Abstract
Objective
The meta-analysis is to objectively evaluate the efficacy of Tai Chi exercise for motor function and sleep quality in patients with stroke.
Methods
Randomized controlled trials(RCTs) about the effects of Tai Chi versus a non-exercise or conventional rehabilitation exercise control group on motor function and sleep quality in patients with stroke were searched from multiple electronic databases(PubMed, Web of Science, the Cochrane Library, EMBASE, AMED, CBM, CNKI, Wanfang and VIP) until August 2016. Two investigators independently screened eligible studies, extracted data, and assessed the methodological quality by using the quality evaluation criteria for RCTs recommended by Cochrane Handbook. Then meta-analysis was performed by RevMan5.3 software.
Results
A total of 17 RCTs with 1209 participants were included. The meta-analysis indicated that there was a significant difference on improving the balance function(P < 0.001) and ability of daily activity (P = 0.0003) of patients with stroke between Tai Chi group and control group. However, no significant effect was found on Tai Chi for walking function and sleep quality(P > 0.05).
Conclusion
Tai Chi exercise can significantly improve the balance function and ability of daily activities of patients with stroke, and there are no significant differences in walking function and sleep quality. Therefore, lots of multicenter, large-sample, higher quality randomized controlled trials are needed to verify the effects of Tai Chi exercise in improving walking function and sleep quality for patients with stroke.
Keywords: Tai Chi exercise, Rehabilitation, Stroke, Meta-analysis
1. Introduction
Stroke, also known as cerebral vascular accident, is a group of acute cerebrovascular diseases which caused by different causes of acute cerebral circulation disorders (cramps, occlusion or rupture) leading to portion or diffuse brain dysfunction [1]. According to reported global estimates, approximately 15 million people suffer from a stroke each year, resulting in 5.5 million deaths, with 5 million cannot live independently because of disability [2]. In 2015, the “Chinese Stroke Prevention Report” pointed out that stroke has become the first leading cause of death among Chinese residents, and the prevalence of stroke continues to increase [3]. Disabilities following stroke can affect daily living activities of patients and lead to great suffering to patients and heavy economic burdens to the family and society [4]. This trend has profound financial and social consequences [5].
Hence, effectively treating stroke is important. Exercise training can promote spontaneous neural functional recovery in patients with cerebrovascular disease, thereby accelerate the process of functional recovery [6]. In recent years, Tai Chi is popular in stroke patients. All the participants noted various physical, functional, and psychological benefits from participating in the Tai Chi exercise, which was perceived as a good way of integrating various skills learned during rehabilitation [7]. Tai Chi,a kind of traditional Chinese low-moderate intensity aerobic exercise, incorporate slowness, rhythmic movements, relaxation, mental concentration, movement coordination, and flow into the next one with elements of meditation, body awareness, and imagery while breathing deeply [8], [9]. Tai Chi exercise mode is a more reasonable way of rehabilitation exercise, and some studies have found that practicing TaiChi exercise can improve the ability of gait and balance, increase muscle strength for motor system function, and promote good mental state, which was useful for patients with stroke, and even for healthy adults [10], [11]. In addition, studies have reported [12], [13], Tai Chi exercise can effectively improve the sleep quality of the elderly. Although the results of some clinical studies investigating the effects of Tai Chi exercise on people with stroke have been reported, their findings have not been widely publicized or acknowledged. The objective of this study was to examine the evidence on the effect of Tai Chi exercise for motor function and sleep quality in stroke patients by performing a systematic review and meta-analysis of relevant randomized controlled trials (RCTs).
2. Methods
2.1. Search strategy
We carried on a comprehensive search of the literature in five English databases: PubMed, Web of Science, the Cochrane Library, EMBASE and AMED, and four Chinese databases: CBM, CNKI, Wanfang and VIP databases, which have been searched from their establishment to August 2016. We used following MeSH terms and all field terms when searching. The language was restricted to Chinese and English. The references of all included articles was searched twice and in order to avoid missing literature. The search strategy for PubMed is showed in Table 1.
Table 1.
Search strategies.
| #1 | Stroke[Mesh] |
| #2 | “Apoplexy” OR “Cerebrovascular Accident” OR “Cerebrovascular” OR “Apoplexy Cerebrovascular Stroke”OR“Brain Vascular Accident” OR“Cerebral Stroke” OR “Acute Stroke” OR “Acute Cerebrovascular Accident” [All fields] |
| #3 | #1 OR#2 |
| #4 | Tai Chi[Mesh] |
| #5 | “Taiji” OR“Tai Ji Quan”OR “Tai Chi Chuan”[All fields] |
| #6 | #4 OR#5 |
| #7 | “randomized controlled trial” OR “random*” OR “RCT″ |
| #8 | #3 AND#6 AND#7 |
MeSH: Medical Subject Heading.
2.2. Eligibility and exclusion criteria
Research papers selected and analyzed in this study had to meet the following eligibility criteria:
P (population): patients meet the 1995 fourth cerebrovascular disease diagnostic criteria, duration ≤6 months, and by electronic computer X-ray tomography technique(CT), magnetic resonance imaging(MRI) confirmed stroke;
I (intervention): TaiChi, Taiji, Tai Ji Quan, Tai Chi Chuan with or without other treatment;
C(comparison):any type of conventional rehabilitation exercise (including general care, routine exercise therapy)
O(outcome): outcome measures followed: (1)Balance function(using the Berg Balance Scale (BBS) to assess); (2)Walking function(using the gait, the Timed Up-and-Go Test(TUG) and Holden walking grading scale to evaluate); (3)Ability of daily activities (using Activities of Daily Living(ADL), Barthel Index, Modified Barthel Index, Tunk Impairment Scale(TIS), physical function scores of Short Form Health Survey 36 (SF-36) and Generic Quality of Life Inventory-74(GQOLI-74) to evaluate); (4)Quality of sleep (using the Pittsburgh Sleep Quality Index(PSQI)to assess).
S(study design): RCT, English and Chinese studies were selected.
Studies were excluded if they met any of the following: (1)case reports or reviews or systematic reviews; (2) duplicate record literature; (3) multiple intervention measures, making it difficult to evaluate the effects of a single measure; (4)can not to obtain effective data. After conducting search, two reviewers perused independently the title and abstract of the studies resulting from the search criteria we had set for qualified studies. Furthermore, we thoroughly read the contents of these research papers and considering select those papers that met the criteria of this study.
2.3. Data extraction
Two reviewers screened independently according to the inclusion and exclusion criteria. Each included study is extracted data independently by two reviewers using a pre-designed data extraction form. The following information was extracted:study characteristics (eg, author and year), subjects characteristics (eg, age and number of sample), study design, place of study, description of interventions, duration of trial period and indexes of assessed outcomes. During the processes above, disagreements between the two reviewers were resolved through consulting, if the consensus could not be reached, the third reviewer was consulted for a final decision.
2.4. Risk of bias assessment
The risk of bias was assessed by two reviewers using the Cochrane Handbook for Systematic Reviews of Interventions [14]. Two reviewers assessed independently for risk of bias in each included study. Six components associated with the risk of bias were assessed: randomization sequence generation, allocation concealment, blinding of outcome assessors, incomplete outcome data, selective reporting, and other biases. Each item would be rated as “low risk of bias”,“unclear risk of bias”, or “high risk of bias” in the light of Cochrane Handbook [14]. In our study, it is impossible to blind researchers and subjects in the non-pharmacological clinical trials. However, it is feasible to blind the outcome assessors (blinding to the study objectives and outcomes). So, for the purposes of this review, blinding of outcome assessors was considered as adequate. The independent evaluation is completed, the two researchers on the evaluation results were discussed and reached a consensus. If there was disagreement, the third researcher was consulted.
2.5. Statistical analysis
The meta-analysis was performed by using the RevMan 5.3 software. When meta-analysis was conducted for continuous variables, if all studies assessed the same outcome by the same scale, the weighted mean difference(WMD) was used as a summary statistic in meta-analysis; if all studies evaluated the same outcome by different scales, the standardized mean difference(SMD) was used as a summary statistic in meta-analysis, and all analysis were calculated 95% confidence interval (95%CI).In meta-analysis, statistical heterogeneity be measured by Chi-square test, I2 and P value. When P > 0.1 and I2<50%, a fixed-effects model would be applied and P < 0.1 and I2≥50%,a random-effects model would be applied if articles were considered clinically similar enough. We only use descriptive analysis if the heterogeneity is too obvious which can not determine the source. Corresponding 95% CI and P value as pooled effect would present the result of meta-analysis. A P < 0.05 was considered to be statistically significant. Publication bias was assessed by means of funnel plot and Egger's test of asymmetry [15].
3. Results
3.1. Study selection
The result of search process is presented in Fig. 1. Our search initially obtained 261 relevant articles. 87 studies were duplicates and excluded, 174 remained. Screening of titles and abstracts of the remaining publications, 39 were screened for proper studies, of which 135 were excluded owing to the following reasons: (1) not RCT(12 studies); (2) duplicate paper (29 studies); (3) reviews and case (30 studies); and (4) not related to topic (64 studies). After reading the 39 full-text literature, 22 studies were excluded due to not meet the inclusion criteria or no empirical data. Finally, a total of eligible 17 studies were included in the meta-analysis.
Fig. 1.
Flow chart of the study selection procedure. Abbreviations: CBM:China Biology Medicine; CNKI:China National Knowledge Infrastructure; VIP:Chinese Sci scientific Journal Database; RCT: randomized controlled trial.
3.2. Study characteristics
This study included 17 RCTs, including 1209 cases, 613 cases in the intervention group and 596 cases in the control group. The study duration ranged from 4 weeks to 48 weeks. Table 2 shows the basic characteristics of the included studies.
Table 2.
Characteristics of the included studies.
| Author(year) | Study design | Place of study | No.of Participants (T/C) | Age (year) T/C | Intervention |
Frequency and duration of Tai Chiexercise | Outcomes | |
|---|---|---|---|---|---|---|---|---|
| T | C | |||||||
| Taylor-Piliae et al. (2012) [16] | RCT | USA | 28(16/12) | 72.8 ± 10.1/ 64.5 ± 10.9 | Yang's 24-posture short-form TaiChi | GC | 12 weeks,3 times/week, 60 min/time | SPPB(gait), SF-36 (physical score), PSQI |
| Taylor-Piliae et al. (2014) [17] | RCT | USA | 101(53/48) | 71.5 ± 10.3/ 68.2 ± 10.3 | Yang's24-posture short-form TaiChi | GC | 12 weeks,3 times/week, 60 min/time | SPPB(gait), SF-36 (physical score), PSQI |
| Au-Yeung et al.(2009) [18] | RCT | Hong Kong, China | 136(74/62) | 61.7 ± 10.5/ 65.9 ± 10.7 | Sun's12-posture short-form TaiChi | GRE | 12 weeks,4 h/week | TUG |
| Kim et al.(2015) [19] | RCT | Korea | 22(11/11) | 53.45 ± 11.54/ 55.18 ± 10.20 | Tai Chi exercise | GRE | 6 weeks, twice/week, 60min/time | TUG, SF-36 (physical score) |
| Wang et al.(2010) [20] | RCT | Japan | 29(16/13) | Over 50 | Yang's TaiChi Chuan | GRE | 12 weeks, once a week, 50min/time | PSQI |
| Fu et al.(2016) [21] | RCT | Jiangsu China | 60(30/30) | 59.7 ± 7.6/ 60.3 ± 8.4 | 24-posture short-form Tai Chi | GRE | 8 weeks,6 times/week, 40min/time | BBS, TIS, Holden walking grading scale |
| Liu et al.(2009) [22] | RCT | Hubei, China | 48(24/24) | 52.13 ± 14.13/ 53.51 ± 12.63 | 24-posture short-form Tai Chi | GRE | 12 weeks, 30 min/time | BBS |
| Zhou et al.(2010) [23] | RCT | Henan, China | 68(34/34) | 52.5 ± 10.8/ 50.4 ± 8.8 | Yang's 24-posture short-form Tai Chi | GRE | 4 weeks,2 times/week | BBS, GQOLI-74 (physical score) |
| Zhou(2013) [24] | RCT | Sichuan, China | 68(34/34) | 62.6 ± 5.7/ 63.3 ± 6.0 | Tai Chi exercise | GRE | 6 weeks, 10 times/week, 20–30min/time | Gait, BBS, MBI |
| Zhou(2015) [25] | RCT | Beijing, China | 40(21/19) | 55.30 ± 9.47/ 54.74 ± 7.02 | Tai Chi exercise | Modern rehabilitation technology | 4 weeks,5 times/week 60 min/time | BBS, BI |
| Yang et al.(2013) [26] | RCT | Jilin,China | 100(50/50) | 54.3 ± 13.8/ 55.2 ± 14.6 | Tai Chi balance method | GRE | 4 weeks | BBS, BI |
| Xu et al.(2014) [27] | RCT | Hebei, China | 80(40/40) | 60.14 ± 10.25/ 48.23 ± 12.32 | Tai Chi exercise | GRE | 12 weeks,20min/time, 2 times everyday | BBS |
| Xie(2008) [28] | RCT | Jilin,China | 48(24/24) | 35–66/ 38–62 | Tai Chi exercise | GRE | 10 weeks | BBS, MBI |
| Miu et al.(2014) [29] | RCT | Shandong, China | 57(29/28) | Unclear | Yang's 24-posture short-form Tai Chi | GRE | 8 weeks,2 times everyday, 30min/time | Gait |
| Yang et al.(2016) [30] | RCT | Jilin,China | 60(30/30) | 58.00 ± 11.27/60.07 ± 7.87 | Tai Chi balance method | GRE | 4 weeks, once a day, 15min/time | Holden walking grading scale, BI |
| Gao et al.(2012) [31] | RCT | Guangdong,China | 158(76/82) | 65.3 ± 12.2/ 63.5 ± 11.3 | Seat type 10-posture Tai Chi | GRE | 4 weeks,2 times/day, 60 min/time | BBS, BI |
| Zheng et al.(2015) [32] | RCT | Guangdong,China | 106(51/55) | 59 ± 13/ 60 ± 12 | Tai Chi exercise | GRE | 48 weeks,2 times everyday, 30 min/time | ADL |
Abbreviations: RCT:randomized controlled trial; T:Tai Chi group; C:control group; GC:general care; GRE:general rehabilitation exercise; BI:Barthel Index; MBI: modified Barthel Index; BBS:the Berg Balance Scale; TUG:Timed Up-and-Go Test; ADL:Activities of daily living; SF-36:the Short Form Health Survey 36; GQOLI-74: Generic Quality of Life Inventory-74; SPPB:Short Physical Performance Battery; TIS:Tunk Impairment Scale; PSQI:the Pittsburgh Sleep Quality Index.
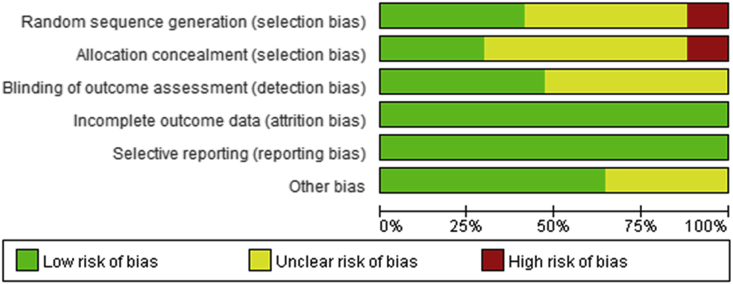
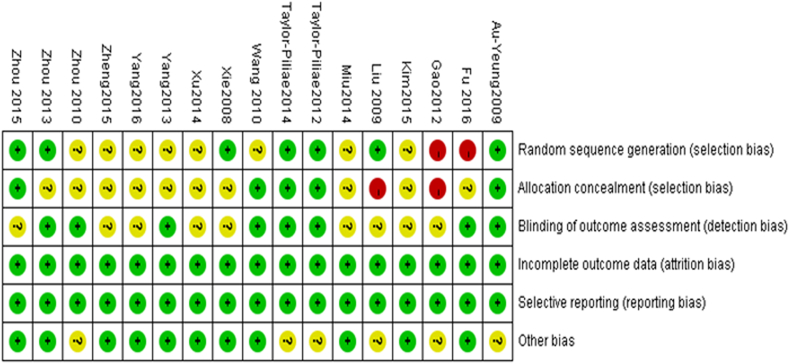
3.3. Risk of bias assessment
The risk of bias of the included studies which is presented in the risk of bias graph and risk of bias summary(Fig. 2, Fig. 3). Of 17 included studies, eight studies described the methods of randomization, by computer-generated or random numbers. Five studies revealed that the allocation concealment was adequate. Most of them have problems about blinding, only eight described assessor blinding. Low-level articles were resulted from incomplete outcome data. Even though reported the dropouts, there was no intention-to-treat (ITT) analyses. All seventeen trials reported important outcomes. Consequently, the seventeen studies can be regarded as at low risk in selective outcome reporting bias.
Fig. 2.
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Fig. 3.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.4. Meta-analysis results
3.4.1. Comparison of balance function between Tai Chi exercise group and the control group
A total of nine studies [21], [22], [23], [24], [25], [26], [27], [28], [31] were included in the study, involving 670 cases and the balance function of the stroke patients was evaluated by the Berg Balance Scale. The result of meta-analysis showed a significant heterogeneity(I2 = 97%). Considering that the effects of different intervention times, therefore subgroup analyses were conducted. The results of subgroup analysis showed Tai Chi exercise can significantly improve the balance function of stroke patients, less than or equal to 1 month (MD = 6.13, 95% CI [5.37, 6.89], P < 0.001), more than 1 month (MD = 12.38, 95% CI [6.67,18.09], P < 0.001) (Fig. 4). Therefore, the results of subgroup analysis suggested that different intervention time is the source of heterogeneity.
Fig. 4.
Comparison of the balance function between Tai Chi exercise group and the control group.
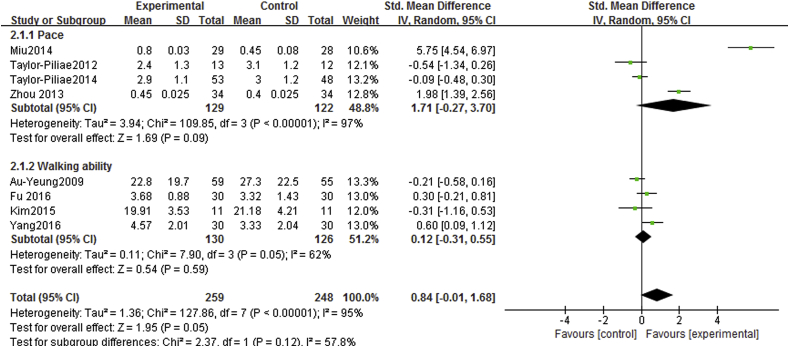
3.4.2. Comparison of walking function between Tai Chi exercise group and the control group
Eight studies involving 507 cases [16], [17], [18], [19], [21], [24], [29], [30]. Four studies [16], [17], [24], [29] of which reported the effects of Tai Chi on the gait of stroke patients. Two studies [18], [19] used the Timed Up-and-Go Test (TUG) and two studies [21], [30] used Holden walking grading scale to assess the effect of Tai Chi exercise on walking ability in stroke patients. Heterogeneity was identified across the included studies (I2 = 95%). Therefore, meta-analysis was based on random-effects model. The results showed that compared with the control group, Tai Chi did not show effective improvements on gait [SMD = 1.71, 95%CI(-0.27,3.70), P = 0.09] or walking ability [SMD = 0.12, 95%CI (−0.31, 0.55), P = 0.59](Fig. 5).
Fig. 5.
Comparison of walking function between Tai Chi exercise group and the control group.
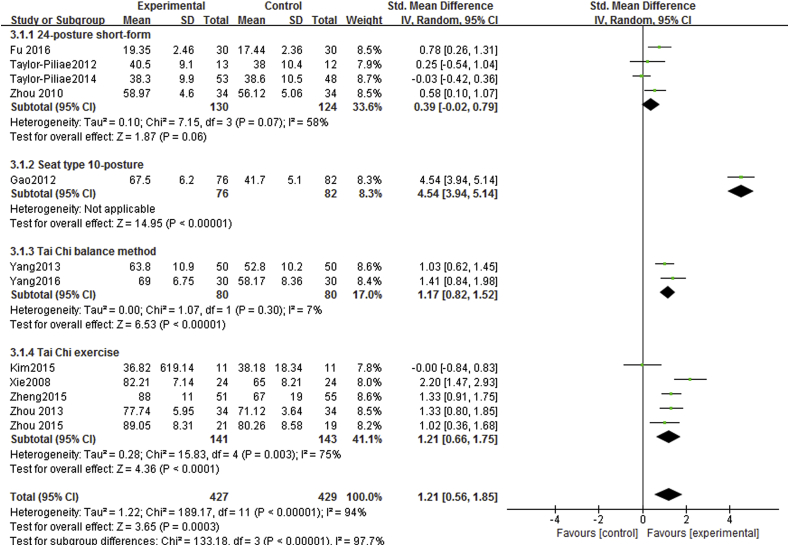
3.4.3. Comparison of daily activities ability between Tai Chi exercise group and the control group
Twelve studies [16], [17], [19], [21], [23], [24], [25], [26], [28], [30], [31], [32] involving 856 cases, seven studies used ADL, Barthel index and Modified Barthel index, and five studies used the SF-36, GQOLZ-74 and TIS, that reported the influence of Tai Chi exercise on daily activities ability in patients with stroke. Homogeneity was detected in the incorporated studies (I2 = 94%), and then a random-effects model was performed. The results showed that, compared with the control group, Tai Chi exercise can improve significantly daily activity ability, the difference was statistically significant [SMD = 1.21, 95%CI(0.56, 1.85), P = 0.0003] (Fig. 6).
Fig. 6.
Comparison of daily activities ability between Tai Chi exercise group and the control group.
Furthermore, we performed a subgroup analysis to eliminate the heterogeneity caused by the different types of Tai Chi: four studies [16], [17], [21], [23] used 24-posture short-form, the results showed that there was no beneficial performance in the daily activity ability compared with control group [SMD = 0.39,95%CI(-0.02, 0.79), P = 0.06]; one study used seat type 10-posture [31], the results showed that Tai Chi group showed better improvements on daily activity ability than the control group [SMD = 4.54, 95%CI (3.94,5.14),P < 0.001]; two studies [26], [30] used Tai Chi balance method, the results suggested that Tai Chi group showed better improvements on daily activity ability than the control group [SMD = 1.17,95%CI(0.82,1.52),P < 0.001]; five studies [19], [24], [25], [28], [32] used Tai Chi exercise, the results indicated that Tai Chi group showed better improvements on daily activity ability than the control group [SMD = 1.21,95%CI(0.66,1.75),P < 0.001] (Fig. 6). The results of subgroup analysis suggested that different type of Tai Chi exercise is the source of heterogeneity.
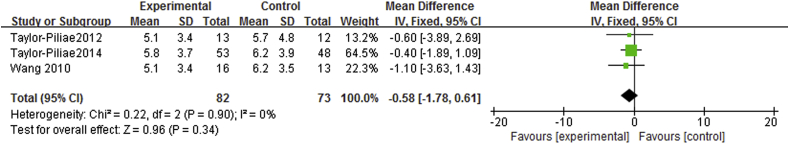
3.4.4. Comparison of sleep quality between Tai Chi exercise group and the control group
Three studies [16], [17], [20] involving 155 cases reported the sleep quality of patients with stroke by PSQI. Heterogeneity was checked in eligible studies (P = 0.90,I2 = 0%), hence, we choose a fixed-effects model. The results of meta-analysis showed that there was no significant difference in sleep quality between Tai Chi exercise and the control groups [WMD = −0.58,95%CI(-1.78,0.61), Z = 0.96,P = 0.34] (Fig. 7).
Fig. 7.
Comparison of sleep quality between Tai Chi exercise group and the control group.
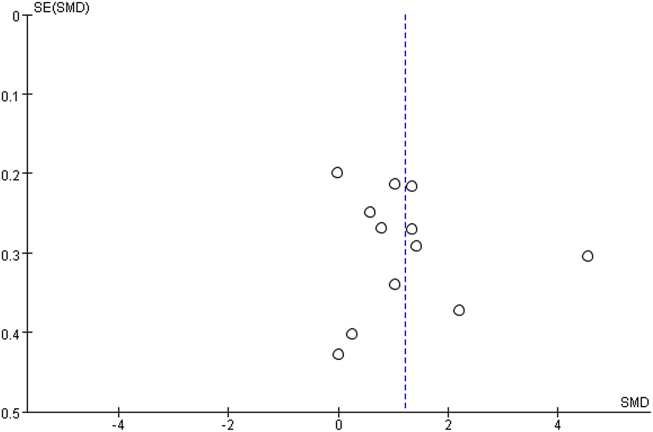
3.5. Funnel plot of publication bias
When the number of studies incorporated was more than 10, we would use funnel plot analysis publication bias. In this meta-analysis, we also used a funnel plot to determine the publication bias of daily activity ability, the results of the funnel plot analyses were symmetry, thereby indicating that no publication bias possibly exists in the included trials. (Fig. 8).
Fig. 8.
Funnel plot for publication bias.
4. Discussion
The objective of this meta-analysis was to examine whether Tai Chi exercise is effective in improving stroke patients' motor function and sleep quality. Our meta-analysis suggests that Tai Chi exercise significantly improves the balance function and ability of daily activity in patients with stroke. This meta-analysis indicated that Tai Chi has benefits in the rehabilitation of physical motor function and should be available in rehabilitation programs as an alternative approach for patients with stroke. For sleep quality, our study found that Tai Chi exercise cannot improve sleep significantly, just with a promising trend(P = 0.34).
Tai Chi is the traditional fitness project in our country, which pay attention to inside and outside, can adjust the Yin-Yang, focusing on static and dynamic combination of the overall movement. In our study, Tai Chi exercise on the functional rehabilitation of patients with stroke were related to a comprehensive evaluation, the results of meta-analysis showed that Tai Chi exercise has a significant effect on improving balance function and daily activity ability of stroke patients, which is consistent with that of Hart et al. [33], [34]. But for improving the walking function of stroke patients, this study has not found the advantages of Tai Chi exercise. The reasons may be related to disease severity condition of stroke patients, intervention duration, exercise intensity, different measurement methods of researchers and other factors.
Sleep is an important physiological phenomenon and good quality of sleep plays an important role in maintenance of normal physiological activity, physical and mental health. Some studies [35] indicated that about 95% of stroke patients with insomnia and sleep structure disorders. Study [36] has shown that, aerobic exercise can make nerve system of body to produce micro-electrical stimulation which can relieve muscle tension and mental stress, make the cerebral cortex relax, relieve psychological stress. Thereby, which contributes to improve sleep quality of stroke patients. And Tai Chi as a kind of low-moderate intensity aerobic exercise, whose fitness effect has been recognized. A narrative review [37] demonstrated Tai Chi exercise had beneficial effects on outcomes of sleep quality including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, and daytime dysfunction in older adults. However, these results are difficult to confirm the effect of Tai Chi exercise for stroke owing to the unclear controls for evaluating the comparisons and unknown methodological quality in included studies.
However, the results of this meta-analysis showed that, compared with control group, the effect of Tai Chi exercise on sleep quality of patients with stroke had no statistically significant. Analysis of the reasons: sleep quality which may be related with stroke patients own disease level, mental status and other factors. In addition, the number of RCTs included in this study is limited, therefore, the results of this meta-analysis still not determine the superiority of Tai Chi exercise in improving sleep quality of stroke patients.
5. Limitations
The review also presents several limitations. First, due to the characteristics of the sample, the Tai Chi intervention time, impact strength and different methods of evaluation may lead to the results heterogeneity increased; Second, most studies with short duration lacked long-term outcomes; thereby, current results are limited to the immediate effects of Tai Chi, and long-term effect on sleep lacks statistical significance possibly because of the limited number of studies and small sample size; Third, the studies included in the rating scale of outcomes is still no unified standard, and subjective evaluation high, which may influence the reliability of the results of this study.
6. Implications for further research
TaiChi is clearly an appropriate option for the motor function rehabilitation of patients with stroke because it has significant advantages in terms of enhance balance function and ability of daily activities. However, due to the restriction of small number of papers and the lack of long-term follow-up evaluation of intervention effects, it is impossible to evaluate accurately the advantages of Tai Chi exercise in improving walking function and sleep quality of stroke patients. Further studies are needed to improve the validity and reliability of the study and provide more reliable evidence for clinical practice, we should consider improving research designs of RCTs, following as: (1) blinding to randomization and implementation; (2) more RCTs with rigorous design, multi-center and large sample; and (3) a longer study period to assess the long-term effects of Tai Chi exercise on walking function and sleep quality in stroke patients.
7. Conclusion
In summary, this systematic review showed that the effect of Tai Chi exercise on the rehabilitation of patients with stroke has certain help, mainly in the balance function and ability of daily activities. Because of the restriction of sample, it may not evaluate accurately the advantages of improving walking function and sleep quality. Therefore, future research results from RCTs with more rigorous standards must be obtained to overcome the limitations of our existing data, and reach more reliable conclusions.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.ijnss.2017.06.001.
Contributor Information
Yufeng Li, Email: lyftulip@163.com.
Changde Jin, Email: jcd1886@sina.cn, jcd1886@hotmail.com.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Sarti C., Rastenyte D., Cepaitis Z., Tuomilehto J. International trends in mornality from stroke, 1968-1994. Stroke. 2000;31(7):1588–1601. doi: 10.1161/01.str.31.7.1588. [DOI] [PubMed] [Google Scholar]
- 2.Taylor-Piliae R.E., Haskel W.L. Tai Chi exercise and stroke rehabilitation. Top Stroke Rehabil. 2007;14(4):9–22. doi: 10.1310/tsr1404-9. [DOI] [PubMed] [Google Scholar]
- 3.Wang L.D. Peking Union Medical College press; Beijing: 2015. China stroke prevention report [M] [Google Scholar]
- 4.Lalu R.E. Changes in the quality of life of cerebral stroke patients in the first year after rehabilitation. Z Gerontol Geriatr. 2003;36(6):484–491. doi: 10.1007/s00391-003-0153-6. [DOI] [PubMed] [Google Scholar]
- 5.He Q., Wu C., Luo H., Wang Z.Y., Ma X.Q., Zhao Y.F., et al. Trends in in-hospital mortality among patients with stroke in China. PLoS One. 2014;9(3):e92763. doi: 10.1371/journal.pone.0092763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krakauer J.W. Motor learning: its relevance to stroke recovery and neuro rehabilitation. Curr Opin Neurol. 2006;19(1):84–90. doi: 10.1097/01.wco.0000200544.29915.cc. [DOI] [PubMed] [Google Scholar]
- 7.Desrochers P., Kairy D., Pan S., Corriveau H., Tousignant M. Tai chi for upper limb rehabilitation in stroke patients: the patient's perspective. Disabil Rehabil. 2016;27:1–7. doi: 10.1080/09638288.2016.1194900. [DOI] [PubMed] [Google Scholar]
- 8.Wang X.Q., Huang L.Y., Liu Y., Li J.X., Wu X., Li H.P., et al. Effects of tai chi program on neuromuscular function for patients with knee osteoarthritis: study protocol for a randomized controlled trial. Trials. 2013;14:375. doi: 10.1186/1745-6215-14-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zheng G., Huang M., Liu F., Li S., Tao J., Chen L. Tai Chi Chuan for the primary prevention of stroke in middle-aged and elderly adults: a systematic review. Evid Based Complement Altern Med. 2015:742152. doi: 10.1155/2015/742152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng G., Li S., Huang M., Liu F., Tao J., Chen L. The effect of tai Chi training on cardiorespiratory fitness in healthy adults: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0117360. doi: 10.1371/journal.pone.0117360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li F., Harmer P., Fitzgerald K., Eckstrom E., Stock R., Galver J., et al. Tai chi and postural stability in patients with Parkinson's disease. N. Engl J Med. 2012;366(6):511–519. doi: 10.1056/NEJMoa1107911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen M.H., Kruse A. A randomized controlled trial of Tai Chi for balance,sleep quality and cognitive performance in elderly vietnamese. Clin Interventions Aging. 2012;7(3):185–190. doi: 10.2147/CIA.S32600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hosseini H., Esfirizi M.F., Marandi S.M., Rezaei A. The effect of Tai Chi exercise on the sleep quality of the elderly residents in Isfahan,Sadeghieh elderly home. Iran Nurs Midwifery Res. 2011;16(1):55–60. [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins J.P.T., Green S. The Cochrane Collaboration; London: 2011. Cochrane handbook for systematic reviews of interventions version5.1.0[M] [Google Scholar]
- 15.Egger M., Davey S.G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor-Piliae R.E., Coull B.M. Community-based Yang-style Tai Chi is safe and feasible in chronic stroke: a pilot study. Clin Rehabil. 2012;26(2):121–131. doi: 10.1177/0269215511419381. [DOI] [PubMed] [Google Scholar]
- 17.Taylor-Piliae R.E., Hoke T.M., Hepworth J.T., Latt D., Najafi B., Coull B.M. Effect of Tai Chi on physical function, fall rates and quality of life among older stroke survivors. Arch Phys Med Rehabil. 2014;95(5):816–824. doi: 10.1016/j.apmr.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 18.Au-Yeung S.S., Hui-Chan C.W., Tang J.C. Short-form Tai Chi improves standing balance of people with chronic stroke. Neurorehabil Neural Repair. 2009;23(5):515–522. doi: 10.1177/1545968308326425. [DOI] [PubMed] [Google Scholar]
- 19.Kim H., Kim Y.L., Lee S.M. Effects of therapeutic Tai Chi on balance,gait,and quality of life in chronic stroke patients. Int J Rehabil Res. 2015;38(2):156–161. doi: 10.1097/MRR.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 20.Wang W., Sawada M., Noriyama Y., Arita K., Ota T., Sadamatsu M., et al. Tai Chi exercise versus rehabilitation for the elderly with cerebral vascular disorder:a single-blinded randomized controlled trial. Psychogeriatrics. 2010;10(3):160–166. doi: 10.1111/j.1479-8301.2010.00334.x. [DOI] [PubMed] [Google Scholar]
- 21.Fu C.X., Zhang Q.Y. Effects of Tai Chi Chuan on balance function and walking ability of stroke patients with hemiplegia. J Sci. 2016;31(05):536–539. [Google Scholar]
- 22.Liu T.J., Qin P., Chen X.Z. The effect of Taijiquan on improving the balance function of stroke patients. Chin J Phys Med J Rehabilitation. 2009;31(11):781–782. [Google Scholar]
- 23.Zhou Q.A., Xu J.Y., Hu A.P. The influence of Tai Chi Chuan on the rehabilitation of patients with cerebral infarction. China Pract nerve Dis. 2010;13(22):20–22. [Google Scholar]
- 24.Zhou Z.G. Medical University; 2013. The effect of intensive Tai Chi gait training on gait parameters and walking ability in stroke patients with hemiplegia in Chengdu. [Google Scholar]
- 25.Zhou L. Beijing traditional Chinese Medicine Learn; 2015. The clinical curative effect of the improved Tai Chi Chuan applied to the rehabilitation of patients with ischemic stroke. [Google Scholar]
- 26.Yang Z.B., Liu D., Sun P., Zhao G.D., Jia L. Clinical Tai Chi balance method in treatment of post-stroke hemiplegia balance disorders research. Contemp Med. 2013;19(24):5–7. [Google Scholar]
- 27.Xu X.D., Bai J., Zhang H.L., Wang L.C. Tai Chi on hemiplegia after stroke balance dysfunction in patients with stroke. J Hebei Chin Med. 2014;08:1149–1150. +1198. [Google Scholar]
- 28.Xie F. Jilin University; 2008. Rehabilitation of stroke patients with balance disorders by Tai Chi rehabilitation. [Google Scholar]
- 29.Miu T., Dai X.N., Yan W.J., Liu J. Effect of Taijiquan training on gait parameters in patients with hemiplegic stroke. China Sanat Med. 2014;11(13):987–988. [Google Scholar]
- 30.Yang Z.B., Liu D., Chang Y.S., Jia L., Qiao H. Clinical analysis of Tai Chi balance method in treatment of stroke hemiplegia after walking dysfunction. Mod distance Educ traditional Chin Med China. 2016;14(15):81–83. [Google Scholar]
- 31.Gao B.J., Feng Y.Z., Li Q.N., Li M.P., Yang H.F., Yin X.M. The therapeutic effect of Taiji ten exercise on stroke patients with hemiplegia. Massage Rehabilitation Med Study. 2012;03(7):71–72. [Google Scholar]
- 32.Zheng W.C., Zhang Y.H., Jiang X.Q., Chen R.Y., Xiao W.M. Continuous Taijiquan curative effect on ischemic stroke patients before rehabilitation A prospective randomized, controlled. J Cardiovasc. 2015;13(3):304–307. [Google Scholar]
- 33.Hart J., Kanner H., Gilboa-Mayo R., Haroeh-Peer O., Rozenthul-Sorokin N., Eldar R. Tai chi chuan practice in community-dwelling persons after stroke. Int J Rehabil Res. 2004;27(4):303–304. doi: 10.1097/00004356-200412000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Rabadi M.H. Review of the randomized clinical stroke rehabilitation trails in 2009. Med Sci Monit. 2011;17(2):460–467. doi: 10.12659/MSM.881382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou J. Characteristics and influencing factors of sleep disorders in patients with stroke: journal of the Chinese. J Cerebrovasc Dis. 2005;2(4):173–174. [Google Scholar]
- 36.Wei M.Z., Li W.Z., Lin L. The effect of aerobic exercise on the quality of sleep in the recovery period of stroke patients. China Pract Med. 2011;6(16):24–25. [Google Scholar]
- 37.Du S.Z., Dong J.S., Zhang H., Jin S.J., Xu G.H., Liu Z.X., et al. Taichi exercise for self-rated sleep quality in older people:A systematic review and meta-analysis. Int J Nurs Stud. 2015;52(1):368–379. doi: 10.1016/j.ijnurstu.2014.05.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.