Abstract
Background:
Prediction of preterm births in the early stage during pregnancy may reduce prevalence of preterm births by appropriate interventions.
Aims/Objective:
The aim of the study is to develop an antenatal risk scoring system/scale for prediction of preterm births.
Subjects and Methods:
From a cohort of 1876 and subset of 380 pregnant women attending Krishna Hospital Karad, Maharashtra, routine antenatal and in-depth information on diet, occupation, and the rest were collected and analyzed using SPSS version 16. A scoring system was developed by multivariate analysis based on the relative risk (RR) and tested on separate set of 251 mothers.
Statistical Analysis Used:
Bivariate analysis by Chi-square test, backward multivariate regression model, receiver operating characteristic curve (ROC) curve analysis, and calculation of RR for identified risk factors. Sensitivity and specificity of newly developed risk scoring scale.
Results:
Out of six risk factors from whole cohort (n = 1876) and three risk factors from subsample (n = 380) identified by bivariate analysis. Further four and three risk factors were retained after multivariate analysis from whole and part of cohort, respectively, and risk scores of “7” and “9” were assigned based on RR cutoff levels of three and five were identified separately for whole and part data by ROC curve analyses together making it “8” with 75.5% sensitivity and 85.5% specificity when tested on 251 independent patients. Based on the prevalence of preterm births, low-, moderate-, and high-risk grading was done by identifying as second cutoff value.
Conclusions:
Identification of low-, moderate-, and high-risk of preterm births was possible at <8, 8, and 9 and equal to ≥10 with high sensitivity at lower cutoff and high specificity at upper cutoff.
Keywords: Antenatal risk scores, attributable risk, population attributable risk, preterm births, relative risk
INTRODUCTION
Preterm birth is, worldwide, the most challenging problem in obstetrics, but the prevention of preterm births has been difficult because of its multifactorial nature and partly due to still unknown etiology.[1,2]
The WHO defines preterm birth as birth before 37 completed weeks. Each year, 15 million preterm babies are born.[3] India is the biggest contributor to the world's prematurity burden. According to the WHO fact sheet 2013, India has 35,19,100 preterm births. It is around 23.6% of the total 15 million world preterm births.
If a scoring system is developed based on the risk factors associated with the preterm births to identify “At risk” mothers early during pregnancy, action can be taken to avert the risk of the preterm births. This primary prevention of preterm births would improve the health and survival of the babies during neonatal period. A hospital-based study was therefore planned to identify the risk factors and develop a scoring system to detect the “At risk” pregnant mothers more likely to give birth to preterm babies.
SUBJECTS AND METHODS
A consecutive sample of 1876 mothers and their singleton babies were included in the study. The enrollment was started from November 1, 2013, till desired sample size was reached, and continued for 10% more enrollments in view of outcome of 71 still births, 33 multiple pregnancies, and 48 though planned to deliver at Krishna Hospital, delivered outside; hence, 152 women were excluded [Flow Chart 1]. Thus, the cohort of 1876 was analyzed for the study. In-depth study was done about occupation, hours of rest during day and hours of sleep at night, and the diet consumed by the mother during antenatal period from randomly selected 380 mothers from original cohort.
Flow Chart 1.
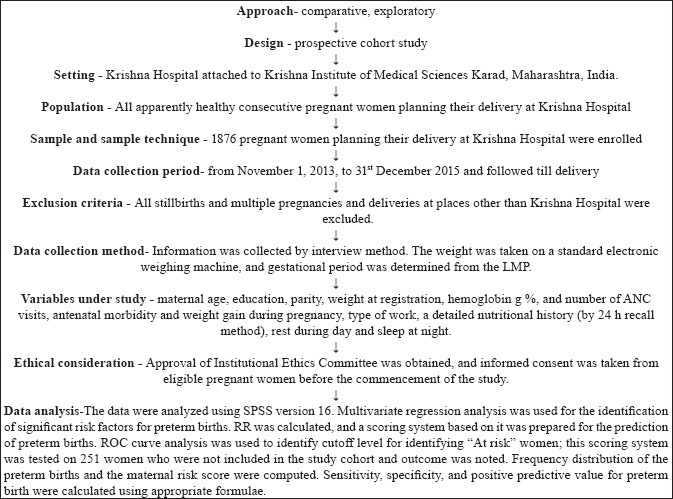
Showing Research participant
RESULTS
The risk factors related to the sociodemographic, anthropometric, and clinical aspects of pregnant mothers were subjected to bivariate analysis. Six risk factors, namely, education (literate), type of family (Nuclear), weight gain <10 kg, number of antenatal care (ANC) visits <4, weight at first trimester <40 kg, and anemia in the first trimester (hemoglobin <11 g%) from the main cohort of 1876 pregnant women were identified. They were subjected to backward multivariate regression model. Out of these six factors, all were retained as significant indicators of preterm births except two, that is, antenatal morbidity and anemia in the first trimester. Three variables were found significantly associated with preterm births by bivariate analysis of subsample of 380 pregnant women, namely, type of work (hard work), number of meals (<4), and hours of rest during day (<2 h); they were subjected to backward multivariate regression model. All the three risk factors were retained as significant indicators of the preterm births. Relative risk (RR) and confidence interval for all risk factors related to preterm births were found to be highly significant. They were arranged in order of magnitude [Table 1].
Table 1.
Relative risk, attributed risk, and population-attributed risk of significant risk factors for preterm births
| Risk factor | n (%) | RR of 95% CI | AR | PAR (%) | Scoring |
|---|---|---|---|---|---|
| Preterm births: From in-depth subsamples study (n=380) (total score-9) | |||||
| Hard work | 23 (6.1) | 3.880 (2.239-6.726) | 74.2 | 14.9 | 4 |
| Number of meals/day <4 | 150 (39.4) | 3.258 (1.866-5.691) | 69.3 | 74.7 | 3 |
| Hours of rest during day <2 h | 267 (70.3) | 2.222 (1.078-4.581) | 55.0 | 46.1 | 2 |
| Preterm births: From whole cohort study (n=1876) (total score-7) | |||||
| Literate | 1751 (93.3) | 1.670 (1.030-2.710) | 40.1 | 36.8 | 2 |
| Weight gain <10 kg | 1295 (69.0) | 1.579 (1.258-1.980) | 36.7 | 28.5 | 2 |
| Number of ANC visits <4 | 665 (34.9) | 1.530 (1.275-1.837) | 34.6 | 15.6 | 2 |
| Nuclear family | 716 (38.1) | 1.330 (1.107-1.598) | 24.8 | 11.2 | 1 |
RR: Relative risk, AR: Attributed risk, PAR: Population-attributed risk, CI: Confidence interval, ANC: Antenatal care
Highest RR, attributed risk for preterm births was observed for hard work (RR = 3.880), followed by number of meals of <4 per day (RR = 3.258) and hours of rest during day <2 h (RR = 2.222). It was followed by education (RR = 1.670), weight gain <10 kg during pregnancy (RR = 1.579), number of ANC visits of < 4 (RR = 1.530), and nuclear type of family (RR = 1.330) [Table 1].
For effective and easy identification of “At risk” mothers for preterm delivery, the scores were given on the basis of RR. Total score of first three variables (type of work, number of meals per day, and rest during day time) from the subsample (n = 380) was “9.” Receiver operating characteristic curve (ROC) analysis revealed cutoff score of “3,” for these three risk factors. Similarly, total scores of four variables available from the whole data (n = 1876) (education, weight gain, number of ANC visits, and type of family) were “7,” which was considered to determine the cutoff score for identification of “At risk” pregnant women. ROC curve analysis revealed cutoff value of “5.” Adding these cutoff values (3 + 5), 8 was identified as final cutoff value for the scoring system of seven risk factors with total score of 16 (9 + 7). The score ≥8 indicated higher probability of preterm delivery and <8 indicated higher probability of nonpreterm delivery. This newly developed scoring system for identification of “At risk” women giving birth to preterm babies was applied to a set of 251 pregnant women who were not included in the study cohort for computing the scoring system. At cutoff score of ≥8, correct classification of preterm births could be done for 83.2% pregnant women. The predictive value for preterm birth was 57.3% and sensitivity of 75.5% and specificity of 85.4% [Table 2].
Table 2.
Classification ability of the cutoff score for preterm (n=251)
| Gestational age score category | Gestational age category | Total (%) | |
|---|---|---|---|
| Preterm, n (%) | Not preterm, n (%) | ||
| Preterm (score ≥8) | 39 (75.0) | 29 (14.6) | 68 (27.1) |
| Nonpreterm (score <8) | 13 (25.0) | 170 (85.4) | 183 (72.9) |
| Total | 52 | 199 | 251 |
The frequency distribution of maternal scores of “At risk” mothers is given in Table 3. There was a sharp increase in the prevalence of preterm birth from 50% to 91.6% when the score increased from 9 to 10. Hence, the 2nd cutoff value was identified at ≥10 risk score. The correct classification was possible for 84.4%, with sensitivity of 30.7%, specificity of 98.4%, and positive predictive value of 84.2%. With identification of this 2nd cutoff value, the risk could be graded as low at <8 score, moderate risk at score 8 and 9, and high risk above the score of 10 or more with high sensitivity at first cutoff value of “8” and higher specificity at second cutoff value of “10.”
Table 3.
Frequency distribution of preterm births according to Gestational age score from 0 to 16 (n=251)
| Score | Frequency (%) | Preterm (%) | Preterm prevalence (%) |
|---|---|---|---|
| <8 | 183 (72.9) | 13 (25.0) | 7.1 |
| 8 | 19 (7.6) | 8 (15.4) | 42.1 |
| 9 | 30 (12.0) | 15 (28.8) | 50.0 |
| 10 | 12 (4.8) | 11 (21.2) | 91.6 |
| 11 | 5 (2.0) | 4 (7.7) | 80.0 |
| 12 | 2 (0.8) | 1 (1.9) | 50.0 |
| Total | 251 (100.0) | 52 (100.0) | 20.7 |
There were 183 (72.9%) women who could be classified as low risk who delivered 13 (7.1%) preterm babies, 49 women (19.5%) could be classified as having moderate risk who delivered 23 (46.9%) preterm babies, and 19 (7.5%) women could be classified as high risk who delivered 16 (84.2%) preterm babies.
DISCUSSION
Scoring systems for identifying the risk of preterm birth in antenatal period were developed by many workers from 2001 to 2014: Talsania and Lala in New Civil Hospital, Ahmadabad, India (2001),[4] Okunade et al. at Lagos Tertiary Hospital in Nigeria (2014),[5] Samiya and Samina at[6] Maternity Hospital of Kashmir (LalaDed Hospital) attached to the Government Medical College, Srinagar (2005), Marete et al.[7] Kasr El Aini Hospital, (2014). In their studies, they have identified the risk factors based on bivariate analysis and multivariate analysis. The common risk factors have been maternal malnutrition, higher pregnancy order, older maternal age at delivery, prior preterm births, history of fetal loss, preeclampsia (hypertension and proteinuria developing >20 weeks’ gestation), fetal distress, intrauterine growth retardation, abruptio placentae, and fetal death. The sensitivity varied from 50% to 95.77%, specificity from 19.69% to 75%, and predictive values from 11.93% to 73.8% for antenatal prediction of preterm births.
The risk factors identified in our study were hard work, <4 meals a day, hours of rest during day <2, literacy, weight gain <10 kg, number of ANC visits <4, and nuclear family in decreasing order of magnitude. The predictive value for preterm birth was 57.3% and sensitivity of 75.5% and specificity of 85.4% at the cutoff value of ≥8 scores. These values are in the range of the values observed by other researchers. Grading was done by Beck et al.[8] grading was done as low risk (<8 score), moderate (8 and 9 score) and high (≥10 score), respectively. Preterm birth is of multifactorial origin as it occurs as a result of play of many risk factors simultaneously present. RR indicates the probability of preterm birth if there is the presence of given risk factor. It is therefore an important measure of risk, and risk scores based on RR are likely to predict preterm births better than the arbitrary scoring system. The scoring system in the present study is based on sound prospective research design with cutoffs determined using advanced statistical tools of multivariate analysis, RR, and ROC curve analysis, and frequency distribution of risk scores, which resulted in good sensitivity at lower cutoff level score of ≥8 of 75.5% and specificity of 98.4% at higher cutoff score of ≥10 more. Therefore, the use of low-risk, moderate-risk, and high-risk scale for prediction of preterm birth would be better than using only one cutoff value at lower or higher level.
It has been noted that prolonged standing at work of ≥7 h/day, working in hot environments, commuting, walking, carrying and lifting heavy weight, and night work have all been seen to be associated with pregnancy loss and preterm birth, especially in women whose nutritional status is compromised.[9,10,11,12,13]
In a study done by TH Kim et al.[14] in Korea, researchers have noted that occupation during pregnancy of laborer had 20% increased risk of preterm delivery as compared to legislators and managers. Peasants are associated with increased risk of preterm delivery probably due to hard working in the farms which trigger early labor and hence lead to preterm birth.
The study conducted by Temu[15] in Northern-eastern Tanzania (2016), Zhang et al.[16] in Beijing (2016), Steer,[17] and Räisänen et al.[18] have noted that women who were involved in hard physical work during pregnancy had more than three-fold increased odds of preterm delivery even after adjusting for the confounders. The high risk of preterm delivery may be explained by increased stress which triggers premature labor, which leads to preterm delivery.
Simpson[19] and Keith and Luke[20] have speculated that strenuous occupations increased uterine contractions and therefore increased the risk of premature birth. Heavy weight lifting increases intra-abdominal pressure, and this may provoke uterine contractions. Heat stress causes dehydration resulting in the release of the antidiuretic hormone and oxytocin, which stimulates the uterus to contract.
The study conducted by Siega-Riz et al.[21] in University of North Carolina, USA (1998) noted that women who consumed meals/snacks less frequently had a higher risk of delivering preterm births (adjusted odds ratio = 1.30, 95% confidence interval: 0.96, 1.76), which supports previous animal model work of an association between decreased frequency of eating and preterm delivery. This could be due to malnutrition due to inadequate food intake and fluctuations in the blood glucose levels.
Tellapragada et al.[22] in South India (2014) Udupi district have observed higher rates of preterm births with higher educational levels of mothers. We have also observed significantly higher rates of preterm births among babies born to literate women.
Maternal poor ANC attendance (ANC visits <4) was associated with increased risk of preterm delivery in our study. Similar findings were noted by Temu[15] in Northeastern Tanzania (2014), Zhang et al.,[16] and Mahande.[23] Diseases or obstetrical complications are more likely to be detected during ANC and treated preventing preterm delivery. Studies from several developing countries have found that “no ANC visit” is a significant risk factor for preterm birth, ranging from 1.3 to 7 times higher risk than for women having any ANC visit.[24,25,26,27]
Studies conducted in Northern India by Saini et al.[28] and Rashmi et al.[29] Mysuru, Karnataka, India, have found that type of family affects the pregnancy outcome. Nuclear family had positive impact by having good socioeconomic status and more leisure.
In the present study, the pregnant women doing hard work like road buildings were 6.1% with higher RR of 3.88 with a prevalence of preterm births of 26.1%. Providing less strenuous work during pregnancy and ensuring adequate nutrition by minimum of 4 meals a day and supplementary feeding under Integrated Child Development Scheme (ICDS) are of paramount importance. Rest in the afternoon for 2 h, ANC visits for minimum four times during pregnancy can be achieved by counseling. The risk factors identified in this study have a strong scientific basis as they are based on RR. Population-attributable risk percentage is determined jointly by the magnitude of RR and the prevalence of the risk factor in the community. The community strategies suggested appear to be feasible, acceptable to the community, and will be a leap forward toward achieving MDG4, and 50% reduction in preterm births by 2015,[30] the announcement by global experts on world prematurity day 2012.
Limitations of the study
Study is limited to mothers delivered at the hospital only. Women not having ANC, referred cases and only coming for delivery are not included in the study.
Implications of the study
Identification of ‘At Risk’ pregnant women is possible during pregnancy with good sensitivity and specificity using the scoring system which can be easily done by preparing a stamp of the same. There is also possibility of primary prevention by modifying the identified risk factors like reducing hard work, increasing frequency of meals to four, taking afternoon rest 2 hours, availing ANC visit at least for four occasions, and monitoring weight gain during pregnancy.
Stamp
Significant risk factors by bivariate analysis from subsample of 380 patients were (Total 3) and from whole cohort, data of 1876 patients were (Total 4). Hence, grand total of all is (7) variables
Risk factors risk scores:
Type of work (Hard work) (4)
Number of meals per day (<4) (3)
Hours of day rest (<2 h) (2)
Education (Literacy) (2)
Weight gain (<10 g) (2)
Number of ANC visits (<4) (2)
Type of family (Nuclear) (1)
Total Risk Score (16)
Instruction: Please encircle/Tick mark appropriately:
Low risk (<8)
Moderate risk (8 to 10)
High risk (≥10)
The results are applied to the local population. It can be applied through trained ANM and ASHA workers in the rural areas and semi-urban areas. In urban areas, municipal hospitals, government hospitals, and urban health centers can use this scoring system routinely in ANC clinics.
CONCLUSIONS
Community-based studies to test the feasibility and acceptability of risk/predictors of preterm births by developing and testing scoring system/tool are required. Once the effective, feasible, and acceptable scoring system is developed, it can be incorporated in the routine ANC services for detection and management of high-risk women for primary prevention of preterm births in routine health-care delivery system. Identification of women at high risk for delivering preterm babies would be improved using this tool developed in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The researchers are thankful to all the participants as well as Dr. R. P Patange; Professor and Head and staff of Obstetrics and Gynecology department, where the study was carried out.
REFERENCES
- 1.Kore SJ, Parikh MP, Lakhotia S, Kulkarni V, Ambiye VR. Prediction of risk of preterm delivery by cervical assessment by transvaginal ultrasonography. J Obstet Gynecol India. 2009;59:131–5. [Google Scholar]
- 2.Kuppusamy N, Vidhyadevi A. Prevalence of Preterm Admissions and the Risk Factors of Preterm Labor in Rural Medical College Hospital. Int J Sci Stud. 2016;4:125–8. [Google Scholar]
- 3.Howson C, Kinney M, Lawn J, editors. Born Too Soon: The Global Action Report on Preterm Birth. Geneva: March of Dimes, PMN, World Health Organization; 2012. [Google Scholar]
- 4.Talsania NJ, Lala MK. Evaluation of antenatal risk scoring in a preterm birth prevention and perinatal loss. Indian J Matern Child Health. 1994;5:5–9. [PubMed] [Google Scholar]
- 5.Okunade KS, Oluwole AA, Adegbesan-Omilabu MA. A study on the association between low maternal serum magnesium level and preterm labour. Adv Med. 2014;2014:704875. doi: 10.1155/2014/704875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Samiya M, Samina M. Identification of high risk pregnancy by a scoring system and correlation with perinatal outcome. Indian J Pract Dr. 2008;5(1) [Google Scholar]
- 7.Marete IK, Wasunna AO, Otieno PA. Clinical risk index for babies (CRIB) II score as a predictor of neonatal mortality among low birth weight babies at Kenyatta national hospital. East Afr Med J. 2011;88:18–23. [PubMed] [Google Scholar]
- 8.Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, et al. The worldwide incidence of preterm birth: A systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31–8. doi: 10.2471/BLT.08.062554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fenster L, Hubbard AE, Windham GC, Waller KO, Swan SH. A prospective study of work-related physical exertion and spontaneous abortion. Epidemiology. 1997;8:66–74. doi: 10.1097/00001648-199701000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Chamberlain G. Effect of work during pregnancy. Obstet Gynecol. 1985;65:747–50. [PubMed] [Google Scholar]
- 11.Senturia KD. A woman's work is never done: Women's work and pregnancy outcome in Albania. Med Anthropol Q. 1997;11:375–95. doi: 10.1525/maq.1997.11.3.375. [DOI] [PubMed] [Google Scholar]
- 12.Gold EB, Tomich E. Occupational hazards to fertility and pregnancy outcome. Occup Med. 1994;9:435–69. [PubMed] [Google Scholar]
- 13.Mozurkewich EL, Luke B, Avni M, Wolf FM. Working conditions and adverse pregnancy outcome: A meta-analysis. Obstet Gynecol. 2000;95:623–35. doi: 10.1016/s0029-7844(99)00598-0. [DOI] [PubMed] [Google Scholar]
- 14.Kim TH, Park JH, Lim S, Lim JY, Kim KI, Han MK, et al. The Korean longitudinal study on health and aging. [Last assessed on 2019 Mar 21];Psychiatry Investig. 2007 4:84–95. Available from: http://www.psychiatryinvestigation.org . [Google Scholar]
- 15.Temu TB. Maternal and obstetric risk factors associated with preterm delivery at a referral hospital in Northern-Eastern Tanzania. Asian Pac J Reprod. 2016;5:365–70. [Google Scholar]
- 16.Zhang YP, Liu XH, Gao SH, Wang JM, Gu YS, Zhang JY, et al. Risk factors for preterm birth in five maternal and child health hospitals in Beijing. PLoS One. 2012;7:e52780. doi: 10.1371/journal.pone.0052780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steer PJ. The epidemiology of preterm labour – Why have advances not equated to reduced incidence? BJOG. 2006;113(Suppl 3):1–3. doi: 10.1111/j.1471-0528.2006.01116.x. [DOI] [PubMed] [Google Scholar]
- 18.Räisänen S, Gissler M, Saari J, Kramer M, Heinonen S. Contribution of risk factors to extremely, very and moderately preterm births – Register-based analysis of 1,390,742 singleton births. PLoS One. 2013;8:e60660. doi: 10.1371/journal.pone.0060660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simpson JL. Are physical activity and employment related to preterm birth and low birth weight? Am J Obstet Gynecol. 1993;168:1231–8. doi: 10.1016/0002-9378(93)90374-r. [DOI] [PubMed] [Google Scholar]
- 20.Keith L, Luke B. The association between women's work, working conditions, and adverse pregnancy outcomes: A review of the literature and directions for future research. Womens Health Issues. 1991;1:113–9. doi: 10.1016/s1049-3867(05)80112-4. [DOI] [PubMed] [Google Scholar]
- 21.Siega-Riz AM, Herrmann TS, Savitz DA, Thorp JM. Frequency of eating during pregnancy and its effect on preterm delivery. Am J Epidemiol. 2001;153:647–52. doi: 10.1093/aje/153.7.647. [DOI] [PubMed] [Google Scholar]
- 22.Tellapragada C, Eshwara VK, Bhat P, Acharya S, Kamath A, Bhat S, et al. Risk factors for preterm birth and low birth weight among pregnant Indian women: A Hospital-based prospective study. J Prev Med Public Health. 2016;49:165–75. doi: 10.3961/jpmph.16.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahande MJ, Daltveit AK, Obure J, Mmbaga BT, Masenga G, Manongi R, et al. Recurrence of preterm birth and perinatal mortality in Northern Tanzania: Registry-based cohort study. Trop Med Int Health. 2013;18:962–7. doi: 10.1111/tmi.12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mavalankar DV, Gray RH, Trivedi CR. Risk factors for preterm and term low birthweight in Ahmedabad, India. Int J Epidemiol. 1992;21:263–72. doi: 10.1093/ije/21.2.263. [DOI] [PubMed] [Google Scholar]
- 25.Feresu SA, Harlow SD, Welch K, Gillespie BW. Incidence of and socio-demographic risk factors for stillbirth, preterm birth and low birthweight among Zimbabwean women. Paediatr Perinat Epidemiol. 2004;18:154–63. doi: 10.1111/j.1365-3016.2003.00539.x. [DOI] [PubMed] [Google Scholar]
- 26.Ferraz EM, Gray RH, Cunha TM. Determinants of preterm delivery and intrauterine growth retardation in North-East Brazil. Int J Epidemiol. 1990;19:101–8. doi: 10.1093/ije/19.1.101. [DOI] [PubMed] [Google Scholar]
- 27.Olusanya BO, Ofovwe GE. Predictors of preterm births and low birthweight in an inner-city hospital in sub-Saharan Africa. Matern Child Health J. 2010;14:978–86. doi: 10.1007/s10995-009-0528-4. [DOI] [PubMed] [Google Scholar]
- 28.Saini S, Singh J, Ahluwalia SK, Mittal A, Singh MM, Qadri S. A cross-sectional study of association of maternal sociodemographic factors and low birth weight in tertiary care centre in Northern India. Ind J Mat Chi Health. 2012;14:1–9. [Google Scholar]
- 29.Rashmi A, Narayanamurthy MR, Vidya GS, Vidyalaxmi K, Renuka M. Risk factors for preterm birth: A community based longitudinal study in rural Mysuru, Karnataka. [Last assessed on 2019 Mar 21];India Int J Community Med Public Health. 2016 3:3576–80. Available from: http://www.ijcmph.com . [Google Scholar]
- 30.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: A systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]


