Abstract
Introduction:
We estimated the unit costs for implementing postpartum intrauterine contraceptive device (PPIUCD) services from the perspective of both health system and development agencies.
Methodology:
Seven districts from two Indian states, i.e., Uttarakhand (UK) and Madhya Pradesh (MP), were selected to study the cost of PPIUCD service. Data on costs incurred both by health system and development agencies for PPIUCD service were collected. Unit costs were estimated for providing PPIUCD and IUCD services by state and district level of care in public health-care system. We also estimated unit cost per couple-year protected (CYP) by the level of the health facility.
Results:
We found that the unit cost per PPIUCD insertion including all costs, i.e., for service delivery and program support, was INR 522 ($8.7) and INR 502 ($8.4) in MP and UK, respectively. Similarly, the unit costs per interval IUCD insertion were INR 287 ($4.8) in UK and INR 281 ($4.7) in MP. Development partners have a share of >50% in overall costs. From a health system's perspective, PPIUCD and interval IUCD cost per CYP at the level of district hospital were INR 440 ($7.3) and INR 449 ($7.5), respectively.
Conclusions:
In India, PPIUCD, being a low-cost procedure, should be considered as a primary strategy targeted toward pregnancy spacing over other contraceptory methods.
Keywords: Couple-year protected, health-care costing, intrauterine contraceptive device, postpartum intrauterine contraceptive device, unit cost
INTRODUCTION
To achieve the goal of “Universal Health Coverage”, it is recommended to include family planning as an integral part of the focused efforts.[1] Therefore, the Government of India has envisaged to expand the family planning services as a part of sustained efforts to achieve Sustainable Development Goals 3.1 and 3.2, which are related to the reduction of maternal and child mortality.[2]
In Indian context, several studies had been undertaken evaluating the postpartum intrauterine contraceptive device (PPIUCD) and interval intrauterine contraceptive device (IUCD) methods of contraception in terms of their efficacy, safety, acceptability, etc.,[3,4,5,6,7] but there is limited evidence on their costs. In order to meet this gap, we undertook a study both from health system and development partner's perspective, to assess the unit cost of delivering PPIUCD services. Second, we compare the unit costs for implementing PPIUCD services and interval IUCD available as routine service for pregnancy spacing.
METHODOLOGY
Study area
Out of 29 states, PPIUCD service is currently being implemented in 19 states of India. Two states were selected to study the cost of PPIUCD service, i.e., Uttarakhand (UK) and Madhya Pradesh (MP). Implementation of PPIUCD program in India is supported by multiple development partners across the states. In UK and MP, PPIUCD program was implemented with technical support from “Jhpiego – an affiliate of Johns Hopkins University.” Another factor which favored the selection of UK was that it is one of the earliest states where program implementation started. Total districts in the two states were first divided into three categories, i.e., low-, moderate-, and high-performing districts based on the number of PPIUCD insertions from April 2013 to March 2014. We selected 10% of districts as well as facilities (out of overall in the state) for data collection in the study. In UK, one low- and one high-performing districts were selected. Similarly, in MP, we selected two high-performing (Bhopal and Narsingpur), one moderately performing (Indore), and two low-performing (Hosangabad and Guna) districts among the fifty districts in MP. In UK, we selected two district hospitals (DH), three community health centers (CHCs), and one primary health center (PHC). Similarly, in MP, we covered five DHs, three CHCs, and one PHC.
Data collection
In the current study, we aimed to assess the economic cost of implementing PPIUCD as a family planning method. Semi-structured questionnaires with pertinent questions were used to capture the costs. These questionnaires were adapted from previous studies with an aim to assess the health service delivery at primary and secondary level in India.[8,9,10,11] We used a bottom-up micro-costing approach to collect the data on health system resources for a time period of 1 year, i.e., from April 2013 to March 2014. Cost centers were identified at each level of facility functioning for service delivery or program support. Similar data were also collected for interval IUCD service which was being delivered as a part of routine family planning services package. Data on salaries and other allowances disbursed to medical, nonmedical, and support staff working at facility level with less or more contribution toward the PPIUCD service were collected. We reviewed the routine records comprised of monthly reports, stock registers, and indent records to collect the data on consumables, drugs, equipment, and overheads. Data on building space being used for the services were captured by doing a physical survey of the facility. Costs which do not come as direct expenses to provide the service were also included to meet the horizon of economic perspective of this study. Such costs include state- and national-level staff involved in the trainings, capacity building, monitoring, and supervision of this service.
Alongside health system costs, resources spent by development partners in the same period (April 2013 to March 2014) to provide technical support at different levels were also captured. Jhpiego as a collaborator provides the technical support, and henceforth their resources utilized at state or national level were also accounted for estimating unit costs.
Data on number of beneficiaries
Month-wise data on the number of beneficiaries in year 2013–2014 of this service were collected from all the health facilities covered for cost data collection, used as denominator in the estimation of unit costs. The data were taken specifically for beneficiaries of either of the two family planning services, i.e., PPIUCD and interval IUCD procedures.
Cost data analysis
Cost data collected for capital and recurrent costs were analyzed using standard methods available in literature.[12,13,14] Health system costs are usually shared in nature with a provision of delivery of package of services, i.e., being used for more than one program or activity. Thus, we apportioned the cost for service being evaluated using apportioning statistics. These apportioning factors were derived on the basis of average time required to perform each procedure and average duration of stay at different places (labor room, operation theater, and in-patient ward) within the health facility which was based on interviews of medical staff at health facilities involved in service delivery. Details of apportioning statistics are provided in supplementary appendix document.
Capital costs such as buildings rented or space utilized at health facility level for providing PPIUCD service along with other maternal health services in health system or by external agencies were estimated using the prevailing market rental prices. Annualized costs of capital goods such as equipment and furniture with useful life of more than a year were calculated. A standard discounting rate of 3% was applied. Average market prices for drugs, consumables, and nonconsumables were preferred over government-subsidized prices in view of the economic perspective of the study as the use of subsidized prices generally leads to underestimation of economic costs. Recurrent costs were also analyzed for the year 2013–2014 to arrive at the overall estimates for providing PPIUCD service. Finally, the cost estimates derived using standard procedures were converted to United States Dollars (USD-$) using the average exchange rates (INR 60 = 1 USD) for the year 2014, to make it comparable at wider level.[15]
Unit cost estimation
We categorized the costs as service delivery costs and program support costs. Service delivery costs mainly comprised of direct cost of consumables, supplies, and personnel costs, whereas, program support costs included costs of monitoring and evaluation, supervision, behaviour change communication (BCC), capacity building, advocacy, and health education. Program support costs were assessed separately for health system and development partners. We estimated per beneficiary unit cost of service delivery and program support from health system and development partners. Unit cost per PPIUCD and interval IUCD insertion at three different levels of health facilities, i.e., district level, CHC level, and PHC level was computed. To estimate the 95% confidence limits around unit cost estimate, 999 data simulations were done using bootstrap technique.
Using the methodology introduced by Janowitz and Bratt, we also estimated unit costs per couple-year protected (CYP) at all the levels of health facility in our study.[14] We used the same assumptions that all IUCD users were followed up thrice in the 1st year and twice in 2nd and 3rd year, with 80% compliance.[16] We assumed that the average duration of IUCD use to be 3 years.[17] Our study data did not have the scope of estimating the cost per outpatient department (OPD) follow-up visit and cost per IUCD removal; therefore, we used the cost estimates per outpatient consultation given by some recent studies. Using these estimates, we estimated the unit cost of service delivery per CYP for DH, CHC, and PHC.[8,18] Further, we assumed cost per IUCD removal to be 50% of the cost of insertion. Hence, cost per CYP was calculated using the following formula:
where; C (insertion) = Cost of IUCD insertion
n = Number of follow-up visits
C (follow-up visit) = Cost per OPD follow-up visit
C (removal) = Cost per IUCD removal
AMC = Average method continuation in years.
Sensitivity analysis
Given assumptions made for CYP estimation, we have performed a univariate sensitivity analysis to assess the impact of uncertainty in the follow-up visit cost and cost of removal of IUCD on CYP estimate. To vary the unit cost per follow-up visit, confidence intervals reported for base estimates from the same studies were used.[8,18] In base case scenario, cost of removal of IUCD was assumed to be 50% of the cost of IUCD insertion. For sensitivity analysis, this cost was varied from 25% to 75% of cost of insertion of IUCD as lower limit (LL) and upper limit (UL). We report the percentage change in CYP cost with change in parameters considered for sensitivity analysis.
RESULTS
Beneficiaries
Overall, we found that 18% of women opted for PPIUCD as a method of contraception. Almost double the women opted for PPIUCD at CHC and PHC level in MP than UK.
Annual costs (service delivery)
Health system costs
The annual cost of delivering PPIUCD was INR 861,842 ($14,364) and INR 1,087,798 ($18,130) in UK and MP, respectively. For interval IUCD, annual service delivery costs were INR 691,330 ($11,522) and INR 685,666 ($11,428) in UK and MP, respectively [Table 1]. Medicines and consumables accounted for >90% of the total expenditure in both the states [Table 2].
Table 1.
Annual service delivery cost of postpartum intrauterine contraceptive device and interval intrauterine contraceptive device service (2013-2014)
| Facility type | Health system costs, INR (USD) | |
|---|---|---|
| PPIUCD | IUCD | |
| DH | 1,564,143 (26,069) | 1,015,810 (16,930) |
| CHC | 288,479 (4808) | 326,281 (5438) |
| PHC | 20,464 (341) | 4802 (80) |
| State | ||
| Madhya Pradesh | 1,087,798 (18,130) | 685,666 (11,428) |
| Uttrakhand | 861,842 (14,364) | 691,330 (11,522) |
INR: Indian National Rupee, USD: United States Dollar, DH: District hospital, CHC: Community health center, PHC: Primary health center, PPIUCD: Postpartum intrauterine contraceptive device, IUCD: Interval intrauterine contraceptive device
Table 2.
Health system costs under different heads for delivering postpartum intrauterine contraceptive device and interval intrauterine contraceptive device services in Madhya Pradesh and Uttrakhand, India
| Cost heads | PPIUCD | IUCD | ||
|---|---|---|---|---|
| INR (USD) | Percentage | INR (USD) | Percentage | |
| Health system Uttarakhand* | ||||
| Personnel | 27,593 (460) | 3.2 | 27,995 (467) | 4.0 |
| Equipment | 137 (2) | 0.0 | 240 (4) | 0.0 |
| Medicines and consumables | 780,024 (13,000) | 90.5 | 635,333 (10,589) | 91.9 |
| Physical infrastructure | 3663 (61) | 0.4 | 5741 (96) | 0.8 |
| Utility/overheads | 884 (15) | 0.1 | 838 (14) | 0.1 |
| State support | 48,384 (806) | 5.6 | 20,677 (345) | 3.0 |
| National support | 1158 (19) | 0.1 | 506 (8) | 0.1 |
| Total | 861,842 (14,364) | 100.0 | 691,330 (11,522) | 100.0 |
| Health system Madhya Pradesh* | ||||
| Personnel | 60,306 (1005) | 5.5 | 62,616 (1044) | 9.1 |
| Equipment | 512 (9) | 0.0 | 532 (9) | 0.1 |
| Medicines and consumables* | 989,997 (16,500) | 91.0 | 601,867 (10,031) | 87.8% |
| Physical infrastructure | 9653 (161) | 0.9 | 11,380 (190) | 1.7% |
| Utility/overheads | 319 (5) | 0.0 | 350 (6) | 0.1% |
| State support | 24,116 (402) | 2.2 | 7656 (128) | 1.1% |
| National support | 2894 (48) | 0.3 | 1265 (21) | 0.2% |
| Total | 1,087,798 (18,130) | 100.0 | 685,666 (11,428) | 100% |
*No extra medicines were given to women undergoing PPIUCD insertion. Therefore, there were no incremental costs of medicines in case of PPIUCD. PPIUCD: Postpartum intrauterine contraceptive device, IUCD: Interval intrauterine contraceptive device, INR: Indian National Rupee, USD: United States Dollar
Unit costs
The overall health system cost per PPIUCD insertion was found to be INR 274 ($4.6) and INR 276 ($4.6) in MP and UK, respectively. Overall, cost per IUCD insertion was slightly higher than the unit costs per PPIUCD insertion, i.e., INR 287 ($4.8) and INR 281 ($4.7) in MP and UK, respectively [Figure 1]. The health system service delivery cost per PPIUCD insertion was INR 267 ($4.5) and INR 260 ($4.3) in MP and UK, respectively. Similarly, service delivery cost per interval IUCD insertion in UK and MP was INR 273 ($4.5) and INR 284 ($4.7), respectively [Figure 1].
Figure 1.
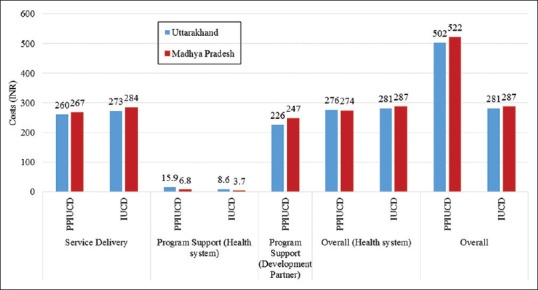
Unit cost for delivering postpartum intrauterine contraceptive device and interval intrauterine contraceptive device services in the two study states, India
Overall, unit cost per PPIUCD insertion including all costs, i.e., for service delivery and program support, was INR 522 ($8.7) and INR 502 ($8.4) in MP and UK, respectively [Figure 1]. Similarly, the unit costs per interval IUCD insertion were INR 287 ($4.8) in UK and INR 281 ($4.7) in MP [Figure 1]. Service delivery costs per PPIUCD insertion at the level of DH, CHC, and PHC were INR 265 ($4.4), INR 287 ($4.8), and INR 207 ($3.4), respectively [Figure 2]. In both the states, health system had >50% share in the total cost.
Figure 2.
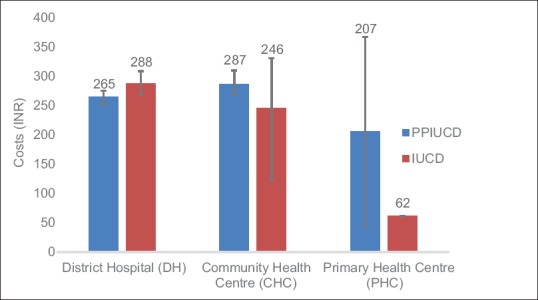
Health system cost per beneficiary for delivering postpartum intrauterine contraceptive device and interval intrauterine contraceptive device services at different levels of facilities in Uttarakhand and Madhya Pradesh, India
Cost of couple-year protected
We also estimated the cost per CYP at all the level of health facilities, i.e., DH, CHC, and PHC. From a health system's perspective, PPIUCD and interval IUCD cost per CYP at the level of DH was INR 440 ($7.3) and INR 449($7.5), respectively. Similarly, PPIUCD and interval IUCD cost per CYP at CHC was INR 459 ($7.6) and INR 461 ($7.7), whereas at PHC, it was INR 359 ($ 6) and INR 290 ($4.8), respectively.
Sensitivity analysis
Findings from univariate sensitivity analysis suggest that, with change in unit cost per follow-up consultation, CYP cost at DH level varied from 15.7% for LL and 24.2% for UL for PPIUCD, whereas for IUCD, it varied from 15.4% for LL and 23.7% for UL. At CHC and PHC level, CYP cost for PPIUCD varied from 18.7% to 23.2% and 15.6% to 17.2%, respectively. Similarly, CYP cost for IUCD varied from 18.6% to 23.1% and 19.3% to 21.2% at CHC and PHC level, respectively. With variation in cost of IUCD removal, CYP cost for PPIUCD and IUCD varied by 5% on either side both for DH and CHC level, while the variation at PHC level was 4.6% and 1.8% on either side for PPIUCD and IUCD, respectively.
DISCUSSION
The study was undertaken to assess the unit cost of service delivery and program support for PPIUCD services in India both from health system and development partner's perspective. Second, we compared the unit costs of service delivery and program support for implementing PPIUCD services and interval IUCD available as routine service for pregnancy spacing and limiting.
Overall cost per PPIUCD insertion had slight variation between the states as it was found to be INR 522 ($8.7) in MP and INR 502 ($8.4) in UK. Service delivery cost per PPIUCD insertion was almost same, i.e., INR 267 ($4.5) in MP and INR 260 ($4.3) in UK. Consumables which include the IUCD device alone account for 90% of the costs.
Our results are in concurrence with the estimates given by the United Nations Population Fund study, wherein it was found that the commodities had the maximum share in the expenditures incurred. Overall health system costs for service provisioning of PPIUCD against interval IUCD were slightly higher as PPIUCD was being carried out immediately after birth, but IUCD had to be carried out separately which involved greater time expense of human resources. The health system costs per beneficiary for delivering PPIUCD services were higher at CHC and PHC level compared to that of IUCD costs. Higher PPIUCD costs at CHC and PHC could be explained in view that the majority of PPIUCD procedures were being done within 10 min after childbirth assisted by a medical doctor, whereas in case of interval IUCD, majority of the procedures are assisted by staff nurse. Therefore, involvement of doctors in PPIUCD procedures is a determinant of higher costs.
The costs per CYP were found to be similar both for PPIUCD and interval IUCD at DH and CHC level. However, costs per CYP for PPIUCD were higher compared to interval IUCD at PHC level. This may be attributed to the fact that there were more number of follow-up visits by the patients in case of PPIUCD as it was carried out after delivery and the patients were visiting the health-care facility for seeking other routine services such as immnuization and outdoor patient services.
Strengths and limitations
The data in our study were collected at all the levels of public health facilities which covered all the aspects of program in terms of provisioning and costing of PPIUCD and interval IUCD as a method of birth spacing in the family planning basket. Our study accounts for both service delivery and program costs incurred by health system and development partners for delivering the PPIUCD services. Costs and effects should be viewed side by side to inform policy decisions, which is possible only by conducting full economic evaluations.
CONCLUSIONS AND RECOMMENDATIONS
At present, in India, the unit cost per PPIUCD insertion is low in DHs and CHCs as compared to that of PHCs. PPIUCD services should be made available at delivery points with high delivery load to make our health-care delivery system more equitable. PPIUCD, being a low-cost procedure, should be considered as a primary strategy targeted toward pregnancy spacing over other contraceptory methods. Currently, almost half of the costs for implementing PPIUCD services in India are incurred by development partners for program support, i.e., for capacity building, supervision, monitoring, and evaluation. However, the government may think of having some alternate and more sustainable mechanism for program support, preferably through the health-care system.
PPIUCD procedure, though a low-cost family planning strategy which makes it favorable, must be evaluated further under full economic evaluations to inform policy decisions.
Financial support and sponsorship
The study was funded by Jhpiego – an affiliate of Johns Hopkins University, New Delhi, India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We gratefully acknowledge the role of Dr. Vikas Yadav and Dr. Sudharsanam Manni Balasubramaniam, Jhpiego – an affiliate of Johns Hopkins University, New Delhi, in facilitating the overall research study including data collection. We are also thankful to Dr. Neeta Bhatnagar and Dr. Jyoti Benawri for the necessary facilitation in the collection of health facility data in the respective states of UK and MP. The study was funded by Jhpiego – an affiliate of Johns Hopkins University, New Delhi, India. The funding agency had no role in the collection of data, its analysis or interpretation, writing of this paper, or the decision to publish.
REFERENCES
- 1.Government of India. India's ‘Vision FP 2020’. Family Planning Division. New Delhi: Ministry of Health and Family Welfare, Government of India; 2014. [Google Scholar]
- 2.United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. United Nations. 2015 [Google Scholar]
- 3.Gautam R, Arya KN, Kharakwal S, Singh S, Trivedi M. Overview of immediate PPIUCD application in Bundelkhand region. J Evol Med Dent Sci. 2014;3:9518–26. [Google Scholar]
- 4.Goswami G, Yadav K, Patel A. A prospective study to evaluate safety, efficacy and expulsion rate of post placental insertion of intra uterine device. J Evol Med Dent Sci. 2013;4:9769–73. [Google Scholar]
- 5.Gupta A, Verma A, Chauhan J. Evaluation of PPIUCD versus interval IUCD (380A) insertion in a teaching hospital of Western U.P. Int J Reprod Contracept Obstet Gynecol. 2013;2:204–8. [Google Scholar]
- 6.Kanhere A, Pateriya P, Jain M. Acceptability and feasibility of immediate postpartum IUCD insertion in a tertiary care centre in central India. Int J Reprod Contracept Obstet Gynecol. 2015;4:179–84. [Google Scholar]
- 7.Singh S, Malik R, Ahalawat R, Taneja BK. Evaluation of efficacy, expulsion and safety of post-placental and intra-cesarean insertion of intrauterine contraceptive devices. Int J Reprod Contracept Obstet Gynecol. 2015;4:2005–9. [Google Scholar]
- 8.Prinja S, Gupta A, Verma R, Bahuguna P, Kumar D, Kaur M, et al. Cost of delivering health care services in public sector primary and community health centres in North India. PLoS One. 2016;11:e0160986. doi: 10.1371/journal.pone.0160986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prinja S, Jeet G, Verma R, Kumar D, Bahuguna P, Kaur M, et al. Economic analysis of delivering primary health care services through community health workers in 3 North Indian states. PLoS One. 2014;9:e91781. doi: 10.1371/journal.pone.0091781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prinja S, Manchanda N, Mohan P, Gupta G, Sethy G, Sen A, et al. Cost of neonatal intensive care delivered through district level public hospitals in India. Indian Pediatr. 2013;50:839–46. doi: 10.1007/s13312-013-0234-6. [DOI] [PubMed] [Google Scholar]
- 11.Prinja S, Mazumder S, Taneja S, Bahuguna P, Bhandari N, Mohan P, et al. Cost of delivering child health care through community level health workers: How much extra does IMNCI program cost? J Trop Pediatr. 2013;59:489–95. doi: 10.1093/tropej/fmt057. [DOI] [PubMed] [Google Scholar]
- 12.Singh S, Darroch JE. New York: Guttmacher Institute and United Nations Population Fund (UNFPA); 2012. Adding It Up: Costs and Benefits of Contraceptive Services: Estimates for 2012. [Google Scholar]
- 13.Methods for Estimating the Costs of Family Planning: Report of The Expert Group Meeting on Family Planning Costing. Carolina Population Center. 2011 [Google Scholar]
- 14.Janowitz B, Bratt JH. Methods for Costing Family Planning Services. United Nations Population Fund and Family Health International (UNFPA) 1994 [Google Scholar]
- 15.Bergkvist S, Wagstaff A, Katyal A, Singh P, Samarth A, Rao M. What a Difference a State Makes: Health Reform in Andhra Pradesh. World Bank Policy Research Working Paper. 2014 [Google Scholar]
- 16.Shukla M, Qureshi S, Chandrawati Post-placental intrauterine device insertion – A five year experience at a tertiary care centre in North India. Indian J Med Res. 2012;136:432–5. [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma M, Joshi S, Nagar O, Sharma A. Determinants of intrauterine contraceptive device discontinuation among Indian women. J Obstet Gynaecol India. 2014;64:208–11. doi: 10.1007/s13224-014-0516-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prinja S, Balasubramanian D, Jeet G, Verma R, Kumar D, Bahuguna P, et al. Cost of delivering secondary-level health care services through public sector district hospitals in India. Indian J Med Res. 2017;146:354–61. doi: 10.4103/ijmr.IJMR_902_15. [DOI] [PMC free article] [PubMed] [Google Scholar]


