Abstract
Study Objectives:
Patients with obstructive sleep apnea (OSA) have been shown to have high levels of inflammatory markers. Anti-inflammatory treatment with montelukast and intranasal steroids have demonstrated efficacy for mild OSA in children; this has not been fully evaluated in adults. This study investigated the response of mild OSA in adults to anti-inflammatory medical therapy.
Methods:
Adults aged ≥ 21 years with an apnea-hypopnea index (AHI) ≤ 15 events/h on polysomnography (PSG) were recruited to a prospective double-blind, randomized control trial. Patients were treated for 12 weeks with montelukast and fluticasone or placebo. All underwent a pretreatment and posttreatment PSG. Epworth Sleepiness Scale (ESS) score was obtained pretreatment and at 6 and 12 weeks posttreatment.
Results:
A total of 26 patients completed the study with 13 in each group. Mean age in the treatment and placebo groups were 58.3 ± 10.3 and 54.8 ± 14 years, respectively. There was no significant difference between groups reporting nasal congestion (P = .186), rhinitis (P = .666), or snoring (P = .177). There was no difference in the pretreatment ESS score (P = .077), body mass index (P = .173), or AHI (P = .535). The posttreatment PSG in the treatment group demonstrated a significant increase in total sleep time (P = .02) and percent of stage R sleep (P = .05). Neither group showed significant change in AHI. In patients in the treatment group, the 6- and 12-week follow-up ESS scores were not significantly different from pretreatment scores (P = .37–.46).
Conclusions:
Intranasal steroids and montelukast did not decrease AHI; however, total sleep time and percent of stage R sleep significantly increased. Self-reported improvement could be explained by observed changes in sleep parameters. Larger prospective studies could help elucidate the effects of medical therapy on adult patients with OSA.
Clinical Trial Registration:
Registry: ClinicalTrials.gov; Title: Montelukast and Nasa ICS for Treatment of Mild Obstructive Sleep Apnea in Adults; Identifier: NCT01089647; URL: https://clinicaltrials.gov/ct2/show/record/NCT01089647
Citation:
Smith DF, Sarber KM, Spiceland CP, Ishman SL, Augelli DM, Romaker AM. Effects of medical therapy on mild obstructive sleep apnea in adult patients. J Clin Sleep Med. 2019;15(7):979–983.
Keywords: fluticasone, medical treatment, mild obstructive sleep apnea, montelukast, sleep quality
BRIEF SUMMARY
Current Knowledge/Study Rationale: Montelukast and intranasal steroids have demonstrated efficacy in the treatment of mild obstructive sleep apnea (OSA) in the pediatric population. In adults with mild OSA and allergic rhinitis, a small randomized control trial did show a significant reduction in the apnea-hypopnea index (AHI) with intranasal corticosteroid treatment.
Study Impact: The aim of this study was to evaluate the response of mild OSA in adults to combined therapy with montelukast and intranasal steroids versus placebo. While we demonstrated no significant change in AHI, sleep quality was improved with increased total sleep time and percentage of sleep time spent in stage R sleep.
INTRODUCTION
Adults with mild obstructive sleep apnea (OSA) represent a growing proportion of patients with sleep apnea.1 Mild OSA (defined as an apnea-hypopnea index [AHI] ≥ 5 to < 15 events/h with comorbidities and/or correlated symptoms2) confers an increased risk of morbidity and has been found to affect sleep architecture and decrease self-reported sleep quality as well as quality of life measures.1,3 Several treatment modalities have been studied for mild OSA. Continuous positive airway pressure (CPAP) is the gold standard against which other treatments are measured. It is highly effective in reducing several cardiovascular risk factors, sleepiness, and improving attention and mood.4–6 However, in order for CPAP to be effective, patients must be adherent, and only approximately 50% of patients wear it during the entire sleep period.7,8 Other treatment options include weight loss, positional therapy, oral appliances, and surgery.
Mild OSA in children is defined as an AHI > 1 to ≤ 5 events/h.2 While adenotonsillar hypertrophy is generally thought of as the primary mechanism for OSA in children, persistent OSA has been found in 34% of children following adenotonsillectomy.9 Medication treatment with montelukast and intranasal steroids have demonstrated efficacy in the treatment of mild OSA in the pediatric population, both before and following adenotonsillectomy.10,11 This indicates that inflammation of the airway mucosa (not just tonsillar tissue) is also present in children, as it is in adults.12,13 This inflammatory process is hypothesized to lead to edema, upper airway dysfunction, and increased collapsibility.
Building on the hypothesis of airway inflammation, a small randomized control trial in adult patients with mild OSA and allergic rhinitis did show a significant reduction in the AHI with treatment of intranasal corticosteroids.14 The aim of this study was to evaluate the response of mild OSA in adults without respect to nasal complaints to combined therapy with montelukast and intranasal steroids versus placebo.
METHODS
Thirty-four consecutive patients were recruited from the sleep medicine clinic at St. Luke's Health System from February 2011 to June 2013. Inclusion criteria were adults aged ≥ 21 years found to have mild OSA, defined as an AHI ≤ 15 events/h, on a standard nocturnal polysomnography (PSG). We did not recruit patients specifically with nasal complaints, although a history was taken for problems with rhinitis, sinusitis, allergies, and nasal obstruction. Patients were excluded if they were taking any medication to treat nasal symptoms or allergies. The protocol used a randomized, double blind, placebo controlled design with treatment lasting 12 weeks. Patients were randomly assigned to receive either fluticasone by aqueous nasal spray (100 ug daily) and oral montelukast (10 mg daily), or a placebo pill, supplied by Astra-Zeneca (Wilmington, Delaware) and Merck (Kenilworth, New Jersey), respectively. The placebo spray was rebottled, labeled saline spray, and provided by the onsite pharmacy to match the deidentified, medicated spray bottle. All patients underwent PSG at the commencement of the study to establish baseline data. Each patient completed the Epworth Sleepiness Scale (ESS) questionnaire at baseline, then at 6 and 12 weeks after starting the study. A posttreatment PSG was obtained at the 12-week interval. The primary study endpoint was the change in AHI between sleep studies performed at the end of the medication or placebo treatment periods. Secondary endpoints were ESS scores, total sleep time (TST), sleep efficiency (SE), percent of TST spent in stage R sleep (%REM), stage R sleep AHI, and SpO2 saturation nadir compared among the same treatment periods.
St. Luke's Health System Internal Review Board approved the study and all patients gave written informed consent.
Polysomnography
PSG was performed using REMbrandt PSG software (version 9.1, Natus Medical, Pleasanton, California). Sleep studies were manually analyzed according to The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications version 2.0 by a single experienced technician who was blinded to the patient's identity and treatment status.15
Statistical Analysis
Demographic data between the groups were compared using a nonpaired t test. Homogeneity of variance was tested using Levene Test of Equality of Variances. Unique demographic and phenotypic characteristics predictive of adults with OSA were identified.
Linear regression was used to assess the relationship between changes in nasal congestion, rhinitis, snoring and phenotypic characteristics of OSA, and to assess the independent effects of potentially confounding variables including baseline characteristics. Between-group comparisons at follow-up were made using a stepwise multivariable logistic model. All analyses were performed using SPSS version 10.1 (SPSS Inc, Chicago, Illinois) by an independent statistician. All P values were 2-sided; P ≤ .05 was considered statistically significant.
RESULTS
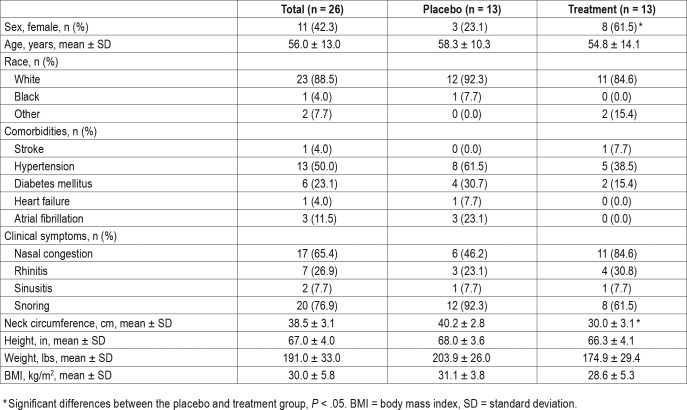
A total of 26 patients completed the study; 15 men and 11 women. There were 8 patients (4 from each arm) that enrolled but did not complete the study; 2 moved out of the area, 1 started CPAP, 1 started oral appliance therapy, 1 dropped out due to upcoming orthopedic surgery, 2 did not follow up, and 1 stopped due to epistaxis (treatment arm). Investigation showed no significant difference in sex, AHI or BMI in those lost to follow up versus those that completed the study. The mean age ± standard deviation of patients in the treatment and placebo groups were 58.3 ± 10.3 and 54.8 ± 14.1 years (P = .487), respectively. There were significantly more females in the treatment group, 8 versus 3 (P = .05). The neck circumference of the treatment group was also significantly smaller than that of the placebo group (P = .01). BMI between the two groups was similar; 28.6 ± 5.3 and 31.1 ± 3.8 kg/m2 (P = .173). There were no significant differences in the number of patients in each group reporting nasal congestion (P = .186), rhinitis (P = .666), or snoring (P = .177). There were no significant differences between comorbidities in each group: hypertension (P = .146), stroke (P = .35), type 2 diabetes mellitus (P = .304), history of fall (P = .307), or atrial fibrillation (P = .069). Table 1 lists the complete demographic data for the cohort.
Table 1.
Demographic details, symptoms, and comorbidities of the total study cohort and the placebo and treatment groups.
Severity of Sleep Apnea and Sleepiness
The mean AHI at baseline PSG in the treatment group was 8.3 ± 2.7 and 9.0 ± 3.2 events/h in the placebo group (P = .535). Similarly, there were no significant differences in baseline stage R sleep AHI or SpO2 nadir between the groups.
The mean AHI at the 12-week PSG was 11.5 ± 9.1 and 11.8 ± 13.4 events/h in treatment and placebo groups, respectively (P = .946). Similar stage R sleep AHI and SpO2 were recorded for both groups (Table 2).
Table 2.
Baseline and 12-week PSG data for placebo and treatment groups.
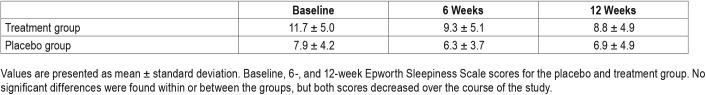
There were no significant changes between baseline and posttreatment measurements for AHI (P = .236), stage R sleep AHI, or SpO2 nadir between the treatment and placebo groups. Baseline ESS scores for the treatment and placebo group were 11.7 ± 5 and 7.9 ± 4.2, respectively (P = .08). There were no significant changes in ESS at the 6- or 12-week follow up between or within the two groups. See Table 3 for ESS results.
Table 3.
Epworth Sleepiness Scale scores.
A subanalysis was performed for patients who reported chronic rhinitis (n = 4) within the treatment group. The pretreatment and posttreatment AHI for those with rhinitis that received medical treatment was not significantly different than that of the entire treatment cohort (P = .358 and P = .352). The mean AHI in this subgroup actually worsened, from 8.25 events/h to 14.75 events/h. The baseline, 6- and 12-week follow-up ESS for patients with rhinitis who received medical therapy did not show a significant difference from the entire treatment group with respect to baseline ESS. There was no significant change in ESS during the study.
Objective Sleep Quality
Details of overnight sleep study parameters are given in Table 2. No significant changes were noted in sleep efficiency within the treatment group compared with placebo. Total sleep time increased significantly in the treatment group, from mean of 342.1 ± 75.23 to 400.27 ± 39.54 minutes (P = .021) with no significant change in the placebo group (P = .29). %REM also significantly increased in the treatment group, from 14.45 ± 7.2% to 20.77 ± 8.4% (P = .050). No significant changes in %REM were seen in the placebo group. No adverse events were reported during the study period, although there were 2 patients in the treatment group with mild epistaxis that spontaneously resolved and did not require pause or discontinuation of medication.
DISCUSSION
As previously stated, intranasal steroids and montelukast were found to be effective in children with mild persistent OSA after adenotonsillectomy.10 Gozal et al compared 22 healthy children to 14 controls in an open-label trial using intranasal budesonide and oral montelukast for 12 weeks.10 At the 16-week posttreatment PSG, AHI and SpO2 nadir significantly improved compared to no improvement in the placebo group. Apnea index improved by a mean of 1.8 events/h and obstructive AHI improved by a mean of 3.6 events/h. The mechanism by which the AHI was reduced was likely secondary to the anti-inflammatory effects of the medication on the upper airway, thereby suggesting that treatment is effective even in those without adenotonsillar hypertrophy.
In adults, this hypothesis was tested in a randomized, control trial in patients that specifically complained of nasal symptoms.14 Kiely et al investigated the effect of 4 weeks of intranasal fluticasone treatment versus placebo in 23 patients with complaints of seasonal or perennial rhinitis and OSA. They reported a significant decrease in AHI (median 6.5 events/h, 95% CI 29.5 to 1.8) in the 13 patients with OSA after intranasal corticosteroid treatment compared with placebo. Nasal steroid treatment did not improve self-reported sleep quality, sleep architecture, or oxygen saturation indices.
In an effort to expand the generalizability of this treatment in mild sleep disordered breathing, our study did not include criteria for nasal symptoms. Incidentally, there was an appreciable proportion of patients in our study in both arms with nasal and/or sinus complaints. Analysis of those patients in the treatment group (n = 4 out of 13) that complained of rhinitis was performed to evaluate if there was a larger change in AHI or ESS in this subgroup compared to the treatment group as a whole. We did not find this to be true; however, “rhinitis” was a “yes/no” answer in a questionnaire and was not further confirmed by evidence of aeroallergens or the relation of symptoms to sleep. This subgroup analysis consisting of only 4 patients was not powered to challenge the findings by Kiely et al.14 In fact, our findings support the idea that OSA has several phenotypic variants, with airway inflammation being one contributor while other anatomic abnormalities, neuromuscular control, central and peripheral respiratory control dysfunction contribute in variable amounts for each individual patient.16,17
In our study, combination medical therapy with montelukast and intranasal fluticasone did not reduce the AHI, although it did result in a demonstrable improvement in both TST and increase in %REM. This finding is consistent with the finding that surgical treatment of nasal airway obstruction improves sleep quality. Three published series of patients with OSA who underwent nasal surgery for nasal obstruction showed a significant increase in TST, sleep efficiency, and/or %REM.18–20 Although there was no significant effect on AHI, a meta-analysis evaluating the effect of nasal surgery for OSA found that ESS scores fell more significantly after treatment than could be explained by placebo effect.21 While the change in ESS did not reach significance in our study, there was a larger decrease in the treatment group than the placebo group (11.7 to 8.8 versus 7.9 to 6.9 events/h). Indeed, the treatment group mean ESS was in the sleepy range22 prior to treatment and below this threshold afterwards. In addition, this change is greater than the improvements reported in ESS for patients treated with CPAP therapy.23
We hypothesize that fluticasone and montelukast may improve nasal airflow and reduce nasal resistance which may in turn result in better sleep quality with longer sleep time and thus more stage R sleep. Increased %REM may explain why patients in the treatment group actually experienced a small increase in the mean AHI as mean %REM increased from 16.7% to 22.1% after treatment. Obstructive events are also known to increase in frequency during stage R sleep in most patients with OSA.24 However, the placebo group also showed a slight increase in the post-study AHI suggesting that this finding may reflect night to night variability known to occur in patients with mild OSA.25,26
Complications during this study were minor. In total, 3 of the 17 patients (17.7%) who received at least one dose of fluticasone nasal spray reported epistaxis. This is higher than the 6% to 7% rate of epistaxis reported by the manufacturer to the FDA. None of these patients were concurrently taking anti-platelet medications. All patients received the medication during the winter months, and all were over 60 years. Epistaxis does increase in incidence during cold months as well as with increasing age.27 The degree of epistaxis was not quantified, but 1 patient withdrew from the study secondary to this adverse event.
Limitations of this study include a small sample size. There is also known night to night variability of AHI on PSG and thus interpretation of the magnitude of change between baseline and 12-week interval may be overestimated or underestimated.28,29 This variability, however, would not have introduced bias between the treatment and the placebo group. Another limitation was the significant difference in sex between the two groups which likely accounts for the significant difference in neck circumference between the two groups. This may result in different pathophysiology between the placebo and active treatment arms; a factor which could be better assessed with larger sample size. Finally, the results of the study may not be generalizable to a more diverse population as the racial makeup of our cohort was primarily white.
Despite the limitations of our study, medical therapy may serve to improve sleep quality in adults with mild OSA. Larger randomized clinical trials will be necessary to confirm these results. Larger trial size will also allow to control for sex differences, difference races, and categories of BMI. A larger study could also analyze the effect of nasal complaints and objective nasal findings to evaluate the efficacy of anti-inflammatory medication on OSA.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. The work was funded in part by Astra Zeneca, Merck, and the senior author. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank James Wu, MD; Syed Nabi, MD; and Michael Bajkowski, RPSGT for their contributions to this manuscript.
ABBREVIATIONS
- %REM
percent of TST spent in stage R sleep
- AHI
apnea-hypopnea Index
- BMI
body mass index
- CI
confidence interval
- CPAP
continuous positive airway pressure
- ESS
Epworth Sleepiness Scale
- OSA
obstructive sleep apnea
- PSG
polysomnography
- REM
rapid eye movement
- SD
standard deviation
- SE
sleep efficiency
- TST
total sleep time
REFERENCES
- 1.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–1239. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3nd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 3.Smith PL, Gold AR, Meyers DA, Haponik EF, Bleecker ER. Weight loss in mildly to moderately obese patients with obstructive sleep apnea. Ann Intern Med. 1985;103(6 (Pt 1)):850–855. doi: 10.7326/0003-4819-103-6-850. [DOI] [PubMed] [Google Scholar]
- 4.Chowdhuri S, Quan SF, Almeida F, et al. An official American Thoracic Society research statement: impact of mild obstructive sleep apnea in adults. Am J Respir Crit Care Med. 2016;193(9):e37–e54. doi: 10.1164/rccm.201602-0361ST. [DOI] [PubMed] [Google Scholar]
- 5.Jackson ML, McEvoy RD, Banks S, Barnes M. Neurobehavioral impairment and CPAP treatment response in mild-moderate obstructive sleep apneas. J Clin Sleep Med. 2018;14(1):47–56. doi: 10.5664/jcsm.6878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ioachimescu OC, Anthony J, Constantin T, Ciavatta MM, McCarver K, Sweeney ME. VAMONOS (Veterans Affairs' Metabolism, Obstructed and Non-Obstructed Sleep) Study: effects of CPAP therapy on glucose metabolism in patients with obstructive sleep apnea. J Clin Sleep Med. 2017;13(3):455–466. doi: 10.5664/jcsm.6502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morgenthaler TI, Kapen S, Lee-Chiong T, et al. Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006;29(8):1031–1035. [PubMed] [Google Scholar]
- 8.Gay P, Weaver T, Loube D, Iber C. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29(3):381–401. doi: 10.1093/sleep/29.3.381. [DOI] [PubMed] [Google Scholar]
- 9.Friedman M, Wilson M, Lin HC, Chang HW. Updated systematic review of tonsillectomy and adenoidectomy for treatment of pediatric obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2009;140(6):800–808. doi: 10.1016/j.otohns.2009.01.043. [DOI] [PubMed] [Google Scholar]
- 10.Kheirandish L, Goldbart AD, Gozal D. Intranasal steroids and oral leukotriene modifier therapy in residual sleep-disordered breathing after tonsillectomy and adenoidectomy in children. Pediatrics. 2006;117(1):e61–e66. doi: 10.1542/peds.2005-0795. [DOI] [PubMed] [Google Scholar]
- 11.Goldbart AD, Greenberg-Dotan S, Tal A. Montelukast for children with obstructive sleep apnea: a double-blind, placebo-controlled study. Pediatrics. 2012;130(3):e575–e580. doi: 10.1542/peds.2012-0310. [DOI] [PubMed] [Google Scholar]
- 12.McNicholas WT. Obstructive sleep apnea and inflammation. Prog Cardiovasc Dis. 2009;51(5):392–399. doi: 10.1016/j.pcad.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Hatipoglu U, Rubinstein I. Inflammation and obstructive sleep apnea syndrome pathogenesis: a working hypothesis. Respiration. 2003;70(6):665–671. doi: 10.1159/000075218. [DOI] [PubMed] [Google Scholar]
- 14.Kiely JL, Nolan P, McNicholas WT. Intranasal corticosteroid therapy for obstructive sleep apnoea in patients with co-existing rhinitis. Thorax. 2004;59(1):50–55. [PMC free article] [PubMed] [Google Scholar]
- 15.Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eckert DJ, White DP, Jordan AS, Malhotra A, Wellman A. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med. 2013;188(8):996–1004. doi: 10.1164/rccm.201303-0448OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deacon-Diaz N, Malhotra A. Inherent vs. Induced loop gain abnormalities in obstructive sleep apnea. Front Neurol. 2018;9:896. doi: 10.3389/fneur.2018.00896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakata S, Noda A, Yasuma F, et al. Effects of nasal surgery on sleep quality in obstructive sleep apnea syndrome with nasal obstruction. Am J Rhinol. 2008;22(1):59–63. doi: 10.2500/ajr.2008.22.3120. [DOI] [PubMed] [Google Scholar]
- 19.Sériès F, St Pierre S, Carrier G. Surgical correction of nasal obstruction in the treatment of mild sleep apnoea: importance of cephalometry in predicting outcome. Thorax. 1993;48(4):360–363. doi: 10.1136/thx.48.4.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi JH, Kim EJ, Kim YS, et al. Effectiveness of nasal surgery alone on sleep quality, architecture, position, and sleep-disordered breathing in obstructive sleep apnea syndrome with nasal obstruction. Am J Rhinol Allergy. 2011;25(5):338–341. doi: 10.2500/ajra.2011.25.3654. [DOI] [PubMed] [Google Scholar]
- 21.Li HY, Wang PC, Chen YP, Lee LA, Fang TJ, Lin HC. Critical appraisal and meta-analysis of nasal surgery for obstructive sleep apnea. Am J Rhinol Allergy. 2011;25(1):45–49. doi: 10.2500/ajra.2011.25.3558. [DOI] [PubMed] [Google Scholar]
- 22.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 23.Giles TL, Lasserson TJ, Smith BJ, White J, Wright J, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006;25(1) doi: 10.1002/14651858.CD001106.pub2. 001106. [DOI] [PubMed] [Google Scholar]
- 24.Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 6th ed. Philadelphia, PA: Elsevier; 2017. [Google Scholar]
- 25.Meyer TJ, Eveloff SE, Kline LR, Millman RP. One negative polysomnogram does not exclude obstructive sleep apnea. Chest. 1993;103(3):756–760. doi: 10.1378/chest.103.3.756. [DOI] [PubMed] [Google Scholar]
- 26.White LH, Lyons OD, Yadollahi A, Ryan CM, Bradley TD. Night-to-night variability in obstructive sleep apnea severity: relationship to overnight rostral fluid shift. J Clin Sleep Med. 2015;11(2):149–156. doi: 10.5664/jcsm.4462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Purkey MR, Seeskin Z, Chandra R. Seasonal variation and predictors of epistaxis. Laryngoscope. 2014;124(9):2028–2033. doi: 10.1002/lary.24679. [DOI] [PubMed] [Google Scholar]
- 28.Prasad B, Usmani S, Steffen AD, et al. Short-term variability in apnea-hypopnea index during extended home portable monitoring. J Clin Sleep Med. 2016;12(6):855–863. doi: 10.5664/jcsm.5886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Punjabi NM, Aurora RN, Patil SP. Home sleep testing for obstructive sleep apnea: one night is enough! Chest. 2013;143(2):291–294. doi: 10.1378/chest.12-2699. [DOI] [PMC free article] [PubMed] [Google Scholar]