Abstract
Study Objectives:
To investigate the correlation between self-reported and objective measures of total sleep time (TST) in adults and examine whether sex, race/ethnicity, and weight status influence this association.
Methods:
Participants were individuals who screened for sleep intervention studies, providing > 7 days of wrist actigraphy sleep data (TSTobj) and reporting sleep duration (TSTPSQI) using the Pittsburgh Sleep Quality Index (PSQI) questionnaire (n = 53 men, 60 women; 59% minority/Hispanics; age 30.9 ± 9.7 years; body mass index 26.2 ± 3.2 kg/m2). In addition, TSTbed/wake was calculated as the difference between bedtime and waketime, minus the time to fall asleep, from the PSQI. Univariate regression analyses were performed to assess the relation between TSTobj and TSTPSQI and TSTbed/wake and compare the relation by sex, race, and ethnicity. Bland-Altman tests were done to assess bias by sex, race/ethnicity, weight status, and sleep quality.
Results:
TSTbed/wake correlated with TSTobj (r = .57, P < .0001). TSTPSQI and TSTbed/wake were greater than TSTobj (0.63 ± 0.99 hours and 0.79 ± 0.76 hours, respectively, both P < .0001). The difference between TSTPSQI and TSTobj did not vary by sex (β = .12, P = .52), race/ethnicity (β = .15, P = .48), age (β = −.01, P = .27), or body mass index (β = .04, P = .13) whereas that between TSTbed/wake and TSTobj varied by age (β = −.020, P = .0051), BMI (β = .054, P = .0021), race/ethnicity (β = .36, P = .021), and sleep efficiency (β = −.089, P < .0001).
Conclusions:
Calculating TST using self-reported bedtimes and wake times provided TST estimate that correlated with TSTobj but greater over-reporting occurred in younger and heavier individuals, non-whites or Hispanics, and those with low sleep efficiency. In clinical and research settings, asking individuals to report bedtimes, wake times, and length of time to fall asleep may more accurately estimate TST than asking about sleep duration alone.
Citation:
St-Onge MP, Campbell A, Salazar I, Pizinger T, Liao M, Aggarwal B. Information on bedtimes and wake times improves the relation between self-reported and objective assessments of sleep in adults. J Clin Sleep Med. 2019;15(7):1031–1036.
Keywords: actigraphy, Pittsburg Sleep Quality Index, sleep duration, subjective sleep
BRIEF SUMMARY
Current Knowledge/Study Rationale: Epidemiological studies utilizing self-reports to characterize total sleep time (TST) provide discordant information on the association between self-reported and objective TST. Some studies find weak or no correlations and bias in reporting of TST based on sex and body mass index, which may impact the relation between TST and chronic diseases.
Study Impact: Our study shows that calculating TST based on self-reported bedtime, wake time, and time to fall asleep provides an estimate of TST that is correlated to actigraphy-measured TST. These questions can be used in clinical settings to obtain information on sleep duration.
INTRODUCTION
Studies show discrepancy in the degree of agreement between self-reported and objective measures of total sleep time (TST). Lauderdale et al found a moderate correlation between self-reported and objective sleep measures but also a systematic over-estimation in TST that varied by other aspects of sleep (sleepiness, apnea risk, efficiency), race and weight status in black and white adults participating in the CARDIA study (n = 669).1 In 56 women with 7 nights of actigraphy-measured sleep, self-reported TST had poor agreement with objective measures.2 In that sample, those with the shortest self-reported TST tended to under-estimate sleep relative to objective measures whereas those with longer self-reported TST (≥ 8 h/night) tended to overestimate their sleep. Those studies, however, have not used the Pittsburgh Sleep Quality Index (PSQI) questionnaire to assess TST. More recently, Jack-owska et al noted no relation between sleep ratings reported by 119 women on the PSQI and sleep duration, efficiency, or latency measured by actigraphy.3 On the other hand, O'Brien et al, in a sample of 63 adults, reported a weak correlation between PSQI self-reported TST and objectively-measured TST, assessed by actigraphy.4 The average difference between the two measures was over 50 minutes. Those with a high global score on PSQI (> 5), indicative of poor sleep quality, had larger discrepancy between self-reported and objective TST, but age, sex, race, and body mass index (BMI) were not related to the discrepancy. Given the variability between studies in the relation between self-reported and objective sleep measures, it is important to determine the extent of agreement between those measures of sleep duration within specific cohort studies. This is particularly relevant since the PSQI was developed as a clinical tool to discriminate between good and poor sleepers, not specifically to assess sleep duration. In fact, in their validation study, Buysse et al noted that PSQI estimates of past month sleep duration and sleep efficiency were greater than those obtained in the laboratory, using polysomnography.5
Therefore, the goals of the present analyses were to (1) determine the difference between self-reported TST, obtained from the PSQI, and objective TST from actigraphy; (2) determine the relation between self-reported and objective TST; and (3) evaluate sources of bias in self-reported TST. Based on prior research, we expected self-reported TST to be over-estimated relative to actigraphy and that this may differ based on sleep quality and participant characteristics (age, sex, race/ethnicity, weight status).
METHODS
Participants were individuals who responded to advertisements and screened for different sleep research studies at Columbia University Irving Medical Center (CUIMC). Studies called for adult men and women, age 20 years and older, who habitually slept 7–9 h/night and had good self-reported sleep quality based on responses on the PSQI,5 no evidence of sleep-disordered breathing based on the Berlin Sleep Questionnaire,6 no history of depression based on the Beck Depression Inventory,7 and no history of drug or alcohol abuse, eating or sleeping disorders, psychiatric disorders, or chronic medical disorders. Study protocols were approved by the CUIMC Institutional Review Board and all participants provided informed consent prior to undergoing screening for these studies. The studies were registered at ClinicalTrials.gov (NCT02347020, NCT02960776, NCT02835261, NCT02770118).
Participants were first screened by telephone interview to obtain additional information about the research and determine potential eligibility. Those interested in participating in the research study and reported meeting some of the inclusion and exclusion criteria listed above were scheduled for an in-person screening. The consent form was reviewed with participants at the in-person screening and formal assessments of eligibility were performed. These measurements included body weight, height, and screening questionnaires, including PSQI. Participants who fulfilled those eligibility criteria were provided a wrist accelerometer (Actigraph GT3X+, ActiLife LLC, Pensacola, Florida) and sleep diary. Actigraphy data were verified after 7 days for adequacy of sleep. If TST was inadequate (average duration < 7 h/night or > 4 nights with < 7 hours of sleep), screening was stopped. If sleep duration seemed to be adequate, screening was continued for an additional 7 days to ensure a stable, average TST of ≥ 7 h/night. Participants in the present analyses were those who fulfilled study eligibility criteria based on weight, height, and questionnaires, and completed at least 7 days of wrist actigraphy. Participants included in the present analyses may have been disqualified for the research for which they were screening based on inadequate sleep during the 7 days of screening with actigraphy.
Outcome variables included three separate measures of TST: (1) TST as self-reported from the following question on the PSQI “During the past month, how many hours of actual sleep did you get that night? (This may be different from the number of hours you spend in bed) (TSTPSQI); (2) average TST from at least 7 nights of actigraphy (TSTobj); and (3) TST as calculated as the difference between self-reported bedtime and wake time, subtracting self-reported time to fall asleep information on the PSQI (TSTbed/wake = PSQI wake time – PSQI bedtime – time to fall asleep) using the following questions: “During the past month, when have you usually gone to bed? How long (in minutes) has it taken you to fall asleep each night? When have you usually gotten up in the morning?” We used paired t tests to compare the group mean differences between TSTobj and TSTbed/wake and between TSTobj and TSTPSQI. Pearson correlation coefficients were used to measure the degree of relation between TSTobj and TSTbed/wake, between TSTobj and TSTPSQI, between TSTobj and PSQI score, between TSTbed/wake and PSQI score, and between TSTPSQI and PSQI score. We examined if the associations between sleep duration assessment measures were modified by sleep quality (PSQI score and sleep efficiency by actigraphy), age, sex, race/ethnicity, and weight status (BMI) using generalized linear models. Bland-Altman plots and Lin concordance correlation coefficient were assessed to determine the degree of agreement between TSTobj and TSTbed/wake and between TSTobj and TSTPSQI. We also dichotomized each sleep time variable and then calculated Cohen kappa coefficient to measure inter-rater agreement for qualitative sleep time. Data are reported as mean ± standard deviation. Significance was determined at P < .05.
RESULTS
Complete data were obtained on 113 adults (n = 53 men and 60 women, Table 1). This was a multi-racial, multi-ethnic sample with 42 white, 25 black, 22 Asian, 2 multi-racial, and 12 participants from other racial backgrounds. Eighty-six participants were non-Hispanic, 18 were Hispanic, and 8 did not report their ethnic background. In this cohort, 34.5% of the participants slept ≤ 7 h/night when measured by actigraphy.
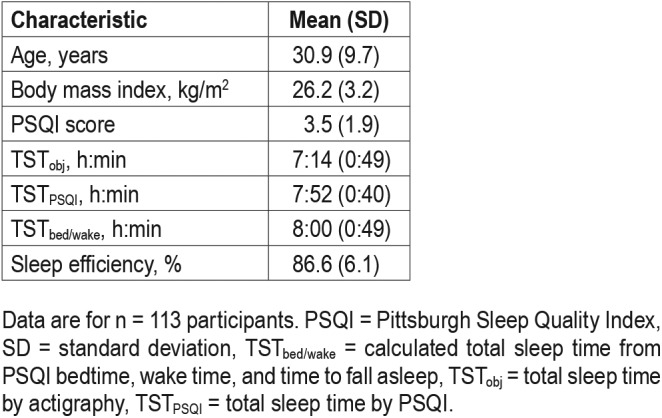
Table 1.
Participant characteristics and sleep duration.
However, 29.2% reported sleeping ≤ 7 h/night on the PSQI and only 4.4% when TST was calculated from bedtime and wake time. Objective sleep duration was not statistically significantly different between men (7.15 ± 0.89 hours) and women (7.29 ± 0.75 hours) (P = .37) or between whites (7.32 ± 0.97 hours) and non-whites (7.19 ± 0.74 hours) (P = .46). Similarly, TSTPSQI and TSTbed/wake were not statistically significantly different when compared between sexes (P = .89 and .24, respectively) or racial groups (P = .92 and .22, respectively). TSTobj and TSTbed/wake were not related to PSQI score (r = .14, P = .28 and r = .17, P = .20, respectively) but TSTPSQI was inversely correlated with PSQI score (r = −.54, P < .0001).
Average TSTPSQI was greater than TSTobj (0.63 ± 0.99 hours, P < .0001). In univariate regression analyses, the difference between TSTPSQI and TSTobj did not vary by sex (β = .12, P = .52), race/ethnicity (β = .15, P = .48), age (β = −.01, P = .27), or BMI (β = .04, P = .13). Overall, there was no correlation between TSTobj and TSTPSQI (r = .12, P = .218), which did not vary when sex was analyzed separately (men: r = .20, P = .15; women: r = .046, P = .73). Lin concordance test of correlation showed no correlation between TSTobj and TSTPSQI (r = .084, CI −.052, .216). In univariate regression analyses, the difference between TSTobj and TSTPSQI varied based on sleep efficiency (β = −.044, P = .0035) and PSQI score (β = −.157, P = .0010) with lower mis-reporting as sleep efficiency and PSQI score increased (Figure 1). There was no difference in reporting bias by sex (β = .120, P = .52), BMI (β = .042, P = .13), or race/ethnicity (β = .148, P = .48).
Figure 1. Fit plot for the difference between TSTobj and TSTPSQI.
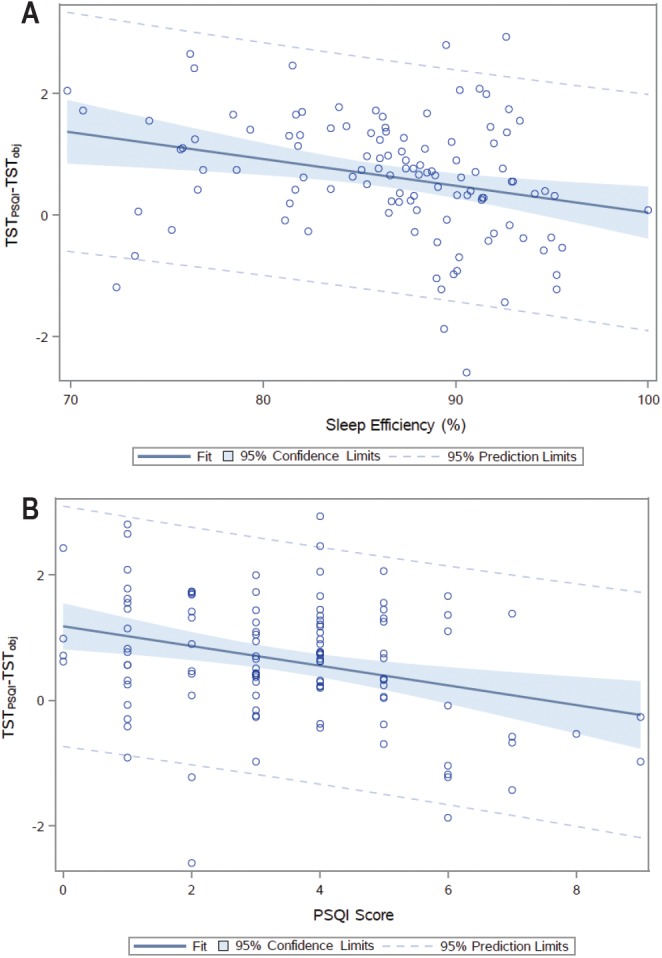
Fit plot for the difference between TSTobj and TSTPSQI as a function of (A) sleep efficiency and (B) global PSQI score. PSQI = Pittsburgh Sleep Quality Index, TSTobj = total sleep time by actigraphy, TSTPSQI = total sleep time by PSQI.
Interestingly, there were moderate and highly significant correlations between self-reported and objective assessments of bedtime (r = .44, P < .0001) and wake time (r = .31, P = .0007). We therefore examined differences and relations between TSTobj, TSTPSQI, and TSTbed/wake. As for TSTPSQI, average TSTbed/wake was greater than TSTobj (0.79 ± 0.76 hours, P < .0001). There was no difference between the two self-reported measures of TST (0.15 ± 1.06 hours, P = .13). There was no correlation between TSTPSQI and TSTbed/wake (r = −.019, P = .843). However, unlike TSTPSQI, this calculated self-reported sleep duration measure was correlated with TSTobj (r = .57, P < .0001); with strong correlation in women (r = .76, P < .0001) and moderate correlation in men (r = .36, P = .0082). There was concordance between TSTobj and TSTbed/wake (r = .387, CI .269, .492) (Figure 2). Similar to TSTPSQI, misreporting decreased as sleep efficiency increased (β = −.089, P < .0001). In this case, the difference between TSTbed/wake and TSTobj varied by age (β = −.020, P = .0051), BMI (β = .054, P = .0021), and race/ethnicity (β = .36, P = .021) (Figure 3) in such a way that misreporting was lower in older adults, leaner individuals, and whites.
Figure 2. Lin concordance correlation coefficient between TSTobj and TSTbed/wake and TSTPSQI.
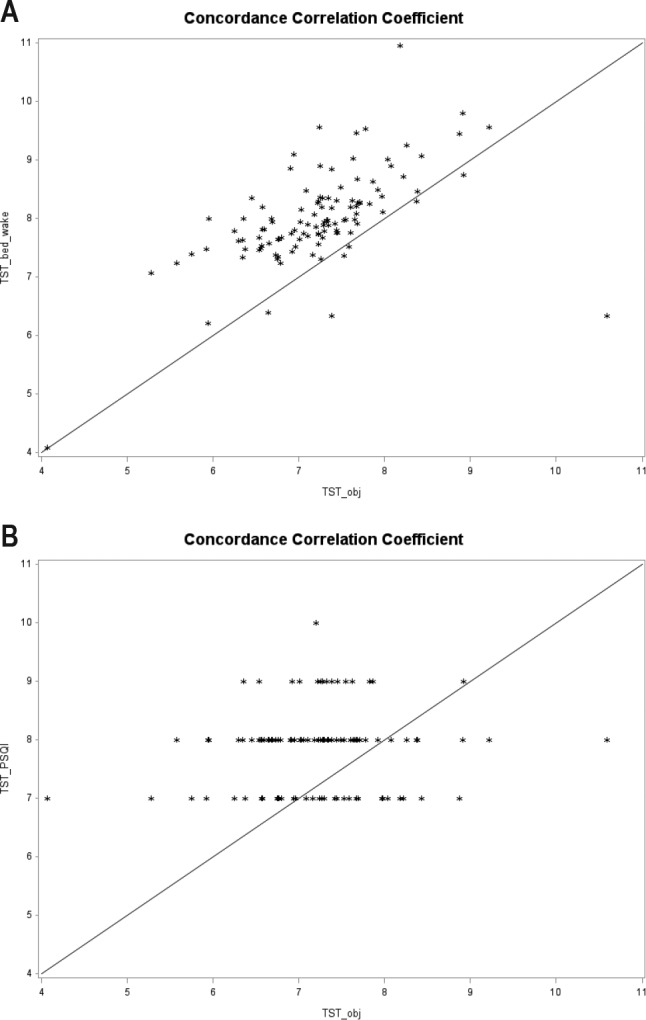
Lin concordance correlation coefficient between TSTobj and TSTbed/wake (A) and TSTobj and TSTPSQI (B). The line represents perfect concordance. Each data point is represented by an asterisk. PSQI = Pittsburgh Sleep Quality Index, TSTbed/wake = calculated total sleep time from PSQI bedtime, wake time, and time to fall asleep, TSTobj = total sleep time by actigraphy, TSTPSQI = total sleep time by PSQI.
Figure 3. Fit plot for the difference between TSTobj and TSTbed/wake.
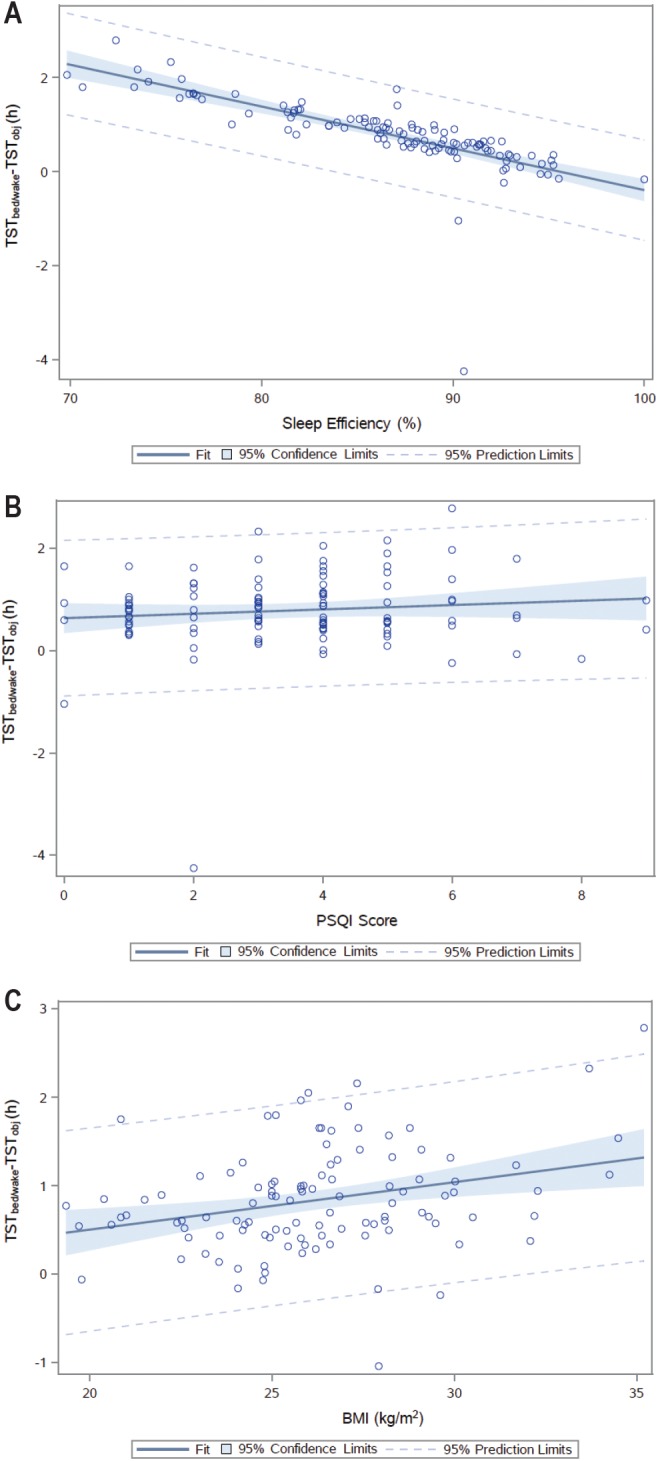
Fit plot for the difference between TSTobj and TSTbed/wake as a function of (A) sleep efficiency, (B) global PSQI score, and (C) BMI. BMI = body mass index, PSQI = Pittsburgh Sleep Quality Index, TSTbed/wake = calculated total sleep time from PSQI bedtime, wake time, and time to fall asleep, TSTobj = total sleep time by actigraphy.
Assessments of inter-rater agreement between TST measures showed poor agreement between TSTPSQI and TSTobj for participants sleeping ≤ 7 h/night versus > 7 h/night (kappa = .15, P = .12) and no agreement for those sleeping ≤ 8 h/night versus > 8 h/night (kappa = −.066, P = .48). No participants reported TSTPSQI of ≤ 6 h/night. We found fair agreement between TSTbed/wake and TSTobj for those sleeping ≤ 6 h/night versus > 6 h/night (kappa = .24, P < .00001) and for those sleeping ≤ 8 h/night versus > 8 h/night (kappa = .27, P < .00001) but no agreement for those sleeping ≤ 7 h/night versus > 7 h/night (kappa = .06, P = .22).
DISCUSSION
Our study shows that asking simple questions related to bedtime, wake time, and time to fall asleep provide a better estimate of TST than asking individuals to report their sleep duration over the past month. This calculated estimate of TST (TSTbed/wake), despite being significantly higher than actigraphy-measured TST, was correlated with objectively-measured sleep whereas the self-reported TST from the PSQI questionnaire (TSTPSQI) was higher by a similar amount than actigraphy-measured TST and only weakly and nonsignificantly correlated with TSTobj.
Our data show that, regardless of how sleep is assessed, self-reported recall of sleep duration overestimates objective measures. Average sleep duration, either by PSQI or calculated from bedtimes and wake times and time to fall asleep, was 38 and 46 minutes longer, respectively, than measured by actigraphy. This has important implications when establishing guidelines related to sleep duration recommendations associated with optimal health. Population studies often rely on self-reported sleep data. Our results highlight the need for objectively measuring sleep in health surveillance research. Several others have reported differences between self-reported sleep duration and actigraphy-measured sleep duration of 40 minutes to 1 hour.1,8,9 However, only TSTbed/wake was significantly correlated with TSTobj. Matthews et al reported similar findings whereby sleep duration, reported on PSQI and calculated from reported bedtimes and wake times and time to asleep, were longer than values obtained from actigraphy.10 As in the present analyses, they also report that TSTbed/wake and TSTobj were substantially associated whereas the correlation between TSTPSQI and TSTobj was moderate. Similar observations were reported by Jackowska and colleagues: TST from daily diaries was highly correlated with actigraphy-measured TST whereas self-reported TST from PSQI was not significantly correlated with objective measures.3
In our study population, the difference between TSTPSQI and TSTobj varied by sleep quality but not by demographic characteristics. Prior studies have reported that differences between self-reported TST from the PSQI questionnaire and objectively-measured TST from actigraphy varied by sex, with women's self-reported TST overestimating objective TST less than men.8,9 Others have also reported that age, insomnia and depression symptoms, and perceptions of overall health10 and demographics and health and sleep variables,1,8 modify the relation between self-reported and objective measures of TST. On the other hand, others have not found variability in degree of misreporting by BMI,4,9 race,4,11 or sex and age.4 In this study, TSTbed/wake and TSTobj discrepancy also differed by sleep efficiency but the difference between those two measures of TST was influenced by demographic factors (age, BMI, race/ ethnicity). We found two studies that used bedtimes, wake times, and time to fall asleep to estimate TST.8,10 In both studies, associations between TSTbed/wake and TSTobj differed by sleep quality (either presence/absence of insomnia symptoms or sleep efficiency and variability). In the study by Cespedes et al, associations also differed by sex, age, education.8
Most participants in our study tended to over-report their sleep duration, by an average of 36–46 minutes. A potential explanation for these findings is that participants genuinely do not know how much they sleep.1 Given the increased awareness campaigns surrounding “healthy sleep” and achieving 7–8 hours of sleep per night, it is possible that participants were compelled to state a sleep duration that was within the healthy range. However, this is unlikely since participants were genuinely healthy sleepers, with average sleep duration of 7 hours 14 minutes and range from 4 h/night to over 10 h/night. It is important to note that all participants included in these analyses were responding to recruitment advertisements specifically calling for “good sleepers” that also included information on monetary incentives associated with their potential participation in research. The influence of those financial incentives on the self-reported measures of TST cannot be ruled out. However, the degree of over-reporting noted herein are within the range of those observed in other studies so these factors likely had little influence on reporting bias.
The extent of over-reporting in our study was higher among racial/ethnic minorities and those with higher BMIs, both of whom are known to suffer from poorer sleep.12,13 It is possible that actigraphy may provide variable estimation of TST among populations with different movement and sleep patterns, such as those with poor sleep.14 There are few studies that have examined racial/ethnic differences in the correlation between self-reported and actigraphy-measured sleep duration.8 In the Hispanic Community Health Study/Study of Latinos Sueño Ancillary Study, Hispanics over-reported sleep duration by ∼ 67 minutes relative to actigraphy-measured sleep, when self-reported sleep was calculated as the difference between bedtimes and wake times, without considering time to fall asleep. There were no differences between subgroups of Hispanics (Cuban, Dominican, Mexican, Puerto Rican, Central American, or South American). If one considers normal sleep onset latency to range between 10 and 20 minutes, then the over-estimation of self-reported sleep duration in that study was similar to what we observed as TSTbed/wake (46 minutes).
Our study is limited by its small sample size (n = 113). However, this was a diverse sample of men and women (53% female, > 55% racial minorities), increasing the generaliz-ability of our results. Also, our sample is limited by the inclusion and exclusion criteria of the studies from which data were obtained. As a result, we had few participants over the age of 45 years (< 10%) and at the low and high range of BMI (< 23 and > 30 kg/m2). Given our findings that the difference between TSTbed/wake and TSTobj varied by age and BMI, confirmation in cohorts with a larger sample of older adults and adults with obesity is warranted. Because we specifically advertised for good sleepers in our recruitment efforts, few participants reported poor sleep quality (PSQI score > 5) or less than 7 hours of sleep. However, the mis-reporting of TST with the calculated estimate of TST (TSTbed/wake) did not vary by PSQI score. This may be a more stable estimate of TST to use over a range of sleep quality but needs validation in populations with poor self-reported sleep quality. Finally, shift workers and individuals with erratic work schedules or traveling across time zones, as well as those with sleep disorders, were excluded from our research and therefore our data only apply to healthy sleepers and regular, nighttime sleep. Studies that include individuals with non-daytime work or variable work schedules as well as individuals with sleep disorders should be done.
Our results show that despite being influenced by age, race/ethnicity, and BMI, a calculated estimate of TST, obtained from simple questions related to habitual bedtime, wake time, and time to fall asleep, has greater concordance with objectively-measured TST with actigraphy than a single question of “how many hours of actual sleep did you get” from the PSQI. It is possible that those behaviors tend to be most stable or easier for individuals to recall than providing an estimate of actual sleep duration. In any case, such questions about bedtimes can be easily included in research and clinical practice. In addition to providing a perhaps more reliable estimate of TST, these questions can also offer important information on the timing of lifestyle behaviors (eg, what time one goes to bed and wakes up) which are increasingly recognized as important for optimal health.15 These simple questions could offer an additional method for health care providers to accurately identify individuals at increased risk for negative health consequences as a result of inadequate sleep.
DISCLOSURE STATEMENT
All authors have read and approved the manuscript. The authors have no conflicts of interest to disclose. This research was funded in part by NIH R56HL119945 and R01HL128226 (St-Onge); AHA 16SFRN27950012 (St-Onge) and 16SFRN28060011 (Aggarwal). The authors have no conflict of interest to disclose.
ABBREVIATIONS
- BMI
body mass index
- CUIMC
Columbia University Irving Medical Center
- PSQI
Pittsburgh Sleep Quality Index
- TST
total sleep time
- TSTbed/wake
total sleep time calculated from bedtimes and wake times
- TSTobj
total sleep time by actigraphy
- TSTPSQI
total sleep time by PSQI
REFERENCES
- 1.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19(6):838–845. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Girschik J, Fritschi L, Heyworth J, Waters F. Validation of self-reported sleep against actigraphy. J Epidemiol. 2012;22(5):462–468. doi: 10.2188/jea.JE20120012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jackowska M, Ronaldson A, Brown J, Steptoe A. Biological and psychological correlates of self-reported and objective sleep measures. J Psychosom Res. 2016;84:52–55. doi: 10.1016/j.jpsychores.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 4.O'Brien E, Hart C, Wing RR. Discrepancies between self-reported usual sleep duration and objective measures of total sleep time in treatment-seeking overweight and obese individuals. Behav Sleep Med. 2016;14(5):539–549. doi: 10.1080/15402002.2015.1048447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 6.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131(7):485–491. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 7.Beck AT, Steer RA, Brown GK. BDI-II: Beck Depression Inventory Manual. 2nd ed. Boston, MA: Harcourt, Brace; 1996. [Google Scholar]
- 8.Cespedes EM, Hu FB, Redline S, et al. Comparison of self-reported sleep duration with actigraphy: results from the Hispanic Community Health Study/ Study of Latinos Sueno Ancillary Study. Am J Epidemiol. 2016;183(6):561–573. doi: 10.1093/aje/kwv251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mezick EJ, Wing RR, McCaffery JM. Associations of self-reported and actigraphy-assessed sleep characteristics with body mass index and waist circumference in adults: moderation by gender. Sleep Med. 2014;15(1):64–70. doi: 10.1016/j.sleep.2013.08.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matthews KA, Patel SR, Pantesco EJ, et al. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 2018;4(1):96–103. doi: 10.1016/j.sleh.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jackson CL, Patel SR, Jackson WB, 2nd, Lutsey PL, Redline S. Agreement between self-reported and objectively measured sleep duration among white, black, Hispanic, and Chinese adults in the United States: Multi-Ethnic Study of Atherosclerosis. Sleep. 2018;41(6) doi: 10.1093/sleep/zsy057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15(12):1456–1462. doi: 10.1016/j.sleep.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Jean-Louis G, Youngstedt S, Grandner M, et al. Unequal burden of sleep-related obesity among black and white Americans. Sleep Health. 2015;1(3):169–176. doi: 10.1016/j.sleh.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blackwell T, Redline S, Ancoli-Israel S, et al. Comparison of sleep parameters from actigraphy and polysomnography in older women: the SOF study. Sleep. 2008;31(2):283–291. doi: 10.1093/sleep/31.2.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.West AC, Bechtold DA. The cost of circadian desynchrony: evidence, insights and open questions. Bioessays. 2015;37(7):777–788. doi: 10.1002/bies.201400173. [DOI] [PMC free article] [PubMed] [Google Scholar]


