Abstract
Rotator cuff calcific tendinopathy (RCCT) is a common and painful shoulder disease characterised by deposition of calcium into the rotator cuff’s tendond. Different therapeutic options have been proposed, but the ultrasound-guided percutaneous irrigation (US-PICT) is been proved as an effective and safe first-line treatment. It can be performed with a single- of a double-needle tecnique, using warm saline solution to improve the dissolution of the calcific deposit. The procedure is ended with an intrabursal injection of local anaesthetics and slow-release steroids to improve the pain relief and to prevent complications. US-PICT leads to significative improvement in the shoulder funtion and pain relief in the short and long term, with a low complications rate. (www.actabiomedica.it)
Keywords: rotator cuff, shoulder, ultrasound-guided procedures, calcific tendinopathy, percutaneus treatments
Introduction
Rotator cuff calcific tendinopathy (RCCT) is a common disease, with a reported prevalence of 2.5% up to 7.5% of asymptomatic adults, and up to 30-40% of painful shoulders, tipically seen in women in the 4th or 5th decade and in sedentary workers (1-3).
Aetiology of this condition is still poorly understood, but the most convincing mechanism is that a decrease of intratendinous oxygen concentration may promote tendon fibrocartilaginous metaplasia and cellular necrosis, followed by deposition of calcium, mainly hydroxyapatite (4).
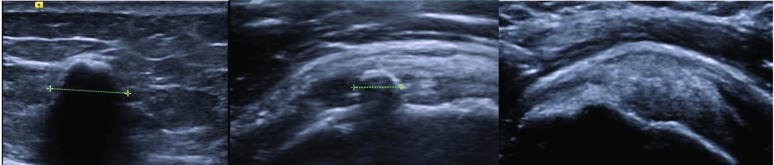
Diagnostic and interventional radiology in the musculoskeletal system are widely used (5-21). Regarding to the US imaging (22-24), three types of calcifications can be found: type I - a hyperechoic focus with a well defined shadow; type II - a hyperechoic focus with a faint shadow; Type III - a hyperecoic focus whithout an acoustic shadow (Fig. 1) (25).
Figure 1.
US findings of shoulder calcifications, as decribed by Farin et al.: (A) a hyperechoic focus with a well defined shadow (B) a hyperechoic focus with a faint shadow (C) a hyperecoic focus whithout an acoustic shadow
In the RCCT’s pathogenesis 4 stages are recognizable:
- Precalcific stage with fibrocartilaginous transformation within the tendon.
- Formative stage with calcium deposition
- Resorptive phase.
- Postcalcific phase, in which self-healing and repair of the affected tendon occurs.
The resorptive phase is characterized by hyperemia, edema, increased intratendinous pressure with possible etravasation of calcium crystals in the subacromial bursa. Usually this stage is associated with the development of acute pain, that can be very disabling (pseudoparalytic shoulder) and unresponsive to conservative treatments such as nonsteroidal anti-inflammatory drugs (NSAIDs) (26).
The most affected tendon of the rotator cuff is the supraspinatus (80%), followed by the lower side of infraspinatus (15%) and the preinsertional area of the subscapularis tendon (5%) (8, 27-31).
Therapeutic options include subacromial steroid injections, arthroscopy, and extracorporeal shockwaves. Currently ultrasound-guided percutaneous irrigation of calcific tendinopathy (US-PICT) is accepted as the first-line safe and effective treatment for RCCT, wth significant pain improvement and a very low rate of minor complications (vasovagal reaction, bursitis) (32).
This procedure is also known as “barbotage” and “lavage”, it does not require hospitalization, is performed under local anesthesia and there is no need of post-procedural immoblization. The patient can go home about 30 minutes after the procedure and return the day after the treatment to his daily activities.
Procedure details
- Pretreatment evaluation:
US-PICT is always indicated in the resorptive phase, in presence of soft or semi-fluid calcifications (type II or III). In case of hard calcification (type I) or mildly symptomatic patient, elective treatment should be considered. With very small calcifications (<5 mm) or migration into the bursal space the procedure is not indicated (33).
- Patient positioning and antisepsis:
The procedure is performed with the patient in semisupine position, the arm of the affected shoulder should lie completely extended along the body with a internal/external rotation according to the calcification’s location.
Ordinary antisepsis is generally sufficient to guarantee a safe procedure for both the patient and the operator.
- Local anaesthesia:
A small amount of local anaesthetic ( up to 10 ml of lidocaine) is injected along the path of the needles, into the subacromial-subdeltoid bursa (almost two thirds) and around the calcifications. In order to preserve the peripheral calcific rim, no anaesthetic solution should be injected directly within the calcification.
Positioning of the needles and irrigation procedure:
The procedure can be done with a single or double needle tecnique (Figg. 2, 3).
Figure 2.
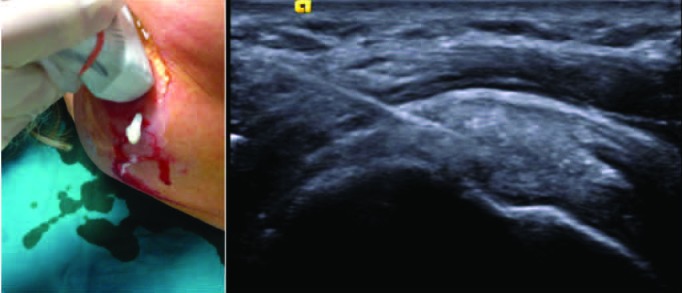
(A) US probe and needle positioning with the one-needle tecnique. (B) Ultrasound image of a soft-fluid calcification (type III). After the puncture and the washing, a leakage of toothpaste-like material is seen from the needle
Figure 3.

Image shows the needles positioning in the double-needle technique. The deeper needle (1) inserted first, than the second needle is inserted superficial to the first one. Is important to position the needles as much perpendicular as possible to the US beam to achieve optimal visualization under US guidance
The size of the needle should be chosen in order to maximize calcium retriveal and avoid obstruction, in other published studies for RCCT treatment varies between 16 and 18 G. Every approach is done under continuous US monitoring, with a free-hand tecnique or with needle guidance kit, but the first one is faster and allows a more flexible approach. In the double-needle tecnique the needles are inserted depending on the location and accessibility to the calcification. Both needles should be as perpedicular as possible to the US beam so anisotropy artifacts are minimyzed and needles can be seen thoroughly (Fig. 4). The deeper needle is first inserted, taking care to preserve the integrity of the calcific shell, than the second needle is inserted superficially. The correct angulation of the needles’s tips should be 25-30°, with both bevels facing each other, to allow a continuous flow of water that is injected from one needle and drained by the other (Fig. 5) (34). Saline solution is normally injected using 20/40-ml syringe in one needle, the plunger pushed repeatedly and when the calcification starts to dissolve, water and calcium debris are drained from the second needle.
Figure 4.
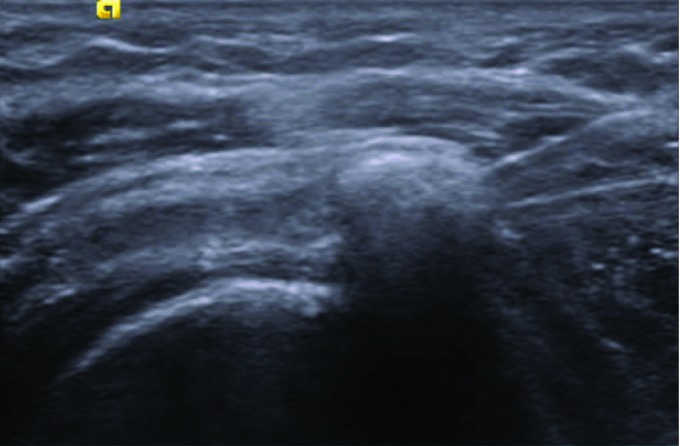
Ultrasound image of the double-needle technique. Both needles lay on the same coronal plane, with a correct angulation (25-30°) and both bevels facing each other
Figure 5.

The flow of saline water, injected from one needle and drained by the other, using the double-needle technique.
During the irrigation procedure needles can be rotated and displaced to increase calcium disaggregation and fragmentation. The use of warm saline solution may shorten the procedure and improve calcification dissolution (Fig. 6) (2).
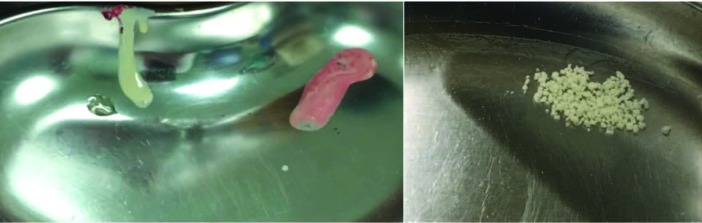
Figure 6.
(A) Out-flow of calcium deposit with toothpaste-like consistency. (B) After few minutes the calcium tends to form aggregates.
Postprocedural treatment
At the end of the procedure, to reduce the risk of postprocedural bursitis, US-guided intrabursal injection of local anaesthetics and slow-release steroids is indicated (35).
After the treatment a short course of nonsteroidal anti-inflammatory drugs (NSAIDs), a period of relative rest (~15 days), and physiokinetic therapy are recommended.
Clinical outcome and complications
In the short-term period the worsening of symptoms is frequent, but normally followed by a quick resolution (~48 h). In the middle and long-term period many authors reported a greater reduction of pain, compared to patients who refused the treatment, and a significant improvement of shoulder function.
A recent sistematic review reported a 10% complication rate: bursitis was the most frequent, that occured in 7% of all procedures. Other complications included vasovagal reactions (2%), frozen shoulder (0,2%), seizures (0,2%), tenosynovitis of the bicipital long head (0,1%) (2) (36).
Conclusions
Magnetic Resonance Imaging (MRI), thanks to its excellent soft tissue contrast and multiplanar capability, is the primary imaging tool for a variety of conditions and diseases both for diagnostic and interventional purposes (37-48) but US-PICT has been demonstreted to be a quick, minimally invasive, low cost and effective procedure for treating RCCT, regardless of the use of a single- or double-needle tecnique. It lead to significant long term improvement in the shoulder function and is very effective in the short term with regard to pain relief.
Ethical approval:
This article does not contain any studies with human participants performed by any of the authors.
Conflict of interest:
None to declare
References
- 1.Speed CA, Hazleman BL. Calcific tendinitis of the shoulder. N Engl J Med. 1999;340:1582–4. doi: 10.1056/NEJM199905203402011. [DOI] [PubMed] [Google Scholar]
- 2.Lanza E, Banfi G, Serafini G, et al. Ultrasound-guided percutaneous irrigation in rotator cuff calcific tendinopathy: what is the evidence? A systematic review with proposals for future reporting. Eur Radiol. 2015;25:2176–83. doi: 10.1007/s00330-014-3567-1. [DOI] [PubMed] [Google Scholar]
- 3.Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87:187–202. doi: 10.2106/JBJS.D.01850. [DOI] [PubMed] [Google Scholar]
- 4.Uhthoff HK, Sarkar K. Calcifying tendinitis. Baillieres Clin Rheumatol. 1989;3:567–81. doi: 10.1016/s0950-3579(89)80009-3. [DOI] [PubMed] [Google Scholar]
- 5.Mariani S, La Marra A, Arrigoni F, et al. Dynamic measurement of patello-femoral joint alignment using weight-bearing magnetic resonance imaging (WB-MRI) Eur J Radiol. 2015;84:2571–78. doi: 10.1016/j.ejrad.2015.09.017. [DOI] [PubMed] [Google Scholar]
- 6.Barile A, Bruno F, Arrigoni F, et al. Emergency and Trauma of the Ankle. Semi Musc Rad. 2017;21:282–89. doi: 10.1055/s-0037-1602408. [DOI] [PubMed] [Google Scholar]
- 7.Splendiani A, D’Orazio F, Patriarca L, et al. Imaging of post-operative spine in intervertebral disc pathology. Musculoskelet Surg. 2017;101:75–84. doi: 10.1007/s12306-017-0453-4. [DOI] [PubMed] [Google Scholar]
- 8.Arrigoni F, Gregori LM, Zugaro L, Barile A, Masciocchi C. MRgFUS in the treatment of MSK lesions: A review based on the experience of the university of L’aquila, Italy. Transl Cancer Res. 2014;3:442–48. [Google Scholar]
- 9.Reginelli A, Zappia M, Barile A, Brunese L. Strategies of imaging after orthopedic surgery. Musculoskelet Surg. 2017;101:1. doi: 10.1007/s12306-017-0458-z. [DOI] [PubMed] [Google Scholar]
- 10.Cicala D, Briganti F, Casale L, et al. Atraumatic vertebral compression fractures: Differential diagnosis between benign osteoporotic and malignant fractures by MRI. Musculoskelet Surg. 2013;97:S169–S79. doi: 10.1007/s12306-013-0277-9. [DOI] [PubMed] [Google Scholar]
- 11.Barile A, Arrigoni F, Bruno F, et al. Present role and future perspectives of interventional radiology in the treatment of painful bone lesions. Future Oncol. 2018;14:2945–55. doi: 10.2217/fon-2017-0657. [DOI] [PubMed] [Google Scholar]
- 12.Arrigoni F, Bruno F, Zugaro L, et al. Developments in the management of bone metastases with interventional radiology. Acta Biomed. 2018;89:166–74. doi: 10.23750/abm.v89i1-S.7020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zappia M, Capasso R, Berritto D, et al. Anterior cruciate ligament reconstruction: MR imaging findings. Musculoskelet Surg. 2017;101:23–35. doi: 10.1007/s12306-017-0460-5. [DOI] [PubMed] [Google Scholar]
- 14.Masciocchi C, Zugaro L, Arrigoni F, et al. Radiofrequency ablation versus magnetic resonance guided focused ultrasound surgery for minimally invasive treatment of osteoid osteoma: a propensity score matching study. Eur Radiol. 2016;26:2472–81. doi: 10.1007/s00330-015-4111-7. [DOI] [PubMed] [Google Scholar]
- 15.Barile A, Regis G, Masi R, et al. Musculoskeletal tumours: Preliminary experience with perfusion MRI. Radiol Med. 2007;112:550–61. doi: 10.1007/s11547-007-0161-5. [DOI] [PubMed] [Google Scholar]
- 16.Barile A, Arrigoni F, Zugaro L, et al. Minimally invasive treatments of painful bone lesions: state of the art. Med Oncol. 2017;34:53. doi: 10.1007/s12032-017-0909-2. [DOI] [PubMed] [Google Scholar]
- 17.Barile A, Arrigoni F, Bruno F, et al. Computed Tomography and MR Imaging in Rheumatoid Arthritis. Radiol Clin North Am. 2017;55:997–1007. doi: 10.1016/j.rcl.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 18.Aliprandi A, Di Pietto F, Minafra P, Zappia M, Pozza S, Sconfienza LM. Femoro-acetabular impingement: What the general radiologist should know. Radiol Med. 2014;119:103–12. doi: 10.1007/s11547-013-0314-7. [DOI] [PubMed] [Google Scholar]
- 19.Cuomo G, Zappia M, Iudici M, Abignano G, Rotondo A, Valentini G. The origin of tendon friction rubs in patients with systemic sclerosis: a sonographic explanation. Arthritis Rheum. 2012;64:1291–93. doi: 10.1002/art.34319. [DOI] [PubMed] [Google Scholar]
- 20.Zappia M, Castagna A, Barile A, Chianca V, Brunese L, Pouliart N. Imaging of the coracoglenoid ligament: a third ligament in the rotator interval of the shoulder. Skeletal Radiol. 2017;46:1101–11. doi: 10.1007/s00256-017-2667-9. [DOI] [PubMed] [Google Scholar]
- 21.Di Pietto F, Chianca V, De Ritis R, et al. Postoperative imaging in arthroscopic hip surgery. Musculoskelet Surg. 2017;101:43–49. doi: 10.1007/s12306-017-0459-y. [DOI] [PubMed] [Google Scholar]
- 22.Perrotta FM, Astorri D, Zappia M, Reginelli A, Brunese L, Lubrano E. An ultrasonographic study of enthesis in early psoriatic arthritis patients naive to traditional and biologic DMARDs treatment. Rheumatol Int. 2016;36:1579–83. doi: 10.1007/s00296-016-3562-8. [DOI] [PubMed] [Google Scholar]
- 23.Barile A, La Marra A, Arrigoni F, et al. Anaesthetics, steroids and platelet-rich plasma (PRP) in ultrasound-guided musculoskeletal procedures. Br J Radiol. 2016;89:20150355. doi: 10.1259/bjr.20150355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Di Giacomo V, Trinci M, van der Byl G, Catania VD, Calisti A, Miele V. Ultrasound in newborns and children suffering from non-traumatic acute abdominal pain: imaging with clinical and surgical correlation. J Ultrasound. 2015;18:385–93. doi: 10.1007/s40477-014-0087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Farin PU, Jaroma H. Sonographic findings of rotator cuff calcifications. J Ultrasound Med. 1995;14:7–14. doi: 10.7863/jum.1995.14.1.7. [DOI] [PubMed] [Google Scholar]
- 26.Tagliafico A, Russo G, Boccalini S, et al. Ultrasound-guided interventional procedures around the shoulder. Radiol Med. 2014;119:318–26. doi: 10.1007/s11547-013-0351-2. [DOI] [PubMed] [Google Scholar]
- 27.Gartner J, Heyer A. [Calcific tendinitis of the shoulder] Orthopade. 1995;24:284–302. [PubMed] [Google Scholar]
- 28.Zoccali C, Rossi B, Zoccali G, et al. A new technique for biopsy of soft tissue neoplasms: a preliminary experience using MRI to evaluate bleeding. Minerva Med. 2015;106:117–20. [PubMed] [Google Scholar]
- 29.Masciocchi C, Conti L, D’Orazio F, Conchiglia A, Lanni G, Barile A. Errors in Musculoskeletal MRI. In: Romano L, Pinto A, editors. Errors in Radiology. Milano: Springer Milan; 2012. pp. 209–17. [Google Scholar]
- 30.Limbucci N, Rossi F, Salvati F, Pistoia LM, Barile A, Masciocchi C. Bilateral suprascapular nerve entrapment by glenoid labral cysts associated with rotator cuff damage and posterior instability in an amateur weightlifter. J Sports Med Phys Fitness. 2010;50:64–7. [PubMed] [Google Scholar]
- 31.Barile A, Bruno F, Mariani S, et al. What can be seen after rotator cuff repair: a brief review of diagnostic imaging findings. Musculoskelet Surg. 2017;101:3–14. doi: 10.1007/s12306-017-0455-2. [DOI] [PubMed] [Google Scholar]
- 32.De Witte PB, Selten JW, Navas A, et al. Calcific tendinitis of the rotator cuff: a randomized controlled trial of ultrasound-guided needling and lavage versus subacromial corticosteroids. Am J Sports Med. 2013;41:1665–73. doi: 10.1177/0363546513487066. [DOI] [PubMed] [Google Scholar]
- 33.Serafini G, Sconfienza LM, Lacelli F, Silvestri E, Aliprandi A, Sardanelli F. Rotator cuff calcific tendonitis: short-term and 10-year outcomes after two-needle us-guided percutaneous treatment--nonrandomized controlled trial. Radiology. 2009;252:157–64. doi: 10.1148/radiol.2521081816. [DOI] [PubMed] [Google Scholar]
- 34.Sconfienza LM, Serafini G, Sardanelli F. Treatment of calcific tendinitis of the rotator cuff by ultrasound-guided single-needle lavage technique. AJR Am J Roentgenol. 2011;197:W366. doi: 10.2214/AJR.10.6295. author reply 67. [DOI] [PubMed] [Google Scholar]
- 35.Sconfienza LM, Bandirali M, Serafini G, et al. Rotator cuff calcific tendinitis: does warm saline solution improve the short-term outcome of double-needle US-guided treatment? Radiology. 2012;262:560–6. doi: 10.1148/radiol.11111157. [DOI] [PubMed] [Google Scholar]
- 36.Oudelaar BW, Schepers-Bok R, Ooms EM, Huis In ‘t Veld R, Vochteloo AJ. Needle aspiration of calcific deposits (NACD) for calcific tendinitis is safe and effective: Six months follow-up of clinical results and complications in a series of 431 patients. Eur J Radiol. 2016;85:689–94. doi: 10.1016/j.ejrad.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 37.Tedeschi E, Caranci F, Giordano F, Angelini V, Cocozza S, Brunetti A. Gadolinium retention in the body: what we know and what we can do. Radiol Med. 2017;122:589–600. doi: 10.1007/s11547-017-0757-3. [DOI] [PubMed] [Google Scholar]
- 38.Briganti F, Leone G, Marseglia M, Cicala D, Caranci F, Maiuri F. P64 Flow Modulation Device in the treatment of intracranial aneurysms: Initial experience and technical aspects. J Neurointerv Surg. 2016;8:173–80. doi: 10.1136/neurintsurg-2015-011743. [DOI] [PubMed] [Google Scholar]
- 39.Arrigoni F, Barile A, Zugaro L, et al. Intra-articular benign bone lesions treated with Magnetic Resonance-guided Focused Ultrasound (MRgFUS): imaging follow-up and clinical results. Med Oncol. 2017;34:55. doi: 10.1007/s12032-017-0904-7. [DOI] [PubMed] [Google Scholar]
- 40.Cirillo M, Caranci F, Tortora F, et al. Structural neuroimaging in dementia. J Alzheimers Dis. 2012;29:16–19. [Google Scholar]
- 41.Schicchi N, Valeri G, Moroncini G, et al. Myocardial perfusion defects in scleroderma detected by contrast-enhanced cardiovascular magnetic resonance. Radiol Med. 2014;119:885–94. doi: 10.1007/s11547-014-0419-7. [DOI] [PubMed] [Google Scholar]
- 42.Tarantini G, Favaretto E, Napodano M, et al. Design and methodologies of the postconditioning during coronary angioplasty in acute myocardial infarction (POST-AMI) trial. Cardiology. 2010;116:110–16. doi: 10.1159/000316967. [DOI] [PubMed] [Google Scholar]
- 43.Salvolini L, Urbinati C, Valeri G, Ferrara C, Giovagnoni A. Contrast-enhanced MR cholangiography (MRCP) with GD-EOB-DTPA in evaluating biliary complications after surgery. Radiol Med. 2012;117:354–68. doi: 10.1007/s11547-011-0731-4. [DOI] [PubMed] [Google Scholar]
- 44.Bertolini L, Vaglio A, Bignardi L, et al. Subclinical interstitial lung abnormalities in stable renal allograft recipients in the era of modern immunosuppression. Transplantation Proceedings. 2011;43:2617–2623. doi: 10.1016/j.transproceed.2011.06.033. ISSN: 0041-1345, doi: 10.1016/j.transproceed.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 45.Palma BD, Guasco D, Pedrazzoni M, et al. Osteolytic lesions, cytogenetic features and bone marrow levels of cytokines and chemokines in multiple myeloma patients: Role of chemokine (C-C motif) ligand20. Leukemia. 2016 Feb;30(2):409–16. doi: 10.1038/leu.2015.259. doi: 10.1038/leu.2015.259. Epub 2015 Sep 30. [DOI] [PubMed] [Google Scholar]
- 46.Bozzetti C, Nizzoli R, Tiseo M, et al. ALK and ROS1 rearrangements tested by fluorescence in situ hybridization in cytological smears from advanced non-small cell lung cancer patients. Diagnostic Cytopathology. 43:941–946. doi: 10.1002/dc.23318. ISSN: 8755-1039, doi: 10.1002/dc.23318. [DOI] [PubMed] [Google Scholar]
- 47.De Filippo M, Gira F, Corradi D, Sverzellati N, Zompatori M, Rossi C. Benefits of 3D technique in guiding percutaneous retroperitoneal biopsies. RAD. MED. 2011;116(3):407–416. doi: 10.1007/s11547-010-0604-2. ISSN: 0033-8362, doi: 10.1007/s11547-010-0604-2. [DOI] [PubMed] [Google Scholar]
- 48.De Filippo M, Onniboni M, Rusca M, et al. Advantages of multidetector row CT with multiplanar reformation in guiding percutaneous lung biopsies. RAD. MED. 2008;113:945–953. doi: 10.1007/s11547-008-0325-y. ISSN: 0033-8362, doi: 10.1007/s11547-008-0325-y. [DOI] [PubMed] [Google Scholar]