Abstract
Objective:
To assess decisional conflict and knowledge about prematurity among mothers facing extreme premature delivery when the counseling clinicians were randomized to counsel using a validated decision aid compared with usual counseling.
Study design:
In this randomized trial, clinicians at 5 level III neonatal intensive care units (NICUs) in the United States were randomized to supplement counseling using the DA or to counsel mothers in their usual manner. We enrolled mothers with threatened premature delivery at 220/7-256/7 weeks of gestation within 7 days of their counseling. The primary outcome was the Decisional Conflict Scale score (DCS). One hundred mothers per group were enrolled to detect a clinically relevant effect size of 0.4 in DSC. Secondary outcomes included knowledge about prematurity; scores on the Preparedness for Decision Making scale; and acceptability.
Results:
Ninety-two clinicians were randomized and 316 mothers were counseled. Of these, 201 (64%) mothers were enrolled. The median gestational age was 24.1wks (IQR 23.7–24.9). In both groups, DCS scores were low (16.3±18.2 v 16.8±17, p=0.97) and Preparedness for Decision Making scores were high (73.4±28.3 v 70.5±31.1, p=0.33). There was a significantly higher knowledge score in the DA group (66.2±18.5 v 57.2±18.8, p=0.005). Most clinicians and parents found the DA useful.
Conclusion:
For parents facing extremely premature delivery, use of a DA did not impact maternal decisional conflict, but it significantly improved knowledge of complex information. A structured DA may improve comprehension of complex information.
Trial registration
Keywords: decision making, decision aids, infant, extremely premature
Parents may not understand nor recall discussing their options for resuscitation when facing extremely premature delivery1. A shared decision model may assist parents facing decisions on resuscitation of periviable infants born at 22 −25 weeks of gestation2–4. However, how best to meet the needs of expectant parents and guide shared decision-making in this clinical context is unknown.5 Most parents want to receive information to enable good decision-making and request discussions on anticipated survival and long-term outcomes.6–12 Some parents want more than statistical information on gestation-specific morbidity and mortality outcomes during the antenatal consult.13–15 For some parents, information on how they can participate in the care of their child in the neonatal intensive care unit (NICU) is important.16 Parents also want sensitivity, compassion, and attention to their goals tempered by honesty about medical uncertainty.1,6,12–13,17–19
The American Academy of Pediatrics emphasizes an individualized and family centered approach to antenatal counseling.2 Guidelines and calculators may minimize site variation in approaches to counseling and help to individualize information on extreme prematurity20–21. Whether providing outcome data enables shared decision-making in antenatal discussions remains uncertain.1,22 Decision aids are tools to inform about potential outcomes and risks and benefits.23 They supplement face-to-face discussions between clinicians and patients to encourage shared decision-making. A Cochrane review of 105 randomized trials showed that, across several diseases, patients counseled with DAs display lower decisional conflict when compared with those who received usual care24. DAs also improved knowledge, clarified health-care values, and enabled patients to take a more active role in decision-making24.
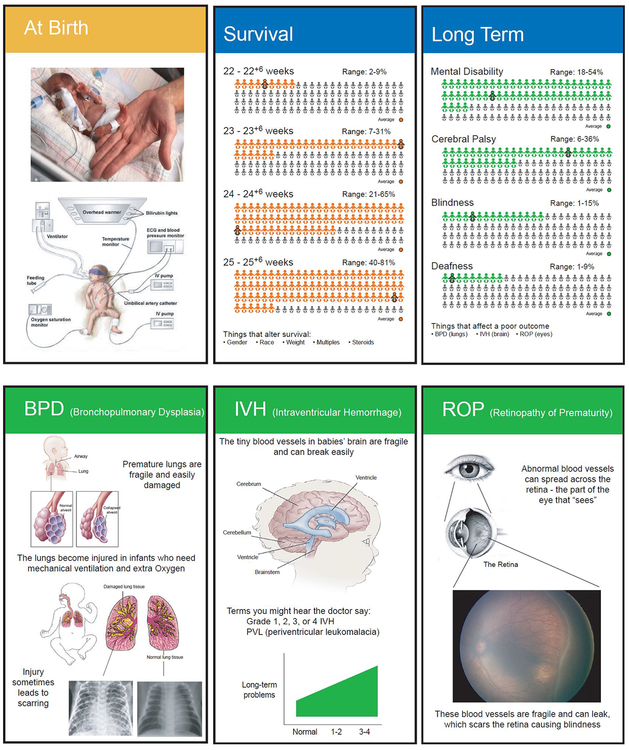
We systematically developed a DA for antenatal counseling at 22–25 weeks of gestation after eliciting information from parents about their experiences.10 The resulting 6-card DA conformed to many criteria outlined by the International Patient Decision Aids Standards (IPDAS) Collaboration (Figure 1) and was validated in a separate cohort.10,23 It is an inexpensive tool that facilitates communication even when limited time is available for counseling should the mother present in active labor. The DA provides survival and outcome data, which can be individualized to the circumstances. It informs and supports decision making without endorsing a particular option. It is presented to help parents evaluate their preferences with the support of a counselor. The objective of this randomized study was to determine whether parents facing extreme premature delivery between 22–25 weeks of gestation experience reduced parental decisional conflict when receiving antenatal counseling using a DA as compared with routine antenatal counseling.
Figure 1:
Decision aid for counseling parents facing extreme prematurity
Methods
This prospective randomized controlled trial was conducted from May 2013 to August 2017 at 5 tertiary care centers in the United States following Institutional Review Board approval at each site. The trial was registered at clinicaltrials.gov ( NCT01713894). Written informed consent was obtained before enrollment of each counseled mother and her counseling clinician. Using a random number generator, clinicians (attending neonatologists, neonatology fellows, neonatal nurse practitioners and physicians’ assistants) who provide antenatal counseling were randomized to supplement counseling using the decision aid (intervention) or to provide their usual routine counseling (control). No crossovers were allowed; each clinician conducted all eligible consults as randomized for the entire study. Clinicians randomized to the intervention arm were trained by the principal investigator on the use of the decision aid. Randomized clinicians used the decision aid to supplement discussions and were not asked to memorize a script. Clinicians randomized to the control arm were asked to complete their consults in their usual manner. None of the sites in this study had any tools already in use for counseling. Within 7 days of counseling, mothers were enrolled into the study. Mothers were included if they were Over 18 years of age; between 22–25 completed weeks of gestation; and had a primary language of English. Mothers were excluded if there were known fetal anomalies or for intrauterine fetal demise before counseling. Baseline demographic information was obtained for enrolled clinicians and mothers.
The primary outcome was decisional conflict using the Decisional Conflict Scale25. Decisional conflict is a state of uncertainty about the course of action to take when making choices involving risk or uncertainty of outcomes. This 16-item validated instrument measures a person’s uncertainty in making a decision, the modifiable factors contributing to uncertainty, and the overall effectiveness of decision-making. Decisional conflict scores range 0–100. Lower scores indicate lower decisional conflict. We measured decisional conflict after counseling was completed.
Secondary outcomes were measured after enrollment following antenatal counseling for threatened extremely preterm birth. Secondary outcomes were: 1) Understanding of the complications of extreme prematurity, measured using a 47-question true/false knowledge test; 2) Preparedness for decision making as measured with the 7-item preparedness for decision making scale. Scores range from 0–100. Higher scores indicate the individual feels prepared to make a decision26; 3) Acceptability survey to assess mothers’ perceptions of the counseling they received; 4) Clinicians in the intervention arm were asked to complete a 5-point survey on the effectiveness of the decision aid after each consult regardless of whether the mother was successfully enrolled in the study27; 5) Both enrolled mothers and clinicians were asked to identify maternal preferences about resuscitation before and after counseling; 6) Enrolled mothers were given the opportunity to provide additional free-text responses about their counseling experience.
Clinicians in the intervention arm reported whether or not they had used the DA as instructed during counseling. They were also asked to document the amount of time spent on a consult. Mothers were also administered the Newest Vital Sign (NVS) Instrument. This widely used validated tool assesses health literacy, where a score ≥4 (out of 6) indicates adequate health literacy28.
We hypothesized that parents who received standardized data on short and long-term sequelae of extreme prematurity with a validated prenatal DA would have lower decisional conflict compared with parents who received current routine counseling.
Sample size and Data Analysis
In the absence of prior studies, we estimated the effect of a neonatal DA on decisional conflict. In adult medicine studies, the decisional conflict scale discriminates between different interventions with an effect size of 0.2 to 1.2 for the total scale29. O’Connor et al recommend basing sample sizes on detecting a minimal clinically relevant effect size of 0.3 to 0.429. Using an effect size of 0.4, for a 2-sided alpha of 0.05 and power of 80%, 96 mothers were needed per group. We compared the observed primary outcome rates between groups using a hierarchical linear model. This model took into account the number of consults that each counselor contributed to the total. An a-priori subgroup analysis of parents who were counseled at 23 and 24 completed weeks of gestation was also conducted. Data were analyzed on the basis of intention to treat. A P value < .05 was considered significant. Qualitative thematic analysis of maternal free-text responses identified items valued for decision-making about delivery room resuscitation. Line-by-line coding of the comments was performed by 2 independent investigators who agreed on each step of the analysis using an iterative process. Identified items were subsequently grouped into themes; ambiguities and inconsistencies were resolved through discussion with other team members.
Results
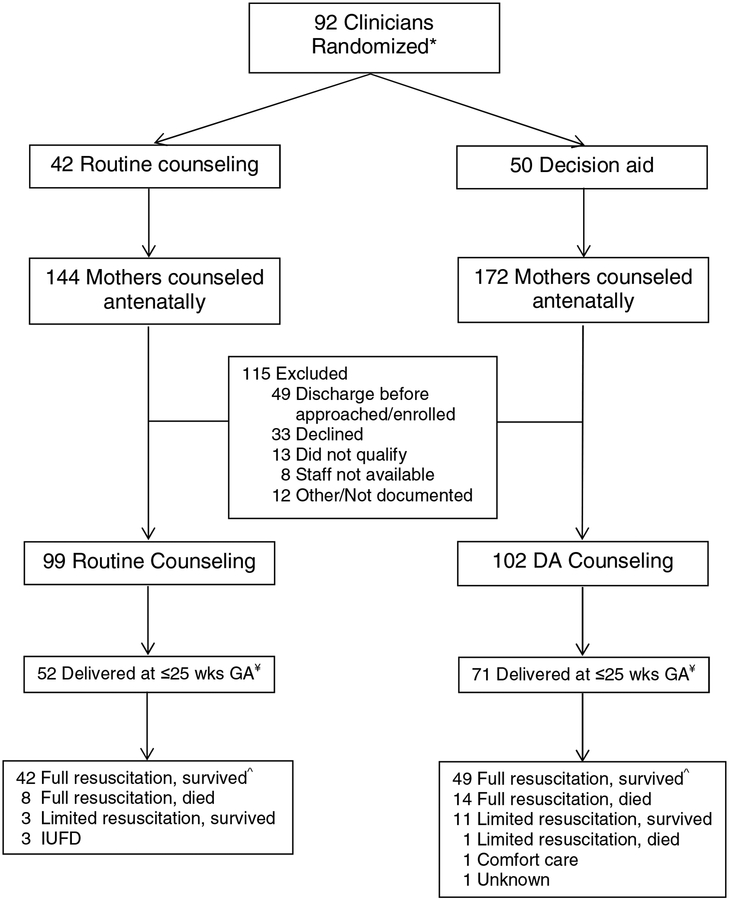
Figure 2 shows the flow of participants through the study. Of the 92 clinicians, 12 in the routine counseling group and 19 in the DA group did not complete any consults in the gestational age window during the study period. Six of the 102 consults of enrolled mothers in the DA group were conducted without the use of the DA. Reasons given were: misplacement (n=1); clinician did not feel it was clinically appropriate to use (n=3); or no reason was documented (n=2). Results for these 6 mothers were included in the DA arm for analysis. Of the 316 mothers counseled, pregnancy outcome data were available for 262. One hundred and fifty-four of the 262 counseled mothers (58.8%) delivered at ≤25 completed weeks gestation. Of the 201 mothers enrolled, 52 (52.5%) in the routine counseling arm and 71 (69.6%) in the DA arm delivered at ≤25 weeks GA.
Figure 2:
Flow Diagram
* Of the 92 clinicians randomized, 12 in the routine counseling and 19 in the DA group did not perform any consults during the study
¥ GA at delivery was unknown for 9 mothers in the routine counseling group and 2 mothers in the DA group
^ survival defined as survival to hospital discharge. 4 sets of twins delivered in the routine counseling group and 1 set of twins, 1 set of triplets, and 1 set of quadruplets delivered in the DA group; IUFD: intrauterine fetal demise
There were no significant demographic differences between the two parent groups (Table I). The median gestational age of those counseled was 24.1wks (IQR 23.7–24.9). Mothers had a health literacy score ≥4 (70.6%) indicating a minimum of adequate health literacy. There were no significant differences between the two groups of randomized clinicians (Table 1). Both groups had equal proportions of attending physicians and fellows enrolled. The 9 enrolled neonatal nurse practitioners did not conduct any consults during the conduct of the study.
Table 1:
Maternal and Clinician self-reported demographics
| RoutineCounseling N=99 |
DA N=102 |
p-value | |
|---|---|---|---|
| Maternal Demographics | |||
| Age, years ± SD | 29.3 ± 5.9 | 29.5 ± 6.0 | 0.688 |
| Race/Ethnicity, n (%) Black White Hispanic or Latino Asian Other |
49 (49.5) 38 (38.4) 7 (7.1) 0 (0) 5 (5.1) |
49 (48.0) 44 (43.1) 3 (2.9) 2 (2.0) 4 (3.9) |
0.416 |
| History of premature delivery: Yes, n (%) | 30 (30.3) | 21 (20.6) | 0.114 |
| GA at time of counseling, weeks 22 23 24 25 |
8 (8.1) 29 (29.3) 34 (34.3) 27 (27.3) |
8 (7.8) 31 (30.4) 42 (41.2) 21 (20.6) |
0.664 |
| Marital status, n (%) Single Living with partner Married Divorced |
34 (34.3) 18 (18.2) 46 (46.5) 1 (1.0) |
35 (34.3) 15 (14.7) 48 (47.1) 4 (3.9) |
0.555 |
| Education, n (%) < High school High school 2yrs college/technical school 4yrs college >4yrs college/graduate school |
8 (8.1) 34 (34.3) 24 (24.2) 22 (22.2) 11 (11.1) |
7 (6.9) 32 (31.4) 26 (25.5) 24 (23.5) 12 (11.8) |
0.989 |
| Adequate health literacy, n (%) | 65 (65.7) | 77 (75.5) | 0.126 |
| Clinician Demographics | N=42 | N=50 | |
| Age‡, years ± SD | 41.4 ± 11.6 | 37.5 ± 10.4 | 0.061 |
| Female, n (%) | 30 (71.4) | 33 (66.0) | 0.532 |
| Race/Ethnicity‡, n (%) Caucasian African American Hispanic or Latino Asian Other |
29 (69.0) 1 (2.4) 1 (2.4) 4 (9.5) 2 (4.8) |
32 (64) 1 (2) 2 (4) 7 (14) 1 (2) |
0.88 |
| Marital status‡, n (%) Single Married Divorced |
4 (9.5) 33 (78.6) |
11 (22) 31 (62) 1 (2) |
0.142 |
| Position‡, n (%) NICU Attending NICU Fellow Neonatal nurse practitioner/Physician assistant |
15 (35.7) 17 (40.5) 5 (11.9) |
14 (28) 25 (50) 4 (8) |
0.542 |
| Years of experience*, n (%) | 16.7 ± 10.9 | 12.7 ± 9.1 | 0.278 |
Missing data for n=5 in Routine and n=7 in DA groups
Years of experience for attending neonatologists and NNP/Pas
GA: gestational age
For the primary outcome, mean decisional conflict scores were low in both the DA (n=96 << >>, 16.3 ± 18.2) and routine counseling arms (n=95<< >>, 16.8 ± 17, p=0.97). There was no significant difference in decisional conflict scores between the two groups.
For the secondary outcomes, knowledge scores in the DA group (n=98 << >>, 66.2 ± 18.5) were higher compared with the routine counseling group (n=96 << >>, 57.2 ± 18.8, p=0.005). The mean preparedness for decision-making score was high in both the DA (n=96 << >>, 73.4 ± 28.3) and the routine counseling arms (n=95 << >>, 70.5 ± 31.1, p=0.33). Mothers in both groups felt the amount of information they received was just right and found the information easy to understand (Table 2; available at www.jpeds.com). Mothers in both groups understood most or all of the information they received, and for a majority, the information they received was new. Clinicians in the DA group counseled a total of 172 women with the DA, including women who were not enrolled in the study. For these, there were 137 (79.7%) clinician acceptability surveys completed. Most clinicians in the DA group thought the DA was of use to patients (Table 3; available at www.jpeds.com). The perceived benefits ranged from understanding the risks associated with prematurity, allowing more involvement in decision-making and making a more informed decision, and improvement in the way time was spent during the consult. A majority of clinicians in the DA group felt the DA was easy to use, easy to understand, and compatible with how counseling should be done. Clinicians did not think using the DA would save them time. This was corroborated by the average times spent counseling, which with the DA was 36.9 ± 13.8 minutes as compared with 32.1 ± 12.2 minutes for counselors in the control arm of the study (p=0.003).
Table 2:
Maternal acceptability survey responses
| Routine Counseling N=96 |
DA N=94 |
|
|---|---|---|
| Describe the amount of information you received: (Just right) | 76 (79.2) | 80 (85.1) |
| The way in which the information was presented was too complicated (Disagree/Strongly Disagree) | 78 (81.2) | 70 (74.5) |
| How easy was the information to understand? (Moderately/Very Easy) | 70 (72.9) | 80 (85.1) |
| How much of the information did you understand? (Most/All) | 87 (90.6) | 89 (94.7) |
| How much of the information was new to you? | 56 (58.3) | 55 (58.5) |
Values are noted as n(%)
Table 3:
Clinician acceptability survey responses for all mothers counseled with the decision aid, n=137
| To what extent did the decision aid… | Quite a bit/A great deal N (%) |
|---|---|
| Help your patient understand the risks associated with extreme prematurity? | 97 (70.8) |
| Help your patient be as involved in the decision making process as she desired? | 85 (62) |
| Help your patient make a more informed decision? | 83 (60.6) |
| Help you to more fully understand the issues that are most important to your patient? | 59 (43) |
| Help you tailor your counseling to your patient’s preference for decision participation? | 65 (47.4) |
| Improve the way time was spent during the consultation? | 90 (65.7) |
| Please show your opinion of the decision aid: | Agree/Strongly Agree |
| The cards were easy for me to use | 115 (83.9) |
| The cards were easy for me to understand | 135 (98.5) |
| It will be easy for me to experiment with using the cards | 123 (89.8) |
| The results of using the cards will be easy to see | 71 (51.8) |
| Using the cards is better than how I usually go about helping patients decide their options | 97 (70.8) |
| This counseling strategy is compatible with the way I think things should be done | 121 (88.3) |
| Compared with my usual approach the cards will result in my patients making more informed decisions | 101 (73.7) |
| Using the cards will save me time | 65 (47.4) |
| The cards are a reliable method of helping patients make decisions about extreme prematurity | 108 (78.8) |
| Pieces or components of the cards can be used by themselves | 135 (98.5) |
| This type of counseling strategy is suitable for helping patients make value laden choices | 123 (89.8) |
| This counseling strategy complements my usual approach | 125 (91.2) |
| Using the cards does not involve making major changes to the way I usually do things | 108 (78.8) |
| There is a high probability that using this strategy may cause/result in more benefit than harm | 111 (81) |
Values are noted as n(%)
Total number of mothers counseled with decision aid by clinicians, n=172. Data missing, n=35
For the subgroup analysis of parents (DA, n=73 << >>; routine counseling, n=63 << >>) who were counseled at 23 and 24 completed weeks of gestation, results were similar to the overall study results. Decisional conflict scores were low in both groups (DA: 15.9 ± 15.6 vs routine: 13.4 ± 15.6, p=0.26). Knowledge scores were significantly higher in the DA group compared with the routine counseling group (64.8 ± 19.2 vs 57.2 ± 17.7, p=0.02). Preparedness for decision-making scores were high in both groups (DA: 73.9 ± 27.1 vs routine: 70.0 ± 31.0, p=0.39).
We investigated whether clinicians accurately identified maternal preferences for resuscitation before and after counseling. 127 of 198 (64%) enrolled mothers stated they had already formed a preference regarding resuscitation before counseling; of these, 110 (86.6%) wanted full resuscitation. Clinicians stated that 78 of 184 (42%) enrolled mothers had a pre-counseling preference regarding resuscitation. Of these, they thought 73 (94%) wanted full resuscitation. Of the 127 mothers who confirmed they had a pre-counseling preference regarding resuscitation, clinicians misidentified 72 of them (56.7%) as not having a preference. Post-counseling, 167 of 201 enrolled mothers (83%) stated they wanted full resuscitation – almost unchanged to their pre-counseling preferences. Clinicians stated that 132 of 201 enrolled mothers (65.7%) wanted full resuscitation. Of the 167 mothers who wanted full resuscitation, clinicians misidentified 54 (32%) as undecided or preferring comfort care or limited intervention.
Of 201 enrolled mothers, 136 provided free-text comments: 79 in the DA group and 57 in the routine counseling group. Three major themes emerged (Table 4). First, some mothers expressed a desire for a tailored approach to antenatal consultation. Second, the theme of clinician sensitivity addressed the importance of giving parents hope, thoughtful timing of consultation, and recognition/support of parents’ emotional state. Last, the theme of shared decision-making included the importance of trust, failure to present options, problems with parent engagement, and values mismatch. Seventy-nine of 102 parents who received counseling with the DA provided additional free-text comments about the DA itself. Seventy-three found the visual depiction of the information helpful and 24 specifically commented on the benefit of providing a visual representation of statistical information; one found it more confusing. A few mothers (n=7) did not find the DA beneficial, and 2 reported negative perceptions. Mothers in both groups noted the importance of engaging diverse learning styles; and many commented on the benefit of using a visual aid or handout.
Table 4.
Items valued by parents in antenatal consultation identified in free-text comments.
| Theme/Subtheme | Study Arm | Parent Free-Text |
|---|---|---|
| Tailored information | ||
| Right Amount | Standard Counseling | “I scheduled a tour of this hospital because I am dealing for the first time with the possibilities of having a severely premature infant. The staff provided me with detailed information regarding the risks, medical interventions that could/could not be provided at the various gestational stages in order for me to make a decision as to the level of care I would like to receive for my child. I am very pleased with the knowledge and information that has been provided, that has assisted me in making an informed decision.” |
| Too Much/Confusing | Standard Counseling | “All of the information was very informative, but particularly for me, comparison to something a little more understandable would’ve been helpful.” |
| Too Little | Decision Aid | “It might have been useful to me to have seen some stats for older premature babies (26–28w, 29–32w, etc.) since it is unknown when I’ll actually deliver. Otherwise, the NICU doctor did a great job explaining all of the process and answering my questions.” |
| Different Focus | Decision Aid | “The info presented in the [Decision Aid] were mostly geared to woman that had ruptured membranes at about 24 weeks gestation. My situation is extremely different because my water broke at 16 weeks. I would like to see visuals that are more befitting to my unique situation.” |
| Clinician Sensitivity | ||
| Good Hope/Comfort/Optimism | Decision Aid | “I liked the [Decision Aid] cards. It gives you hope. I really appreciate that. I know if one week passes, another week, my chances are better. The cards stick in mind. When it’s just talking it doesn’t make sense. It’s not just something coming out of her head. She really knows the information.” |
| Poor Hope/Comfort/Optimism | Standard Counseling | “I would only suggest that although it’s about the baby, to try to take the mom’s feelings into consideration just a little more. I felt like my feedback was all negative without any reassurance of something positive :((still loved him though!)” |
| Timing of Consultation | Decision Aid | “I was VERY upset when the NICU* [Physician Assistant] came to Labor & Delivery when I first arrived. It’s the WRONG time. At least give the nurses time to get the patient situated especially if contractions have died down, before hurling words at them like ‘resuscitation’ and ‘decision making’. That was the worse possible time to discuss that.” |
| Recognition/Support of Parent Emotions | Standard Counseling | “I suggest that there be a support person present to assist the patient with emotional support & the partner is not available. Counseling services should be made available so patients can express their emotional concerns after dealing with the medical pros and cons.” |
| Shared Decision-Making | ||
| Presentation of Options | Standard Counseling | “For me, the down play of the extreme negative effect was helpful. I was stressed out enough and knowing there some hope got me through. I would have appreciated a bit more info on the fact there was an option of care. I did not realize there were levels of choice - comfort measures vs. full revival etc when discussing. I thought it was more the doctors would automatically do whatever they could to keep the baby alive and if something changed, we would make the decision at that time.” |
| Parent Engagement | Standard Counseling | “Engage with the parent how much they want to know. Personally I agreed out of fear and didn’t say anything.” |
| Values Mismatch | Standard Counseling | “On our first visit before the cerclage the first option presented was about terminating the pregnancy. I don’t feel, emotionally, that was beneficial to our decision. It was more of a knife being turned as opposed to helping us realize the gravity of the situation.” |
| Trust/Honesty | Decision Aid | “There is no ideal easy time. Sitting close, eye contact, honesty, and urgency. I love the way it happened.” |
Neonatal Intenstive Care Unit (NICU)
Discussion
This randomized controlled trial of a previously validated decision aid for resuscitation decisions at the margin of gestational viability systematically evaluated the effects of a decision aid on parental decisional conflict and knowledge, as well as mothers’ attitudes about counseling and preparedness for decision making. Although the DA did not significantly impact our primary outcome of decisional conflict, it improved knowledge scores. A majority of mothers in this cohort had already come to a decision about resuscitation before counseling. Clinicians were unable to consistently identify which mothers had already made resuscitation decisions. Finally, mothers in the DA group found the visual representation of information useful, but mothers in both groups desired a tailored approach to counseling and recognition of their emotional needs.
We hypothesized that the DA would reduce maternal decisional conflict and improve preparedness for decision-making at the margin of gestational viability, but we found no improvements in either, whether for the whole cohort or in a subgroup analysis. In both the DA group and the routine counseling groups, decisional conflict was low and preparedness for decision-making was high. Our hypothesis stemmed from literature on the impact of decisions aids in randomized trials in other clinical settings, such as women facing cancer treatment options and patients with chest pain presenting to the emergency department. In these patients, lower rates of decisional conflict were found in groups counseled with DAs as compared with usual counseling24. Only limited data exist on decisional conflict in parents facing extreme prematurity. In a small group of parents (n=20), Moore et al found an elevated median decisional conflict score of 50 (IQR 32–70) prior to antenatal counseling at 23 weeks of gestation.30 The majority of parents in that cohort were female (55%), married (60%), and well educated (60%). Following counseling with a DA, the median decisional conflict score decreased to 0 (IQR 0–18). However, they did not have a control group for comparison.
There are a number of potential explanations for our findings. It is likely that our results were impacted by the demographics of the women enrolled. Lower health literacy may affect patients’ decision-making abilities. A systematic review of patient DA trials showed that lower health literacy was associated with lower patient health knowledge and higher decision uncertainty and regret.31 In this study a majority of the mothers enrolled were well educated and health literate. Moreover, a majority of these mothers had already formed pre-counseling preferences regarding resuscitation. There is evidence that individuals bring well-articulated preferences regarding resuscitation to decision-making32. Because many mothers in our study had already formed clear preferences, it is possible that they had low decisional conflict prior to randomization. Alternatively, it is possible that many of these mothers, free of labor, never perceived themselves at risk for premature delivery. Approximately 43% of mothers who were not enrolled were missed because they were discharged free of labor, before they could be approached for enrollment. Additionally, 39% of the mothers enrolled did not proceed to deliver at ≤25 completed weeks gestation. In settings such as oncology, DAs help patients decide between interventions that are definitely indicated. However, mothers in our study were not certain that a premature delivery would occur. It is possible that even mothers who ultimately delivered at ≤25 completed weeks gestation remained hopeful during counseling that delivery would not occur and therefore did not have decisional conflict.
Nonetheless the DA did significantly improve maternal knowledge scores compared with the control group. In other clinical settings ranging from parents facing decisions about prenatal screening to patients with cancer facing different medical and surgical treatment options, randomized studies show that DAs consistently improve knowledge and accuracy of risk perceptions.33–42 there was no correlation between improved knowledge scores and decisional conflict. Potentially, the construct of decisional conflict is distinct from knowledge, and changes in one may not influence the other.
Mothers and clinicians in the DA arm of the study had positive feelings about the DA. Similarly, studies evaluating the use of a DA for different cancer screening and treatment found that patients counseled with a DA felt more satisfied with their decision and the decision-making process as compared with routine counseling.43–44 Among clinicians, favorable attitudes towards the DA point to a subjective sense by antenatal counselors that a structured approach to counseling such as one using a DA is better than unstructured routine counseling for margin-of-viability decision making. It may also suggest clinicians’ perceptions of their own limitations to effectively convey complex information, elicit values, or support decision-making without the benefit of a DA. we demonstrated high preparedness for decision-making in most participants, which may indicate adequate counseling by clinicians in both groups. We did not evaluate potential differences in clinicians’ perceptions of the DA by age or years of experience. It is possible that the overall positive acceptance of the DA is driven by younger, more inexperienced clinicians.
The themes we identified in mothers’ comments agree with previous studies and further inform how clinicians should approach the antenatal consultation encounter.1,10,12,16,22 In this study, many mothers in the DA arm found graphic outcome statistics understandable, and many in routine counseling suggested a visual aid would have helped them. This supports that clinicians should explore parents’ desire for information and tailor counseling to parental needs.5 For some parents, shared decision-making involves personalized information including amount and type and not just an enumeration of risks.15 A systematic review of parent communication needs suggests that the quality of the consult when facing extreme prematurity is not solely data driven, but is also dependent on the way in which it is provided.16 In this study, mothers noted other aspects of the consultation influential to their experiences, suggesting that clinicians should individualize counseling regarding timing, support for parent emotions, and provision of hope. Likewise, many opportunities to improve parents’ participation in shared decision-making were identified, including clearer communication of the decision and options, parent engagement, and elicitation of values.
Clinicians failed to consistently identify both whether mothers had pre-determined preferences about resuscitation, and the nature of those preferences. Zupancic et al described this malalignment-clinicians could not accurately identify the 45% of parents who felt strongly about their decision-making autonomy.45 We found 64% of mothers had pre-counseling preferences, where counseling supplemented by a DA may not have been useful. Some clinicians argue that neonatologists should first actively treat and only then seek consent to withdraw in adverse conditions.46–47 However, this does not account for the parents who ultimately decide to forgo resuscitative efforts - an equally acceptable parental value and preference. For the 36% of mothers in this study who had no pre-formed preference, the antenatal consult is potentially beneficial. And, counseling supplemented with a DA, tailored to the informational needs of the mother could be helpful. Default intervention does not leave room for shared decision-making and parental autonomy. Misunderstanding mothers’ expectations about goals of consultation (anticipatory guidance vs. decision-making) may contribute to patient dissatisfaction and vital miscommunication about resuscitation plans. We acknowledge limitations. First, decisional conflict was not measured prior to the counseling session. This was to avoid adversely influencing mothers’ perceptions during counseling. Second, clinicians within each site were randomized to minimize potential bias from variation of patient populations by site. However, contamination of counseling methods was possible because those randomized to routine counseling may have become aware of the decision aid. This may have affected their approach to counseling. Third, we did not assess clinicians’ perceptions about resuscitation and counseling at the limits of gestational viability. Religious and cultural differences may influence clinician/patient interactions.48–50 Clinicians navigate between what is best for an infant and what is best for a family, and their feelings about either.46,51 We did not ask participating clinicians or parents to identify their religious or spiritual preferences. As discussed above, some physicians believe that proactive perinatal management should be the standard of care for all extreme premature deliveries.47 It is possible that clinicians’ own biases may have influenced their counseling, thereby influencing mothers’ perceptions and decisions. Finally, clinicians in this study may have had a strong interest in periviability counseling which led to their participation in this study and overall good communication with mothers in both groups. Nonetheless, we demonstrate that a practical and inexpensive tool to support the counselor in providing individualized antenatal counseling at the margin of gestational viability improves maternal knowledge and is acceptable to clinicians and patients. Although a majority of mothers had already come to a decision about resuscitation before counseling, for those mothers who have not decided, counseling supplemented by a decision aid may be useful. The decision aid provides a way to present accurate and consistent information, facilitates a dialogue between mothers and clinicians in order to elicit mothers’ values, and is a step towards a shared process of decision-making.
Acknowledgments
Supported by an Institutional Development Award (IDeA) from the National Institutes of Health (U54-GM104941). The authors declare no conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Boss RD, Hutton N, Sulpar LJ, West AM, Donohue PK. Values Parents Apply to Decision-Making Regarding Delivery Room Resuscitation for High-Risk Newborns. Pediatrics. 2008;122:583–589. [DOI] [PubMed] [Google Scholar]
- 2.Cummings J; Committee on Fetus and Newborn. Antenatal counseling regarding resuscitation and intensive care before 25 weeks of gestation. Pediatrics. 2015. September;136:588–95 [DOI] [PubMed] [Google Scholar]
- 3.Jefferies AL, Kirpalani HM, Canadian Paediatric Society Fetus and Newborn Committee. Counseling and management for anticipated extremely preterm birth. Paediatr Child Health. 2012. October; 17:443–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lemyre B, Moore G. Canadian Paediatric Society Fetus and Newborn Committee. Counseling and management for anticipated extremely preterm birth. Paediatr Child Health. 2017. September, 22:334–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haward MF, Gaucher N, Payot A, Robson K, Janvier A. Personalized decision making: practical recommendations for antenatal counseling for fragile neonates. Clinical Perinatology 2017;44:429–445 [DOI] [PubMed] [Google Scholar]
- 6.Kavanaugh K, Moro TT, Savaga TA, Reyete M, Wydra M. Supporting parents’ decision making surrounding the anticipated birth of an extremely prematre infant. J Perinat Neonatal Nurs 2009;23:159–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Partridge JC, Martinez A, Nishida H, Boo N-Y, Tan KW, Yeung C-Y, et al. International comparison of care for very low birth weight infants: parents’ perceptions of counseling and decision-making. Pediatrics 2005;116:3263–71 [DOI] [PubMed] [Google Scholar]
- 8.Young E, Tsai E, O’Riordan A. A qualitative study of predelivery counselling for extreme prematurity. Paediatr Child Heal. 2012;17:432–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grobman WA, Kavanaugh K, Moro T, DeRegnler R-A, Savage T. Providing advice to parents for women at acutely high risk of periviable delivery. Obstet Gynecol 2010;115:904–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guillen U, Suh S, Munson D, Posencheg M, Truitt E, Zupancic JA, et al. Development and pretesting of a decision-aid to use when counseling parents facing imminent extreme premature delivery. Journal of Pediatrics. 2012. March;160:382–7 [DOI] [PubMed] [Google Scholar]
- 11.Roscigno CI, Savaga TA, Kavanaugh K, Moro TT, Kilpatrick SJ, Strassner HT, et al. Divergent views of hope influencing communications between parents and hospital providers. Qual Health Res 2012;22:1232–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drago MJ, Guillen U, Schiaratura M, Batza J, Zygmunt A, Mowes A, et al. Constructing a culturally informed Spanish decision-aid to counsel Latino parents facing imminent extreme premature delivery. Matern Child Health J. 2018. July;22:950–957 [DOI] [PubMed] [Google Scholar]
- 13.Payot A, Gendron S, Lefebvre F, Doucet H. Deciding to resuscitate extremely premature babies: how do parents and neonatologists engage in the decision? Soc Sci Med 2007;64:1487–500 [DOI] [PubMed] [Google Scholar]
- 14.Daboval T, Shidler S, Thomas D. Shared decision making at the limit of viability: a blue print for physician action. PloS One 2016;11:e0166151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Staub K, Baardsnes J, Hebert N, Hebert M, Newell S, Pearce R. Our child is not just a gestational age. A first-hand account of what parents want and need to know before premature birth. Acta Paediatrica 2014; 103:1035–8 [DOI] [PubMed] [Google Scholar]
- 16.Kharrat A, Moore GP, Beckett S, Nicholls SG, Sampson M, Daboval T. Antenatal consultations at extreme prematurity: a systematic review of parent communication needs. J Pediatr 2018. May;196:109–115.e7 [DOI] [PubMed] [Google Scholar]
- 17.Keenan HT, Doron MW, Seyda BA. Comparison of mothers’ and counselors’ perceptions of predelivery counseling for extremely premature infants. Pediatrics 2005;116:104–11 [DOI] [PubMed] [Google Scholar]
- 18.Kaempf JW, Tomlinson MW, Campbell B, Ferguson L, Stewart VT. Counseling pregnant women who may deliver extremely premature infants: medical care guidelines, family choices, and neonatal outcomes. Pediatrics 2009;123:1509–15 [DOI] [PubMed] [Google Scholar]
- 19.Guillen U, Suh S, Wang E, Stickelman V, Kirpalani H. Development of a video decision aid to inform parents on potential outcomes of extreme prematurity. J Perinatol 2016;36:939–43 [DOI] [PubMed] [Google Scholar]
- 20.Kaempf JW, Tomlinson M, Arduza C, Anderson S, Campbell B, Ferguson LA, et al. Medical staff guidelines for periviability pregnancy counseling and medical treatment of extremely premature infants. Pediatrics. 2006;117:22–9. [DOI] [PubMed] [Google Scholar]
- 21.Tyson JE, Parikh NA, Langer J, Green C, Higgins RD, for the National Institute of Child Health and Human Development Neonatal Research Network. Intensive care for extreme prematurity: moving beyond gestational age. New England Journal of Medicine. 208;358:1672–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tucker Edmonds B, Savage TA, Kimura RE, Kilpatric SJ, Kuppermann M, Grobman W, et al. Prospective parents’ perspectives on antenatal decision making for the anticipated birth of a periviable infant. J Matern Fetal Neonatal Med. November 2017: 1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elwyn G, O’Connor A, Stacey D, Volk R, Edwards A, Coulter A, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333:417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017. April 12;4:CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O’Connor AM. Validation of a decisional conflict scale. Medical Decision Making. 1995. Jan-Mar;15:25–30 [DOI] [PubMed] [Google Scholar]
- 26.Bennett C, Graham ID, Kristjansson E, Kearing SA, Clay KF, O’Connor AM. Validation of a preparation for decision making scale. Patient Educ Couns. 2010. January;78:130–3 [DOI] [PubMed] [Google Scholar]
- 27.O’Connor AM & Cranney A. User Manual – Aceptability [document on the Internet]. Ottawa: Ottawa Hospital Research Institute; 1996. [modified 2002]. Available from http://decisionaid.ohri.ca/docs/develop/User_Manuals?UM_Acceptability.pdf [Google Scholar]
- 28.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the Newest Vital Sign. Ann Fam Med 2005;3:514–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Connor AM. User Manual – Decisional Conflict Scale (16 item statement format) [document on the Internet]. Ottawa: Ottawa Hospital Research Institute; 1993. [updated 2010]. Available from http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Decisional_Conflict.pdf [Google Scholar]
- 30.Moore GP, Lemyre B, Daboval T, Ding S, Dunn S, Akiki S, et al. Field testing of a decision coaching with a decision aid for parents facing extreme prematurity. Journal of Perinatology 2017. June;37:728–734 [DOI] [PubMed] [Google Scholar]
- 31.McCaffery KJ, Homes-Rovner M, Smith SK, Rovner D, Nutbeam D, Clayman ML, et al. Addressing health literacy in patient decision aids. BMC Medical Informatics & Decision Making. 2013;13:S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haward MF, John LK, Lorenz JM, Fischhoff B. Effects of description of options on parental perinatal decision-making. Pediatrics 2012;129:891–902 [DOI] [PubMed] [Google Scholar]
- 33.Vandemheen KL, O’Connor A, Bell SC, Freitag A, Bye P, Jeanneret A, et al. Randomized trial of a decision aid for patients with cystic fibrosis considering lung transplantation. Am J Respir Crit Care Med. 2009. October 15;180:761–8 [DOI] [PubMed] [Google Scholar]
- 34.Bjorklund U, Marsk A, Levin C, Ohman SG. Audiovisual information affects informed choice and experience of information in antenatal Down syndrome screening-a randomized controlled trial. Patient Education and Counseling 2012;86:390–5 [DOI] [PubMed] [Google Scholar]
- 35.Hess EP, Knoedler MA, Shah ND, Kline JA, Breslin M, Branda ME, et al. The chest pain choice decision aid: a randomized trial. Circulation: Cardiovascular Quality and Outcomes 2012;5:251–9 [DOI] [PubMed] [Google Scholar]
- 36.Man-Son-Hing M, Laupacis A, O’Connor AM, Biggs J, Drake E, Yetisir E, et al. A patient decision aid regarding antithrombotic therapy for stroke prevention in atrial fibrillation: a randomized controlled trial. JAMA 1999;282:737–43 [DOI] [PubMed] [Google Scholar]
- 37.Kuppermann M, Pena S, Bishop JT, Nakagawa S, Gregorich SE, Sit A, et al. Effect of enhanced information, values clarification, and removal of financial barriers on use of prenatal genetic testing: a randomized clinical trial. JAMA 2014;312:1210–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leighl NB, Shepherd HL, Butow PN, Clarke SJ, McJannett M, Beale PJ, et al. Supporting treatment decision making in advanced cancer: a randomized trial of a decision aid for patients with advanced colorectal cancer considering chemotherapy. Journal of Clinical Oncology 2011;29:2077–84 [DOI] [PubMed] [Google Scholar]
- 39.Nassar N, Roberts CL, Raynes-Greenow CH, Barratt A, Peat B, Decision aid for breech presentation trial collaborators. Evaluation of a decision aid for women with breech presentation at term: a randomized controlled trial. BJOG: An International Journal of Obstetrics and Gynaecology 2007;114:325–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Peperstraten A, Nelen W, Grol R, Zielhuis G, Adang E, Stalmeier P, et al. The effect of a multifaceted empowerment strategy on decision making about the number of embryos transferred in in vitro fertilization: randomized controlled trial. BMJ 2010;341:c2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Whelan T, Sawka C, Levine M, Gafni A, Reyno L, Willan A, et al. Helping patients make informed choices: a randomized trial of a decision aid for adjuvant chemotherapy in lymph node-negative breast cancer. Journal of the National Cancer Institute 2003;95:581–7 [DOI] [PubMed] [Google Scholar]
- 42.Wong SS, Thornton JG, Gbolade B, Bekker HL. A randomized controlled trial of a decision-aid leaflet to facilitate women’s choice between pregnancy termination methods. BJOG: An international journal of Obstetrics and Gynaecology 2006;113:688–94 [DOI] [PubMed] [Google Scholar]
- 43.Schroy PC 3rd, Emmons K, Peters E, Glick JT, Robinson PA, Lydotes MA, et al. The impact of a novel computer-based decision aid on shared decision making for colorectal cancer screening: a randomized trial. Medical Decision Making 2011;3:93–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barry MJ, Cherkin DC, Chang Y, Fowler FJ, Skates S. A randomized trial of a multimedia shared decision-making program for men facing a treatment decision for benign prostatic hyperplasia. Disease Management and Clinical Outcomes 1997;1:5–14 [Google Scholar]
- 45.Zupancic J, Kirpalani H, Barrett J, Stewart S, Gafni A, Streiner D, et al. Characterising doctor-patient communication in counseling for impending preterm delivery. Arch Dis Child Fetal Neonat Ed. 2002; 87:F113–F7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marmion P. Periviability and the ‘god committee’. Acta Paediatrica 2017. June;106:857–859 [DOI] [PubMed] [Google Scholar]
- 47.EXPRESS Group, Fellman V, Hellstrom-Westas L, Norman M, Westgren M, Kallen K, et al. One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA. 209 June 3;301:2225–33 [DOI] [PubMed] [Google Scholar]
- 48.Curlin FA, Lawrence RE, Chin MH, Lantos JD. Religion, conscience, and controversial clinical practice. N Engl J Med 2007;356:593–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Catlin EA, Guillemin JH, Thiel MM, Hammond S, Wang ML, O’Donnell J. Spiritual and religious components of patient care in the neonatal intensive care unit: sacred themes in a secular setting. J Perinatol 2001. Oct-Nov;21:426–30 [DOI] [PubMed] [Google Scholar]
- 50.Coughlin K, Mackley A, Kwadu R, Shanks V, Sturtz W, Munson D, et al. Characterization of spirituality in maternal-child caregivers. J Palliat Med. 2017. September;20:994–997 [DOI] [PubMed] [Google Scholar]
- 51.Navne LE, Svendsen MN. A clinical careography: steering life-and-death decisions through care. Pediatrics 2018. September;142:S558–S566 [DOI] [PubMed] [Google Scholar]