Worldwide, only 10% of the approximately 1.7 million patients on dialysis are treated with home-based peritoneal dialysis (PD); the majority receive facility-based hemodialysis (HD), although most patients prefer PD when educated about their options (1). There is substantial geographic variation in PD utilization. Between-country variation may result from cost of treatments; cultural, educational, and health care system differences; or reimbursement policies that incentivize the use of one therapy. Within-country variation may reflect regional differences in facility infrastructure, expertise, resources, and home dialysis education.
Physician education, training, and experience with home PD remain limited. A recent survey identified home dialysis training as the leading educational gap among United States nephrologists in training (2). Although few absolute contraindications to PD exist, recommendations to more challenging patients can vary. This may stem from a lack of comfort with PD as a therapy or an inherent negative perception regarding its suitability.
We compared differences in attitudes of the medical directors of both PD and in-center HD units toward patient eligibility and the barriers to PD utilization. We hypothesized that, regardless of country and by virtue of limited exposure, the leaders of HD facilities may use more restrictive and varied eligibility criteria and perceive different barriers to PD use compared with their PD counterparts.
We examined 2014–2018 data from the Dialysis Outcomes and Practice Patterns Study (DOPPS) Phases 5 and 6 and the Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS) Phase 1. The DOPPS and the PDOPPS are ongoing, international prospective cohort studies of dialysis facility practices and patient outcomes for adult in-center HD and PD participants. Study participants are ≥18 years old and selected randomly from a national sample of patients at dialysis facilities (http://www.dopps.org) (3,4). A central institutional review board approved each study phase; we obtained additional approvals and informed patient consents as required by national and local regulations.
The DOPPS asked medical directors of PD and HD facilities in Canada, Japan, the United Kingdom, and the United States (1) to rate the level of PD training and support in their units, (2) whether certain patient factors would influence PD recommendations, and (3) about potential reasons why PD was not more widely used in their program.
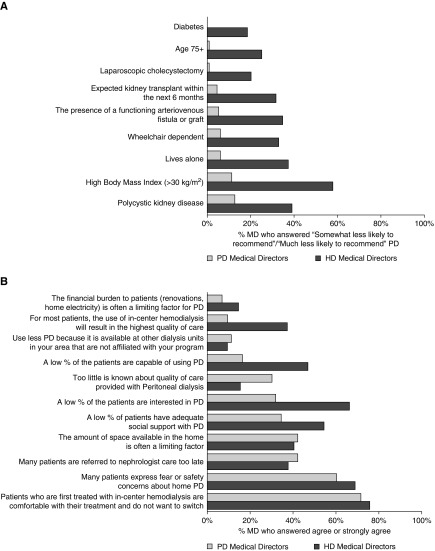
One hundred eighty-five (73% response rate) HD and 116 (66% response rate) PD directors responded. PD directors perceived greater PD training and enthusiasm among their nephrologists and nursing staff (72%–97% versus 69%–84%, respectively). HD directors were much less likely to recommend PD for patients across a host of conditions and patient characteristics (Figure 1A).
Figure 1.
Hemodialysis (HD) medical directors were less likely to recommend peritoneal dialysis (PD) and had different opinions about the reasons for low PD use than PD medical directors. (A) The survey question was as follows: “How likely are you to discourage the use of peritoneal dialysis based on the following conditions alone?” In total, 116 medical directors (MDs) in PD facilities (Canada, 15; Japan, 25; the United Kingdom, 34; and the United States, 42) and 185 MDs in HD facilities (Canada, 25; Japan, 61; the United Kingdom, 20; and the United States, 79) responded. Answer choices for HD MDs were much more likely to recommend, somewhat more likely to recommend, remain neutral, somewhat less likely to recommend, and much less likely to recommend, whereas for PD MDs, answer choices were strongly encourage, encourage, remain neutral, discourage, and strongly discourage. (B) The survey question was: “The following questions refer to the reasons PD is not more widely used at your program. Answer your level of agreement with the following.” In total, 116 MDs in PD facilities (Canada, 15; Japan, 25; the United Kingdom, 34; and the United States, 42) and 185 MDs in HD facilities (Canada, 25; Japan, 61; the United Kingdom, 20; and the United States, 79) responded. Answer choices were the same for both groups: strongly disagree, disagree, neither agree nor disagree, agree, and strongly agree.
HD and PD directors held different opinions about the reasons for low PD use in their programs (Figure 1B). HD directors were more likely to cite patient factors, such as low interest, social support, and capability to use PD, as the cause of lower use. Nearly 40% of HD medical directors compared to only 10% of PD medical directors indicated the perception of HD's superior quality impeding PD growth at their unit. The only major intercountry variation that we noted was in Japan—staff members in these HD units were generally the least enthusiastic about PD (35%–40% versus 61%–100% in other countries).
It is troubling that these beliefs translate into strikingly wide gaps in recommending PD for incident patients with common comorbid conditions. One half of United States patients starting dialysis have diabetes, one quarter are age 75 years old or older, and one third are obese. Choosing not to consider PD for these patients will restrict their choice of modality, a decision more appropriately made on the basis of broader clinical and patient-centered outcomes, such as quality of life.
HD medical directors’ responses also indicated misconceptions about PD eligibility. They may have been unfamiliar with the option of assisted PD for patients traditionally viewed as poor candidates or less current with literature that has refuted the myths that minor surgeries, polycystic kidney disease, or impending transplant are contraindications to PD. Physicians may also steer patients with a functioning fistula or graft toward HD.
HD medical directors were more likely to cite patient preferences as a barrier to PD use, a view potentially influenced by interaction with patients who have chosen HD over PD. Physicians’ belief that patients prefer HD may consciously or unconsciously alter their approach to presenting PD as a treatment option.
Improved personnel education has the potential to reduce bias against home dialysis in HD units. A 3-hour education initiative improved the attitudes of in-center HD nurses toward home dialysis (5). Similar interventions for HD-focused physicians may catalyze PD growth.
Another solution involves creation of dedicated transitional care units that provide incident patients on dialysis with the comprehensive support and unbiased education that they need to make an informed modality choice (6). This is especially salient among patients urgently starting dialysis. Many “crash start” patients initiate HD by default without the opportunity to be adequately informed. Almost 80% of both HD and PD directors agreed that the preference of patients on in-center HD not to switch modalities was a major barrier to PD growth. After patients are established in traditional HD centers, education about treatment options may be limited and delivered by personnel who may strongly favor HD (5).
Study limitations include that physician opinions may not reflect actual practice and that results may not be generalizable to the excluded directors who practice in units with <20 patients on PD or HD and countries not included in the survey. We also did not quantify PD exposure and expertise among respondents and surveyed on select barriers, which did not include physician reimbursement policies.
Notwithstanding these limitations, HD medical directors had staff members with less training in and enthusiasm for PD, were less likely to recommend PD, and were more likely to cite patient preference as a barrier to PD growth. Educating physicians and staff, particularly about PD feasibility among various patients, may lead to greater utilization. The addition of transitional care units to ensure complete and unbiased patient education would help support informed modality decision making, particularly for those unexpectedly starting dialysis. Only through a multipronged solution that engages a range of practitioners can we expect to see major gains in PD use.
Disclosures
Dr. Robinson and Dr. Pisoni report grants from a large consortium of funders of the DOPPS Program. Dr. Shen reports personal fees from Baxter outside the submitted work. Dr. Schreiber reports being employed by DaVita. Dr. Mehrotra reports personal fees from Zytoprotec outside the submitted work. Dr. Oliver reports grants and personal fees from Baxter Healthcare, and grants from Medtronics, during the conduct of the study, personal fees from Pursuit Vascular outside the submitted work, and is the founder and owner of Oliver Medical Management Inc., which manufactures and distributes DMAR systems software. Dr. Ghaffari is a speaker for Baxter Healthcare and a consultant/speaker for DaVita Healthcare. Dr. Lambie has received a research grant and speaker’s honoraria from Baxter Healthcare, a speaker’s honorarium from Fresenius Medical Care, and a consultancy fee from NxStage all outside the scope of the submitted work. Dr. Perl reports grants from the Canadian Institute for Health Research, grants from Baxter Healthcare, and personal fees from Arbor Research Collaborative for Health during the conduct of the study and personal fees from Baxter Healthcare, Fresenius Medical Care, DaVita Healthcare, DCI, and Satellite Healthcare outside the submitted work. Dr. Zhao, Dr. Tomo, Dr. Tungsanga, and Dr. Teitelbaum have nothing to disclose.
Acknowledgments
Shauna Leighton, a Medical Editor with Arbor Research Collaborative for Health, provided editorial assistance on the manuscript. Janet Leslie, a Medical Technical Writer with Arbor Research Collaborative for Health assisted in revising the presentation of the researchers’ results and finalizing the manuscript.
Dr. Shen is supported by National Institutes of Health grant K23DK103972. Global support for the ongoing Dialysis Outcomes and Practice Patterns Study (DOPPS) Programs is provided without restriction on publications by a variety of funders (details are available at https://www.dopps.org/AboutUs/Support.aspx).
The authors acknowledge and thank the following individuals for their contributions: The Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS) Steering Committee members were David Johnson (University of Queensland, Australia), Dr. Perl (University of Toronto, Canada), Mauricio Sanabria (Baxter RTS Latino-America, Colombia), Hideki Kawanishi (Tsuchiya General Hospital, Japan), Yong-Lim Kim (Kyungpook National University, South Korea), Talerngsak Kanjanabuch (Chulalongkorn University, Thailand), Simon Davies (Keele University, United Kingdom), Angelito Bernardo (Baxter Healthcare Inc., United States), Dr. Pisoni (Arbor Research Collaborative for Health, United States), Dr. Robinson (Arbor Research Collaborative for Health, United States), and Dr. Shen (David Geffen School of Medicine at UCLA, United States). Additional PDOPPS Research Group members included Sunil Badve (St. George Hospital, Australia), Neil Boudville (The University of Western Australia, Australia), Fiona Brown (Monash University, Australia), Josephine Chow (University of Tasmania, Australia), John Collins (Auckland City Hospital, Australia), Rachael Morton (The University of Sydney, Australia), Scott Wilson (Monash University, Australia); Andreas Vychytil (Medical University of Vienna, Austria); Wim Van Biesen (Ghent University, Belgium); Ana Figueiredo (Pontifícia University, Brazil) and Thyago de Moraes (Pontifícia University, Brazil); Gillian Brunier (Sunnybrook Health Sciences Centre, Canada), Arsh Jain (London Health Sciences Centre, Canada), Vanita Jassal (Toronto General Hospital Research Institute, Canada), Sharon Nessim (McGill University, Canada), Matthew Oliver (Sunnybrook Health Sciences Centre, Canada), Valerie Price (Horizon Health Network, Canada), Rob Quinn (The University of Calgary, Canada); Wei Fang (Renji Hospital, China); C.C. Szeto (The Chinese University of Hong Kong, Hong Kong); Angela Wang (University of New South Wales, Australia); Mizuya Fukasawa (University of Yamanashi, Japan), Yasuhiko Ito (Nagoya University, Japan), Munekazu Ryuzaki (Tokyo Saiseikai Central Hospital, Japan), and Dr. Tomo (Japanese Society for Dialysis Therapy, Japan); Alfonso Cueto Manzano (Mexican Institute of Social Security, Mexico); Mark Marshall (Middlemore Hospital, New Zealand); Susanne Ljungman (Sahlgrenska University Hospital, Sweden); Sarinya Boongird (Mahidol University, Thailand), Chanchana Boonyakrai (Taksin Hospital, Thailand), Areewan Cheawchanwattana (Srinagarind Hospital, Thailand), Guttiga Halue (Prayao Hospital, Thailand), Suchai Sritippayawan (Siriraj Hospital, Thailand), Sajja Tatiyanupanwong (Khon Kaen University, Thailand), Kriang Tungsanga (Chulalongkorn University, Thailand); Elaine Bowes (Kings College London, United Kingdom), Edwina Brown (Imperial College London, United Kingdom), Richard Fluck (Royal Derby Hospital, United Kingdom), Bak Leong Goh (Serdang Hospital, United Kingdom), Helen Hurst (Manchester University Foundation, United Kingdom), Martin Wilkie (Sheffield Teaching Hospitals, United Kingdom), Graham Woodrow (Leeds Teaching Hospitals, United Kingdom); and Filitsa Bender (DCI Renal Services Pittsburgh, United States), Judith Bernardini (University of Pittsburgh, United States), Dinesh Chatoth (Fresenius Medical Care, United States), John Crabtree (Society for Education and Research in Peritoneal Access Surgery, United States), Fred Finkelstein (Yale New Haven Hospital, United States), Arshia Ghaffari (Keck School of Medicine of USC, United States), Raj Mehrotra (University of Washington, United States), Beth Piraino (University of Pittsburgh School of Medicine, United States), Martin Schreiber (DaVita Kidney Care, United States), and Isaac Teitelbaum (University of Colorado Hospital, United States).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Devoe DJ, Wong B, James MT, Ravani P, Oliver MJ, Barnieh L, Roberts DJ, Pauly R, Manns BJ, Kappel J, Quinn RR: Patient education and peritoneal dialysis modality selection: A systematic review and meta-analysis. Am J Kidney Dis 68: 422–433, 2016 [DOI] [PubMed] [Google Scholar]
- 2.Rope RW, Pivert KA, Parker MG, Sozio SM, Merell SB: Education in nephrology fellowship: A survey-based needs assessment. J Am Soc Nephrol 28: 1983–1990, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perl J, Davies SJ, Lambie M, Pisoni RL, McCullough K, Johnson DW, Sloand JA, Prichard S, Kawanishi H, Tentori F, Robinson BM: The Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS): Unifying Efforts to Inform Practice and Improve Global Outcomes in Peritoneal Dialysis. Perit Dial Int 36: 297–307, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pisoni RL, Gillespie BW, Dickinson DM, Chen K, Kutner MH, Wolfe RA: The Dialysis Outcomes and Practice Patterns Study (DOPPS): Design, data elements, and methodology. Am J Kidney Dis 44[Suppl 2]: 7–15, 2004 [DOI] [PubMed] [Google Scholar]
- 5.Phillips M, Wile C, Bartol C, Stockman C, Dhir M, Soroka SD, Hingwala J, Bargman JM, Chan CT, Tennankore KK: An education initiative modifies opinions of hemodialysis nurses towards home dialysis. Can J Kidney Health Dis 2: 16, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bowman B, Zheng S, Yang A, Schiller B, Morfín JA, Seek M, Lockridge RS: Improving incident ESRD care via a transitional care unit. Am J Kidney Dis 72: 278–283, 2018 [DOI] [PubMed] [Google Scholar]