Abstract
IMPORTANCE
Three months of a once-weekly combination of rifapentine and isoniazid for treatment of latent tuberculosis infection is safe and effective for persons 12 years or older. Published data for children are limited.
OBJECTIVES
To compare treatment safety and assess noninferiority treatment effectiveness of combination therapy with rifapentine and isoniazid vs 9 months of isoniazid treatment for latent tuberculosis infection in children.
DESIGN, SETTING, AND PARTICIPANTS
A pediatric cohort nested within a randomized, open-label clinical trial conducted from June 11, 2001, through December 17, 2010, with follow-up through September 5, 2013, in 29 study sites in the United States, Canada, Brazil, Hong Kong (China), and Spain. Participants were children (aged 2–17 years) who were eligible for treatment of latent tuberculosis infection.
INTERVENTIONS
Twelve once-weekly doses of the combination drugs, given with supervision by a health care professional, for 3 months vs 270 daily doses of isoniazid, without supervision by a health care professional, for 9 months.
MAIN OUTCOMES AND MEASURES
We compared rates of treatment discontinuation because of adverse events (AEs), toxicity grades 1 to 4, and deaths from any cause. The equivalence margin for the comparison of AE-related discontinuation rates was 5%. Tuberculosis disease diagnosed within 33 months of enrollment was the main end point for testing effectiveness. The noninferiority margin was 0.75%.
RESULTS
Of 1058 children enrolled, 905 were eligible for evaluation of effectiveness. Of 471 in the combination-therapy group, 415 (88.1%) completed treatment vs 351 of 434 (80.9%) in the isoniazid-only group (P = .003). The 95% CI for the difference in rates of discontinuation attributed to an AE was −2.6 to 0.1, which was within the equivalence range. In the safety population, 3 of 539 participants (0.6%) who took the combination drugs had a grade 3 AE vs 1 of 493 (0.2%) who received isoniazid only. Neither arm had any hepatotoxicity, grade 4 AEs, or treatment-attributed death. None of the 471 in the combination-therapy group developed tuberculosis vs 3 of 434 (cumulative rate, 0.74%) in the isoniazid-only group, for a difference of −0.74% and an upper bound of the 95% CI of the difference of +0.32%, which met the noninferiority criterion.
CONCLUSIONS AND RELEVANCE
Treatment with the combination of rifapentine and isoniazid was as effective as isoniazid-only treatment for the prevention of tuberculosis in children aged 2 to 17 years. The combination-therapy group had a higher treatment completion rate than did the isoniazid-only group and was safe.
TRIAL REGISTRATION
clinicaltrials.gov Identifier: NCT00023452
A substantial portion of the global burden of active and latent tuberculosis (TB) is found in children.1–3 Treatment of latent Mycobacterium tuberculosis infection (LTBI) in children is beneficial, both for the child and for public health, because it prevents development of TB and limits future M tuberculosis transmission.4–7 The benefits of treatment of LTBI are greater for children than for adults for several reasons: LTBI in children younger than 5 years is always recently acquired (ie, within 5 years), and recent infection has a higher likelihood of progression to disease than infection acquired less recently; children have an increased risk of developing severe TB with sequela (eg, meningitis and disseminated disease); children have more years at risk for the development of TB than adults; and children tolerate treatment for LTBI better than adults.
Soon after effective treatment was established for active TB, studies began to determine whether treatment of LTBI could prevent active TB, as well as in what settings and with what duration. In the 1950s and 1960s, Lincoln and Vera Cruz8,9 and Ferebee et al10,11 established that isoniazid given daily for 12 months was effective in preventing TB in adults and children with LTBI. Shorter LTBI treatment regimens are associated with improved adherence and treatment completion in adults and children.12–14 Supervised (ie, directly observed) LTBI therapy in children increased adherence by 57% in South Africa.15 In the United States, some TB control departments use directly observed therapy for the administration of LTBI treatment to persons at highest risk of developing TB, including children, if sufficient resources are available.16,17 Recently, the PREVENT TB (Three Months of Rifapentine and Isoniazid for Latent Tuberculosis Infection)18 clinical trial demonstratedthat a short-course combination regimen of rifapentine and isoniazid for 3 months given with direct observation was as effective as the reference-standard 9-month regimen of self-administered isoniazid in persons 12 years or older; combination therapy with rifapentine and isoniazid was safe and had a higher treatment completion rate. However, too few children were enrolled for safety and effectiveness to be evaluated separately. Along with additional evidence from 2 smaller clinical trials,19,20 the findings of the PREVENT TB trial led the Centers for Disease Control and Prevention to recommend use of the new 3-month regimen for treatment of LTBI in adults and children at least 12 years of age.21
The pharmacokinetics of rifapentine in children younger than 12 years were not known at the start of the PREVENT TB study. When these data became available in 2005,22 enrollment criteria were modified to include children aged 2 to 11 years. We report here the results among all children aged 2 to 17 years from this multicenter randomized clinical trial.
Methods
Population, Treatment, and Monitoring
Children and adolescents were enrolled from 29 study sites in the United States, Canada, Brazil, Hong Kong (China), and Spain in 23 Tuberculosis Trials Consortium (TBTC) sites and 6 International Maternal Pediatric and Adolescents AIDS Clinical Trials Group (IMPAACT) sites. The study protocol was approved by institutional review boards at the Centers for Disease Control and Prevention, the National Institutes of Health, and all study sites. Children had informed consent signed by at least 1 parent and provided informed assent in accordance with local human subjects protection regulations. Children were eligible to participate in the trial if they met specific criteria indicating high risk for TB according to age, tuberculin skin test (TST) results, and TB exposure history and did not meet any study exclusion criteria (eAppendix 2 in the Supplement). Enrollment did not require knowledge of human immunodeficiency virus (HIV) serostatus or HIV testing. The age criterion for inclusion of children in the PREVENT TB trial changed with protocol amendments over time: from June 5, 2001, to November 22, 2005, enrollment included children aged 12 years to younger than 18 years; from November 23, 2005, to February 15, 2008 (starting as soon as was feasible after pharmacokinetic data became available), children aged 2 years to younger than 18 years; and from February 16, 2008 (end of parent trial enrollment), to December 17, 2010, children aged 2 years to younger than 12 years regardless of HIV serostatus and 12 years to younger than 18 years only if they were known to be HIV seropositive (eFigure in the Supplement).
Children in the isoniazid-only group were prescribed 270 daily doses of isoniazid dispensed in 30-day allotments. For this arm of the trial, isoniazid was either self-administered (ie, by the patient or the parent, without supervision by a health care professional) or directly observed, following the study site administration guidelines for children. If directly observed therapy was used during isoniazid-only treatment, frequency remained daily. Children enrolled in the combination-therapy group were prescribed a regimen of 12 weekly doses of a combination of rifapentine and isoniazid (eTable in the Supplement23). All doses for rifapentine plus isoniazid were given by directly observed therapy. Directly observed therapy was defined as treatment for which a study health care professional prepared and observed ingestion of each dose. Completion of rifapentine plus isoniazid therapy was defined as administration of 11 of no more than 12 weekly, directly observed therapy doses in 10 to 16 weeks. Completion of isoniazid only was defined as receipt of 240 of no more than 270 daily doses in 35 to 52 weeks. Receipt of isoniazid doses was assessed by interview with the parent and child and verified by pill count at monthly clinic visits, which included standardized symptom evaluations.
Clinician investigators reported adverse events (AEs) from enrollment through 60 days after the last dose of study medications. Information regarding type, management, seriousness,24 toxicity grade,25 and relatedness to the study medications (definite, probable, possible, unlikely, or not related) was reported for each event. We categorized AEs as not attributed to treatment when they had been determined to be unlikely or not related to the study drugs. Serious AEs included death during therapy or within 60 days of the last dose, life-threatening events, hospitalization, disability or permanent damage, and congenital anomaly. Posttreatment follow-up began after the participant completed or discontinued treatment with study medications. In each treatment arm, follow-up evaluations were conducted every 3 months until 21 months after enrollment, then every 6 months (months 27 and 33) until the end of study follow-up (33 months after enrollment). Case finding was active, following protocol guidelines, with follow-up evaluations conducted by telephone until the final visit, which was in person and conducted at a clinic with specialized experience in the diagnosis and treatment of TB in children. The trial protocol defined TB in children as either confirmed by M tuberculosis in culture or diagnosed clinically based on the TB diagnostic criteria of the American Thoracic Society and Centers for Disease Control and Prevention,26 with diagnosis and treatment guidance from the American Academy of Pediatrics.27
Randomization, Study Objectives, and Populations for Analysis
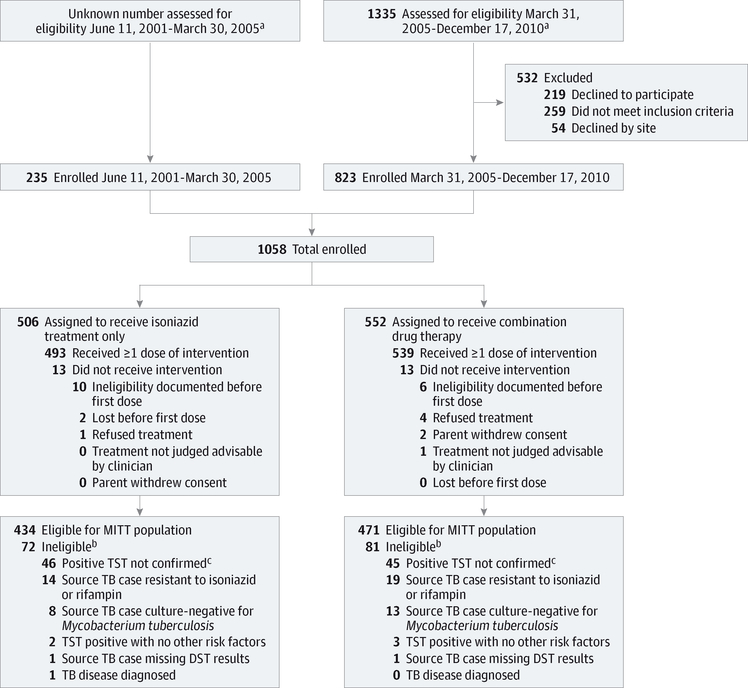
The trial used a parallel-design unrestricted randomization method. Children were randomized either individually or by household. If 2 or more inhabitants agreed to participate in the trial, they were assigned to the same study treatment as the first enrolled member of their household (eAppendix 3 in the Supplement). The primary objective of the PREVENT TB pediatric study was the equivalence comparison of treatment safety between the 2 study arms. The secondary objective was to assess the treatment effectiveness of combination therapy for noninferiority compared with the isoniazid-only regimen for the prevention of TB. We used 3 study populations for analysis: (1) intention to treat–which included all children in the study–for the analysis of demographic characteristics and evaluation of differences between arms; (2) safety population–which included all children who took 1 or more doses of the study medication; and (3) modified intention to treat–which included all children who were protocol eligible–for the analysis of treatment completion and treatment effectiveness (Figure 1). Follow-up continued through September 5, 2013. Tuberculosis end points were evaluated and confirmed by consensus of an independent 3-person panel of experts who were masked to the study arm and the study site that reported the TB end point.
Figure 1. Flowchart of Study Participants (Children Aged 2–17 Years): CONSORT Criteria.
This flowchart shows the number of participants who were enrolled, received the assigned treatment, and were analyzed for the safety and effectiveness outcomes. Combination drug therapy indicates 3 months of directly observed once-weekly combination of rifapentine and isoniazid; isoniazid therapy, 9 months of self-administered daily isoniazid; DST, drug susceptibility testing; MITT, modified intention-to-treat; TB, tuberculosis; TST, tuberculin skin test.
a Eligibility screening data for the randomized clinical trial were obtained from March 31, 2005, onward, with the implementation of an eligibility screening log. This log was implemented in response to the publication of the CONSORT (Consolidated Standards of Reporting Trials) reporting recommendations for randomized clinical trials, which were vetted after the PREVENT TB trial started.
b Enrollment of participants was allowed before Mycobacterium tuberculosis culture and susceptibility data were available in the source case of tuberculosis.
c Results of TST not confirmed as positive on postenrollment TST repeated at 8 to 12 weeks; enrollment of close contacts was allowed if children were younger than 5 years or human immunodeficiency virus seropositive and enrolling clinicians had the option to discontinue treatment.
Sample Size, Study Power, and Statistical Methods
We tested the hypothesis that there would be no difference in the rates of treatment discontinuation attributed to AEs between the 2 treatment arms. We considered results with 5% or less difference between the rates of treatment discontinuation attributed to AEs to be clinically equivalent. Assuming 15% loss to follow-up, 80% power, a type 1 error rate of 0.05, and 1% rate of discontinuation attributed to AEs in the standard treatment arm, the sample size estimate for testing the main safety hypothesis was 322 children per arm. The 95% CI of the difference of the rates of discontinuation attributed to AEs was calculated and then compared with the equivalence region (−5% to 5%). P values were calculated using the Fisher exact test to determine whether the rates were significantly different.
For the PREVENT TB core trial population composed mostly of adults and some adolescents, the primary objective was an evaluation for noninferiority of the treatment effectiveness of the combination therapy with rifapentine and isoniazid.18 In this nested study, treatment effectiveness testing was a secondary objective, and there was neither a separate sample size calculation nor a different proposed noninferiority margin for testing the effectiveness in children. Because of the small number of TB endpoints available for the estimation of noninferior effectiveness in children, the Wilson Score Interval for rare binomial events28,29 was used. This procedure allowed the construction of a highly conservative (ie, wider) 95% CI for comparison against the noninferiority margin. If the upper bound of the 95% CI was less than the noninferiority margin of 0.75%, then the noninferiority of the experimental arm would be established. To evaluate the potential effects of age and sex imbalances between study arms on the noninferiority test statistic, we ran a Monte Carlo sampling distribution simulation, weighted for age and sex, to eliminate potential bias from imbalances in enrollment (eAppendix 4 in the Supplement).
Results
We enrolled 1058 participants aged 2 to 17 years from June 11, 2001, through December 17, 2010. There were 552 in the combination-therapy group and 506 in the isoniazid-only group (intention-to-treat population) (Table 1, Figure 1, and eFigure in the Supplement). Fifteen children (3%) enrolled in the isoniazid-only group received at least some daily doses by directly observed therapy. Of the 1058 children enrolled, 905 were eligible for the efficacy analysis (modified intention-to-treat population) and 1032 received 1 or more dose of study medication (safety population). The most common reason for exclusion after enrollment was the finding of a negative TST result 8 to 12 weeks after a baseline negative TST result among children 5 years or younger who had a history of contact with an infectious patient with TB (91 of 153 [59%] children) (Figure 1). Of 1058 children enrolled, 989 (93%) were enrolled as contacts and 69 (7%) were enrolled with TST conversion (eAppendix 2 in the Supplement). Five (<1%) were infected with HIV. The differences by treatment arm in age and sex were larger than expected: the median age for the combination-therapy group was 10 years (interquartile range, 4–15) vs 12 years for the isoniazid-only group (interquartile range, 4–15); in the combination-therapy group, 54% were male vs 48% male in the isoniazid-only group (Table 1). The median TST size of the 929 participants with a TST reaction size of 5 mm or greater at enrollment was 15 mm (interquartile range, 12–20) and there was no significant difference in TST reaction size by age category (Table 1).
Table 1.
Clinical and Demographic Characteristics of the Study Population
| Patients by Treatment Arma |
||||
|---|---|---|---|---|
| Characteristic | Isoniazid (n = 506) | Rifapentine Plus Isoniazid (n = 552) | Total (N = 1058) | P Valueb |
| Indication for treatment of LTBI | ||||
| Close contact | 470 (92.9) | 519 (94.0) | 989 (93.5) | .46 |
| Recent TST result converter | 36 (7.1) | 33 (5.9) | 69 (6.5) | .46 |
| Age, median (IQR) | 12 (4–15) | 10 (4–15) | 11 (4–15) | .02 |
| Male sexc | 241 (47.6) | 297 (53.8) | 538 (50.9) | .005 |
| 2–4 y | 66 (13.0) | 85 (15.4) | 151 (14.3) | |
| 5–11 y | 45 (8.9) | 68 (12.3) | 113 (10.7) | |
| 12–17y | 130 (25.7) | 144 (26.1) | 274 (25.9) | |
| Race/ethnicity | ||||
| North America | ||||
| White Hispanicc | 301/431 (69.8) | 337/453 (74.4) | 638/884 (72.2) | .13 |
| 2–4 y | 92/431 (21.3) | 113/453 (24.9) | 205/884 (23.2) | |
| 5–11 y | 82/431 (19.0) | 93/453 (20.5) | 175/884 (19.8) | |
| 12–17 y | 127/431 (29.5) | 131/453 (28.9) | 258/884 (29.2) | |
| White non-Hispanicc | 18/431 (4.2) | 22/453 (4.9) | 40/884 (4.5) | .75 |
| 2–4 y | 2/431 (0.5) | 3/453 (0.7) | 5/884 (0.6) | |
| 5–11 y | 2/431 (0.5) | 6/453 (0.1) | 8/884 (0.9) | |
| 12–17 y | 14/431 (3.2) | 13/453 (2.9) | 27/884 (3.1) | |
| Blackc | 56/431 (13.0) | 51/453 (11.3) | 107/884 (12.1) | .47 |
| 2–4 y | 11/431 (2.6) | 17/453 (3.8) | 28/884 (3.2) | |
| 5–11 y | 8/431 (1.9) | 8/453 (1.8) | 16/884 (1.8) | |
| 12–17 y | 37/431 (8.6) | 26/453 (5.7) | 63/884 (7.1) | |
| Otherc | 56/431 (13.0) | 43/453 (9.5) | 99/884 (11.2) | .11 |
| 2–4 y | 13/431 (3.0) | 11/453 (2.4) | 24/884 (2.7) | |
| 5–11 y | 7/431 (1.6) | 15/453 (3.3) | 22/884 (2.5) | |
| 12–17 y | 36/431 (8.4) | 17/453 (3.8) | 53/884 (6.0) | |
| Brazilc,d | 73/504 (14.5) | 98/551 (17.8) | 171/1055 (16.2) | .16 |
| 2–4 y | 10/504 (2.0) | 24/551 (4.4) | 34/1055 (3.2) | |
| 5–11 y | 9/504 (1.8) | 11/551 (2.0) | 20/1055 (1.9) | |
| 12–17y | 54/504 (10.7) | 63/551 (11.4) | 117/1055 (11.1) | |
| Enrollment site | ||||
| US/Canada | 431 (85.2) | 453 (82.1) | 884 (83.6) | .18 |
| Brazil/Spain/Hong Kong | 75 (14.8) | 99 (17.9) | 174 (16.4) | .18 |
| HIV seropositivee | 1/111 (0.9) | 4/105 (3.8) | 5/216 (2.3) | .20 |
| Persons enrolled in a cluster | 155 (30.6) | 197 (35.7) | 352 (33.3) | .09 |
| TST reaction size, median (IQR), mmc,f | 15 (11–20) | 15 (12–20) | 15 (12–20) | |
| 2–4 y | 14 (11–18) | 15 (13–20) | 15 (12–20) | .46 |
| 5–11 y | 15 (12–20) | 15 (12–20) | 15 (12–20) | |
| 12–17y | 15 (11–20) | 15 (11–19) | 15 (11–20) | |
| BMI, median, (IQR)c | 19 (17–23) | 19 (16–23) | 19 (17–23) | |
| 2–4 y | 16 (15–18) | 17 (15–18) | 16 (15–18) | .29 |
| 5–11 y | 17 (16–20) | 18 (16–21) | 18 (16–21) | |
| 12–17y | 22 (19–26) | 22 (20–26) | 22 (20–26) | |
| Homeless | 5 (0.9) | 3 (0.5) | 8 (0.8) | .49 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HIV, human immunodeficiency virus; IQR, interquartile range; LTBI, latent tuberculosis infection; TST, tuberculin skin test.
Includes all children aged 2 to 17 years. Data are presented as number/total (percentage) unless otherwise specified.
P values are for Fisher exact test comparing proportions and the median scores for comparing continuous distributions. Although randomization was unrestricted, there was evidence in the parent study that household-based clustering resulted in some imbalance between arms.
P value refers to the overall characteristic by regimen, not age group.
Race not reported in US categories. Three children were outside North America or Brazil: 2 in the 5 to 11 age group and 1 in the 12 to 17 age group.
Of children with known HIV status.
Of children with TST result size greater than 0 mm (combined total, 929; 449 in the isoniazid-only group and 480 in the combination-therapy group). A total of 129 close contacts had enrollment TST result size of zero; of these, 128 were younger than 5 years, and 1 was aged 12 years and HIV seropositive.
The overall treatment completion rates were 88.1% in the combination-therapy group and 80.9% in the isoniazid-only group (P = .003) (Table 2). The rates of treatment discontinuation attributed to AEs were 1.7% in the combination-therapy group and 0.5% in the isoniazid-only group (P = .11) (Table 2). The 95% CI for the difference in rates of discontinuation attributed to an AE was −2.6 to 0.1, which is within the equivalence range of −5% to 5% (Table 2). The AEs that led to treatment discontinuation in the combination-therapy group included 3 influenza-like events, 3 cutaneous events (all with pruritic rash and 1 with oral blisters and fever), and 2 gastrointestinal tract events. The AEs that led to treatment discontinuation in the isoniazid-only group were 1 cutaneous reaction and 1 gastrointestinal tract event. In the combination-therapy group, treatment discontinuation attributed to unavailability for follow-up for 3 months or more during the treatment phase was significantly less than in the isoniazid-only group (P < .001) (Table 2), and no serious AEs were reported (Table 3).
Table 2.
Tolerability and Reasons for Discontinuation Among Children in the Modified Intention-to-Treat Population
| Patients, No. (%) |
||||
|---|---|---|---|---|
| Characteristic | Isoniazid (n = 434) | Rifapentine Plus Isoniazid (n = 471) | P Valuea | Difference (95% CI)b |
| Treatment completion | 351 (80.9) | 415 (88.1) | .003 | −7.2 (−2.0 to −2.5) |
| Reason for not completing treatment | ||||
| All reasons | 83 (19.2) | 56 (11.9) | .003 | 7.2 (2.5 to 12.0) |
| Discontinuation because of AEc | 2 (0.5) | 8 (1.7) | .11 | −1.2 (−2.6 to 0.1) |
| Withdrawal of informed consent | 5 (1.2) | 4 (0.9) | .74 | 0.3 (−1.0 to 1.6) |
| Lost for ≥3 mo during treatment | 26 (6.0) | 5 (1.1) | <.001 | 4.9 (2.5 to 7.4) |
| Physician decision to cancel other than AE | 7 (1.6) | 3 (0.6) | .21 | 1.0 (−0.4 to 2.4) |
| Participant refusal | 15 (3.5) | 16 (3.4) | >.99 | 0.1 (−2.3 to 2.4) |
| Total dose count and/or administration period outside of protocol guidelinesd | 28 (6.5) | 20 (4.3) | .18 | 2.2 (−0.7 to 5.2) |
Abbreviation: AE, adverse event.
P value based on Fisher exact test.
95% CI for the difference in proportions using the Wilson Score Interval method.
Combination-therapy group included 3 influenza-like AEs (grade 2), 3 cutaneous (all with pruritic rash [2 were grade 2], 1 with oral blisters and fever [grade 3]), and 2 gastrointestinal reactions (1 was grade 1 and 1 was grade 2). Isoniazid-only group included 1 cutaneous AE (grade 2) and 1 gastrointestinal reaction (grade 3).
Measure of adherence.
Table 3.
Safety End Points Among Children Who Received at Least 1 Dose of Study Medication
| Patients, No. (%) |
||||
|---|---|---|---|---|
| Characteristic | Isoniazid (n = 493) | Rifapentine Plus Isoniazid (n = 539) | P Valuea | Difference (95% CI)b |
| AEs attributed to treatment | ||||
| Grades 1 and 2 | 5 (1.0) | 11 (2.0) | .21 | −1.0 (−2.5 to 0.5) |
| Grade 3 | 1 (0.2) | 3 (0.6) | .63 | −0.4 (−1.1 to 0.4) |
| Grade 4 | 0 | 0 | NA | NA |
| Grade 5, death | 0 | 0 | NA | NA |
| Serious AEs | 0 | 0 | NA | NA |
| AEs not attributed to treatment | ||||
| Grades 1 and 2 | 35 (7.1) | 25 (4.6) | .11 | 2.0 (−0.4 to 5.3) |
| Grade 3 | 5 (0.2) | 3 (0.6) | .49 | 0.4 (−0.6 to 1.5) |
| Grade 4 | 2 (0.4) | 1 (0.2) | .61 | 0.2 (−0.5 to 0.9) |
| Grade 5, deathc | 2 (0.4) | 0 | .23 | 0.4 (−0.2 to 1.0) |
| Serious AEsd | 7 (1.4) | 0 | .01 | 1.0 (0.4 to 2.5) |
Abbreviations: AE, adverse event; NA, not available.
P value based on Fisher exact test.
95% CI for the differences in proportions using the Wilson Score Interval method.
Death 1 was due to malignant arrhythmia in a 16-year-old girl on day 201 of study treatment; death 2, gunshot injury in a 16-year-old boy at study day 901 (approximately 657 days after the end of the study treatment phase).
Serious AEs include deaths while receiving therapy or within 60 days of the last dose, life-threatening events, hospitalization, disability or permanent damage, and congenital anomaly. For children aged 2 through 16 years, 6 had 1 serious AE and 1 had more than 1 serious AE.
Four AEs attributed to treatment were scored as toxicity grade 3, including 3 of 539 (0.6%) in the combination-therapy group (1 influenza-like event and 2 cutaneous events) and 1 of 493 (0.2%) in the isoniazid-only group (hepatomegaly and rash) (Table 3). No hepatic events were attributed to treatment in either arm. One hepatic event was not attributed to treatment in a 3-year-old with a new diagnosis of Kawasaki disease and elevated liver enzyme values. No AEs were attributed to treatment among the 5 pediatric participants (aged 12–17 years) who were known to be HIV infected. There were 2 deaths in adolescents, both in the isoniazid-only group. One was caused by cardiac arrhythmia on day 201 of study treatment, and 1 was caused by a gunshot injury 657 days after completing treatment (Table 3).
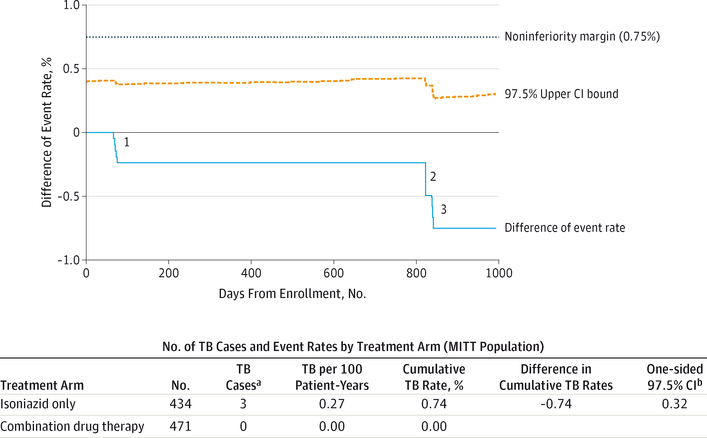
The modified intention-to-treat population (n = 905) accumulated 2320 person-years of follow-up. The cumulative proportion of children in whom TB was diagnosed was zero of 471 (0%) in the combination-therapy group vs 3 of 434 (cumulative rate, 0.74%) in the isoniazid-only group (1 with sputum culture positive for M tuberculosis and 2 by clinical criteria alone), for rates of 0 vs 0.27 per 100 person-years of follow-up. The observed difference in the rates of TB was −0.74%, of which the upper limit of the 1-sided 97.5% CI was 0.32%. This limit was below the noninferiority margin of 0.75% (Figure 2). The strength of rejecting the null hypothesis and the claim of noninferiority of the combination therapy with rifapentine and isoniazid compared with that of isoniazid only was not affected by the age and sex imbalance between the 2 study arms (eAppendix 4 in the Supplement).
Figure 2. Difference in Tuberculosis Disease Rates Between the 2 Treatment Regimens Over Time (MITT Population).
The figure shows how the noninferiority criterion was met when none of the 471 patients in the combination-therapy arm developed tuberculosis vs 3 of 434 in the isoniazid-only arm (cumulative rate, 0.74%), for a difference of −0.74% and an upper bound of the 97.5% CI of the difference of +0.32%. Per-protocol population effectiveness analysis showed similar results. The difference in cumulative TB disease rate is the rate in the combination-therapy arm minus the rate in the isozanid-only arm. The noninferiority margin was 0.75% for all analyses. Combination drug therapy indicates 3 months of directly observed, once-weekly combination of rifapentine and isoniazid; isoniazid only, 9 months of self-administered daily isoniazid; MITT, modified intention-to-treat; TB, tuberculosis.
a None had evidence of re-exposure to infectious TB: (1) one 14-year-old female was diagnosed 72 days after the first dose, with 2 cultures positive for Mycobacterium tuberculosis; (2) one 5-year-old male was clinically diagnosed 818 days after the first dose; and (3) one 2-year-old male was clinically diagnosed 839 days after the first dose.
b One-sided 97.5% CI for the difference in cumulative TB disease rates (percentage) using a conservative adjustment for a rare binomial event.28
Our trial was an open-label study in which children in the combination-therapy group were seen for treatment every week by a study health care professional, whereas participants in the isoniazid-only group were seen monthly. The knowledge of treatment assignment and increased frequency of contact with the study health care professional in the combination-therapy group could have introduced ascertainment bias when determining events to be attributed to study drugs. However, visits for clinical evaluation occurred at the same frequency (ie, monthly) in both study arms. The sample size obtained for this study population was larger than necessary for the 80% power needed to assess the main hypothesis of the safety of the 2 regimens. Unfortunately, we were unable to enroll children younger than 2 years, and only 5 children with HIV infection were enrolled, limiting generalizability to those high-risk groups.
Evaluation of the effectiveness of any regimen for LTBI is challenging because of the large sample size required for analysis.3,30,31 Our article describes a large pediatric population (approximately 1000 participants), including 539 children younger than 12 years and 296 children aged 2 to 4 years. Trial enrollment was expanded to the lower age ranges as soon as was feasible after completion of targeted pharmacokinetic studies. Even with active case finding, it is possible that some cases were missed. However, there is no evidence that ascertainment of cases varied by treatment arm.
Discussion
We found that combination therapy with rifapentine and isoniazid was well tolerated and safe in children aged 2 to 17 years who were treated for LTBI. The overall treatment completion rate was higher for combination therapy than isoniazid only (88.1% vs 80.9%). This outcome was consistent with findings in the main study18 as well as those of previous articles,12,13 which indicated that a shorter treatment regimen and direct observation of therapy correlate with higher completion rates. The rates of treatment discontinuation attributed to abandonment or refusal of further treatment for reasons other than medical indication were high, and were significantly higher among children who were treated with isoniazid only; the rates of treatment discontinuation attributed to an AE were low and similar in both treatment groups. Hepatotoxicity attributed to treatment–one of the AEs of most concern in adults treated with isoniazid–was not observed in children in this study. Deaths and serious AEs were rare and not related to either treatment regimen.
In general, children tolerate larger doses per kilogram of body weight and have fewer AEs when treated with anti-TB medications.32 Drug exposure was 1.3-fold higher in children compared with the exposures obtained with successful treatment for LTBI in adults in a pharmacokinetic substudy.33 By nesting a case-control pharmacokinetic evaluation comparing 81 children aged 2 to 11 years with 80 matched adults enrolled in the PREVENT TB trial, we were able to verify that the weight-based dosage recommendations for LTBI therapy with rifapentine (for 10–14 kg, 300 mg; 14.1–25 kg, 450 mg; 25.1–32 kg, 600 mg; and 32.1–50 kg, 750 mg) achieved the minimum target area under the concentration curve from time zero to infinity in almost all children. After evaluating several approaches the study protocol allowed for crushing the rifapentine tablets and producing a slurry by mixing the crushed medication with some types of food.23 This method of medication administration is not well standardized and adds complexity to treating children for LTBI. There is, at present, no pediatric formulation for rifapentine; a water-dispersible tablet for use in children is in development (Marilyn Maroni, MD, Sanofi, oral presentation, October 15, 2014).
The pharmacokinetic substudy confirmed that food increases rifapentine bioavailability in children by 40%.33 However, crushing the tablets to give them with food resulted in a 26% decrease in bioavailability, and between-subject variability in clearance was 40%.33 An evaluation of whether food influenced the safety or effectiveness of treatment was beyond the scope of this study. Current recommendations do not address whether combination therapy with rifapentine and isoniazid should be given with food.21
Our study also demonstrated that, in children, directly observed, once-weekly therapy with rifapentine plus isoniazid for 12 doses was as effective as isoniazid that was mostly self-administered daily for 9 months. The clinical trial setting might have increased the effect of isoniazid compared with its effect in an operational setting without the close monitoring and motivation of a clinical trial. This difference between clinical trial and operational settings might have less influence on a much shorter regimen, giving the short regimen an effectiveness advantage. Furthermore, the shorter regimen might encourage more treatment starts because of the promise of a briefer time commitment. More treatment starts and greater completion rates might together result in a standard regimen whereby rifapentine plus isoniazid prevent more cases of TB than are prevented by isoniazid alone.
Conclusions
Latent TB infection and TB in children are sentinel events for recent M tuberculosis transmission. Treating children with LTBI with a well-tolerated and safe regimen that is more likely to be completed than previous treatment regimens provides an improved opportunity to diminish the reservoir from which future TB cases and subsequent transmission will arise, although this effect will be smaller in high-incidence settings.
A 3-month (12-dose) regimen given by direct observation is a new alternative regimen to isoniazid for treatment of LTBI in children and adolescents.34
Supplementary Material
Acknowledgments
Funding/Support: Sanofi provided the rifapentine for this study and has donated more than $2.5 million to the CDC Foundation to supplement available US federal funding for rifapentine research.
Role of the Funder/Sponsor: Sanofi had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: Mr Scott and Dr Moro report being employed by the CDC Foundation, which receives funds for rifapentine research from Sanofi. Dr Weiner reports receiving a grant to perform rifapentine pharmacokinetics studies in children and adults for the University of Texas Health Science Center at San Antonio from Sanofi. Dr Sterling reports giving a 1-day consultation for Sanofi for presentation of PREVENT TB study data to the US Food and Drug Administration and being on the data safety monitoring board for a clinical trial sponsored by Otsuka Pharmaceutical. No other disclosures were reported.
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the CDC.
Group Information: A list of the International Maternal Pediatric and Adolescents AIDS Clinical Trials Group (IMPAACT) and the Tuberculosis Trials Consortium (TBTC) members is included in eAppendix 1 in the Supplement.
Previous Presentation: Preliminary results of this study were presented at ID Week 2012, a Joint Meeting of the Infectious Diseases Society of America, Society for Healthcare Epidemiology of America, HIV Medicine Association, and Pediatric Infectious Diseases Society; October 20, 2012; San Diego, California.
Contributor Information
M. Elsa Villarino, Division of Tuberculosis Elimination, Centers for Disease Control and Prevention (CDC), Atlanta, Georgia.
Nigel A. Scott, Division of Tuberculosis Elimination, Centers for Disease Control and Prevention (CDC), Atlanta, Georgia; CDC Foundation, Atlanta, Georgia.
Stephen E. Weis, Department of Medicine, University of North Texas Health Science Center at Ft Worth.
Marc Weiner, Department of Medicine, Audie L. Murphy San Antonio Veterans Administration Medical Center, San Antonio, Texas.
Marcus B. Conde, Department of Medicine, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil.
Brenda Jones, Department of Medicine, University of Southern California, Los Angeles.
Sharon Nachman, Department of Pediatrics, State University of New York at Stony Brook.
Ricardo Oliveira, Department of Pediatrics, Pediatric Institute, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil.
Ruth N. Moro, Division of Tuberculosis Elimination, Centers for Disease Control and Prevention (CDC), Atlanta, Georgia; CDC Foundation, Atlanta, Georgia.
Nong Shang, Division of Tuberculosis Elimination, Centers for Disease Control and Prevention (CDC), Atlanta, Georgia.
Stefan V. Goldberg, Division of Tuberculosis Elimination, Centers for Disease Control and Prevention (CDC), Atlanta, Georgia.
Timothy R. Sterling, Department of Medicine, Vanderbilt University School of Medicine, Nashville, Tennessee.
REFERENCES
- 1.Swaminathan S, Rekha B. Pediatric tuberculosis: global overview and challenges. Clin Infect Dis. 2010;50(suppl 3):S184–S194. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Global Tuberculosis Report 2012. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 3.Perez-Velez CM, Marais BJ. Tuberculosis in children. N Engl J Med. 2012;367(4):348–361. [DOI] [PubMed] [Google Scholar]
- 4.Ferebee SH. An epidemiological model of tuberculosis in the United States. Bull Nat Tubercu Assoc. 1967;53:4–7. [Google Scholar]
- 5.Heymann SJ, Brewer TF, Wilson ME, Colditz GA, Fineberg HV. Pediatric tuberculosis: what needs to be done to decrease morbidity and mortality. Pediatrics. 2000;106(1):1. [DOI] [PubMed] [Google Scholar]
- 6.Morrison J, Pai M, Hopewell PC. Tuberculosis and latent tuberculosis infection in close contacts of people with pulmonary tuberculosis in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2008;8(6):359–368. [DOI] [PubMed] [Google Scholar]
- 7.Rutherford ME, Hill PC, Triasih R, Sinfield R, van Crevel R, Graham SM. Preventive therapy in children exposed to Mycobacterium tuberculosis: problems and solutions. Trop Med Int Health. 2012; 17(10):1264–1273. [DOI] [PubMed] [Google Scholar]
- 8.Lincoln EM. The effect of antimicrobial therapy on the prognosis of primary tuberculosis in children. Am Rev Tuberc. 1954;69(5):682–689. [DOI] [PubMed] [Google Scholar]
- 9.Lincoln EM, Vera Cruz PG. Progress in treatment of tuberculosis: results of antimicrobial therapy in a group of 420 children with tuberculosis. Pediatrics. 1960;25(6):1035–1042. [PubMed] [Google Scholar]
- 10.Ferebee S, Mount FW, Anastasiades A. Prophylactic effects of isoniazid on primary tuberculosis in children: a preliminary report. Am Rev Tuberc. 1957;76(6):942–963. [DOI] [PubMed] [Google Scholar]
- 11.Ferebee SH. Controlled chemoprophylaxis trials in tuberculosis: a general review. Bibl Tuberc. 1970; 26:28–106. [PubMed] [Google Scholar]
- 12.International Union Against Tuberculosis Committee on Prophylaxis. Efficacy of various durations of isoniazid preventive therapy for tuberculosis: five years of follow-up in the IUAT trial. Bull World Health Organ. 1982;60(4):555–564. [PMC free article] [PubMed] [Google Scholar]
- 13.Horsburgh CR Jr, Goldberg S, Bethel J, et al. ; Tuberculosis Epidemiologic Studies Consortium. Latent TB infection treatment acceptance and completion in the United States and Canada. Chest. 2010;137(2):401–409. [DOI] [PubMed] [Google Scholar]
- 14.Spyridis NP, Spyridis PG, Gelesme A, et al. The effectiveness of a 9-month regimen of isoniazid alone versus 3- and 4-month regimens of isoniazid plus rifampin for treatment of latent tuberculosis infection in children: results of an 11-year randomized study. Clin Infect Dis. 2007;45(6):715–722. [DOI] [PubMed] [Google Scholar]
- 15.van Zyl S, Marais BJ, Hesseling AC, Gie RP, Beyers N, Schaaf HS. Adherence to anti-tuberculosis chemoprophylaxis and treatment in children. Int J Tuberc Lung Dis. 2006;10(1):13–18. [PubMed] [Google Scholar]
- 16.Pediatric Tuberculosis Collaborative Group. Targeted tuberculin skin testing and treatment of latent tuberculosis infection in children and adolescents. Pediatrics. 2004;114(4):1175–1201. doi: 10.1542/peds.2004-0809. [DOI] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Latent tuberculosis infection: a guide for primary health care providers. Bethesda, MD: US Dept of Health and Human Services, Centers for Disease Control and Prevention; 2013. http://www.cdc.gov/tb/publications/LTBI/default.htm. Accessed November22, 2014. [Google Scholar]
- 18.Sterling TR, Villarino ME, Borisov AS, et al. ; TB Trials Consortium PREVENT TB Study Team. Three months of rifapentine and isoniazid for latent tuberculosis infection. N Engl J Med. 2011;365(23): 2155–2166. [DOI] [PubMed] [Google Scholar]
- 19.Schechter M, Zajdenverg R, Falco G, et al. Weekly rifapentine/isoniazid or daily rifampin/pyrazinamide for latent tuberculosis in household contacts. Am J Respir Crit Care Med. 2006;173(8):922–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martinson NA, Barnes GL, Moulton LH, et al. New regimens to prevent tuberculosis in adults with HIV infection. N Engl J Med. 2011;365(1):11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Recommendations for use of an isoniazid-rifapentine regimen with direct observation to treat latent Mycobacterium tuberculosis infection. MMWR Morb Mortal Wkly Rep. 2011;60(48):1650–1653. [PubMed] [Google Scholar]
- 22.Blake MJ, Abdel-Rahman SM, Jacobs RF, Lowery NK, Sterling TR, Kearns GL. Pharmacokinetics of rifapentine in children. Pediatr Infect Dis J. 2006;25(5):405–409. [DOI] [PubMed] [Google Scholar]
- 23.Peloquin CA, Durbin D, Childs J, Sterling TR, Weiner M. Stability of antituberculosis drugs mixed in food. Clin Infect Dis. 2007;45(4):521. [DOI] [PubMed] [Google Scholar]
- 24.Food and Drug Administration. Guidance for industry and investigators on safety reporting requirements for investigational new drug applications and BA/BE studies. Washington, DC: US Dept of Health and Human Services, Food and Drug Administration; 2012. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm227351.pdf. Accessed November 22, 2014. [Google Scholar]
- 25.Cancer Therapy Evaluation Program. Common terminology criteria for adverse events. Bethesda, MD: National Cancer Institute, US National Institutes of Health; 1999. http://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcv20_4-30-992.pdf. Accessed November 22, 2014. [Google Scholar]
- 26.American Thoracic Society; US Department of Health and Human Services; US Public Health Service; Centers for Disease Control and Prevention. Diagnostic standards and classification of tuberculosis in adults and children. Washington, DC: US Dept of Health and Human Services, Public Health Service; 2000. [Google Scholar]
- 27.Pickering LK, Baker CJ, Kimberlin DW, Long SS. Red Book: 2012 Report of the Committee on Infectious Diseases. Elk Grove Village, IL: American Academy of Pediatrics; 2012. [Google Scholar]
- 28.Agresti AC, Brent A. Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat. 1998;52(2):119–126. doi: 10.2307/2685469. [DOI] [Google Scholar]
- 29.Newcombe RG. Interval estimation for the difference between independent proportions: comparison of eleven methods. Stat Med. 1998;17 (8):873–890. [DOI] [PubMed] [Google Scholar]
- 30.Brent AJ, Anderson ST, Kampmann B. Childhood tuberculosis: out of sight, out of mind? Trans R Soc Trop Med Hyg. 2008;102(3):217–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burman WJ, Cotton MF, Gibb DM, Walker AS, Vernon AA, Donald PR. Ensuring the involvement of children in the evaluation of new tuberculosis treatment regimens. PLoS Med. 2008;5(8):e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Starke JR. Childhood tuberculosis: treatment strategies and recent advances. Paediatr Respir Rev. 2001;2(2):103–112. [DOI] [PubMed] [Google Scholar]
- 33.Weiner MS, Mac Kenzie WR, Wing D, et al. Rifapentine pharmacokinetics and tolerability in children and adults treated once weekly with rifapentine and isoniazid for latent tuberculosis infection [published online January 16,2014]. J Ped Infect Dis Soc. doi: 10.1093/jpids/pit077. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization. Guidelines on the management of latent tuberculosis infection. Geneva, Switzerland: World Health Organization; 2015. http://www.who.int/tb/publications/ltbi_document_page/en/. Accessed November 22,2014. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.