Abstract
Geographic isolation has long been hypothesized to have a role in the origins and development of mental disabilities. A considerable body of research has established such a correlation. However, study designs have limited researchers’ ability to establish a causal connection and rule out rival hypotheses.
This study, therefore, aims to assess the strength of the geographic isolation - mental disability relationship and to disentangle it from alternative possibilities, namely that it reflects socioeconomic status, social isolation, economic inequality, or reverse causation. The study employs an analysis of variations in the rates of mental disability throughout 2960 U.S. counties using both Census and CDC data. In addition to partial correlation and ordinary least square analyses, the study employs two-stage least squares regression with instrumental variables (2SLS-IV), a procedure that permits resolution of the problem of endogeneity involving the potential effects of unmeasured variables and reverse causation.
Results reveal that the initial bivariate effects of geographic isolation on rates of mental disability are robust after controls for socioeconomic status, income inequality, social isolation, and other predictors are introduced and when tested with the 2SLS-IV procedure. Most variation (54.4%) in county mental disability rates is accounted for by the independent effects of geographic isolation, socioeconomic status, income inequality, and other variables. The results presented, although not conclusive, supports more targeted service planning and more equitable resource investments in rural parts of the United States and other nations.
Keywords: Geographic isolation, Mental disability, Social isolation, Socioeconomic status, Income inequality
Highlights
-
•
Isolation is a moderately strong predictor of mental disability.
-
•
Socioeconomic status has a moderate negative correlation with mental disability.
-
•
Income inequality compounds the effects of isolation and SES on mental disability.
-
•
Most of variation in MI disability rates explained by isolation, SES, and inequality.
The impact of geographic isolation on mental disability in the United States
In recent years a plethora of research results have been reported on the role of socio-cultural and other environmental conditions, particularly socioeconomic status, in the etiology and development of many types of mental illness (Silva, Loureiro, & Cardoso, 2016). Geographic isolation has also been intermittently hypothesized to contribute to elevated rates of mental disorders, yet this body of research, with few exceptions, has not been able to invalidate competing explanations, such as spuriousness and reverse causation. One example involves its potential confounding with socioeconomic status. If geographic isolation generates risks for mental disability, then a range of practical interventions could be further developed for the promotion of mental health in isolated localities. These include group work and community-building interventions, such as psychiatric clubhouses; a variety of networking, outreach, and self-help methods; telehealth services; and basic services such as transportation, especially for those in rural areas (see Holt-Lunstad, 2017; Lubben, 2017).
The current study, thus, aims to disentangle the unique role of geographic isolation in accounting for rates of mental disability in U.S. counties from that of socioeconomic status and related conditions. Despite much to suggest that mental disability by itself can lead to individuals being socially and geographically isolated, this study focuses on the specific effect of geographic isolation on mental disability. To do so, an approach to causal inference known as two-stage least squares regression with instrumental variables (2SLS-IV) (Bowden & Turkington, 1984) is used with national U.S. data from the U.S. Census Bureau and the Center for Disease Control (CDC), that is known to effectively address problems of spuriousness and reverse causation when certain assumptions are met.
Background
Origins
The isolation-mental illness hypothesis was first proposed by Robert Faris in 1934 as part of his study on the role of the cultural environment for persons with schizophrenia. Faris found that social isolation was associated with rates of schizophrenia, but because such social isolation was studied in inner city areas, it was not possible to disentangle this from low social-economic status (see Kohn & Clausen, 1955). Only a handful of studies on isolation have been published since, mostly on its role in the etiology of schizophrenia. During this period, the hypothesis was partially supported by demographic-ecological investigations (Faris & Dunham, 1939; Jaco, 1954), clinical observations (Sullivan, 1953), and experimental studies (Smith, 1962). One early clinical study, conducted by Kohn and Clausen (1955), failed to find evidence for the hypothesis, as the investigators stated that their data led to the conclusion that “social isolation in this early period [early childhood] does not seem to have appreciably influenced the development of the illness.” (p. 271). However, their study, which used a group matched on age, sex, and fathers’ occupation, was small and nongeneralizable with only 58 respondents.
Definition and measurement of isolation
In the years since, research on the isolation-mental disability hypothesis has varied dramatically based on diverse definitions of isolation and mental disability, data sources, and methodologies. The most pertinent such variation has been whether the focus was broadly on social isolation, including related concepts, or more narrowly on geographic isolation, which has primarily involved the degree of physical isolation of local populations, commonly associated with rurality. Whereas this study involves the more easily operationalized concept of geographic isolation, this notion exists as an overlapping condition with social isolation. Social isolation has often been regarded as comprised of both external and internal characteristics such as the objective lack of contacts or exchanges and unhappiness with their quality. In an in depth review of related concepts, Wang et al. (2017) conclude by proposing that social isolation includes the following domains: social network quantity; social network structure; social network quality; appraisal of relationships emotional; and appraisal of relationships resources. The concept has been defined as “a deprivation of social connectedness” (Zavaleta, Samuel, & Mills, 2014).
In contrast to the relational emphasis of the concept of social isolation, the term geographic isolation has often been used to refer to physical separation from others in remote rural areas, often ones delineated by tangible barriers of jungles, rivers, or mountains. For example, Zavaleta et al. (2014) note that the “physical isolation associated with living somewhere remote and ill-served by infrastructure may at times make people feel that their communities’ physical isolation permits the authorities to neglect them with impunity.” (p. 8). While physical isolation certainly does not guarantee the experiential concomitants of social isolation, such as loneliness or alienation, it constitutes an important contributor to such experiences, and can best be regarded as a type of isolation that overlaps with social isolation which can take place also in the midst of crowds. Whereas social isolation has been studied on an individual level through data from interviews or questionnaires, geographic isolation is more commonly investigated through population level indicators. One such recently developed measure uses population density of local and nearby geographic areas, has been successfully validated in the U.S. by Doogan et al. (2018), and will be employed in this study (see Methodology).
The correlation of isolation and mental disability
The professional literature has thoroughly documented the correlation between isolation and the development of mental disability. This research has been reviewed in detail elsewhere, most notably by Leigh-Hunt et al. (2017) who examined 40 systematic reviews of primarily observational studies on the question, including several meta-analyses. The findings suggest that social isolation and loneliness are strongly correlated with poor mental health outcomes, and somewhat more weakly correlated with diminished physical health outcomes. Such correlational findings have been corroborated by several studies of first person accounts. For example, a survey by MIND (2004), a UK mental health advocacy group, found that over two-thirds of people who report experiencing mental distress believe that isolation is often a cause or contributor to their condition (Zavaleta et al., 2014). Similarly, Wang et al. (2017) found that their sample of mental health service recipients reported greater loneliness and smaller social network size than the general population.
Most studies, in contrast to the foregoing, have examined particular mental health conditions that appear to be sequela of social isolation. Among those conditions for which one or more studies have reported a link with isolation are anxiety (Leigh-Hunt et al., 2017; Pate, 2014), depression (Santini, Koyanagi, Tyrovolas, Mason, & Haro, 2015), cognitive impairment and dementia (Cacioppo & Hawkley, 2009; Crooks, Lubben, Petitti, Little, & Chiu, 2008; Pate, 2014), personality disorders (Wang, 2017), psychosis (Horan, Subotnik, Snyder, & Nuechterlein, 2006), and suicidality (Schwarzbach, Luppa, Forstmeier, König, & Riedel-Heller, 2014; Pate, 2014). For example, Fontanella et al. (2015) report that the adolescent and young-adult suicide rate in the United States is almost double in rural than in urbanized areas between 1996 and 2010.
Theoretical explanations of the correlation
Many of those who have reported correlational results have sought to rule out alternative explanations for the relationship, or to provide a plausible theory for it. These include psychological theories, studies of socio-cultural determinants, and proposed economic, geographic, and biological explanations. An example of a psychological theory about intervening processes that could mediate such a relationship, but one that was not supported by the research, was that of Kohn and Clausen (1955) who utilized the psychoanalytical theory that parental over-solicitude produces a “spoiled child syndrome” among offspring, leading to isolation from non-family members. This isolation is believed to lead to persecution, discrimination or exclusion by children outside the family, and eventually to withdrawal and depression when the child's attempts at friendship are rebuffed.
More common have been attempts to interpret and test the isolation-mental disability correlation through the lens of socio-cultural theories and variables. Historically, isolation has been viewed as a by-product of modernity, including growing urbanization that leaves many in rural areas increasingly isolated. This raises the possibility that, given the well-known negative correlation of socio-economic status with mental illness, that low SES may be a precursor to isolation, as low-economic status is found in many rural areas. Surprisingly, this possibility has not been systematically investigated. Researchers report that individuals are increasingly “bowling alone” (Putnam, 2000) or even dying alone (Klinenberg, 2001). These date back to the work of Erik Fromm (1942/2001) who argued that “the modern industrial system affects people in two simultaneous ways: in part, they become more independent, and yet they also become more alone, separate, and isolated” (Zavaleta et al., 2014, p. 21).
A common interpretation of the isolation-mental disability relationship is that isolation undermines the ability of individuals to secure social supports and services, which in turn, cascades into emotional conditions such as depression and anxiety. Wilson pursues this hypothesis in his comment that social isolation is “the lack of contact or of sustained interaction with individuals or institutions that represent mainstream society” (Wilson, 1987, p. 60). Whether lack of supports is a fundamental part of isolation, a result or cause of it, is yet to be clarified. Social ties have frequently been found to be a buffer against stress or anxiety (Leigh-Hunt et al., 2017; Schwarzer, Bowler, & Cone, 2013). Rohde (2016) points out that associations have been found between geographic regions with low social capital and various adverse behavioral tendencies including suicide (Helliwell, 2003), alcohol abuse (Weitzman & Kawachi, 2000), and crime (Buonanno, Montolio, & Vanin, 2009).
Economic explanations of the isolation-mental disability relationship mainly involve the lack of service and health care supports in rural areas, with scant attention devoted to the subsequent impact of such deficits on the rates of mental illness. Two surveys, which investigated the relationship of isolation with service utilization, were conducted in North Carolina (Arcury et al., 2005) and Wisconsin (Tittman, Harteau, & Beyer, 2016). Arcury (2005) investigated the impact of geographic isolation among 1059 respondents in 12 Appalachian communities, using a logistic regression to control for various demographic, social, cultural, and health status factors. Their multivariable model showed that distance to services was important in determining the number of regular health care visits a person had in a year, with greater distance resulting in fewer regular check-up visits. In a smaller survey of 113 rural Wisconsin women, Tittman et al. (2016) also investigated the impact of distance to services and found that the correlation between geographic isolation and overall social support, when controlling for age and socioeconomic status, was not statistically significant. However, when they examined subscales of social support, it was found that geographic isolation was a negative predictor of both belonging support and tangible support. Although no specific studies on the impact on mental health services were located, it is known that rural areas suffer from a lack of mental health services. Such shortages could conceivably play a role in the relationship of geographic isolation and mental disability. Other potentially explanatory economic factors may include issues of economies of scale in funding mental health services in rural areas, levels and types of health insurance coverage, and depressed incomes among those who are socially and geographically isolated, involving growing income disparities.
Particularly neglected have been proposed biological explanations for the isolation-mental disability relationship. These include laboratory findings, genetic studies of geographically isolated populations, and investigations of environmental conditions such as geographic altitude. In a laboratory study of mice, Zelikowsky et al. (2018) found that prolonged social isolation leads to an array of behavioral changes. These include aggressiveness towards unfamiliar mice, persistent fear, and hypersensitivity to threatening stimuli.
Studies of humans have focused on minority populations that are particularly isolated, socially or geographically. Populations such as the Roma in Europe and Bedouins in the Middle East have been known to have high rates of serious mental disability (Hudson & Soskolne, 2012; López, García, & Martí, 2018), which have been attributed to their poverty, marginalization, and geographic and cultural isolation. In addition, Rudan (2006) argues that isolation has an impact on the genetic structure of the isolated population, such as reduction of genetic diversity through genetic drift and increase in consanguinity due to limited mate choice (p. 528).
Several studies in recent years have reported a correlation between altitude and rates of depression and suicidality in the United States. Such a finding may potentially account for the impact of geographic isolation, due to an association of altitude with rural communities. The researchers theorize that hypoxia, or a deficiency in the amount of oxygen reaching the tissues, influences the body's metabolism of serotonin, a neurotransmitter related to aggressive behavior and suicidality. Several studies suggest that chronic hypoxia increases mood disturbances, especially in patients with emotional instability. Thus, it is plausible that there are multiple pathways through which psychological and socio-cultural conditions involving geographic isolation influence the development of various mental disabilities.
The range of sociocultural and other conditions impacting the development of mental illness, sometimes through social isolation, is reflected in the conclusion of a systematic review of 150 studies on socioeconomic and economic risk factors of mental illness. Silva et al. (2016) report that the main individual factors found to have a statistically significant association with worse mental health are low income, not living with a partner, lack of social support, female gender, low level of education, low socioeconomic status, unemployment, financial strain, and perceived discrimination. The authors conclude this review by arguing that ameliorating the economic difficulties of individuals, enhancing community connectedness, and combating neighborhood disadvantage and isolation may improve a population's mental health (Silva et al., 2016).
The question of time order and causal impact
With rare exceptions, the body of research on the isolation-mental disability relationship has not been able to establish that social isolation precedes the development of mental disability and has a causal impact. This research has mostly involved cross-sectional surveys that examine the effect at a single point in time, thus, the alternative hypothesis that mental disability leads to social isolation cannot be eliminated. A true experiment that can test such hypotheses is not possible. Cross-sectional multivariable studies can control for many alternative explanations, but inevitably there are many that are not included. Some longitudinal and other quasi-experimental designs can eliminate the possibility that reverse causation and unmeasured variables explain the observed effect, most notably, the use of instrumental variables through two-stage least squares regression, an established procedure common in econometrics. Two such projects have been conducted, most notably one undertaken by Rohde, D’Ambrosio, Tang, and Rao (2016) who utilized Australian panel data to examine the impact of isolation on psychological well-being using a natural source of random variation, namely, those who have been forced to relocate due to work or school. They found that the resulting isolation had negative consequences for well-being, particularly among women and older adults. They tested the assumptions associated with their use of several instrumental variables and found that these results were robust, and capable of supporting the estimate that a 10% reduction in social isolation would enable a $3 billion AUD reduction in Australia's mental health budget.
Similarly, Sironi and Wolff (2018) used the seventh round of the European Social Survey to investigate, using instrumental variables, the impact of isolation on subjective health appraisals. The instrumental variables employed consisted of minority status and a history of serious family conflicts. The study supported the conclusion that changes in social isolation have a causal impact on subjective general health.
Conclusion and study hypotheses
Thus, while evidence for the correlation of geographic isolation with several types of mental disability is strong, evidence that such a correlation includes the specific causal impact of social isolation needs to be further investigated. For this reason, continued research on the impact of geographic isolation needs to concentrate on disconfirming the possibility that the relationship is entirely due to the symptoms of mental disability and other conditions, such as socio-economic status. In addition, studies that address this possibility have not been conducted in the U.S., nor have generalizable studies been conducted on an entire nation which also examine the issue of the potential spuriousness involved in the isolation-mental disability hypothesis. For these reasons, the current study will test the following hypotheses:
-
1.
That the greater the geographic isolation of U.S. counties, the higher will be the rates of mental disability;
-
2.
That the socioeconomic status of counties will have an independent negative correlation with levels of mental disability;
-
3.
That the level of income inequality of U.S. counties will be positively correlated with levels of mental disability;
We expect that the combined impact of geographic isolation, low SES, income inequality, and other selected sociodemographic conditions, will account for at least a moderate proportion of variation in indicators of mental disability in U.S. counties.
Methodology
Overview
To test this study's hypotheses, a secondary analysis was conducted using data from the U.S. Census and other governmental sources. After indices were computed for variables of interest, including county geographic and social isolation, socioeconomic status, and income inequality; preliminary exploratory and descriptive analyses were completed. The hypotheses were initially tested using linear regression analyses through SPSS 25.0, and then using StataMP 13.0. Because the traditional OLS analyses cannot disconfirm the threats of endogeneity involving the effects of unmeasured variables or reverse causation, the final analysis undertaken here employed two-stage least squared regression with instrumental variables (2SLS-IV). This procedure, now well established in econometrics, has the advantage of isolating a subset of variation in the endogenous independent variables (i.e., geographic isolation) that can be said to be randomly allocated by the conditions or processes represented by the instrumental variables. Assuming appropriate instruments, the approach effectively discards all other variation in the independent variable, including the undesirable variation caused by the dependent variable and some unobserved confounder variables. The 2SLS-IV procedure, thus, capitalizes on the effects of one or more instrumental variables on the endogeneous predictor, that are not otherwise correlated with either the error term or the dependent variable, mental disability, simulating the effects of a controlled experiment with random assignment (Rose & Stone, 2011). Since this project employed aggregated census and related data, and did not include any on individual human subjects, human subjects approval was not required.
Variables and data sources
All variables used in the analysis constituted rates or other indices descriptive of the range of U.S. counties and their populations. These variables are listed in Table 1, along with their sources.
Table 1.
Univariate statistics for key variables.
| Variable | Valid N | Mean | Median | SD |
| Proportion mentally disabled, 2000a | 3136 | .048 | .046 | .012 |
| Poor mental health daysb | 3014 | 3.804 | 3.773 | .466 |
| Frequent mental distress (% frequent)b | 3014 | 11.592 | 11.486 | 1.502 |
| Suicide rate, smoothed for 2008–2014c | 3136 | 12.501 | 12.053 | 3.535 |
| Geographic isolation indexd | 3137 | 5.211 | 4.969 | 1.678 |
| Social isolation indexa | 3014 | .007 | .026 | .381 |
| Index of county socio-economic statusa | 3137 | .577 | .534 | .639 |
| Income inequality indexb | 3014 | 4.763 | 4.702 | .767 |
| Mean elevation in feete | 3137 | 851.091 | 628.478 | 1155.650 |
| Mental health providersb | 3000 | 216.519 | 194.197 | 143.059 |
| Percent white (non-Hispanic)a | 3014 | 17.373 | 10.217 | 17.112 |
| Proportion living out of county 5 yrs earlier a | 3136 | .212 | .205 | .074 |
| Residential white/non-white segregation indexa | 3000 | 37.832 | 35.836 | 11.727 |
| Instruments | ||||
| Air pollution particulate matterb | 2993 | 10.026 | 9.900 | 1.916 |
| Proportion county that is watera | 3136 | .102 | .029 | .157 |
| Proportion driving alone to workb | 3014 | 76.607 | 79.459 | 11.926 |
NOTES: Weighted by relative county population.
U.S. Census (2000). STF-3 Datafile. Downloaded from “FTP Download” https://www.census.gov/census2000/sumfile3.html.
Robert Wood Johnson Foundation. (2018). County Health Rankings and Roadmaps. State Rankings Data & Reports. Downloaded fromwww.countyhealthrankings.org/explore-health-rankings/rankings-data-documentation.
Center for Disease Control. WISQARS (2008–2014), Fatal Injury Mapping. Downloaded from: http://wisqars.cdc.gov:8443/cdcMapFramework.
Doogan, N.J., Roberts, M.E., Tanenbaum, E.R., Mumford, E.A., & Stillman, F.A. (2017). Validation of a New Geographic Isolation Scale and Urban-Rural Continuum. (2018, in press). Social Science & Medicine, Data file provided by N.J. Doogan.
United States Board on Geographic Names. (2018). States, Territories, Associated Areas of the United States. Datafile: NationalFile_20180801.zip, downloaded from https://geoname.usgs.gov/domestic/download_data.htm.
SOURCES:
Dependent variable
The key dependent variable of the study, mental disability, involves the aggregated responses from a question in the long-version of the 2000 U.S. Decennial Census involving a mental disability, as perceived by the respondent, in each of the family members inquired about. Specifically, the census taker, using the long-form, asks about the presence of a physical, mental, or emotional condition lasting six months or longer involving a difficulty in learning, remembering, or concentrating. Because this is broader than many traditional definitions of mental disability which have focused on mental illness, especially in that it includes physical problems affecting cognition, its validity as a measure of mental disability was investigated using other indicators of the variable. This item was found to have a strong correlation with two items, both on the county level, from the CDC's behavioral health survey: (i) Number of mentally unhealthy days in the previous month (r = 0.725; p < .001), and (ii) Number of days the respondent reported frequent mental distress (r = 0.743; p < .001).
In addition, this same census measure of mental disability was found in previous research (Hudson, 2009) to be strongly correlated with estimates of serious mental illness derived, using small area estimation (SAE) methods, from the National Comorbidity Study-Replication (NCS-R) (Kessler, Chieu, Demler, & Walters, 2005) for U.S. states and the towns and cities of Massachusetts. Given this earlier validation, the data on the census mental disability item was adopted for this study as the best available county-level measure of mental disability. The U.S. Census Bureau reports totals for such individuals for each U.S. county (Summary Level 050), including frequencies for gender and age subgroups. The total of these subgroups was calculated for each county, and divided by the corresponding population denominator to give a proportion of the population with a mental disability.
Independent variables
The primary predictor investigated in this study is the level of geographic isolation of each U.S. county. It employs a scale of geographic isolation that was developed and validated by Doogan et al. (2018). Isolation is measured at the Census tract level, and it is a function of the population density of the tract and its neighbors while accounting for the distance to those neighbors. All well-known measures of rurality used in US research are based on similar continuous underlying conceptualizations of distance-to-population. Doogan and colleagues bypass the issue defining rurality by developing a measure that continuously quantifies a reasonable conceptualization of distance-to-population and stopping there, allowing researchers to define rurality, if they so choose, according to their research needs. Their validation study showed that this approach, compared with rural classification approaches, is superior at explaining the geographic distribution of some health related resources and key health outcomes (Doogan et al., 2018). In this study, we are interested in the effect of geographic isolation, and no particular threshold thereof, making it an ideal measure for our purpose. Because geographic isolation was measured on the census tract level when originally developed, the measure was aggregated to the county level for the current study, based on its component census tracts, with each census tract isolation score weighted by its proportion of the county's population.
A closely related measure of isolation used as a control variable in this study, is social isolation, conceptually defined as the relative level of active social relationships among the county's population. As a proxy measure or index, it was calculated using several indicators from the CDC and the U.S. Census: Percent of Youth Disconnected, percent who drive alone to work; proportion of single person households; and proportion linguistically isolated. These measures were converted to z-scores, and then averaged to form a single social isolation score for each county.
One of the most important control variables for this study is the socioeconomic status (SES) of each county. This was computed based on a measure developed as part of an earlier study (Hudson, 2005) that used the mean household income, educational attainment, and occupational status as indicators of SES. Occupational status was calculated as a weighted average based on the relative size of each of the census-defined occupational groups, multiplied by the reported occupational status score for each of these groups as determined by an earlier national survey (Davis, Smith, Hodge, Nakao, & Treas, 1991).
Another important variable is income inequality, given its likely effects on mental health as indicated by the work of Richard Wilkinson (2005). The level of income inequality for each U.S. county was measured using the ratio of the household income at the 75th percentile and the 25th percentile, as reported by the Robert Wood Johnson Foundation's County Health Rankings and Roadmaps (2018).
Finally, because prior research indicated geographic altitude to be predictive of suicide rates (Brenner, 2006), mean county altitude was included and was calculated by the mean measured altitudes of each populated place within the county, obtained from the USGS places database (2018). Overall, each county had a mean of 61.8 such data points, ranging from 1 to 3672.
In order to control for the mean length of time each resident has lived in a county, and thus has potentially been influenced by its level of geographic isolation and related conditions, a measure of social mobility was calculated from U.S. Census data. This is simply the proportion of the county's population that had lived outside of the county five years earlier (the higher the mobility, the less this effect might be expected).
Instrumental variables
The final analysis undertaken in this study, 2SLS-IV, requires the identification and use of one or more variables predictive of each independent variable that is believed to be subject to endogeneity error. Towards this end, a search of potential county measures from the Census and CDC revealed three variables which not only have a potential impact on geographic isolation but no known connection with rates of mental disability. These variables are the proportion of each county's land area which is water (US Census, 2000), proportion of people who drive alone to work and air pollution (RWJ, 2018). Pearson correlation coefficients were used to investigate the relationship of these instrumental variables with geographic isolation and mental disability. Each were found to have a moderately strong relationship with geographic isolation (respectively: r = -.315, .554, & −0.322; p < .001).
Population sample
The units of analysis are U.S. counties and county-equivalents in the 50 states (and DC), excluding those in U.S. territories. They also exclude a small number of counties with missing data on any of the key variables. The number of counties with complete data ranged between 2993 and 3137 (or between 95.3% and 99.9%) of the 3142 total counties depending on the particular variable considered. The regression analyses employed listwise deletion of missing data which resulted in a 5.64% reduction in the number of available counties in the OLS and 2SLS-IV analyses. Also, because the various rates and indices all ultimately involve an aggregation of individual risks or other individual variables, each county in the various analyses was weighted by its relative population size.
Analysis
Preparation of the data included aggregation of the isolation and suicide measures to the county level; merging of the various data files through use of the state and county FIPSs codes; and computation of the county level indices. Preliminary descriptive statistics, both univariate and bivariate were reviewed to check assumptions for non-normality and multicollinearity, and including bivariate examination of the suitability of various potential predictors for multivariable analyses. In addition, several partial correlation analyses were undertaken as a preliminary exploration of the isolation-mental disability relationship and whether it would be explained away by key control variables, and to test for violations of assumptions central to the 2SLS-IV procedure. Other preliminary analyses included testing for differences between counties with complete versus incomplete data. To establish a baseline for comparison with 2SLS–IV results, an initial OLS regression was conducted, with estimation of standardized regression coefficients in both cases. After exploratory analyses, variables with p > .05 and with partial coefficients < .10 were dropped from the final OLS regression and the subsequent 2SLS-IV procedure. The level of multicollinearity of the predictors was checked by examining both the tolerance ratio, which was no less than the standard of 0.2 (Menard, 1995), and the Variance inflation factor (VIF), which did not exceed the standard of 5 (Ringle, Wende, & Becker, 2015). The 2SLS-IV procedure was implemented using the IVREGRESS procedure in StataMP 13.0. The first stage of this procedure calculated the overall contributions of the instrumental variables, as well as the other predictor variables, to accounting for variation in the endogeneous variable of interest, in this case, geographic isolation, using the R2 statistic. The resulting coefficients for the predictors were then used by the algorithm to calculate corrected values for the endogenous variable, geographic isolation, for each case, and this new variable is then employed in the second stage regression, including the other predictors, to account for its unique effects on levels of mental disability. The suitability of the first stage predictors was evaluated primarily through the F test, which was substantially over the recommended minimum threshold of 10–12. Other potential tests of assumptions, such as the Sargan-Hansen test for overidentification were not computable through the Stata IVREGRESS algorithm, given that it had not been developed to take into account the data weighting that was used in this study.
Results
Hypothesis 1
The central hypothesis of this study is that the greater the geographic isolation, the higher will be the levels of mental disability. The zero-order relationship of the county geographic isolation index and levels of mental disability was initially examined, with isolation found to have a moderately strong positive correlation with the rates of mental disability (r = .369; p < .001) (see Table 2 ). Levels of mental disability ranged from 4.71% of the population in the 10 percent of the counties with the lowest mean geographic isolation, to 5.99% in the counties in the highest decile of geographic isolation, with rates progressively increasing to this level.
The supplemental indicators of mental disability were included in the bivariate analyses, with all displaying a similar pattern. The correlation of the mean number of poor mental health days with isolation was very strong (r = 0.725; p < .001), though modest in its impact as there was a low mean of mental disability of 3.673 in the least isolated counties which rose to 4.072 in the most isolated decile. Similarly, the percentage of the population with frequent mental distress correlated also at a strong level with isolation, ranging from 11.133 in the least isolated decile of counties to 12.641 in the most isolated decile. The correlation of isolation with suicide rates was only found to have a moderately strong and positive correlation (r = 0.371; p < 001), but very strong in its potential effect, with a mean suicide rate ranging from 8.172 in the least isolated counties, to 15.721 in the most isolated decile.
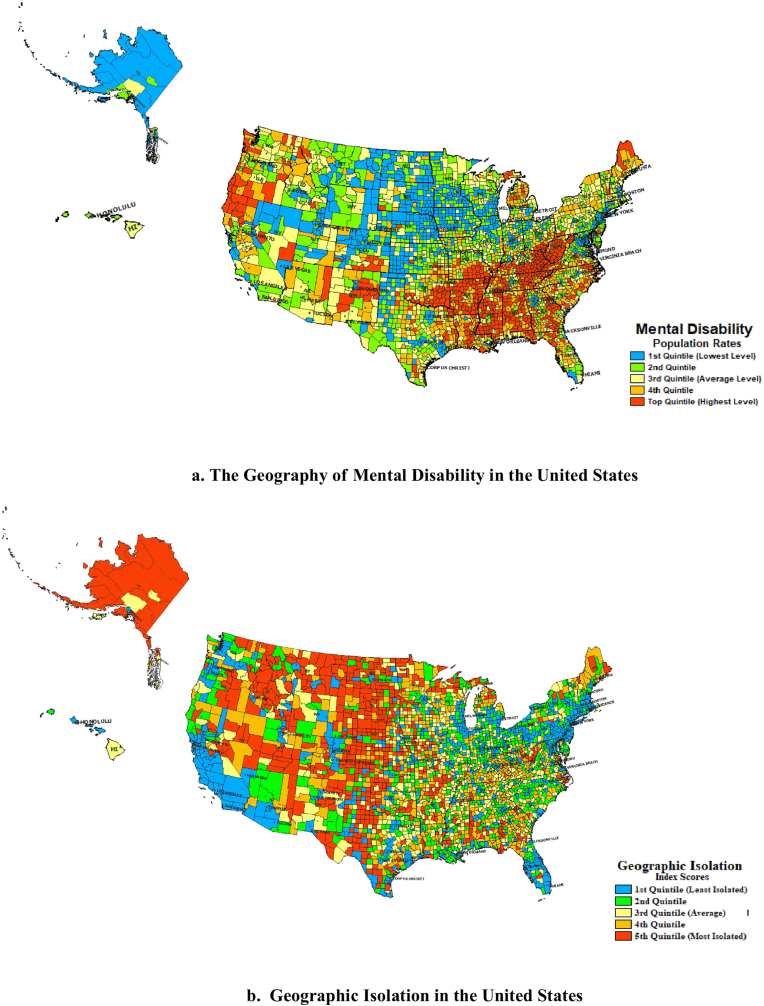
A visual examination of the geographic distribution of the rates of mental disability and isolation, in both cases broken down into quintiles, reveals partially overlapping yet distinct geographic patterns. Fig. 1a reveals the greatest levels of mental disability (in red) throughout the Appalachian region and Southeast, parts of the southwest, upper Pacific coast, and northern Maine and Michigan, with the lowest levels in the Northeast corridor, Alaska, southern Florida, and upper Midwest (in blue). In contrast, Fig. 1b, which maps the levels of isolation, reveals moderate to high levels in the southeast, high levels in the west, and Alaska, with low levels in the northeast corridor, upper Midwest, southern Florida, and the Southwest and Pacific. Thus, it is apparent that there is modest positive relationship of isolation and mental disability, suggested by the juxtaposition of these two maps, as well as the significant and moderate correlations with mental disability and distress.
Hypothesis 2
A competing hypothesis is that it is not geographic isolation per se, but relatively lower levels of socioeconomic status in isolated areas that account for the apparent effect of geographic isolation. Just as the association of low SES with mental disability has been established in scores of previous studies (Dohrenwend et al., 1992), low SES is also found, as revealed by this study's data, to be associated with geographic isolation at a moderate level. For this reason, this study hypothesizes that the isolation-mental disability relationship will only partially be accounted for by controls for socioeconomic status.
Hypothesis 2 was provisionally tested through a partial correlation analysis, one that also considers the possibility that it is not so much geographic as social isolation that contributes to relatively high levels of mental disability. Higher levels of social isolation in urban areas may very well counteract the impact of geographic isolation in rural areas. Table 3 reveals that whereas the moderate geographic isolation-mental disability relationship has a zero-order correlation of 0.356 (p < .001), when SES is controlled for, this relationship is only partially accounted for, leaving a weak effect of .139 (p < .001) still unexplained. In contrast, the partial correlation analysis with control of social isolation introduced suggests that indeed this relationship had been camouflaged by this type of isolation, since with this control introduced, the geographic isolation-disability relationship increases to .446 (p < .001). Finally, when the controls for both social isolation and SES are introduced, a significant portion the impact of geographic isolation on mental disability remains at a low moderate level of 0.222 (p < .001), providing significant yet provisional support for Hypothesis 2.
Hypothesis 3
The study tested whether economic inequality, measured by the difference between the income of those at the 25th and 75th percentiles, is positively associated with the rate of mental disability in U.S. counties. In all cases, this association was found to be statistically significant. Whereas its zero-order Pearson correlation, without controls for additional variables, was found to be r = .241 (p < .001), when controls for the various other predictors considered are included in the OLS and the 2SLS-IV regressions, the effect is found to be at a moderate level of ß = .326 (p.001) and ß = .327 (p < .001), respectively(see Table 2 and Table 4).
Fig. 1.
a. The Geography of Mental Disability in the United States, b. Geographic Isolation in the United States.
Table 3.
Partial Correlations between Mental Disability and. Geographic and Social Isolation, Controlling for Socioeconomic Status.
| Zero-order correlation of mental disability and geographic isolation | .356* |
| With control for social isolation only | .446* |
| With control for socioeconomic status only | .139* |
| With control for both socioeconomic status and social isolation | .222* |
NOTES: Correlations are Pearson coefficients. Data weighted by relative county population. Listwise n = 3010.
*p < .000.
Table 2.
Zero-order correlations of rates of mental disability. Indicators of mental illness and key predictors.
| Variable | Valid N | Pearson r | pa |
|---|---|---|---|
| Indicators of Mental Illness | |||
| Poor mental health days | 3014 | .725 | .000 |
| Frequent mental distress (% frequent) | 3014 | .743 | .000 |
| Suicide rate, smoothed for 2008–2014 | 3135 | .371 | .000 |
| Key Predictors | |||
| Geographic isolation index | 3136 | .369 | .000 |
| Social isolation index | 3014 | .440 | .000 |
| Index of county socio-economic status | 3136 | -.572 | .000 |
| Income inequality index | 3014 | .241 | .000 |
| Mean elevation in feet | 3137 | -.037 | .020 |
| Mental health providers | 2999 | -.029 | .053 |
| Percent white (non-Hispanic) | 3014 | -.180 | .000 |
| Proportion living out of county 5 yr earlier | 3136 | -.287 | .000 |
| Residential white/non-white segregation index | 2999 | .029 | .053 |
NOTES: Weighted by relative county population.
One tailed F test used.
Table 4.
Regression of Mental Disability Rates, on Geographic Isolation and. Other Predictors, Using OLS and 2SLS (n = 2960).
| Variables | Ordinary Least Squares (OLS) |
Two Stage Least Squares, with Instrumental Variables (2SLS-IV) |
||
|---|---|---|---|---|
| Beta | p | Beta | p | |
| Endogenous Variable | ||||
| Geographic Isolation | – | – | .370 | .000 |
| Independent Variables | ||||
| Constant | .000 | 5.91e-15 | .000 | |
| Geographic isolation | .165 | .000 | – | – |
| Social isolation | – | – | – | – |
| Index of county SES: Occupational status, education, income--mean Z-score | -.588 | .000 | -.490 | .000 |
| Income inequality--Income ratio | .326 | .000 | .327 | .000 |
| Population Non-Hispanic white--percent | -.338 | .000 | -.172 | .000 |
| Population Hawaiian/other Pacific Islander – percent | .141 | .000 | – | – |
| Mental health providers--rate | .142 | .000 | .190 | .000 |
| Proportion living out of county five years earlier | -.154 | .000 | -.126 | .000 |
| Residential segregation non-white/white index | -.108 | .000 | – | – |
| Instrumental Variables: First Stage Statistics, Instrumental Variables -- | ||
|---|---|---|
| Air pollution particulate matter | ||
| Proportion county that is water | ||
| Proportion driving alone to work | ||
| R2 | – | .677 |
| R2 Adjusted | – | .676 |
| F | – | 180.371 |
| Significance | – | .000 |
| Shea's Partial R2 | .166 | |
| Shea's Partial R2 Adjusted | .164 | |
| Goodness of Fit Statistics | ||
| R | .767 | .738 |
| R2 | .588 | .544 |
| R2 Adjusted | .587 | |
| df | 8, 2960 | |
| F | 528.566 | |
| Wald | 3289.040 | |
| Significance | .000 | .000 |
NOTES: OLS calculated with SPSS 24.0 and 2SLS-IV with StataMP 15.0. Data weighted with relative population size. Only predictors with significant and non-negligible effects were retained in the final OLS and 2SLS-IV models.
Overall
Finally, the study hypothesizes that the combined impact of geographic isolation, low socioeconomic status, and other selected sociodemographic predictors such as social isolation and income inequality, will account for at least a moderate proportion (30%–60%) of the variation in mental disability in U.S. county populations. Specifically, it is hypothesized that there is an independent causal effect of geographic isolation on rates of mental disability, over and above other measured and unmeasured variables, including the possibility of a reverse effect of mental disability in causing individuals to become isolated. These possibilities are tested first with ordinary least squares (OLS) regression to provide a baseline for comparison, and finally with two stage least squares regression with instrumental variables (2SLS-IV) to consider the possibilities of unmeasured variables and reverse causation.
Both the OLS and the 2SLS-IV regressions account a similar overall level, over half, of variation of mental disability, respectively 58.8% (R2 = 0.588; F = 528.566; p < .001) and 54.4% (R2 = 0.544; Wald = 3289.040; p < .001) (see Table 4). Whereas the OLS procedure indicates that the effect of geographic isolation has a ß of only 0.165, the 2SLS-IV procedure reveals a moderately strong effect of 0.370 as the independent effect of isolation on mental disability. For each standard deviation increase in isolation, there is a 0.37 SD increase in the level of mental disability. SES clearly does explain away the isolation effect, even partially, as suggested by the OLS procedure; instead the negative effect of SES is reduced, but only slightly from −0.588 to −0.490 when isolation and the other variables and reverse causation are controlled for.
In both analyses, income inequality has a moderately strong effect, over and above SES and isolation, in accounting for mental disability rates (ß = 0.326 & 0.327; p < .001). For each SD increase in income inequality, there an increase of 0.33 SD units in levels of mental disability (ß = 0.33). The effect of rates of available mental health providers was also found, in both analyses, to have a weak but positive and significant association with mental disability. Specifically, for each increase in a standard unit of mental health providers, there is a corresponding increase of 0.190 such units of mental disability (ß = 0.190; p < .001). Among the measured predictors, the proportion of the population county that is white (non-Hispanic) and the proportion which lived out of the county five years earlier in both cases are associated with lower levels of mental disability, but only at a weak level (ß = −0.328 & −0.178; p < .001). Because it was only possible to introduce instrumental variables for geographic isolation, and not the other measured predictors, it is not possible to discount the possibility of other unmeasured variables or reverse causation accounts for the effects of these variables. Since the instrumental variables and other predictors (see Table 4) accounted for 67.7% (R2 = 0.677; p < .001) of the variation in geographic isolation, with an F score of 180.371, there is clear evidence that the assumption, essential to the first stage of the 2SLS-IV procedure, that the three instruments substantially account for the predictor of interest, geographic isolation, is met. Thus, it is unlikely that there are other unmeasured variables or reverse effects that this procedure has not controlled for.
Discussion
This study has uncovered substantial evidence supporting the hypothesized effect of geographic isolation on rates of mental disability in U.S. counties. This effect is supported not only by the preliminary correlational analyses, but most importantly, by the two stage least squared procedure with instrumental variables that disconfirms that unmeasured variables or reverse causation explain away the effect of geographic isolation. Thus, the effect of isolation on elevating levels of mental disability proves to be robust. This finding, however, does not minimize the role of many other conditions in the genesis of mental disability in the U.S. Nor does it negate the reverse possibility that some types of mental disability also lead people to isolate themselves, as both possibilities may certainly co-exist.
Multiple interpretations of the isolation-mental disability relationship are possible. It is, however, clear from this analysis that whatever the contributions of social isolation, low socioeconomic status, formal mental health services, or the impact of income inequality may be, that geographic isolation has a unique effect over and above these and other conditions. Perhaps one of the most salient interpretations is that proximity to others and availability of social relationships has a pervasive prophylactic effect in minimizing the risk of mental disability either in its genesis or its development or both.
The final model tested explains more than half (54.4%) of the variation in mental disability levels, with just under a half unexplained. The 2SLS-IV procedure used strongly supports the inference that this unexplained variation involves either random effects, or effects that do not explain away the specific role of geographic isolation and mental disability levels. This model replicates several important findings from previous research on the isolation-mental disability relationship (Rohde, 2016; Silva, 2016; Sironi & Wolff, 2018), as well as the negative effect of socioeconomic status on mental disability (Hudson, 2005), as well as an independent effect of income inequality on mental disability levels (Wilkinson, 2005).
The contributions of the remaining control variables to explaining mental disability levels have less obvious interpretations. That an important indicator of mental health service availability – rate of mental health professionals – is positively predictive of mental disability levels is not surprising. Perhaps the most compelling interpretation of its positive relationship is that mental health professionals gravitate toward areas with higher levels of mental disability, notwithstanding their often cited scarcity (HRSA, 2005; NCBH, 2017) in rural areas. An alternative interpretation is that there may be enhanced awareness of mental health disabilities when there are a greater number of mental health professionals available to diagnosis them.
Also relevant are variables that did not contribute significantly to levels of mental disability as expected. Mental disability, unlike suicide rates (Brenner, 2006), was not found to be predicted by altitude, perhaps because the earlier research on the effect of altitude on suicide rates only used data aggregated to the state and not county level. Although social isolation did have a moderately strong positive effect in the zero-order analyses on mental disability levels, this effect was explained away in both preliminary OLS and 2SLS-IV regressions, and thus, was not included in the final model, perhaps due to the more powerful effect of the other predictors that were modeled.
A limitation of this study is that there is no available ‘gold standard’ measure of mental disability or mental illness, available for U.S counties and that has been fully validated with established reliability. So instead, this study used an alternative strategy involving the use of a proxy census item that has been partially validated through its correlation with the three other indicators of mental disability reported by the CDC and with previous results from a study that employed the WHO-CIDI instrument (see Methodology). Because instrumental variables were not available for predictors other than geographic isolation, it has not been possible to entirely rule out alternative explanations for these predictors, including reverse causation. The 2SLS-IV regression requires adherence to the procedure's assumptions, namely that the instrumental variables are correlated with the predictor(s) of interest, in this case geographic isolation, but not the residual error term. While the high F score for the first stage clearly supports the first assumption; and the bivariate correlations provide only partial support for the second assumption; there is no means to fully discount the possibility of correlation of geographic isolation with the error term. Also, some tests of 2SLS-IV assumptions, such as the Sargan-Hansen test, could not be employed in this study as they are not designed to accommodate population weighting.
It should also be pointed out that population studies, those involving ecological correlations, may be subject to the ecological fallacy that involves making conclusions based on populations and indiscriminately applying them to individuals when not warranted. Such a possibility is an example of the potential impact of theoretically important but unmeasured variables which the 2SLS-IV procedure addresses when its assumptions are met. In addition, the body of previous individual-level surveys, reviewed in this paper's background section, provides an interpretive framework and constraints against the ecological fallacy. For example, the study's results on the association of income inequality with rates of mental disability are consistent with a variety of previous studies (see Wilkinson, 2005).
The results of this study, however, are consistent with virtually all of the other individual level studies reviewed, and in particular two of them which employed a similar 2SLS-IV procedure in Australia and Europe (Rohde, 2016; Sironi & Wolff, 2018). Although the strengths of this study, particularly the large population represented through the preponderance of U.S. counties covered, and the 2SLS-IV analytic strategy, provide considerable support for the hypotheses, the study cannot be considered conclusive given the limitations identified here.
Implications of this research for practice and policy are multiple. Considerable attention needs to be paid to effects of geographic isolation as they manifest in the rural parts of the U.S. Even though the scarcity of mental health professionals may not be as dire as some previous reports suggest, attention needs to be paid to the types of services and other supports provided. Use of groups, both of a supportive and therapeutic nature, is likely needed to enhance community building. Emerging modalities based on internet technologies, such as telehealth, need to be fully researched and tested, even when they may not be as optimal as in person services. Population sparsity poses considerable challenges to service provision in rural areas given the well-known difficulties of achieving economies of scale when service populations are so spread out. Concrete services, particularly individualized transportation networks, also need to be further developed in rural areas, both to provide access to services, as well as to people and communities. The development of primary supports, including mutual aid and self-help groups, holds particular promise in many isolated areas. Finally, an important application of these findings involves better targeting of public mental health resources based on social indicators such as population isolation and socioeconomic status as key indicators of unmet needs. Use of waiting lists, historical service rates, and absolute population sizes for the various catchment areas all favor more highly populated areas. A long established correlation with mental health service application and use is the physical distance to the closest community agency or hospital (Packness et al., 2017).
Continued research on the isolation-mental disability relationship and associated questions is needed. For example, procedures need to be further developed and implemented for testing assumptions inherent in the use of the 2SLS-IV with weighted data, as well as with spatial autocorrelation. Of critical importance is the further development of brief mental health inventory scales that can be incorporated into large census and other data collection initiatives, and that can be used in conjunction with small area estimation methodologies to provide mental health measures for local areas across nations such as the U.S. To the extent that relevant datasets can be developed, longitudinal studies are needed to clarify the dynamic two-way relationships. Also needed is research on particular diagnoses, particularly depression, drug abuse, schizophrenia, dementia, and suicidality, as well as conditions affecting older and less educated individuals who become economically trapped in isolated rural areas and who become increasingly out of step with developments in contemporary society. Broad studies such as the one reported here provide only the general outlines within which details on the individual, community, and macro-levels can continue to be filled in by further research and planning to inform a diverse array of services that are responsive to both isolated and urban communities.
Ethics review statement
None required (anonymous and aggregated census and secondary data sources used)
Note
The authors do not have any conflict of interest in regard to this study. There are no grants or contracts to acknowledge.
References
- Arcury T.A., Gesler W.M., Preisser J.S., Sherman J., Spencer J., Perin J. Special populations, special services The effects of geography and spatial behavior on health care utilization among the residents of a rural region. HSR: Health Services Research. 2005;40(1):135–156. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowden R.J., Turkington D.A. Cambridge University; Cambridge, England: 1984. Instrumental variables. [Google Scholar]
- Brenner B. Vol. 13. Academic Emergency Medicine; 2006. Suicide rates strongly correlate with altitude: A study of 3,060 U.S. Counties. 5Supplement 1. [Google Scholar]
- Buonanno P., Montolio D., Vanin P. Does social capital reduce crime? The Journal of Law and Economics. 2009;52:145–170. [Google Scholar]
- Cacioppo J.T., Hawkley L.C. Perceived social isolation and cognition. Trends in Cognitive Sciences. 2009;10:447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crooks V.C., Lubben J., Petitti D.B., Little D., Chiu V. Social network, cognitive function, and dementia incidence among elderly women. American Journal of Public Health. 2008;(7):1221–1227. doi: 10.2105/AJPH.2007.115923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis J.A., Smith T.W., Hodge R.W., Nakao W., Treas J. National Opinion Research Center; Chicago, IL: 1991. Occupational prestige ratings from the 1989 general social survey [computer file] [producer], 1991. Ann Arbor, MI: Inter-university Consortium for Political and Social Research. [Google Scholar]
- Dohrenwend B.P., Levav I., Shrout P.E., Schwartz S., Naveh N., Link B.G. Socioeconomic status and psychiatric disorders: The causation selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- Doogan N.J., Roberts M.E., Wewers M.E., Tanenbaum E.R., Mumford E.A., Stillman F.A. Validation of a new continuous geographic isolation scale: A tool for rural health disparities research. Social Science & Medicine. 2018 doi: 10.1016/j.socscimed.2018.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faris R.E.L., Dunham H.W. University of Chicago Press; Chicago: 1939. Mental disorders in urban areas. [Google Scholar]
- Fontanella C.A., Hiance-Steelesmith D.L., Phillips G.S., Bridge J.A., Lester N., Sweeney H.A. Widening rural-urban disparities in youth suicides, United States, 1996-2010. JAMA Pediatrics. 2015 doi: 10.1001/jamapediatrics.2014.3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fromm E. Routledge; London and New York: 1942/2001. The fear of freedom. [Google Scholar]
- Health Resources and Services Administration [HRSA] Office of Rural Health Policy; Washington DC: 2005. Mental Health and rural America, 1994-2005. [Google Scholar]
- Helliwell J. Well-being and social capital: Does suicide pose a puzzle? Social Indicators Research. 2003;81:455–496. [Google Scholar]
- Holt-Lunstad J. The potential public health relevance of social isolation and loneliness: Prevalence, epidemiology, and risk factors. Public Policy & Aging Report. 2017;27(4):127–130. [Google Scholar]
- Horan W.P., Subotnik K.L., Snyder K.S., Nuechterlein K.H. Do recent-onset schizophrenia patients experience a “social network crisis”? Psychiatry. 2006;69(2):115–129. doi: 10.1521/psyc.2006.69.2.115. [DOI] [PubMed] [Google Scholar]
- Hudson C.G. Socioeconomic status and mental illness: Tests of the social causation and selection hypotheses. American Journal of Orthopsychiatry. 2005;75(1):3–18. doi: 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- Hudson C.G. Validation of a model for estimating state and local prevalence of serious mental illness. International Journal of Methods in Psychiatric Research. 2009;18(4):251–264. doi: 10.1002/mpr.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson C.G., Soskolne V. Health & Place; 2012. Disparities in the geography of serious mental illness in Israel. [DOI] [PubMed] [Google Scholar]
- Jaco E.G. The social isolation hypothesis and schizophrenia. American Sociological Review. 1954;19:567–577. [Google Scholar]
- Kessler R.C., Chieu W.T., Demler O., Walters E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV Disorders in the National Comoribidity survey replication. Archives of General Psychiatry. 2005;62:617–709. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinenberg E. Dying alone: The social production of urban isolation. Ethnography. 2001;2:501–531. [Google Scholar]
- Kohn M.L., Clausen J.A. Social isolation and schizophrenia. Sociological Review. 1955;20(3):265–273. [Google Scholar]
- Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- López J.A., García R.F., Martí T.S. Drugs and mental health problems among the Roma: Protective factors promoted by the Iglesia Evangélica Filadelfia. International Journal of Environmental Research and Public Health. 2018;15(2):335. doi: 10.3390/ijerph15020335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubben J. Addressing social isolation as a potent killer! Public Policy & Aging Report. 2017;27(4):136–138. [Google Scholar]
- Menard S. Sage University; Thousand Oaks, CA: Sage: 1995. Applied logistic regression analysis. Sage university series on quantitative applications in the social sciences. Series on Quantitative Applications in the Social Sciences. [Google Scholar]
- MIND . MIND; London: 2004. Not alone? Isolation and mental distress. [Google Scholar]
- National Council for Behavioral Health [NCBH] National Council for Behavioral Health; Washington DC: 2017. The psychiatric shortage causes and solutions. Retrieved from https://www.thenationalcouncil.org/wp-content/uploads/2017/03/Psychiatric-Shortage_National-Council-.pdf. [Google Scholar]
- Packness A., Waldorff F.B., Christensen R. deP., Hastrup L.H., Simonsen E., Vestergaard M. Impact of socioeconomic position and distance on mental health care utilization: A nationwide Danish follow-up study. Social Psychiatry and Psychiatric Epidemiology. 2017;52(11):1405–1413. doi: 10.1007/s00127-017-1437-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pate A. 2014. Social isolation: Its impact on the mental health and wellbeing of older Victorians. [Google Scholar]
- Putnam R. Simon & Schuster; New York: 2000. Bowling alone: The collapse and revival of American community. [Google Scholar]
- Ringle C.M., Wende S., Becker J. 2015. SmartPLS 3. Bönningstedt: SmartPLS.http://www.smartpls.com Retrieved from. [Google Scholar]
- Robert Wood Johnson Foundation [RWJ] 2018. County health Rankings and Roadmaps. State Rankings data & reports.www.countyhealthrankings.org/explore-health-rankings/rankings-data-documentation Downloaded from. [Google Scholar]
- Rohde N., D'Ambrosio C., Tang K.K., Rao P. Estimating the mental health effects of social isolation. Applied Research in Quality of Life. 2016;11(3):853–869. [Google Scholar]
- Rose R.A., Stone S.I. Instrumental variable estimation in social work research: A technique for estimating causal effects in nonrandomized settings. Journal of the Society for Social Work and Research. 2011;76(2) [Google Scholar]
- Rudan I. Health effects of human population isolation and admixture. Croatian Medical Journal. 2006;47(4):526–531. [PMC free article] [PubMed] [Google Scholar]
- Santini Z.I., Koyanagi A., Tyrovolas S., Mason C., Haro J.M. The association between social relationships and depression: A systematic review. Journal of Affective Disorders. 2015;175(2015):53e65. doi: 10.1016/j.jad.2014.12.049. [DOI] [PubMed] [Google Scholar]
- Schwarzbach M., Luppa M., Forstmeier S., König H., Riedel-Heller S.G. Social relations and depression in late life-A systematic review. International Journal of Geriatric Psychiatry. 2014;29:1–21. doi: 10.1002/gps.3971. [DOI] [PubMed] [Google Scholar]
- Schwarzer R., Bowler R., Cone J. Social integration buffers stress in New York police after the 9/11 terrorist attack. Anxiety, Stress & Coping. 2013;1:18–26. doi: 10.1080/10615806.2013.806652. [DOI] [PubMed] [Google Scholar]
- Silva M., Loureiro A., Cardoso G. Social determinants of mental health: A review of the evidence. European Journal of Psychiatry. 2016;30(4):259–292. [Google Scholar]
- Sironi E., Wolff A.N. The impact of social isolation on subjective health: an instrumental variable approach. Preprints. 2018:2018020164. [Google Scholar]
- Smith S. Clinical aspects of perceptual isolation. Proceedings of the Royal Society of Medicine. 1962;55:1003–1005. [PubMed] [Google Scholar]
- Sullivan H.S. Norton; New York: 1953. The interpersonal theory of psychiatry. [Google Scholar]
- Tittman S.M., Harteau C., Beyer K.M.L. The effects of geographic isolation and social support on the health of Wisconsin women. Wisconsin Medical Journal. 2016;115(2):65–69. [PubMed] [Google Scholar]
- United States Board on Geographic Names [USGS] States, Territories, associated areas of the United States. Datafile: NationalFile_20180801. 2018. https://geoname.usgs.gov/domestic/download_data.htm zip, downloaded from.
- United States Census [US Census] STF-3 datafile. 2000. https://www.census.gov/census2000/sumfile3.html Downloaded from “FTP Download”.
- United States, Center for Disease Control WISQARS (2008-2014), fatal Injury mapping. http://wisqars.cdc.gov:8443/cdcMapFramework Downloaded from.
- Wang J., Lloyd-Evans B., Giacco D., Forsyth R., Nebo C., Mann F. Social isolation in mental health: A conceptual and methodological review. Social Psychiatry and Psychiatric Epidemiology. 2017;52(12):1451–1461. doi: 10.1007/s00127-017-1446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman E., Kawachi I. Giving means receiving: The protective effect of social capital on binge drinking on college campuses. American Journal of Public Health. 2000;90:1936–1939. doi: 10.2105/ajph.90.12.1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson R.G. New Press; New York: 2005. The impact of inequality: How to make sick societies healthier. [Google Scholar]
- Wilson W.J. The University of Chicago Press; Chicago and London: 1987. The truly disadvantaged: The inner city, the underclass, and public policy. [Google Scholar]
- Zavaleta D., Samuel K., Mills C. 2014. Social isolation: A conceptual and measurement proposal.http://www.ophi.org.uk/social-isolation-a-conceptual- and-measurement-proposal/ OPHI Working Paper 67. Retrieved from. [Google Scholar]
- Zelikowsky M., Hui M., Karigo T., Choe A., Yang B., Blanco M.R. The neuropeptide tac2 controls a distributed brain state induced by chronic social isolation stress. Cell. 2018;173(5):1265. doi: 10.1016/j.cell.2018.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]