Abstract
IMPORTANCE:
Nonalcoholic fatty liver disease (NAFLD) is rapidly evolving into one of the most common pediatric liver diseases and currently is the most common cause for liver transplantation in young adults. Therefore, early recognition of risk factors, disease prevention, and diagnosis during childhood is paramount for effective management.
OBJECTIVE:
The primary objective of this review is to discuss updated recommendations for screening, diagnosis and management of NAFLD. The secondary objective is to review the extent and impact of pediatric NAFLD in Oklahoma through our center’s participation in a multi-center prospective study.
EVIDENCE REVIEW:
We reviewed updated guidelines from the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN), the approach used in our clinic and data from a multi-center collaboration on NAFLD, known as TARGET-NASH.
FINDINGS:
Our review highlights that obese and Hispanic children are at greatest risk for developing NAFLD. Screening with ALT should be considered between ages 9–11 years for children with BMI more than the 95th percentile. Liver biopsy is the gold standard for diagnosis of NAFLD and currently lifestyle modification is the only effective therapy for management of NAFLD.
CONCLUSION AND RELEVANCE:
All obese children, especially those who are Hispanics or have a family history of NAFLD should be considered for screening with serum ALT between the ages of 9 and 11 years. Children with ALT values that are elevated more than twice the upper limit of normal for more than 3 months must be referred to pediatric hepatology for timely evaluation.
Keywords: Pediatric, NAFLD, Oklahoma, Obesity, Liver
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) is defined as liver fat accumulation (steatosis) that exceeds 5% by volume, confirmed by imaging or histology, and not secondary to genetic/metabolic disorders, infections, use of steatogenic medications, ethanol consumption, or malnutrition. NAFLD is a spectrum ranging from nonalcoholic fatty liver (NAFL), which is simple steatosis, to nonalcoholic steatohepatitis (NASH) marked by steatosis, inflammation, fibrosis, and cirrhosis, which leads to end stage liver disease requiring liver transplantation. NAFLD-related cirrhosis is the leading indication for liver transplantation in young adults (1). The prevalence of pediatric NAFLD and NASH rose in parallel with the increase in obesity over the past 30 years (2). Data from the National Health and Nutritional Examination Survey (NHANES) showed that the number of adults with NAFLD and advanced fibrosis or cirrhosis rose by 2- and 2.5-fold, respectively, over the period from 1999 to 2012 (3). That analysis estimated that 4.1 million American adults had NAFLD with advanced fibrosis in 2010. Amid many controversial reports that obesity prevalence in children and adolescents has remained stable or decreased in recent years, Skinner et al. (4) recently analyzed NHANES data from 1999–2016 and found there has been a significant increase in severe obesity in children between 2 and 5 years of age in last 5 years. It is no coincidence then that over one third of the adult population in the United States is obese and that obesity prevalence is expected to continue to increase. Recent CDC statistics for the state of Oklahoma show that the prevalence of obesity in adolescents is 11.8%, and that 15.3% adolescents are overweight. Additionally, Weedn et al. (5, 6) reported that overweight and obese youth are more likely to come from households with low socioeconomic status and from Hispanic backgrounds. These risk factors of developing obesity in Oklahoma’s children exacerbate the healthcare disparities and the burden of disease associated with NAFLD in this state. All these data put together underlie a major healthcare concern because obesity and NAFLD developed at an early age are likely to contribute to high rates of NASH in adults.
INCIDENCE, PREVALENCE AND RISK FACTORS
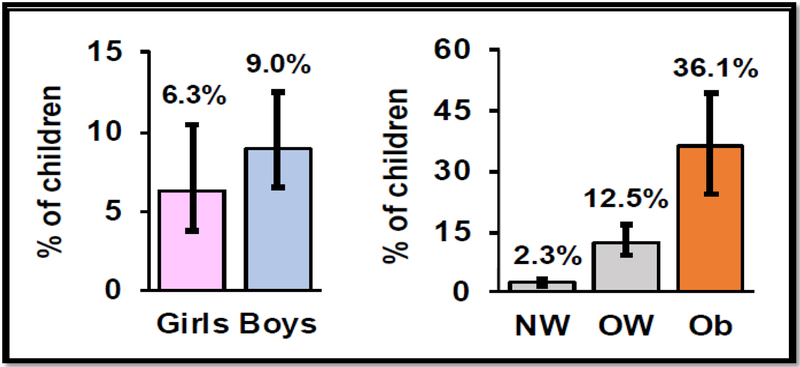
The incidence of pediatric NAFLD is unknown. Prevalence of NAFLD has increased 2.7-fold over the last 20–30 years and varies by age (increasing prevalence with age), sex (higher in boys), race/ethnicity (higher in minority populations in the United States) and body mass index (BMI, strongly associated with obesity)(7). There is increased prevalence of NAFLD in children who have risk factors such as type 2 diabetes, obstructive sleep apnea (OSA), or panhypopituitarism. Prevalence rates also vary among the population being screened (general versus high risk) and screening method used (blood tests, imaging, or liver biopsy). Studies done in North America showed that NAFLD prevalence ranges from 0.7% in children between ages 2–4 years at time of autopsy to 29–38% in obese children (8–11). NAFLD is 4-fold more prevalent in Hispanic children; it is also more common in Hispanics, Asians, and Caucasian youth than it is in the African American population. Males and obese children are also more likely to be affected compared to females and children with normal weight as shown in Figure 1 (12). Recent NANHES analysis using alanine aminotransferase (ALT) elevation showed that prevalence of NAFLD increased 2.7 fold from late 1980s to current period (7).
Figure 1.
Prevalence of pediatric NAFLD. Values are mean +/− 95% confidence interval. Left: boys > girls. Right: obese > overweight > normal weight. NW: normal weight; OW: over weight; Ob: Obese.
NATURAL HISTORY
Nonalcoholic fatty liver disease can be classified into nonalcoholic fatty liver, which denotes bland (uncomplicated) steatosis, and nonalcoholic steatohepatitis (NASH), which is marked by steatosis and lobular inflammation and hepatocellular injury. If the disease process continues, it leads to fibrosis and cirrhosis, which represents a more severe phenotype. The increased mortality observed in adult patients with NAFLD is secondary to cardiovascular disease, cirrhosis, and hepatocellular carcinoma. Ekstedt et al (13) have shown that the stage of fibrosis at baseline diagnosis is the most predictive feature of liver disease related mortality in adults. The worst prognosis was noted in patients who had advanced fibrosis (stage 3 or 4 out of 4). Natural history data for children are limited, but the available evidence suggests that pediatric NAFLD has a more aggressive phenotype and a more severe course compared to NAFLD in adults. For example, 15% of children diagnosed with NAFLD have stage 3 or 4 fibrosis at time of diagnosis (14). In addition, some children have a unique pattern of portal/ periportal fibrosis that is rarely seen in adults (15). The significance of this unique pattern of injury is unknown and thus studies are needed to increase our understanding about pediatric NASH.
CURRENT APPROACHES TO SCREENING AND DIAGNOSIS OF NAFLD
Non-NAFLD conditions that can cause steatosis in liver include metabolic or genetic problems, use of specific medications, infections, and excessive alcohol intake, as shown in Table 1. Guidelines for diagnosing NAFLD and NASH in children were updated in 2017 by the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (2). That expert report emphasized those obese children should be prioritized for screening because of their likelihood to have NAFLD (Figure 1). Currently, the only recommended blood test for screening is ALT. An advantage of ALT is that it is inexpensive, and the measurement has been standardized among laboratories. ALT greater than 2 times the sex-specific upper limit of normal (ALT >50 units for boys, >44 units for girls) in overweight and obese children has a sensitivity of 88% and specificity of 26% for the diagnosing NAFLD. Children with persistently (>3 months) elevated ALT that is more than 2-times the upper limit of normal should be evaluated for other causes of chronic hepatitis like hepatitis, Wilson’s disease, autoimmune and alpha 1 anti-trypsin, in addition to NAFLD. Other risk factors that may warrant screening with ALT include insulin resistance, prediabetes, type 2 diabetes, dyslipidemia, central adiposity, or identity as specific ethno-racial populations. The American Academy of Pediatrics (AAP) and the North American Society of Pediatric Gastroenterology society (NASPGHAN) recommend measuring ALT in children who are 9 to 11 years old who are obese (BMI ≥95th percentile for age and sex). ALT screening should also be performed in 9 to 11 year-old children who are overweight (BMI: 85th to 94th percentile) and have additional risk factors like insulin resistance, diabetes, dyslipidemia, sleep apnea, central adiposity, or family history of NAFLD.
Table 1:
Causes of hepatic steatosis other than non-alcoholic fatty liver disease.
| Genetic/Metabolic disorders | Medications | Dietary | Infections |
|---|---|---|---|
| Lysosomal Acid Lipase (LAL-D) deficiency | Corticosteroids | Alcohol | Hepatitis C (genotype 3) |
| Citrin deficiency | Amiodarone | Rapid weight loss | |
| Wilson’s disease | Methotrexate | Parenteral nutrition | |
| Lipodystrophies | Antipsychotics | Protein-energy malnutrition | |
| Abeta-/hypobeta lipoproteinemia | Antidepressants | ||
| Uncontrolled diabetes |
Steatosis present on abdominal B-mode ultrasonography in the setting of an elevated ALT may lead to diagnosis of NAFLD. However abdominal ultrasonography is not a routine screening tool and is currently not recommended to diagnose NAFLD due to its low sensitivity and specificity in detecting steatosis, particularly in those children who have steatosis in less than a third of hepatocytes. Advanced imaging techniques like ultrasound-based elastography and magnetic resonance-based spectroscopy are used at many centers, including ours, but unfortunately are not widely available (16).
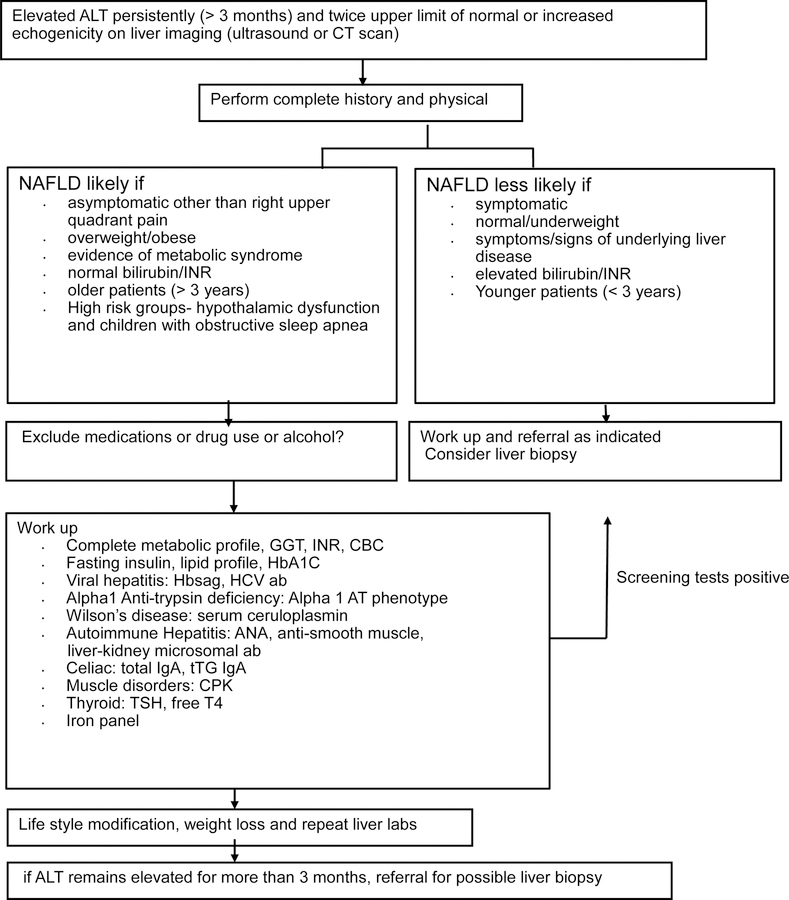
Liver biopsy is currently the gold-standard approach to determine the presence and severity of NAFLD. Liver biopsy is generally safe and but clinical application, and the optimal timing of biopsy has not been firmly established, so the use of biopsies varies among medical centers. In our center, we use liver biopsy to differentiate NAFL from NASH and to exclude the presence of other liver conditions like autoimmune disease, Wilson’s disease, and other metabolic disorders. Our current approach for testing children with nonalcoholic fatty liver disease is summarized in Figure 2.
Figure 2.
our current approach for testing children with non alcoholic fatty liver disease (NAFLD). ALT = alanine aminotransferase; GGT= gamma glutamyltransferase; INR= International normalized ratio CBC= complete blood count; Hbsag= Hepatitis B surface antigen; HCV ab = hepatitis c virus antibody
TREATMENT
The primary goal of treatment in NAFLD is a reduction of steatosis, inflammation, and/or fibrosis. A decrease in ALT at a single point in time does not correlate with the degree of hepatic inflammation, making serum testing inherently unreliable as a means for monitoring a change in the patient’s disease severity (2). However, a study done in adults with nonalcoholic fatty liver disease showed that a decrease in ALT of 10U/L for 96 weeks was associated with 1.28 relative odds of improvement in liver histology and 1.37 relative odds of resolution of NASH (17). Thus, there appears to be some clinical utility for following trends in ALT values over time, through the use of repeated testing.
The staple of NAFLD management is lifestyle and dietary modification. Decreasing sugary beverages and increasing aerobic and resistance exercise have been shown to decrease hepatic steatosis and inflammation (18). Currently there are no medications approved by the Food and Drug Administration (FDA) for the treatment of NAFLD; metformin, vitamin E, docosahexaenoic acid (DHA), and fish oil have not proven to result in significant improvement in hepatic steatosis in the pediatric population (19).
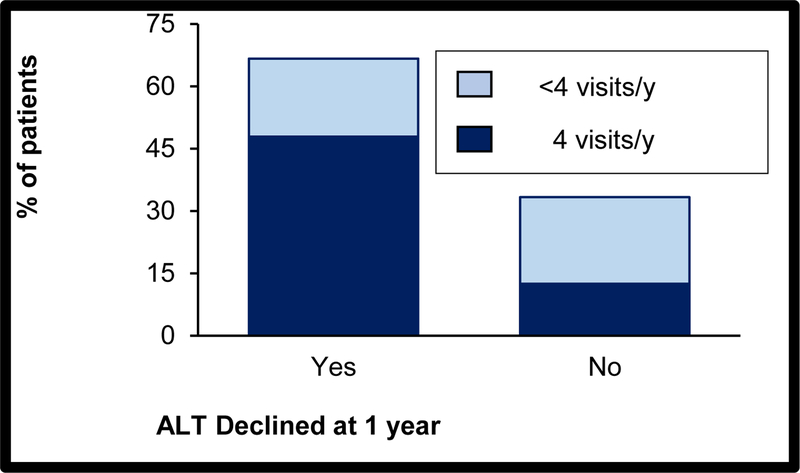
Our center has a dedicated multi-disciplinary NAFLD clinic, which handles more than 250 unique patient visits per year. Since there are no pharmaceutical treatments yet available that directly reduce liver fat or fibrosis, our patients are offered a multi-disciplinary lifestyle improvement program. Patients receive counselling sessions with a registered dietician and a psychologist. We use the “5210 Let’s Go” guidelines, in which patients are advised to consume 5 daily servings of fruits and vegetables, limit non-educational screen time on TV, computer, or mobile devices to less than 2 hours per day, accrue 1 hour per day of moderate to vigorous physical activity, and consume 0 sugar-sweetened beverages. Follow-up visits are scheduled every three months. We annually screen all our NAFLD population for comorbidities like hypertension, dyslipidemia, diabetes, and obstructive sleep apnea. A case series of 48 patients followed for 1 year revealed that 60% met the attendance target and 66% had a decline in ALT (Figure 3). Additionally, bariatric surgery may be considered as an option for morbidly obese adolescents for management of non-cirrhotic NAFLD, comorbidities of sleep apnea, or idiopathic intracranial hypertension, although it is not recommended as a specific therapy for NAFLD. Randomized placebo-controlled trials designed to study therapeutic options have been difficult to perform in the pediatric age group due to the lack of reliable serum biomarkers and a poor understanding of the natural history of NALFD in this age group.
Figure 3.
ALT activity was most likely to decline in children who completed 4 follow-up visits to our fatty liver clinic over 1 year. ALT: alanine aminotransferase.
OUR EXPERIENCE AT THE UNIVERSITY OF OKLAHOMA
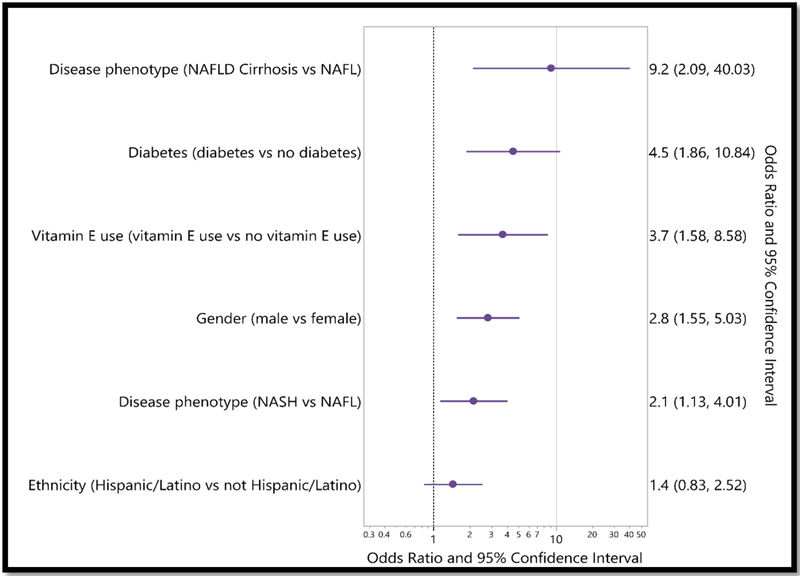
Our center is part of a multi-center longitudinal observational study conducted among pediatric participants (age < 18 years) with NAFLD (20). In this study, approved by our Institutional Review Board, data from medical records including narratives, blood tests, imaging, pathology, procedures, and clinical outcomes are centrally abstracted and monitored. Detailed demographics, patient comorbidities, medications, and disease progression are assessed, as are adverse outcomes. As shown in Table 2, the median age of participants is 14 years, and median BMI is 32 kg/m2. The majority of participants enrolled in this study so far have NASH (72%), with the remainder having either uncomplicated NAFL (24%) or NAFLD-related-cirrhosis (4%). Patient demographics reveal that the majority of patents are male (68%), while Hispanic/Latino is the most common ethnicity (62%). Rates of comorbidities such as diabetes, sleep apnea, hypertension, and anxiety/depression are higher than the general population. Of the 302 children, nearly 34% of them were prescribed medications like metformin and vitamin E. In this pediatric NAFLD cohort, most children (75%) have ALT greater than 70 IU/L and 13% have substantially elevated ALT (> 250 U/L), suggesting that the common perception of low levels of ALT in NAFLD is not reflective of the entire range of disease. Those with high ALT values were more likely to be treated with vitamin E (OR 3.7). It is interesting to note that the high ALT group was more likely to have diabetes (OR of 4.5), suggesting that this may be an important group to target for diabetes screening (Figure 4). Long term follow-up is ongoing in this cohort to determine differences in outcomes for pediatric patients with and without comorbidities and substantial elevations in ALT
Table 2.
showing clinical characteristics based on disease phenotype of participants enrolled in multi-center collaborative study from our center.
| All Participants (302) |
Non Alcoholic Fatty Liver (NAFL) N=73 |
Non Alcoholic Steatohepatitis (NASH) N=218 |
NAFLD Cirrhosis N=11 |
|
|---|---|---|---|---|
| Age at enrollment Median Min-Max |
14 7–19 |
14 7–18 |
14 7–19 |
14 9–16 |
| Gender (female) | 97 (32.1%) | 20 (27.4%) | 72 (33% ) | 5 (45.5%) |
| Ethnicity, n (%) n Hispanic or Latino Not Hispanic or Latino Not Reported Not Available |
302 186 (61.6%) 12(37.1%) 4 (1.3%) 0 |
73 45 (61.6%) 26 (35.6%) 2 (2.7%) 0 |
218 136 (62.4%) 80 (36.7%) 2 (0.9%) 0 |
11 5 (45.5%) 6 (54.5%) 0 |
| BMI at enrollment Median Min-Max |
32.0 17–61 |
31.0 19–56 |
32.0 24–61 |
33.0 27–45 |
| Diabetes | 6.0% | 6.5% | 5.6% | 12.5% |
| Cardiovascular disease | 2.2% | 3.2% | 2.1% | 0 |
| Hypertension | 9.8% | 6.5% | 10.4% | 12.5% |
| Anxiety/Depression | 9.3% | 3.2% | 11.1% | 0 |
| Sleep Apnea | 9.3% | 3.2% | 9.7% | 25.0% |
| Medication: Metformin | 17.1% | 13.3% | 17.1% | 25.0% |
| Supplement: Vitamin E | 17.1% | 6.7% | 17.9% | 25.0% |
Figure 4.
Showing the association of highest ALT level with common risk factors in NAFLD participants enrolled in multi-center collaborative study from our center.
CONCLUSION
NAFLD, a progressive liver disease ranging from hepatic steatosis to fibrosis and cirrhosis requiring liver transplantation, can be a diagnostic and management challenge for both general practitioners and subspecialists. Obesity, male sex, and Hispanic/Latino ethnicity are risk factors in developing NAFLD. Oklahoma children who have some or all of those risk factors are most likely to develop obesity and NAFLD. Successful management of pediatric NAFLD requires that clinicians identify children with the highest risk through early screening, understand the comorbidities, and offer a multi-disciplinary treatment approach that emphasizes diet and physical activity modification and support for parents and families.
Acknowledgement:
Research reported in this publication was supported by the National Institutes of Health under Award Numbers UG1OD024950 and U54GM104938. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest: The authors, Drs. Shakir, Suneja, Short, and Palle have not conflicts of interest
REFERENCES
- 1.Doycheva I, Issa D, Watt KD, Lopez R, Rifai G, Alkhouri N. Nonalcoholic Steatohepatitis is the Most Rapidly Increasing Indication for Liver Transplantation in Young Adults in the United States. J Clin Gastroenterol 2018;52:339–346. [DOI] [PubMed] [Google Scholar]
- 2.Vos MB, Abrams SH, Barlow SE, Caprio S, Daniels SR, Kohli R, Mouzaki M, et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children: Recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J Pediatr Gastroenterol Nutr 2017;64:319–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kabbany MN, Conjeevaram Selvakumar PK, Watt K, Lopez R, Akras Z, Zein N, Carey W, et al. Prevalence of Nonalcoholic Steatohepatitis-Associated Cirrhosis in the United States: An Analysis of National Health and Nutrition Examination Survey Data. Am J Gastroenterol 2017;112:581–587. [DOI] [PubMed] [Google Scholar]
- 4.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics 2018. [DOI] [PMC free article] [PubMed]
- 5.Weedn AE, Ang SC, Zeman CL, Darden PM. Obesity prevalence in low-income preschool children in Oklahoma. Clin Pediatr (Phila) 2012;51:917–922. [DOI] [PubMed] [Google Scholar]
- 6.Weedn AE, Hale JJ, Thompson DM, Darden PM. Trends in obesity prevalence and disparities among low-income children in Oklahoma, 2005–2010. Child Obes 2014;10:318–325. [DOI] [PubMed] [Google Scholar]
- 7.Welsh JA, Karpen S, Vos MB. Increasing prevalence of nonalcoholic fatty liver disease among United States adolescents, 1988–1994 to 2007–2010. J Pediatr 2013;162:496–500 e491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics 2006;118:1388–1393. [DOI] [PubMed] [Google Scholar]
- 9.Louthan MV, Theriot JA, Zimmerman E, Stutts JT, McClain CJ. Decreased prevalence of nonalcoholic fatty liver disease in black obese children. J Pediatr Gastroenterol Nutr 2005;41:426–429. [DOI] [PubMed] [Google Scholar]
- 10.Strauss RS, Barlow SE, Dietz WH. Prevalence of abnormal serum aminotransferase values in overweight and obese adolescents. J Pediatr 2000;136:727–733. [PubMed] [Google Scholar]
- 11.Rehm JL, Connor EL, Wolfgram PM, Eickhoff JC, Reeder SB, Allen DB. Predicting hepatic steatosis in a racially and ethnically diverse cohort of adolescent girls. J Pediatr 2014;165:319–325 e311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLoS One 2015;10:e0140908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, Hultcrantz R. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology 2015;61:1547–1554. [DOI] [PubMed] [Google Scholar]
- 14.Crespo M, Lappe S, Feldstein AE, Alkhouri N. Similarities and differences between pediatric and adult nonalcoholic fatty liver disease. Metabolism 2016;65:1161–1171. [DOI] [PubMed] [Google Scholar]
- 15.Schwimmer JB, Behling C, Newbury R, Deutsch R, Nievergelt C, Schork NJ, Lavine JE. Histopathology of pediatric nonalcoholic fatty liver disease. Hepatology 2005;42:641–649. [DOI] [PubMed] [Google Scholar]
- 16.Ferraioli G, Calcaterra V, Lissandrin R, Guazzotti M, Maiocchi L, Tinelli C, De Silvestri A, et al. Noninvasive assessment of liver steatosis in children: the clinical value of controlled attenuation parameter. BMC Gastroenterol 2017;17:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vuppalanchi R, Jain AK, Deppe R, Yates K, Comerford M, Masuoka HC, Neuschwander-Tetri BA, et al. Relationship between changes in serum levels of keratin 18 and changes in liver histology in children and adults with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 2014;12:2121–2130 e2121–2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van der Heijden GJ, Wang ZJ, Chu ZD, Sauer PJ, Haymond MW, Rodriguez LM, Sunehag AL. A 12-week aerobic exercise program reduces hepatic fat accumulation and insulin resistance in obese, Hispanic adolescents. Obesity (Silver Spring) 2010;18:384–390. [DOI] [PubMed] [Google Scholar]
- 19.Lavine JE, Schwimmer JB, Molleston JP, Scheimann AO, Murray KF, Abrams SH, Rosenthal P, et al. Treatment of nonalcoholic fatty liver disease in children: TONIC trial design. Contemp Clin Trials 2010;31:62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barritt ASt, Gitlin N, Klein S, Lok AS, Loomba R, Malahias L, Powell M, et al. Design and rationale for a real-world observational cohort of patients with nonalcoholic fatty liver disease: The TARGET-NASH study. Contemp Clin Trials 2017;61:33–38. [DOI] [PubMed] [Google Scholar]