Abstract
Background
Progressive resistance training (PRT) is consistently shown to improve muscle strength in older adults. The efficacy of PRT to improve muscle fatigue in older adults with demonstrated mobility limitations remains unclear.
Methods
Mobility-limited (Short Physical Performance Battery [SPPB] ≤ 9) older adults (age 70–92 years) were recruited for this study and randomized to either PRT or home-based flexibility (FLEX) 3 d/wk for 12 weeks. Muscle fatigue and strength outcomes were assessed at baseline and 12 weeks. The primary outcome was torque capacity, a composite measure of strength and fatigue, defined as the sum of peak torques from an isokinetic fatigue test.
Results
Seventy participants were randomized (mean [SD] age 78.9 [5.4] years; 60% female; mean [SD] SPPB 7.5 [1.6]). At follow-up, the PRT group improved significantly in torque capacity, mean between-group difference (95% confidence interval) 466.19 (138.4, 793.97) Nm (p = .006), and maximal strength 127.3 (60.96, 193.61) Nm (p = .0003), when compared with FLEX group. Neither group demonstrated significant changes in muscle fatigue or torque variability.
Conclusion
Twelve weeks of PRT improved torque capacity, as well as strength in mobility-limited older adults. These results demonstrate PRT improves multiple age-related muscular impairments.
Keywords: Exercise, Function, Power, Torque
Declines in maximal strength and power production with advancing age are widely recognized as important factors contributing to mobility disability, loss of independence, and death (1,2). More recently, muscle fatigue, or the inability to maintain a given level of force output, has been explored and is emerging as a key factor contributing to the functional decline in older adults (3). Compared with measures of maximal strength, fatigue-inducing assessments of muscle function more closely reflect the physical demands of prolonged functional tasks encountered in the everyday life of an older adult (3,4). Initial studies investigating the effect of aging on fatigue utilized isometric or low-velocity testing conditions and demonstrated a resistance to fatigue with age (5). Contemporary reports that have utilized faster movement speeds, replicating the angular velocities required to carry out functional tasks, report greater muscle fatigue with advancing age (6,7). Kent-Braun and colleagues have expanded on previous study by developing a standardized fatigue protocol that captures several age-related muscular impairments (3). Quantifying the muscle dysfunction occurring during fatigue may provide novel targets for therapeutic interventions in older adults.
For older adults to maintain independence, it is critical that their muscular system be able to meet the torque demands required for the completion of activities of daily living (8,9). Many older adults carry out basic functional tasks (eg, getting out of a chair) just above the minimum threshold of torque production required for successful task completion (9). This increases the level of effort required to complete basic functional tasks and can lead to adverse outcomes when faced with fatigue-inducing physical demands (9). Aging is also associated with an increased fluctuation in torque production during muscle contractions that has been shown to be detrimental to the completion of functional tasks (10). Although task-specific practice improves variability in torque production, whether progressive resistance training (PRT) can lead to reduced torque variability remains unknown. Several studies have demonstrated that PRT positively influences maximal levels of muscle strength attained at rest. However, very few clinical trials have investigated the efficacy of PRT’s influence on fatigue-induced muscular dysfunction in mobility-limited older adults (11,12). Our objective was to determine whether PRT is an effective treatment for fatigue-induced muscle dysfunction in a population at risk for mobility disability.
We compared the effects of 12 weeks of PRT to 12 weeks of home-based flexibility (FLEX) on changes in muscle torque capacity, a measure of strength and fatigue, in mobility-limited older adults. Secondary outcomes assessed the effects of the intervention on measures of muscle strength, torque variability, and fatigue index. Additional aims of this study were to establish the reliability of the fatigue protocol developed by Kent-Braun and colleagues and determine its sensitivity to detect PRT-induced changes in muscle fatigue and strength (3). We hypothesized that compared with FLEX, PRT would lead to greater improvements in muscle torque capacity.
Methods
Study Design
This study was a single-blind, parallel group, randomized controlled trial comparing the effects of 12 weeks of PRT program with 12 weeks of FLEX on knee extensor muscle torque capacity, fatigue, strength, and power in mobility-limited older adults.
Study Population
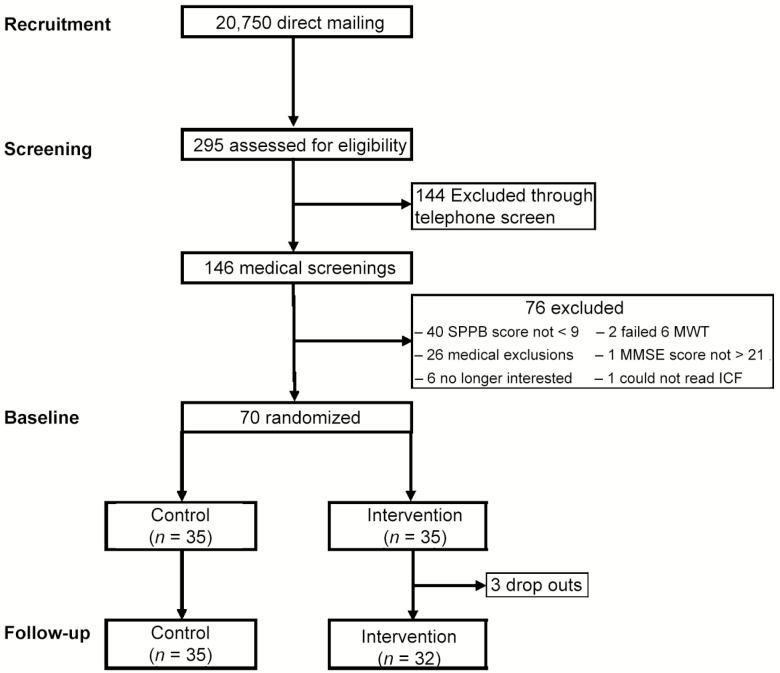
Participants were recruited from the Greater Boston area through a direct mailing campaign to 20,750 older adults (see Figure 1 for CONSORT diagram). Participants were initially prescreened by telephone and deemed eligible if they were community dwelling, 70 years and older, and sedentary (≤20 min/wk of moderate-intensity physical activity). If eligible, participants were invited to the research center for a medical screening visit. At screening visits, participants performed the Short Physical Performance Battery (SPPB) test for assessment of mobility status. Participants with an SPPB score of less than or equal to 9 (mobility limited) completed a medical history questionnaire, a resting electrocardiogram, standard blood chemistry and urinalysis, and underwent a physical examination. Participants were excluded if they were not able to complete greater than 200 m during the 6-minute walk test without an assistive device (single straight cane was acceptable) or the help of another person, had a body mass index less than 18.5 kg/m2 or greater than 35.0 kg/m2, acute or terminal illness, cognitive impairment (Mini-Mental State Examination score < 23), or reported myocardial infarction or upper/lower extremity fracture in the previous 6 months, symptomatic coronary artery disease, congestive heart failure, uncontrolled hypertension (>150/90 mm Hg), neuromuscular disease, using any medications, non-medical compounds, or dietary aids/food supplements to improve physical function or muscle mass, or any other condition, which in the opinion of the investigator, precluded the participant’s successful participation in the trial. Participants who met the study entry criteria and were given medical clearance by the study physician were deemed eligible. Signed informed consent was obtained from all study participants. The study was approved by the Tufts University Health Sciences Institutional Review Board.
Figure 1.
CONOSRT diagram of study recruitment, enrollment, and randomization. SPPB = Short Physical Performance Battery; 6MWT = 6-min walk test.
PRT Intervention
Blood pressure and heart rate were recorded before each training session, followed by 5 minutes of treadmill walking. All participants trained in small groups (three to four participants) three times per week for 12 weeks. Participants performed leg press, seated row, leg extension, chest press, and leg curl. Participants initially performed two sets of 10 repetitions progressing to three sets of 12 repetitions throughout the 12-week intervention period. Each set was followed by a 2- to 3-minute rest period. Participants performed the training exercises progressing to 80% of their 1 repetition maximum (RM). The 1 RM was assessed at baseline and re-evaluated monthly. All training was performed on Cybex VR2 machines (Cybex International, Medway, MA).
Home-Based Flexibility
Participants performed four different stretching exercises three times per week for 12 weeks at home. Each stretch was performed once for 30 seconds and targeted either the hamstrings, quadriceps, chest, or upper back. Participants were instructed on the exercises once they were randomized. Participants were contacted via telephone every 4 weeks to check-in and collect adherence, any adverse events (AEs), changes in medications, or issues with the flexibility program. We utilized home-based flexibility as our control group in an effort to increase the retention of these participants and minimize loss to follow-up. Larger scale clinical trials that have utilized a comparable strategy, with the addition of on-site monitoring, have similarly shown modest improvements in certain outcome measures (13).
Study Assessments
All outcome measures were conducted by a blinded assessor at the initial baseline visit and repeated at 12 weeks. Measures derived from the fatigue test were also collected at a second baseline visit that occurred between 3 and 7 days following the initial baseline visit.
Fatigue Test
The fatigue test was performed with the nondominant leg using the Biodex System 3 Isokinetic Dynamometer (BiodexMedical Systems, Shirley, NY). Participants were seated with restraining straps over the pelvis and trunk in accordance with the manufacturer’s guidelines. The input axis of the dynamometer was aligned with the axis of the knee. Fatigue measures were collected as previously described (3). Briefly, participants were instructed to perform 120 maximal effort knee extensions traveling through a range of motion of 75° (90°–15°). Participants were asked to complete a contraction every 2 s, with the whole test lasting 4 minutes. Knee extension velocity was set to 120°/s, and knee flexion was passive (240°/s). Participants were provided strong verbal encouragement throughout the test and provided with a verbal cue to “kick” every 2 seconds to ensure a 4-minute testing period. No real-time force feedback was provided during the test. Peak torque values were determined at a velocity of 120°/s. As the reliability of isokinetic testing is known to increase when an average of more than one measure is utilized, an average of baseline visit 1 and baseline visit 2 measures was used in all analyses (14). Where applicable, fatigue measures were expressed as measure relative to the percent peak of peak torque achieved at rest (pretest peak torque) to control for the influence of increased maximal torque production at rest on measures of fatigue and recovery.
Torque Capacity (Summed Torque)
The summed torque was calculated by summing the peak torque generated during each of the 120 repetitions performed during the fatigue test.
Torque at Fatigue
The ability to generate torque at fatigue was also measured and quantified as the mean peak torque of the last five repetitions (116–120).
Fatigue Index
A fatigue index was quantified as previously described (3):
This index provides the percent force generated at the end of the test relative to the beginning of the test.
Torque Variability
For each participant, torque variability throughout the fatigue test was assessed pre- and post-intervention. Using peak torque values over a single testing session, linear regression using log summed torque was used to generate a curve for the prediction of torque generation throughout the 120 repetitions. Residuals were then calculated by subtracting actual from predicted torque. The absolute values of these residuals were summed. Residual sums were adjusted to sum torque (normalized residual) for each participant. The difference between pre- and post-normalized residuals (normalized residual difference) was used to assess for a torque variability treatment effect. In this manner, a positive residual difference is evidence of increased torque variability, whereas a negative residual difference suggests the opposite. As muscle fatigue was a primary focus of this study, in addition to investigating torque variability over the duration of the test, we also compared pre- versus post-torque variability during the early (contractions 1–40), middle (41–80), and late (81–120) phases of the trial to assess the hypothesis that torque variability increases as a function of fatigue.
Recovery From Fatigue
To quantify recovery from the fatigue test, three maximal effort repetitions at 120°/s were performed at 2, 5, and 10 minutes after completion of the fatigue test to attain a peak torque value at each time interval. Post-fatigue torque values (2, 5, and 10 minutes) were then compared with pre-fatigue peak torque to calculate recovery from the fatigue test.
Isokinetic and Isometric Testing
Isokinetic and isometric peak torque were determined for the knee flexors and extensors of the nondominant leg using the Biodex System 3 Isokinetic Dynamometer. Participants were positioned as described earlier. Isokinetic knee extension and flexion peak torque were measured at 60°/s. This velocity was selected because of its proven reliability and association with physical performance in this population (14). Isokinetic knee extension was also measured at 120°/s with a passive flexion phase (240°/s) to simulate the conditions of the fatigue test. This measure was recorded as pre-fatigue test peak torque. The peak torque value recorded during the fatigue test was also captured and recorded as fatigue test peak torque. Two- to three-minute rest periods were given between each strength test.
Muscle Strength and Power
Leg press strength and power were evaluated using a pneumatic bilateral seated leg press (K400, Keiser Sports Health Equipment, Fresno, CA). Assessment of muscle strength and peak power has been previously described and validated (15). Briefly, strength was assessed by 1 RM measurement of leg press. After 1 RM testing, leg press peak muscle power was assessed. Each participant was instructed to complete five repetitions as quickly as possible through their full range of motion at 40% and 70% of 1 RM; each separated by 30 seconds of rest.
Statistical Analysis
Linear regression, adjusted for gender (stratification variable), was used to assess the between-group treatment effect (change from baseline to follow-up). The intraclass correlation coefficient was used to describe the reliability of the summed peak torque fatigue measure collected at baseline visits 1 and 2. Between-group changes in torque variability were compared using Wilcoxon rank sum p values. SAS 9.4 was used for all analyses. Hypothesis testing was conducted at the two-sided level of p less than .05.
Results
Baseline Characteristics
Baseline characteristics were similar between groups and are presented in Table 1.
Table 1.
Participant Characteristics at Baseline
| PRT (n = 35) | FLEX (n = 35) | |
|---|---|---|
| Age, y | 77.4 (4.4) | 80.3 (6.3) |
| Male (n, %) | 14 (40) | 14 (40) |
| Height, m | 1.7 (0.1) | 1.7 (0.1) |
| Body mass, kg | 78.0 (13.1) | 77.1 (14.9) |
| Body mass index, kg/m2 | 28.6 (4.0) | 27.7 (3.9) |
| MMSE score | 27.6 (2.0) | 28.1 (1.7) |
| Number of medical diagnoses | 3.9 (2.1) | 3.1 (2.7) |
| SPPB | 7.6 (1.4) | 7.3 (1.7) |
Note: FLEX = home-based flexibility; MMSE = Mini-Mental State Exam; PRT = progressive resistance training; SPPB = Short physical performance battery. Results are means ± SD, unless otherwise stated.
Intervention Adherence and Safety
The mean session attendance for PRT was 83%, and completion of stretching exercises in FLEX was 96%. A total of 12 AEs were reported in the PRT group. Four AEs were deemed possibly related to the intervention. Three participants in PRT dropped out post-randomization. One participant lost interest, and two participants could not continue for medical reasons (unrelated to the intervention). A total of 10 AEs were reported in the FLEX group with one deemed being possibly related to the intervention. No serious AEs were reported in either group. There were no AEs directly related to the fatigue testing session. The four AEs that were deemed possibly related to the intervention were related to PRT, not the testing itself.
Fatigue Test Reliability and Tolerability
The reliability of the summed torque measure was found to be excellent (intraclass correlation coefficient = .92). The reliability of the fatigue index was found to be fair (intraclass correlation coefficient = .44). The test was also well tolerated, as 96% of participants were able to successfully complete the test at baseline.
Fatigue Measures
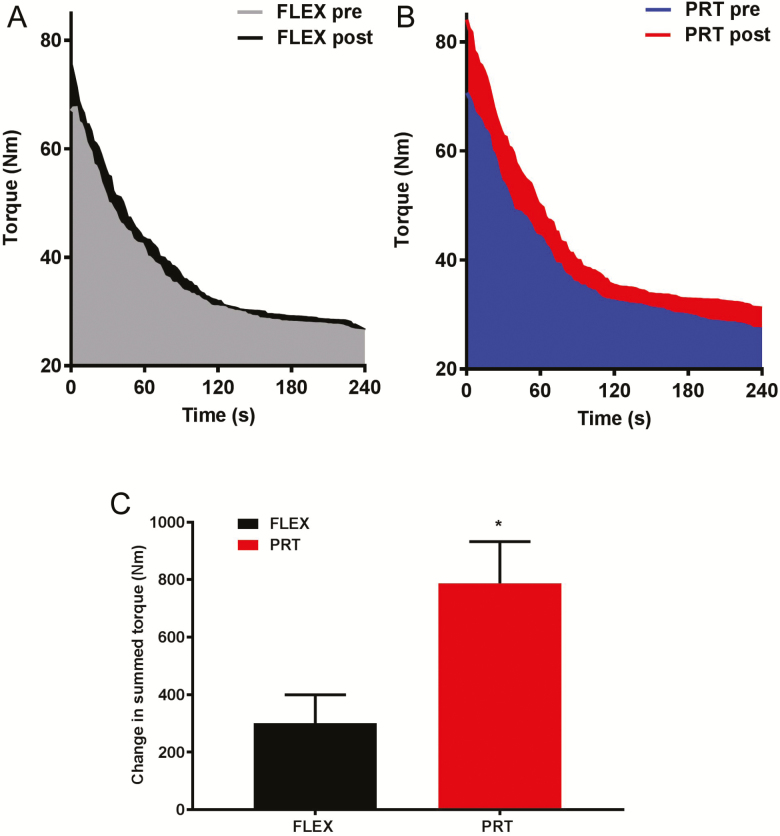
Table 2 shows baseline and changes from baseline in measures of fatigue. At 12 weeks, participants in the PRT group experienced an improvement in summed torque when compared with FLEX (Figure 1), mean between-group difference (95% confidence interval [CI]) 466.19 (138.4, 793.97) Nm (p = .006). Pretest peak torque and fatigue test peak torque improved significantly more in the PRT group compared with the FLEX group, mean between-group difference (95% CI) 7.54 (1.46, 13.63) Nm (p = .02) and 7.3 (0.4, 14.19) Nm (p = .04). Participants in the PRT group experienced greater improvements in torque at 2 and 5 minutes post-fatigue after the intervention period when compared with the FLEX group, mean between-group difference (95% CI) 4.83 (0.21,9.44) Nm (p = .04) and 7.04 (1.85,12.23) Nm (p = .009). Fatigue index was not influenced in either group. Absolute percent changes and relative percent changes for fatigue measures are presented in Figure 2.
Table 2.
Baseline Values and Absolute Mean Changes in Fatigue Test Measures
| PRT | FLEX | Between Group | p Value | |||
|---|---|---|---|---|---|---|
| Baseline | Δ | Baseline | Δ | Δ | ||
| Pretest peak torque, Nm | 68.9 ± 24.2 | 13.1 ± 14.7 | 70.1 ± 32.3 | 5.6 ± 11.6 | 7.54 (1.46, 13.63) | .02 |
| Fatigue test peak torque, Nm | 71.0 ± 25.8 | 14.6 ± 18 | 69.9 ± 30.8 | 6.9 ± 12.9 | 7.3 (0.4, 14.19) | .04 |
| Torque at fatigue, Nm | 28.3 ± 10.2 | 3.6 ± 6 | 26.5 ± 9 | 1.2 ± 4.2 | 2.25 (−0.11, 4.61) | .06 |
| 2-minute post-peak torque, Nm | 61.2 ± 21.4 | 8.8 ± 11.3 | 60.6 ± 27.2 | 3.8 ± 9.5 | 4.83 (0.21, 9.44) | .04 |
| 5-minute post-peak torque, Nm | 66.7 ± 23.3 | 12.3 ± 13.2 | 64.9 ± 27.2 | 5 ± 10.4 | 7.04 (1.85, 12.23) | .009 |
| 10-minute post-peak torque, Nm | 71.2 ± 25.6 | 12.6 ± 13.5 | 67.8 ± 29.4 | 7.6 ± 11.3 | 4.69 (−0.87, 10.25) | .10 |
| Fatigue index | 0.4 ± 0.1 | 0 ± 0.1 | 0.4 ± 0.1 | 0 ± 0.1 | −0.02 (−0.06, 0.03) | .50 |
| Summed torque, Nm | 4,440.7 ± 1,521.3 | 787.7 ± 856.2 | 4,228.0 ± 1,537.7 | 301.2 ± 581.1 | 466.19 (138.4, 793.97) | .006 |
Note: FLEX = home-based flexibility; PRT = progressive resistance training. Average of baseline visit 1 and baseline visit 2 measures was used in all analyses. All measures in this table were determined at 120°/s. Between-group change and the p value were calculated with a linear regression model adjusting for gender. Baseline and within-group Δ (change) values are mean ± SD. Between-group Δ values are mean change estimated from the model (with 95% confidence interval).
Figure 2.
Progressive resistance training (PRT) and home-based flexibility (FLEX) groups. Peak torque for all contractions performed during the fatigue test before and after the intervention period in FLEX (A) and PRT (B) groups. Absolute change (± SE) in summed torque in the PRT and FLEX groups (C). *Significant change between groups: p = .006.
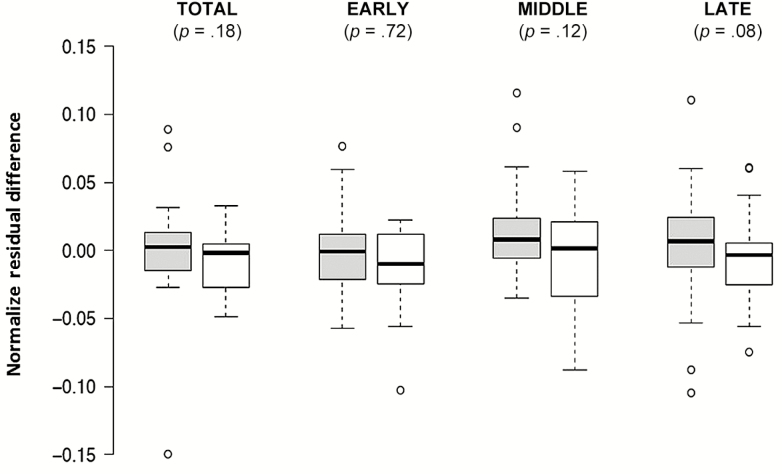
Torque Variability
Changes in torque variability between groups did not reach statistical significance (Figures 3 and 4).
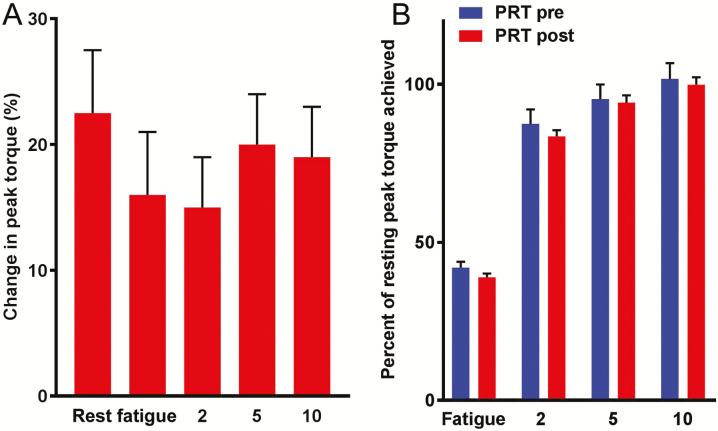
Figure 3.
Progressive resistance training (PRT) group only. (A) Percent change (± SE) in peak torque at rest (average of pre-fatigue and fatigue test peak torque), at fatigue (average of repetitions 116–120), and at 2, 5, and 10 min after the fatigue test in the PRT group. (B) Percentage of peak torque at rest achieved (± SE) during fatigue and at 2, 5, and 10 min post the fatigue test before and after the intervention.
Figure 4.
Box plots of change in torque variability after 12 wk of home-based flexibility (FLEX; gray) or progressive resistance training (PRT; white). Positive and negative values indicate an increase or decrease, respectively. Plots generated using BoxPlotR (PMID: 24481215).
Maximal Muscle Strength, Power, and Torque
Table 3 shows baseline and changes from baseline in measures of maximal muscle strength, power, and torque. Participants in the PRT group experienced greater improvements in 1 RM in the leg press than those in the FLEX group, mean between-group difference (95% CI) 127.28 (60.96, 193.61) N (p = .0003). There were no significant differences at follow-up in measures of muscle power at 40% or 70% of 1 RM, mean between-group difference (95% CI) 23.04 (−19.63, 65.71) W (p = .28) and 17.53 (−20.91, 55.97) W (p = .37). Participants in the PRT group experienced greater improvements in isokinetic (120°/s) knee extension peak torque than those in the FLEX group, mean between-group difference (95% CI) 7.54 (1.46, 13.63) Nm (p = .02). There was not a significant difference between changes in flexion, mean between-group difference (95% CI) 3.36 (−3.21, 9.93) Nm (p = .31).
Table 3.
Baseline Values and Absolute Changes in Maximal Strength, Power, and Torque
| PRT | FLEX | Between Group | p Value | |||
|---|---|---|---|---|---|---|
| Baseline | Δ | Baseline | Δ | Δ | ||
| Knee extension peak torque, Nm (60°/s) | 88.3 ± 33.1 | 19.1 ± 18.2 | 85.6 ± 40.2 | 9.4 ± 18.2 | 9.8 (1.14, 18.36) | .03 |
| Knee flexion peak torque, Nm (60°/s) | 39 ± 17.9 | 4.2 ± 10.5 | 38.6 ± 22.07 | 0.9 ± 15.5 | 3.4 (−3.21, 9.93) | .31 |
| 1-RM leg extension, N | 890.5 ± 251.9 | 161.1 ± 166.8 | 854.8 ± 319.48 | 29.3 ± 102 | 127.3 (60.96, 193.61) | .0003 |
| Leg extension peak power, W (40%) | 206.06 ± 94.09 | 61.76 ± 107.25 | 228.32 ± 115.97 | 34.97 ± 72.08 | 23.04 (−19.63, 65.71) | .28 |
| Leg extension peak power, W (70%) | 226.13 ± 102.94 | 34.91 ± 96.03 | 236.30 ± 115.41 | 15.7 ± 54.86 | 17.53 (−20.91, 55.97) | .37 |
Note: FLEX = home-based flexibility; PRT = progressive resistance training. Between-group change and the p value are from a linear regression model adjusting for gender. Baseline and within-group Δ (change) values are mean ± SD. Between-group Δ values are mean change estimated from the model (with 95% confidence interval).
Discussion
The main finding from this study was that 12 weeks of PRT lead to robust improvements in the total amount of torque produced (torque capacity) over the duration of the fatigue test (summed torque) and during recovery. Furthermore, this study demonstrates that the fatigue test developed by Kent-Braun and colleagues is a reliable, sensitive, and well-tolerated measure of torque capacity and fatigue in mobility-limited older adults, establishing this test as a viable outcome measure in clinical trials, which aim to have therapeutic effects in older adults at risk for mobility disability.
Interestingly, we found that the absolute decline of torque over the course of the fatigue test (~60%) was not influenced by 12 weeks of PRT and that although torque production at 2 and 5 minutes of recovery was increased, when these values are normalized to torque values attained at rest, it appears the rate of recovery was not influenced. These findings indicate that the magnitude of, and ability to recover from, fatigue were not significantly influenced by PRT. This highlights the importance of discriminating between absolute and relative improvements in muscle fatigue and provides a basis for the interpretation of our results and their implications for meaningful real-world outcomes. For instance, improved (absolute) torque-generating capacity over a sustained period of time increases the total amount of fatigue that can be tolerated by the muscular system before decrements in torque production ultimately lead to task failure (8,9). This may provide older adults with a functional reserve in torque production critical for the successful completion of daily tasks that induce muscle fatigue (eg, ascending/descending a flight of steps, getting across the street safely). Furthermore, improved (absolute) torque production during recovery from fatigue may reduce the time needed to resume and complete certain functional tasks. Increased maximal torque production coupled with an unaltered rate of torque decline and recovery appears to be driving the improved performance of the fatigue test.
The inability to generate force consistently has been shown to play a role in diminishing functional performance (10). If PRT improves age-related inconsistencies in force, production was previously unexplored. As such, an exploratory aim of this study was to assess the ability of 12-wk PRT to attenuate age-related increases in torque variability. Although torque variability in the PRT group appears to be reduced over the course of the test, these improvements did not reach statistical significance. It is interesting to note, however, that changes in torque variability between PRT and FLEX were most apparent during the late phase of the test (p = .08). This adaptation may be attributed to a delay in fatigue-induced muscle dysfunction that enables a more consistent level of torque production. Future investigations are encouraged to examine the impact of a more endurance-specific PRT protocol (eg, 3 × 30) on torque variability and other fatigue-related measures.
In the present study, we observed ~20% increase in maximal muscle strength, consistent with others who have investigated the effects of PRT in similar cohorts (16,17). We also observed substantial improvements in measures of isokinetic torque (newton meter) at 60°/s and 120°/s. Similar to others who have assessed muscle power (watt) after 12 weeks of PRT in mobility-limited older adults, we did not observe a statistically significant improvement (18,19). However, a recent report suggests that PRT induced a clinically meaningful improvement in leg extension power (20). The contrasting results between measures obtained with the Biodex and Kieser may be due to the movement velocity constraints inherent to isokinetic (constant angular velocity) testing that are not present during unconstrained testing. Likely, a higher velocity (power) training stimulus would have augmented improvements in muscle power (18,21). Alternatively, aging has been shown to be associated with reduced skeletal muscle adaptability in response to PRT, and this could have led to a blunting of certain training effects (22). It would be interesting to explore whether an identical PRT program would yield more robust skeletal muscle benefits (fatigue, recovery, power) in a higher-functioning/more active cohort of older adults. Future investigations are encouraged to explore alternative PRT techniques that may yield improved musculoskeletal outcomes in mobility-limited older adults.
In conclusion, this trial supports the use of PRT to improve torque-generating capacity and strength in mobility-limited older adults. Evidence from this trial promotes the use of the fatigue test as a standardized outcome to assess muscle performance and impairments in response to various interventional strategies.
Funding
This study was supported in part by Astellas Pharma. In addition, this study was also supported by the U.S. Department of Agriculture (USDA), under Agreement No. 58-1950-4-003, and the Boston Claude D. Pepper Center Older American Independence Centers (1P30AG031679). Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the authors and do not necessarily reflect the view of the USDA. The project described was also supported by the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), Award No. UL1TR001064. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Conflict of Interest
R.A.F is a paid consultant to Astellas Pharma and received grant support from Astellas Pharma to support this project. The funders had no role in the conduct of the study R.A.F is an Associate Editor of the Journals of Gerontology: Series A, Medical Sciences.
Acknowledgments
R.A.F. designed the research; R.A.F. and D.A.E. conducted the research; L.L.P. analyzed data and performed statistical analysis; D.A.E. wrote the paper; D.A.E., R.A.F., and G.J.G. had primary responsibility for final content; C.L. oversaw medical aspects of the trial; M.I. and M.K. collaborated on the design of the trial and the interpretation of results. All authors read and approved the final mansucript.
ClinicalTrials.gov Identifier: NCT03083275
References
- 1. Newman AB, Kupelian V, Visser M, et al. Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci. 2006;61:72–77. [DOI] [PubMed] [Google Scholar]
- 2. Foldvari M, Clark M, Laviolette LC, et al. Association of muscle power with functional status in community-dwelling elderly women. J Gerontol A Biol Sci Med Sci. 2000;55:M192–M199. [DOI] [PubMed] [Google Scholar]
- 3. Kent-Braun JA, Callahan DM, Fay JL, Foulis SA, Buonaccorsi JP. Muscle weakness, fatigue, and torque variability: effects of age and mobility status. Muscle Nerve. 2014;49:209–217. doi: 10.1002/mus.23903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reginster JY, Cooper C, Rizzoli R, et al. Recommendations for the conduct of clinical trials for drugs to treat or prevent sarcopenia. Aging Clin Exp Res. 2016;28:47–58. doi: 10.1007/s40520-015-0517-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Christie A, Snook EM, Kent-Braun JA. Systematic review and meta-analysis of skeletal muscle fatigue in old age. Med Sci Sports Exerc. 2011;43:568–577. doi: 10.1249/MSS.0b013e3181f9b1c4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dalton BH, Power GA, Vandervoort AA, Rice CL. The age-related slowing of voluntary shortening velocity exacerbates power loss during repeated fast knee extensions. Exp Gerontol. 2012;47:85–92. doi: 10.1016/j.exger.2011.10.010 [DOI] [PubMed] [Google Scholar]
- 7. Jevsevar DS, Riley PO, Hodge WA, Krebs DE. Knee kinematics and kinetics during locomotor activities of daily living in subjects with knee arthroplasty and in healthy control subjects. Phys Ther. 1993;73:229–239; discussion 240. [DOI] [PubMed] [Google Scholar]
- 8. Ploutz-Snyder LL, Manini T, Ploutz-Snyder RJ, Wolf DA. Functionally relevant thresholds of quadriceps femoris strength. J Gerontol A Biol Sci Med Sci. 2002;57:B144–B152. [DOI] [PubMed] [Google Scholar]
- 9. Hortobágyi T, Mizelle C, Beam S, DeVita P. Old adults perform activities of daily living near their maximal capabilities. J Gerontol A Biol Sci Med Sci. 2003;58:M453–M460. [DOI] [PubMed] [Google Scholar]
- 10. Kornatz KW, Christou EA, Enoka RM. Practice reduces motor unit discharge variability in a hand muscle and improves manual dexterity in old adults. J Appl Physiol (1985). 2005;98:2072–2080. doi: 10.1152/japplphysiol.01149.2004 [DOI] [PubMed] [Google Scholar]
- 11. Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009:Cd002759. doi: 10.1002/14651858.CD002759.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev. 2012;40:4–12. doi: 10.1097/JES.0b013e31823b5f13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Santanasto AJ, Glynn NW, Lovato LC, et al. ; LIFE Study Group Effect of physical activity versus health education on physical function, grip strength and mobility. J Am Geriatr Soc. 2017;65:1427–1433. doi: 10.1111/jgs.14804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Frontera WR, Hughes VA, Dallal GE, Evans WJ. Reliability of isokinetic muscle strength testing in 45- to 78-year-old men and women. Arch Phys Med Rehabil. 1993;74:1181–1185. [PubMed] [Google Scholar]
- 15. Callahan D, Phillips E, Carabello R, Frontera WR, Fielding RA. Assessment of lower extremity muscle power in functionally-limited elders. Aging Clin Exp Res. 2007;19:194–199. [DOI] [PubMed] [Google Scholar]
- 16. Leenders M, Verdijk LB, van der Hoeven L, van Kranenburg J, Nilwik R, van Loon LJ. Elderly men and women benefit equally from prolonged resistance-type exercise training. J Gerontol A Biol Sci Med Sci. 2013;68:769–779. doi: 10.1093/gerona/gls241 [DOI] [PubMed] [Google Scholar]
- 17. Churchward-Venne TA, Tieland M, Verdijk LB, et al. There are no nonresponders to resistance-type exercise training in older men and women. J Am Med Dir Assoc. 2015;16:400–411. doi: 10.1016/j.jamda.2015.01.071 [DOI] [PubMed] [Google Scholar]
- 18. Fielding RA, LeBrasseur NK, Cuoco A, Bean J, Mizer K, Fiatarone Singh MA. High-velocity resistance training increases skeletal muscle peak power in older women. J Am Geriatr Soc. 2002;50:655–662. doi: 10.1046/j.1532-5415.2002.50159.x [DOI] [PubMed] [Google Scholar]
- 19. Reid KF, Callahan DM, Carabello RJ, Phillips EM, Frontera WR, Fielding RA. Lower extremity power training in elderly subjects with mobility limitations: a randomized controlled trial. Aging Clin Exp Res. 2008;20:337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kirn DR, Reid KF, Hau C, Phillips EM, Fielding RA. What is a clinically meaningful improvement in leg-extensor power for mobility-limited older adults?J Gerontol A Biol Sci Med Sci. 2016;71:632–636. doi: 10.1093/gerona/glv207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Englund DA, Sharp RL, Selsby JT, Ganesan SS, Franke WD. Resistance training performed at distinct angular velocities elicits velocity-specific alterations in muscle strength and mobility status in older adults. Exp Gerontol. 2017;91:51–56. doi: 10.1016/j.exger.2017.02.072 [DOI] [PubMed] [Google Scholar]
- 22. Rivas DA, Lessard SJ, Rice NP, et al. Diminished skeletal muscle microRNA expression with aging is associated with attenuated muscle plasticity and inhibition of IGF-1 signaling. FASEB J. 2014;28:4133–4147. doi: 10.1096/fj.14-254490 [DOI] [PMC free article] [PubMed] [Google Scholar]