Abstract
This histologic analysis of cutaneous manifestations of dermatomyositis examines whether skin eruptions can be histopathologically classified into myositis-specific autoantibodies-associated groups.
A number of myositis-specific autoantibodies have been identified in patients with dermatomyositis (DM), including anti–aminoacyl-transfer RNA synthetase (ARS), antimelanoma differentiation-associated protein 5 (MDA5), and antitranscriptional intermediary factor 1 (TIF1)γ antibodies, each of which is respectively associated with characteristic cutaneous manifestations.1,2 We analyzed the histologic findings of finger lesions based on these 3 myositis-specific autoantibodies.
Methods
This retrospective observational study was performed on patients with DM diagnosed with typical rash and the presence of anti-ARS, anti-MDA5, and TIF1γ antibodies detected using enzyme-linked immunosorbent assay kits (Medical and Biological Labratories) in our dermatology departments from September 2007 to August 2018. We found 74 cases (30, 19, and 25 cases in the ARS, MDA5, and TIF1γ groups, respectively) where patients underwent skin biopsies of finger eruptions (eTable in the Supplement). The medical ethics review committee of each hospital exempted this study from ethical approval and waived the need for patient written informed consent because all data used were deidentified. Hematoxylin-eosin–stained skin specimens were classified into classic cutaneous histopathologic classifications, including interface dermatitis, psoriasiform dermatitis, eczematous reaction, and vascular injury (eFigure in the Supplement).
Immunohistochemical staining with antibody targeting myxovirus resistance protein A (MxA, sc-166412 by Santa Cruz Biology)3 was performed. Data were analyzed by the the χ2 and Kruskal-Wallis tests using Prism 8 (version 8.1.0, GraphPad Software). P values <.05 were deemed statistically significant. The analyses were performed from September to December in 2018, then additional statistical analyses using Prism were performed in April 2019.
Results
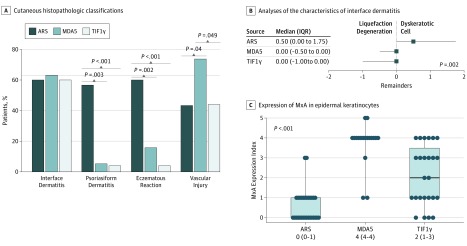
Interface dermatitis was observed in more than half of the specimens from each group. Psoriasiform dermatitis was observed at a significantly higher frequency in the ARS group (17 cases, 57%) than in the MDA5 group (1 case, 5%) and TIF1γ group (1 case, 4%) (Figure, A). Patients in ARS group (18 cases, 60%) developed eczematous reaction at a significantly higher frequency than did the MDA5 (3 cases, 16%) and TIF1γ groups (1 case, 4%). Vascular injury was observed more often in the MDA5 group (14 cases, 74%) than in the ARS (13 cases, 43%) and TIF1γ groups (11 cases, 44%). These results were not significantly related to the finger location of skin biopsies.
Figure. Histologic Analyses.
The percentages of patients grouped into anti–aminoacyl-transfer RNA synthetase (ARS, dark blue bars), antimelanoma differentiation-associated protein 5 (MDA5, blue bars), and antitranscriptional intermediary factor 1γ (TIF1γ, light blue bars) antibodies-associated dermatomyositis groups showing interface dermatitis, psoriasiform dermatitis, eczematous reaction, and vascular injury in the upper dermis, respectively. Interface dermatitis was determined using a total score of 2 or greater, which was evaluated with liquefaction degeneration of the basal layer and dyskeratotic cells (0, absent; 1, <5 cells per field [ × 100]; and 2, ≥5 cells per field, respectively). Psoriasiform dermatitis was determined by a total score of 2 or greater, which was evaluated with psoriasiform acanthosis (0, absent; 1, present) and parakeratosis (0, absent; 1, <50% of field; and 2, ≥50% of field). Eczematous reaction was determined by the presence or absence of spongiosis (absent, <50% of field; and present, ≥50% of field), and vascular injury was assessed by inflammatory cell infiltration into vessel walls and bleeding. B, The remainders (score for dyskeratotic cells minus the score for liquefaction degeneration of the basal layer) for each group were calculated. The squares and bars represent medians and interquartile ranges (IQRs), respectively. C, The MxA expression index in each group was evaluated by calculating the percentage of MxA-expressing epidermal areas (0, 0%; 1, 1%-24%; 2, 25%-49%; 3, 50%-74%; 4, 75%-99%; 5, 100%). The boxes containing lines and bars represent the IQRs with medians and full ranges, respectively. The dots indicate individual MxA values.
The remainders (the scores for dyskeratotic cells minus the scores for liquefaction degeneration of the basal layer) in the ARS group (median, 0.5; interquartile range [IQR], 0-1.7) were significantly higher than those in the MDA5 (median, 0; IQR, −0.5 to 0) and TIF1γ groups (median, 0; IQR, −1 to 0) (Figure, B).
The expression of MxA, a type 1 interferon (IFN)-inducible protein, in the epidermal keratinocytes was significantly higher in the MDA5 (index median, 4; IQR, 4-4]) than in the TIF1γ group (index median, 2; IQR, 1-3]), and this expression was also rarely observed in the ARS group (index median, 0; 0-1) (Figure, C).
Discussion
To our knowledge, this study is the first histologic analysis of cutaneous manifestations to demonstrate that skin eruptions can be histopathologically classified into myositis-specific autoantibodies-associated groups, suggesting the systemic pathologies of the different types of antibody-associated DM, as shown in the eFigure in the Supplement. Anti-ARS antibody-associated DM is an independent subset characterized by a mixture of psoriasiform dermatitis and eczematous reaction with dyskeratotic cell-rich interface dermatitis. In addition, the eruption related to anti-MDA5 antibody-associated DM was characterized by vascular injury. We also found that MxA expression on epidermal keratinocytes was absent in the ARS group, which is similar to findings from a previous study examining muscle fibers.4 In addition, high MxA epidermal expression was observed especially in the MDA5 group, as suggested previously,5and also in the TIF1γ group.
Because the findings of this study were limited by the small number of Japanese patients, further large-scale studies are required to clarify the pathologies of DM.
eTable. Clinical characteristics and histopathological classifications in the analyzed cases
eFigure. Histopathologic classification of skin eruptions in myositis-specific autoantibody-associated groups
References
- 1.Concha JSS, Merola JF, Fiorentino D, Werth VP. Re-examining mechanic’s hands as a characteristic skin finding in dermatomyositis. J Am Acad Dermatol. 2018;78(4):769-775.e2, e762. [DOI] [PubMed] [Google Scholar]
- 2.Fiorentino D, Chung L, Zwerner J, Rosen A, Casciola-Rosen L. The mucocutaneous and systemic phenotype of dermatomyositis patients with antibodies to MDA5 (CADM-140): a retrospective study. J Am Acad Dermatol. 2011;65(1):25-34. doi: 10.1016/j.jaad.2010.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uruha A, Suzuki S, Nishino I. Author update: sarcoplasmic MxA expression: a valuable marker of dermatomyositis. Neurology. 2017;89(2):215. doi: 10.1212/WNL.0000000000004102 [DOI] [PubMed] [Google Scholar]
- 4.Uruha A, Nishikawa A, Tsuburaya RS, et al. Sarcoplasmic MxA expression: a valuable marker of dermatomyositis. Neurology. 2017;88(5):493-500. doi: 10.1212/WNL.0000000000003568 [DOI] [PubMed] [Google Scholar]
- 5.Zhang SH, Zhao Y, Xie QB, Jiang Y, Wu YK, Yan B. Aberrant activation of type I interferon system may contribute to the pathogenesis of anti-MDA5 dermatomyositis. Br J Dermatol. 2018;180(5):1090-1098. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Clinical characteristics and histopathological classifications in the analyzed cases
eFigure. Histopathologic classification of skin eruptions in myositis-specific autoantibody-associated groups