Abstract
Background/Objective:
Although there is growing interest in screening for food insecurity in the clinical setting, little evidence exists regarding screening formats that maximize disclosure and caregiver comfort.
Methods:
In this randomized trial, we asked English-speaking adult caregivers of pediatric patients in the ED at an urban, freestanding children's hospital to complete a validated, two-question screen for FI. Respondents were assigned via block randomization to complete the survey by either verbal interview or electronic tablet. Caregivers reported perceived importance of the screening questions, comfort level with screening in the ED or in their child's primary care site, and their preference of screening modality.
Results:
20.6% of the 1818 participants screened positive for FI. There was a significantly higher rate of reported FI for those screened by tablet (23.6%) compared to those screened verbally (17.7%) (p=0.002). Of those who had a preference of screening modality, 83.2% of all participants, and 84.5% of patients reporting FI, preferred tablet-based screen over verbal interview. Overall, more participants reported comfort completing the screen in the ED compared to their child's doctor's office however comfort in both of these setting were rated highly (86.1% vs. 80.2%, p<0.001).
Conclusions:
While both verbal and tablet-based screening modalities were effective in identifying FI, tablet-based screening had a higher disclosure rate and was the participants' preferred screening method. There is a high level of comfort with screening regardless of clinical setting; it is possible that an added level of anonymity in the ED enhanced participants' comfort levels.
Keywords: Food Insecurity, Screening Modality, Social Determinants of Health
Introduction:
Children are disproportionately affected by the rise in poverty rates in the United States. Economic hardships can compromise their development, negatively affect their overall health, and adversely affect their abilities to succeed in school and in life.1-4 Food insecurity (FI)—the limited or uncertain availability of nutritionally adequate or safe foods— while strongly associated with poverty, is an independent predictor of poor health outcomes for children.5,6 FI experienced in childhood is associated with poorer overall heath, increased hospitalizations, and increased rates of anxiety, aggression, anemia, asthma, and cognitive delay, among other health outcomes. 7-13 Unfortunately, a large proportion of American children experience FI, and it often goes unnoticed.14 Currently, food insecurity in Philadelphia county affects 21.7% of children, exceeding the national average of 16.5%.15,16
The Emergency Department (ED) of academic medical centers often serves as a point of care entry for impoverished and high-risk families.17-19 Although there is a growing interest in the healthcare system’s ability to address Social Determinants of Health (SDH), little is known about food insecurity screening in the pediatric ED. The American Academy of Pediatrics and the American Pediatric Association have recommended FI screening in all pediatric settings.20,21 The implementation of these recommendations has been difficult, particularly in the ED, because of medical provider concerns with time, limited knowledge of local resources, and the possibility of patient and provider discomfort in screening.22 Additionally, there are limited data on how to implement FI screening into practice in a way that maximizes elicitation of social need, while assuring patient and family comfort.23
In order to compare modalities for FI screening in the pediatric ED, this prospective randomized study compared face-to-face verbal screening to screening using a tablet computer with an optional audio-assist, applying a validated, two-question screen for food insecurity. We also collected information regarding caregiver comfort with screening by modality and location.
Methods:
Setting, Participants, and Eligibility Criteria
Participants were drawn from a consecutive sample of adult caregivers accompanying pediatric patients in the emergency department of a large, urban children’s hospital in Philadelphia. According to internal review, in 2017 this ED saw 66,952 unique patients over a total of 99,369 encounters; 55% were African American, and 9% Latino; 3% were non-English speaking. Prior to initiation of study procedures, there was no food insecurity screening or referral protocol. Eligibility criteria for participation included English-speaking caregivers presenting with patients age <18 years, in non-critical condition, who were not previously enrolled. Patients triaged to the fast-track, low acuity section of the ED were excluded in order to ensure a representative sample of the general ED patient population.
Study Design and Procedures
This was a prospective, randomized trial comparing verbal and tablet-based screening for food insecurity, and exploring caregiver preferences regarding screening modality and location. Four-hour periods were pre-assigned between the hours of 8am and 11pm, 7 days a week from June-November 2017, for study recruitment. Caregivers were approached in room order (1 through 47), with an attempt to enroll all eligible patients. Patients are randomly allocated to rooms; therefore, the ordinal approach was expected to ensure consecutive sampling while minimizing selection bias. Caregivers meeting eligibility criteria were verbally consented for participation using the language contained in Appendix 1. Consenting participants were assigned to a study group using block randomization that was predetermined and allocated by a computer program (REDCap).24 Participants completed a two-question validated FI screen either by face-to-face interview or via tablet-based self-completed questionnaire with an optional audio assist by text-to-voice functionality. Face-to-face interviews were performed by research assistants with training in medical interviewing techniques. Those randomized to the tablet-based group were given a brief tutorial regarding use of the tablet and text-to-voice functionality. A brief survey assessing comfort and preferences regarding screening location and modality, as well as demographic information, followed the FI screen by the corresponding modality. Questionnaires were completed in individual clinical rooms between medical evaluations, during waiting periods, or after discharge. Identical surveys were used for both arms and were written at the fifth-grade reading level. All study procedures were conducted on a designated study tablet (iPad), with information recorded directly into REDCap. All respondents were provided with a paper-based list of food resources including information regarding federal programs, local emergency food assistance, and free and reduced-price produce by the research assistant following the questionnaire. Participants screening positive for FI were also given the option of direct-contact by a food resource agency that assists with enrollment in federal programs and provides navigation to emergency food assistance after the ED visit; this option was provided at the time of positive screen in the same modality as the remainder of the questionnaire. Per the hospital’s routine protocol, a social worker was always available on premises to assist families by request. All study procedures were deemed exempt from review by the hospital’s Committee for the Protection of Human Subjects.
Measures
Participant Demographics
We collected information on patient age and level of acuity based on the 5-level Emergency Severity Index (ESI) system for each patient.25 Respondents self-reported race and ethnicity.
Food Insecurity Reporting:
We measured food insecurity using the validated two-question “Hunger Vital Sign” screening tool, with yes/no responses.26 These two questions are: within the past 12 months “we worried whether our food would run out before we got money to buy more” and “the food we bought just didn't last and we didn't have money to get more.”
Comfort with Screening Modality
Respondents rated their comfort with this screening process in the Emergency Department and expected comfort level with the same screen in their child’s doctor’s office. Likert scale options were: “strongly disagree,” “disagree,” “neutral,” “agree,” “strongly agree.” Information was not collected regarding current screening practices in the primary care setting. Participants were asked which modality would make them feel most comfortable with the screening questions: “on an iPad/Tablet,” “by talking with a healthcare provider,” or “I would feel just as comfortable with either.”
Data Analysis
Sample size calculation was based on 2-sided Fisher’s exact test comparing two independent proportions with type I error rate of 0.05. With a targeted sample size of 1808, the study had 80% power to detect a 5% difference in the rate of disclosed FI by screening modality. Likert responses were coded in a binary format (“agree” or “strongly agree” vs. any other response) to indicate comfort with screening. Chi-square tests were used to compare tablet-based and verbal screen groups with regard to their comfort level with screening modality and screening location. We also compared these outcomes for those who reported FI and those who did not. Statistical analysis was preformed using SPSS 21.0 and Stata 14.2.
Results:
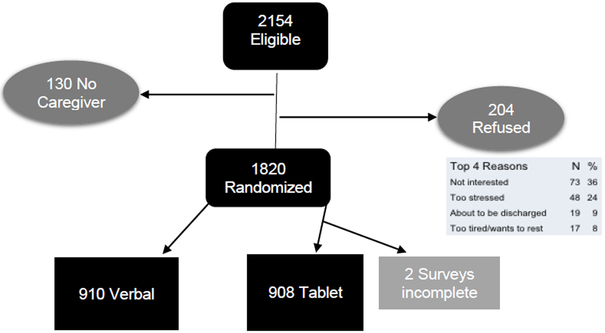
Of 2154 approached patients, 130 were excluded as there was no caregiver present, and 204 (10%) refused. Ultimately 1820 caregivers were randomized, 910 to each group. 2 tablet-based questionnaires (0.2%) were incomplete, leading to an overall response rate of 89.9% of eligible respondents (Figure 1). There were no significant differences between age, race, ethnicity, or triage level of acuity between groups (Table 1).
Figure 1:
Study Flow Diagram
Table 1:
Characteristics of Participants by Study Arm
| Total (N=1818) | Verbal (N=910) | Tablet (N=908) | |
|---|---|---|---|
| Patient Age, Mean (SD) | 10.04 (6.9) | 10.12 (6.9) | 9.96 (6.9) |
| Race, N (%) | |||
| American Indian/Alaska | 16 (0.9) | 3 (0.3) | 13 (1.4) |
| Asian | 73 (4.0) | 39 (4.3) | 34 (3.8) |
| Hawaiian/Pacific Islander | 4 (0.2) | 2 (0.2) | 2 (0.2) |
| Black/African American | 764 (42.0) | 397 (43.7) | 367 (40.5) |
| White | 783 (43.1) | 383 (42.1) | 400 (44.2) |
| More than one | 64 (3.5) | 29 (3.2) | 35 (3.9) |
| Not listed | 111 (6.1) | 56 (6.2) | 55 (6.1) |
| Ethnicity, N(%) | |||
| Hispanic or Latino | 150 (8.3) | 76 (8.4) | 74 (8.2) |
| Not Hispanic or Latino** | 1583 (87.1) | 817 (90.0) | 766 (84.5) |
| Unknown/Not Reported** | 81 (4.5) | 15 (1.7) | 66 (7.3) |
| Level of Acuity, N (%) | |||
| 1 (sickest) | 4 (0.2) | 1 (0.1) | 3 (0.3) |
| 2 | 642 (35.3) | 332 (36.7) | 308 (33.9) |
| 3 | 925 (50.9) | 447 (49.1) | 478 (52.6) |
| 4 | 236 (13.0) | 120 (13.2) | 116 (12.8) |
| 5 (least sick) | 11 (0.6) | 8 (0.9) | 3 (0.3) |
p<0.01,
p<0.05
Of the 1818 participants, 20.6% screened positive for FI. There was a higher rate of reported FI for those screened by tablet compared to those screened verbally (23.6% and 17.7%, p=0.002). There were no significant differences in patient age or level of acuity between FI and non-FI groups. Rates of reported FI were higher among caregivers who identified as Black/African American, Hispanic or Latino, and if race was not listed, or if ethnicity was unknown/not reported. Rates of reported FI were lower among caregivers identifying as White and not Hispanic or Latino (Table 2).
Table 2:
Demographics by Reported FI
| Total (N=1818) | Food Insecure (N=375) | NOT Food Insecure (N=1441) | |
|---|---|---|---|
| Patient Age, Mean (SD) | 10.04 (6.9) | 9.15 (6.9) | 10.27 (6.9) |
| Race, N(%) | |||
| American Indian/Alaska | 16 (0.9) | 5 (1.3) | 11 (0.8) |
| Asian* | 73 (4.0) | 7 (1.9) | 66 (4.6) |
| Hawaiian/Pacific Islander | 4 (0.2) | 1 (0.3) | 3 (0.2) |
| Black/African American** | 764 (42.0) | 236 (69.2) | 528 (36.7) |
| White** | 783 (43.1) | 74 (19.7) | 709 (49.2) |
| More than one | 64 (3.5) | 17 (4.5) | 47 (3.3) |
| Not listed** | 111 (6.1) | 35 (9.3) | 76 (5.3) |
| Ethnicity, N(%) | |||
| Hispanic or Latino** | 150 (8.3) | 51 (13.6) | 99 (6.9) |
| Not Hispanic or Latino* | 1583 (87.1) | 298 (79.7) | 1285 (89.2) |
| Unknown/Not Reported** | 81 (4.5) | 25 (6.7) | 56 (3.9) |
| Level of Acuity, N(%) | |||
| 1 (sickest) | 4 (0.2) | 1 (0.3) | 3 (0.2) |
| 2 | 642 (35.3) | 141 (37.6) | 501 (34.7) |
| 3 | 925 (50.9) | 173 (46.1) | 752 (52.1) |
| 4 | 236 (13.0) | 55 (14.7) | 181 (12.5) |
| 5 (least sick) | 11 (0.6) | 5 (1.3) | 6 (0.4) |
p<0.01
p<0.05
Of the 614 (33.8%) caregivers who expressed any preference of screening modality, 83.2% preferred the tablet-based screen over verbal interview; 84.5% of those with FI reported a similar preference (Table 3). A slightly greater proportion of participants reported comfort completing the screen in the ED compared to their child’s doctor’s office, however comfort in both of these settings was rated highly (86.1% vs. 80.2%, p<0.001). Similar findings were noted for the subpopulation reporting FI (77.6% vs 70.7%, p=0.03) (Table 4).
Table 3:
Screening Modality Preferences by Reported FI (614/1818 (33.8%) of participants reported any preference)
| Verbal | Tablet | Significance | |
|---|---|---|---|
| N (%) | N (%) | P-value | |
| Total with a preference N=614 | 103 (16.9) | 511 (83.2) | p<0.001 |
| Food Insecure N=162 | 25 (15.4) | 265 (84.6) | p<0.001 |
| NOT Food Insecure N=452 | 78 (17.3) | 374 (82.8) | p<0.001 |
Table 4:
Comfort with FI Screen by Location by Reported FI
| ED | PCP | Significance | |
|---|---|---|---|
| N (%) | N (%) | P-value | |
| Total with a preference N=1818 | 1563 (86.0) | 1457 (80.1) | p<0.001 |
| Food Insecure N=375 | 291 (77.6) | 265 (70.7) | p=0.03 |
| NOT Food Insecure N=1441 | 1272 (88.3) | 1192 (82.7) | p<0.001 |
Discussion:
With increasing recognition of the importance of FI and other SDH, there is a growing need for evidence regarding how to most effectively and efficiently identify social risk within medical settings. Maximizing the caregiver comfort and acceptability of screening mechanisms may enhance the accuracy of information collected. Specifically, the perceived anonymity of screening—such as with use of electronic tablet-based self-reporting—may improve disclosure and serve to enhance participant comfort. This study found that there is an overall high rate of acceptability with FI screening in a pediatric ED, and that caretaker comfort levels and disclosure of social risk are higher with tablet-based screening compared to verbal screening.
As FI is a potentially stigmatizing condition, it may elicit concerns regarding social desirability in responses depending on format of screening. In agreement with our study findings, previous studies on intimate partner violence and substance use have shown electronic based screening is acceptable to caregivers, and results in equal or greater disclosures.27,28 Caregivers have reported discomfort in discussing social risk in front of their children, concerns regarding involvement of Child Protective Services upon disclosure of FI, and discomfort with disclosure has been shown to be most prevalent among those with highest social risk.29 Similarly, prior literature has explored provider-level concern regarding FI screening, including patient discomfort or stigmatization and the time and ability to address social risk, once identified.30 Providers have also reported time required for screening as a barrier.31 Tablet-based screening may help ameliorate these concerns, provide similarly accurate responses, and align well with both participant and provider preferences.
Although the majority of the literature regarding social risk screening focuses on routine medical visits, our study demonstrates that the ED is an acceptable screening location and may in fact be preferred by caretakers. We anticipate— similar to the mechanism described above— that the anonymity inherent to being a patient in the ED may serve as a protective factor for families, improving comfort with reporting social risk. This is particularly valuable as families presenting to the ED have a higher rate of social risk and lower access to primary care, in addition to an increased wait time, increasing feasibility of screening as compared to other clinical settings.32,33 Our study showed rates of FI concordant with city-wide reports, along with low non-response and refusal rates, supporting the accuracy and feasibility of screening in the ED and acute care setting.
To our knowledge, this was the first study of FI or SDH screening to be undertaken with the intention to obtain a representative sample of caretakers of pediatric ED patients across all levels of acuity. This allowed us to compare the ESI triage level between patients whose caregivers report FI. Although it is frequently expected that social need such as FI is associated with higher rates of ED utilization for non-urgent complaints,34 the results of our study do not support this notion as we found no difference in rates of FI based on ESI. This suggests the need for universal screening and intervention rather than targeted screening for patients and families who use the ED for non-urgent complaints.
Strengths and Limitations
Our large sample size and randomized design provide rigorous and robust evidence of the relative rates of FI disclosure between verbal and tablet-based screening. The low literacy level of the questions and availability of audio-assist increases the generalizability of our findings, although we did not directly assess education or literacy. Enrollment by pre-selected time-periods and consecutive sampling were undertaken to limit selection bias; ultimately, the study sample reflected a similar distribution of racial and ethnic diversity of our urban ED population.
Limitations of the study include the inability to verify the self-reported data, including actual FI, as well as self-report of race/ethnicity. Although we interpret the higher rates of self-reported FI in the tablet-based format as suggestive of more honest responses, we cannot verify this statement. Future studies might consider a crossover design, with caretakers answering in both formats, however that method may be impractical to perform during a real-time ED visit.
Furthermore, non-English speaking families were excluded from this study due to the low prevalence in our ED population. This patient population may be at particular risk for food insecurity, and we acknowledge that the exclusion of this population limits the generalizability of our results. Further research in a more language diverse patient population is needed to evaluate screening preferences among non-English speaking families.
Additionally, we acknowledge that FI is only one of many Social Determinants of Health. Given that FI has a validated, highly sensitive and specific screening tool, and well-defined local and federal resources (i.e. SNAP, WIC, and food pantries), it was our intention to study FI as a proxy for other SDH. Our data cannot provide definitive evidence for any other Social Determinant.
Finally, this study focuses on the screening process in terms of modality and location, without explicit attention to engagement with resources after screening and referral, and the effect on subsequent FI. We acknowledge that the resources available have limitations in their abilities to meet the needs of families.35 Additional work evaluating the acceptability, feasibility, and effectiveness of interventions to address social needs in clinical settings is needed before we can suggest broad implementation of FI screening practices.
Conclusion:
While both verbal and tablet-based screening modalities were effective in identifying FI, tablet-based screening had a higher disclosure rate and was participants’ preferred screening method in a pediatric ED. This suggests that written, tablet-based screening is a feasible and effective tool that may allow us to streamline routine inquiry into FI and possibly other SDH while improving detection and enhancing patient and provider comfort. While there is a high level of comfort with screening regardless of clinical setting; it is possible that an added level of anonymity in the ED enhanced participants’ comfort levels. We hope that these results help guide the implementation of FI and other social determinants screening and interventions, particularly in the ED setting.
Supplementary Material
What’s New:This study compares food insecurity disclosure rates in face-to-face interviews versus electronic formats, and explores caregiver preferences regarding screening modality and location, in a large, urban pediatric emergency department.
Acknowledgements:
We appreciate the generous funding support of the University of Pennsylvania Leonard Davis Institute of Health Economics and the Ruth L. Kirschstein National Research Service Award (NRSA T32-HP10026). Thank you to Dr. Judy Shea and Dr. Peter Yang for their review of the manuscript. Thank you to Dr. Megan Attridge and Dr. Dori Abel for their efforts in study recruitment. Thank you also to the research coordinators, academic associates, and research group at the Children’s Hospital of Philadelphia.
Funding source:
University of Pennsylvania Leonard Davis Institute of Health Economics
Ruth L. Kirschstein National Research Service Award (NRSA)- T32-HP10026
The funding sources had no role in study design; data collection, analysis, or interpretation; writing of the report, or submission of the article for publication.
Footnotes
Declarations of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Douglas-Hall A, Chau M. Basic Facts about Low-Income Children: Birth to Age 3: National Center for Children in Poverty; 2007. [Google Scholar]
- 2.Shonkoff J, Phillips DA, eds. From Neurons to Neighborhoods: The Science of Early Childhood Development National Research Council and Institute of Medicine. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 3.Frank DA, Casey PH, Black MM, et al. Cumulative hardship and wellness of low-income young children: multisite surveillance study. Pediatrics. 2010; 125(5). [DOI] [PubMed] [Google Scholar]
- 4.Rose-Jacobs R, et al. Household Food Insecurity: Associations with at-risk infant and toddler development. Pediatrics. 2008;121(1):65–72. [DOI] [PubMed] [Google Scholar]
- 5.Ann Sue Anderson, ed., “Core Indicators of Nutritional State for Difficult-to-Sample Populations,” Journal of Nutrition 120 (1990): S1555–1600. [DOI] [PubMed] [Google Scholar]
- 6.Cook JT, Black M, Chilton M, et al. Are food insecurity’s health impacts underestimated in the US population? Marginal food security also predicts adverse health outcomes in young US children and mothers. Adv Nutr. 2013;4(1):51–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook JT, Frank DA, Berkowitz C, et al. Food Insecurity Is Associated with Adverse Health Outcomes among Human Infants and Toddlers J. Nutr 2004. 134: 61432–1438 [DOI] [PubMed] [Google Scholar]
- 8.Gundersen Craig. and Ziliak James P.. "Childhood Food Insecurity in the U.S.: Trends, Causes, and Policy Options." The Future of Children 24.2 (2014): 1–19. [Google Scholar]
- 9.Eicher-Miller HA, Mason A, Weaver C, McCabe G, Boushey C. Food insecurity is associated with iron deficiency anemia in U.S. adolescents. Am J Clin Nutr. 2009;90:1358–71. [DOI] [PubMed] [Google Scholar]
- 10.Skalicky A, Meyers A, Adams W, Yang Z, Cook J, Frank D. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J. 2006;10:177–85. [DOI] [PubMed] [Google Scholar]
- 11.Howard L Does food insecurity at home affect non-cognitive performance at school? A longitudinal analysis of elementary student classroom behavior. Econ Educ Rev. 2011;30:157–76. [Google Scholar]
- 12.Cook JT, Frank D, Levenson S, et al. Child food insecurity increases risks posed by household food insecurity to young children’s health. J Nutr. 2006;136:1073–6. [DOI] [PubMed] [Google Scholar]
- 13.Whitaker RC, Phillips S, Orzol S. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006; 118:e859–68. [DOI] [PubMed] [Google Scholar]
- 14.Hassan A, Blood EA, et al. Youths' health-related social problems: concerns often overlooked during the medical visit. J Adolesc Health. 2013. August;53(2):265–71. [DOI] [PubMed] [Google Scholar]
- 15.Coleman-Jensen Alisha, Gregory Christian, and Singh Anita. Household Food Security in the United States in 2016, ERR-237, U.S. Department of Agriculture, Economic Research Service, September 2017. [Google Scholar]
- 16.Gundersen C, Dewey A, Crumbaugh A, Kato M & Engelhard E. Map the Meal Gap 2018: A Report on County and Congressional District Food Insecurity and County Food Cost in the United States in 2016. Feeding America, 2018. [Google Scholar]
- 17.Baker DW, Stevens CD, Brook RH. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. JAMA. 1994;271:1909–1912. [PubMed] [Google Scholar]
- 18.Pane GA, Farner MC, Salness KA. Health care access problems of medically indigent emergency department walk-in patients. Ann Emerg Med. 1991;20:730–733. [DOI] [PubMed] [Google Scholar]
- 19.Hirshon JM, Morris DM. Emergency medicine and the health of the public: the critical role of emergency departments in US public health. Emerg Med Clin N Am. 2006;24(4):815–819. [DOI] [PubMed] [Google Scholar]
- 20.Promoting Food Security for All Children. Council on Community Pediatrics, Committee On Nutrition. Pediatrics, October 2015. [DOI] [PubMed] [Google Scholar]
- 21.APA Task Force on Childhood Poverty. A Strategic Road-Map: Committed to Bringing the Voice of Pediatricians to the Most Important Problem Facing Children in the US Today. 2013. Available at: www.academicpeds.org/public_policy/pdf/APA_Task_Force_Strategic_Road_Mapver3.pdf.
- 22.Anderson E, Lippert S, Newberry J, et al. Addressing social determinants of health from the emergency department through social emergency medicine. West J Emerg Med 2016;17:487–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torres J, De Marchis E, Fichtenberg C, Gottlieb L. Identifying Food Insecurity in Health Care Settings: A Review of the Evidence. 2017. San Francisco, CA: Social Interventions Research & Evaluation Network; Available online: https://sirenetwork.ucsf.edu/tools-resources/resources/identifying-food-insecurity-health-care-settings-review-evidence. [Google Scholar]
- 24.Harris Paul A., Taylor Robert, Thielke Robert, Payne Jonathon, Gonzalez Nathaniel, Conde Jose G., Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform. 2009. April;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tanabe P, Gimbel R, Yarnold PR, Kyriacou DN, & Adams JG (2004). Reliability and Validity of Scores on the Emergency Severity Index Version 3. Academic Emergency Medicine, 11(1), 59–65. DOI: 10.1197/j.aem.2003.06.013 [DOI] [PubMed] [Google Scholar]
- 26.Hager E, et al. Development and Validity of a 2-Item Screen to Identify Families at Risk for Food Insecurity. Pediatrics. 2010;126(1):e26–32. [DOI] [PubMed] [Google Scholar]
- 27.Gottlieb L, et al. A Randomized Trial on Screening for Social Determinants of Health: the iScreen Study. Pediatrics. 2014;134(6):e1611–1618. [DOI] [PubMed] [Google Scholar]
- 28.Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff S. Families’ health-related social problems and missed referral opportunities. Pediatrics. 2007;119(6):e1332–1341. [DOI] [PubMed] [Google Scholar]
- 29.Barnidge E, LaBarge G, Krupsky K, Arthur J. Screening for food insecurity in pediatric clinical settings: opportunities and barriers. J Community Health. 2017;42(1):51–57. [DOI] [PubMed] [Google Scholar]
- 30.Palakshappa D, Vasan A, Khan S, Seifu L, Feudtner C, Fiks AG. Clinicians’ perceptions of screening for food insecurity in suburban pediatric practice. Pediatrics. 2017; 140(1). [DOI] [PubMed] [Google Scholar]
- 31.Bottino CJ, Rhodes ET, Kreatsoulas C, Cox JE, Fleegler EW. Food insecurity screening in pediatric primary care: can offering referrals help identify families in need? Acad Pediatr. 2017. [DOI] [PubMed] [Google Scholar]
- 32.Berry A, Brousseau D, Brotanek JM, Tomany-Korman S, Flores G. Why do parents bring children to the emergency department for nonurgent conditions? A qualitative study. Ambul Pediatr. 2008;8(6):360–367 [DOI] [PubMed] [Google Scholar]
- 33.Piehl MD, Clemens CJ, Joines JD. “Narrowing the Gap”: decreasing emergency department use by children enrolled in the Medicaid program by improving access to primary care. Arch Pediatr Adolesc Med. 2000;154(8):791–795 [DOI] [PubMed] [Google Scholar]
- 34.Lawson N, et al. The Impact of Well-Child Care Compliance and Social Risks on Emergency Department Utilization. Clinical Pediatrics. 2017;56(10). [DOI] [PubMed] [Google Scholar]
- 35.Gilbert D, Nanda J, Paige D.: Securing the Safety Net: Concurrent Participation in Income Eligible Assistance Programs. Maternal and Child Health Journal 18(3): 604–612, April 2014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.