The third part was Higham Chart, which was Pictorial Blood Assessment Chart (PBAC). If the blood spots on the pad were light or less than 50%, score 1 would be given, in the case that the blood spots were medium and 50% of a pad was contaminated, score 5 would be given, and if it was completely stained with blood or more than 50% of the pad was contaminated, score 20 would be given. If there was also a small clot, score 1, and if there was a large, score 5 could be given, and at the end of the examination, the forms would be handed to the researcher. Participants’ bleeding was assessed by the researcher. Scores of 100 or over indicated abnormal bleeding, while the scores less than 100 indicated normal bleeding for women. It is the best tool available for the assessment of menstrual blood loss with 86% sensitivity and 89% accuracy.[22] Since Higham chart is valid, there was no need for its retest validity To determine the reliability, test--retest was used with 10 days intervals on 48 subjects (r = 0.75).
One kg of aerial parts of cultivated rosemary was collected from a garden in Shandiz region, Razavi Khorasan Province, northeast of Iran. The plant was identified by Mrs. M. Souzani from herbarium of School of Pharmacy, Mashhad University of Medical Sciences, Iran, where voucher specimen was deposited (No. 13209). From 1 kg of rosemary leaves, 220 g of alcoholic extract was obtained in the same capsules of mefenamic acid as 220 mg of rosemary extract and 30 g of glucose.
After controlling the two cycles, participants were randomly divided into two groups of A and B, according to the form numbers, using the PASS software. Participants in the mefenamic acid group received 250 mg capsules from the onset of the menstrual period, every 8 h, for 2 cycles. The rosemary group received 250 mg capsules from the onset of the menstrual period, every 8 h, for 2 cycles. Participants of both groups were asked to record the intensity of pain and amount of bleeding during menstruation.
Data analysis was performed by SPSS software (version 24, IBM SPSS Statistics), and the tests’ results were examined using independent t-test, paired t-test, covariance, and Mann--Whitney tests were examined. The significance level was considered as p < 0.05.
Ethical considerations
A written informed consent was obtained from all participants prior to the research. In addition, the subjects were ensured of the confidentiality terms regarding their personal information. Furthermore, they were allowed to withdraw from the research at any time. The research was confirmed by the Ethics Committee of Mashhad University of Medical Sciences (code IR.MUMS.REC.1395.162 on 20/06/2016).
Results
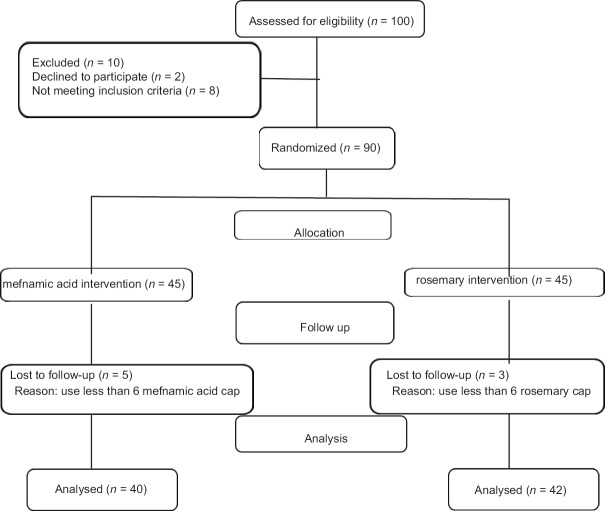
A total of 82 female students aged 18-25 years who complained about primary dysmenorrhea were contacted [Figure 1]. Demographic characteristics of research groups are presented in Table 1. As specified in the table, the subjects of the study groups were similar in age, number of days of menstruation, age at first menstruation and dysmenorrhea, and the differences in menstrual bleeding intervals were not statistically significant.
Figure 1.
The process of the study
Table 1.
Comparison of individual characteristics and menstrual status in the studied groups
| Variable (unit) | Rosemary middle (Mid-range) n=42 |
Mefenamic acid middle (Mid-range) n=40 |
Mann-Whitney Test |
p |
|---|---|---|---|---|
| Age (year) | 22 (2.25) | 22 (3) | 1.81 | 0.07 |
| Menarche age (year) | 13 (2) | 13 (2) | 0.35 | 0.72 |
| Dysmenorrhea age (year) | 15 (3.25) | 15 (2.75) | 1.08 | 0.27 |
| Interval of menstrual cycle (day) | 28 (2.50) | 28 (2) | 1.74 | 0.82 |
| Menstruation cycle duration (day) | 7 (1) | 7 (2) | 0.51 | 0.60 |
The means and standard deviations of the pain intensity score before and after intervention are presented in Table 2. As shown in Table 2, results of the independent t-test revealed a significant difference in the pain intensity score between groups before intervention. To control the heterogeneous of the pain intensity score, a covariance analysis was conducted in which the results did not indicate significant statistical differences (p = 0.70). The mean scores for pain intensity after the intervention was lower than before in both groups. Results of the independent paired t-test revealed a significant difference in the pain intensity score between rosemary (t41 = 9.90, p < 0.001) and mefnamic acid (t39 = 9.10, p < 0.001) groups.
Table 2.
The Mean and standard deviation of pain intensity based on visual Analog scale instrument in two groups
| Intensity of pain (mm) | Rosemary group Mean (SD) n=42 |
Mefenamic acid group Mean (SD) n=40 |
Independent t-test |
df | p |
|---|---|---|---|---|---|
| Mean pain intensity In two cycles before intervention | 40.39 (11.41) | 46.75 (13.32) | 2.32 | 80 | 0.02 |
| Mean pain intensity Two cycles of after intervention | 23.57 (12.78) | 28.29 (17.21) | 1.40 | 80 | 0.16 |
| Paired t-test result | p<0.001 t=9.90 | p<0.001 t=9.10 |
The means and standard deviations of the amount of menstrual bleeding before and after the intervention are presented in Table 3. As shown in Table 3, the mean scores for amount of menstrual bleeding after the intervention were lower than before in both groups. Results of the independent paired t-test revealed a significant difference in amount of menstrual bleeding between rosemary (t41 = 2.60, p = 0.01) and mefnamic acid groups (t39 = 2.10, p = 0.01). Also, the participants did not report any side effects caused by using the drugs.
Table 3.
The mean and standard deviation of the amount of menstrual bleeding according Hingham chart in two groups
| The amount of bleeding (mark) | Rosemary mean (SD) n=42 |
Mefenamic acid mean (SD) n=40 |
Independent t-test |
df | p |
|---|---|---|---|---|---|
| Mean menstrual bleeding In two cycles before intervention | 55.21 (21.32) | 51.05 (23.87) | 0.83 | 80 | 0.40 |
| Mean menstrual bleeding In two cycles after intervention | 46.30 (24.16) | 43.43 (29.47) | 0.48 | 80 | 0.63 |
| Paired t-test result | t=2.60,P=0.01 | t=2.10,P=0.01 |
Discussion
The results of the present study indicated that the mean pain intensity in rosemary and mefenamic acid groups was decreased, in which there was not significant differences between the two groups. Mengoni et al. (2011) indicated that the ethanol extract of rosemary includes bioactive compounds (CA) and (CS) which have anti-inflammatory activity, and both compounds selectively inhibited COX-2 but not COX-1. Prostaglandins are produced by cyclooxygenase and lipoxygenase from arachidonic acid.[18] One of the mechanisms behind creating dysmenorrhea is prostaglandins production in endometrium, which stimulates myometrium contractions.[11] In the menstruation blood of women suffering from dysmenorrhea, the concentrations of prostaglandin F2a and E2 are higher. Nonsteroidal anti-inflammatory drugs such as mefenamic acid inhibit prostaglandins synthesis through inhibition of cyclooxygenase activity.[23] Furthermore, rosemary ethanol extract has relieving and anti-inflammatory effects, and can be used for treating smooth muscle disorders. So it may be effective on pain relief in dysmenorrhea.
The results of the present study indicated that the mean amount of menstrual bleeding in rosemary and mefenamic acid groups was decreased, in which there was no significant difference between the two groups. Sinkovik et al. (2011) indicated that oral rosemary extract supplementation with the active substances including CS, CA, and rosemarinic acid resulted in a significant decrease in mean serum plasminogen--activator--inhibitor-1 (PAI-1) activity, a significant improvement of endothelial dysfunction but they did not report the significant reduction in platelet counts which affects menstrual discontinuation.[24] The mechanism which controls menstrual bleeding is vague but the recent studies indicate that imbalance secretion of prostaglandins is effective in abnormal menstrual bleeding; therefore, antiprostaglandin synthesis drugs can be effective in reducing menstrual bleeding.[25] Platelet plug is established during vessel wall injury and limit the hemorrhage.[11] Therefore, since the rosemary plant does not have any effects on the platelet counts, it also does not increase the amount of menstrual bleeding.
The amount of bleeding in rosemary group in comparison with the mefenamic acid group has more reduction but between these two groups, there is no significant statistical difference. The results of Karimian et al. (2011) indicated that the reduction in the amount of bleeding in people who took chamomile (Matricaria chamomilla) capsule was higher than people who took mefenamic acid, but between these two groups, there were no significant statistical difference.[26] The mechanism of the reduction in menstrual bleeding caused by chamomile is due to the anti-inflammatory activity. The most important strength of this study was using rosemary for the first time in Iran which led to the evaluation of dysmenorrhea severity and amount of bleeding in menstruation. For the researcher, the possibility of evaluation of participants by methods such as transvaginal sonography, laparoscopy, smear and culture of cervical discharges, pelvic examination were not available (due to the fact that the units were unmarried) for rejection of secondary dysmenorrhea, but it remained under control by a 2-month monitoring and recording the symptoms to differentiate the primary and secondary dysmenorrhea. Controlling some factors affecting the pain intensity such as mental characteristics and personality differences are difficult, but it was partially handled using random assignment.
Moreover, the threshold of pain tolerance is not the same in people, which was of the absolute limitations of the study.
Conclusion
Rosemary capsule reduce the amount of menstrual bleeding and dysmenorrhea the same as mefenamic acid. As a result, rosemary can be a substitute drug for mefenamic acid as a drug with fewer side effects.
Financial support and sponsorship
Mashhad University of Medical Sciences
Conflicts of interest
Nothing to declare.
Acknowledgement
This is a part of the midwifery Master's thesis which was approved by the research assistance in Mashhad University of Medical Science with code number 941793. The authors would like to express their appreciation to the students who participated in this study.
References
- 1.Jalambadani Z, Shojaeezadeh D, Hosseini M, Sadeghi R. Effect of relaxation education, based on theory of planned behavior on students’ painful dismenorrhea. J Birjand Univ Med Sci. 2015;22:238–47. [Google Scholar]
- 2.Berek J. Berek and Novak's Gynecology. 15th ed. Tehran: Golban; 2012. pp. 459–62. [Google Scholar]
- 3.Charandabi SM, Nashtaei MS, Kamali S, Majlesi R. The effect of acupressure at the Sanyinjiao point (SP6) on primary dysmenorrhea in students resident in dormitories of Tabriz. Iran J Nurs Midwifery Res. 2011;16:309–17. [PMC free article] [PubMed] [Google Scholar]
- 4.De Sanctis V, Soliman AT, Elsedfy H, Soliman NA, Soliman R, El Kholy M. Dysmenorrhea in adolescents and young adults: A review in different country. Acta Bio Medica Atenei Parmensis. 2016;87:233–46. [PMC free article] [PubMed] [Google Scholar]
- 5.Kharaghani R, Damghanian M. The prevalence of dysmenorrhea in Iran: A systematic review and meta-analysis. Irani Red Crescent Med J. 2017;19:e40856. [Google Scholar]
- 6.Bakhtshirin F, Abedi S, YusefiZoj P, Razmjooee D. The effect of aromatherapy massage with lavender oil on severity of primary dysmenorrhea in Arsanjan students. Iran J Nurs Midwifery Res. 2015;20:156–60. [PMC free article] [PubMed] [Google Scholar]
- 7.Farahmand M, Zahedi Asl S, Abbaspur Z, AbdolRahman R. Effects of vitamin E and Ibuprofen on amount, duration and interval of bleeding in patients with primary dysmenorrhea. Kowsar Med J. 2009;14:49–52. [Google Scholar]
- 8.Mohammad Alizadeh Charandabi S, Mirghafourvand M, Javadzadeh Y, Nezamivand Chegini S. Effect of calcium with and without magnesium on amount and duration of menstrual bleeding in students with primary dysmenorrhea. Iran J Obstet Gynecol Infertil. 2014;16:1–8. [Google Scholar]
- 9.Rahimi M, Ziaee S, Babaei G, Rabiei M. The effect of vitamin E in the treatment of menorrhagia in patient with dysfunctional uterine bleeding. Daneshvar. 2009;16:59–66. [Google Scholar]
- 10.Shobeiri F, Zeraati F, Araghchian M, Nazari M. The effect of fennelin, vitagnus and mefenamic acid in the treatment of menstrual bleeding. Sci J Hamadan Univ Med Sci. 2014;21:171–6. [PMC free article] [PubMed] [Google Scholar]
- 11.Speroff L, Fritz MA, editors. Clinical Gynecologic Endocrinology and Infertility. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 12.Bokaie M, Enjezab B. The effects of oral fennel extract on the intensity of menstrual bleeding in relieving dysmenorrheal: A randomized clinical trial. Community Health J. 2014;8:55–62. [Google Scholar]
- 13.Zeraati F, Shobeiri F, Nazari M, Araghchian M, Bekhradi R. Comparative evaluation of the efficacy of herbal drugs (fennelin and vitagnus) and mefenamic acid in the treatment of primary dysmenorrhea. Iran J Nurs Midwifery Res. 2014;19:581–4. [PMC free article] [PubMed] [Google Scholar]
- 14.Davari M, Reihani M, Khoshrang N. The aromatherapy effect of rosemary and lavander on primary dysmenorrhea: A clinical controlled trial. J Isfahan Med Sch. 2014;32:1–9. [Google Scholar]
- 15.Jafarnejad F, Mohanazadeh Falahieh F, Rakhshandeh H, Shakeri MT. Comparison of the effect of nigella sativa and mefenamic acid on menstrual hemorrhage in the students with primary dysmenoreha. Iran J Obstet Gynecol Infertil. 2016;18:5–10. [Google Scholar]
- 16.Shoja N, Dianat M, Hoseyni Nik S, Ramazani G. The evaluation of the protective effects of the hydro-alcoholic extract of rosemary (Rosmarinus officinalis L.) on ventricular arrhythmias in rats. J Babol Univ Med Sci. 2015;17:66–72. [Google Scholar]
- 17.Emami A, Fasihi M, Mehregan A. Reference Book of Medicinal Plants. Vol. 2. Tehran: Andishavar; 2013. pp. 1199–201. [Google Scholar]
- 18.Mengoni ES, Vichera G, Rigano LA, Rodriguez-Puebla ML, Galliano SR, Cafferata EE, et al. Suppression ofCOX-2, IL-1β and TNF-α expression and leukocyte infiltration in inflamed skin by bioactive compounds from Rosmarinus officinalis L. Fitoterapia. 2011;82:414–21. doi: 10.1016/j.fitote.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 19.Moaveni P. Medicinal Plants. Shahryar: Gods; 2009. pp. 81–2. [Google Scholar]
- 20.Bahrami-Taghanaki H, Javanmard Khoshdel M, Noras M, Azizi H, Azizi H, Hafizi Lotfabadi L. Effects of acupuncture and Mefenamic acid on primary dysmenorrhea. Iran J Obstet Gynecol Infertil. 2017;19:31–41. [Google Scholar]
- 21.Phumdoung S, Rattanaparikonn A, Maneechot K. Pain during the first stage of laber. Songklanagarind Med J. 2004;22:163–71. [Google Scholar]
- 22.Biri A, Bozkurt N, Korucuoǧlu Ü, Yilmaz E, Tıraş B, Güner H. Use of pictorial chart of managing menorrhagia among Turkish women. J Turk Ger Gynecol Assoc. 2007;9:35–7. [Google Scholar]
- 23.Shirvani MA, Motahari-Tabari N, Alipour A. The effect of mefenamic acid and ginger on pain relief in primary dysmenorrhea: A randomized clinical trial. Arch Gynecol Obstet. 2015;291:1277–81. doi: 10.1007/s00404-014-3548-2. [DOI] [PubMed] [Google Scholar]
- 24.Sinkovic A, Suran D, Lokar L, Fliser E, Skerget M, Novak Z, et al. Rosemary extracts improve flow-mediated dilatation of the brachial artery and plasma PAI-1 activity in healthy young volunteers. Phytother Res. 2011;25:402–7. doi: 10.1002/ptr.3276. [DOI] [PubMed] [Google Scholar]
- 25.Sekhavat L, Zare TF, Karimzadeh MMA. Comparison of mefenamic acid, and tranexamic acid in treatment of hypermenorrhea. Iran J Obstet Gynecol Infertil. 2007;9:17–22. [Google Scholar]
- 26.Karimian Z, Sadat Z, Abedzadeh M, Sarafraz N, Kafaei Atrian M, Bahrami N. Comparison the effect of mefenamic acid and Matricariachamomilla on primary dysmenorrhea in Kashan medical university students. J Ardabil Univ Med Sci. 2013;13:413–20. [Google Scholar]