Abstract
Objective:
African-American women are more likely than other women in the United States to experience poor HIV-related health; HIV stigma may contribute to these outcomes. This study assessed the relationship between HIV stigma and viral load, over time, among a sample of African-American women receiving treatment for HIV, and explored social support and depressive symptoms as mediators.
Design:
Secondary analysis of longitudinal data.
Methods:
Data came from a randomized trial of an intervention to reduce HIV stigma among African-American women in HIV care in Chicago, Illinois and Birmingham, Alabama. Sociodemographic and psychosocial data were collected at up to six study visits over 14 months. Viral loads were extracted from medical records during the study period. Generalized linear mixed effects models were used to estimate associations between overall, internalized, and enacted HIV stigma and viral load over time. Mediation analyses were used to estimate indirect effects via social support and depressive symptoms.
Results:
Data from 234 women were analyzed. Overall HIV stigma was significantly associated with subsequent viral load (adjusted β = 0.24, p = 0.005). Both between-subject (adjusted β = 0.74, p < 0.001) and within-subject (adjusted β = 0.34, p = 0.005) differences in enacted stigma were associated with viral load. Neither social support nor depressive symptoms were statistically significant mediators.
Conclusions:
Ongoing experiences of HIV stigmatization may contribute to increased viral load among African-American women in primary HIV care. Interventions should aim to alleviate the consequences of stigma experienced by patients and prevent future stigmatization.
Keywords: HIV, stigma, viral load, women, African-American, longitudinal
Introduction
African-American women are over-represented and over-burdened among women living with HIV in the United States (US) [1–3]. Despite representing only 13% of the total female population, they account for 61% of new HIV diagnoses among women in the US [4]. African-American women living with HIV are also less likely to be on antiretroviral therapy (ART), more likely to initiate ART late, and more likely to discontinue ART early [5–7], resulting in higher rates of morbidity and mortality than among other women living with HIV [8, 9]. Improving rates of viral suppression in this population would reduce morbidity, mortality, and the risk of onward transmission of the virus [10].
African-American women living with HIV have multiple marginalized social identities at the intersection of race, sex, and health, and may therefore be especially vulnerable to HIV stigma [11]. HIV stigma is the co-occurrence of labeling, stereotyping, separating, status loss, and/or discrimination associated with HIV in the context of power imbalance [12]. HIV stigma has several dimensions. Enacted stigma refers to an individual’s actual experiences of prejudice and discrimination because of their HIV status. On the other hand, internalized stigma refers to an individual’s acceptance of negative attitudes or beliefs related to their HIV status [13]. Stigma can lead to loss of relationships, employment, education, and housing; reduction in help- or treatment-seeking behavior; negative emotional and behavioral changes; and poor health outcomes [14–19]. HIV stigma has consistently been shown to be associated with higher rates of depression, lower social support, and lower levels of treatment adherence [20–24]. Among African-American women in particular, HIV stigma has been associated with isolation [25, 26], decreased psychological functioning [27], and symptoms of depression [26, 28, 29].
Recent cross-sectional analyses have suggested a plausible link between HIV stigma and poor viral control among African-American women receiving treatment for HIV [30]. However, to date no study has established prospective associations between changes in individual dimensions of HIV stigma and subsequent changes in viral load in this population and no study has identified potential mechanisms for these changes. The primary objective of this study was to assess the relationship between multi-dimensional HIV stigma and viral load, over time, in a sample of African-American women receiving treatment for HIV. The secondary objective was to explore social support and depressive symptoms as potential mediators of this relationship.
Methods
We analyzed longitudinal data from the Unity Study, a multisite randomized controlled trial testing the effectiveness of a behavioral intervention to reduce HIV stigma among African-American women living with HIV [31]. Trial and intervention methods, alongside primary outcome results, are described in detail elsewhere [32]. From May 2013 to October 2015, African-American women living with HIV were recruited from three clinical sites: the Northwestern University HIV clinic (NU) and the Ruth M. Rothstein CORE Center (CORE) in Chicago, Illinois, and the University of Alabama, Birmingham 1917 HIV clinic (UAB) in Birmingham, Alabama. Women were eligible for the Unity Study if they self-identified as African-American, were at least 18 years old, were living with HIV, and were receiving HIV services from one of the three clinical sites. Because research suggests that immigrant Black Americans have unique experiences related to HIV and HIV stigma [33–35], women were excluded from the Unity Study if they were foreign-born and had lived in the US for less than ten years.
Participants provided written consent to participate in the study and signed HIPAA authorizations allowing access to their medical records. Sociodemographic and psychosocial data were collected during up to six study visits, via tablet-based audio computer assisted self-interview (ACASI), at baseline, post-intervention, and 4, 6, 8, and 12 months post-intervention. Relevant clinical data, including data from HIV-1 RNA levels (viral loads) and CD4 T-lymphocyte counts, were extracted from participant medical records over the course of the study. Participants’ study visit data were included in the present analysis if participants reported having a prescription for ART at the time of the given study visit, to ensure modifiability of participant viral load via treatment.
All Unity Study procedures were approved by the University of Washington Institutional Review Board and by institutional review boards at each clinical site. The Unity Study was registered under Clinicaltrials.gov number NCT01893112.
Outcome
The primary outcome of interest was viral load, parameterized as the log of the mean of all viral loads following a given study visit (time = t), prior to any subsequent study visit (time = t+1) or 180 days post-study visit, whichever came first. Figure 1 describes the structure of the data and the relevant time intervals. We took the log to reduce the skew of the variable, as recommended for viral load data [36]. Most study visits were followed by another study visit within 60 days; we used the 180 day interval to bound viral loads collected after a participant’s final study visit. The secondary outcome of interest was durable viral suppression, defined as having all viral loads under 200 copies/ml following a given study visit (time = t), prior to the subsequent study visit (time = t+1) or 180 days post-study visit, whichever came first. As a sensitivity analysis, for both log mean viral load and viral suppression, we also restricted our analysis to viral loads collected within 90 days following a given study visit or prior to the subsequent study visit, whichever came first.
Figure 1:
Data structure and approach to linking viral loads with study visits
Predictor
The predictor of interest was self-reported HIV stigma at each study visit, measured using the 14-item Stigma Scale for Chronic Illness (SSCI). The SSCI measures enacted and internalized stigma and has been validated for use with African-Americans living with HIV (Cronbach α = 0.93) [37, 38]. It includes statements like, “Because of my illness, people were unkind to me,” related to enacted stigma, and “I felt embarrassed about my illness,” related to internalized stigma. All items used a 5-point Likert-type scale ranging from 1 = “Never” to 5 = “Always”. An overall HIV stigma score, ranging from 14 to 70, was created by summing SSCI scale responses at each study visit. As secondary predictors of interest, we also summed the SSCI sub-scales for enacted and internalized stigma, both ranging from 7 to 35. Higher scores indicated greater HIV stigmatization.
Mediators
The first mediator of interest was perceived social support at each study visit, measured using the emotional/information support and positive social interaction subscales of the Medical Outcomes Study-Social Support Survey (MOS-SSS). The MOS-SSS assesses the degree to which respondents’ interpersonal relationships serve particular support functions in their lives and has been used extensively in chronic disease contexts [39]. The second mediator of interest was depressive symptom severity at each study visit, measured using the 8-item Patient Health Questionnaire (PHQ-8) [40]. This is an abridged version of the PHQ-9 with the suicidality item omitted. The PHQ-9 is commonly used to screen for and monitor depression [41]. Summary social support and depressive symptom scores were created by taking the sum of scale responses. Higher scores indicated greater perceived social support and greater depressive symptom severity, respectively.
Covariates
Covariates were chosen to account for potential observed confounding. These included Unity Study arm (binary), time from baseline in months (continuous), the interaction of arm and time, study site (NU, CORE, or UAB), years of age (continuous), years lived with HIV (continuous), level of education (less than high school, high school degree or equivalent, some college, or college degree and beyond), occupation (employed, homemaker, student, or other), and number of children (none, 1–3, or 4+). We did not adjust for ART adherence or CD4 count, as we hypothesized that these were part of the causal pathway linking HIV stigma and viral load [42].
Analysis
Descriptive analyses, including t tests and χ2 tests, were conducted to summarize and compare participant characteristics at baseline, stratified above and below the mean overall HIV stigma score at baseline. We then assessed missingness in the data and used linear and logistic regression models to look for associations between participant characteristics and patterns of missing data, including study loss to follow-up, to better understand whether data were missing at random. We next used bootstrapping-based expectation-maximization multiple imputation to impute missing data. All available covariates along with prior and subsequent viral loads were included as predictors in the imputation. We imputed ten datasets and assessed fit using over-imputation diagnostic plots. Imputed viral loads were logged and dichotomized, and scale scores were calculated from individually imputed items, after the imputation and prior to inferential analysis. Scale scores were standardized so that one-unit changes in the scale scores corresponded to increases or decreases of one standard deviation.
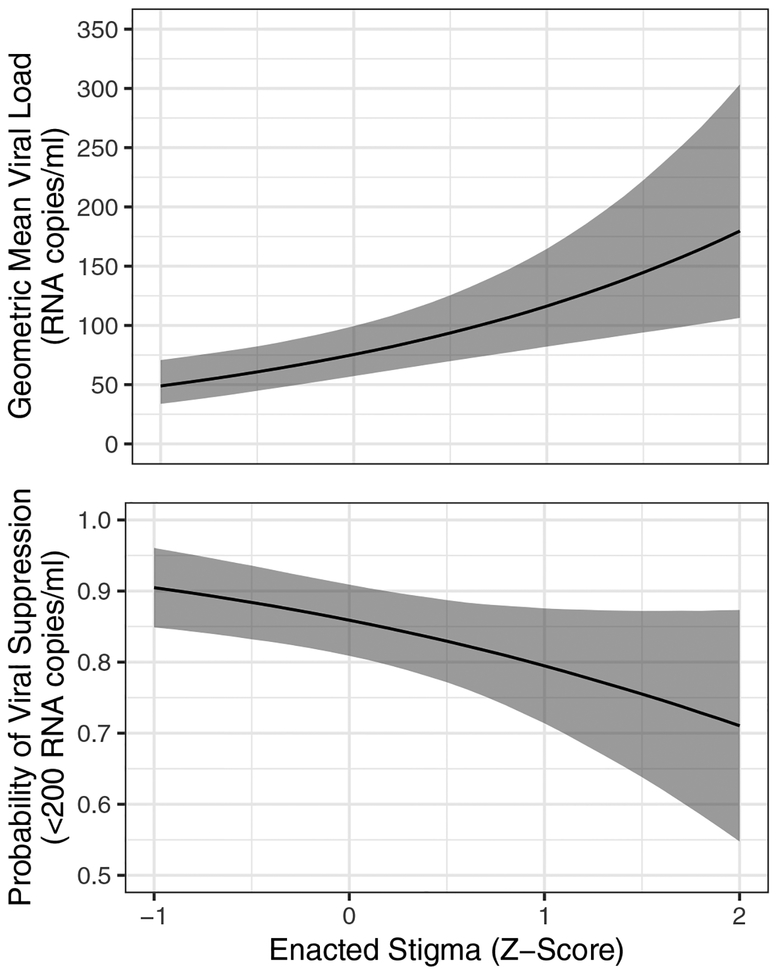
We used four types of generalized linear mixed effects models to estimate prospective associations between HIV stigma and primary and secondary viral load outcomes. Models 1a and 1b used overall HIV stigma as the predictor of interest, treating HIV stigma as unidimensional. Models 2a and 2b used internalized and enacted stigma as the predictors of interest, dividing HIV stigma into the two distinct dimensions available in the SSCI measure. Models 1a and 2a used standardized person-time stigma scores as predictors, producing population average estimates that combined within- and between-subject differences in stigma. These models did not distinguish between changes in stigma across individuals and changes in stigma within the same individual over time. Models 1b and 2b used Mundlak (within-between) correction, including both the subject-level mean HIV stigma and subject-time deviations from the subject-level mean as predictors [43]. These models explicitly distinguished between changes in stigma across individuals (between-subject) and changes in stigma within the same individual over time (within-subject). Mundlak correction minimizes observed and unobserved time-invariant confounding because each participant serves as her own control, and has been shown to outperform traditional random and fixed effects models [44]. For each model, we considered three levels of covariate adjustment: unadjusted, adjusting for trial arm, time, and their interaction, and fully adjusting for all covariates. Models with the log mean viral load outcome used the Gaussian family and identity link, while models with the durable viral suppression outcome used the binomial family and logit link. All models included a random subject-specific intercept. All models were estimated on each of the ten imputed datasets, and Rubin’s rules were used to pool coefficient and standard error estimates [45]. Finally, we used the estimates from Model 2a to calculate and plot the predicted geometric mean viral loads and probabilities of viral suppression over the observed range of standardized enacted HIV stigma sub-scale scores (−1 SD to +2 SD), with all other covariates at their means [46].
To estimate the indirect effects of overall HIV stigma on viral load via social support and depressive symptom severity, we conducted two causal mediation analyses. We used two sets of linear mixed effects models for each. The first set estimated associations between overall HIV stigma and the respective mediator, while the second set estimated associations between the respective mediator and log mean viral load, adjusting for overall HIV stigma. As above, all models used random subject-specific intercepts, and all were fully adjusted for the same set of potential confounders. Causal mediation analysis proceeded first by predicting the mediator given contrasting predictor values; we contrasted overall HIV stigma from −1 to +1 SD. It then predicted the outcome given the predictor, both with and without the mediator; took the difference of these predicted outcomes to estimate the mediated effect; and finally bootstrapped to estimate uncertainty [47]. Each causal mediation analysis was run using 1,000 simulations, on all ten imputed datasets. Final estimates were pooled using Rubin’s rules [45].
All analyses were performed in version 3.4.0 of R [48]. Multiple imputation was performed using version 1.7.5 of the Amelia II package [49] and causal mediation was performed using version 4.4.6 of the mediation package [50].
Sensitivity Analyses
All models were also estimated using complete case analysis to test the sensitivity of the results to missing data. We also tested an alternative parameterization of the viral load outcomes, considering only viral loads collected within 90 days following a given study visit, instead of 180 days, strengthening the temporal link between HIV stigma and viral load.
Results
Two hundred and thirty nine participants were enrolled in the Unity Study. Two hundred and thirty four participants had a prescription for ART and were included in this analysis. Table 1 summarizes participant characteristics at baseline, stratified above or below mean overall stigma (32.89, standard deviation [SD]: 13.15). Mean internalized stigma at baseline was 19.13 (SD: 7.34), and mean enacted stigma was 13.74 (SD: 7.08). One hundred and twenty nine participants had below-average overall stigma scores, while 105 had stigma scores above the mean. Mean age was 46.7 years (SD: 10.5); individuals with higher overall stigma scores were more likely to be older than individuals with lower scores (p = 0.026). Compared to individuals with lower overall stigma scores, individuals with higher stigma scores were more likely never to have been married (44.2% vs. 30.5%, p = 0.021) and more likely to be from the CORE site (47.6% vs. 26.4%, p = 0.003). Individuals with higher stigma scores reported more days of missed ART doses in the previous month (p = 0.007), lower social support (p = 0.001), and higher depressive symptom severity (p < 0.001). They had similar CD4 counts (overall mean 604.3, SD: 371.1), but they had higher log mean viral load (p = 0.006) and were less likely to be virally suppressed (70.5% vs. 85.2%, p = 0.077). Between 0 and 18 (7.7%) participants were missing covariate data at baseline, while 136 (58%) did not have eligible viral loads over the time period from baseline to the next study visit. Participants completed a mean of 4.3 study visits (SD: 1.9) with 42% (n = 98) completing all six study visits. Older participants, separated/divorced participants, and participants with higher social support were slightly more likely to complete all six study visits. Eligible viral loads were linked to 568 out of 1,016 (55.9%) total participant-study visits; the other 44.1% were imputed in the primary analysis.
Table 1:
Participant descriptive statistics at baseline (n=234)
| Missing at baseline | ≤ mean overall HIV stigma | > mean overall HIV stigma | Total | p | |
|---|---|---|---|---|---|
| N | 129 | 105 | 234 | ||
| Age (years), mean (SD) | 1 | 48.1 (10.4) | 45.0 (10.5) | 46.7 (10.5) | 0.026 |
| Education | 7 | 0.41 | |||
| Less than High School | 42 (33.9%) | 44 (42.7%) | 86 (37.9%) | ||
| High School degree or equivalent | 28 (22.6%) | 25 (24.3%) | 53 (23.3%) | ||
| Some College/AA/Technical Degree | 42 (33.9%) | 27 (26.2%) | 69 (30.4%) | ||
| College degree or above | 12 (9.7%) | 7 (6.8%) | 19 (8.4%) | ||
| Occupation | 18 | 0.49 | |||
| Employed | 56 (47.1%) | 40 (41.2%) | 96 (44.4%) | ||
| Homemaker | 37 (31.1%) | 31 (32.0%) | 68 (31.5%) | ||
| Student | 6 (5.0%) | 10 (10.3%) | 16 (7.4%) | ||
| Other | 20 (16.8%) | 16 (16.5%) | 36 (16.7%) | ||
| Marital Status | 2 | 0.021 | |||
| Never been married | 39 (30.5%) | 46 (44.2%) | 85 (36.6%) | ||
| Married or living with partner | 27 (21.1%) | 26 (25.0%) | 53 (22.8%) | ||
| Separated, Divorced, Widowed | 62 (48.4%) | 32 (30.8%) | 94 (40.5%) | ||
| Number of Children | 6 | 0.91 | |||
| No children | 74 (59.2%) | 59 (57.3%) | 133 (58.3%) | ||
| 1–3 children | 43 (34.4%) | 36 (35.0%) | 79 (34.6%) | ||
| 4+ children | 8 (6.4%) | 8 (7.8%) | 16 (7.0%) | ||
| Years lived with HIV, mean (SD) | 4 | 14.3 (7.7) | 14.0 (6.6) | 14.2 (7.2) | 0.73 |
| Site | 0 | 0.003 | |||
| Northwestern University | 30 (23.3%) | 18 (17.1%) | 48 (20.5%) | ||
| CORE Center | 34 (26.4%) | 50 (47.6%) | 84 (35.9%) | ||
| University of Alabama, Birmingham | 65 (50.4%) | 37 (35.2%) | 102 (43.6%) | ||
| Days of ART doses missed in previous 30 days, median (IQR) | 5 | 0 (0, 2) | 1 (0, 3) | 0 (0, 2) | 0.007 |
| Social support (MOS-SSS), mean (SD) | 0 | 32.6 (11.5) | 27.5 (12.4) | 30.3 (12.2) | 0.001 |
| Depressive symptoms (PHQ-8), mean (SD) | 0 | 5.4 (4.8) | 10.4 (6.6) | 7.7 (6.2) | <0.001 |
| CD4 Count, mean (SD) | 13 | 623.3 (367.9) | 580.9 (375.5) | 604.30 (71.1) | 0.40 |
| Log of mean viral load, median (IQR) | 136 | 2.9 (2.9, 3.7) | 3.7 (2.9, 6.5) | 3.5 (2.9, 4.6) | 0.006 |
| Virally suppressed (<200 copies/ml) | 136 | 46 (85.2%) | 31 (70.5%) | 77 (78.6%) | 0.077 |
SD: standard deviation; IQR: inter-quartile range; ART: anti-retroviral therapy
Table 2 is a summary of estimates from the generalized linear mixed effects models evaluating associations between HIV stigma and viral load. Estimates were consistent across the three levels of adjustment; only fully adjusted estimates are presented in Table 2. In Model 1a each standard deviation increase in overall HIV stigma is associated with an increase in log mean viral load (adjusted β [aβ]: 0.24, 95% confidence interval [CI]: 0.07, 0.41) and reduced odds of durable viral suppression (adjusted odds ratio [aOR]: 0.69, 95% CI: 0.52, 0.91). Model 1b, which decomposed this association into between- and within-subject effects, found that between-subject differences in overall stigma were associated with log mean viral load (aβ: 0.39, 95% CI: 0.11, 0.67) and viral suppression (aOR: 0.58, 95% CI: 0.40, 0.85), while within-subject differences were not. In Model 2a, where internalized and enacted HIV stigma sub-scales were evaluated as separate predictors, enacted stigma was associated with log mean viral load (aβ: 0.44, 95% CI: 0.24, 0.64) and viral suppression (aOR: 0.62, 95% CI: 0.43, 0.90), whereas internalized stigma was not. Finally, Model 2b decomposed these sub-scale associations into between-and within-subject effects, and found that both between-subject differences in enacted stigma (aβ: 0.74, 95% CI: 0.33, 1.15) and within-subject differences in enacted stigma (aβ: 0.34, 95% CI: 0.10, 0.58) were associated with log mean viral load. Only between-subject differences in enacted stigma were associated with viral suppression (aOR: 0.51, 95% CI: 0.29, 0.89). Complete model estimates, including measures of association for confounders, are presented in Supplemental Digital Content 1 (Table); key models are highlighted in green.
Table 2:
Generalized linear mixed effects model estimates of associations between HIV stigma and viral load
| Model | Log mean viral load | Durable viral suppression (<200 copies/ml) | |||||
|---|---|---|---|---|---|---|---|
| aβ1 | 95% CI | p | aOR1 | 95% CI | p | ||
| 1a | Overall HIV stigma | 0.24 | 0.07, 0.41 | 0.005 | 0.69 | 0.52, 0.91 | 0.010 |
| 1b | Subject mean overall HIV stigma2 | 0.39 | 0.11, 0.67 | 0.007 | 0.58 | 0.40, 0.85 | 0.005 |
| Subject deviation overall HIV stigma3 | 0.17 | −0.04, 0.38 | 0.115 | 0.84 | 0.56, 1.28 | 0.420 | |
| 2a | Internalized HIV stigma | −0.18 | −0.39, 0.03 | 0.097 | 1.08 | 0.72, 1.62 | 0.706 |
| Enacted HIV stigma | 0.44 | 0.24, 0.64 | <0.001 | 0.62 | 0.43, 0.90 | 0.012 | |
| 2b | Subject mean internalized HIV stigma2 | −0.30 | −0.71, 0.11 | 0.148 | 1.09 | 0.61, 1.96 | 0.762 |
| Subject deviation internalized HIV stigma3 | −0.17 | −0.42, 0.09 | 0.196 | 1.13 | 0.64, 1.98 | 0.680 | |
| Subject mean enacted HIV stigma2 | 0.74 | 0.33, 1.15 | <0.001 | 0.51 | 0.29, 0.89 | 0.017 | |
| Subject deviation enacted HIV stigma3 | 0.34 | 0.10, 0.58 | 0.005 | 0.75 | 0.45, 1.23 | 0.253 | |
Note: all stigma scores have been standardized. One unit is equivalent to a one standard deviation increment in stigma score.
estimates fully adjusted for all covariates;
between-subject effects;
within-subject effects
CI: confidence interval; aβ: adjusted β coefficient; aOR: adjusted odds ratio
Figure 2 presents predicted geometric mean viral loads and predicted probability of viral suppression, with confidence intervals, given the observed range of enacted stigma. Under these counterfactual scenarios, the predicted geometric mean viral load rose from 49.90 (95% CI: 33.82, 70.71) at low levels of enacted stigma to 179.64 (95% CI: 106.36, 303.41) at high levels of enacted stigma. The predicted probability of viral suppression fell from 90.47% (95% CI: 84.90%, 96.05%) at low levels of enacted stigma to 71.05% (95% CI: 54.77%, 87.33%) at high levels of enacted stigma.
Figure 2:
Predicted geometric mean viral load and probability of viral suppression by levels of enacted stigma
Table 3 presents parameter estimates from the mediation models estimating direct and indirect effects of overall HIV stigma on log mean viral load, via social support and depressive symptoms. While overall HIV stigma was found to be negatively associated with social support in the first step of the first mediation model (aβ: −0.32, 95% CI: −0.39, −0.25), social support was not associated with log mean viral load independently of stigma in the second step. This resulted in an estimated direct effect (DE) of 0.40 (95% CI: −0.01, 0.81) and an average causal mediation effect (ACME) of 0.09 (95% CI: −0.02, 0.20), suggesting that 19% (95% CI: −67%, 104%) of the effect of overall HIV stigma on log mean viral load was mediated by social support. The estimated indirect effect was not statistically significant. In the first step of the second mediation model, overall HIV stigma was found to be positively associated with depressive symptoms (aβ: 0.50, 95% CI: 0.43, 0.55), though again depressive symptoms were not independently associated with log mean viral load in the second step. This resulted in an estimated DE of 0.48 (95% CI: 0.036) and an ACME of 0.00 (95% CI: −0.19, 0.19), suggesting that 0% (95% CI: −82%, 82%) of the effect of stigma on log mean viral load was mediated by depressive symptoms. Again, the estimated indirect effect was not statistically significant.
Table 3:
Mediation estimates of direct and indirect effects of overall HIV stigma on log mean viral load, via social support and depressive symptoms
| β | 95% CI | p | β | 95% CI | p | |
|---|---|---|---|---|---|---|
| Overall HIV Stigma → Mediator | −0.32 | −0.39, −0.25 | <0.001 | 0.50 | 0.43, 0.55 | <0.001 |
| Mediator → Log Mean Viral Load | −0.14 | −0.29, 0.01 | 0.076 | 0.00 | −0.17, 0.17 | 1.000 |
| Average causal mediation effect | 0.09 | −0.02, 0.20 | 0.111 | 0.00 | −0.19, 0.19 | 0.998 |
| Direct effect | 0.40 | −0.01, 0.81 | 0.059 | 0.48 | 0.03, 0.93 | 0.036 |
| Total effect | 0.49 | 0.07, 0.90 | 0.022 | 0.48 | 0.07, 0.89 | 0.021 |
| % Mediated | 18% | −67%, 104% | 0.675 | 0% | −82%, 82% | 0.996 |
CI: confidence interval
Supplemental Digital Content 1 (Table) presents results of sensitivity analyses, including the complete case analyses, assessments of the alternative parametrization of viral load, and the test of the assumption that all missing viral loads were not virally suppressed. All results from sensitivity analyses were consistent with the primary results.
Discussion
This study examined longitudinal associations between HIV stigma and viral load among African-American women receiving treatment for HIV. Results suggest that HIV stigma and viral load are closely linked. Specifically, women with higher overall HIV stigma scores were more likely to have higher subsequent viral loads than women with lower overall HIV stigma scores. Within-person changes in overall HIV stigma were not significantly associated with subsequent viral load, but assessment of internalized and enacted HIV stigma as independent predictors revealed that both between- and within-person differences in enacted HIV stigma were significantly associated with subsequent viral load. This suggests that ongoing experiences of stigma related to HIV may have immediate, deleterious effects on HIV-related health and hinder the transition to viral suppression in this population. Aside from treatment non-adherence, the mechanism for these effects is not clear; our analyses did not identify social support or depressive symptoms as statistically significant mediators of the relationship between HIV stigma and viral load.
Our results reinforce the notion that the unique dimensions of HIV stigma are differentially associated with patient health and wellbeing [51]. While internalized stigma may be predictive of affective or cognitive outcomes, enacted HIV stigma may be uniquely tied to HIV-related physical health. Other studies in the US have found associations between enacted stigma and HIV symptoms [52], CD4 count [51], and viral load [53]. Interestingly, these studies also failed to identify mediators or moderators of this relationship, aside from treatment non-adherence, suggesting a more direct relationship between the stress of enacted stigma and subsequent health outcomes [51, 54]. Future research might elucidate this relationship by testing other possible mediators, including care-seeking behavior and clinical care engagement, and by measuring changes in behavior over short periods of time immediately following experiences of HIV stigma.
Our findings have significant implications for future interventions. African-American women are at higher risk for HIV-related morbidity and mortality [8, 9], and ongoing experiences of HIV stigma appear to interfere with maintenance of or progress towards viral suppression in this population. As such, interventions should aim to alleviate internalized stigma among women living with HIV, as well as target the sources of stigma to prevent future experiences of stigma. Stigmatization of African-American women living with HIV may come from many places – friends, family, partners, health care workers, community members, and societal structures – and may magnify existing vulnerabilities on account of disadvantaged race and sex [55]. Notably, the source of the stigma matters; evidence suggests that stigmatization by healthcare workers may be especially detrimental to HIV treatment outcomes [53].
Our results are supported by our use of longitudinal data and the prospective analysis in which all associations were assessed between psychosocial predictors measured prior to the viral load outcomes. However, the study had several limitations. First, almost half of the viral load outcomes were missing. Tis was a structural missingness, as study visits were more frequent than routine viral load assessments; thus, many visits were not followed by eligible viral loads. The use of multiple imputation in our analysis helped to avoid the bias and loss of efficiency that can result from missing data [56], Moreover, our use of multiple imputation had the advantage of leveraging all available self-reported psychosocial data and ensured that measures of association were prospective. It should be noted that sensitivity analyses demonstrated that the findings were consistent regardless of how we treated the missing data. Second, we could not adjust for several variables that are known to be strongly associated with viral load, including alcohol/substance use and homelessness/housing insecurity [57, 58]. In response, we used the fixed-effects estimator as part of the Mundlak correction to attempt to account for all observed and unobserved time-invariant confounding [44]. Third, we did not adjust for possible observed or unobserved time-varying confounders. Potential time-varying confounders would include participants’ prior HIV stigma status and her prior viral load. Future analyses may consider applying g-computation or instrumental variables to account for possible time-varying confounding [59, 60]. Fourth, our models tested a particular pathway, assuming that HIV stigma would affect viral load [13]. It is possible that the true pathway is from viral load to stigma, perhaps via visible symptoms of ill health or increased exposure to the health system. Further analyses are needed to confirm the direction of causality between HIV stigma and viral load. Fifth, ordinary least-squares regression with a logged outcome (log-OLS) may be imprecise or even biased compared to generalized linear models (GLM) under certain circumstances [61]. Further studies may consider GLMs with log link and gamma probability distribution that directly accommodate the positively skewed distribution of the outcome. However, log-OLS has been shown to outperform GLM with heavy-tailed distributions, as was the case in this study [61]. Sixth, though we identified a link between ongoing experiences of HIV stigma and higher viral loads, our data did not identify the sources of these experiences. Future study is needed to assess whether stigmatization by particular sources (e.g., family members, healthcare workers) is especially detrimental in this population. Finally, this was a secondary analysis of data from a sample of women on treatment who participated in a group-based stigma reduction intervention. They may have differed from the broader population of African American women living with HIV in substantive ways; for example, they may have had higher overall HIV stigma levels, or self-selected into the intervention due to issues with low social support. Our findings should be confirmed using a larger, representative sample of African American women living with HIV.
In conclusion, we assessed the relationship between HIV stigma and viral load among African-American women receiving treatment for HIV. Our study indicates that ongoing experiences of HIV stigma may have negative effects on viral load in this population over relatively short periods of time. These effects do not appear to be mediated by social or depressive symptoms. To ensure that interventions to alleviate stigma among African-American women living with HIV have a beneficial impact on patient health, they may need to broaden their focus to target the sources of stigma, rather than just those who are stigmatized.
Supplementary Material
Supplemental Digital Content 1 (Table): Complete model estimates for primary and sensitivity analyses
Acknowledgements
CK, LL, DH, and DR conceived of the study. CK developed the analytic plan and conducted the analysis with support from LL and DH. DR led the trial that collected data used for this study, with support from DH, PN, JT, JS, SC, MB, BB, MA, and MM. CK drafted the manuscript, and all authors contributed to revisions. All authors read and approved the final manuscript.
Financial support was provided by NIMH 1R01MH098675–01 (PI: Rao) and NIMH 1F31MH112397–01A1 (PI: Kemp).
We would like to acknowledge and thank the participants of the Unity study. We also thank Dr. Brandon Guthrie and Dr. Marco Carone, both at the University of Washington, for valuable comments on early analytic plans.
Footnotes
Conflicts of Interest: None
References
- 1.CDC. Fact sheet: HIV among African Americans. In; 2017.
- 2.CDC. Fact sheet: HIV in the United States: The Stages of Care In: Centers for Disease Control and Prevention; 2014. pp. CDC Fact Sheet. [Google Scholar]
- 3.Beer L, Mattson CL, Bradley H, Skarbinski J. Understanding Cross-Sectional Racial, Ethnic, and Gender Disparities in Antiretroviral Use and Viral Suppression Among HIV Patients in the United States. Medicine 2016; 95(13):e3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CDC. HIV Surveillance in Women (through 2016). Atlanta: CDC; 2017. [Google Scholar]
- 5.Lillie-Blanton M, Stone VE, Snow Jones A, Levi J, Golub ET, Cohen MH, et al. Association of race, substance abuse, and health insurance coverage with use of highly active antiretroviral therapy among HIV-infected women, 2005. American journal of public health 2010; 100(8):1493–1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen MH, Cook JA, Grey D, Young M, Hanau LH, Tien P, et al. Medically eligible women who do not use HAART: the importance of abuse, drug use, and race. American journal of public health 2004; 94(7):1147–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Losina E, Schackman BR, Sadownik SN, Gebo KA, Walensky RP, Chiosi JJ, et al. Racial and sex disparities in life expectancy losses among HIV-infected persons in the united states: impact of risk behavior, late initiation, and early discontinuation of antiretroviral therapy. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2009; 49(10):1570–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lesko CR, Cole SR, Miller WC, Westreich D, Eron JJ, Adimora AA, et al. Ten-year Survival by Race/Ethnicity and Sex Among Treated, HIV-infected Adults in the United States. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2015; 60(11):1700–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meditz AL, MaWhinney S, Allshouse A, Feser W, Markowitz M, Little S, et al. Sex, race, and geographic region influence clinical outcomes following primary HIV-1 infection. The Journal of infectious diseases 2011; 203(4):442–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Modjarrad K, Chamot E, Vermund SH. Impact of small reductions in plasma HIV RNA levels on the risk of heterosexual transmission and disease progression. AIDS (London, England) 2008; 22(16):2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao D, Andrasik MP, Lipira L. HIV stigma among black women in the United States: Intersectionality, support, resilience. In: American Public Health Association; 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Link BG, Phelan JC. Conceptualizing stigma. Annual review of Sociology 2001; 27(1):363–385. [Google Scholar]
- 13.Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. American journal of public health 2017; 107(6):863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mak WW, Poon CY, Pun LY, Cheung SF. Meta-analysis of stigma and mental health. Social science & medicine 2007; 65(2):245–261. [DOI] [PubMed] [Google Scholar]
- 15.Logie C, Gadalla T. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS care 2009; 21(6):742–753. [DOI] [PubMed] [Google Scholar]
- 16.Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social science & medicine 2010; 71(12):2150–2161. [DOI] [PubMed] [Google Scholar]
- 17.Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. American Psychologist 2013; 68(4):225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tucker A, Liht J, de Swardt G, Jobson G, Rebe K, McIntyre J, et al. Homophobic stigma, depression, self-efficacy and unprotected anal intercourse for peri-urban township men who have sex with men in Cape Town, South Africa: a cross-sectional association model. AIDS care 2014; 26(7):882–889. [DOI] [PubMed] [Google Scholar]
- 19.Maleke K, Daniels J, Lane T, Struthers H, McIntyre J, Coates T. How social stigma sustains the HIV treatment gap for MSM in Mpumalanga, South Africa. Global health promotion 2017:1757975917737509. [DOI] [PubMed] [Google Scholar]
- 20.Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ open 2016; 6(7):e011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS care 2007; 19(1):28–33. [DOI] [PubMed] [Google Scholar]
- 22.Rintamaki LS, Davis TC, Skripkauskas S, Bennett CL, Wolf MS. Social stigma concerns and HIV medication adherence. AIDS patient care and STDs 2006; 20(5):359–368. [DOI] [PubMed] [Google Scholar]
- 23.Edwards LV. Perceived social support and HIV/AIDS medication adherence among African American women. Qualitative health research 2006; 16(5):679–691. [DOI] [PubMed] [Google Scholar]
- 24.Carr RL, Gramling LF. Stigma: a health barrier for women with HIV/AIDS. The Journal of the Association of Nurses in AIDS Care : JANAC 2004; 15(5):30–39. [DOI] [PubMed] [Google Scholar]
- 25.Grodensky CA, Golin CE, Jones C, Mamo M, Dennis AC, Abernethy MG, et al. “I should know better”: the roles of relationships, spirituality, disclosure, stigma, and shame for older women living with HIV seeking support in the South. The Journal of the Association of Nurses in AIDS Care : JANAC 2015; 26(1):12–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Turan B, Smith W, Cohen MH, Wilson TE, Adimora AA, Merenstein D, et al. Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: the mediating roles of social isolation and depression. Journal of acquired immune deficiency syndromes (1999) 2016; 72(2):198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clark HJ, Lindner G, Armistead L, Austin BJ. Stigma, disclosure, and psychological functioning among HIV-infected and non-infected African-American women. Women & health 2003; 38(4):57–71. [DOI] [PubMed] [Google Scholar]
- 28.Wingood GM, Diclemente RJ, Mikhail I, McCree DH, Davies SL, Hardin JW, et al. HIV discrimination and the health of women living with HIV. Women & health 2007; 46(2–3):99–112. [DOI] [PubMed] [Google Scholar]
- 29.Vyavaharkar M, Moneyham L, Corwin S, Saunders R, Annang L, Tavakoli A. Relationships between stigma, social support, and depression in HIV-infected African American women living in the rural Southeastern United States. Journal of the Association of Nurses in AIDS Care 2010; 21(2):144–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lipira L, Williams EC, Huh D, Kemp CG, Nevin PE, Greene P, et al. HIV-Related Stigma and Viral Suppression Among African-American Women: Exploring the Mediating Roles of Depression and ART Nonadherence. AIDS and behavior 2018:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rao D, Desmond M, Andrasik M, Rasberry T, Lambert N, Cohn SE, et al. Feasibility, acceptability, and preliminary efficacy of the unity workshop: an internalized stigma reduction intervention for African American women living with HIV. AIDS patient care and STDs 2012; 26(10):614–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rao D, Kemp CG, Huh D, Nevin PE, Turan J, Cohn SE, et al. Stigma reduction among African American women with HIV: UNITY Health Study. Jaids Journal of Acquired Immune Deficiency Syndromes 2018; 78(3):269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kerani RP, Kent JB, Sides T, Dennis G, Ibrahim AR, Cross H, et al. HIV among African-born persons in the United States: a hidden epidemic? JAIDS Journal of Acquired Immune Deficiency Syndromes 2008; 49(1):102–106. [DOI] [PubMed] [Google Scholar]
- 34.Koku EF. HIV-related stigma among African immigrants living with HIV/AIDS in USA. Sociological Research Online 2010; 15(3):1–14. [Google Scholar]
- 35.Ojikutu B, Nnaji C, Sithole J, Schneider KL, Higgins-Biddle M, Cranston K, et al. All black people are not alike: differences in HIV testing patterns, knowledge, and experience of stigma between US-born and non–US-born blacks in Massachusetts. AIDS patient care and STDs 2013; 27(1):45–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rose CE, Gardner L, Craw J, Girde S, Wawrzyniak AJ, Drainoni M-L, et al. A comparison of methods for analyzing viral load data in studies of HIV patients. PloS one 2015; 10(6):e0130090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rao D, Choi SW, Victorson D, Bode R, Peterman A, Heinemann A, et al. Measuring stigma across neurological conditions: the development of the stigma scale for chronic illness (SSCI). Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation 2009; 18(5):585–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rao D, Molina Y, Lambert N, Cohn SE. Assessing Stigma among African Americans Living with HIV. Stigma and health 2016; 1(3):146–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sherbourne CD, Stewart AL. The MOS social support survey. Social science & medicine 1991; 32(6):705–714. [DOI] [PubMed] [Google Scholar]
- 40.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of affective disorders 2009; 114(1–3):163–173. [DOI] [PubMed] [Google Scholar]
- 41.Center for quality assessment and improvement in mental health. The patient health questionnaire (PHQ-9) overview In: STABLE resource toolkit 1999. [Google Scholar]
- 42.Haubrich RH, Little SJ, Currier JS, Forthal DN, Kemper CA, Beall GN, et al. The value of patient-reported adherence to antiretroviral therapy in predicting virologic and immunologic response. Aids 1999; 13(9):1099–1107. [DOI] [PubMed] [Google Scholar]
- 43.Mundlak Y On the pooling of time series and cross section data. Econometrica: journal of the Econometric Society 1978:69–85. [Google Scholar]
- 44.Dieleman JL, Templin T. Random-effects, fixed-effects and the within-between specification for clustered data in observational health studies: A simulation study. PloS one 2014; 9(10):e110257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley & Sons; 2004. [Google Scholar]
- 46.King G, Tomz M, Wittenberg J. Making the most of statistical analyses: Improving interpretation and presentation. American journal of political science 2000:347–361. [Google Scholar]
- 47.Imai K, Keele L, Yamamoto T. Identification, inference and sensitivity analysis for causal mediation effects. Statistical science 2010:51–71. [Google Scholar]
- 48.R Core Team. R: A language and environment for statistical computing. In. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 49.Honaker J, King G, Blackwell M. Amelia II: A program for missing data. Journal of statistical software 2011; 45(7):1–47. [Google Scholar]
- 50.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R package for causal mediation analysis. 2017.
- 51.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS and Behavior 2013; 17(5):1785–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Earnshaw VA, Lang SM, Lippitt M, Jin H, Chaudoir SR. HIV stigma and physical health symptoms: Do social support, adaptive coping, and/or identity centrality act as resilience resources? AIDS and Behavior 2015; 19(1):41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kay ES, Rice WS, Crockett KB, Atkins GC, Batey DS, Turan B. Experienced Hiv-related Stigma in Health Care and Community Settings: Mediated Associations With Psychosocial and Health Outcomes. Jaids Journal of Acquired Immune Deficiency Syndromes 2018; 77(3):257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Leserman J Role of depression, stress, and trauma in HIV disease progression. Psychosomatic Medicine 2008; 70(5):539–545. [DOI] [PubMed] [Google Scholar]
- 55.Fletcher F, Ingram LA, Kerr J, Buchberg M, Bogdan-Lovis L, Philpott-Jones S. “She Told Them, Oh That Bitch Got AIDS”: Experiences of Multilevel HIV/AIDS-Related Stigma Among African American Women Living with HIV/AIDS in the South. AIDS patient care and STDs 2016; 30(7):349–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. Bmj 2009; 338:b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Neblett RC, Hutton HE, Lau B, McCaul ME, Moore RD, Chander G. Alcohol consumption among HIV-infected women: impact on time to antiretroviral therapy and survival. Journal of Women’s Health 2011; 20(2):279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Muthulingam D, Chin J, Hsu L, Scheer S, Schwarcz S. Disparities in engagement in care and viral suppression among persons with HIV. JAIDS Journal of Acquired Immune Deficiency Syndromes 2013; 63(1):112–119. [DOI] [PubMed] [Google Scholar]
- 59.Daniel RM, De Stavola BL, Cousens SN. gformula: Estimating causal effects in the presence of time-varying confounding or mediation using the g-computation formula. Stata Journal 2011; 11(4):479. [Google Scholar]
- 60.Arellano M, Bond S. Some tests of specification for panel data: Monte Carlo evidence and an application to employment equations. The review of economic studies 1991; 58(2):277–297. [Google Scholar]
- 61.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? Journal of health economics 2001; 20(4):461–494. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1 (Table): Complete model estimates for primary and sensitivity analyses