Abstract
The aim of this article is to provide an imaging review of normal anatomy, most common anatomical variants and pathologies of the long head of the biceps tendon (LHB) encountered during the daily practice. (www.actabiomedica.it)
Keywords: LHB, MR, MR-Arthrography
Anatomy
The term “biceps brachii” derives from the Latin Language and it stands for the “two heads of the arm”. As the same name suggests, this muscle has two separate origins, but both are innervated by the musculocutaneous nerve, a mixed nerve originating from the lateral cord (C5-C7) (1). The short head has an extraarticular localization and it has origin from the coracoid process of the scapula blending with the coracobrachial tendon. LHB is long about 9 cm and has partially origin from the tubercle; at first, it passes in the intraarticular location to leave then the capsule and enter its bone groove (2-4). The LHB tendon is innervated by a network of sensory sympathetic fibers with a higher degree of innervation at the origin, and it explains the role in the genesis of anterior shoulder pain (5).
Intraarticular portion
During its intra-articular course, the long head of the biceps passes through the rotator interval, a triangle formed super-laterally from the anterior edge of the supraspinatus tendon and inferiorly from the upper edge of the subscapularis tendon. The base of the triangle corresponds to the base of the coracoid process and the apex of the transverse ligament. The rotator interval can be considered a rotator cuff defect formed by the protrusion of the coracoid process between the tendons of the supraspinatus and subscapularis (6). Along with its course in the rotator interval, the LHB tendon is stabilized by a capsule-ligamentous complex called the bicipital pulley, formed by the coracohumeral and superior glenohumeral ligaments (Fig. 1).
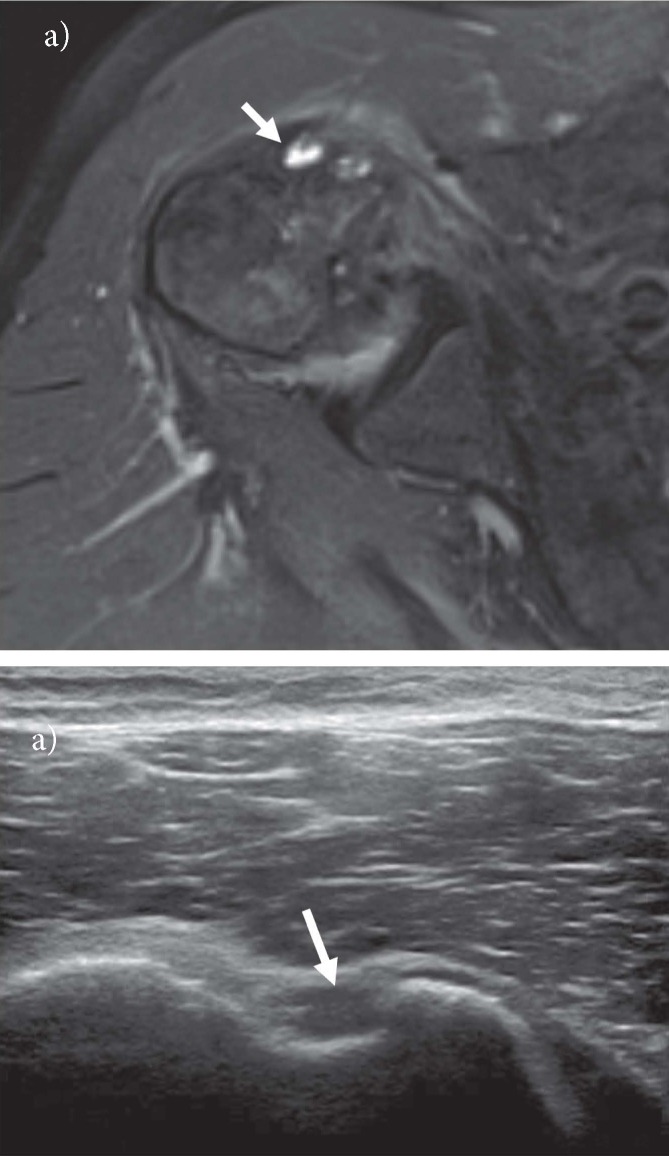
Figure 1.
Oblique sagittal fat-saturated T1-weighted magnetic resonance arthrographic (MRA) image depicts biceps pulley (black arrow) forming a sling around LHB tendon (white arrow)
The coraco-humeral ligament originates from the postero-lateral portion of the base of the coracoid process and distally opens into two bands; the medial and smaller band pass over the LHB and look at the small tuberosity and the lateral and broader band pass on the great tuberosity and the anterior portion of the supraspinatus tendon. The superior glenohumeral ligament has origin from the superior glenoid tubercle, anteriorly to the biceps tendon, and it inserts on the lesser tuberosity (7). There is a third ligament in the rotator interval of the shoulder, the coracoglenoid ligament (CGL), that forms a part of the anterosuperior capsuloligamentous complex of the shoulder (8) (Fig. 2).
Figure 2.
Axial T1w MRA image shows an independent course of coraco-glenoid ligament (arrow) from the anterior aspect of the glenoid to the proximal aspect of the coracoid
Extra-articular portion
Distally to its pulley, the LHB tendon leaves the articular joint space entering the bicipital groove, formed by the greater and lesser humeral tuberosity. At the exit of the articular cavity, the LHB is covered by a sheath deriving from a synovial extroflection of the glenohumeral articular capsule. The LHB sheath inserts into the third proximal of the humerus.
Inside this synovial sheath we could find a structure called “vinculum”, a membrane which develops from the humeral groove to the LHB, inserting superiorly on the rotator interval, contributing to the vascular supply of the tendon (Fig. 3). The integrity of this structure during the complete lesions of the LHB seems to prevent the “Popeye” deformity (9). The term vinculum has not to be confused with the mesotenon (some of mesotenons are called vincula, too) which connect the intraarticular portion of the LHB tendon with the superior capsular one (10).
Figure 3.
Axial T1w MRA image shows a vinculum (arrow) in the synovial sheath of LHB tendon
In the proximal portion of the bicipital groove, the tendon appears to be covered by the transverse ligament. Described at the beginning of the XXth century, this structure does not play a significant role in LHB stability. However, today, the transverse ligament is not purely considered a ligament but represents the expansion of the subscapularis tendon joined with the supraspinatus tendon, the coracohumeral ligament (8) and, according to some authors, with the pectoralis minor too (11).
Anatomical variants
The LHB tendon shows a great variability among individuals and the radiological literature is rich of works about that.
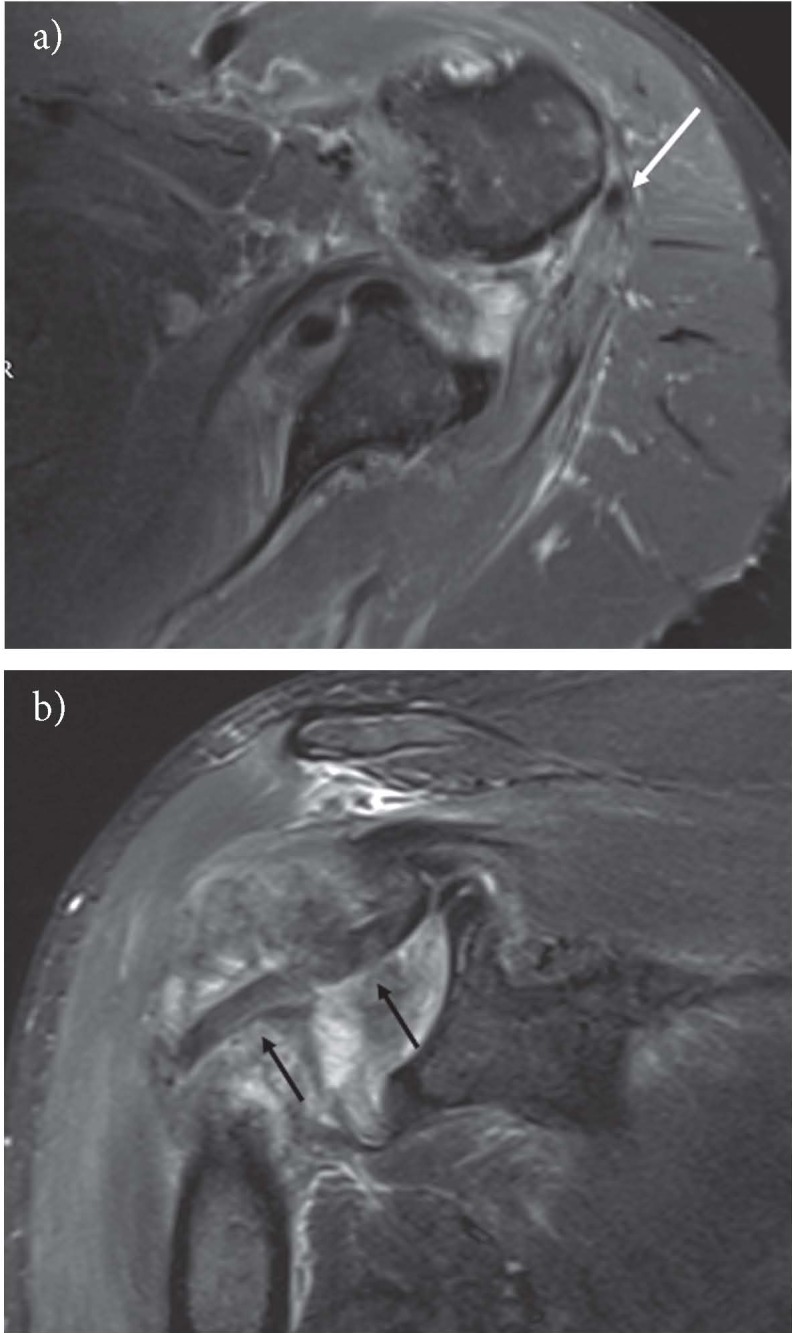
A first element of this variability can be the number of tendons. The tendon and the muscular head can be absent (12). It is not uncommon the visualization of a double tendon of the LHB, both with Ultrasound (US) and Magnetic Resonance (MR) (Fig. 4a-b) (13). The two tendons could have a common origin from the supraglenoid tubercle splitting then later, or, as it more often happens, they could have a double origin (14). In the case of a double origin, a tendon has origin from the supraglenoid tubercle while the other one from the superior capsule (13, 15). Some authors think that in these cases, the second structure present in the bicipital sheath is not a second tendon but an aponeurotic expansion (16). In literature, some cases, where the brachial biceps appears with three or more heads, have been reported (17-19).
Figure 4.
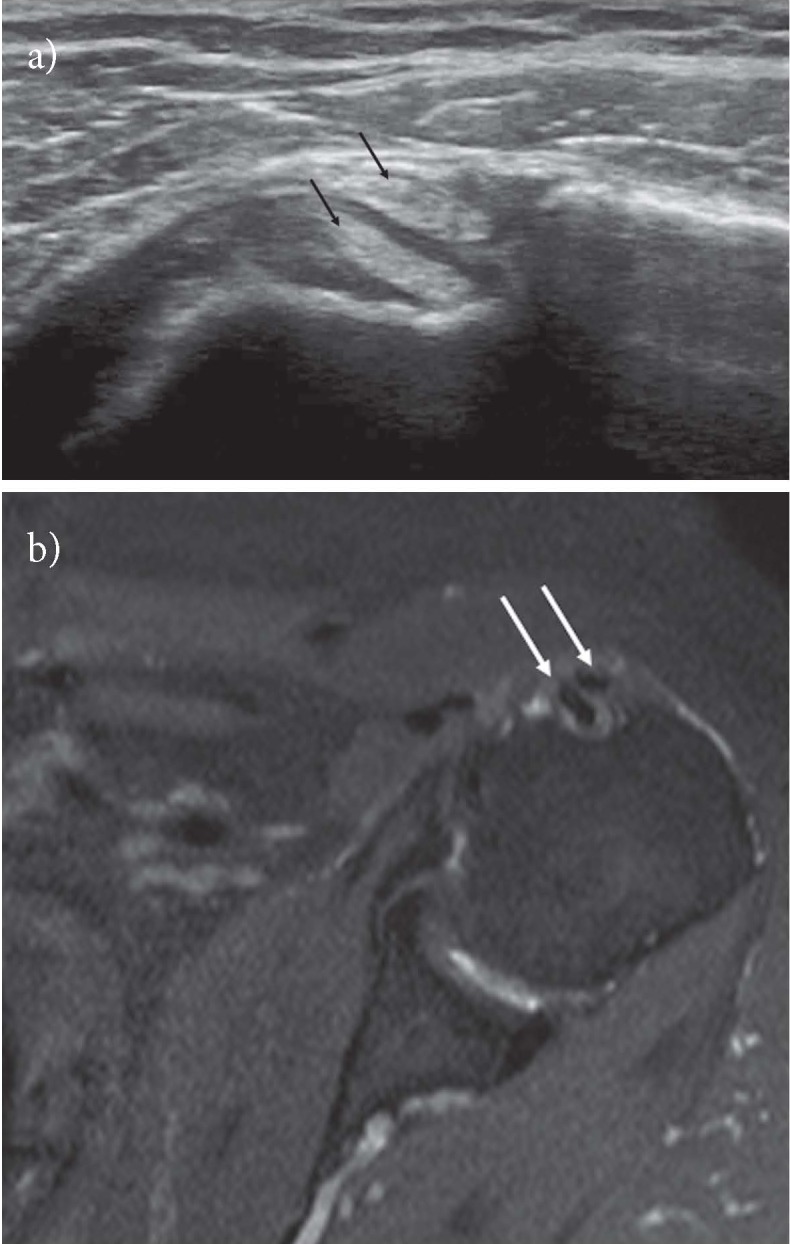
Two separate LHB tendons within the bicipital groove are demonstrated on US short scan image (a) (black arrows) and on axial PD fat-saturated image (b) (white arrows)
Even if there are few works about that, the presence of anatomical variants of the LHB are considered the cause of a pathology (10, 20).
The proximal insertion of the LHB represents a further site of variability. The presence of recesses or of a “meniscoid insertion” could be the cause of pitfalls in MR and MR-Arthrography. The last element of variability is represented by the presence of the mesotenon, that is the structure connecting the intraarticular portion of the LHB and the superior capsule. These structures, in according to our knowledge, have never been studied with imaging.
The presence of recesses or “meniscoid insertion” can represent a pitfall in MR and MR arthrography. The last element of variability is the presence of mesotenon, a synovial band connecting the rotator cuff with the intrarticular portion of LHB (10). According to our knowledge, the mesotenon has never been studied with imaging.
Biomechanics
The role of the LHB tendon is still controversial; many electromyographical studies demonstrate that it does not play an active role in shoulder movements but only in the elbow ones (21), while some authors assert that it has an active role in the depression of the humeral head during shoulder abduction (22, 23).
LHB tendon instabilities
The instabilities of the long head of the biceps are widely discussed in the radiological and orthopedic literature. For an educational purpose, it is possible to distinguish the microinstability forms of the LHB characterized by the initial lesion of its pulley where the tendon appears instable only in its intraarticular portion, from the most severe and tardive forms which affect also the extraarticular portion of the tendon (24).
LHB pulley lesions
The lesions of the biceps pulley have been identified as “primum movens” of the LHB instability and they represent a cause of chronic shoulder pain, resistant to the conservative therapy.
These lesions could be caused by acute traumas, repeated microtraumas, degenerative causes, or they could be associated to lesions of the rotator cuff (7). Habermayer et al. have distinguished the pulley lesions in 4 groups (25): group 1 - isolated lesion of the superior glenohumeral ligament; group 2 - lesion of the superior glenohumeral ligament associated to a partial articular lesion of the supraspinatus tendon; group 3 - lesion of the superior glenohumeral ligament associated to a partial articular lesion of the subscapular; group 4 - lesion of the superior glenohumeral ligament associated to a partial articular lesion both of the supraspinatus tendon and the subscapularis one. These lesions were defined by Walch as “Hidden Lesions” because they were arthroscopically difficult to identify (26).
Imaging
Magnetic resonance (MR) and Ultrasonography (US) are the most largely used imaging tool in many diagnostic and interventional settings in radiology and particularly in musculoskeletal radiology (27-38).
In the isolated pulley lesions, although the LHB is unstable in its intraarticular portion, it may not show a clear instability in the extraarticular portion and for this reason there may be no contact loss between the tendon and its bone groove (39). Therefore, the radiological examination plays no role in this pathological phase.
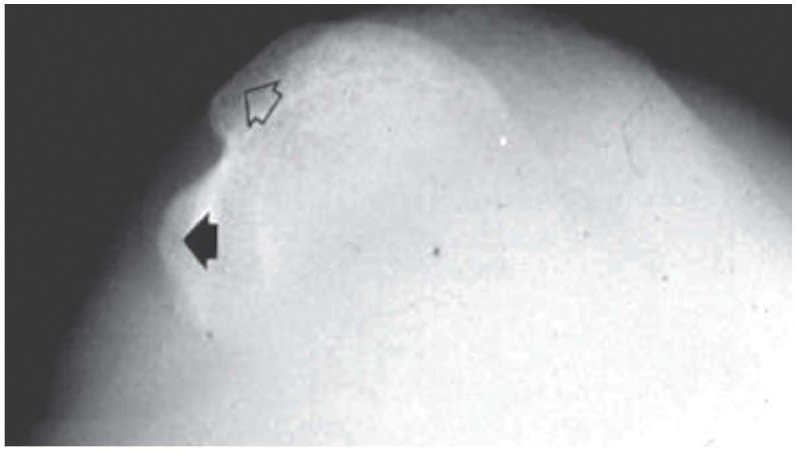
Although it is possible to identify the LHB pulley with ultrasound, there are no studies in literature which demonstrate the possibility of directly assessing its lesions. However, it is possible to identify an indirect sign of pulley lesion, called “Chondral print” (40) (Fig. 5). As assessed by the arthroscopic studies of Castagna et al., the increase of the LHB intraarticular portion mobility caused by the lesion of its pulley, determines the erosion of the underlying cartilaginous humeral profile. With an accuracy of the 96%, the ultrasound identification of the chondral print can be used as an indirect sign to reveal also those early forms of the LHB instability caused by the pulley isolated lesions (41).
Figure 5.

Short axis US scan of intrarticular portion of LHB shows a subchondral irregularity called “chondral print” (arrow) on humeral head at the level of the rotator interval
The standard MR images show only some parts of the LHB intracapsular portion and the ligaments of the bicipital pulley are poorly evaluable. Only on MR arthrography it is possible to directly evaluate the LHB pulley and its lesions (7, 42-44).
Barile et al. revealed a weak agreement between arthroscopy and MR imaging for Habermayer group 1 injury, an excellent agreement for group 2 and group 4 lesions and a good one for group 3 lesion (39).
On contrary, Schaeffeler et al. demonstrated high accuracy in the detection of the isolated pulley lesions using the “displacement sign” in the oblique sagittal sequences (45) (Fig. 6).
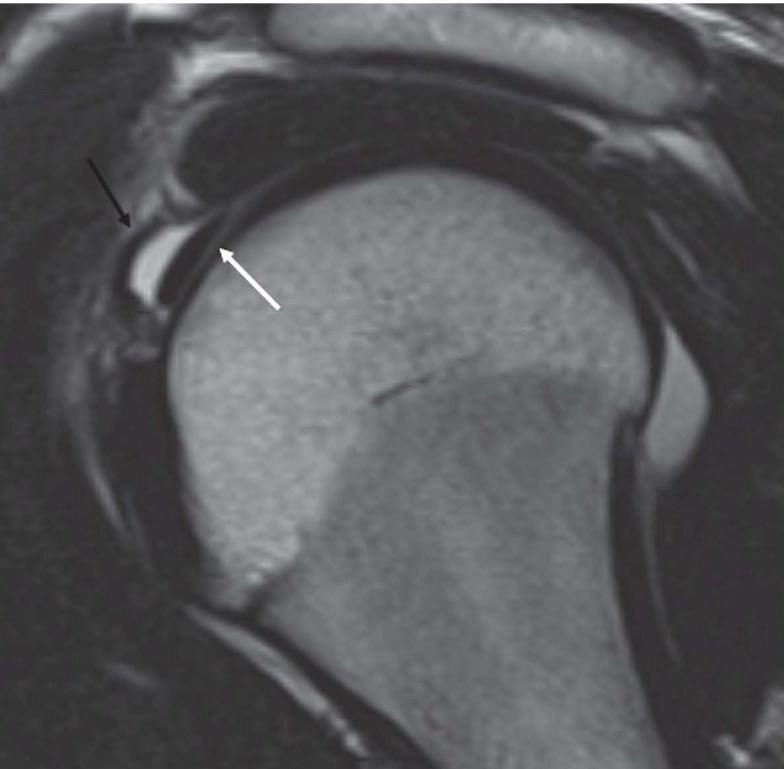
Figure 6.
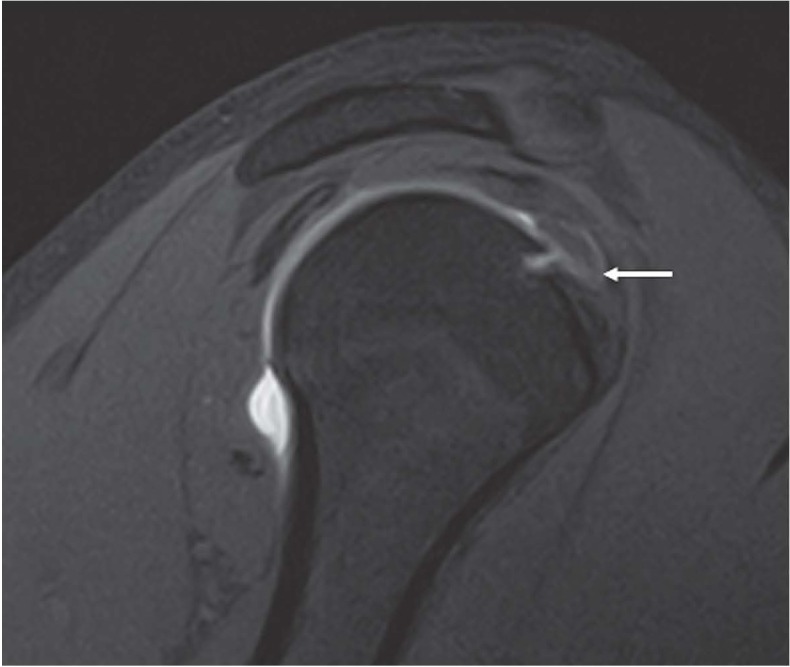
Sagittal PDw fat-saturated MRA image shows “displacement sign”. The LHB tendon (arrow) is dislocated inferiorly, on the superior border of the SSC tendon
Chandiani et al. reported for the MR arthrography 100% sensitivity, 94% specificity and 94% diagnostic accuracy in the diagnosis of superior glenohumeral ligament lesions (46).
Luxation and subluxation of LHB
The instabilities which involve also the extraarticular portion of the tendon could be considered an advanced stage of this pathology. The complete pulley lesion, associated or not with a rotator cuff lesion, determines a partial loss of contact (subluxation) or a complete one (dislocation) between the LHB tendon and its bone groove. The classification of Walch et al. is still among the most used (47). In their work Walch defines the LHB subluxation as a partial and reducible loss of the contact between the tendon and its bone groove. The dislocation was defined as a permanent loss of contact between the tendon and the intertubercular groove and it has been classified into four types:
- LHB tendon dislocation “inside” the subscapularis tendon (Fig. 7)
Figure 7.
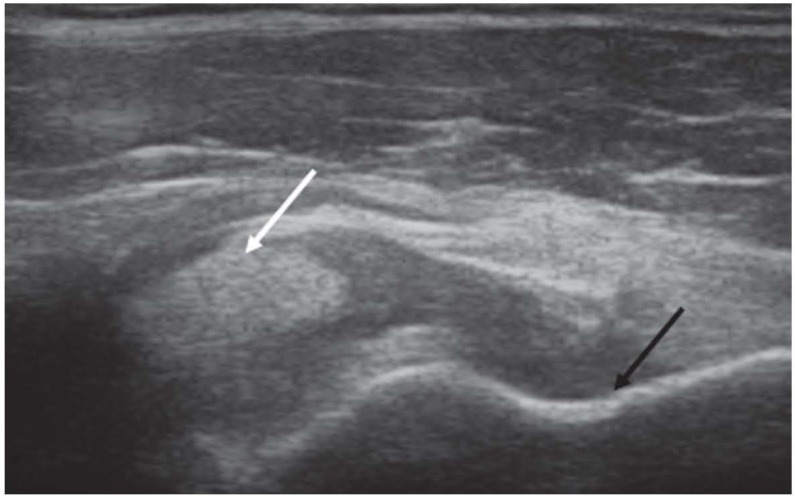
Short axis US scan of LHB shows medial dislocation of tendon (white arrow) inside subscapularis fibers. The LHB bone groove is empty (black arrow)
- intraarticular tendon dislocation with complete tearing of all anterior muscle and ligaments, but there is intact anterior fascia.
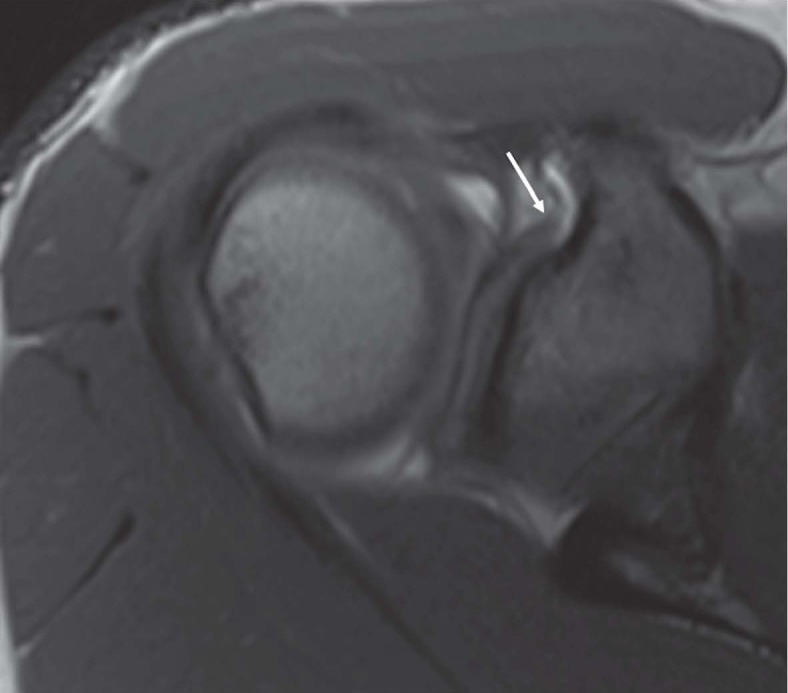
- intraarticular tendon dislocation with complete tear of both subscapularis tendon and the anterior fascia; rarely the LHB dislocated intraarticularly can be incarcerated in the gleno-humeral joint space (Fig. 8)
Figure 8.

Axial T1w MRA image shows complete tear of subscapularis tendon. The LHB tendon is dislocated medially and it is incarcerated in the joint space (arrow)
- extraarticular dislocation of the LHB tendon over the intact suprascapular tendon as a consequence of a supraspinatus lesion extending and involving the lateral band of the coraco-humeral ligament (Fig. 9).
Figure 9.
Axial PDw MRA image shows a dislocated LHB tendon (arrow) over the intact fibers of suprascapular tendon
The posterior dislocation of the LHB tendon as a consequence of the anterior dislocation of the humeral head has been described (48-51) (Fig. 10 a-b).
Figure 10.
Axial PDw fat-saturated image (a) shows posterior dislocation of the humeral head. The LHB (white arrow) is dislocated posteriorly to the humeral head. Coronal oblique PDw fat-saturated image (b) shows the oblique course of the dislocated tendon.
Imaging
The radiographic examination, through the modified projection of Fisk, allows a good evaluation of the characteristics of the bicipital bone sulcus (52) (Fig. 11). Cone et al. have highlighted as the presence of a bicipital groove less than 4 mm of depth on the radiographic examination represents one of the predisposing causes of bicipital dislocation (53). The presence of “geodes”, sclerosis and osteophytes, on the other hand, represents the consequence of the pathological movements of the tendon, which will be more evident as the tendinous instability increases (Fig. 12).
Figure 11.
Fisk radiographic projection shows the normal aspect of the bicipital groove with regular medial (black arrowhead) and lateral (white arrowhead) contour.
Figure 12.
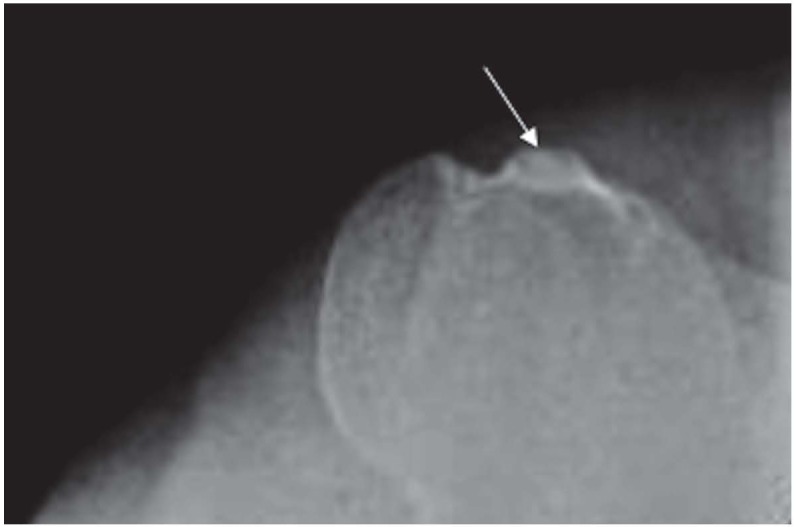
Fisk radiographic projection shows sclerosis (arrows) on the medial aspect of the bicipital groove
Ultrasound shows an excellent diagnostic accuracy in detecting both the dislocations and subluxations of the LHB (54, 55). Also MR and MR arthrography can easily identify the various forms of dislocation and subluxation of LHBT (56, 57).
Tendinopathy and tendon tear
Tendinopathy of LHB tendon is caused by several pathologies such as subacromial impingement, tendon instability or tendon entrapment (hourglass biceps) (58, 59). These biomechanical alterations produce excessive traction, pressure and friction forces to the tendon (60, 61).
Tendon degeneration identifies a range of histopathologic changes. Tendinopathy is characterized by mucoid fibrous changes, increased vascularization and pallor, infiltration and replacement by adipocytes and frequent chondrocytic/chondrometaplasia differentiations. Higher levels of inflammation may occur in the more proximal two-thirds of the LHB tendon (62).
Tendinopathy is associated with chronic pain that has an insidious onset and a progressive course. Repeated stress applied to a degenerate tendon can determine partial or complete tear (63).
Contrary to the tendon, in patients with anterior chronic pain the synovium of the sheath of the shoulder does not show significant inflammatory changes (62).
Imaging
Ultrasonography (US) is the least invasive imaging examination, well tolerated by patients. This technique does not employ ionizing radiations, as Magnetic Resonance (MR), and is widely used musculoskeletal radiology (64-73).
US is accurate to diagnose a normal biceps tendon or full-thickness tear, but it is less accurate in the identification of partial-thickness tear and tendinopathy (74). In tendinopathy the LHB may appear abnormally hypoechoic and possibly thickened and may eventually progress to longitudinal partial tear (Fig. 13). The use of Color-Doppler is useful for the evaluation of active inflammation of the tendon (75). A moderate tenosynovitis could be associated to the tendinopathy, and synovial hypoechoic fluid or synovial hyperechoic hypertrophy tissue around the LHB tendon could be detected (60, 76).
Figure 13.
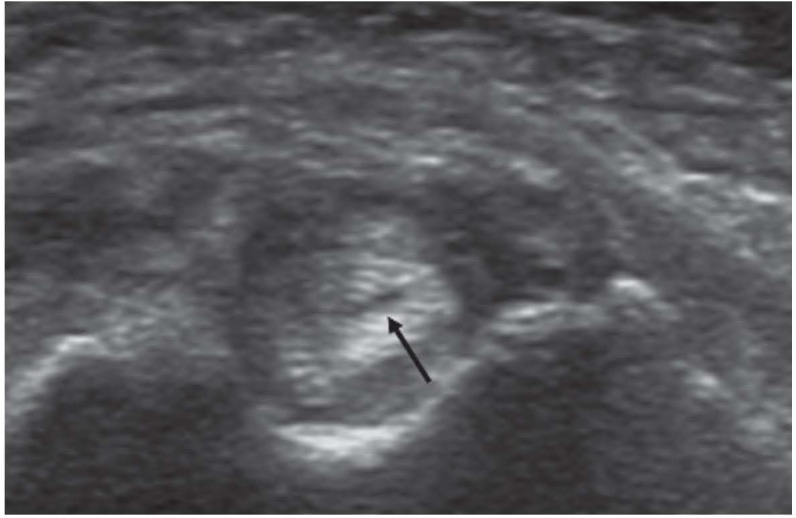
Short axis US scan of LHB shows a thickened tendon with a focal hypoechoic area due to a longitudinal tear (arrow)
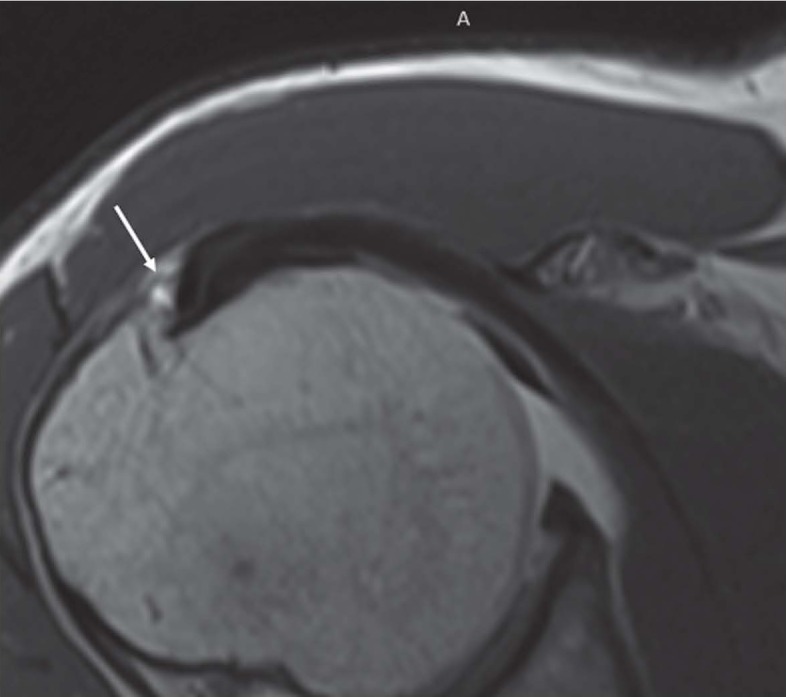
Using arthroscopy as reference standard, the MR has shown adequate accuracy in diagnosis of tendinopathy, partial and full thickness tears (77). On the contrary, MR does not correlate with histologic severity of tendinopathy. Higher levels of inflammatory and histopathologic changes have been found in tendons that had appeared normal in MR (62). The thickening of the intrarticular portion of the tendon on sagittal sequences is the most specific sign of tendinopathy (23, 77) (Fig. 14).
Figure 14.
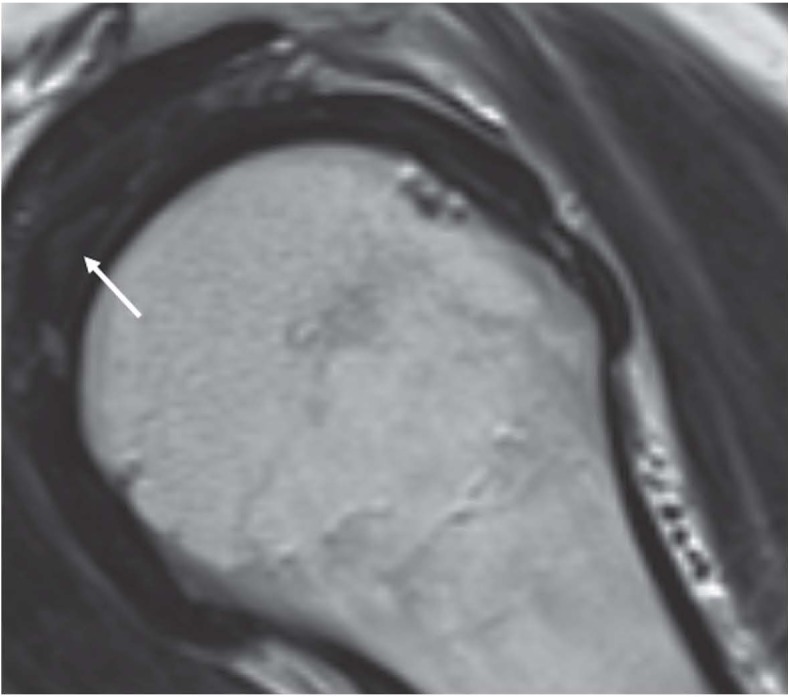
Oblique sagittal T2w image shows thickened and hyperintense LHB tendon (arrow)
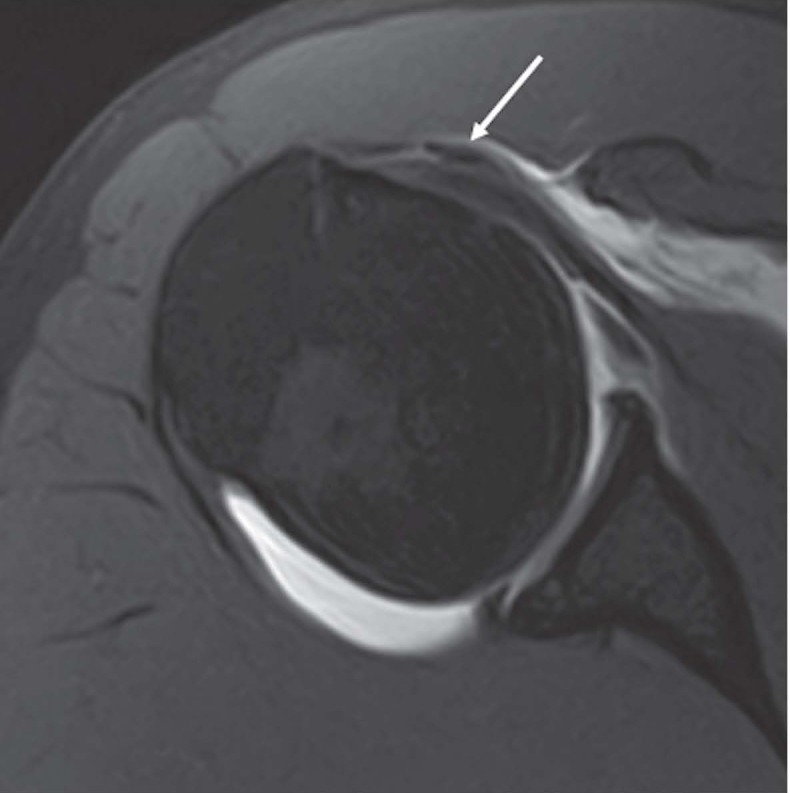
The presence of high signal within the tendon on T2w sequences indicates circumferential or longitudinal partial-thickness tear (Fig. 15). The absence of the LHB tendon in its bony groove indicates a complete rupture or a previous tenotomy (Fig. 16 a-b) (78) .
Figure 15.
Axial PDw fat-saturated MRI shows high signal (arrow) within the tendon, indicating partial-thickness tear
Figure 16.
(a) Axial PDw fat-saturated MRI and (b) short axis US scan of LHB show the absence of the tendon and empty bicipital groove (arrow)
Conflict of interest:
None to declare
References
- 1.Sirico F, Castaldo C, Baioccato V, et al. Prevalence of musculocutaneous nerve variations: Systematic review and meta-analysis. Clin Anat. 2019;32:183–95. doi: 10.1002/ca.23256. [DOI] [PubMed] [Google Scholar]
- 2.Beltran J, Jbara M, Maimon R. Shoulder: labrum and bicipital tendon. Top Magn Reson Imaging. 2003;14:35–49. doi: 10.1097/00002142-200302000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Vangsness CT Jr, Jorgenson SS, Watson T, Johnson DL. The origin of the long head of the biceps from the scapula and glenoid labrum. An anatomical study of 100 shoulders. J Bone Joint Surg Br. 1994;76:951–4. [PubMed] [Google Scholar]
- 4.Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011;27:581–92. doi: 10.1016/j.arthro.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 5.Alpantaki K, McLaughlin D, Karagogeos D, Hadjipavlou A, Kontakis G. Sympathetic and sensory neural elements in the tendon of the long head of the biceps. J Bone Joint Surg Am. 2005;87:1580–3. doi: 10.2106/JBJS.D.02840. [DOI] [PubMed] [Google Scholar]
- 6.Jost B, Koch PP, Gerber C. Anatomy and functional aspects of the rotator interval. J Shoulder Elbow Surg. 2000;9:336–41. doi: 10.1067/mse.2000.106746. [DOI] [PubMed] [Google Scholar]
- 7.Nakata W, Katou S, Fujita A, Nakata M, Lefor AT, Sugimoto H. Biceps pulley: normal anatomy and associated lesions at MR arthrography. Radiographics. 2011;31:791–810. doi: 10.1148/rg.313105507. [DOI] [PubMed] [Google Scholar]
- 8.Zappia M, Castagna A, Barile A, Chianca V, Brunese L, Pouliart N. Imaging of the coracoglenoid ligament: a third ligament in the rotator interval of the shoulder. Skeletal Radiol. 2017;46:1101–11. doi: 10.1007/s00256-017-2667-9. [DOI] [PubMed] [Google Scholar]
- 9.Gothelf TK, Bell D, Goldberg JA, et al. Anatomic and biomechanical study of the biceps vinculum, a structure within the biceps sheath. Arthroscopy. 2009;25:515–21. doi: 10.1016/j.arthro.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 10.Dierickx C, Ceccarelli E, Conti M, Vanlommel J, Castagna A. Variations of the intra-articular portion of the long head of the biceps tendon: a classification of embryologically explained variations. J Shoulder Elbow Surg. 2009;18:556–65. doi: 10.1016/j.jse.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 11.MacDonald K, Bridger J, Cash C, Parkin I. Transverse humeral ligament: does it exist? Clin Anat. 2007;20:663–7. doi: 10.1002/ca.20459. [DOI] [PubMed] [Google Scholar]
- 12.Kumar CD, Rakesh J, Tungish B, Singh DM. Congenital absence of the long head of biceps tendon & its clinical implications: a systematic review of the literature. Muscles Ligaments Tendons J. 2017;7:562–69. doi: 10.11138/mltj/2017.7.3.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gheno R, Zoner CS, Buck FM, et al. Accessory head of biceps brachii muscle: anatomy, histology, and MRI in cadavers. AJR Am J Roentgenol. 2010;194:W80–3. doi: 10.2214/AJR.09.3158. [DOI] [PubMed] [Google Scholar]
- 14.Enad JG. Bifurcate origin of the long head of the biceps tendon. Arthroscopy. 2004;20:1081–3. doi: 10.1016/j.arthro.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Wittstein J, Lassiter T Jr, Taylor D. Aberrant origin of the long head of the biceps: a case series. J Shoulder Elbow Surg. 2012;21:356–60. doi: 10.1016/j.jse.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 16.Moser TP, Cardinal E, Bureau NJ, Guillin R, Lanneville P, Grabs D. The aponeurotic expansion of the supraspinatus tendon: anatomy and prevalence in a series of 150 shoulder MRIs. Skeletal Radiol. 2015;44:223–31. doi: 10.1007/s00256-014-1993-4. [DOI] [PubMed] [Google Scholar]
- 17.Vazquez T, Rodriguez-Niedenfuhr M, Parkin I, Sanudo JR. A rare case of a four-headed biceps brachii muscle with a double piercing by the musculocutaneous nerve. Surg Radiol Anat. 2003;25:462–4. doi: 10.1007/s00276-003-0146-6. [DOI] [PubMed] [Google Scholar]
- 18.Nayak SR, Krishnamurthy A, Kumar M, Prabhu LV, Saralaya V, Thomas MM. Four-headed biceps and triceps brachii muscles, with neurovascular variation. Anat Sci Int. 2008;83:107–11. doi: 10.1111/j.1447-073X.2007.00171.x. [DOI] [PubMed] [Google Scholar]
- 19.Battaglia PJ, Welk AB, Kettner NW. Ultrasound appearance and dynamic evaluation of variant long head of the biceps tendon anatomy with MRI correlation. J Ultrasound. 2015;18:187–9. doi: 10.1007/s40477-014-0125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang AL, Gates CH, Link TM, Ma CB. Abnormal origins of the long head of the biceps tendon can lead to rotator cuff pathology: a report of two cases. Skeletal Radiol. 2014;43:1621–6. doi: 10.1007/s00256-014-1910-x. [DOI] [PubMed] [Google Scholar]
- 21.Yamaguchi K, Riew KD, Galatz LM, Syme JA, Neviaser RJ. Biceps activity during shoulder motion: an electromyographic analysis. Clin Orthop Relat Res. 1997:122–9. doi: 10.1097/00003086-199703000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Warner JJ, McMahon PJ. The role of the long head of the biceps brachii in superior stability of the glenohumeral joint. J Bone Joint Surg Am. 1995;77:366–72. doi: 10.2106/00004623-199503000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Buck FM, Dietrich TJ, Resnick D, Jost B, Pfirrmann CW. Long biceps tendon: normal position, shape, and orientation in its groove in neutral position and external and internal rotation. Radiology. 2011;261:872–81. doi: 10.1148/radiol.11110914. [DOI] [PubMed] [Google Scholar]
- 24.Zappia M, Reginelli A, Russo A, et al. Long head of the biceps tendon and rotator interval. Musculoskelet Surg. 2013;97(2):S99–108. doi: 10.1007/s12306-013-0290-z. [DOI] [PubMed] [Google Scholar]
- 25.Habermeyer P, Magosch P, Pritsch M, Scheibel MT, Lichtenberg S. Anterosuperior impingement of the shoulder as a result of pulley lesions: a prospective arthroscopic study. J Shoulder Elbow Surg. 2004;13:5–12. doi: 10.1016/j.jse.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 26.Walch G, Nove-Josserand L, Levigne C, Renaud E. Tears of the supraspinatus tendon associated with “hidden” lesions of the rotator interval. J Shoulder Elbow Surg. 1994;3:353–60. doi: 10.1016/S1058-2746(09)80020-7. [DOI] [PubMed] [Google Scholar]
- 27.Barile A, Bruno F, Arrigoni F, et al. Emergency and Trauma of the Ankle. Semi Musc Rad. 2017;21:282–89. doi: 10.1055/s-0037-1602408. [DOI] [PubMed] [Google Scholar]
- 28.Barile A, Bruno F, Mariani S, et al. What can be seen after rotator cuff repair: a brief review of diagnostic imaging findings. Musculoskelet Surg. 2017;101:3–14. doi: 10.1007/s12306-017-0455-2. [DOI] [PubMed] [Google Scholar]
- 29.Splendiani A, D’Orazio F, Patriarca L, et al. Imaging of post-operative spine in intervertebral disc pathology. Musculoskelet Surg. 2017;101:75–84. doi: 10.1007/s12306-017-0453-4. [DOI] [PubMed] [Google Scholar]
- 30.Arrigoni F, Gregori LM, Zugaro L, Barile A, Masciocchi C. MRgFUS in the treatment of MSK lesions: A review based on the experience of the university of L’aquila, Italy. Transl Cancer Res. 2014;3:442–48. [Google Scholar]
- 31.Reginelli A, Zappia M, Barile A, Brunese L. Strategies of imaging after orthopedic surgery. Musculoskelet Surg. 2017;101:1. doi: 10.1007/s12306-017-0458-z. [DOI] [PubMed] [Google Scholar]
- 32.Masciocchi C, Conti L, D’Orazio F, Conchiglia A, Lanni G, Barile A. Errors in Musculoskeletal MRI. In: Romano L, Pinto A, editors. Errors in Radiology. Milano: Springer Milan; 2012. pp. 209–17. [Google Scholar]
- 33.Cicala D, Briganti F, Casale L, et al. Atraumatic vertebral compression fractures: Differential diagnosis between benign osteoporotic and malignant fractures by MRI. Musculoskelet Surg. 2013;97:S169–S79. doi: 10.1007/s12306-013-0277-9. [DOI] [PubMed] [Google Scholar]
- 34.Barile A, Arrigoni F, Bruno F, et al. Present role and future perspectives of interventional radiology in the treatment of painful bone lesions. Future Oncol. 2018;14:2945–55. doi: 10.2217/fon-2017-0657. [DOI] [PubMed] [Google Scholar]
- 35.Arrigoni F, Bruno F, Zugaro L, et al. Developments in the management of bone metastases with interventional radiology. Acta Biomed. 2018;89:166–74. doi: 10.23750/abm.v89i1-S.7020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arrigoni F, Barile A, Zugaro L, et al. Intra-articular benign bone lesions treated with Magnetic Resonance-guided Focused Ultrasound (MRgFUS): imaging follow-up and clinical results. Med Oncol. 2017;34:55. doi: 10.1007/s12032-017-0904-7. [DOI] [PubMed] [Google Scholar]
- 37.Tarantini G, Favaretto E, Napodano M, et al. Design and methodologies of the postconditioning during coronary angioplasty in acute myocardial infarction (POST-AMI) trial. Cardiology. 2010;116:110–16. doi: 10.1159/000316967. [DOI] [PubMed] [Google Scholar]
- 38.Salvolini L, Urbinati C, Valeri G, Ferrara C, Giovagnoni A. Contrast-enhanced MR cholangiography (MRCP) with GD-EOB-DTPA in evaluating biliary complications after surgery. Radiol Med. 2012;117:354–68. doi: 10.1007/s11547-011-0731-4. [DOI] [PubMed] [Google Scholar]
- 39.Barile A, Lanni G, Conti L, et al. Lesions of the biceps pulley as cause of anterosuperior impingement of the shoulder in the athlete: Potentials and limits of MR arthrography compared with arthroscopy. Radiol Med. 2013;118:112–22. doi: 10.1007/s11547-012-0838-2. [DOI] [PubMed] [Google Scholar]
- 40.Zappia M, Carfora M, Romano AM, et al. Sonography of chondral print on humeral head. Skeletal Radiol. 2016;45:35–40. doi: 10.1007/s00256-015-2238-x. [DOI] [PubMed] [Google Scholar]
- 41.Castagna A, Mouhsine E, Conti M, et al. Chondral print on humeral head: an indirect sign of long head biceps tendon instability. Knee Surg Sports Traumatol Arthrosc. 2007;15:645–8. doi: 10.1007/s00167-006-0211-x. [DOI] [PubMed] [Google Scholar]
- 42.Chung CB, Dwek JR, Cho GJ, Lektrakul N, Trudell D, Resnick D. Rotator cuff interval: evaluation with MR imaging and MR arthrography of the shoulder in 32 cadavers. J Comput Assist Tomogr. 2000;24:738–43. doi: 10.1097/00004728-200009000-00014. [DOI] [PubMed] [Google Scholar]
- 43.Ho CP. MR imaging of rotator interval, long biceps, and associated injuries in the overhead-throwing athlete. Magn Reson Imaging Clin N Am. 1999;7:23–37. [PubMed] [Google Scholar]
- 44.Lee JC, Guy S, Connell D, Saifuddin A, Lambert S. MRI of the rotator interval of the shoulder. Clin Radiol. 2007;62:416–23. doi: 10.1016/j.crad.2006.11.017. [DOI] [PubMed] [Google Scholar]
- 45.Schaeffeler C, Waldt S, Holzapfel K, et al. Lesions of the biceps pulley: diagnostic accuracy of MR arthrography of the shoulder and evaluation of previously described and new diagnostic signs. Radiology. 2012;264:504–13. doi: 10.1148/radiol.12112007. [DOI] [PubMed] [Google Scholar]
- 46.Chandnani VP, Gagliardi JA, Murnane TG, et al. Glenohumeral ligaments and shoulder capsular mechanism: evaluation with MR arthrography. Radiology. 1995;196:27–32. doi: 10.1148/radiology.196.1.7784579. [DOI] [PubMed] [Google Scholar]
- 47.Walch G, Nove-Josserand L, Boileau P, Levigne C. Subluxations and dislocations of the tendon of the long head of the biceps. J Shoulder Elbow Surg. 1998;7:100–8. doi: 10.1016/s1058-2746(98)90218-x. [DOI] [PubMed] [Google Scholar]
- 48.Freeland AE, Higgins RW. Anterior shoulder dislocation with posterior displacement of the long head of the biceps tendon. Arthrographic findings. A case report. Orthopedics. 1985;8:468–9. doi: 10.3928/0147-7447-19850401-06. [DOI] [PubMed] [Google Scholar]
- 49.Strobel K, Treumann TC, Allgayer B. Posterior entrapment of the long biceps tendon after traumatic shoulder dislocation: findings on MR imaging. AJR Am J Roentgenol. 2002;178:238–9. doi: 10.2214/ajr.178.1.1780238. [DOI] [PubMed] [Google Scholar]
- 50.McArthur C, Welsh F, Campbell C. Posterior dislocation of long head of biceps tendon following traumatic anterior shoulder dislocation: imaging and intra-operative findings. J Radiol Case Rep. 2013;7:19–26. doi: 10.3941/jrcr.v7i9.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mullaney PJ, Bleakney R, Tuchscherer P, Boynton E, White L. Posterior dislocation of the long head of biceps tendon: case report and review of the literature. Skeletal Radiol. 2007;36:779–83. doi: 10.1007/s00256-007-0285-7. [DOI] [PubMed] [Google Scholar]
- 52.Fisk C. Adaption of the technique for radiography of the bicipital groove. Radiol Technol. 1965;37:47–50. [PubMed] [Google Scholar]
- 53.Cone RO, Danzig L, Resnick D, Goldman AB. The bicipital groove: radiographic, anatomic, and pathologic study. AJR Am J Roentgenol. 1983;141:781–8. doi: 10.2214/ajr.141.4.781. [DOI] [PubMed] [Google Scholar]
- 54.Farin PU, Jaroma H, Harju A, Soimakallio S. Medial displacement of the biceps brachii tendon: evaluation with dynamic sonography during maximal external shoulder rotation. Radiology. 1995;195:845–8. doi: 10.1148/radiology.195.3.7754019. [DOI] [PubMed] [Google Scholar]
- 55.Armstrong A, Teefey SA, Wu T, et al. The efficacy of ultrasound in the diagnosis of long head of the biceps tendon pathology. J Shoulder Elbow Surg. 2006;15:7–11. doi: 10.1016/j.jse.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 56.Chan TW, Dalinka MK, Kneeland JB, Chervrot A. Biceps tendon dislocation: evaluation with MR imaging. Radiology. 1991;179:649–52. doi: 10.1148/radiology.179.3.2027968. [DOI] [PubMed] [Google Scholar]
- 57.Cervilla V, Schweitzer ME, Ho C, Motta A, Kerr R, Resnick D. Medial dislocation of the biceps brachii tendon: appearance at MR imaging. Radiology. 1991;180:523–6. doi: 10.1148/radiology.180.2.2068322. [DOI] [PubMed] [Google Scholar]
- 58.Becker DA, Cofield RH. Tenodesis of the long head of the biceps brachii for chronic bicipital tendinitis. Long-term results. J Bone Joint Surg Am. 1989;71:376–81. [PubMed] [Google Scholar]
- 59.Boileau P, Ahrens PM, Hatzidakis AM. Entrapment of the long head of the biceps tendon: the hourglass biceps--a cause of pain and locking of the shoulder. J Shoulder Elbow Surg. 2004;13:249–57. doi: 10.1016/j.jse.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 60.Skendzel JG, Jacobson JA, Carpenter JE, Miller BS. Long head of biceps brachii tendon evaluation: accuracy of preoperative ultrasound. AJR Am J Roentgenol. 2011;197:942–8. doi: 10.2214/AJR.10.5012. [DOI] [PubMed] [Google Scholar]
- 61.Joseph M, Maresh CM, McCarthy MB, et al. Histological and molecular analysis of the biceps tendon long head post-tenotomy. J Orthop Res. 2009;27:1379–85. doi: 10.1002/jor.20868. [DOI] [PubMed] [Google Scholar]
- 62.Nuelle CW, Stokes DC, Kuroki K, Crim JR, Sherman SL. Radiologic and Histologic Evaluation of Proximal Bicep Pathology in Patients With Chronic Biceps Tendinopathy Undergoing Open Subpectoral Biceps Tenodesis. Arthroscopy. 2018;34:1790–96. doi: 10.1016/j.arthro.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 63.Ahrens PM, Boileau P. The long head of biceps and associated tendinopathy. J Bone Joint Surg Br. 2007;89:1001–9. doi: 10.1302/0301-620X.89B8.19278. [DOI] [PubMed] [Google Scholar]
- 64.Zappia M, Capasso R, Berritto D, et al. Anterior cruciate ligament reconstruction: MR imaging findings. Musculoskelet Surg. 2017;101:23–35. doi: 10.1007/s12306-017-0460-5. [DOI] [PubMed] [Google Scholar]
- 65.Masciocchi C, Zugaro L, Arrigoni F, et al. Radiofrequency ablation versus magnetic resonance guided focused ultrasound surgery for minimally invasive treatment of osteoid osteoma: a propensity score matching study. Eur Radiol. 2016;26:2472–81. doi: 10.1007/s00330-015-4111-7. [DOI] [PubMed] [Google Scholar]
- 66.Barile A, Regis G, Masi R, et al. Musculoskeletal tumours: Preliminary experience with perfusion MRI. Radiol Med. 2007;112:550–61. doi: 10.1007/s11547-007-0161-5. [DOI] [PubMed] [Google Scholar]
- 67.Barile A, Arrigoni F, Zugaro L, et al. Minimally invasive treatments of painful bone lesions: state of the art. Med Oncol. 2017;34:53. doi: 10.1007/s12032-017-0909-2. [DOI] [PubMed] [Google Scholar]
- 68.Barile A, Arrigoni F, Bruno F, et al. Computed Tomography and MR Imaging in Rheumatoid Arthritis. Radiol Clin North Am. 2017;55:997–1007. doi: 10.1016/j.rcl.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 69.Perrotta FM, Astorri D, Zappia M, Reginelli A, Brunese L, Lubrano E. An ultrasonographic study of enthesis in early psoriatic arthritis patients naive to traditional and biologic DMARDs treatment. Rheumatol Int. 2016;36:1579–83. doi: 10.1007/s00296-016-3562-8. [DOI] [PubMed] [Google Scholar]
- 70.Barile A, La Marra A, Arrigoni F, et al. Anaesthetics, steroids and platelet-rich plasma (PRP) in ultrasound-guided musculoskeletal procedures. Br J Radiol. 2016;89:20150355. doi: 10.1259/bjr.20150355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cuomo G, Zappia M, Iudici M, Abignano G, Rotondo A, Valentini G. The origin of tendon friction rubs in patients with systemic sclerosis: a sonographic explanation. Arthritis Rheum. 2012;64:1291–3. doi: 10.1002/art.34319. [DOI] [PubMed] [Google Scholar]
- 72.Di Pietto F, Chianca V, De Ritis R, et al. Postoperative imaging in arthroscopic hip surgery. Musculoskelet Surg. 2017;101:43–49. doi: 10.1007/s12306-017-0459-y. [DOI] [PubMed] [Google Scholar]
- 73.Aliprandi A, Di Pietto F, Minafra P, Zappia M, Pozza S, Sconfienza LM. Femoro-acetabular impingement: What the general radiologist should know. Radiol Med. 2014;119:103–12. doi: 10.1007/s11547-013-0314-7. [DOI] [PubMed] [Google Scholar]
- 74.Sconfienza LM, Albano D, Allen G, et al. Clinical indications for musculoskeletal ultrasound updated in 2017 by European Society of Musculoskeletal Radiology (ESSR) consensus. Eur Radiol. 2018 doi: 10.1007/s00330-018-5474-3. [DOI] [PubMed] [Google Scholar]
- 75.Albano D, Chianca V, Tormenta S, Migliore A, Sconfienza LM. Old and new evidence concerning the crucial role of ultrasound in guiding intra-articular injections. Skeletal Radiol. 2017;46:963–64. doi: 10.1007/s00256-017-2644-3. [DOI] [PubMed] [Google Scholar]
- 76.Martinoli C, Bianchi S, Prato N, et al. US of the shoulder: non-rotator cuff disorders. Radiographics. 2003;23:381–401. doi: 10.1148/rg.232025100. quiz 534. [DOI] [PubMed] [Google Scholar]
- 77.Zanetti M, Weishaupt D, Gerber C, Hodler J. Tendinopathy and rupture of the tendon of the long head of the biceps brachii muscle: evaluation with MR arthrography. AJR Am J Roentgenol. 1998;170:1557–61. doi: 10.2214/ajr.170.6.9609174. [DOI] [PubMed] [Google Scholar]
- 78.Albano D, Chianca V, Zappia M, et al. Imaging of Usual and Unusual Complication of Rotator Cuff Repair. J Comput Assist Tomogr. 2019 doi: 10.1097/RCT.0000000000000846. [DOI] [PubMed] [Google Scholar]