Abstract
Peritonitis is a common and severe complication in peritoneal dialysis (PD). Detailed recommendations on the prevention and treatment of PD-associated peritonitis have been published by the International Society for Peritoneal Dialysis (ISPD), but there is a substantial variation in clinical practice among dialysis units. Prophylactic antibiotics administered before PD catheter insertion, colonoscopy, or invasive gynecologic procedures, daily topical application of antibiotic cream or ointment to the catheter exit site, and prompt treatment of exit site or catheter infection are key measures to prevent PD-associated peritonitis. When a patient on PD presents with clinical features compatible with PD-associated peritonitis, empirical antibiotic therapy, with coverage of both Gram-positive and Gram-negative organisms (including Pseudomonas species), should be started once the appropriate microbiologic specimens have been obtained. Intraperitoneal is the preferred route of administration. Antifungal prophylaxis, preferably oral nystatin, should be added to prevent secondary fungal peritonitis. Once the PD effluent Gram stain or culture and sensitivity results are available, antibiotic therapy can be adjusted accordingly. A detailed description on the dosage of individual antibiotic can be found in the latest recommendations by the ISPD. The duration of antibiotics is usually 2–3 weeks, depending on the specific organisms identified. Catheter removal and temporary hemodialysis support is recommended for refractory, relapsing, or fungal peritonitis. In some patients, a new PD catheter could be inserted after complete resolution of the peritonitis. PD catheter removal should also be considered for refractory exit site or tunnel infections. After the improvement in clinical practice, there is a worldwide trend of reduction in PD-associated peritonitis rate, supporting the use of PD as a first-line dialysis modality.
Keywords: end-stage renal disease, dialysis, Infection, Antibiotic, microbiology, peritoneal dialysis, Peritonitis
Introduction
Peritonitis is a common and serious complication of peritoneal dialysis (PD). PD-associated peritonitis is the direct or major contributing cause of death in >15% of patients on PD (1,2). Moreover, a single episode of severe peritonitis or multiple peritonitis episodes frequently leads to diminished peritoneal ultrafiltration capacity and is the most common cause of conversion to long-term hemodialysis (3).
Over the past 30 years, recommendations on the treatment and prevention of PD-associated peritonitis were published and revised regularly under the auspices of the International Society for Peritoneal Dialysis (ISPD). In the 2010 version, two sets of recommendations were issued: one on the treatment of PD-associated peritonitis and catheter-related infections (4), and another on their prevention (5). In the latest 2016 version, however, both the treatment and prevention of PD-associated peritonitis were combined into one set of recommendations (6), and a separate set of recommendations on catheter-related infections was published in 2017 (7). Because their focuses are different, their specific recommendations are not entirely identical. In this review, we focus on the prevention and treatment of PD-associated peritonitis.
Reporting of Peritonitis Rate
The ISPD recommendations emphasize that every PD program should monitor the PD-associated peritonitis rate at least on a yearly basis (6). The rate should be reported as the number of episode per patient-year but not the number of patient-months per episode (6). In addition to the overall peritonitis rate, the peritonitis rates of specific organisms, percentage of peritonitis-free patients per year, and the spectrum of antibiotic resistance should be monitored (6). During the calculation of peritonitis rate, relapsing episodes should be counted only once, and all episodes that develop after PD training has commenced (not completed) should be counted (6). Although the recommendations state that the overall peritonitis rate should be below 0.5 episodes per patient-year, there is a wide variation in the peritonitis rates reported by different countries, as well as by different centers within the same country (8). A recent study shows highly variable rates of adopting the ISPD recommendations across different centers, and such variations probably account for the difference in infection risk between PD centers (9).
Prevention of PD-Associated Peritonitis
PD Equipment and Training.
At least four randomized, controlled trials support the use of prophylactic antibiotics before PD catheter insertion (6,10). Intravenous vancomycin, cefazolin, gentamicin, and cefuroxime have been tested (10). The optimal choice of antibiotic, however, is not well defined, and should be determined by the local spectrum of antibiotic resistance. Besides prophylactic antibiotics, other aspects of catheter insertion practice, including the method of catheter placement (mini-laparotomy, laparoscopy, or peritoneoscopy), site of skin incision (midline or lateral), catheter design (e.g., extended, presternal, or upper abdominal catheter), configuration (straight or swan-neck, single or double cuff), and the direction of exit site do not significantly affect the peritonitis rate (11,12). Nonetheless, a large, observational study suggests that the double-cuff catheter is associated with a reduction in peritonitis caused by Staphylococcus aureus (13).
Disconnect PD systems with a “flush before fill” design are consistently associated with a lower peritonitis rate than the traditional spike systems, and are the standard of continuous ambulatory peritoneal dialysis (CAPD) practice nowadays (11,14). There is no significant difference in peritonitis rate between various disconnect systems (Y-set, double-bag, or luer lock) (11,14), or between CAPD and machine-assisted automated PD (15,16). It is uncertain whether the choice of dialysis solution (conventional glucose-based solutions or biocompatible solutions with neutral pH and low glucose-degradation product) leads to any differences in peritonitis occurrence (17).
Training and Nursing Practice.
A good PD training program would logically minimize the peritonitis rate. It is generally accepted that PD training should be conducted by nursing staff with the appropriate qualifications and experience, and the latest ISPD recommendations for teaching PD patients and their caregivers should be followed (18,19). However, published data are limited, and the critical elements of a training program that determine the peritonitis rate remain undefined. The ongoing Targeted Education Approach to Improve Peritoneal Dialysis Outcomes Trial, to be completed in 2023 (20), will help to clarify the benefit of comprehensive PD training programs.
After PD training is completed, a home visit by PD nurse is valuable in detecting unforeseen practical problems with home dialysis (6). However, the benefit of home visit on peritonitis risk has not been formally tested. In addition to the initial training, retraining should be considered after peritonitis or catheter infection episodes; any change in dexterity, vision, or mental acuity; change in supplier or connection system; prolonged hospitalization; or interruption of PD because of other reasons (6). Early studies suggest that a continuous quality improvement (CQI) program in the PD center may help to reduce peritonitis rates (6,21). Nationwide CQI programs have been found to sustainably reduce peritonitis rates (22). A detailed description on the organization of CQI programs is beyond the scope of this review. Nonetheless, a multidisciplinary team that runs CQI programs should meet and review performance metrics regularly (6).
Exit Site and Catheter Infections.
Exit site and catheter tunnel infections are an important risk factor of PD-associated peritonitis (23). Their early detection and prompt antibiotic treatment are logical steps to minimize the risk of subsequent peritonitis (6). The proper care of catheter exit site plays a pivotal role in prevention. Daily topical application of antibiotic cream or ointment to the catheter exit site is recommended (6), and mupirocin cream or ointment should be the agent of choice (24). Daily application of mupirocin cream or ointment to the skin around the exit site reduces the rate of S. aureus exit site infection and probably decreases the rate of peritonitis (24,25). Intranasal mupirocin is effective for reducing S. aureus exit site infection, but not peritonitis (26). Excessive amounts of topical mupirocin directly applied onto the polyurethane or silicone catheter surface can cause catheter erosion (27). Patients must be educated about the proper method of application.
Topical gentamicin is a reasonable alternative to mupirocin for exit site care (28), but the evidence seems less robust. Gentamicin offers an advantage over mupirocin in centers with a high rate of exit site infection by Gram-negative organisms, but the possibility of gentamicin resistance, which affects the choice of antibiotic for peritonitis treatment, is a definite concern. Other alternative strategies, such as topical antibacterial honey (29) or triple ointment (polymyxin, bacitracin, and neomycin) (30), have been tested, but none is shown to be superior than topical mupirocin. In general, regular systemic antibiotic prophylaxis is not advisable. Although intermittent oral rifampicin reduces the rate of S. aureus peritonitis (31), rifampicin resistance, adverse effects, and drug interactions are all serious concerns.
Other Modifiable Risk Factors.
Many other modifiable risk factors for PD peritonitis have been reported (8), but their absolute risk (e.g., cirrhosis, polycystic kidney disease, left ventricular assist device, neutropenia during chemotherapy) are not well defined, and interventions to only very few have been proved to reduce peritonitis risk. Peritonitis often follows invasive endoscopic procedures (e.g., colonoscopy, hysteroscopy) in patients on PD (32). Prophylactic systematic antibiotic before colonoscopy or invasive gynecologic procedures should be considered (6). Although the optimal antibiotic regimen is unknown, intravenous ampicillin with or without aminoglycoside or metronidazole is most commonly used (10). The efficacy of prophylactic antibiotic given intraperitoneally before other invasive procedures is not proved. Prophylactic antibiotics should also be considered after wet contamination or other breaches in technique (5), but there is no widely accepted regimen (6). Although it is a common practice to change the extension tubings after touch contamination, published evidence is limited. Constipation, enteritis, and hypokalemia are associated with an increased risk of peritonitis by enteric organisms (6,8), and these conditions deserve treatment on their own right.
Secondary Prevention.
Most fungal peritonitis episodes are preceded by the use of systemic antibiotics (6,33). Randomized, controlled trials and a systematic review show that the use of either oral nystatin or fluconazole during antibiotic therapy reduces the risk of secondary fungal (especially Candida) peritonitis (6,10). In countries where nystatin is available, it should be the preferred choice because it has no systematic effect or drug interactions. Antifungal prophylaxis may also reduce the risk of fungal peritonitis when a patient on PD receives systemic antibiotics for nonperitonitis infections (10), but this practice does not seem to be widely adopted.
After each episode of peritonitis, a root cause analysis should be performed to determine the etiology and possible interventions to prevent further episodes (6). For example, exchange technique should be reviewed after peritonitis episodes caused by touch contamination, and replacement of PD catheter should be considered after relapsing or repeat peritonitis episodes (6). The key measures for the prevention of PD-associated peritonitis are summarized in Table 1.
Table 1.
Key measures for the prevention of PD-associated peritonitis
| Prevention Measures |
|---|
| Primary preventiona |
| Systemic prophylactic antibiotics before PD catheter insertion |
| Disconnect systems with a “flush before fill” design for CAPD |
| PD training by nursing staff with the appropriate qualifications and experience |
| Daily topical application of antibiotic cream or ointment to the catheter exit site |
| Prompt treatment of exit site or catheter tunnel infection |
| Antibiotic prophylaxis before colonoscopy or invasive gynecologic procedures |
| Secondary prevention |
| Antifungal prophylaxis during antibiotic therapy |
| Determine the cause and possible interventions |
PD, peritoneal dialysis; CAPD, continuous ambulatory peritoneal dialysis.
The strength of recommendation and the quality of the supporting evidence can be found in the latest International Society for Peritoneal Dialysis (ISPD) treatment recommendations (6).
Management of PD-Associated Peritonitis
Diagnosis.
The diagnosis of PD-associated peritonitis requires any two of the following features: (1) clinical features consistent with peritonitis, i.e., abdominal pain or cloudy dialysis effluent; (2) dialysis effluent white cell count >100/μl (after a dwell time of at least 2 hours), with >50% neutrophils; and (3) positive dialysis effluent culture (6). However, prompt clinical diagnosis and early initiation of antibiotic therapy are key to successful treatment. Therefore, patients presenting with cloudy effluent should be presumed to have peritonitis and treated as such until the diagnosis is confirmed or excluded (6). Whenever peritonitis is suspected, PD effluent should be tested for cell count, differential, Gram stain, and bacterial culture (6). Blood culture bottle kits are the preferred technique for bacterial culture (6). If immediate delivery of the inoculated culture bottles to the laboratory is not possible, they should be incubated at 37°C. Other effluent concentration techniques may further increase the yield, but are cumbersome to use. There is insufficient evidence for other novel laboratory techniques (e.g., reagent strip or molecular-based tests) (6).
Empirical Antibiotic Therapy.
Once the appropriate microbiologic specimens have been obtained, empirical antibiotic therapy should be started (6). No single antibiotic regimen has been proved to be superior than the others, and the choice should be center-specific (34). The basic principle is to provide adequate coverage of both Gram-positive and Gram-negative organisms, including Pseudomonas species. The current recommendations are vancomycin or first-generation cephalosporin for Gram-positive organism coverage, and third-generation cephalosporin or aminoglycoside for Gram-negative organism coverage (6). The choice of vancomycin versus first-generation cephalosporin should depend on the prevalence of methicillin-resistant organisms in each center.
Intraperitoneal administration of antibiotics is the preferred route unless there are features of systemic sepsis (6). When there is a foreseeable delay in administering intraperitoneal antibiotics, however, the systemic route should be used as a temporary measure so as to ensure a prompt treatment (35). Vancomycin, aminoglycosides, and cephalosporin can be mixed in the same dialysis solution bag (36). However, vancomycin and ceftazidime are incompatible if combined in the same syringe for injection (6). The recommended dosages of antibiotics are summarized in the latest ISPD recommendations (6), but many of them are on the basis of clinical experience rather than pharmacokinetic studies. The dosage of many antibiotics needs to be adjusted for patients with substantial residual kidney function (4,6). A fixed generic dosage for all patients may explain the observation that residual kidney function is associated with treatment failure (37).
Intraperitoneal antibiotics can be given as continuous (in each exchange) or intermittent dosing (6). Intermittent dosing is often possible because many antibiotics have substantial systemic absorption during peritonitis, which permit reentry into the peritoneal cavity in subsequent PD cycles. When given intermittently, the antibiotic-containing PD solution should dwell for at least 6 hours to allow adequate absorption. For β-lactams, both continuous and intermittent intraperitoneal dosing are reasonable options, but continuous dosing has a theoretical advantage because the bactericidal activity is time-dependent (i.e., the reduction in bacterial density is proportional to the time above minimal inhibitory concentration), and should be the preferred regimen (6). However, intermittent dosing is often effective and may be the only feasible regimen when the patient requires helpers or health care visitors to administer the antibiotics, or in patients on automated PD who could not be converted to CAPD temporarily (6).
Unlike β-lactams, intraperitoneal vancomycin is more commonly administered intermittently every 4–5 days. The serum vancomycin level should be kept >15 μg/ml to maintain efficacy (38). Intraperitoneal aminoglycoside is also preferably administered as daily intermittent dosing (6). Short-term aminoglycoside therapy does not accelerate the loss of residual kidney function (39), but prolonged or repeated exposure is associated with vestibular toxicity (40) and should be avoided.
Patients on automated PD who develop peritonitis may switch temporarily to CAPD, so as to facilitate intraperitoneal antibiotics therapy, but conversion is not always feasible for pragmatic reasons (6). For patients who remain on automated PD, the intermittent intraperitoneal dosing should be given in the day dwell (6). Unfortunately, there is a substantial knowledge gap regarding the antibiotic dosing for the treatment of peritonitis in automated PD. Because extrapolation of pharmacokinetic data from CAPD to automated PD may result in significant underdosing in patients on automated PD (6), a higher daily dose is often required.
Adjunctive Measures.
Most patients with PD-associated peritonitis could be managed as outpatients. The decision of hospital admission depends on the clinical severity, hemodynamic status, and often practical considerations of treatment. Antifungal prophylaxis, preferably oral nystatin, should be given along with antibiotic therapy (6). Intraperitoneal heparin is usually added when the PD effluent is cloudy, so as to prevent catheter occlusion by fibrin. In addition, careful blood glucose monitoring is advisable in patients with diabetes because glucose absorption from the PD solution may be increased during peritonitis. Peritoneal protein loss is also increased during peritonitis and malnutrition may develop quickly.
Subsequent Management.
Once the PD effluent Gram stain or culture results are known, antibiotic therapy should be adjusted (6). In general, if Gram-positive organisms are identified, antibiotic coverage for Gram-negative bacteria (i.e., aminoglycoside or third-generation cephalosporin) could be stopped, and vice versa once sensitivities are available. PD effluent leukocyte counts and bacterial culture should be performed again 2–3 days after antibiotic therapy, especially when there is no clinical improvement. PD effluent leukocyte count >1090/µl on day 3 may predict treatment failure (41).
The current ISPD recommendations provide a detailed description on the treatment of peritonitis episodes caused by specific organisms (6). In essence, if the clinical response is satisfactory, peritonitis caused by coagulase-negative staphylococci, streptococci, or culture-negative episodes should be treated for 2 weeks (6). For culture-negative episodes, it remains controversial whether the antibiotic for Gram-negative coverage should be discontinued. The current recommendations state that if aminoglycoside is used as the empirical Gram-negative coverage, it should be stopped to minimize the risk of ototoxicity from repeated exposure (6), although a small study has suggested that N-acetylcysteine may prevent aminoglycoside-related ototoxicity (42).
For the treatment of peritonitis episodes caused by S. aureus, enterococci, Corynebacterium species, Gram-negative bacilli (Pseudomonas or non-Pseudomonas species), and polymicrobial peritonitis, effective antibiotics should be continued for 3 weeks. Because enterococci have intrinsic resistance to cephalosporin, and ampicillin is rapidly inactivated when given intraperitoneally (43), enterococcal peritonitis should be treated with intraperitoneal vancomycin unless there is vancomycin resistance (6). Unlike other bacterial causes, Pseudomonas peritonitis should be treated with two effective antibiotics with different mechanisms of action (e.g., gentamicin or oral ciprofloxacin with ceftazidime or cefepime) (6,44,45). If multiple enteric organisms are identified from PD effluent and when there is no prompt clinical response to empirical antibiotics, surgical evaluation should be obtained immediately, and metronidazole should be used with vancomycin and either an aminoglycoside or ceftazidime (6). In contrast, if multiple Gram-positive organisms are identified from the PD effluent, antibiotic treatment alone is usually effective (46). Standard antituberculous chemotherapy is highly effective for peritonitis caused by Mycobacterium tuberculosis. The treatment regimen for nontuberculous mycobacterial peritonitis is not well defined, but catheter removal is usually needed.
Severe Episodes.
The indications of PD catheter removal are summarized in Table 2. Specifically, refractory peritonitis episode is now defined as failure of the effluent to clear after 5 days of appropriate antibiotics (6), whereas relapsing peritonitis refers to the episode that occur within 4 weeks of completion of therapy of a prior episode with the same organism or being culture negative (6). Recurrent peritonitis refers to an episode that occurs within 4 weeks of completion of therapy of a prior episode but with a different organism (6), whereas repeat peritonitis refers to an episode that occurs >4 weeks after completion of therapy of a prior episode with the same organism (6).
Table 2.
Indications for catheter removal
| Indications for Catheter Removal |
|---|
| Refractory peritonitisa |
| Relapsing and recurrent peritonitis |
| Refractory exit site and tunnel infection |
| Fungal and non-tuberculous mycobacterial peritonitis |
| Catheter removal may also be considered for |
| Repeat peritonitis |
| Peritonitis caused by Mycobacterium tuberculosis |
| Multiple enteric organisms |
Adapted from reference 6, with permission.
After catheter removal for fungal or refractory peritonitis, effective antibiotics should be continued for another 2 weeks (6,47). Insertion of a new PD catheter and return to PD is sometimes possible (47,48), but should be performed at least 2 weeks after catheter removal and complete resolution of peritoneal symptoms (6). PD catheter should also be removed for refractory exit site or tunnel infections (6). If there is no concomitant peritonitis (or after PD effluent has cleared up from the concomitant episode), a new PD catheter could be inserted simultaneously and PD could be continued (7).
Conclusions
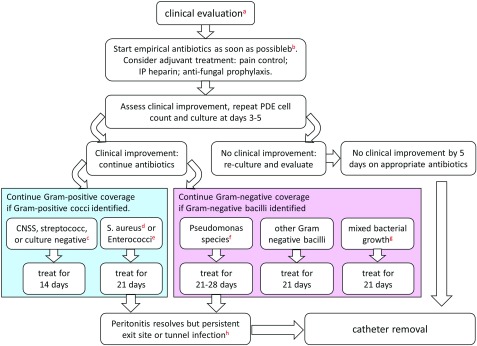
Although comprehensive recommendations on PD-associated peritonitis are available (6), there are important gaps of knowledge that deserve further studies. Notably, the correction of many modifiable risk factors for PD-associated peritonitis does not appear to reduce the risk, the optimal treatment regimen for patients on machine-assisted automated PD is poorly defined, important pharmacokinetic data are not available for many new antibiotics, the chemical stability of many antibiotics in modern PD solutions is unknown, and the effective means to prevent relapsing or recurrent peritonitis episodes are wanting. On the basis of the current recommendations (6), the overall management algorithm of PD-associated peritonitis is summarized in Figure 1. With the connectology system improvement, better hygiene, and implementation of global PD peritonitis guidelines for enhancing prevention and management, we do observe a worldwide reduction of peritonitis in PD (8,49), supporting the use of PD as a first-line dialysis modality (50).
Figure 1.
Algorithm for the management of peritoneal dialysis-related peritonitis. aClinical evaluation includes routine history, physical examination, examination of exit site and catheter tunnel, collection of PDE for cell count, differential count, Gram stain, and bacterial culture. bThe choice of empirical antibiotics coverage should be on the basis of patient history and center sensitivity patterns. cIn centers with a high prevalence of Gram-negative peritonitis, empirical Gram-negative coverage may be continued for culture negative peritonitis episodes. dNeed to screen for S. aureus carrier. eNeed to use vancomycin or other appropriate agents if enterococci identified. fGive two effective antibiotics according to sensitivity; also apply to Stenotrophomonas and other Pseudomonas-like species. gConsider surgical problem; in addition to Gram-negative coverage, consider metronidazole and vancomycin. hEspecially for peritonitis episodes caused by S. aureus or Pseudomonas species. CNSS, coagulase negative staphylococcal species; IP, intraperitoneal; PDE, peritoneal dialysis effluent.
Disclosures
Dr. Szeto reports grants and personal fees from Baxter Healthcare, during the conduct of the study. Dr. Li has nothing to disclose.
Acknowledgments
This work was supported in part by the Chinese University of Hong Kong research accounts 6901031 and 6900570.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Szeto CC, Wong TY, Chow KM, Leung CB, Li PK: Are peritoneal dialysis patients with and without residual renal function equivalent for survival study? Insight from a retrospective review of the cause of death. Nephrol Dial Transplant 18: 977–982, 2003 [DOI] [PubMed] [Google Scholar]
- 2.Boudville N, Kemp A, Clayton P, Lim W, Badve SV, Hawley CM, McDonald SP, Wiggins KJ, Bannister KM, Brown FG, Johnson DW: Recent peritonitis associates with mortality among patients treated with peritoneal dialysis. J Am Soc Nephrol 23: 1398–1405, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Htay H, Cho Y, Pascoe EM, Darssan D, Nadeau-Fredette AC, Hawley C, Clayton PA, Borlace M, Badve SV, Sud K, Boudville N, McDonald SP, Johnson DW: Multicenter registry analysis of center characteristics associated with technique failure in patients on incident peritoneal dialysis. Clin J Am Soc Nephrol 12: 1090–1099, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li PK, Szeto CC, Piraino B, Bernardini J, Figueiredo AE, Gupta A, Johnson DW, Kuijper EJ, Lye WC, Salzer W, Schaefer F, Struijk DG; International Society for Peritoneal Dialysis: Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int 30: 393–423, 2010 [DOI] [PubMed] [Google Scholar]
- 5.Piraino B, Bernardini J, Brown E, Figueiredo A, Johnson DW, Lye WC, Price V, Ramalakshmi S, Szeto CC: ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit Dial Int 31: 614–630, 2011 [DOI] [PubMed] [Google Scholar]
- 6.Li PK, Szeto CC, Piraino B, de Arteaga J, Fan S, Figueiredo AE, Fish DN, Goffin E, Kim YL, Salzer W, Struijk DG, Teitelbaum I, Johnson DW: ISPD peritonitis recommendations: 2016 update on prevention and treatment. Perit Dial Int 36: 481–508, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Szeto CC, Li PK, Johnson DW, Bernardini J, Dong J, Figueiredo AE, Ito Y, Kazancioglu R, Moraes T, Van Esch S, Brown EA: ISPD catheter-related infection recommendations: 2017 update. Perit Dial Int 37: 141–154, 2017 [DOI] [PubMed] [Google Scholar]
- 8.Cho Y, Johnson DW: Peritoneal dialysis-related peritonitis: Towards improving evidence, practices, and outcomes. Am J Kidney Dis 64: 278–289, 2014 [DOI] [PubMed] [Google Scholar]
- 9.Boudville N, Johnson DW, Zhao J, Bieber BA, Pisoni RL, Piraino B, Bernardini J, Nessim SJ, Ito Y, Woodrow G, Brown F, Collins J, Kanjanabuch T, Szeto CC, Perl J: Regional variation in the treatment and prevention of peritoneal dialysis-related infections in the Peritoneal Dialysis Outcomes and Practice Patterns Study [published online ahead of print July 23, 2018]. Nephrol Dial Transplant doi: 10.1093/ndt/gfy204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strippoli GF, Tong A, Johnson D, Schena FP, Craig JC: Antimicrobial agents to prevent peritonitis in peritoneal dialysis: A systematic review of randomized controlled trials. Am J Kidney Dis 44: 591–603, 2004 [PubMed] [Google Scholar]
- 11.Strippoli GF, Tong A, Johnson D, Schena FP, Craig JC: Catheter-related interventions to prevent peritonitis in peritoneal dialysis: A systematic review of randomized, controlled trials. J Am Soc Nephrol 15: 2735–2746, 2004 [DOI] [PubMed] [Google Scholar]
- 12.Hagen SM, Lafranca JA, IJzermans JN, Dor FJ: A systematic review and meta-analysis of the influence of peritoneal dialysis catheter type on complication rate and catheter survival. Kidney Int 85: 920–932, 2014 [DOI] [PubMed] [Google Scholar]
- 13.Nessim SJ, Bargman JM, Jassal SV: Relationship between double-cuff versus single-cuff peritoneal dialysis catheters and risk of peritonitis. Nephrol Dial Transplant 25: 2310–2314, 2010 [DOI] [PubMed] [Google Scholar]
- 14.Daly C, Cody JD, Khan I, Rabindranath KS, Vale L, Wallace SA: Double bag or Y-set versus standard transfer systems for continuous ambulatory peritoneal dialysis in end-stage kidney disease. Cochrane Database Syst Rev 8: CD003078, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rüger W, van Ittersum FJ, Comazzetto LF, Hoeks SE, ter Wee PM: Similar peritonitis outcome in CAPD and APD patients with dialysis modality continuation during peritonitis. Perit Dial Int 31: 39–47, 2011 [DOI] [PubMed] [Google Scholar]
- 16.Lan PG, Johnson DW, McDonald SP, Boudville N, Borlace M, Badve SV, Sud K, Clayton PA: The association between peritoneal dialysis modality and peritonitis. Clin J Am Soc Nephrol 9: 1091–1097, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Htay H, Johnson DW, Wiggins KJ, Badve SV, Craig JC, Strippoli GF, Cho Y: Biocompatible dialysis fluids for peritoneal dialysis. Cochrane Database Syst Rev 10: CD007554, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Figueiredo AE, Bernardini J, Bowes E, Hiramatsu M, Price V, Su C, Walker R, Brunier G: A syllabus for teaching peritoneal dialysis to patients and caregivers. Perit Dial Int 36: 592–605, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang L, Hawley CM, Johnson DW: Focus on peritoneal dialysis training: Working to decrease peritonitis rates. Nephrol Dial Transplant 31: 214–222, 2016 [DOI] [PubMed] [Google Scholar]
- 20.Boudville NC, Chow JS, Cho Y: Targeted Education ApproaCH to Improve Peritoneal Dialysis Outcomes Trial (TEACH-PD), 2019. Available at https://clinicaltrials.gov/ct2/show/NCT03816111. Accessed February 14, 2019
- 21.Wang J, Zhang H, Liu J, Zhang K, Yi B, Liu Y, Liu J, Zhang X, Ji Y: Implementation of a continuous quality improvement program reduces the occurrence of peritonitis in PD. Ren Fail 36: 1029–1032, 2014 [DOI] [PubMed] [Google Scholar]
- 22.Nataatmadja M, Cho Y, Johnson DW: Continuous quality improvement initiatives to sustainably reduce peritoneal dialysis-related infections in Australia and New Zealand. Perit Dial Int 36: 472–477, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Diepen AT, Tomlinson GA, Jassal SV: The association between exit site infection and subsequent peritonitis among peritoneal dialysis patients. Clin J Am Soc Nephrol 7: 1266–1271, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu G, Tu W, Xu C: Mupirocin for preventing exit-site infection and peritonitis in patients undergoing peritoneal dialysis. Nephrol Dial Transplant 25: 587–592, 2010 [DOI] [PubMed] [Google Scholar]
- 25.Wong C, Luk IW, Ip M, You JH: Prevention of gram-positive infections in peritoneal dialysis patients in Hong Kong: A cost-effectiveness analysis. Am J Infect Control 42: 412–416, 2014 [DOI] [PubMed] [Google Scholar]
- 26.Piraino B: Mupirocin for preventing exit-site infection and peritonitis in patients undergoing peritoneal dialysis. Was it effective? Nephrol Dial Transplant 25: 349–352, 2010 [DOI] [PubMed] [Google Scholar]
- 27.Gardezi AI, Schlageter KW, Foster DM, Astor BC, Chan MR, Waheed S: Erosion of the silicone peritoneal dialysis catheter with the use of gentamicin cream at the exit site. Adv Perit Dial 32: 15–18, 2016 [PubMed] [Google Scholar]
- 28.Bernardini J, Bender F, Florio T, Sloand J, Palmmontalbano L, Fried L, Piraino B: Randomized, double-blind trial of antibiotic exit site cream for prevention of exit site infection in peritoneal dialysis patients. J Am Soc Nephrol 16: 539–545, 2005 [DOI] [PubMed] [Google Scholar]
- 29.Johnson DW, Badve SV, Pascoe EM, Beller E, Cass A, Clark C, de Zoysa J, Isbel NM, McTaggart S, Morrish AT, Playford EG, Scaria A, Snelling P, Vergara LA, Hawley CM; HONEYPOT Study Collaborative Group: Antibacterial honey for the prevention of peritoneal-dialysis-related infections (HONEYPOT): A randomised trial. Lancet Infect Dis 14: 23–30, 2014 [DOI] [PubMed] [Google Scholar]
- 30.McQuillan RF, Chiu E, Nessim S, Lok CE, Roscoe JM, Tam P, Jassal SV: A randomized controlled trial comparing mupirocin and polysporin triple ointments in peritoneal dialysis patients: The MP3 study. Clin J Am Soc Nephrol 7: 297–303, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bernardini J, Piraino B, Holley J, Johnston JR, Lutes R: A randomized trial of Staphylococcus aureus prophylaxis in peritoneal dialysis patients: Mupirocin calcium ointment 2% applied to the exit site versus cyclic oral rifampin. Am J Kidney Dis 27: 695–700, 1996 [DOI] [PubMed] [Google Scholar]
- 32. Yip T, Tse KC, Lam MF, Cheng SW, Lui SL, Tang S, Ng M, Chan TM, Lai KN, Lo WK. Risks and outcomes of peritonitis after flexible colonoscopy in CAPD patients. Perit Dial Intern 27: 560–564, 2007. [PubMed]
- 33.Prasad KN, Prasad N, Gupta A, Sharma RK, Verma AK, Ayyagari A: Fungal peritonitis in patients on continuous ambulatory peritoneal dialysis: A single centre Indian experience. J Infect 48: 96–101, 2004 [DOI] [PubMed] [Google Scholar]
- 34.Ballinger AE, Palmer SC, Wiggins KJ, Craig JC, Johnson DW, Cross NB, Strippoli GF: Treatment for peritoneal dialysis-associated peritonitis. Cochrane Database Syst Rev 26: CD005284, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Muthucumarana K, Howson P, Crawford D, Burrows S, Swaminathan R, Irish A: The relationship between presentation and the time of initial administration of antibiotics with outcomes of peritonitis in peritoneal dialysis patients: The PROMPT study. Kidney Int Rep 1: 65–72, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Vin F, Rutherford P, Faict D: Intraperitoneal administration of drugs in peritoneal dialysis patients: A review of compatibility and guidance for clinical use. Perit Dial Int 29: 5–15, 2009 [PubMed] [Google Scholar]
- 37.Whitty R, Bargman JM, Kiss A, Dresser L, Lui P: Residual kidney function and peritoneal dialysis-associated peritonitis treatment outcomes. Clin J Am Soc Nephrol 12: 2016–2022, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blunden M, Zeitlin D, Ashman N, Fan SL: Single UK centre experience on the treatment of PD peritonitis--antibiotic levels and outcomes. Nephrol Dial Transplant 22: 1714–1719, 2007 [DOI] [PubMed] [Google Scholar]
- 39.Szeto CC, Kwan BC, Chow KM, Chung S, Yu V, Cheng PM, Leung CB, Law MC, Li PK: Predictors of residual renal function decline in patients undergoing continuous ambulatory peritoneal dialysis. Perit Dial Int 35: 180–188, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tokgoz B, Somdas MA, Ucar C, Kocyigit I, Unal A, Sipahioglu MH, Oymak O, Utas C: Correlation between hearing loss and peritonitis frequency and administration of ototoxic intraperitoneal antibiotics in patients with CAPD. Ren Fail 32: 179–184, 2010 [DOI] [PubMed] [Google Scholar]
- 41.Chow KM, Szeto CC, Cheung KK, Leung CB, Wong SS, Law MC, Ho YW, Li PK: Predictive value of dialysate cell counts in peritonitis complicating peritoneal dialysis. Clin J Am Soc Nephrol 1: 768–773, 2006 [DOI] [PubMed] [Google Scholar]
- 42.Tokgoz B, Ucar C, Kocyigit I, Somdas M, Unal A, Vural A, Sipahioglu M, Oymak O, Utas C: Protective effect of N-acetylcysteine from drug-induced ototoxicity in uraemic patients with CAPD peritonitis. Nephrol Dial Transplant 26: 4073–4078, 2011 [DOI] [PubMed] [Google Scholar]
- 43.Kussmann M, Schuster L, Zeitlinger M, Pichler P, Reznicek G, Wiesholzer M, Burgmann H, Poeppl W: The influence of different peritoneal dialysis fluids on the in vitro activity of ampicillin, daptomycin, and linezolid against Enterococcus faecalis. Eur J Clin Microbiol Infect Dis 34: 2257–2263, 2015 [DOI] [PubMed] [Google Scholar]
- 44.Szeto CC, Chow KM, Leung CB, Wong TY, Wu AK, Wang AY, Lui SF, Li PK: Clinical course of peritonitis due to Pseudomonas species complicating peritoneal dialysis: A review of 104 cases. Kidney Int 59: 2309–2315, 2001 [DOI] [PubMed] [Google Scholar]
- 45.Siva B, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Johnson DW: Pseudomonas peritonitis in Australia: Predictors, treatment, and outcomes in 191 cases. Clin J Am Soc Nephrol 4: 957–964, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Szeto CC, Chow KM, Wong TY, Leung CB, Li PK: Conservative management of polymicrobial peritonitis complicating peritoneal dialysis--a series of 140 consecutive cases. Am J Med 113: 728–733, 2002 [DOI] [PubMed] [Google Scholar]
- 47.Szeto CC, Chow KM, Wong TY, Leung CB, Wang AY, Lui SF, Li PK: Feasibility of resuming peritoneal dialysis after severe peritonitis and Tenckhoff catheter removal. J Am Soc Nephrol 13: 1040–1045, 2002 [DOI] [PubMed] [Google Scholar]
- 48.Ram R, Swarnalatha G, Dakshinamurty KV: Reinitiation of peritoneal dialysis after catheter removal for refractory peritonitis. J Nephrol 27: 445–449, 2014 [DOI] [PubMed] [Google Scholar]
- 49.Li PK, Kwong VW: Current challenges and opportunities in PD. Semin Nephrol 37: 2–9, 2017 [DOI] [PubMed] [Google Scholar]
- 50.Li PK, Chow KM, Van de Luijtgaarden MW, Johnson DW, Jager KJ, Mehrotra R, Naicker S, Pecoits-Filho R, Yu XQ, Lameire N: Changes in the worldwide epidemiology of peritoneal dialysis. Nat Rev Nephrol 13: 90–103, 2017 [DOI] [PubMed] [Google Scholar]