Significance Statement
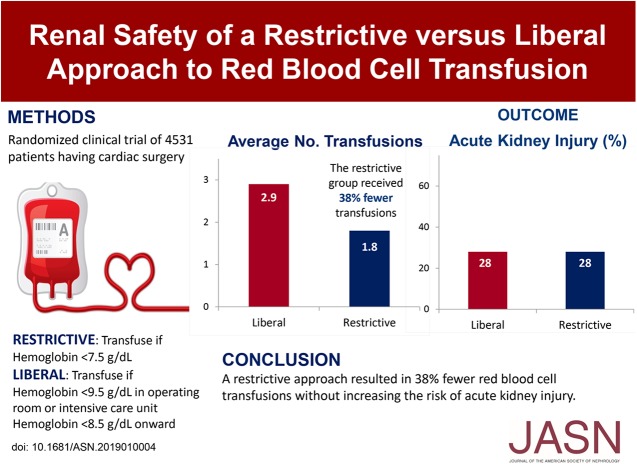
Safely reducing red blood cell transfusions could prevent transfusion-related adverse effects. Both anemia and transfusion may harm the kidney, but how reducing transfusions might affect AKI risk is unknown. To investigate this issue, the authors conducted a prespecified kidney substudy of a multinational, randomized noninferiority trial of 4531 patients undergoing cardiac surgery with cardiopulmonary bypass. Patients were randomized to a restrictive approach for receiving red blood cell transfusion (transfuse if hemoglobin<7.5 g/dl) or a more liberal approach (transfuse if hemoglobin<9.5 g/dl). Patients in the restrictive group received 38% fewer transfusions than patients in the liberal group (1.8 versus 2.9 transfusions, on average, respectively), and both approaches were equally safe with respect to AKI risk. Results were similar in patients with preoperative CKD.
Keywords: acute kidney injury, red blood cell transfusion, Cardiac surgery
Visual Abstract
Abstract
Background
Safely reducing red blood cell transfusions can prevent transfusion-related adverse effects, conserve the blood supply, and reduce health care costs. Both anemia and red blood cell transfusion are independently associated with AKI, but observational data are insufficient to determine whether a restrictive approach to transfusion can be used without increasing AKI risk.
Methods
In a prespecified kidney substudy of a randomized noninferiority trial, we compared a restrictive threshold for red blood cell transfusion (transfuse if hemoglobin<7.5 g/dl, intraoperatively and postoperatively) with a liberal threshold (transfuse if hemoglobin<9.5 g/dl in the operating room or intensive care unit, or if hemoglobin<8.5 g/dl on the nonintensive care ward). We studied 4531 patients undergoing cardiac surgery with cardiopulmonary bypass who had a moderate-to-high risk of perioperative death. The substudy’s primary outcome was AKI, defined as a postoperative increase in serum creatinine of ≥0.3 mg/dl within 48 hours of surgery, or ≥50% within 7 days of surgery.
Results
Patients in the restrictive-threshold group received significantly fewer transfusions than patients in the liberal-threshold group (1.8 versus 2.9 on average, or 38% fewer transfusions in the restricted-threshold group compared with the liberal-threshold group; P<0.001). AKI occurred in 27.7% of patients in the restrictive-threshold group (624 of 2251) and in 27.9% of patients in the liberal-threshold group (636 of 2280). Similarly, among patients with preoperative CKD, AKI occurred in 33.6% of patients in the restrictive-threshold group (258 of 767) and in 32.5% of patients in the liberal-threshold group (252 of 775).
Conclusions
Among patients undergoing cardiac surgery, a restrictive transfusion approach resulted in fewer red blood cell transfusions without increasing the risk of AKI.
Safely reducing exposure to red blood cell transfusion can prevent transfusion-related adverse effects, conserve the blood supply, and reduce costs.1–4 Untreated anemia, however, is also associated with adverse effects,5,6 particularly in patients having cardiac surgery who are susceptible to anemia-induced tissue hypoxia.7 Prompted by the need for better evidence on the safety of a lower hemoglobin threshold to trigger transfusion (a restrictive approach), the Transfusion Requirements in Cardiac Surgery–III (TRICS-III) trial was conducted to compare a restrictive approach with a liberal approach in patients having cardiac surgery with cardiopulmonary bypass who were estimated to have a moderate-to-high risk of perioperative death. This noninferiority trial found that a restrictive approach was as safe as a liberal approach with respect to a composite primary outcome of all-cause mortality, myocardial infarction, new focal neurologic deficit, and new kidney failure treated with dialysis.8 While there were small differences between groups with respect to the duration of mechanical ventilation, and the duration of stay in the intensive care unit and the hospital (described in the main report), most safety outcomes were similar between groups. Although approximately 1%–3% of patients who undergo cardiac surgery will develop acute kidney failure treated with dialysis, many more—>15%—will develop AKI,9–11 which is associated with longer hospital stays, higher health care costs, and death.12,13 Patients with CKD are particularly vulnerable to these outcomes.14–16 Both anemia and red blood cell transfusion are independently associated with AKI9,11,17–19 and it is impossible to know from observational data whether a restrictive approach to transfusion increases the risk of AKI.20
We conducted a prespecified21 kidney substudy of TRICS-III to determine whether a restrictive approach to red blood cell transfusion was noninferior to a liberal approach on the risk of AKI. This substudy was developed during the conduct of TRICS-III to better understand whether a restrictive approach to red blood cell transfusion can be used without increasing the risk of AKI, defined in several ways not reported in the primary TRICS-III report (including staging definitions of injury). We also wanted to know whether treatment effects were similar in several subgroups, including in patients with preoperative CKD and in those with a higher preoperative risk of developing severe postoperative AKI. We also wanted to understand the mean nadir hemoglobin for patients with and without CKD with a restrictive versus liberal approach to red blood cell transfusion, and the proportions transfused in each of the groups.
Methods
The TRICS-III Trial
TRICS-III (NCT02042898)—an open-label, randomized, controlled, noninferiority trial—compared a restrictive versus liberal approach to red blood cell transfusion in adults who had cardiac surgery with cardiopulmonary bypass. Trial methods and the primary outcome results are described elsewhere.8,22,23 Briefly, patients estimated to have a moderate-to-high risk of perioperative death (as defined by a preoperative score of 6 or more using the additive European System for Cardiac Operative Risk Evaluation I [EuroSCORE I]) underwent randomization at 73 centers in 19 countries between January of 2014 and March of 201722,24 (eligibility criteria are detailed in Supplemental Table 1). All participating centers obtained ethical approval to conduct the trial, and all participants were required to provide written, informed consent before enrollment.
TRICS-III AKI Substudy
The protocol and analytic plan for this substudy were prespecified and published previously,21 and the substudy received separate grant funding from the Kidney Foundation of Canada. Changes to the published protocol were minor and are summarized in Supplemental Table 2. Study reporting follows guidelines for randomized noninferiority trials (Supplemental Appendix).25
Substudy Eligibility Criteria
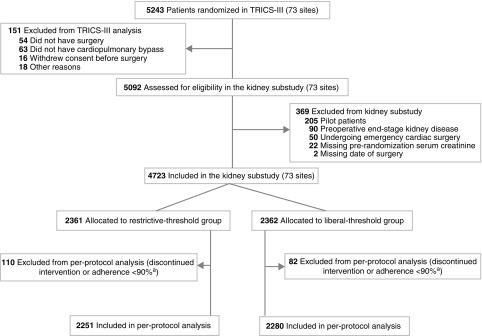
All 73 TRICS-III sites agreed to participate in this substudy and all patients enrolled in the main trial were assessed for eligibility in the substudy (205 patients in the pilot phase of the main trial were not included because no kidney function testing was done in these patients). Additional exclusion criteria (and rationale) for the kidney substudy were as follows (numbers excluded are shown in Figure 1):
Figure 1.
A total of 4723 patients were included in this substudy, and 4531 were included in the per-protocol analysis. aNonadherence to the assigned treatment was considered to have occurred if (1) a transfusion was given without a protocol-defined hemoglobin threshold being met, (2) a transfusion was not initiated after a threshold was met, or (3) a repeat hemoglobin value above the threshold was not documented within the protocol-defined time period. All other aspects of care were left to the discretion of attending clinicians.
1. Prerandomization ESKD, defined as receipt of dialysis, an eGFR<15 ml/min per 1.73 m2, or anuria or oliguria<10 ml/h (these patients were excluded because the assessment of AKI is less relevant).
2. Patients missing a value for the preoperative serum creatinine concentration or date of surgery (because both are needed to define AKI).
3. Patients having emergency cardiac surgery (because they frequently have AKI or other complications before surgery and so their preoperative serum creatinine may be unstable, and many die, either in the operating room or shortly thereafter, before postoperative AKI develops).
Trial Procedures
Details of the study design and intervention have been previously described.8,22 Briefly, patients were randomly assigned to a restrictive red blood cell transfusion strategy (transfuse if the hemoglobin level was <7.5 g/dl, starting from induction of anesthesia) or a liberal strategy (transfuse if the hemoglobin level was <9.5 g/dl in the operating room or the intensive care unit, or if the hemoglobin was <8.5 g/dl on the nonintensive care ward). Attending physicians followed the assigned transfusion protocol from induction of anesthesia until either hospital discharge or 28 days after surgery, whichever came first.
Patients were allocated in a 1:1 ratio with the use of a concealed, centralized, Web-based system, stratified according to center, with computer-generated random permuted blocks of varying sizes from two to six. Although it was not possible to blind patients or medical staff to the assigned transfusion strategy, patients were not actively informed of the allocated intervention, and outcome adjudicators were unaware of the intervention assignment.
Serum Creatinine Measurement
Preoperative serum creatinine was obtained within the 30-day period before surgery; the most recent value before surgery was used as the baseline value. The kidney substudy provided additional funding to participating sites to measure postoperative serum creatinine on days 1–3 and 5 after surgery, and also to record in the trial database any serum creatinine measures taken as part of routine care (recording both their value and their date of measurement).
Substudy Outcomes
The primary outcome of this substudy was perioperative AKI defined as an increase in postoperative serum creatinine (from the preoperative value) of 0.3 mg/dl or greater (≥26.5 μmol/L) within 48 hours of surgery, or an increase of 50% or greater within 7 days of surgery.26
Secondary Definitions of AKI
To examine whether the primary results were robust, five secondary definitions of AKI were examined:
1. A composite outcome of AKI (primary definition) or death within 5 days of surgery (to account for the potential effect of early deaths on outcome ascertainment).
2. AKI (primary definition) for at least 2 days within 7 days of surgery.
3. Stage 2 AKI (or higher), defined as a postoperative increase in serum creatinine of 100% or more from the preoperative value or an increase to an absolute value of 4.0 mg/dl or more (≥353.6 μmol/L) within 7 days of surgery, or receipt of dialysis within 30 days of surgery.
4. Stage 3 AKI, defined as a postoperative increase in serum creatinine of 200% or more from the preoperative value or an increase to an absolute value of 4.0 mg/dl or more (≥353.6 μmol/L) within 7 days of surgery, or receipt of dialysis within 30 days of surgery.
5. Receipt of dialysis within 30 days of surgery.
Sample Size
It was anticipated that at least 4000 patients enrolled in the main TRICS-III trial would be eligible for the kidney substudy, providing at least 85% power to detect noninferiority at a two-sided α of 0.05 with a margin of 3.5% for the absolute risk difference between the two groups, assuming an event rate of 15% and <2% missing postoperative creatinine data due to death.27,28
Statistical Analyses
The prespecified primary analysis was a per-protocol analysis that included all randomized patients who underwent surgery with cardiopulmonary bypass, except for those who had a protocol adherence of <90% (Figure 1), and those who were withdrawn from the trial by the treating physician at any time, or who withdrew consent. The unadjusted absolute risk difference was calculated as the rate of AKI in the restrictive group minus the rate of AKI in the liberal group. The 95% confidence interval (95% CI) for the absolute risk difference was calculated using the normal approximation for a difference in proportions. Noninferiority was accepted if the upper limit of the two-sided 95% CI for the risk difference was less than the noninferiority margin of 3.5% (i.e., if the risk of AKI was 15% with the liberal approach, the risk would be no higher than 18.5% with the restrictive approach). At least one postoperative serum creatinine measurement was available for 99.6% of patients; AKI was considered absent in the 18 patients with no available measurements (16 of 18 died within 1 day of surgery and none had dialysis within 30 days of surgery).
Four prespecified supporting analyses were conducted. First, a complete-case analysis was conducted that excluded 18 patients missing a postoperative serum creatinine value. Second, a mixed-effects logistic regression analysis was conducted that included center (randomization stratum) as a random effect and seven prespecified covariates assessed before surgery (defined in Supplemental Table 3). Third, an intention-to-treat noninferiority analysis was conducted, and, fourth, an intention-to-treat superiority analysis was conducted.
Several subgroup analyses were conducted to determine whether the effect of the transfusion strategy varied in different groups of patients. The subgroup analysis by preoperative CKD was prespecified (defined by a prerandomization eGFR<60 ml/min per 1.73 m2),21 and the remainder were post hoc exploratory analyses (subgroups defined by age, cardiopulmonary bypass time, surgery type, EuroSCORE I, and a preoperative score to predict the risk of severe postoperative AKI16). The absolute risk differences between intervention groups were examined for each subgroup, and the P values for the interaction terms were obtained from logistic regression models, without adjusting for other covariates. All analyses were conducted using SAS 9.2.
Results
Patient Enrollment and Baseline Characteristics
Enrollment in the main trial began on January 20, 2014; the last patient was randomized on March 20, 2017; and the last day of follow-up was April 29, 2017. The flow of patients from enrollment, allocation, follow-up, and analysis is shown in Figure 1. Of 5243 patients randomized in the TRICS-III trial, 5092 were assessed for eligibility in the kidney substudy, 4723 patients were enrolled, and 4531 were included in the per-protocol analysis (2251 in the restrictive-threshold group and 2280 in the liberal-threshold group). The median (interquartile range) time from randomization to surgery was 16.2 hours (1.5–30.6) in the restrictive group and 16.0 hours (1.4–30.4) in the liberal group.
Baseline characteristics of 4531 patients included in the per-protocol analysis are shown in Table 1 (characteristics of patients in the per-protocol analysis of the main TRICS III trial [n=4683] are shown in Supplemental Table 4). Patients had a mean (SD) age of 72 years (10) and 65% were men. The mean eGFR at baseline was 68 ml/min per 1.73 m2 (19) and 13% had an eGFR<45 ml/min per 1.73 m2. There were no clinically important differences between groups. Characteristics of patients in the intention-to-treat analysis (n=4723) are shown in Supplemental Table 5.
Table 1.
Baseline characteristics of patients in the TRICS-III kidney substudy (n=4531)
| Characteristic | Treatment Group | |
|---|---|---|
| Restrictive (n=2251) | Liberal (n=2280) | |
| Preoperative characteristics | ||
| Mean age (SD), year | 72 (10) | 72 (10) |
| Men, n (%) | 1437 (63.8) | 1487 (65.2) |
| Mean body mass index (SD), kg/m2a | 28 (5) | 28 (5) |
| Mean height (SD), cma | 168 (10) | 168 (10) |
| Mean weight (SD), kg | 79 (16) | 79 (17) |
| Race/ethnicity, n (%) | ||
| White | 2037 (90.5) | 2058 (90.3) |
| South Asian | 76 (3.4) | 82 (3.6) |
| East Asian | 33 (1.5) | 35 (1.5) |
| African descent | 17 (0.8) | 14 (0.6) |
| Other | 88 (3.9) | 91 (4.0) |
| Treated hypertension, n (%) | 1663 (73.9) | 1685 (73.9) |
| Mean systolic BP (SD), mm Hgb | 130 (20) | 131 (20) |
| Mean diastolic BP (SD), mm Hgb | 70 (11) | 71 (12) |
| Diabetes, n (%) | 582 (25.9) | 631 (27.7) |
| Diabetes requiring insulin, n (%) | 221 of 582 (38.0) | 230 of 631 (36.5) |
| Left ventricular function, n (%) | ||
| Good | 1387 of 2251 (61.6) | 1442 of 2278 (63.3) |
| Moderate | 670 of 2251 (29.8) | 654 of 2278 (28.7) |
| Poor | 150 of 2251 (6.7) | 145 of 2278 (6.4) |
| Very poor | 44 of 2251 (2.0) | 37 of 2278 (1.6) |
| Mean serum creatinine (SD), μmol/L | 94 (32) | 95 (34) |
| Mean eGFR (SD), ml/min per 1.73 m2c | 68 (19) | 68 (20) |
| eGFR categories, n (%)c | ||
| ≥60 ml/min per 1.73 m2 | 1484 (65.9) | 1505 (66.0) |
| 45–59 ml/min per 1.73 m2 | 475 (21.1) | 464 (20.4) |
| 30–44 ml/min per 1.73 m2 | 225 (10.0) | 223 (9.8) |
| 15–29 ml/min per 1.73 m2 | 67 (3.0) | 88 (3.9) |
| Mean hemoglobin (SD), g/dl | 13.2 (1.7) | 13.2 (1.7) |
| Previous cardiac surgery, n (%) | 287 (12.8) | 263 (11.5) |
| Aspirin use within 1 wk before surgery, n (%) | 1179 of 2249 (52.4) | 1211 of 2276 (53.2) |
| Operative characteristics | ||
| Type of surgery, n (%) | ||
| CABG only | 570 (25.3) | 590 (25.9) |
| CABG and valve surgery | 426 (18.9) | 439 (19.3) |
| CABG and other nonvalve surgery | 192 (8.5) | 191 (8.4) |
| Valve surgery only | 648 (28.8) | 681 (29.9) |
| Non-CABG surgery | 415 (18.4) | 379 (16.6) |
| Mean duration of cardiopulmonary bypass (SD), mind | 121 (59) | 121 (57) |
CABG, coronary artery bypass graft.
Data missing in 1 patient.
Systolic BP is missing in six patients. Diastolic BP is missing in seven participants.
eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation36: eGFR=141×min (Scr/κ, 1)α×max (Scr/κ, 1)−1.209×. Min, minimum; max, maximum 0.993Age×1.018 [if female]×1.159 [if black], where Scr is serum creatinine (mg/dl), κ=0.7 for females and 0.9 for males, α=−0.329 for females and −0.411 for males.
Duration of cardiopulmonary bypass is missing in one patient.
Hemoglobin Concentration and Number of Transfusions
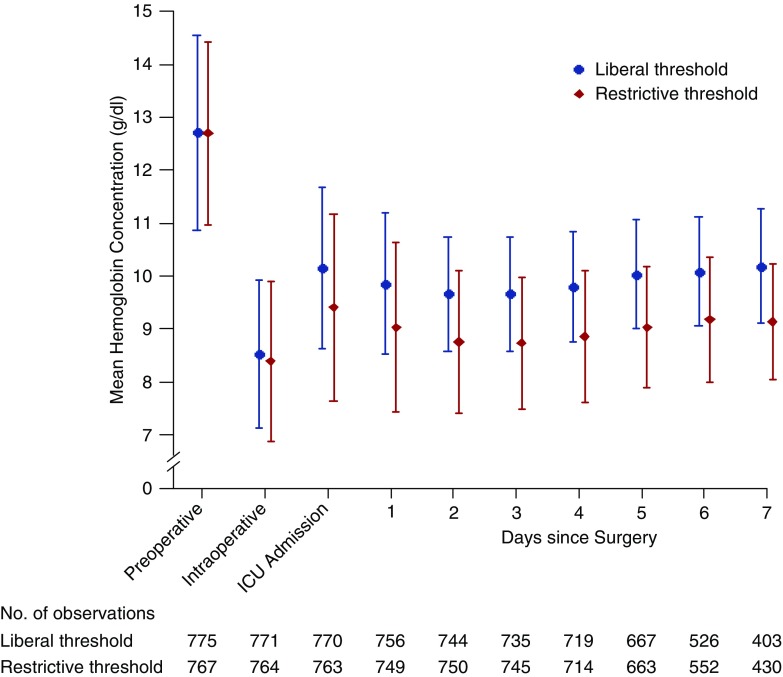
The mean hemoglobin concentration of patients at baseline was 13.2 g/dl (1.7). During the 7-day postoperative period, the mean nadir hemoglobin concentration was 8.1 g/dl (1.3) in the restrictive-threshold group and 8.7 g/dl (1.1) in the liberal-threshold group (Supplemental Figure 1). The mean difference (95% CI) between groups was −0.7 g/dl (−0.8 to −0.6) on postoperative day 1 and −0.8 g/dl (−0.8 to −0.7) on postoperative day 2. The mean between-group difference in patients with CKD is shown in Figure 2.
Figure 2.
During the 7-day post-operative period, the mean hemoglobin concentration in patients with CKD was approximately 1 g/dl lower in the restrictive-threshold group than the liberal-threshold group. ICU, intensive care unit.
On average, patients in the restrictive-threshold group received 38% fewer red blood cell transfusions than patients in the liberal-threshold group (1.8 [3.1] versus 2.9 [3.8], respectively; P<0.001), and similar results were seen in patients with CKD (2.1 [3.2] versus 3.4 [4.0], respectively; P<0.001). Overall, the proportion of patients transfused was 50.6% in the restrictive-threshold group and 71.8% in the liberal-threshold group (between-group difference, −21.2%; 95% CI, −24.0% to −18.4%). Differences in the number of red blood cells transfused are shown in Supplemental Table 6; 5.5% of patients in the restrictive-threshold received 5 or more units of red blood cells compared with 20.7% in the liberal-threshold group. In patients with CKD, 59.7% were transfused in the restrictive-threshold group and 77.6% in the liberal-threshold group (between-group difference, −17.8%; 95% CI, −22.4 to −13.3%), and 13.3% of patients in the restrictive-threshold received 5 or more units of red blood cells compared with 26.2% in the liberal-threshold group (Supplemental Table 7).
Effect of a Restrictive versus Liberal Approach to Red Blood Cell Transfusion on AKI
Perioperative AKI occurred in 624 of 2251 patients (27.7%) in the restrictive-threshold group and in 636 of 2280 patients (27.9%) in the liberal-threshold group; between-group difference, −0.2% (95% CI, −2.8% to 2.4%) (Table 2). The noninferiority of the restrictive transfusion approach was consistent across five alternative definitions of AKI (Table 2). Within 30 days of surgery, 54 of 2251 patients (2.4%) in the restrictive-threshold group were treated with dialysis compared with 65 of 2280 patients (2.9%) in the liberal-threshold group; between-group difference, −0.5% (95% CI, −1.4% to 0.5%).
Table 2.
Effect of a restrictive versus liberal approach to red blood cell transfusion on AKI in patients undergoing cardiac surgery (n=4531)
| AKI outcome definition | Number of Eventsa (%) | Risk Differenceb (95% CI) | |
|---|---|---|---|
| Restrictive (n=2251) | Liberal (n=2280) | ||
| Primary definition | |||
| AKIc | 624 (27.7) | 636 (27.9) | −0.2% (−2.8% to 2.4%) |
| Secondary definitions | |||
| AKI or deathd | 636 (28.3) | 662 (29.0) | −0.8% (−3.4% to 1.9%) |
| AKI for at least 2 de | 363 (16.1) | 354 (15.5) | 0.6% (−1.5% to 2.7%) |
| Stage 2 (or higher) AKIf | 166 (7.4) | 150 (6.6) | 0.8% (−0.7% to 2.3%) |
| Stage 3 AKIg | 75 (3.3) | 84 (3.7) | −0.4% (−1.4% to 0.7%) |
| Acute dialysis within 30 d of surgeryh | 54 (2.4) | 66 (2.9) | −0.5% (−1.4% to 0.4%) |
At least one postoperative serum creatinine assessment was available for 99.6% of patients. AKI was considered absent in 18 patients with no available assessments (five in the restrictive group and 13 in the liberal group); 16 of these 18 patients died within 1 d of surgery; none had dialysis within 30 d of surgery.
The unadjusted absolute risk difference was calculated as the proportion of patients with AKI in the restrictive group minus the proportion in the liberal group. A two-sided 95% CI for the risk difference was calculated using the normal approximation for the difference in proportions.
The primary outcome of the TRICS-III kidney substudy is perioperative AKI, defined as a postoperative increase in the serum creatinine concentration (from the preoperative value) of 0.3 mg/dl or more (≥26.5 μmol/L) within 48 h of surgery, or 50% or more within 7 d of surgery.
Met the primary definition of AKI or died within 5 d of surgery. This accounts for the potential effect of early deaths (38 of 2251 [1.7%] in the restrictive group; 52 of 2280 [2.3%] in the liberal group) on the ascertainment of AKI.
Defined as an increase in postoperative serum creatinine (from the preoperative value) of 0.3 mg/dl or more (≥26.5 μmol/L) within 48 h of surgery, or 50% or more within 7 d of surgery—on at least 2 d (not necessarily consecutive). This definition was examined because a longer duration of AKI is associated with worse outcomes.
Defined as an increase in postoperative serum creatinine of 100% or more from the preoperative value or an increase to an absolute value of 4.0 mg/dl or more (≥353.6 μmol/L) within 7 d of surgery, or receipt of dialysis within 30 d of surgery.
Defined as an increase in postoperative serum creatinine of 200% or more from the preoperative value or an increase to an absolute value of 4.0 mg/dl or more (≥353.6 μmol/L) within 7 d of surgery, or receipt of dialysis within 30 d of surgery.
This definition was examined as an indication of severe AKI. In patients who received dialysis, the median increase in the serum creatinine concentration from the preoperative value to the peak postoperative value was 1.1 mg/dl (interquartile range, 0.6–1.9) (99 μmol/L [interquartile range, 52–169]).
Supporting Analyses
The noninferiority of the restrictive transfusion approach was consistent in the four supporting analyses: the complete-case analysis (Supplemental Table 8), the adjusted analysis (Supplemental Table 9), the intention-to-treat noninferiority analysis (Supplemental Table 10), and the intention-to-treat superiority analysis (P values in Supplemental Table 10).
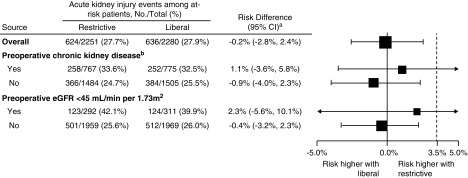
Subgroup Analyses
In the prespecified subgroup analysis of patients with CKD (Figure 3), AKI occurred in 258 of 767 patients (33.6%) in the restrictive-threshold group and in 252 of 775 patients (32.5%) in the liberal-threshold group; absolute risk difference, 1.1% (95% CI, −3.6% to 5.8%; P=0.48 for the interaction). Results were consistent when prerandomization eGFR was analyzed as a continuous variable (P=0.25 for the interaction between treatment and eGFR). No interactions with treatment were evident in additional exploratory subgroup analyses (Supplemental Table 11).
Figure 3.
A restrictive approach to red blood cell transfusion was noninferior to a liberal approach on the risk of AKI in patients with and without CKD.
Discussion
In this randomized clinical trial of 4531 higher-risk patients having cardiac surgery with cardiopulmonary bypass, a restrictive approach resulted in on average 38% fewer red blood cell transfusions and was noninferior to a liberal approach on the risk of AKI. Results were consistent across several different definitions of AKI and in the per-protocol and intention-to-treat analyses.
Nearly all patients who undergo cardiac surgery with cardiopulmonary bypass experience some degree of ischemia-reperfusion kidney injury.29,30 Whether patients recover from this insult without developing AKI or other sequelae depends on the severity and duration of kidney hypoxia, the ensuing inflammatory response, and on other factors including patient comorbidities.29 With the exception of the TRICS-III trial,8 previous cardiac trials comparing a restrictive versus liberal approach to transfusion have not been large enough to precisely define how the risk of AKI differs between the two approaches.1,31,32 The TRICS-III kidney substudy provides robust evidence that the risk of AKI is similar with a restrictive versus liberal approach to red blood cell transfusion. Effect estimates were derived from 4531 patients recruited from 73 centers across 19 countries. The pragmatic design of this randomized clinical trial and broad eligibility criteria mean that effect estimates are widely generalizable to patients with a moderate-to-high risk for perioperative death.
Preexisting CKD is one of the strongest risk factors for developing perioperative AKI.1–4 Patients with CKD often have anemia and are particularly vulnerable to superimposed AKI from vascular insufficiency, maladaptive repair mechanisms, and reduced nephron number.14,15 For these reasons, we conducted a prespecified subgroup analysis of patients with CKD. Although the smaller sample size (n=1542) means that this comparison had less precision than the primary comparison, results were consistent when prerandomization eGFR was analyzed as a continuous variable (P>0.05 for the interaction with treatment). These findings suggest that there may be little to no benefit of transfusing patients with CKD who have hemoglobin concentrations ≥7.5 g/dl. Given that both anemia and transfusion may be harmful to the kidneys (anemia via impaired tissue oxygen delivery and transfusion via free circulating hemoglobin and the other effects of stored blood), future research should focus on developing strategies that optimize hemostasis and maintain or increase a patient’s own red cell mass.
Limitations
This study has some limitations. First, patients and health care staff were not blinded to the assigned transfusion strategy. Although this increases the potential for ascertainment bias, the assigned groups had the same prespecified schedule of serum creatinine assessment, and outcome adjudicators were unaware of the group assignment. The number and timing of postoperative serum creatinine measurements were similar between groups (Supplemental Table 12). Second, the between-group difference on mean hemoglobin concentration was approximately 1 g/dl, which is smaller than the difference between the preset transfusion triggers in the restrictive and liberal arms (2 g/dl). Although a smaller than anticipated between-group separation is common in this type of trial,33–35 adherence in the per-protocol group was >90%, and the proportion of patients transfused was significantly lower in the restrictive group than the liberal group (51% versus 72%). Third, because all historic serum creatinine data predating the surgery were not available, it was not possible to exclude all patients with preoperative AKI; however, we did exclude patients having emergency surgeries because preoperative AKI is more likely to be present in these patients. Fourth, perioperative AKI as defined by biochemical criteria, although consistent with recent kidney clinical practice guidelines, is a surrogate end point that may not directly affect how a patient feels, functions, or survives. However, results were consistent for more severe outcomes, including stage 2 and 3 AKI and new-onset renal failure treated with dialysis. As well, in the main trial, the proportion of patients who received dialysis in the 6-month period after randomization was similar between groups: 3.9% in the restrictive group and 4.2% in the liberal group.23 Finally, the estimates for several subgroups and for severe AKI events were imprecise, and should be interpreted cautiously.
In higher-risk patients having cardiac surgery with cardiopulmonary bypass, a restrictive approach to red blood cell transfusion resulted in significantly fewer red blood cell transfusions and was as safe as a liberal approach on the risk of AKI. Results were consistent in patients with and without CKD.
Disclosures
Dr. Garg reports grants from the Kidney Foundation of Canada during the conduct of the study. Dr. Bagshaw reports grants and personal fees from Baxter Healthcare Corp, outside of the submitted work. Dr. Parikh reports personal fees from Genfit Biopharmaceutical Company, other from Renalytix AI, grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and grants from the National Heart, Lung and Blood Institute, outside of the submitted work. Dr. Shehata reports grants from the Canadian Institute for Health Research, other from the Canadian Institute for Health Research, and grants from Health Canada, during the conduct of the study, and is a Consultant for Canadian Blood Services. Dr. Verma reports grants and personal fees from Amgen, grants and personal fees from AstraZeneca, personal fees from Bayer, grants and personal fees from Boehringer-Ingelheim, grants from Bristol-Myers Squibb, personal fees from Eli Lilly, personal fees from Janssen, personal fees from Merck, personal fees from Novartis, personal fees from Novo Nordisk, and personal fees from Sanofi, outside of the submitted work. Dr. Mazer reports grants from the Canadian Institutes for Health Research during the conduct of the study; and grants from Quark, personal fees from Boehringer Ingelheim, personal fees from Amgen, and personal fees from Octapharma, outside of the submitted work.
FUNDING
The Transfusion Requirements in Cardiac Surgery–III (TRICS-III) kidney substudy was funded by the Kidney Foundation of Canada (KFOC180004). The main TRICS-III trial was funded by the Canadian Institutes of Health Research, the Canadian Blood Services–Health Canada (the Kenneth J. Fyke Award to Dr. Shehata), the National Health and Medical Research Council of Australia, and the Health Research Council of New Zealand. Dr. Garg was supported by the Dr. Adam Linton Chair in Kidney Health Analytics and a Canadian Institutes of Health Research Clinician Investigator Award, Dr. Sean M Bagshaw was supported by a Canada Research Chair in Critical Care Nephrology, and Dr. Parikh was supported by the National Institutes of Health (RO1HL085757).
Supplementary Material
Acknowledgments
An abstract of this work was presented as an oral presentation at the late-breaking clinical trial session at the American Society of Nephrology in 2018, which is available as a video on the American Society of Nephrology website: https://www.asn-online.org/education/kidneyweek/2018/webcast.aspx.
The funding sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Concept and design: All authors. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Dr. Garg, Dr. Sontrop, and Dr. Mazer. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Dr. Cuerden. Obtained funding: Dr. Garg and Dr. Mazer. All authors approved the final version of the manuscript, and all are accountable for all aspects of the submitted work.
The following list includes individuals in the TRICS Investigators and Perioperative Anesthesia Clinical Trials Group by country (# enrolled in TRICS III/TRICSII in parentheses):
Canada.
Centre Hospitalier Universitaire de Sherbrooke: É de Médicis*, MH Masse, J Marchand.
Foothills Medical Centre (308/48): A Gregory*, C MacAdams*, D Seal, A Ferland, I Ali, K Maier.
Hamilton Health Sciences Centre (530/19): R Whitlock, S Syed*, T Creary, L Tittley, J Spence*, I Jaffer, S Brodutch.
Institut Universitaire de Cardiologie et de Pneumologie de Québec (IUCPQ) (115/22): F Lellouche*, J Bussières*, F Dagenais, P Lizotte, N Gagné, H Tremblay, C Breton, P Bouchard.
London Health Sciences Centre (24/-): D Bainbridge, T Bentall.
Jewish General Hospital, McGill University (10/-): F Béïque, S Ramachandran.
Montreal Heart Institute (29/-): A Rochon, M Vervais, S Grenier.
St. Boniface Hospital (135/22): H Grocott*, H Kashani, E Ambrose, J McVagh.
St. Michael's Hospital (110/50): Mazer*, Hare*, Verma, C Crescini, S Yagnik, S Brodutch, A Slabiak, K Han.
Sunnybrook Health Sciences Centre (27/3): S Fremes, R Karkhanis.
University of Alberta (63/18): SM Bagshaw, N Baig, S Sidhu, R MacArthur, K Reid, S Boehnke.
University of Ottawa Heart Institute (36/13): C Hudson*, FD Rubens, D Winch.
Vancouver General Hospital (63/-): R Klein, R Grey.
Southlake Regional Health Centre (39/-): K Teoh, W Wiley, C Darby.
Kingston General Hospital (70/-): A Ho, T Saha*, D DuMerton Shore*, J Shelley.
Hôpital du Sacré-Coeur de Montréal (34/-): Y Lamarche, C Sirois.
St John Regional Hospital (31/-): CD Brown, C Dube, K Holden, L Roy, B Rolfe, S Brown.
Kelowna General Hospital (97/-): N Badner, R Saczkowski, W Senner.
Centre Hospitalier de l’Universite de Montreal (CHUM) (222/-): FM Carrier, N Noiseux, P Hebert, F Benettaib, A Ghamraoui, M Lebrasseur.
Toronto General Hospital/ UHN (12/-): WS Beattie*, J Carroll, H Poonawala.
Health Sciences Centre (Memorial University) (21/-): G Zbitnew, S Howells, R Mawhinney, S Sampson*, C Yegappan.
United States.
Durham VA Medical Center (8/-): R Schroeder, S Perfect, M Jones.
Montefiore Medical Center (19/-): J Leff, S Nair, KA Moncada, C Joco, M Harrison.
University of Texas Southwestern Medical Center (3/-): P Greilich, K Landgraf.
Maine Medical Center (13/-): RS Kramer, B Gallant.
Yale-New Haven Hospital (17/-): M Fontes, K Stavris.
Baylor Medical College (5/-): T Rosengart, Michael E. Debakey.
VA Medical Center (2/-): S Omer, K Coffey, E Broussard.
San Francisco VA Medical Center (12/-): E Tseng, MJ London, KM Stanley, L Casson, M Julien.
Australia.
Alfred Hospital (57/-): P Myles, S Wallace, W Galagher, A Ditoro.
Royal Melbourne Hospital (151/-): A Royse, C Royse, Z Williams, L Tivendale, N Dong.
Royal North Shore Hospital (22/-): S Judelman, J Leyden, E Yarad, M Doane, C Player.
St Vincent’s Hospital (Melbourne) (45/-): DA Scott, B Slater, P Corcoran.
Austin Health (Melbourne) (86/-): R Hu, S Sidiropoulos, S Baulch.
Cabrini Hospital (41/-): D Brewster, S Simpson.
Monash Health (68/-): J Smith, A Hulley.
Royal Adelaide Hospital (101/-): T Painter, L de Prinse.
Royal Prince Alfred (RPA) (20/-): P Bannon, L Turner, L Beattie.
Westmead Hospital (10/-): A Eslick, L Cope, B Sanderson.
Flinders Medical Centre (22/-): RA Baker, B Pesudovs, JS Bennetts.
Barwon Health (Melbourne) (6/-): D Dimovski, N Duggan, K Ives, C Yap.
New Zealand.
Waikato Hospital (201/-): K Byrne, G Mans, J Termaat.
Wellington Hospital (219/-): P Young, E Ridgeon, S Reddy, S Hurford, D Mackle, T Baker, A Hunt, R Cruz, Christchurch Hospital (23/-): S Henderson, J Mehrtens.
Auckland Hospital (186/-): S McGuinness, R Parke, E Gilder, K Cowdrey, J Dalton, M Butler, S Long, A Lammert, A Blakemore.
Dunedin Hospital (4/-): C Walker, D France, R Hutchison.
China.
Ren Ji Hospital (20/-): S Xue, J Gu.
Shanghai Yodak Cardiothoracic Hospital (19/-): X Chen, A Fan.
Malaysia.
Institut Jantung Negara (17/4): S Suraya, N Raja, I Yusnida, T Azura T Saibon, M Tze Bing.
Singapore.
National Heart Centre Singapore (NHCS) (15/-): NC Hwang, RS Tan, F Ang, TT Chin.
India.
S.A.L. Hospital (115/-): C Mehta, A Jain, P Sharma, R Shah, P Shaikh.
Narayana Hrudayalaya Hospitals (19/-): M Kanchi, A Sigamani, K Anusha.
Denmark.
Rigshospitalet– Copenhagen University Hospital (341/-): B Khanykin, P Johansson, T Anderson, L Olesen, N, Lilleør, S Rasmussen, A Fenger.
Germany.
Charité-Universitätsmedizin Berlin (2/-): S Treskatsch, V Mezger, E Falk, M Habicher.
Giessen Heart Centre (13/-): M Sander, F Edinger, C Koch, A Boening, I Oswald, S Bulat-Genc.
Switzerland.
University Hospital Basel (119/-): D Bolliger Seeberger, J Fassl, E Seeberger.
University Hospital Bern (Inselspital) (10/-): B Eberle, J Takala, M Stucki.
Spain.
Consorcio Hospital General de Valencia (40/-): E Mateo, J Moreno, T Gabaldon, I Cobo, JJ Peña, C Ferrer.
Instituto De Investigación Sanitaria La Fe (29/-): P Carmona, M. Lopez Cantero, A. Pajares, I Zarragoikoetxea.
Hospital de la Santa Creu i Sant Pau (81/-): J Galan, G Urrutia, MJ Martínez-Zapata, M Rivilla, V Cegarra, R Acosta-Isaac.
Ramón y Cajal (9/-): L Gajate-Martin, A Candela-Toha.
Greece.
University of Thessaly (97/-): GI Tagarakis, V Simopoulos, D Karangelis.
Romania.
Emergency Institute of Cardiovascular Diseases (52/-): D Filipescu, A Paunescu.
Egypt.
Tanta University Hospitals (56/-): H Fawzy, W Mawlana.
Israel.
Sheba Medical Center (12/-): S Preisman, E Raanani, D Kogan.
Tel Aviv Medical Centre (9/-): I Matot, A Cattan, H Artsi.
Brazil.
National Institute of Cardiology (16/-): C Galhardo, S Olival, R Toledo.
Colombia.
Fundación Cardioinfantil - Instituto de Cardiología (FCI) (167/-): JC Villar, E Hernandez, FR Montes, E Váquiro, C Garavito.
Fundación clínica SHAIO (FCS) (85/-): M Abello, E Váquiro.
Instituto de Corazón de Bucaramanga (ICB) (32/-): EJ Manrique, SM Vásquez, LA Aguilar.
Hospital de San José (16/-): M Coral, H Rodríguez.
Marly Clinic (Clinica Marly S.A) (83/-): JC Tellez, C Martinez.
South Africa.
University of KwaZulu-Natal (21/-): BM Biccard, CS Alphonsus.
TRICSII Only.
Virginia Commonwealth Medical Center (VCU) (0/3): BD Spiess.
*Indicates Perioperative Anesthesia Clinical Trials (PACT) Group Investigator, Other PACT investigators contributing to this study include R Hall, B Kent, A Denault, A Deschamps.
The study protocol and statistical analysis plan are available upon request from Amit.garg@lhsc.on.ca. Additional questions about the trial data can be directed to Dr. C. David Mazer mazerd@smh.ca.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
Group Information: The TRICS Investigators are listed at the end of this article.
Trial Registration: ClinicalTrials.gov Identifier: NCT02042898.
See related editorial, “Restricting Red-Cell Transfusions in Cardiac Surgery: No Increase in AKI,” on pages 1143–1144.
Contributor Information
for the TRICS Investigators and Perioperative Anesthesia Clinical Trials Group:
É de Médicis, A. Gregory, C. MacAdams, S. Syed, J. Spence, F. Lellouche, J. Bussières, H. Grocott, C.D. Mazer, G. Hare, C. Hudson, T. Saha, D. DuMerton Shore, W.S. Beattie, and S. Sampson
Supplemental Material
This article contains the following supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2019010004/-/DCSupplemental.
Supplemental Appendix. CONSORT – Checklist for Non-inferiority and Equivalence Trials.
Supplemental Table 1. TRICS-III patient eligibility criteria.
Supplemental Table 2. Justification of changes made to the published protocol of the TRICS-III kidney substudy.
Supplemental Table 3. Prespecified covariates assessed before surgery and used in adjusted analyses.
Supplemental Table 4. Baseline characteristics of patients in the per-protocol analyses of the TRICS-III main trial (nonpilot patients) (N=4683) and the kidney substudy (N=4531).
Supplemental Table 5. Baseline characteristics of patients in the per-protocol analysis (N=4531) and the intention-to-treat analysis of the kidney substudy (N=4723).
Supplemental Table 6. Number of units of red blood cells transfused (N=4531).
Supplemental Table 7. Number of units of red blood cells transfused in patients with CKD (N=1542).
Supplemental Table 8. Prespecified supporting analysis: Complete-case analysis. Effect of a restrictive versus liberal approach to red blood cell transfusion on AKI in patients undergoing cardiac surgery.
Supplemental Table 9. Prespecified supporting analysis: Adjusted analysis. Effect of a restrictive versus liberal approach to red blood cell transfusion on AKI in patients undergoing cardiac surgery (N=4531).
Supplemental Table 10. Prespecified supporting analysis: Intention-to-treat noninferiority analysis. Effect of a restrictive versus liberal approach to red blood cell transfusion on AKI in patients undergoing cardiac surgery (N=4723).
Supplemental Table 11. Post hoc subgroup analyses.
Supplemental Table 12. Number of daily postoperative serum creatinine measurements and day of measurement during the hospital stay in the per-protocol intervention groups.
Supplemental Figure 1. Mean nadir hemoglobin concentration from baseline to postoperative day 7 (N=4531).Supplemental Appendix. Guidelines for randomized noninferiority trials.
References
- 1.Carson JL, Stanworth SJ, Roubinian N, Fergusson DA, Triulzi D, Doree C, et al.: Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev 10: CD002042, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rohde JM, Dimcheff DE, Blumberg N, Saint S, Langa KM, Kuhn L, et al.: Health care-associated infection after red blood cell transfusion: A systematic review and meta-analysis. JAMA 311: 1317–1326, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vlaar APJ, Hofstra JJ, Determann RM, Veelo DP, Paulus F, Kulik W, et al.: The incidence, risk factors, and outcome of transfusion-related acute lung injury in a cohort of cardiac surgery patients: A prospective nested case-control study. Blood 117: 4218–4225, 2011 [DOI] [PubMed] [Google Scholar]
- 4.Delaney M, Wendel S, Bercovitz RS, Cid J, Cohn C, Dunbar NM, et al.: Biomedical Excellence for Safer Transfusion (BEST) Collaborative : Transfusion reactions: Prevention, diagnosis, and treatment. Lancet 388: 2825–2836, 2016 [DOI] [PubMed] [Google Scholar]
- 5.Miceli A, Romeo F, Glauber M, de Siena PM, Caputo M, Angelini GD: Preoperative anemia increases mortality and postoperative morbidity after cardiac surgery. J Cardiothorac Surg 9: 137, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loor G, Li L, Sabik JF 3rd, Rajeswaran J, Blackstone EH, Koch CG: Nadir hematocrit during cardiopulmonary bypass: End-organ dysfunction and mortality. J Thorac Cardiovasc Surg 144: 654–662.e4, 2012 [DOI] [PubMed] [Google Scholar]
- 7.Docherty AB, O’Donnell R, Brunskill S, Trivella M, Doree C, Holst L, et al.: Effect of restrictive versus liberal transfusion strategies on outcomes in patients with cardiovascular disease in a non-cardiac surgery setting: Systematic review and meta-analysis. BMJ 352: i1351, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mazer CD, Whitlock RP, Fergusson DA, Hall J, Belley-Cote E, Connolly K, et al.: TRICS Investigators and Perioperative Anesthesia Clinical Trials Group : Restrictive or liberal red-cell transfusion for cardiac surgery. N Engl J Med 377: 2133–2144, 2017 [DOI] [PubMed] [Google Scholar]
- 9.Thiele RH, Isbell JM, Rosner MH: AKI associated with cardiac surgery. Clin J Am Soc Nephrol 10: 500–514, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiers HD, van den Boogaard M, Schoenmakers MCJ, van der Hoeven JG, van Swieten HA, Heemskerk S, et al.: Comparison and clinical suitability of eight prediction models for cardiac surgery-related acute kidney injury. Nephrol Dial Transplant 28: 345–351, 2013 [DOI] [PubMed] [Google Scholar]
- 11.Rosner MH, Okusa MD: Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol 1: 19–32, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW: Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16: 3365–3370, 2005 [DOI] [PubMed] [Google Scholar]
- 13.Coca SG, Yusuf B, Shlipak MG, Garg AX, Parikh CR: Long-term risk of mortality and other adverse outcomes after acute kidney injury: A systematic review and meta-analysis. Am J Kidney Dis 53: 961–973, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McClellan W, Aronoff SL, Bolton WK, Hood S, Lorber DL, Tang KL, et al.: The prevalence of anemia in patients with chronic kidney disease. Curr Med Res Opin 20: 1501–1510, 2004 [DOI] [PubMed] [Google Scholar]
- 15.Chawla LS, Kimmel PL: Acute kidney injury and chronic kidney disease: An integrated clinical syndrome. Kidney Int 82: 516–524, 2012 [DOI] [PubMed] [Google Scholar]
- 16.Wijeysundera DN, Karkouti K, Dupuis JY, Rao V, Chan CT, Granton JT, et al.: Derivation and validation of a simplified predictive index for renal replacement therapy after cardiac surgery. JAMA 297: 1801–1809, 2007 [DOI] [PubMed] [Google Scholar]
- 17.Karkouti K, Wijeysundera DN, Yau TM, Callum JL, Cheng DC, Crowther M, et al.: Acute kidney injury after cardiac surgery: Focus on modifiable risk factors. Circulation 119: 495–502, 2009 [DOI] [PubMed] [Google Scholar]
- 18.Karkouti K: Transfusion and risk of acute kidney injury in cardiac surgery. Br J Anaesth 109[Suppl 1]: i29–i38, 2012 [DOI] [PubMed] [Google Scholar]
- 19.Khan UA, Coca SG, Hong K, Koyner JL, Garg AX, Passik CS, et al.: Blood transfusions are associated with urinary biomarkers of kidney injury in cardiac surgery. J Thorac Cardiovasc Surg 148: 726–732, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karkouti K, Grocott HP, Hall R, Jessen ME, Kruger C, Lerner AB, et al. : Interrelationship of preoperative anemia, intraoperative anemia, and red blood cell transfusion as potentially modifiable risk factors for acute kidney injury in cardiac surgery: A historical multicentre cohort study. Can J Anesth 62: 377–384, 2015 [DOI] [PubMed] [Google Scholar]
- 21.Garg AX, Shehata N, McGuinness S, Whitlock R, Fergusson D, Wald R, et al.: Risk of acute kidney injury in patients randomized to a restrictive versus liberal approach to red blood cell transfusion in cardiac surgery: A substudy protocol of the transfusion requirements in cardiac surgery III noninferiority trial. Can J Kidney Health Dis 5: 2054358117749532, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shehata N, Whitlock R, Fergusson DA, Thorpe KE, MacAdams C, Grocott HP, et al.: Transfusion Requirements in Cardiac Surgery III (TRICS III): Study design of a randomized controlled trial. J Cardiothorac Vasc Anesth 32: 121–129, 2018 [DOI] [PubMed] [Google Scholar]
- 23.Mazer CD, Whitlock RP, Fergusson DA, Belley-Cote E, Connolly K, Khanykin B, et al. : Six-month outcomes after restrictive or liberal transfusion for cardiac surgery. N Engl J Med 379: 1224–1233, 2018 [DOI] [PubMed] [Google Scholar]
- 24.Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al.: Risk factors and outcome in European cardiac surgery: Analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg 15: 816–822, discussion 822–823, 1999 [DOI] [PubMed] [Google Scholar]
- 25.Piaggio G, Elbourne DR, Pocock SJ, Evans SJW, Altman DG; CONSORT Group : Reporting of noninferiority and equivalence randomized trials: Extension of the CONSORT 2010 statement. JAMA 308: 2594–2604, 2012 [DOI] [PubMed] [Google Scholar]
- 26.KDIGO : Kidney disease: Improving Global Outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2: 1–138, 2012 [Google Scholar]
- 27.Garg AX, Devereaux PJ, Yusuf S, Cuerden MS, Parikh CR, Coca SG, et al.: CORONARY Investigators : Kidney function after off-pump or on-pump coronary artery bypass graft surgery: A randomized clinical trial. JAMA 311: 2191–2198, 2014 [DOI] [PubMed] [Google Scholar]
- 28.Parikh CR, Coca SG, Thiessen-Philbrook H, Shlipak MG, Koyner JL, Wang Z, et al.: TRIBE-AKI Consortium : Postoperative biomarkers predict acute kidney injury and poor outcomes after adult cardiac surgery. J Am Soc Nephrol 22: 1748–1757, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ho J, Lucy M, Krokhin O, Hayglass K, Pascoe E, Darroch G, et al.: Mass spectrometry-based proteomic analysis of urine in acute kidney injury following cardiopulmonary bypass: A nested case-control study. Am J Kidney Dis 53: 584–595, 2009 [DOI] [PubMed] [Google Scholar]
- 30.Mazzone AL, Baker RA, Gleadle JM: Mending a broken heart but breaking the kidney. Nephrology (Carlton) 21: 812–820, 2016 [DOI] [PubMed] [Google Scholar]
- 31.Curley GF, Shehata N, Mazer CD, Hare GMT, Friedrich JO: Transfusion triggers for guiding RBC transfusion for cardiovascular surgery: A systematic review and meta-analysis*. Crit Care Med 42: 2611–2624, 2014 [DOI] [PubMed] [Google Scholar]
- 32.Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, et al.: Clinical Transfusion Medicine Committee of the AABB : Red blood cell transfusion: A clinical practice guideline from the AABB*. Ann Intern Med 157: 49–58, 2012 [DOI] [PubMed] [Google Scholar]
- 33.Koch CG, Sessler DI, Mascha EJ, Sabik JF 3rd, Li L, Duncan AI, et al.: A randomized clinical trial of red blood cell transfusion triggers in cardiac surgery. Ann Thorac Surg 104: 1243–1250, 2017 [DOI] [PubMed] [Google Scholar]
- 34.Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA, Angelini GD, et al.: TITRe2 Investigators : Liberal or restrictive transfusion after cardiac surgery. N Engl J Med 372: 997–1008, 2015 [DOI] [PubMed] [Google Scholar]
- 35.Hajjar LA, Vincent J-L, Galas FRBG, Nakamura RE, Silva CM, Santos MH, et al.: Transfusion requirements after cardiac surgery: The TRACS randomized controlled trial. JAMA 304: 1559–1567, 2010 [DOI] [PubMed] [Google Scholar]
- 36.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al.: CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) : A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604–612, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.