Abstract
Serum was analyzed from 146 healthy adult volunteers in eastern Africa to evaluate measles virus (MV) and canine distemper virus (CDV) neutralizing antibody (nAb) prevalence and potency. MV plaque reduction neutralization test (PRNT) results indicated that all sera were positive for MV nAbs. Furthermore, the 50% neutralizing dose (ND50) for the majority of sera corresponded to antibody titers induced by MV vaccination. CDV nAbs titers were low and generally were detected in sera with high MV nAb titers. A mutant CDV was generated that was less sensitive to neutralization by human serum. The mutant virus genome had 10 nucleotide substitutions, which coded for single amino acid substitutions in the fusion (F) and hemagglutinin (H) glycoproteins and two substitutions in the large polymerase (L) protein. The H substitution occurred in a conserved region involved in receptor interactions among morbilliviruses, implying that this region is a target for cross-reactive neutralizing antibodies.
Keywords: Canine distemper virus, Measles virus, Plaque reduction neutralization test, Neutralizing antibody, Hemagglutinin, Pre-existing immunity, Cross-neutralization
Introduction
Canine distemper virus (CDV) is a member of the Morbillivirus genus, which also includes measles virus (MV), rinderpest virus (RPV), peste des petits ruminants virus and morbilliviruses that infect aquatic mammals (Blixenkrone-Moller, 1993; Di Guardo et al., 2005). These related viruses generally each have a restricted natural host range. For example MV infects humans, RPV infects cattle and other even-toed ungulates, and CDV infects a variety of carnivorous animals. However, CDV infection has been observed in monkey colonies indicating that its host range can extend to primates (Qiu et al., 2011; Sakai et al., 2013a), but so far, there is no conclusive evidence linking CDV to human disease in spite of its speculative association to illness of unknown etiology (Rima and Duprex, 2006). Lab-adapted CDV has been injected into humans without causing symptoms of infection suggesting that humans are not a permissive host for the virus (Hoekenga et al., 1960), which is consistent with recent studies showing that mutations facilitating both entry and replication are needed for CDV to efficiently adapt to human cells (Otsuki et al., 2013; Sakai et al., 2013b). Prevalent MV immunity induced by universal vaccination or natural infections might also play a role in preventing CDV from crossing the human barrier (de Vries et al., 2014). Despite considerable characterization of antigenic and immunological relationships between CDV and MV (Haile et al., 1982; Orvell and Norrby, 1974, 1980; Stephenson and ter Meulen, 1979), CDV neutralizing antibodies (nAbs) in humans have not been extensively investigated.
Morbilliviruses are attractive candidates for development of replication-competent vectors because modified live vaccines (e.g. MV, CDV, and RPV) have proven to be very safe and efficacious (Buczkowski et al., 2014), and promising preclinical results have been generated with a number of experimental vectors (Brandler et al., 2007; Brandler and Tangy, 2008; Despres et al., 2005; Gauvrit et al., 2008; Guerbois et al., 2009; Miest and Cattaneo, 2014; Wang et al., 2012). Morbilliviruses seem particularly relevant for development of replication-competent AIDS vaccine vectors since this genera of viruses replicates in lymphoid tissues like HIV (Draper and Heeney, 2010; Koff et al., 2013; Parks et al., 2013). Pre-existing MV immunity may interfere with use of MV vectors, and unlike other viral vector systems in which rare serotype viruses can be used as vector alternatives (Mingozzi et al., 2013; Santra et al., 2009), MV has just one serotype. Thus, CDV has been considered as a MV alternative to minimize the effect of widespread anti-MV antibodies (Miest et al., 2011; Zhang et al., 2013b). Because antibodies specific to MV do cross-react with CDV (Appel et al., 1984; de Vries et al., 2014; Rima, 1983; Taylor et al., 1991), it is important to evaluate the prevalence and potency of CDV neutralizing activity in humans.
In this study, 146 serum samples collected from healthy adults in three eastern Africa countries were surveyed for both MV and CDV nAbs. We found that MV nAbs were prevalent in these samples while the frequency of samples with significant CDV nAb titers was low. Moreover, when CDV neutralizing activity was detected, it correlated with high anti-MV titers. We also used human anti-serum to derive an in vitro escape mutant CDV strain with increased resistance to neutralization. Genomic sequence analysis of the resistant strain revealed an amino acid substitution in a conserved region of the MV and CDV hemagglutinin (H) proteins that may help identify the domain recognized by cross-reactive nAbs and aide in future design H variants that are less sensitive to the effect of anti-vector immunity.
Results
MV nAbs in African serum samples
Serum was collected from 146 healthy adult male and female volunteers between 19 and 50 years of age (Table 1). The volunteers were participants in vaccine trial preparedness cohorts (Kamali et al., 2014) enrolled at 5 clinical research centers (CRCs) supported by IAVI in Kenya (Kilifi and Nairobi), Rwanda (Kigali), and Uganda (Masaka and Entebbe).
Table 1.
Demographic characteristics of volunteers involved in the study (n = 146). CRC: Clinical Research Center.
| CRC | Total | Volunteer sex | Volunteer age | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | ||||||||
| N | % | N | % | Median | Mean | Min | Max | ||
| Kigali | 30 | 14 | 46.7 | 16 | 53.3 | 27.5 | 30.2 | 20 | 50 |
| Masaka | 30 | 20 | 66.7 | 10 | 33.3 | 36.5 | 36.7 | 23 | 48 |
| Kilifi | 26 | 13 | 50.0 | 13 | 50.0 | 32.5 | 32.2 | 20 | 46 |
| Nairobi | 30 | 17 | 56.7 | 13 | 43.3 | 26.5 | 29.0 | 20 | 41 |
| Entebbe | 30 | 15 | 50.0 | 15 | 50.0 | 30.5 | 30.1 | 19 | 45 |
| Total | 146 | 79 | 54.1 | 67 | 45.9 | 32.0 | 31.6 | 19 | 50 |
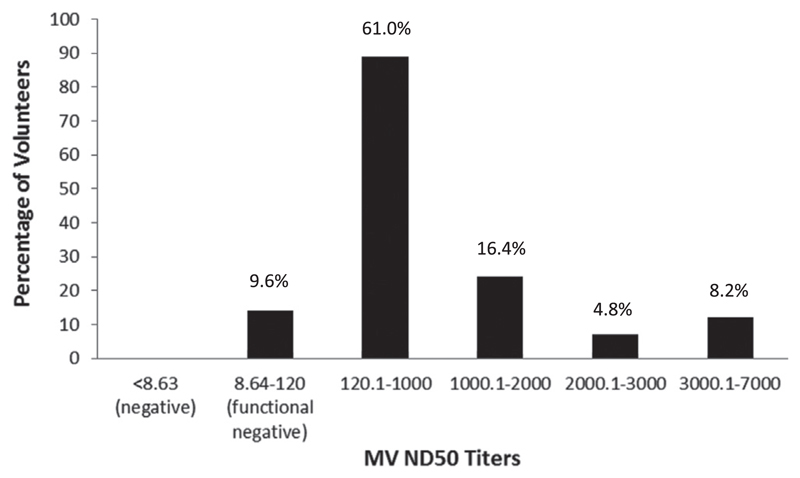
The threshold for MV nAb positivity was defined as average ND50 titer of naïve macaque serum plus 3 times standard deviation. When the PRNT was performed with the naïve macaque serum control, the threshold was calculated as 8.63. All serum samples from African volunteers were positive for MV nAbs since their titers were above this threshold (Fig. 1) and the ND50 values ranged from 16.0 to 6270. For comparison, serum analyzed from a monkey vaccinated with an MV vaccine had an ND50 value of 1446 and earlier studies in college students indicated that ND50 titers below 120 do not prevent measles (Chen et al., 1990). Overall, 77.4% of the African serum MV ND50 values fell between 120 and 2000, which is approximately equivalent to 300–5000 milli-International Units (mIU) of WHO international standard MV antibodies (Cohen et al., 2007). The 300–5000 mIU range is consistent with MV nAb levels induced by routine vaccination (Hussain et al., 2013; Leuridan et al., 2010), suggesting that these volunteers probably were vaccinated, although an MV vaccination history was not available to confirm this. Thirteen percent of the samples exhibited MV ND50 titers above 2000, which was indicative of a stronger response than typically observed after vaccination suggesting that some volunteers had contracted measles at some point (Leuridan et al., 2010). No significant difference in ND50 titers was observed across gender or age groups. Overall antibody titers were similar among the regions except for Nairobi where volunteers exhibited significantly lower titers than other regions (p = 0.01).
Fig. 1.
Distribution of MV nAb titers. Negative threshold was defined as the average nAb titer of unvaccinated monkey serum plus 3 × standard deviation. Functional negative threshold was ND50 titers 120 since MV ND50 titer slower than that do not prevent measles (Chen et al., 1990). For the 146 volunteers, 90.4% had MV titers higher than 120 and majority of the titers were in ranges of 120.1–1000(61.0%) and 1000–2000 (16.4%), which correspond to MV antibodies induced by vaccinations (Hussain et al., 2013; Leuridan et al., 2010).
Generally low CDV nAbs titers in African serum samples and their correlation with the magnitude of MV nAbs
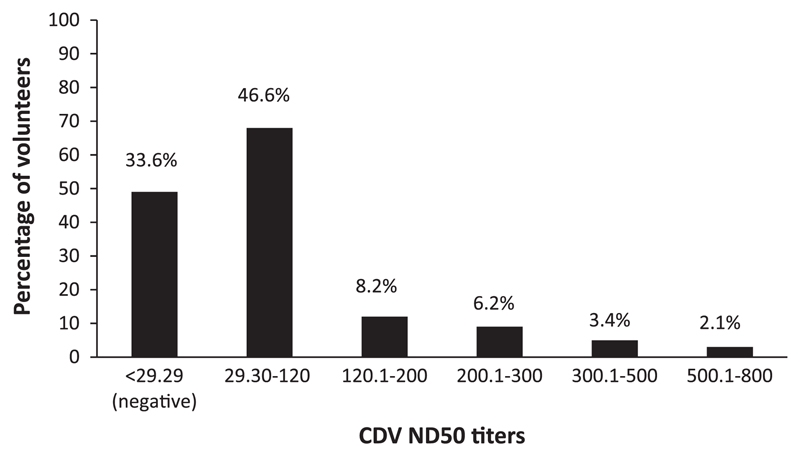
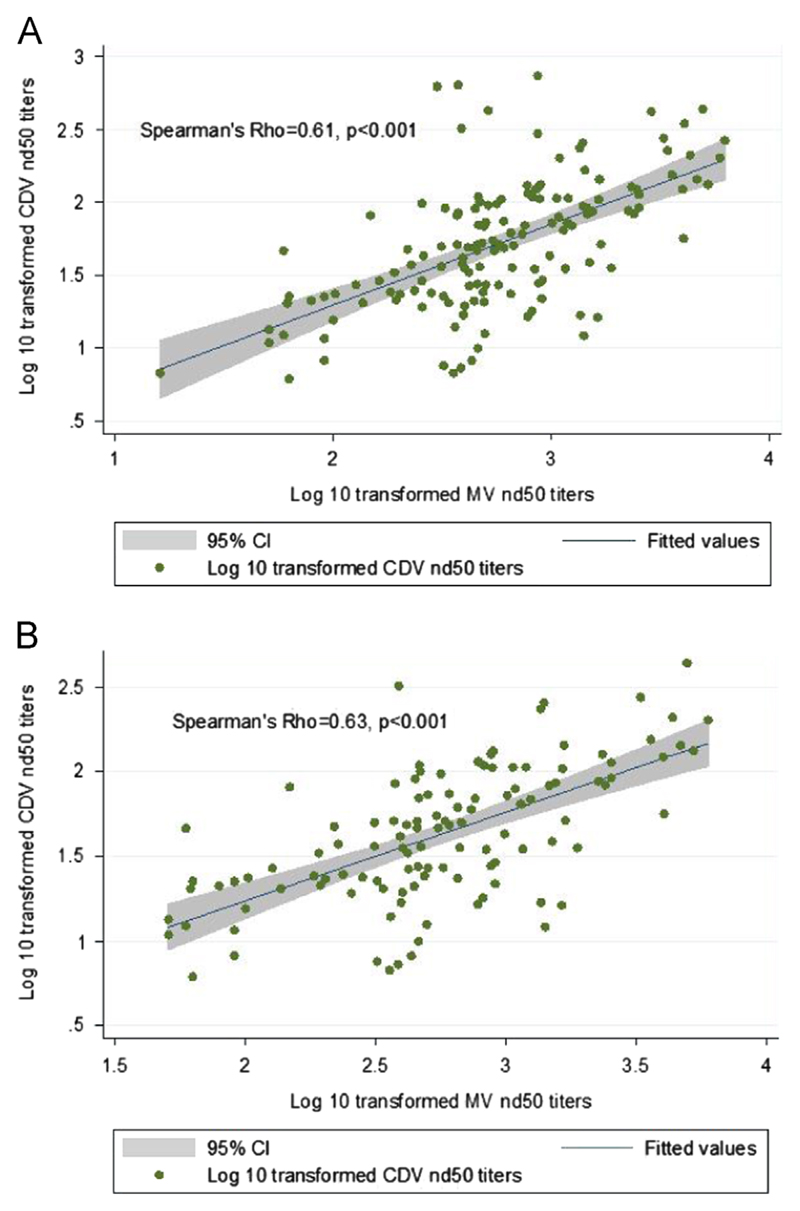
When the CDV PRNT was performed with naïve ferret serum, the average CDV ND50 titer plus 3 times standard deviation was determined to be 29.29, which we employed as our threshold for positivity. Based on this, approximately 33.6% of the African volunteer serum samples were negative. ND50 titers in 46.6% of the volunteers were between 29.3 and 120 (Fig. 2) and the remaining 19.8% had CDV ND50 titers above 120 but below 800. For comparison, serum from a ferret recently vaccinated with live-attenuated CDV was 33,551. Similar to MV nAbs, CDV ND50 titers were not significantly different across gender. With the exception of the volunteers from the Masaka CRC where higher CDV nAbs (p < 0.001) were detected, no significant difference was observed for the other geographical regions. Although the CDV nAb titers overall were low, positive CDV nAb values generally correlated with higher magnitude MV titers (Fig. 3A, Spearman's ρ= 0.61, p < 0.001). This relationship persisted when the correlation analyses were performed using nAb data that were stratified by volunteer enrollment site, gender, and age. Notably, the correlation did not significantly change when the analysis was performed without including data points from Masaka CRC in which the volunteers had higher CDV nAb titers (Fig. 3B, Spearman's ρ = 0.63, p < 0.001). This indicated that the correlation relationship between CDV and MV nAbs was general and was not due to this individual CRC. Given the lack of epidemiologic evidence to support frequent infection of CDV in humans, this result suggests that CDV neutralization is due to cross-neutralizing MV antibodies, which are present in low quantities and are detectable with the CDV PRNT only in volunteers with relatively high MV ND50 titers.
Fig. 2.
Distribution of CDV nAb titers. Negative threshold was defined as the average ND50 titer of unvaccinated ferret serum plus 3 × standard deviation. Total 80.2% of the volunteers had CDV ND50 titers either below the negative threshold or in 29.30–120 range.
Fig. 3.
Strong correlation was found between MV and CDV nAb using Spearman's rank correlation analysis. (A) Correlation statistics from analyzing MV and CDV nAb titers of all 146 volunteers (Spearman's coefficient ρ=0.61, p < 0.001) suggest that CDV neutralization is due to cross-reactive MV nAbs that are present at low quantities in the volunteers who had relatively high MV nAb titers. Relationship between log 10 transformed MV and CDV ND50 titers is shown by the fitted line. The shaded area represented 95% confidence interval of the fitted values. (B) Analysis of the nAb values from the remaining 116 volunteers after excluding data points of Masaka CRC still showed a strong correlation between the MV and CDV nAb titers (Spearman's coefficient ρ=0.63, p < 0.001) and thus indicated that the observed correlation was general and was not due to the individual CRC in which the volunteers had relatively high level of CDV nAbs.
A mutant CDV was generated that was more resistant to neutralization by human serum
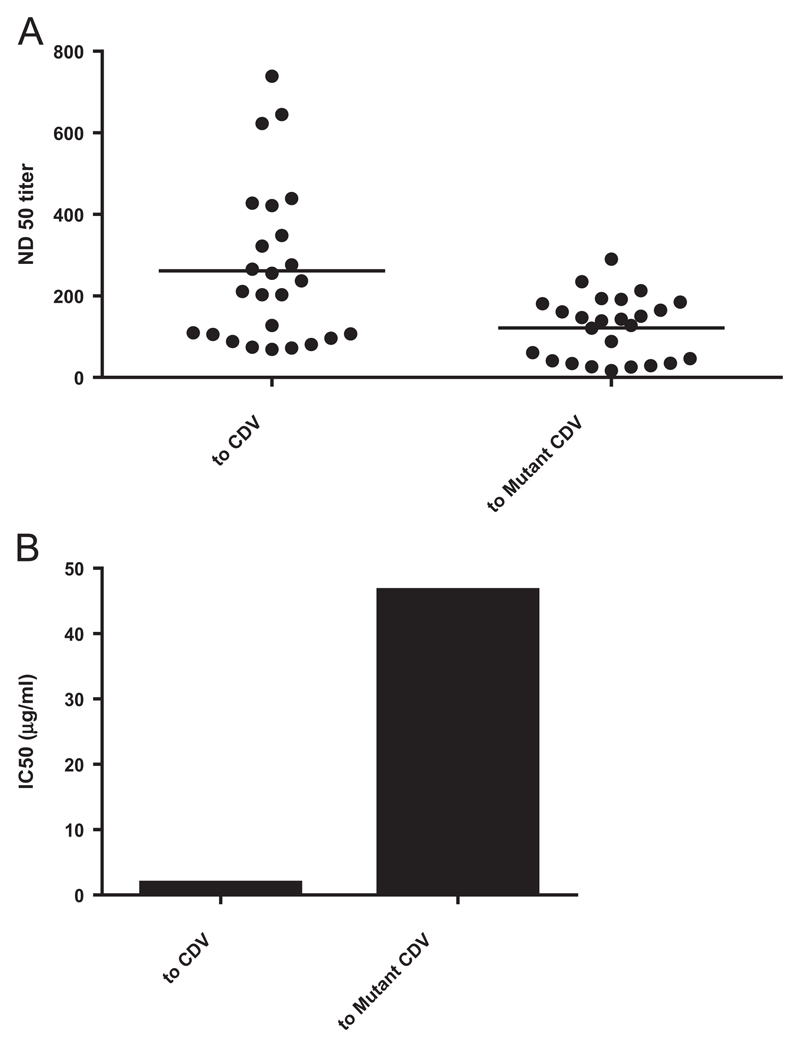
To better understand the molecular basis of the cross-neutralization, a neutralization-resistant CDV mutant was isolated and its genomic nucleotide sequence determined. The neutralization-resistant CDV mutant was selected using a single healthy adult donor serum of American origin that was available from a commercial source and had detectable CDV and MV nAbs. The neutralization-resistant CDV mutant grew in Vero cells with similar kinetics as the progenitor virus (data not shown) indicating that the escape mutation(s) had a little effect on replication in culture. When the mutant was analyzed with the CDV PRNT using 25 serum samples randomly selected from the African volunteers, it was more resistant to neutralization in all sera tested. Across the 25 samples, the ND50 titer determined with the mutant virus was decreased by 2.1 fold compared to the progenitor CDV (Fig. 4A).
Fig. 4.
Neutralization of CDV and the neutralization-resistant mutant by human serum and mAb 2F4. (A) ND50 titers of serum. Dots on the left represent 25 serum samples randomly selected from the 146 volunteers and the two lines represented mean ND50 values to each virus. The average ND50 titer to mutant CDV was 2.1 fold lower than that to CDV indicating the mutant CDV was more resistant to the serum neutralization. (B) IC50 of the 2F4 antibody. The bars represented concentrations of the 2F4 antibody needed to neutralize 50% of the input CDV or the CDV mutant. The highest dilution of the monoclonal antibody causing 50% neutralization of CDV was 1017 and calculated IC50 was 1.8 μg/ml based on this dilution. In contrast, the maximal dilution to neutralize 50% of the mutant virus was only 39.7, which was equivalent to IC50 of 46.6 μg/ml, suggesting the Y to D substitution in the receptor binding site of H diminished the antibody binding.
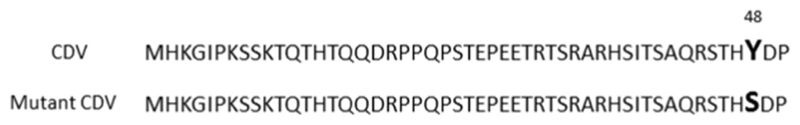
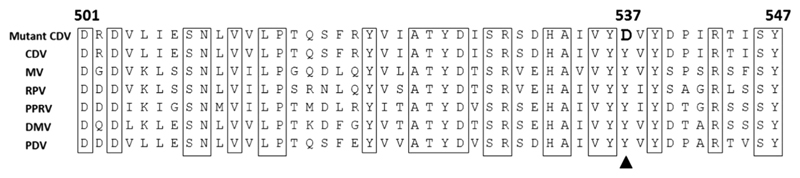
Genomic sequence analysis was performed on the resistant virus population and 10 nucleotide substitutions were detected. Five of the substitutions were in protein coding sequences but were silent in terms of amino acid coding and one mutation was detected in the trailer region (Table 2). Four mutations caused amino acid coding changes with one in the fusion (F), one in the H and two in the large polymerase (L) proteins. The F gene mutation resulted in a tyrosine (Y) to serine (S) substitution at amino acid (aa) 48 in the signal peptide (Fig. 5), while the H mutation resulted in a Y to aspartic acid (D) substitution at aa537 (Fig. 6). The H amino acid substitution occurred in a region that is involved in virus receptor interactions and is conserved across morbilliviruses (Fig. 6).
Table 2. Summary of nucleotide changes and amino acid substitutions between the CDV and neutralization resistant CDV mutant.
| Nucleotide differences between CDV and the neutralization resistant CDVa | ||||
|---|---|---|---|---|
| ntb | CDV | Mutant CDV | aa Substitutionc | |
| M gene nt 3432–4439 | ||||
| 3665 | A | G | Silent | |
| 3707 | A | G | Silent | |
| 3710 | A | G | Silent | |
| F gene nt 4935–6923 | ||||
| 5077 | A | C | Y to S | |
| H gene nt 7079–8902 | ||||
| 7786 | T | A | Silent | |
| 8687 | T | G | Y to D | |
| L gene nt 9030–15,584 | ||||
| 11,455 | A | G | Q to R | |
| 14,298 | A | G | I to V | |
| 14,324 | C | T | Silent | |
| Trailer nt 15,585–15,690 | ||||
| 15,591 | A | G | N/A | |
Genomic cDNA sequences of the two viruses were compared. Uniform length of 15,690 nt was achieved for each genomic cDNA after trimming sequence ends and assembly.
Nucleotide locations of genes and positions for nt changes in each gene are shown.
Amino acid coding substitutions caused by the nt changes are shown for each gene.
Fig. 5.
Mutation in F gene of the neutralization escape CDV isolate. A point mutation changed the tyrosine to serine at aa position 48 as highlighted in bold. The mutation locates in signal peptide region of CDV F. The signal peptide is from amino acid 1–135 in precursor F protein (Plattet et al., 2007) and residues 1–50 are shown.
Fig. 6.
Alignment of aa 501–547 of CDV H and corresponding regions in H proteins of MV, rinderpest virus (P09460), peste des petits ruminants virus (PPRV AHA58209), dolphin morbillivirus (DMV Q66411) and phocine distemper virus (PDV P28882). Amino acid residues conserved among all 6 morbilliviruses are boxed. The CDV H is 607 aa in length and the point mutation changed Y to D at aa position 537 (pointed by the triangular arrow) in H of the neutralization-resistant mutant. This sequence corresponds to aa 505–551 in MV H (Masse et al., 2004), which is involved in H binding to MV receptors and is fully conserved among a variety of MV isolates including Edmonston, Schwarz, Moraten and Zagreb vaccine viruses (H protein sequence accession # in GenBank: P08362, AAA566657, CAL40872, and AM237414, respectively).
The mouse monoclonal antibody 2F4 was used to confirm that the Y537D substitution altered antibody recognition in the receptor binding region. The 2F4 antibody is specific for the receptor binding region of MV H and is a potent neutralizer (Tahara et al., 2013). Stock concentration of the 2F4 antibody used in this study was 1.85 mg/ml and its neutralizing activity against MV was confirmed. When the antibody was tested in CDV PRNT, the dilution causing 50% neutralization was determined to be 1017 and the calculated 50% inhibitory concentration (IC50) was 1.8 μg/ml based on this dilution (Fig. 4B). In contrast, the 2F4 antibody had a relatively little inhibitory effect on infection with the CDV mutant as shown by the significantly lower PRNT value of 39.7, which was equivalent to IC50 of 46.6 μg/ml. These results indicated that the Y to D substitution diminished binding by antibody 2F4 in the receptor-binding region, suggesting that the amino acid substitution had a similar effect on antibodies responsible for neutralization activity in human serum.
Discussion
Results from this study showed that anti-CDV neutralizing activity was relatively low or absent in sera from African clinical trial volunteers. To our knowledge, this is the first human serosurvey involving a large number of volunteers conducted to investigate the prevalence and potency of CDV nAbs. The results also indicated that CDV neutralizing activity likely was related to cross-reactive MV-specific antibodies. We analyzed a smaller number of American serum samples obtained from a commercial source and found their CDV neutralization potency was similarly low (data not shown). CDV nAbs have been reported before, for example in serum from subacute sclerosing panencephalitis (SSPE) patients and in a small number of human samples, which were shown to weakly neutralize a MV-CDV chimeric virus (Miest et al., 2011; Sato et al., 1973), but these studies were not designed to estimate the prevalence of anti-CDV neutralization. Our serosurvey results indicate that low level CDV nAbs can exist in a significant proportion of human populations probably induced by MV vaccination or infection. This contrasts with data from dogs, mice, and non-human primates vaccinated with live MV or vectors expressing MV F and H proteins in which detectable CDV nAbs were not elicited although MV vaccination prevented infection or disease progression following pathogenic CDV challenge (Appel et al., 1984; de Vries et al., 2014; Taylor et al., 1991; Wild et al., 1993). These results seem to suggest that MV vaccines induce human antibodies that can cross-neutralize CDV, but that this is less common in animal models.
Among the 146 volunteers in the survey, 66.4% were positive for low CDV nAbs. This frequency of positivity suggests that MV vaccination or MV infection is the likely inducer of the CDV nAbs, although responses induced by CDV exposure cannot be ruled out. Among the 5 CRCs in the survey, samples from the Masaka CRC had the highest CDV nAb titers. This may be related to the rural location of the Masaka site compared with the other 4 CRC locations. It is conceivable that rural locality could increase the risk of human CDV exposure due to a presence of unvaccinated domestic dogs and wild animal species that are occasionally infected by CDV during distemper outbreaks (Guiserix et al., 2007; Leisewitz et al., 2001; van de Bildt et al., 2002). The prevalence of higher titers in Masaka was not solely responsible for the association between high MV titers and CDV neutralizing antibodies as the same trend was seen if the Masaka data were omitted from the statistical analysis.
The results showed that MV nAbs are prevalent since MV ND50 titers are all above the positive cutoff value of 8.63 that was calculated based on average titers of a negative monkey serum sample. In another study where PRNT was used for analysis of clinical human samples, a titer of 8 was found to be the threshold for detecting low levels of nAbs (Ratnam et al., 1995), which is similar to our cutoff value. Although all of the samples we analyzed were positive for MV antibodies, 9.6% had ND50 titers lower than 120, which is the threshold for prevention of illness due to measles virus infection (Chen et al., 1990). If we assume that CDV ND50 titers greater than 120 are needed to inhibit infection with a vector based on CDV, then 80.2% of the African volunteers were below this threshold.
Two amino acid substitutions were identified in the glycoproteins and two in the L protein of the CDV mutant that was selected for increased resistance to human serum neutralization. Because the membrane glycoproteins F and H are the only known targets of nAbs (Orvell and Norrby, 1974, 1980), the L mutations likely did not contribute to neutralization resistance. The F amino acid substitution was located in the signal peptide that is present in the precursor protein but absent in mature form, and therefore was considered less likely to affect neutralization resistance (Plattet et al., 2007; von Messling et al., 2004). H gene diversity is common and often implicated in CDV evolution driven by immunologic pressure (Martella et al., 2006; Sekulin et al., 2011; Trebbien et al., 2014). The Y537D substitution in CDV H was located in a region that is conserved among morbilliviruses and corresponds to amino acid Y541 in MV H. This region of MV H contains residues involved in binding to cellular CD46 and Nectin, and is associated with antibody neutralization (Mateo et al., 2013; Santiago et al., 2010; Tahara et al., 2013; Zhang et al., 2013a). Due to high sequence identity in this H region, it is likely that nAbs induced by MV vaccination will bind the same domain in CDV H, and our data indicates that the Y to D substitution affected an epitope recognized by some cross-reactive nAbs in human serum. This conclusion agrees with our results with the MV H-specific monoclonal antibody 2F4, which we found to neutralize CDV but was significantly less active against the mutant virus. It was evident that the Y537D substitution did not abolish neutralization activity in human serum indicating that there were other binding sites recognized by nAbs, which is consistent with polyclonal nature of human antiserum against MV (Santibanez et al., 2005, 2002).
The CDV H mutant might be useful for development of vaccine vectors or oncolytic agents because it is less sensitive to pre-existing MV-specific antibodies. Further characterization of the mutant H incorporated in a recombinant CDV will be required to determine if the Y537D substitution is stable during CDV propagation without constant application of selective pressure, if the substitution is attenuating, and whether it alters receptor specificity. The general approach used to select the H mutant resistant to human serum may also be valuable for developing modified glycoproteins that are less susceptible to effects of anti-vector immunity.
Materials and methods
Cell and virus
Vero cells were used in the CDV or MV plaque reduction neutralization test (PRNT). The cells were maintained in Dulbecco's modified Eagle's medium (DMEM, Gibco) supplemented with 10% fetal bovine serum. The CDV used was a clonal isolate derived from a commercial vaccine (Schering-Plough, USA) prepared from the live-attenuated Onderstepoort virus. Isolation and culture of the CDV mutant are described below. Neutralization sensitivity of the mutant CDV was assessed with a subset of the serum samples from clinical trial volunteers. MV used in these studies was an attenuated Edmonston strain derived from a commercial vaccine preparation (ATTENUVAX, MERCK & CO., USA). All three viruses were propagated in Vero cells and plaque forming units (PFU) were quantified as described previously for CDV (Zhang et al., 2013b).
Serum samples
A total of 146 human serum samples were analyzed with the CDV and MV PRNT. These samples were collected from three eastern African countries from healthy adults, ages 19–50, enrolled in vaccine-trial preparatory studies to determine regional HIV incidence (Kamali et al., 2014). For CDV PRNT, sera from naïve and CDV-vaccinated ferrets served as negative and positive controls. Naïve and MV-vaccinated monkey sera were used for MV PRNT controls. All serum samples were inactivated at 56 °C for 30 min before conducting the PRNT.
CDV and MV PRNT
The PRNT was conducted with CDV, mutant CDV, or MV according to a standard MV PRNT protocol with slight modifications (Cohen et al., 2007). Notably, infections were performed using Vero monolayers instead of infecting cells in suspension. Briefly, four-fold serial dilutions were made with each serum sample starting with a 1:4 dilution made by mixing 12.5 μl of serum with 37.5 μl of DMEM in duplicate wells in 96-well plates. The next dilution was made by transferring 12.5 μl of the diluted serum samples to 37.5 μl of DMEM and so on. To each well of diluted serum, an equal volume (37.5 μl) of CDV or MV solution was added and incubated for 2 h. Thus, the first serum dilution on the plate was 1:8. For each experiment, either ferret or monkey sera were used as negative and positive controls and were processed in the same way as test samples. Vero cell monolayers were prepared one day before in 24-well plates and were approximately 80% confluent the following day when they were fed with 0.2 ml of fresh medium. After mixtures of virus and diluted serum were incubated for 2 h to allow antibody binding, the suspension (50 μl) was transferred from the 96-well plates to the 24-well plates containing Vero cell monolayers. Following 2 h virus adsorption, the medium was removed and cells were fed with 1 ml DMEM containing 0.75% methylcellulose. Three days later, medium was removed and cells were washed once with PBS and then fixed with 100% cold methanol for 30 min. For viral plaque detection, the cells were incubated with a rabbit antiserum specific for CDV nucleoprotein or a commercial monoclonal antibody specific for MV nucleoprotein (AbCAM, USA). After removing the primary antibody, incubation was conducted with anti-rabbit or anti-mouse secondary antibodies conjugated with horse-radish peroxidase (HRP). Staining was performed by addition of 3-Amino-9-ethylcarbazole (AEC) substrate for HRP (Sigma). Average plaque numbers were calculated from the duplicated wells at every dilution for each serum sample. For determining neutralization titers, the assay was standardized to generate about 30 plaques per well when virus was treated without serum. At least four identical wells were infected with the virus only for generating an average plaque number in each experiment. Fifty percent neutralization dose (ND50) titers were defined as the reciprocal of the serum dilution at which the number of plaques is reduced to 50% relative to virus only controls. The calculation of ND50 titers followed the Karber formula as described for MV PRNT (Cohen et al., 2007). The serum samples were considered positive for CDV or MV nAbs if the titers were greater than the average ND50 titer of the respective naïve ferret or monkey serum plus 3 times the standard deviation.
The PRNT was conducted in the same way for the mouse monoclonal antibody 2F4 except the starting dilution was 1:80 instead of 1:10 used in serum neutralization test due to limited antibody availability. The 2F4 antibody is specific to the receptor binding region of MV H protein and is a potent neutralizer to MV (Tahara et al., 2013). Concentration of the antibody was 1.85 mg/ml before dilution. Fifty percent inhibitory concentration (IC50) was calculated for the 2F4 antibody according to dilutions needed to neutralize 50% CDV.
Selection of neutralization escape mutants using human immune serum
Neutralization resistant CDV was isolated using a commercial human serum prepared from a single healthy adult donor in USA (Innovative Research, USA). The serum sample was positive for both MV and CDV neutralizing antibodies. A commercial human serum was used because sufficient quantity was available to make it possible to conduct serial virus passage in the presence of nAbs, and this also allowed us to preserve our limited quantities of serum from the African volunteers. For selecting CDV mutants that resisted neutralization, 1 × 106 PFU of CDV in 1 ml of culture medium was incubated with 200 μl of the undiluted serum in 37 °C incubator for 1 h, after which the virus was added to a Vero cell monolayer cultured in T25 flask (Nunc, USA). After 1 h adsorption, the virus inoculum was replaced with 5 ml of cell culture growth medium that was supplemented with 5% human immune serum. Medium supernatant was harvested 6 days later and 20% was used to infect a fresh monolayer that was subsequently incubated in medium containing 5% human immune serum. The supernatant was harvested when a cytopathic effect (CPE) appeared. Virus passage in the presence of human serum was repeated 2 more times. After the 4th round of infection, virus was analyzed with the PRNT using a subset of the African serum samples. The genomes of parental and mutant CDV were sequenced and compared.
Analysis of CDV genomic nucleotide sequences
Genomic sequences were determined by extracting RNA from infected cell lysates, performing reverse transcription and PCR (RT-PCR) using primers based on the CDV nucleotide sequence in GenBank (accession number AF014953), and performing DNA sequencing on amplified DNA fragments. Overlapping sequences were assembled and analyzed using Vector NTI (version 11.5, Life Technologies). Genomic sequences from CDV and the neutralization-resistant mutant were aligned with ClustalW program in Lasergene software (DNASTAR Inc.).
Statistical analysis
Data analyses were conducted using Stata (v13.1, College Station, TX, USA). Spearman's rank correlation analyses were performed to determine the relationship between CDV and MV nAb titers. Spearman's correlation coefficient Rho and p values were given. The titers were transformed to Log10 expression for the correlation analyses and linear regression shown in Fig. 3. To consider potential confounding geographical impact, CDV and MV nAb data were stratified and the correlation analyses were controlled for volunteer enrollment site, gender, and age at the time of blood sample draw.
Acknowledgments
IAVI's work is made possible by generous support from many donors including: the Bill & Melinda Gates Foundation; the Ministry of Foreign Affairs of Denmark; Irish Aid; the Ministry of Finance of Japan; the Ministry of Foreign Affairs of the Netherlands; the Norwegian Agency for Development Cooperation (NORAD); the United Kingdom Department for International Development (DFID), and the United States Agency for International Development (USAID). The full list of IAVI donors is available at www.iavi.org. This study is made possible by the generous support of the American people through USAID and is supported by the Bill and Melinda Gates Foundation Collaboration for AIDS Vaccine Discovery (CAVD). The contents are the responsibility of the International AIDS Vaccine Initiative and do not necessarily reflect the views of USAID or the United States Government. The authors are grateful for Emmanuel Cormier, Laura Sharpe and Brendan McAtarsney for serum sample management. We also thank Wayne Koff, Rick King, Josephine Cox and Beth Rasmussen for helpful suggestions and advice, and acknowledge Heather Arendt and Joanne DeStefano for critical reading of the manuscript. The authors also thank Shinji Ohno and Makoto Takeda from Kyushu University for providing the 2F4 mouse monoclonal antibody.
References
- Appel MJ, Shek WR, Shesberadaran H, Norrby E. Measles virus and inactivated canine distemper virus induce incomplete immunity to canine distemper. Arch Virol. 1984;82:73–82. doi: 10.1007/BF01309369. [DOI] [PubMed] [Google Scholar]
- Blixenkrone-Moller M. Biological properties of phocine distemper virus and canine distemper virus. APMIS Suppl. 1993;36:1–51. [PubMed] [Google Scholar]
- Brandler S, Lucas-Hourani M, Moris A, Frenkiel MP, Combredet C, Fevrier M, Bedouelle H, Schwartz O, Despres P, Tangy F. Pediatric measles vaccine expressing a dengue antigen induces durable serotype-specific neutralizing antibodies to dengue virus. PLoS Negl Trop Dis. 2007;1:e96. doi: 10.1371/journal.pntd.0000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandler S, Tangy F. Recombinant vector derived from live attenuated measles virus: potential for flavivirus vaccines. Comp Immunol Microbiol Infect Dis. 2008;31:271–291. doi: 10.1016/j.cimid.2007.07.012. [DOI] [PubMed] [Google Scholar]
- Buczkowski H, Muniraju M, Parida S, Banyard AC. Morbillivirus vaccines: recent successes and future hopes. Vaccine. 2014;32:3155–3161. doi: 10.1016/j.vaccine.2014.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen RT, Markowitz LE, Albrecht P, Stewart JA, Mofenson LM, Preblud SR, Orenstein WA. Measles antibody: reevaluation of protective titers. J Infect Dis. 1990;162:1036–1042. doi: 10.1093/infdis/162.5.1036. [DOI] [PubMed] [Google Scholar]
- Cohen BJ, Audet S, Andrews N, Beeler J, W.H.O.w.g.o.m.p.r.n. test Plaque reduction neutralization test for measles antibodies: description of a standardised laboratory method for use in immunogenicity studies of aerosol vaccination. Vaccine. 2007;26:59–66. doi: 10.1016/j.vaccine.2007.10.046. [DOI] [PubMed] [Google Scholar]
- de Vries RD, Ludlow M, Verburgh RJ, van Amerongen G, Yuksel S, Nguyen DT, McQuaid S, Osterhaus AD, Duprex WP, de Swart RL. Measles vaccination of non-human primates provides partial protection against infection with canine distemper virus. J Virol. 2014;88:4423–4433. doi: 10.1128/JVI.03676-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Despres P, Combredet C, Frenkiel MP, Lorin C, Brahic M, Tangy F. Live measles vaccine expressing the secreted form of the West Nile virus envelope glycoprotein protects against West Nile virus encephalitis. J Infect Dis. 2005;191:207–214. doi: 10.1086/426824. [DOI] [PubMed] [Google Scholar]
- Di Guardo G, Marruchella G, Agrimi U, Kennedy S. Morbillivirus infections in aquatic mammals: a brief overview. J Vet Med A: Physiol Pathol Clin Med. 2005;52:88–93. doi: 10.1111/j.1439-0442.2005.00693.x. [DOI] [PubMed] [Google Scholar]
- Draper SJ, Heeney JL. Viruses as vaccine vectors for infectious diseases and cancer. Nat Rev Microbiol. 2010;8:62–73. doi: 10.1038/nrmicro2240. [DOI] [PubMed] [Google Scholar]
- Gauvrit A, Brandler S, Sapede-Peroz C, Boisgerault N, Tangy F, Gregoire M. Measles virus induces oncolysis of mesothelioma cells and allows dendritic cells to cross-prime tumor-specific CD8 response. Cancer Res. 2008;68:4882–4892. doi: 10.1158/0008-5472.CAN-07-6265. [DOI] [PubMed] [Google Scholar]
- Guerbois M, Moris A, Combredet C, Najburg V, Ruffie C, Fevrier M, Cayet N, Brandler S, Schwartz O, Tangy F. Live attenuated measles vaccine expressing HIV-1 Gag virus like particles covered with gp160DeltaV1V2 is strongly immunogenic. Virology. 2009;388:191–203. doi: 10.1016/j.virol.2009.02.047. [DOI] [PubMed] [Google Scholar]
- Guiserix M, Bahi-Jaber N, Fouchet D, Sauvage F, Pontier D. The canine distemper epidemic in Serengeti: are lions victims of a new highly virulent canine distemper virus strain, or is pathogen circulation stochasticity to blame? J R Soc Interface/R Soc. 2007;4:1127–1134. doi: 10.1098/rsif.2007.0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haile R, Smith P, Read D, Nassim D, Warlow C, Russell WC. A study of measles virus and canine distemper virus antibodies, and of childhood infections in multiple sclerosis patients and controls. J Neurol Sci. 1982;56:1–10. doi: 10.1016/0022-510x(82)90055-7. [DOI] [PubMed] [Google Scholar]
- Hoekenga MT, Schwarz AJ, Carrizo Palma H, Boyer PA. Experimental vaccination against measles. II. Tests of live measles and live distemper vaccine in human volunteers during a measles epidemic in Panama. J Am Med Assoc. 1960;173:868–872. doi: 10.1001/jama.1960.03020260008002. [DOI] [PubMed] [Google Scholar]
- Hussain H, Akram DS, Chandir S, Khan AJ, Memon A, Halsey NA. Immune response to 1 and 2 dose regimens of Measles vaccine in Pakistani children. Hum Vaccines Immunother. 2013;9:2529–2532. doi: 10.4161/hv.25993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamali A, Price MA, Lakhi S, Karita E, Inambao M, Sanders EJ, Anzala O, Latka MH, Bekker LG, Kaleebu P, Asiki G, et al. The IAVI Africa HIV Prevention Partnership, Creating an African HIV clinical research and prevention trials network: HIV prevalence, incidence and transmission. PloS One. 2015;10:e0116100. doi: 10.1371/journal.pone.0116100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koff WC, Burton DR, Johnson PR, Walker BD, King CR, Nabel GJ, Ahmed R, Bhan MK, Plotkin SA. Accelerating next-generation vaccine development for global disease prevention. Science. 2013;340 doi: 10.1126/science.1232910. 1232910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leisewitz AL, Carter A, van Vuuren M, van Blerk L. Canine distemper infections, with special reference to South Africa, with a review of the literature. J S Afr Vet Assoc. 2001;72:127–136. doi: 10.4102/jsava.v72i3.635. [DOI] [PubMed] [Google Scholar]
- Leuridan E, Hens N, Hutse V, Ieven M, Aerts M, Van Damme P. Early waning of maternal measles antibodies in era of measles elimination: longitudinal study. Br Med J. 2010;340:c1626. doi: 10.1136/bmj.c1626. [DOI] [PubMed] [Google Scholar]
- Martella V, Cirone F, Elia G, Lorusso E, Decaro N, Campolo M, Desario C, Lucente MS, Bellacicco AL, Blixenkrone-Moller M, Carmichael LE, Buonavoglia C. Heterogeneity within the hemagglutinin genes of canine distemper virus (CDV) strains detected in Italy. Vet Microbiol. 2006;116:301–309. doi: 10.1016/j.vetmic.2006.04.019. [DOI] [PubMed] [Google Scholar]
- Masse N, Ainouze M, Neel B, Wild TF, Buckland R, Langedijk JP. Measles virus (MV) hemagglutinin: evidence that attachment sites for MV receptors SLAM and CD46 overlap on the globular head. J Virol. 2004;78:9051–9063. doi: 10.1128/JVI.78.17.9051-9063.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateo M, Navaratnarajah CK, Syed S, Cattaneo R. The measles virus hemagglutinin beta-propeller head beta4–beta5 hydrophobic groove governs functional interactions with nectin-4 and CD46 but not those with the signaling lymphocytic activation molecule. J Virol. 2013;87:9208–9216. doi: 10.1128/JVI.01210-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miest TS, Cattaneo R. New viruses for cancer therapy: meeting clinical needs. Nat Rev Microbiol. 2014;12:23–34. doi: 10.1038/nrmicro3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miest TS, Yaiw KC, Frenzke M, Lampe J, Hudacek AW, Springfeld C, von Messling V, Ungerechts G, Cattaneo R. Envelope-chimeric entry-targeted measles virus escapes neutralization and achieves oncolysis. Mol Ther: J Am Soc Gene Ther. 2011;19:1813–1820. doi: 10.1038/mt.2011.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mingozzi F, Chen Y, Edmonson SC, Zhou S, Thurlings RM, Tak PP, High KA, Vervoordeldonk MJ. Prevalence and pharmacological modulation of humoral immunity to AAV vectors in gene transfer to synovial tissue. Gene Ther. 2013;20:417–424. doi: 10.1038/gt.2012.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orvell C, Norrby E. Further studies on the immunologic relationships among measles, distemper, and rinderpest viruses. J Immunol. 1974;113:1850–1858. [PubMed] [Google Scholar]
- Orvell C, Norrby E. Immunological relationships between homologous structural polypeptides of measles and canine distemper virus. J Gen Virol. 1980;50:231–245. doi: 10.1099/0022-1317-50-2-231. [DOI] [PubMed] [Google Scholar]
- Otsuki N, Nakatsu Y, Kubota T, Sekizuka T, Seki F, Sakai K, Kuroda M, Yamaguchi R, Takeda M. The v protein of canine distemper virus is required for virus replication in human epithelial cells. PloS One. 2013;8:e82343. doi: 10.1371/journal.pone.0082343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks CL, Picker LJ, King CR. Development of replication-competent viral vectors for HIV vaccine delivery. Curr Opin HIV AIDS. 2013;8:402–411. doi: 10.1097/COH.0b013e328363d389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plattet P, Cherpillod P, Wiener D, Zipperle L, Vandevelde M, Wittek R, Zurbriggen A. Signal peptide and helical bundle domains of virulent canine distemper virus fusion protein restrict fusogenicity. J Virol. 2007;81:11413–11425. doi: 10.1128/JVI.01287-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu W, Zheng Y, Zhang S, Fan Q, Liu H, Zhang F, Wang W, Liao G, Hu R. Canine distemper outbreak in rhesus monkeys China, Emerg. Infect Dis. 2011;17:1541–1543. doi: 10.3201/eid1708.101153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratnam S, Gadag V, West R, Burris J, Oates E, Stead F, Bouilianne N. Comparison of commercial enzyme immunoassay kits with plaque reduction neutralization test for detection of measles virus antibody. J Clin Microbiol. 1995;33:811–815. doi: 10.1128/jcm.33.4.811-815.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rima BK. The proteins of morbilliviruses. J Gen Virol. 1983;64(Pt 6):1205–1219. doi: 10.1099/0022-1317-64-6-1205. [DOI] [PubMed] [Google Scholar]
- Rima BK, Duprex WP. Morbilliviruses and human disease. J Pathol. 2006;208:199–214. doi: 10.1002/path.1873. [DOI] [PubMed] [Google Scholar]
- Sakai K, Nagata N, Ami Y, Seki F, Suzaki Y, Iwata-Yoshikawa N, Suzuki T, Fukushi S, Mizutani T, Yoshikawa T, Otsuki N, et al. Lethal canine distemper virus outbreak in cynomolgus monkeys in Japan in 2008. J Virol. 2013a;87:1105–1114. doi: 10.1128/JVI.02419-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai K, Yoshikawa T, Seki F, Fukushi S, Tahara M, Nagata N, Ami Y, Mizutani T, Kurane I, Yamaguchi R, Hasegawa H, et al. Canine distemper virus associated with a lethal outbreak in monkeys can readily adapt to use human receptors. J Virol. 2013b;87:7170–7175. doi: 10.1128/JVI.03479-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santiago C, Celma ML, Stehle T, Casasnovas JM. Structure of the measles virus hemagglutinin bound to the CD46 receptor. Nat Struct Mol Biol. 2010;17:124–129. doi: 10.1038/nsmb.1726. [DOI] [PubMed] [Google Scholar]
- Santibanez S, Niewiesk S, Heider A, Schneider-Schaulies J, Berbers GA, Zimmer-mann A, Halenius A, Wolbert A, Deitemeier I, Tischer A, Hengel H. Probing neutralizing-antibody responses against emerging measles viruses (MVs): immune selection of MV by H protein-specific antibodies? J Gen Virol. 2005;86:365–374. doi: 10.1099/vir.0.80467-0. [DOI] [PubMed] [Google Scholar]
- Santibanez S, Tischer A, Heider A, Siedler A, Hengel H. Rapid replacement of endemic measles virus genotypes. J Gen Virol. 2002;83:2699–2708. doi: 10.1099/0022-1317-83-11-2699. [DOI] [PubMed] [Google Scholar]
- Santra S, Sun Y, Korioth-Schmitz B, Fitzgerald J, Charbonneau C, Santos G, Seaman MS, Ratcliffe SJ, Montefiori DC, Nabel GJ, Ertl HC, et al. Heterologous prime/boost immunizations of rhesus monkeys using chimpanzee adenovirus vectors. Vaccine. 2009;27:5837–5845. doi: 10.1016/j.vaccine.2009.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato TA, Yamanouchi K, Shishido A. Presence of neutralizing antibody to canine distemper virus in sera of patients with subacute sclerosing panence-phalitis. Arch Gesamte Virusforsch. 1973;42:36–41. doi: 10.1007/BF01250505. [DOI] [PubMed] [Google Scholar]
- Sekulin K, Hafner-Marx A, Kolodziejek J, Janik D, Schmidt P, Nowotny N. Emergence of canine distemper in Bavarian wildlife associated with a specific amino acid exchange in the haemagglutinin protein. Vet J. 2011;187:399–401. doi: 10.1016/j.tvjl.2009.12.029. [DOI] [PubMed] [Google Scholar]
- Stephenson JR, ter Meulen V. Antigenic relationships between measles and canine distemper viruses: comparison of immune response in animals and humans to individual virus-specific polypeptides. Proc Natl Acad Sci USA. 1979;76:6601–6605. doi: 10.1073/pnas.76.12.6601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahara M, Ohno S, Sakai K, Ito Y, Fukuhara H, Komase K, Brindley MA, Rota PA, Plemper RK, Maenaka K, Takeda M. The receptor-binding site of the measles virus hemagglutinin protein itself constitutes a conserved neutralizing epitope. J Virol. 2013;87:3583–3586. doi: 10.1128/JVI.03029-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J, Pincus S, Tartaglia J, Richardson C, Alkhatib G, Briedis D, Appel M, Norton E, Paoletti E. Vaccinia virus recombinants expressing either the measles virus fusion or hemagglutinin glycoprotein protect dogs against canine distemper virus challenge. J Virol. 1991;65:4263–4274. doi: 10.1128/jvi.65.8.4263-4274.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trebbien R, Chriel M, Struve T, Hjulsager CK, Larsen G, Larsen LE. Wildlife reservoirs of canine distemper virus resulted in a major outbreak in Danish farmed mink (Neovison vison) PloS One. 2014;9:e85598. doi: 10.1371/journal.pone.0085598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Bildt MW, Kuiken T, Visee AM, Lema S, Fitzjohn TR, Osterhaus AD. Distemper outbreak and its effect on African wild dog conservation. Emerg Infect Dis. 2002;8:211–213. doi: 10.3201/eid0802.010314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Messling V, Milosevic D, Devaux P, Cattaneo R. Canine distemper virus and measles virus fusion glycoprotein trimers: partial membrane-proximal ectodomain cleavage enhances function. J Virol. 2004;78:7894–7903. doi: 10.1128/JVI.78.15.7894-7903.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Feng N, Ge J, Shuai L, Peng L, Gao Y, Yang S, Xia X, Bu Z. Recombinant canine distemper virus serves as bivalent live vaccine against rabies and canine distemper. Vaccine. 2012;30:5067–5072. doi: 10.1016/j.vaccine.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Wild TF, Bernard A, Spehner D, Villeval D, Drillien R. Vaccination of mice against canine distemper virus-induced encephalitis with vaccinia virus recombinants encoding measles or canine distemper virus antigens. Vaccine. 1993;11:438–444. doi: 10.1016/0264-410x(93)90285-6. [DOI] [PubMed] [Google Scholar]
- Zhang X, Lu G, Qi J, Li Y, He Y, Xu X, Shi J, Zhang CW, Yan J, Gao GF. Structure of measles virus hemagglutinin bound to its epithelial receptor nectin-4. Nat Struct Mol Biol. 2013a;20:67–72. doi: 10.1038/nsmb.2432. [DOI] [PubMed] [Google Scholar]
- Zhang X, Wallace O, Wright KJ, Backer M, Coleman JW, Koehnke R, Frenk E, Domi A, Chiuchiolo MJ, DeStefano J, Narpala S, et al. Membrane-bound SIV envelope trimers are immunogenic in ferrets after intranasal vaccination with a replication-competent canine distemper virus vector. Virology. 2013b;446:25–36. doi: 10.1016/j.virol.2013.07.012. [DOI] [PubMed] [Google Scholar]