Abstract
Background
During the first three months of pregnancy, the developing embryo may be susceptible to external and internal factors, which may lead to structural and functional congenital anomalies. The main objective of this study was to determine the prevalence of congenital anomalies in Addis Ababa and the Amhara region, Ethiopia.
Methods
A descriptive cross-sectional study was conducted on children 0–17 years of age who visited the 16 selected hospitals in Addis Ababa and the Amhara Region between January 1 and July 5, 2015. The proportions of neonates, infants, and children with external and internal congenital anomalies whether the anomalies were major or minor were estimated.
Results
Out of 76,201 children, 1518 of whom 57.6% were male identified with congenital anomalies. The overall proportion of congenital anomaly was 1.99% (95% CI: 1.89–2.091) i.e., 199 per 10,000 children. The proportion of neural tube defects, orofacial clefts, masculo-skeletal system anomalies, syndrome disorders, and cardiovascular system problems were 40.3% 37.7–43, 23.3% 21.3–25.4, 23.1% 20.9–25.2, 8% 6.7–9.4, and 2.6% 1.8–3.4, with a 95% CI, respectively. The majority (72.5%) of the mothers were multigravidae; 38(2.5%) of the mothers and 32(2.1%) of the fathers had history of other children with congenital anomalies. Similarly, 20(1.3%) of the participant children’s mothers and 17(1.1%) of the fathers had familial history of congenital anomaly. Iron folate and multivitamin use by mothers during preconception and early pregnancy was found to be low.
Conclusion
Neural tube defects, orofacial clefts, and musculoskeletal anomalies were the observed prevalent problems. Maternal illness, viral infections, and malnutrition were seen in a significant number of the mothers. Iron folate/folic acid and multivitamin use by the mothers during and before pregnancy was very low.
Keywords: Congenital anomaly, Children, Ethiopia
Background
During the first three months of pregnancy, the developing embryo may be susceptible to external and internal factors which may lead to congenital anomalies (CAs) [1–3]. CAs which can or cannot be observed at birth but often detected later in life are either structural or functional defects [4–6]. These occur in 3% of all births [7], affecting one in 33 babies [8, 9]; 2–3% [10] of the anomalies which account for 15–30% of the pediatric admissions are detected by the fifth year of life [9].
Genetic and environmental factors as well as maternal health conditions/diseases, substance abuse, and micronutrient deficiencies have linkages with the occurrences of CAs [2, 3, 7, 11–16]; which are also associated with chromosomal abnormalities; occurring due to errors in the numbers or structures of the chromosomes. For many CAs however the causes are still unknown [7, 17–22].
CAs cause deaths of children aged less than 1 year, particularly. Most CAs cause physical and mental disabilities in the affected children [23–26] as well as pregnancy losses through miscarriage and stillbirths [27, 28]. Worldwide, 6% (8.1 million) of new born children have CAs of genetic or partially genetic origins. Moreover, 3.3 million neonates die each year before they reach their fifth year, while 3.2 million children are disabled due to CAs [7, 23, 27–29].
The problems can occur as isolated or multiple anomalies [30] and can affect any part of the organ system of the developing embryo and vary in prevalence from country to country, race to race, or ethnicity to ethnicity [31, 32]. Problems that do not need medical treatment and have either no or just minimal cosmetic effects are known as minor anomalies, while those which require medical treatment [33, 34] and have serious health, psychosocial, and cosmetic effects are called major [35]. About 94% of the major CAs occur in developing countries, and death caused by them accounts for about 95% of all mortalities [23].
CAs can either be visible, like spina bifida (neural tube defects), orofacial clefts, omphalocele, gastroschisis, and reduction limb defects or invisible, such as heart defects, patent ductus arteriousus, tracheoesophageal atresia, and duodenal atresia [36].
In our previously published article, we reported the magnitude of birth defects as 1.9% [37] on the basis of a review of records from 2010 to 2014. The present study was conducted by using primary data collected between January 1 and July 5, 2015 because it was essential to explore the magnitude of the problem by using different data sources. In Ethiopia, CAs are neglected public health problems for parents/families who are affected with the problems. Besides, knowledge on the burden and the etiologies of the anomalies are limited. The main objective of this study was therefore to investigate the situation of CAs in Addis Ababa and the Amhara region and provide valuable information that may be used as baseline for further studies on the problem.
Methods
Study sites
Addis Ababa, the capital of Ethiopia and the Amhara region, the second largest in Ethiopia, were purposively selected.
Addis Ababa has an estimated total population of 3,273,001(47.4% male, 52.6% female) [38]. Almost all of the hospitals in the city provide various inpatient and outpatient services, including delivery. Only Cure International Children’s Hospital does not provide delivery services.
The Amhara region has an estimated total population of 20,399,004 (50.1% male, 49.9% female) [38]. The majority of the people live in rural areas. All of the hospitals in the regional state render different kinds of inpatient and outpatient services, including delivery.
Design of the study
The study was descriptive cross sectional. All children 0–17 years who visited the study hospitals for various medical services were screened for CAs. After diagnosis by pediatricians and other experienced medical doctors, the mothers/caretakers of children with CAs were interviewed to estimate the proportion of victims.
Sampling and sample size determination methods
Ten hospitals in Addis Ababa (6 public, 4 private) and six in the Amhara region (3 public, 3 private) were purposively included on the basis of case load. To screen children with CAs, we used the single population proportion formula and determined the minimum sample size required. We were bound to consider the prevalence of 1.9% [37] CAs on the 0–17 years of age group reported in Ethiopia. By using a 95% confidence interval, a 0.2% margin of error, and a design effect of 2, the minimal calculated sample size for screening for CAs was 36,950. Then, by adding a 10% contingency, the final sample size required for screening CAs was 41,056. However, to increase the degree of precision of the estimate, all children (76,201) visiting the study hospitals in the two regions during the study were screened for CAs. Then, only the mothers/caretakers of 1518 children with CAs were interviewed. All children with external and internal CAs whether the problems were major or minor were included without considering ethnicity, religion, social strata, residence, region, occupation, and education of parents/families/caretakers. Mothers/caretakers voluntarily participated on behalf of children.
Study population
The source population was all children in the age group of 0–17 years who visited the health facilities for various medical reasons during the study, while the study population included children 0-17 years who visited the facilities with CAs.
Data collection method
The data were collected in public and private hospitals which neonates, infants, and children visited for various medical care services. In the two study sites, children with CAs were carefully examined and diagnosed by pediatricians and other experienced medical doctors. After the diagnoses, relevant information was gathered by trained nurses, midwives, other health professionals, and the primary investigator by interviewing only mothers/caretakers whose children had CAs by using the structured questionnaire and a checklist. Data collected on the day the children were diagnosed with CAs included parental socio-economic status, residence, ethnicity, occupation, educational and nutritional status, exposures to teratogenic agents, CA history, pregnancy adverse outcomes, and parity. The data were collected in delivery rooms/wards, neonatal units, pediatric wards, clinics, and centers of cleft lip and palate between January 1 and July 5, 2015.
Data management and analysis
The data carefully checked daily by collectors were further examined by the primary investigator and entered into Epi-Info version 3.5.1 and transferred into SPSS version 21 for analysis. Data cleaning, error checking, and analysis were conducted by using SPSS, version 21. The confidence interval for the overall proportion of anomalies was calculated manually and the rest of the proportions and statistical analysis were conducted by using SPSS version 21. Descriptive frequency and proportion (with its corresponding 95% CI) were used to describe the results.
Ethical considerations
The ethical approval letter was collected from Addis Ababa University, College of Health Sciences Institutional Review Board; the National Research Ethics Review Committee; HARI-ALERT Ethical Review Committee; Addis Ababa City Administration Health Bureau Ethical Clearance Committee; and the Amhara National Regional State Health Bureau Regional Health Research Laboratory Center. Support letters were written to zonal health departments and the study hospitals by the health bureaus. The ethical and support letters were submitted to all study hospital administrators/medical directors. The purpose of the study was explained to the participant children’s mothers/caretakers. Data were collected after permission was obtained from the authorities and written consent was obtained from the children’s mother/caretakers. Data collected from the participants were kept in a secured and locked cabinet to maintain confidentiality.
Results
A total of 76,201 children visited the study hospitals for various medical care and treatment between January 1 and July 5, 2015. Out of these, 1518 were diagnosed with CAs. The overall proportion of CA was 1.99% (95% CI: 1.89–2.09) i.e. 199 children with CAs per 10,000. Of the total 1518 children with anomalies, 57.6% were male and 42.4% female with the age range of 0-17 years. One thousand two hundred eighty-nine (84.9%) of the children were 0-4 years old. About 52.4% were urban and 47.6% rural dwellers. Of the anomalies, the prevalence of neural tube, orofacial clefts, musculoskeletal system, syndrome disorders, cardiovascular system, genitourinary system, ear-nose-eye and head, and other defects were 40.3% (95% CI: 37.7–43), 23.3% (95% CI: 21.3–25.4), 23.1% (95% CI: 20.9–25.2), 8% (95% CI: 6.7–9.4), 2.6% (95% CI: 1.8–3.4), 1.7% (95% CI: 1.1–2.4), 0.7% (95% CI: 0.3–1.2), and 0.2% (95% CI: 0.0–0.5), respectively. The mean age of mothers 28.31 ranged from 15 to 49 years. About 83% of mothers was between 20 and 35 years old (see Table 1). Among the participant mothers, 90.3% were married, 40.4% had no formal education, and 57% were house wives (see Table 1). More than half of the participants were Christians (1043(68.7%)), followed by Muslims (466(30.7%)), and others were only 9(0.6%). The majority, 1470(48.42%) of the participants were Amhara, and Oromo, Guragie, Somali, Tigre, Siltie, and other ethnic groups constituted 870(28.66%), 181(5.96%), 133(4.38%), 122(4.02%), 87(2.86%), 173(5.7%) of the participants, respectively.
Table 1.
Socio-demographic characteristics of participants, Addis Ababa and the Amhara Region, Ethiopia, 2016
| Variable | Addis Ababa(n = 1076) | Amhara Region(n = 442) | Total | |||
|---|---|---|---|---|---|---|
| Number | (%) | Number | (%) | Number | (%) | |
| Child Gender | ||||||
| Male | 609 | 56.6 | 265 | 60 | 874 | 57.6 |
| Female | 467 | 43.4 | 177 | 40 | 644 | 42.4 |
| Child Age | ||||||
| 0-4 year | 909 | 84.5 | 380 | 86 | 1289 | 84.9 |
| 5-9 year | 109 | 10.1 | 50 | 11.3 | 159 | 10.5 |
| 10-14 year | 52 | 4.8 | 11 | 2.5 | 63 | 4.2 |
| 13-17 year | 6 | 0.6 | 1 | 0.2 | 7 | 0.5 |
| Residence | ||||||
| Urban | 628 | 58.4 | 167 | 37.8 | 795 | 52.4 |
| Rural | 448 | 41.6 | 275 | 62.2 | 723 | 47.6 |
| Children mother age | ||||||
| < 20 years | 60 | 5.6 | 16 | 3.6 | 76 | 5 |
| 20-35 years | 937 | 87.1 | 323 | 73.1 | 1260 | 83 |
| > 35 years | 79 | 7.3 | 103 | 23.3 | 182 | 12 |
| Marital status of mothers | ||||||
| Married | 973 | 90.4 | 397 | 89.8 | 1370 | 90.3 |
| Never married | 58 | 5.4 | 29 | 6.6 | 87 | 5.7 |
| Divorced/widowed | 45 | 4.2 | 16 | 3.7 | 61 | 4 |
| Occupation(child mother) | ||||||
| Housewife | 611 | 56.8 | 249 | 56.3 | 860 | 56.65 |
| Farmer | 103 | 9.6 | 120 | 27.1 | 223 | 14.69 |
| Employee | 208 | 19.3 | 27 | 6.1 | 235 | 15.48 |
| Merchant | 51 | 4.7 | 24 | 5.4 | 75 | 4.94 |
| Othera | 103 | 15.8 | 22 | 5 | 125 | 8.23 |
| Occupation(child father) | ||||||
| Employee | 469 | 43.6 | 92 | 20.8 | 560 | 36.89 |
| Farmer | 333 | 30.9 | 276 | 62.4 | 609 | 40.12 |
| Jobless | 158 | 14.7 | 52 | 11.8 | 210 | 13.83 |
| Student | 93 | 8.6 | 17 | 3.9 | 110 | 7.25 |
| Othera | 23 | 2.1 | 5 | 1.1 | 28 | 1.84 |
| Wealth quantile | ||||||
| Low income | 467 | 43.4 | 179 | 40.5 | 646 | 42.55 |
| Middle income | 521 | 48.4 | 223 | 50.5 | 744 | 49.01 |
| High income | 88 | 8.2 | 40 | 9.0 | 128 | 8.43 |
| Educational level | ||||||
| No education | 366 | 34 | 248 | 56.1 | 614 | 40.4 |
| Primary school(1-8th grade) | 348 | 32.3 | 119 | 26 | 467 | 30.8 |
| Secondary school(9-12grade) | 251 | 23.3 | 53 | 12.0 | 304 | 20.02 |
| College and above | 111 | 10.4 | 22 | 5 | 133 | 8.76 |
Othersa = Somali, Afar, Guragie, Argoba Benishangul, merchant, jobless, student, nomad
About 38(2.5%) of the mothers and 32(2.1%) of the fathers had history of other children with CA. Similarly, 20(1.3%) of the participant’s mothers and 17(1.1%) of the fathers had familial history of CA.
The majority, (72.5%), of the mothers were multigravidae. That is, CAs were more frequent in multigravidae and lower in primigravidae mothers. Some, (10.6%), of the mothers had history of 1–2 preterm babies, 11% 1–2 miscarriages, and 6.1% 1–2 still births. Of the children, 34.15% were 2nd order; 17.7% of the mothers had no antenatal care (ANC) follow ups, while 41.1% started ANC visits at 4-6 months (see Table 2).
Table 2.
Selected reproductive history of children’s mothers, Addis Ababa and the Amhara Region, Ethiopia, 2016 (n = 1518)
| Characteristics | Frequency | Percent | |
|---|---|---|---|
| Gravidity/Parity | Prim gravid | 417 | 27.50 |
| Multi-gravid | 1101 | 72.50 | |
| Total number of pregnancy | 1 | 417 | 27.50 |
| 2–3 | 627 | 41.30 | |
| 4–5 | 316 | 20.80 | |
| > 5 | 158 | 10.40 | |
| Full and post term | Post term | 38 | 2.50 |
| 1–2 full term | 842 | 55.50 | |
| 3–4 full term | 412 | 27.10 | |
| > 4 full term | 226 | 14.90 | |
| Preterm | None | 1357 | 89.40 |
| 1–2 | 161 | 10.60 | |
| Elective termination | None | 1427 | 94.00 |
| 1–2 | 91 | 6.00 | |
| Spontaneous miscarriage | None | 1350 | 88.90 |
| 1–2 | 167 | 11.00 | |
| 3–4 | 1 | 0.10 | |
| Still birth | None | 1425 | 93.90 |
| 1–2 | 93 | 6.10 | |
| Living children | None | 35 | 2.30 |
| 1–2 | 872 | 57.40 | |
| 3–4 | 410 | 27.00 | |
| > 4 | 201 | 13.20 | |
| Infant/child death | None | 1358 | 89.5 |
| 1–2 | 152 | 10 | |
| 3–4 | 7 | 0.5 | |
| > 4 | 1 | 0.1 | |
| Birth Order in multigravidae | 1st | 77 | 6.99 |
| 2nd | 376 | 34.15 | |
| 3rd | 253 | 22.98 | |
| 4th | 159 | 14.44 | |
| 5th | 113 | 10.26 | |
| >5th | 123 | 11.17 | |
| Antenatal Care (ANC) | Yes | 1249 | 82.3 |
| No | 269 | 17.7 | |
| Gestational age at first ANC | None | 269 | 17.7 |
| 1-3 months | 625 | 41.2 | |
| 4-6 months | 624 | 41.1 | |
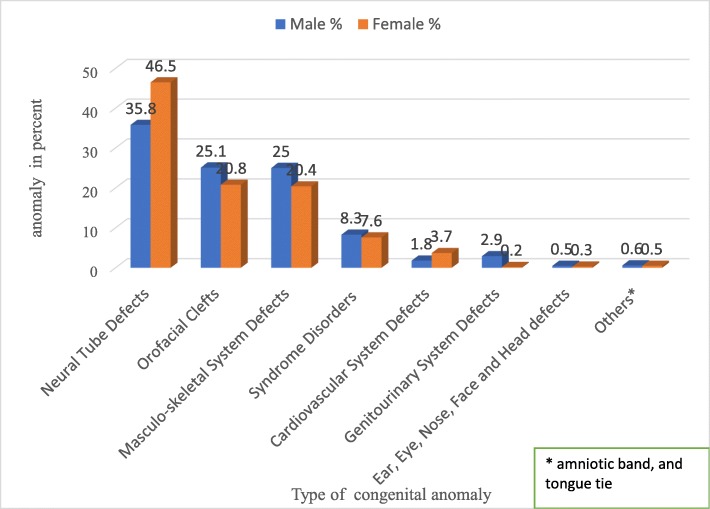
As presented in Table 3, the highest proportion (40.3%) of the anomalies were neural tube defects. With regard to sex, about 46.5% females had neural tube defects, whereas 25.1% of the males had orofacial clefts. Likewise, 25.0% of the males had masculo-skeletal anomalies, while 3.7% of the females had cardiovascular anomalies. On the other hand, there were 7.6% syndrome disorders (Down, Crouzon, Edward, TAR, and Rubellar) among the female children. Almost 2.9% of the genitourinary system anomalies occurred in the males (see Fig. 1). The distributions of some selected anomalies by type are presented in Table 4.
Table 3.
Congenital anomalies prevalence by study site and type of anomaly, Addis Ababa and the Amhara Region, Ethiopia, 2016
| Variable | Addis Ababa | Amhara Region | Total | |||
|---|---|---|---|---|---|---|
| Number | (%) | Number | (%) | Number | (%) | |
| Neural Tube Defect | 478 | 44.4 | 134 | 30.3 | 612 | 40.3 |
| Orofacial Cleft | 210 | 19.5 | 144 | 32.6 | 354 | 23.3 |
| Musculoskeletal System Defects | 290 | 27.0 | 60 | 13.6 | 350 | 23.05 |
| Syndrome Disorder | 29 | 2.7 | 93 | 21.0 | 122 | 8.04 |
| Cardiovascular System defects | 38 | 3.5 | 2 | 0.5 | 40 | 2.6 |
| Genitourinary System Defects | 22 | 2.0 | 4 | 0.9 | 26 | 1.7 |
| Ear, Eye, Nose, Face and Head Defects | 4 | 0.37 | 2 | 0.45 | 6 | 0.39 |
| Othersa | 5 | 0.46 | 3 | 0.67 | 8 | 0.53 |
aamniotic band, tongue tie
Fig. 1.
Distribution of congenital anomalies by sex, Addis Ababa and the Amhara Region, Ethiopia, 2016
Table 4.
Percentage distribution of selected congenital anomalies by types of anomaly, Addis Ababa and the Amhara Region, Ethiopia, 2016
| Type of congenital anomalies | Frequency | Percent |
|---|---|---|
| Spina bifida | 268 | 17.70 |
| Hydrocephalus | 180 | 11.90 |
| Spina bifida with hydrocephalus and club foot | 58 | 3.82 |
| Anencephaly | 36 | 2.40 |
| Bilateral cleft lip and palate | 25 | 1.60 |
| Bilateral cleft lip | 24 | 1.60 |
| Unilateral cleft lip and palate | 13 | 0.90 |
| Ventricular septal defect | 20 | 1.30 |
| Omphalocele | 14 | 0.90 |
| Syndrome disorders (Down syndrome, Edward Syndrome etc) | 103 | 6.80 |
| Bilateral club foot | 108 | 7.10 |
| Unilateral club foot | 72 | 4.74 |
| Imperforated anus | 23 | 1.50 |
| Spine defects(Congenital Scoliosis) | 51 | 3.30 |
| Hypospadia | 15 | 1.00 |
| Tracheoesophageal fistula | 10 | 0.70 |
As shown in Table 5, among the children’s mothers, about 9.7% had maternal illness; 17.1% had history of passive smoking of cigarettes; 11.5% used un-prescribed/illicit drugs; 5.5% had history of blood relationship with the children’s fathers; 4.9% had history of exposure to chemicals; and 1.8% had history of exposure to radiation during early pregnancy.
Table 5.
Response of children’s mothers (“yes” response) for selected risk factors for congenital anomalies, Addis Ababa and the Amhara region, Ethiopia, 2016 (n = 1518)
| Characteristics | Frequency | Percent |
|---|---|---|
| Maternal illness during early pregnancy | 148 | 9.7 |
| Smoked cigarette during pregnancy | 13 | 0.85 |
| Passively Smoked during pregnancy | 259 | 17.1 |
| Drunk alcohol during pregnancy | 403 | 26.5 |
| Used un-prescribed/illicit drug early pregnancy | 175 | 11.5 |
| Exposure to radiation (child mother) | 28 | 1.8 |
| Child father exposed to radiation | 29 | 1.9 |
| Blood relation between child parents | 83 | 5.5 |
| Exposed to chemicals | 74 | 4.9 |
| Other exposure that concern parents | 86 | 5.7 |
| Viral infection during early pregnancy | 14 | 0.9 |
| Contraceptive pills use around conception | 154 | 10.1 |
| Anemia during early pregnancy | 244 | 16.1 |
| Fertility enhancing drug use | 38 | 2.5 |
| Folic acid use during pregnancy | 75 | 4.94 |
| Iron use during early pregnancy | 53 | 3.5 |
| Multivitamins use before pregnancy | 13 | 0.9 |
| Multivitamins use during pregnancy | 16 | 1.1 |
| Food shortage during pregnancy | 160 | 10.5 |
| Used vegetables/fruits during pregnancy | 458 | 30.2 |
Out of the mothers, 0.9% had viral infections and 16.1% anemia during the first 3 months of pregnancy. Around 4.94% of the mothers took folic acid during early pregnancy, while the majority of the mothers (95.06%) took (consumed) no folic acid during early pregnancy. Besides, 3.5% of the mothers took iron for the treatment of anemia (see Table 5).
Almost 10.5% of the mothers had food shortage during pregnancy. In terms of vegetables/fruits use, nearly 30.2% of the mothers took vegetable/fruit combined with other food items (staple food) during pregnancy, while 69.8% took (consumed) no vegetables/fruits throughout their pregnancy. Only 0.9 and 1.1% of the mothers consumed multivitamins before and during pregnancy, respectively (see Table 5).
The proportion of anomalies were 979(64.5%) for Addis Ababa and 539(35.5%) for the Amhara region. The frequency of CAs by study hospitals in Addis Ababa and the Amhara region are presented in Table 6.
Table 6.
Congenital anomalies prevalence among the study hospitals, Addis Ababa and the Amhara Region, Ethiopia, 2016
| Hospital name, level by national millennium standard, ownership, and study place | |||
|---|---|---|---|
| Level of hospital | Number of CA cases | Percent | |
| Addis Ababa | |||
| Public Hospitals | |||
| Zewditu Memorial Hospital | Secondary | 495 | 46.0 |
| Tikur Anbesa General Specialized Hospital | Tertiary | 242 | 22.5 |
| Yekatit 12 Hospital Medical College | Secondary | 81 | 7.5 |
| St. Paul’s Hospital Millennium Medical College | Tertiary | 25 | 2.3 |
| ALERT Center (Hospital) | Secondary | 12 | 1.1 |
| Ghandi Hospital | Secondary | 7 | 0.7 |
| Private Hospitals | |||
| Cure Ethiopia International Children’s Hospital | aSpecial | 171 | 15.9 |
| Addis Hiwet General Hospital | Secondary | 12 | 1.1 |
| MCM Korean General Hospital | Secondary | 20 | 1.9 |
| Betsegah Special Women’s and Children’s Hospital | aSpecial | 11 | 1.0 |
| Amhara Region | |||
| Public Hospitals | |||
| Desse Referral Hospital | Secondary | 160 | 36.3 |
| Felegehiwet Comprehensive Specialized Hospital | Tertiary | 78 | 17.6 |
| University of Gondar Specialized Hospital | Tertiary | 78 | 17.6 |
| Private Hospitals | |||
| Gamby Teaching Medical Sciences College Hospital | Secondary | 86 | 19.5 |
| Ibex General Hospital | aSecondary during data collection period, but now leveled as primary | 24 | 5.4 |
| Selam General Hospital | Secondary | 16 | 3.6 |
aCA Congenital Anomaly
One thousand three hundred seventy-nine (90.8%) of the anomalies were single, while 139(9.2%) were multiple (i.e. more than one anomaly in one child in two or more organ systems). About 39(2.6%) of the victims of neural tube defects had other associated CAs (i.e. multiple anomalies). Other anomalies that had associated CAs, just like neural tube defects were Down syndrome and omphalocele, which accounted for 7(0.46%) and 5(0.33%) of the participants, respectively. Furthermore, 1499(98.7%) of the anomalies were major, whereas 19(1.3%) were minor.
Discussion
In this study, the overall proportion of CAs was 1.99%, almost 2%. This finding is quite close to the result (1.9%) of our previous study on birth defects [37]. Another point to consider here is that our work published previously was carried out by using record reviews from 2010 to 2014. In contrast, the present study was conducted by using primary data (by interviewing children’s mothers/caretakers). The similarity of the two findings may be due to the correspondence of the participants in terms of some characteristics, for instance, residence, geographical area, socioeconomic status, and behavioral factors. Here, the point is to check whether it is necessary to determine the magnitude of CAs by using a variety of data sources at different time or in various years. Thus, these studies could help to find out the similarities or differences in magnitude of two different data sources.
Furthermore, the finding of this study is similar to that of a study conducted in Egypt (2%) by Shawky and Sadik [33], and close to the result of a study done in India (2.22%) by Sarkar et al. [39], but higher than those of studies carried out in Lahore (0.75/10,000) by Parker et al. [40], and Saudi Arabia (1.14%) by Al Bu Ali et al. [41], and less than the findings of studies conducted in Lebanon (2.4%) by Francine et al. [7], and Iran (2.8%) by Karbasi et al. [16]. Again, the finding of the present study is lower compared to those of studies conducted in Tanzania (29%) [42], Nigeria (28.15 per 1000 children) [43], and Palestine (21%) [29], and Gaza (14%) [44]. Furthermore, the finding of this study was less than the findings of those studies conducted in the United States of America, the United Kingdom, Italy, and Canada [45–48]. These differences could be due to variations in environmental factors and the instruments used for diagnosing CAs, such as ultrasound, x-ray, electrocardiograph, and magnetic resonance imaging (MRI scan). In this study, we didn’t use the magnetic resonance imaging device because the majority of the study hospitals had no such devices during the data collection. Basically, we are confident that the finding of our study is adequate to give a clear picture of the situation of CAs in Ethiopian. In addition, from the present study, we can learn that CAs are a big problem that merit due attention. Also, it should be noted that Ethiopia has no surveillance and registry systems for CAs which are lifelong risks for citizens. Hence, policy makers, programmers, and health care providers should plan to teach the community about CAs and schedule for surveillance and registry systems, and monitor the occurrence of the problem in the population and provide comprehensive treatment, care, and rehabilitation services for affected children.
In the current study, the most frequent CAs were neural tube defects. This high rate could be due to no or low use of iron folate during peri-conception and early pregnancy. Moreover, the high prevalence of neural tube defects could be due to the fact that children with neural tube defects survive despite the dangerous nature of the problem. Studies conducted in Tanzania [42], Nigeria [43], Palestine [29], and China [49] reported the occurrence of central nervous system anomalies as 29.8, 6.87, 18.81 and 20.1%, respectively. These findings suggest that central nervous system anomalies are the most frequently manifested problems.
In the present study, spina bifida were the most frequent neural tube defects, followed by hydrocephalus, and anencephaly. These findings were different from the spina bifida and anencephaly of 10.6 and 6.9 per 10,000, respectively, reported in China [49]. This variation may be due to genetic/environmental factors and low use of iron folate.
In this study, the second most frequently observed CAs were orofacial clefts followed by masculo-skeletal system anomalies, syndrome disorders (Down, Crouzon, Edward, and congenital Rubellar) plus cardiovascular and genitourinary system anomalies, and others. However, this finding does not correspond to those of other studies in terms of proportion and sequence.
In our study, more males were affected than females by most types of the CAs observed. The reason why we showed the difference between sexes was to indicate the proportion of anomalies among male and female children. Similar findings, which showed that more males were affected than females reported the contrast as follows: Nigeria 52 and 48% [43], Iran 51.9 and 48.1% [10], and Pakistan 68.3 and 31.7% [16]. The reason why males were more affected by CAs than females may be that chromosomal abnormalities and mutations in genes that influence the genetic pathways may be more common in males than in females. This, however needs further scientific investigations.
Furthermore, in the present study, the majority of the anomalies were major rather than minor. This could be due to the fact that children with minor anomalies were not visiting hospitals for diagnosis. Likewise, the majority of the anomalies were single, while the minority were multiple. Multiple anomalies were observed in children with neural tube defects. Similarly, children who had syndrome disorders (for example Down’s syndrome) and omphalocele were seen with other associated CAs. This finding was different from those of other studies maybe due to differences in causative agents, study places, and genetic variations.
In the present study, the majority of the mothers were multigravidae rather than primigravidae, showing the positive relationship between gravidity and CAs. Similarly, Sarkar et al. [39], Lei et al. [50], and Anyanwu et al. [43] reported associations between gravidity and CAs.
Some of the mothers reported that they had maternal illness; some said they were passive smokers; others informed us that they suffered from viral infections; and a small group reported that they were malnourished during early pregnancy. On the other hand, other similar studies indicated that malnutrition, smoking cigarettes, and illicit drugs were associated with CAs [51]. However, it should be noted that cigarette smoking is not common among Ethiopian women.
In our study, folic acid/iron folate, vegetable/fruit use, and multivitamin consumption before and during pregnancy were very low. This finding was similar with our previous study [52]. This might be due to the fact that the majority of the women could not get iron folate/folic acid and multivitamin in their peri-conception and early pregnancy. In addition, it might be due to low awareness of mothers about iron folate, multivitamin, and vegetable uses for normal body functions and healthy living. Several studies suggested that folic acid [53–55] and multivitamin containing folic acid usage during early pregnancy reduce/protect from the occurrence of CAs [55–61].
In this study, parental lifestyle factors, such as alcohol use, un-prescribed/illicit drugs, blood relationship among parents, exposure to chemicals, exposure to radiation, preterm, miscarriage, still birth, infant death, family history, birth order, anemia, and occupation had notable relationships with CAs. Furthermore, many studies indicated that the associations of the factors mentioned and CAs were positively related [10, 13, 36, 49, 62–66].
The limitation of this study was that it was not supported by special tests, such as genetic/chromosomal defect laboratory investigations and viral infection markers. In addition, medical geneticists and pediatric surgeons were not involved in the study. The other inherent limitation was recall bias. To minimize the bias, we made efforts to retrieve information by giving enough time to participants to enable them remember events during pregnancy and after delivery. We wish to suggest that large population-based studies are required to determine the prevalence of CAs rather than hospital-based attempts like ours.
Conclusion
In conclusion, this study indicated that neural tube defects, orofacial clefts, and musculoskeletal anomalies were momentous and influential problems which need attention. Maternal illnesses, viral infections, and malnutrition were observed in a significant number of mothers. In addition, iron folate/folic acid and multivitamin use by mothers was very low. On the whole, the proportions observed in the study indicated that a significant number of children were affected and suffered from the impacts of CAs. The problem thus necessitates immediate preventive actions. One of the prevention methods is iron folate supplementation. Therefore, women in the reproductive age groups should be supplemented with iron folate during peri-conception and early pregnancy by health care providers. Further investigations should also be conducted to explore/identify the associated risk factors of CAs and determine prevalence rates. We recommend that researchers conduct analytical and home-based birth studies in the future.
Acknowledgements
We would like to express our deep appreciation and acknowledgement to midwives, nurses, and other health professionals working at the study hospitals for their active participation and assistance. We wish to acknowledge the medical directors and managers of the respective hospitals for their support and permission. We would like to thank Addis Ababa University and the University of Gondar for their support.
Abbreviations
- ANC
Antenatal care
- CA
Congenital anomaly
- CAs
Congenital anomalies
- CI
Confidence interval
Authors’ contributions
Conceived the idea: MT. Designed the study methodology: MT, AW. Conducted the study: MT, MA, WF, ED, AW. Analyzed the data: MT, MA, ED, AW. Interpreted the results: MT, MA, WF, ED, AW. Wrote the draft manuscript: MT. Revised and edited the final manuscript: MT, MA, WF, ED, AW. Approved the manuscript: MT, MA, WF, ED, AW.
Funding
This study received money from Addis Ababa University and the University of Gondar for data collection only. The authors declare that they have received no funds for the publication of this manuscript and that they have no external source of fund for both data collection and publication.
Availability of data and materials
The data set supporting this study are available in the manuscript.
Ethics approval and consent to participate
This study obtained ethical approval from Addis Ababa University, College of Health Sciences Institutional Review Board, the National Research Ethics Review Committee, HARI/ALERT Ethics Review Committee, Addis Ababa City Administration Health Bureau Ethical Clearance Committee, and the Amhara National Regional State Health Bureau Regional Health Research Laboratory Center. The participants gave written informed consent prior to interviews and discussions.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Molla Taye, Email: mollataye2@gmail.com.
Mekbeb Afework, Email: m.afework@yahoo.com.
Wondwossen Fantaye, Email: fawondwossen@yahoo.com.
Ermias Diro, Email: ermi_diro@yahoo.com.
Alemayehu Worku, Email: alemayehuwy@yahoo.com.
References
- 1.Musumeci G, Castrogiovanni P, Trovato F, Parenti R, Szychlinska M, Imbesi R. Pregnancy, embryo-fetal development and nutrition: physiology around fetal programming. J Histol Histopathol. 2015;2(1). 10.7243/2055-7091X-7242-7241http://www.hoajonline.com/journals/pdf/2055-7091X-7242-7241.pdf.
- 2.Ekwere EO, McNeil R, Agim B, Jeminiwa B, Oni O, Pam S. A retrospective study of congenital anomalies presented at tertiary health facilities in JOS. Nigeria JPCS. 2011;3:24–8. https://pdfs.semanticscholar.org/.../dd885c1fa85c908e529984b69cd2b87a.
- 3.The McGraw-Hill Companies . Congenital malformations. In: Kumar P, Burton B, editors. Evidence Base Evaluation and Management, USA. 2008. [Google Scholar]
- 4.Boyle B, McConkey R, Garne E, Loane M, Addor MC, Bakker MK, Boyd PA, Gatt M, Greenlees R, Haeusler M, et al. Trends in the prevalence, risk and pregnancy outcome of multiple births with congenital anomaly: a registry-based study in 14 European countries 1984-2007. BJOG. 2013;120(6):707–716. doi: 10.1111/1471-0528.12146. [DOI] [PubMed] [Google Scholar]
- 5.Campana H, Pawluk MS, Lopez Camelo JS, Grupo de Estudio del E Births prevalence of 27 selected congenital anomalies in 7 geographic regions of Argentina. Arch Argent Pediatr. 2010;108(5):409–417. doi: 10.1590/S0325-00752010000500006. [DOI] [PubMed] [Google Scholar]
- 6.Arbour L, Beking K, Le ND RPA, Spinelli JJ, Teschke K, Gallagher RP, Abanto ZU, Dimich-Ward H. Rates of congenital anomalies and other adverse birth outcomes in an offspring cohort of registered nurses from British Columbia, Canada. Can Public Health Assoc. 2010;101(3):230–234. doi: 10.1007/BF03404379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Francine R, Psascale S, Aline H. Congenital anomalies: prevalence and risk factors. Universal J Public Health. 2014;2(2):58–63. [Google Scholar]
- 8.Lemacks J, Fowles K, Mateus A, Thomas K. Insights from parents about caring for a child with birth defects. Int J Environ Res Public Health. 2013;10:3465–3482. doi: 10.3390/ijerph10083465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohammed AR, Mohammed SA-R, AbdulFetah AMH. Congenital anomalies among children: knowledge and attitude of Egyptian and Saudi mothers. J Biol Agric Healthcare. 2013;3(20):18–29. [Google Scholar]
- 10.Raza MZ, Sheikh A, Ahmed SS, Sajid A, Naqvi SMA. Risk factors associated with birth defects at a tertiary care center in Pakistan. Ital J Pediatr. 2012;38(68):1–7. doi: 10.1186/1824-7288-38-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alborz A. Environmental characteristics and prevalence of birth defects among children in post-war Iraq: implications for policies on rebuilding the Iraqi education system. Med Confl Surviv. 2013;29(1):26–44. doi: 10.1080/13623699.2013.765197. [DOI] [PubMed] [Google Scholar]
- 12.Gianicolo EA, Mangia C, Cervino M, Bruni A, Andreassi MG, Latini G. Congenital anomalies among live births in a high environmental risk area--a case-control study in Brindisi (southern Italy) Environ Res. 2014;128:9–14. doi: 10.1016/j.envres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Kalaskar R, Kalaskar A, Naqvi FS, Tawani GS, Walke DR. Prevalence and evaluation of environmental risk factors associated with cleft lip and palate in a central Indian population. Pediatr Dent. 2013;35(3):279–283. [PubMed] [Google Scholar]
- 14.Obu HA, Chinawa JM, Uleanya ND, Adimora GN, Obi IE. Congenital malformations among newborns admitted in the neonatal unit of a tertiary hospital in Enugu, south-East Nigeria- a retrospective study. BMC Res Notes. 2012;5(177):1–6. doi: 10.1186/1756-0500-5-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurinczuk JJ, Hollowell J, Boyd PA, Oakley L, Brocklehurst P, Gray R. Inequalities in infant mortality project briefing paper 4: the contribution of congenital anomalies to infant mortality. Oxford: National Perinatal Epidemiology Unit; 2010. pp. 1–13. [Google Scholar]
- 16.Karbasi SA, Golestan M, Fallah R, Mirnaseri F, Barkhordari K, Bafghee MS. Prevalence of congenital malformations. Acta Med Iran. 2009;47(2):149–153. [Google Scholar]
- 17.Boyd PA, Loane M, Garne E, Khoshnood B, Dolk H, Group Ew Sex chromosome trisomies in Europe: prevalence, prenatal detection and outcome of pregnancy. Eur J Hum Genet. 2011;19(2):231–234. doi: 10.1038/ejhg.2010.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chuchracki M, Szczepaniak A, Sedziak A, Ziolkowska K, Opala T. Frequency of prevalence of turner syndrome in fetuses of patients referred to genetic amniocentesis in 2007-2011. Przegl Lek. 2012;69(10):1011–1014. [PubMed] [Google Scholar]
- 19.Alhalabi M, Kenj M, Monem F, Mahayri Z, Abou Alchamat G, Madania A. High prevalence of genetic abnormalities in Middle Eastern patients with idiopathic non-obstructive azoospermia. J Assist Reprod Genet. 2013; 30(6):799–805.doi:710.1007/s10815-10013-19995-zhttp://www.ncbi.nlm.nih.gov/pubmed/23615726. [DOI] [PMC free article] [PubMed]
- 20.Loane M, Morris JK, Addor MC, Arriola L, Budd J, Doray B, Garne E, Gatt M, Haeusler M, Khoshnood B, et al. Twenty-year trends in the prevalence of Down syndrome and other trisomies in Europe: impact of maternal age and prenatal screening. Eur J Hum Genet. 2013;21(1):27–33. doi: 10.1038/ejhg.2012.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Presson AP, Partyka G, Jensen KM, Devine OJ, Rasmussen SA, McCabe LL, McCabe ER. Current estimate of Down syndrome population prevalence in the United States. J Pediatr. 2013;163(4):1163–1168. doi: 10.1016/j.jpeds.2013.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pournima G, Monica Y, Meghna S. Crouzon syndrome: a case report. Eur J Dent Med. 2012;4:8–13. [Google Scholar]
- 23.Canaku D, Toçi E, Roshi E, Burazeri G. Prevalence and factors associated with congenital malformations in Tirana Albania during 2011–2013. Mater Sociomed. 2014;26(3):158–162. doi: 10.5455/msm.2014.26.158-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mutafoglu-Uysal K, Gunes D, Tufekci O, Kalelihan-Cankal A, Sarialioglu F, Olgun N. The incidence of congenital malformations in children with cancer. Turk J Pediatr. 2009;51(5):444–452. [PubMed] [Google Scholar]
- 25.Nader S, Ghasem S, Fakher R, Sohayla N. Incidence of head and neck birth defects in Iran: a cross-sectional study from southwest region. Pak J Med Sci. 2009;25(5):770–774. [Google Scholar]
- 26.Serra-Juhe C, Rodriguez-Santiago B, Cusco I, Vendrell T, Camats N, Toran N, Perez-Jurado LA. Contribution of rare copy number variants to isolated human malformations. PLoS One. 2012;7(10):1–8. doi: 10.1371/journal.pone.0045530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization, Regional Office for South-East Asia. Workshop on birth defects surveillance. Colombo Sri Lanka. 10-13 April 2012.
- 28.Dai L, Zhu J, Liang J, Wang Y-P, Wang H, Mao M. Birth defects surveillance in China. World J Pediatr. 2011;7(4):302–310. doi: 10.1007/s12519-011-0326-0. [DOI] [PubMed] [Google Scholar]
- 29.Butt F, Shahzad R, Pasha I. Pattern and outcome of congenital anomalies and maternal risk factors association. Biomedica. 2013;29:234–239. [Google Scholar]
- 30.Tayebi N, Yazdani K, Naghshin N. The prevalence of congenital malformations and its correlation with consanguineous marriages. Oman Med J. 2010;25(1):37–40. doi: 10.5001/omj.2010.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Delport SD, Christianson AL, van den Berg HJ, Wolmarans L, Gericke GS. Congenital anomalies in black south African liveborn neonates at an urban academic hospital. S Afr Med J. 1995;85(1):15–20. [PubMed]
- 32.Kucik JE, Alverson CJ, Gilboa SM, Correa A. Racial/ethnic variations in the prevalence of selected major birth defects, metropolitan Atlanta, 1994-2005. Public Health Rep. 2012;127:52–61. doi: 10.1177/003335491212700106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shawky RM, Sadik DI. Congenital malformations prevalent among Egyptian children and associated risk factors. Egypt J Med Hum Genet. 2011;12:69–78. [Google Scholar]
- 34.Sun G, Xu ZM, Liang JF, Li L, Tang DX. Twelve-year prevalence of common neonatal congenital malformations in Zhejiang Province, China. World J Pediatr. 2011;7(4):331–336. doi: 10.1007/s12519-011-0328-y. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization/US-Center for Disease Control and Prevention/International Clearance House on Birth Defects Surveillance and Research . Birth defects surveillance: a manual for programme managers. Geneva: World Health Organization; 2014. [Google Scholar]
- 36.Prajapati V, Kacha AR, Kakkad KM, Damor PB, Nandaniya AM. Study of congenital malformation in neonates born at tertiary care hospital. Nat J Community Med. 2015;6(1):30–34. [Google Scholar]
- 37.Taye M, Afework M, Fantaye W, Diro E, Worku A. Magnitude of Birth Defects in Central and Northwest Ethiopia from 2010–2014: A Descriptive Retrospective Study. PLoS ONE. 2016;11(10):e0161998. doi: 10.1371/journal.pone.0161998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Central Statistical Agency {Ethiopia}. Statistical abstracts: population projection of Ethiopia for all Regions at Wereda Levels, from 2014-2017. Addis Ababa, Ethiopia, Central Statistical Agency; 2013.
- 39.Sarkar S, Patra C, Dasgupta MK, Nayek K, Karmakar PR. Prevalence of congenital anomalies in neonates and associated risk factors in a tertiary care hospital in eastern India. J Clin Neonatology. 2013;2(3):131–134. doi: 10.4103/2249-4847.119998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, Anderson P, Mason CA, Collins JS, Kirby RS, et al. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010;88(12):1008–1016. doi: 10.1002/bdra.20735. [DOI] [PubMed] [Google Scholar]
- 41.Al Bu Ali WH, Balaha MH, Al Moghannum MS, Hashim I. Risk factors and birth prevalence of birth defects and inborn errors of metabolism in Al Ahsa, Saudi Arabia. Pan Afr Med J. 2011;8:14. doi: 10.4314/pamj.v8i1.71064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mashuda F, Zuechner A, Chalya PL, Kidenya BR, Manyama M. Pattern and factors associated with congenital anomalies among young infants admitted at Bugando medical centre, Mwanza, Tanzania. BMC Res Notes. 2014;7(195). 10.1186/1756-0500-1187-1195http://www.biomedcentral.com/1756-0500/1187/1195. [DOI] [PMC free article] [PubMed]
- 43.Anyanwu L-JC, Danborno B, Hamman WO. Birth prevalence of overt congenital anomalies in Kano Metropolis: overt congenital anomalies in the Kano. Universal J Public Health. 2015;3(2):89–96. [Google Scholar]
- 44.Naim A, Al Dalies H, El Balawi M, Salem E, Al Meziny K, Al Shawwa R, Minutolo R, Manduca P. Birth defects in Gaza: prevalence, types, familiarity and correlation with environmental factors. Int J Environ Res Public Health. 2012;9(5):1732–1747. doi: 10.3390/ijerph9051732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Egbe A, Uppu S, Lee S, Stroustrup A, Ho D, Srivastava S. Congenital malformations in the newborn population: A Population Study and Analysis of the Effect of Sex and Prematurity. Pediatr Neonatol. 2015; 56: 25–30. 10.1016/j.pedneo.2014.1003.1010. Available online at www.sciencedirect.com. journal homepage: http://www.pediatr-neonatol.com. [DOI] [PubMed]
- 46.Glinianaia VS, Tennant WGP, Rankin J. Risk estimates of recurrent congenital anomalies in the UK: a population-based register study. BMC Med. 2017;15:20. doi: 10.1186/s12916-017-0789-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Santoro M, Minichilli F, Pierini A, Astolfi G, Bisceglia L, Carbone P, Conti S, Dardanoni G, et al. Congenital anomalies in contaminated sites: A Multisite Study in Italy. Int. J. Environ. Res. Public Health. 2017;14, 292 doi:210.3390/ijerph14030292. www.mdpi.com/journal/ijerph. [DOI] [PMC free article] [PubMed]
- 48.Zhao JP, Sheehy O, Bérard A. Regional variations in the prevalence of major congenital malformations in Quebec: the importance of fetal growth environment. J Popul Ther Clin Pharmacol. 2015;22(3):e198–e210. [PubMed] [Google Scholar]
- 49.Zhang X, Li S, Wu S, Hao X, Guo S, Suzuki K, Yokomichi H, Yamagata Z. Prevalence of birth defects and risk-factor analysis from a population-based survey in Inner Mongolia, China. BMC Pediatr. 2012;12(125). 10.1186/1471-2431-12-125. [DOI] [PMC free article] [PubMed]
- 50.Lei RL, Chen HS, Huang BY, Chen YC, Chen PK, Lee HY, Chang CW, Wu CL. Population-based study of birth prevalence and factors associated with cleft lip and/or palate in Taiwan 2002-2009. PLoS One. 2013;8(3):e58690. doi: 10.1371/journal.pone.0058690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhu M, Druschel C, Lin S. Maternal birthplace and major congenital malformations among New York Hispanics. Birth Defects Res (Part A) 2006;76:467–473. doi: 10.1002/bdra.20270. [DOI] [PubMed] [Google Scholar]
- 52.Taye M, Afework M, Fantaye W, Diro E, Worku A. Factors associated with congenital anomalies in Addis Ababa and the Amhara region, Ethiopia: a case-control study. BMC Pediatr. 2018;18:142. doi: 10.1186/s12887-018-1096-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kondo A, Kamihira O, Ozawa H. Neural tube defects: prevalence, etiology and prevention. Int J Urol. 2009;16:49–57. doi: 10.1111/j.1442-2042.2008.02163.x. [DOI] [PubMed] [Google Scholar]
- 54.Salih MAM, Murshid WR, Mohamed AG, Ignacio LC, Jesus JE, Baabbad R, Bushra HME. Risk factors for neural tube defects in Riyadh City, Saudi Arabia: case-control study. Sudanese J Paediatr. 2014;14(2):49–60. [PMC free article] [PubMed] [Google Scholar]
- 55.Kishimba RS, Mpembeni R, Mghamba J. Factors associated with major structural birth defects among newborns delivered at Muhimbili National Hospital and Municipal Hospitals in Dar Es Salaam, Tanzania 2011–2012. Pan Afr Med J. 2015;20(153). 10.11604/pamj.12015.11620.11153.14492 available online at: http://www.panafrican-med-journal.com/content/article/11620/11153/full/. [DOI] [PMC free article] [PubMed]
- 56.Bedard T, Lowry RB, Sibbald B, Harder JR, Trevenen C, Horobec V, Dyck JD. Folic acid fortification and the birth prevalence of congenital heart defect cases in Alberta, Canada. Birth Defects Res A Clin Mol Teratol. 2013;97(8):564–570. doi: 10.1002/bdra.23162. [DOI] [PubMed] [Google Scholar]
- 57.Csaky-Szunyogh M, Vereczkey A, Kosa Z, Gerencser B, Czeizel AE. Risk and protective factors in the origin of conotruncal defects of heart--a population-based case-control study. Am J Med Genet A. 2013;161(10):2444–2452. doi: 10.1002/ajmg.a.36118. [DOI] [PubMed] [Google Scholar]
- 58.Fernandez N, Henao-Mejia J, Monterrey P, Perez J, Zarante I. Association between maternal prenatal vitamin use and congenital abnormalities of the genitourinary tract in a developing country. J Pediatr Urol. 2012;8:121–126. doi: 10.1016/j.jpurol.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 59.Khoshnood B, Loane M, Garne E, Addor MC, Arriola L, Bakker M, Barisic I, Bianca S, Boyd P, Calzolari E, et al. Recent decrease in the prevalence of congenital heart defects in Europe. J Pediatr. 2013;162(1):108–113. doi: 10.1016/j.jpeds.2012.06.035. [DOI] [PubMed] [Google Scholar]
- 60.De Wals P, Tairou F, Allen MIV, Soo-Hong U, Lowry RB, Sibbald B, Evans JA, Van den Hof MC, Zimmer P, Crowley M, et al. Reduction in neural-tube defects after folic acid fortification in Canada. N Engl J Med. 2007;357(2):135–142. doi: 10.1056/NEJMoa067103. [DOI] [PubMed] [Google Scholar]
- 61.Bailey LB, Berry RJ. Folic acid supplementation and the occurrence of congenital heart defects, orofacial clefts, multiple births, and miscarriage 1–3. Am J Clin Nutr. 2005;81(1):1213S–12137S. doi: 10.1093/ajcn/81.5.1213. [DOI] [PubMed] [Google Scholar]
- 62.Barseghyan K, Aghajanian P, Miller DA. The prevalence of preterm births in pregnancies complicated with fetal gastroschisis. Arch Gynecol Obstet. 2012;286(4):889–892. doi: 10.1007/s00404-012-2394-3. [DOI] [PubMed] [Google Scholar]
- 63.Bittles AH, Black ML. The impact of consanguinity on neonatal and infant health. Early Hum Dev. 2010;86(11):737–741. doi: 10.1016/j.earlhumdev.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 64.Desrosiers TA, Herring AH, Shapira SK, Hooiveld M, Luben TJ, Herdt-Losavio ML, Lin S, Olshan AF, Study NBDP. Paternal occupation and birth defects: findings from the national birth defects prevention study. Occup Environ Med. 2013;69(8):534–542. doi: 10.1136/oemed-2011-100372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.O'Leary CM, Nassar N, Kurinczuk JJ, de Klerk N, Geelhoed E, Elliott EJ, Bower C. Prenatal alcohol exposure and risk of birth defects. Pediatrics. 2010;126(4):e843–e850. doi: 10.1542/peds.2010-0256. [DOI] [PubMed] [Google Scholar]
- 66.Forrester MB, Merz RD. Risk of selected birth defects with prenatal illicit drug use, Hawaii, 1986–2002. J Toxicol Environ Health A. 2007;70:7–18. doi: 10.1080/15287390600748799. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data set supporting this study are available in the manuscript.