Abstract
A healthy nurse work environment is a workplace that is safe, empowering, and satisfying. Many research studies were conducted on nurse work environments in the last decade; however, it lacks an overview of these research studies. The purpose of this review is to identify, evaluate, and summarize the major foci of studies about nurse work environments in the United States published between January 2005 and December 2017 and provide strategies to improve nurse work environments. Databases searched included MEDLINE via PubMed, CINAHL, PsycINFO, Nursing and Allied Health, and the Cochrane Library. The literature search followed the PRISMA guideline. Fifty-four articles were reviewed. Five major themes emerged: 1) Impacts of healthy work environments on nurses' outcomes such as psychological health, emotional strains, job satisfaction, and retention; 2) Associations between healthy work environments and nurse interpersonal relationships at workplaces, job performance, and productivity; 3) Effects of healthy work environments on patient care quality; 4) Influences of healthy work environments on hospital accidental safety; and 5) Relationships between nurse leadership and healthy work environments. This review shows that nurses, as frontline patient care providers, are the foundation for patient safety and care quality. Promoting nurse empowerment, engagement, and interpersonal relationships at work is rudimental to achieve a healthy work environment and quality patient care. Healthier work environments lead to more satisfied nurses who will result in better job performance and higher quality of patient care, which will subsequently improve healthcare organizations' financial viability. Fostering a healthy work environment is a continuous effort.
Keys words: Care quality, Nurse, Nursing leadership, Self-care, Work environments
1. Introduction
A healthy nurse work environment is a workplace that is safe, empowering, and satisfying [1]. The Institute of Medicine (IOM), a leader in providing leadership and guidance to the healthcare system in the United States, released two landmark reports: To Err Is Human: Building a Safer Health System [2] and Crossing the Quality Chasm: A New Health System for the 21st Century [3], in 1999 and 2001 respectively. These two reports recognized the issues about patient safety and care quality that challenged the healthcare system in the United States.
Currently, medical errors are the third leading cause of death in the United States [4]. To prevent medical errors, having a healthy work environment and a stable nursing workforce are critical. The current nursing turnover rate is as high as 27% and estimated to cost hospitals an average of $5.13M-$7.86 M per year [5]. Establishing and sustaining a healthy work environment are vital for nurse satisfaction and retention, patients' safety, and care quality, which play a fundamental role in healthcare organizations' financial viability [6].
As part of the efforts to improve patient safety and care quality, professional organizations such as the IOM and the American Nurses Credentialing Center (ANCC) have placed great emphases on promoting nurse work environments. Having recognized the importance of nurse work environment in patient care, the IOM issued a report in 2004: Keeping Patients Safe: Transforming the Work Environment of Nurses [7]. Magnet Designation®, a performance-driven recognition for healthcare organizations with excellent nursing care, is another program that distinguishes hospitals having a healthy work environment and positive nurse and patient outcomes [8].
1.1. Background
With the increased appreciation of healthy work environments, many research studies were conducted examining nurse work environments [9]. A search for systematic reviews was conducted in PubMed, CINAHL, PsycINFO, and Cochrane Library on studies about healthy nurse work environments published in the past decade. It was noticed that the existing systematic reviews mainly focused on specific areas of nurse work environments. For instance, Copanitsanou and colleagues [10] reviewed 10 studies from the MEDLINE database about the effects of work environments on patient and nurse outcomes. Shirey [11] reviewed 10 articles from PubMed about leadership practices to promote healthy nurse environments. Ma and colleagues [12] conducted a review of 10 studies about the influences of nurse work environments on patients' readmission risk.
1.2. Purpose
While providing valuable information about nurse work environments, these systematic reviews do not offer an overview of studies about nurse work environments in the past decade. With the continuing changes in healthcare, knowing the current state of the science on the nurse work environment can help nurses, leaders, and researchers understand the present trends of nurse work environments, evaluate existing practice approaches, and strategize future research tactics. Therefore, the purpose of this article is to identify, evaluate, and summarize the major foci of studies about nurse work environment in the United States published between January 2005 and December 2017 and provide strategies to improve nurse work environments.
2. Methods
2.1. Design
This is a systematic review with a narrative synthesis. The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13]. Before initiating the search for literature, our research team developed a plan of study. In this plan, our team identified databases, key words, and terms to be searched, set inclusion and exclusion criteria and quality appraisal tools to screen and appraise articles, and strategized approaches to extract data and conduct data analysis.
2.2. Data sources and searches
Databases searched included MEDLINE via PubMed, CINAHL, PsycINFO, Nursing and Allied Health (ProQuest), and the Cochrane Library (CENTRAL, Cochrane Database of Systematic Reviews, and DARE). Search terms included a combination of subject headings, terms, and keywords such as ‘healthy work environment,’ ‘work environment,’ ‘workplace environment,’ and ‘nurses,’ “nurse,” or ‘nursing.’ The date limits were set between January 2005 and December 2017. PubMed search query included: “work environment” [tiab] OR “work environments” [tiab] OR “workplace environment” [tiab] OR “workplace environments” [tiab]; “Nurses” [Mesh] OR “nurse” [tiab] OR “nurses” [tiab] OR “nursing” [tiab]. Search query for CINAHL and PsycINFO included: TI “healthy work environment” OR TI “healthy work environments” OR TI “nurse work environment” OR TI “workplace environment” OR TI “workplace environments” AND TI “nurse” OR TI nurses; AB “healthy work environment” OR AB “healthy work environments” OR AB “nurse work environment” OR AB “workplace environment” OR AB “workplace environments” AND AB “nurse” OR AB nurses.
2.3. Inclusion and exclusion criteria and quality appraisals
Studies were selected based on inclusion and exclusion criteria set forth by the research team of this review. Inclusion criteria were that studies should be primary research studies with empirical data; focused on nurse work environment as indicated in the titles and abstracts of the articles; and published in English in the United States between January 2005 and December 2017. To ensure a homogeneous set of studies for this review, studies were excluded if they were conducted outside the United States. Due to the complexity of the healthcare systems across the globe and the volume of studies about nurse work environment worldwide, it is beyond the scope of this review to examine and compare studies of nurse work environments worldwide.
The quality of the studies was appraised based on the Critical Appraisal Tools by the Joanna Briggs Institute [14]. Studies were selected and screened based on the combination of inclusion/exclusion criteria and the Critical Appraisal Tools [14]. The selection and quality appraisals of the studies were a collaborative effort by the first (HW) and second (KS) authors.
2.4. Search results
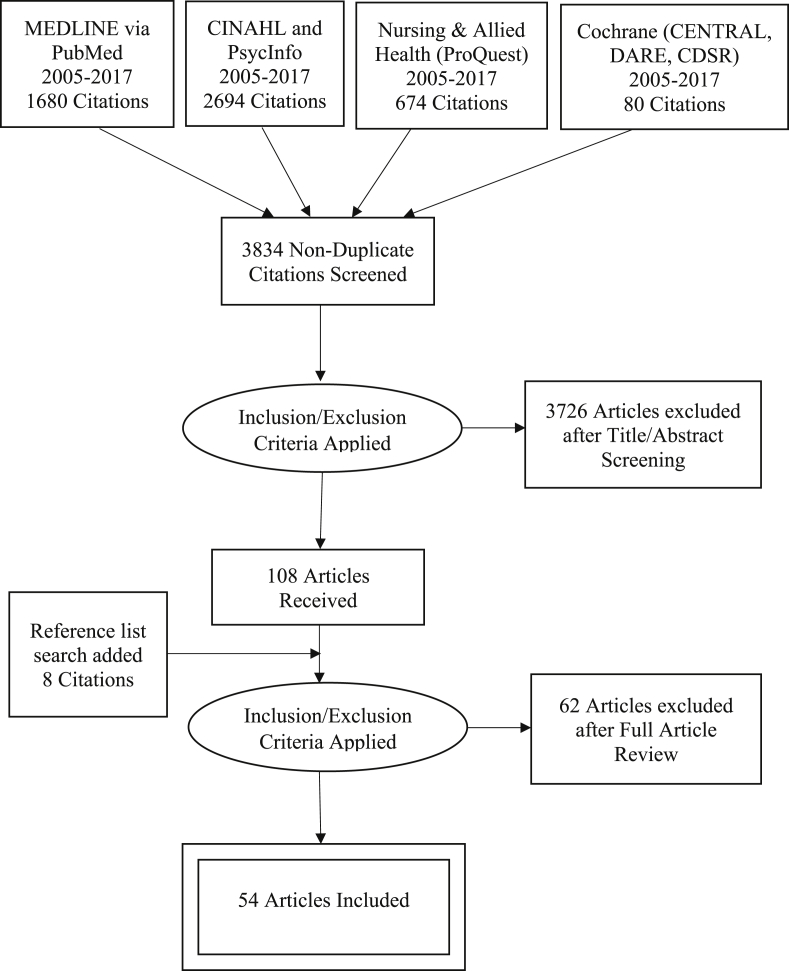
The initial literature search retrieved 5128 records after the combinations of the search terms were entered in each database, with 3834 articles remaining after the initial records were de-duplicated using Rayyan. One hundred and eight articles remained after the titles and abstracts of the articles were screened. Eight articles were added through reference searches. After full articles were read and screened, a final count of fifty-four studies was included in the review. The details of the search process were displayed in a PRISMA flow chart (Diagram 1).
Diagram 1.
Selection process based on the PRISMA [13] flow chart.
2.5. Data extraction and synthesis
Data analysis was conducted based on Miles, Huberman and Saldana's [15] constant comparative method to compare findings across studies. An information extraction table was developed to collect data including the purposes, designs, samples, measurements, and main findings of the studies. The first (HW) and second (KS) authors conducted the data extraction individually and cross-checked each other's work for accuracy, which was concurred by the co-authors. Through constant comparison of the data, themes were developed inductively.
3. Results
3.1. General characteristics of the studies reviewed
A total of fifty-four studies was included and reviewed. The studies were predominantly descriptive. The conceptual models that were referred to the most were the Structure-Process-Outcome Model [16], the System Research Organizing Model [17], and the Contingency Theory of Organizations [18]. Nurse work environments were operationalized differently based on the measures used in the studies. The top three instruments used to evaluate nurse work environments were the Practice Environment of the Nursing Work Index Revised [19], Essentials of Magnetism II [20], and the American Association of Critical-Care Nurses (AACN) Healthy Work Environment Assessment Tool [21]. Table 1 lists a summary of the studies reviewed. Table 2 displays the top three measurements used to evaluate nurse work environments.
Table 1.
Summaries of the studies reviewed.
| 1st Author/year | Purpose studied | Design/Sample | Nurse outcome variables | Nurse workplace relationships | Patient care quality | Hospital accidental safety | Nurse leadership influences |
|---|---|---|---|---|---|---|---|
| Aiken, 2008 [22] |
The effects of work environments on nurses' and patients' outcomes with the consideration of nurse staffing and education | Descriptive correlational study; Surveys and patients' medical records 10,184 nurses and 232,342 surgical patients in 168 Pennsylvania hospitals |
X Intent-to-leave; Job satisfaction |
X Burnout |
X Patients’ 30-day mortality; Failure-to- rescue; Nurse report of Quality of Care |
||
| Aiken, 2011 [23] |
The effects of nurse staffing, education, and work environments on patients' outcomes | Descriptive correlational study; Surveys and patients' medical records 39,038 nurses; 1,262,120 patients' discharge abstracts from 665 acute care hospitals in California (n = 271), Pennsylvania (n = 153), Florida (n = 168), and New Jersey (n = 73) |
X Nurse-patient staffing ratio; Organizational aspects of nurse work environments; Nurse education |
X Patient deaths; Failure-to-rescue |
|||
| Baernholdt, 2009 [24] |
The characteristics of hospitals and units, nurse work environments, nurse job satisfaction, and turnover rates in rural and urban hospitals | Descriptive correlational study; Surveys (Secondary analysis) 194 nursing units in 97 (22 rural and 75 urban) hospitals in the United States |
X Job satisfaction; Turnover rates |
||||
| Beal, 2008 [25] |
The essential elements of an optimal work environment | Descriptive qualitative study design; Interviews (a subset data from a larger qualitative study) 36 experienced clinical nurses; 3 tertiary, and 1 community hospitals located in the northeastern US |
X Career development |
||||
| Blake, 2013 [26] |
Impacts of communication, collaboration, and leadership on nurses' intent to leave | Descriptive correlational study; Surveys 415 Pediatric critical care nurses; 10 hospital PICU from different parts of the US |
X Intent-to-leave; Turn over |
X Leadership support |
|||
| Boev, 2012 [27] |
Relationships between nurses' perceptions of work environments and patients' satisfaction | Descriptive correlational study; Surveys 671 nurses; 1532 patient surveys; ICUs from a university affiliated hospital in Western New York |
X Job satisfaction |
X Patient satisfaction |
X Managers' leadership and ability |
||
| Budin, 2013 [28] |
Relationships between nurse-to-nurse verbal abuse and nurse demographics, and work-attitudes of new graduate nurses | Descriptive correlational study; Surveys 1407 nurses; Data are from the fourth wave of a national panel survey of early career nurses |
X Job satisfaction; Intent to stay |
X Nurse-nurse verbal abuse |
X Organizational commitment |
||
| Burtson, 2010 [29] |
Relationships of nurses' compassion satisfaction, job satisfaction, stress, burnout, and compassion fatigue, to nurse caring | Descriptive correlational study; Surveys 126 nurses; An academic medical center |
X Job satisfaction |
X Caring; Compassion satisfaction; Stress; Burnout |
|||
| Carthon, 2015 [30] |
Relationships between missed nursing care and hospital readmissions | Descriptive correlational study; Surveys and medical records Medical records of 160,930 patients from 419 hospitals in the US; These patients were 65–90 years old with a principal diagnosis of heart failure |
X Patient readmission |
||||
| Clarke, 2007 [31] |
Organizational factors predicting nurses' sharps injuries in acute care hospitals | Descriptive correlational study; Surveys 11,516 nurses from 188 Pennsylvania acute care hospitals |
X Nurses' sharps injuries |
||||
| Cohen, 2009 [32] |
Factors to improve RN job satisfaction and retention | Descriptive correlational study; Surveys 453 staff RNs working in acute care units; 2 acute care hospitals located in northern California |
X Supervisor support |
||||
| Cortelyou-Ward, 2010 [33] |
Impacts of work environments on nurses' intent-to-leave | Descriptive correlational study; Surveys 85 direct care nurses at a rural hospital in Central Florida |
X Intent-to-leave |
X Nurse-physician relationship |
X Organizational support |
||
| Cox, 2007 [34] |
Pediatric nurses' perceptions of work environments | Descriptive quantitative study; Surveys 4584 nurses; pediatric or non-pediatric settings in facilities from multiple states |
X Job satisfaction |
||||
| Farag, 2015 [35] |
Relationships between work environments and their inclination to report medication errors | Descriptive correlational study; Surveys 40 direct care nurses; Ambulatory surgical settings |
X Medication error reporting |
X Nurse managers' leadership styles |
|||
| Fennessey, 2016 [36] |
Relationships between nurse-reported burnout, knowledge of physical assessment, work environments, and patient assessment skills | Descriptive correlational study; Surveys 150 nurses; two hospitals: one suburban and one urban |
X Nurse burnout |
X Patients' physical assessment |
|||
| Flynn, 2012 [37] |
Relationships between work environment, staffing levels, and interception of medication errors | Descriptive correlational study Surveys 686 nurses; From 82 medical-surgical units of 14 acute care hospitals in the US |
X Nurses' medical error interception; Medication error rates |
||||
| Friese, 2005 [38] |
Relationships between work environments and nurse outcomes such as nurse reported job satisfaction, emotional burnout, and quality of care | Descriptive correlational study; Surveys 1956 Nurses from 22 hospitals |
X Job satisfaction; Emotional exhaustion |
X Nurse perceived quality of care |
|||
| Gormley, 2011 [39] |
Nurses' and managers' perceptions of work environments and quality of care | Descriptive quantitative study design; Surveys 336 nurses and managers from 2 Midwestern hospitals |
X Nurses' anticipated turnover |
X Nurse managers' perceptions of work environments |
|||
| Hartung, 2013 [40] |
Nurse managers' perspectives on leadership communication and unit subculture | Descriptive qualitative study design; Interviews 6 nurse managers from a tertiary hospital in Pennsylvania |
X Nurse managers' views on leadership communication |
||||
| Hinsley, 2016 [41] |
Using a daily assessment tool to evaluate staff's perceptions of work environments | Descriptive observational study; A visual survey tool with facial expressions indicating feelings of work environments that day 20 nurses, 10 Cath technicians, 4 MRI technicians, and 6 administrative staff in a cardiac catheterization laboratory |
X Nurses' feelings toward work environments |
||||
| Huddleston, 2016 [42] |
Nurses' and nurse leaders' perceptions of healthy work environments (HWEs) | Descriptive quantitative study design; Surveys 321 nurse leaders and direct care nurses |
X Nurses' perceptions of HWEs |
X Nurse leaders' perceptions of HWEs |
|||
| Huddleston, 2016 [43] |
Nurses' and nurse leaders' perceptions of the characters and meaning of HWEs | Descriptive qualitative study design; Focus group interview 9 focus groups (72 nurse leaders from 10 hospitals) and 10 focus groups (57 nurses in 11 hospitals) Fort Worth, Dallas |
X Nurses' perceptions of HWEs |
X Nurse leaders' perceptions of HWEs |
|||
| Kotzer, 2006 [44] |
Hospital environmental factors that empower nursing staff and improve nurse retention and satisfaction | Descriptive quantitative study design; Surveys 77 nursing staff of a pediatric hospital |
X Nurse empowerment; Retention; Job satisfaction |
X Managerial control |
|||
| Kramer, 2011 [45] |
Confirmations of units' HWE by nurses working on the unit for more than a year | Descriptive quantitative study design; Surveys 10,752 experienced RNs on 540 clinical units of 28 Magnet® hospitals that were the best of the best in national reputation and were award winners such as Balbridge, 100 Top Hospitals, Best Places to Work. |
X Nurses' perceptions of quality of care |
||||
| Kramer, 2012 [46] |
Effects of HWE and multistage nurse residency programs on newly licensed nurses' retention rates | Descriptive quantitative study design; Surveys 5316 newly licensed RNs (NLRNs) from 28 Magnet® hospitals rewarded with awards such as Balbridge, 100 Top Hospitals, Best Places to Work. |
X Newly licensed nurses' retention rates |
||||
| Kramer, 2013 [47] |
Issues, concerns, and factors affecting new graduate nurses' immersion in their first nursing work environments | Descriptive quantitative study design; Surveys 468 new graduate nurses on 191 clinical units of 17 Magnet® hospitals that had one or more awards such as Top 10 Hospitals, Best Places to Work in the United States |
X New graduate nurses' immersion in their first nursing work environments |
||||
| Kutney-Lee, 2013 [48] |
Nurse burnout, intent to leave, and job dissatisfaction over time | Descriptive quantitative study design; Surveys 137 hospitals in Pennsylvania |
X Burnout; Intent-to-leave; Job dissatisfaction |
||||
| Lewis, 2011 [49] |
Nurses' perceptions of workplace incivility (WPI) and WPI-related cost | Descriptive quantitative study design; Surveys 659 staff nurses in Texas |
X WPI; Productivity |
X Managers' competence in handling WPI |
|||
| Ma, 2014 [50] |
Nurses' perceptions QOC at unit levels and the association between unit-level work environments and QOC | Descriptive quantitative study design; Surveys 179,052nurses from 7677 units of 577 hospitals in 49 states in the US. |
X Nurses' perceptions of quality of care |
||||
| Ma, 2015 [51] |
Relationships between organizational nursing factors, such as unit-level work environments and hospitals' Magnet® status, and hospital-acquired pressure ulcers | Descriptive correlational study; Surveys 33,845 nurses from 1381 units of 373 hospitals in the US |
X Hospital-acquired pressure ulcers |
||||
| Manojlovich, 2007 [52] |
Relationships between nurses' perceptions of work environments, nurse and physician communication, and patients' outcomes | Descriptive correlational study; Surveys 449 critical care nurses from 25 intensive care units in southeastern Michigan |
X Nurse-physician communication |
X Frequencies of VAP, catheter-related sepsis, medication errors |
|||
| Mathias, 2016 [53] |
Relationships between work environments and patient care outcomes | Descriptive correlational study; Surveys 25,752 Medicare patients in 35 focal hospitals recognized with good working environments and 62,882 patients from 293 control hospitals in Illinois, New York and Texas 2004–2006 |
X Patients’ 30-day mortality rates; 30-day failure-to-rescue rates; ICU stay rates; Hospital length-of-stay |
||||
| McHugh, 2016 [54] |
Relationships between nurse staffing, work environments, and in-hospital cardiac arrest survival | Descriptive correlational study; Surveys 11,160 patients in 75 hospitals of 4 states (Pennsylvania, Florida, California, and New Jersey). |
X In-hospital cardiac arrest survival |
||||
| Mixer, 2015 [55] |
Relationships between work environments and culturally sensitive care in perinatal hospice care |
Descriptive correlational study; Surveys 995 nurses |
X Culturally sensitive care: interpreter services and multilingual staff |
||||
| Moore, 2013 [56] |
Interactions between nurses at workplace | Descriptive quantitative and qualitative design with only qualitative findings presented in this study; 82 nurses from five chapters of Sigma Theta Tau in southwestern Ohio |
X Nurse-to-nurse relationships; Intent-to-leave |
X Nurse managers' roles in workplace relationships |
|||
| Olds, 2017 [57] |
Effects of hospital safety climate and work environments on patient mortality | Descriptive quantitative cross-sectional secondary analysis 27,009 nurse survey respondents and 852,974 surgical patients from 600 hospitals; Acute care hospitals in California, Florida, New Jersey, and Pennsylvania |
X Patient in-hospital mortality |
||||
| Patrician, 2009 [58] |
Effects of work environments on nurses' medication error reporting | Descriptive correlational study; Surveys The overall response rates for cross-sectional and longitudinal surveys were 16% (43/268) and 11% (462 of 4125); Nurses (civilian, military and contract) working two or more days each week at a military medical center |
X Medication errors and reporting |
||||
| Rathert, 2007 [59] |
Nurses' perceptions of patient-centered care, comfort level of reporting medical errors, and perceived occurrence of medical errors | Descriptive quantitative study design; Surveys 307 direct care nurses |
X Nurses' perceptions of occurrences and reports of medication errors |
||||
| Schmalenberg, 2007 [60] |
The perceptions of work environments by nurses from different types of ICUs | Descriptive quantitative study design; Surveys 698 adult critical care nurses from 34 intensive care units (medical, surgical, neonatal and pediatric; medical-surgical) in 8 Magnet® hospitals |
X Nurses' perceptions of Essentials of Magnetism |
||||
| Schmalenberg, 2008 [20] |
Confirming that nurses in Magnet® designated hospitals have significantly higher scores on the Essential of Magnetism II measure than their counterparts | Descriptive quantitative study design; Surveys 10,514 staff nurses in 34 hospitals |
X Nurses' perceptions of the Essentials of Magnetism between Magnet® designated and not designated hospitals |
||||
| Schmalenberg, 2008 [61] |
Factors affecting nurses' perceptions of HWE | Descriptive quantitative study design; Surveys 2990 staff nurses from 206 clinical units in 8 Magnet® hospitals |
X Nurses' perceptions of HWE differentiated by units |
||||
| Shirey, 2009 [62] |
Relationships between leadership, organizational culture, and HWEs | Descriptive qualitative study design; Interviews 21 nurse managers from 3 acute care hospitals |
X Organizational culture and leadership |
||||
| Shively, 2011 [63] |
Relationships between work environment features and nurse stress | Descriptive observational design; Surveys 119 nurses; Acute and critical care settings of three hospitals |
X Extrinsic and intrinsic factors affecting nurses' job performance |
||||
| Silber, 2016 [64] |
Influences of work environments on patient outcomes (30-day mortality and costs reflecting resource) | Descriptive retrospective matched-cohort design; Patient's medical records 25,076 pair-matched patients with 130 surgical procedures from 35 focal hospitals where nurse-to-bed ratio was 1.51 and 293 controls with the ratio being 0.69 |
X Patients’ 30-day mortality rates and costs |
||||
| Stone, 2006 [65] |
Influences of characteristics of nurses, hospitals, and work conditions on nurses' occupational safety in adult ICUs | Descriptive quantitative study design; Surveys 837 nurses from 39 adult ICUs in 23 hospitals that participated in the CDC National Nosocomial Infections Surveillance system. |
X Nurses' occupational injuries, i.e., musculoskeletal injury and bloody and body fluid exposures |
||||
| Teclaw, 2015 [66] |
Influences of nurse work shift on nurses' perceptions of work environments | Descriptive quantitative study design; Surveys 4497 nurses in 2008; 5124 nurses in 2010; 4436 nurses in 2012; From 141 Veterans Health Administration facilities |
X Nurses' perceptions of workplace environments; Intent-to-leave; Overall satisfaction |
X Supervisors' performance |
|||
| Trinkoff, 2011 [67] |
Relationships between nursing work environments and patient outcomes at hospital-level | Descriptive quantitative cross-sectional secondary data analysis; Surveys and Agency for Healthcare Research and Quality inpatient quality indicators and patient safety indicators 633 nurses in 71 hospitals in North Carolina and Illinois |
X Inpatient quality indicators |
X Patient safety indicators |
|||
| Ulrich, 2005 [68] |
Registered nurses' perceptions of their work environments | Descriptive quantitative study design; Surveys 1783 nurses from a national database in the US |
X Workplace relationships |
X Roles of nurse managers and management |
|||
| Ulrich, 2006 [69] |
A baseline status report of critical care nurses' perceptions of their work environments | Descriptive quantitative study design; Surveys 4034 members of the AACN across the US |
X Nurses' concerns about physical and mental safety |
X Leadership roles in nurse retention |
|||
| Ulrich, 2007 [70] |
Nurses' perceptions of their work environments in organizations that are or are not Magnet or Beacon awarded | Descriptive quantitative study design; Surveys 3332 nurses indicated Magnet® status; 2897 nurses indicated Beacon status of work unit; (Survey responses indicated nurses' hospital Magnet and/or Beacon status) |
X Nurse-nurse, nurse-physician, and nurse-frontline managers communication |
||||
| Ulrich, 2007 [71] |
Registered nurses' perceptions of their work environments and nursing shortage accounting for their organizations' Magnet status. | Descriptive quantitative study design; Surveys 1783 nurses |
X Nurse-to-nurse, nurse-to-manager, nurse-to-physician and supportive staff relationships |
X Influences of nurse shortage on patients' care such as patients' wait time for surgery or tests and patient-centered care |
|||
| Ulrich, 2009 [72] |
The status of critical care work environments | Descriptive quantitative study design; Surveys 5562 AACN members |
X Job satisfaction; Intent-to-stay |
X Workplace abuse, sexual harassment, discrimination, and disruptive behaviors. |
X Nurses' perceptions of quality of care |
X Nurse and front-line managers |
|
| Ulrich, 2014 [73] |
The present status of the work environments for critical care nurses | Descriptive quantitative study design; Surveys 8444 AACN members |
X Trends of Magnet® designation and nurses' perceptions of HWEs in critical care 2006 to 2013 |
||||
| Zori, 2010 [74] |
Effects of nurse managers' critical thinking dispositions and their staff nurses' perceptions of the work environments | Descriptive quantitative study design; Surveys 12 nurse managers and 132 of the staff nurses in a 490-bed tertiary care hospital |
X Nurse managers' leadership ability |
Note: X = denotes the primary outcomes of the studies.
Table 2.
The top three measurements used to evaluate nurse work environments.
| 1st Author/year | Practice Environment of the Nursing Work Index or Revised versions | Essentials of Magnetism II | AACN Healthy Work Environment Assessment Tool or modified versions by authors |
|---|---|---|---|
| Aiken, 2008 [22] | x | ||
| Aiken, 2011 [23] | x | ||
| Blake, 2013 [26] | x | ||
| Boev, 2012 [27] | x | ||
| Clarke, 2007 [31] | x | ||
| Flynn, 2012 [37] | x | ||
| Friese, 2005 [38] | x | ||
| Huddleston, 2016 [42] | x | ||
| Kramer, 2011 [45] | x | ||
| Kramer, 2012 [46] | x | ||
| Kramer, 2013 [47] | x | ||
| Ma, 2014 [50] | x | ||
| Ma, 2015 [51] | x | ||
| Manojlovich, 2007 [52] | x | ||
| Schmalenberg, 2007 [60] | x | ||
| Schmalenberg, 2008 [20] | x | ||
| Schmalenberg, 2008 [61] | x | ||
| Ulrich, 2006 [69] | x | ||
| Ulrich, 2007 [70] | x | ||
| Ulrich, 2009 [72] | x | ||
| Ulrich, 2014 [73] | x | ||
| Zori, 2010 [74] | x |
Note: X = denotes the measurements used to evaluate nurse work environments.
3.2. Major themes
Based on the findings of the studies reviewed, five major themes emerged. The themes included: 1. The impacts of healthy work environments on nurses' outcomes such as psychological health, emotional strains, job satisfaction, and job retention; 2. The associations between healthy work environments and nurse workplace interpersonal relationships, job performance, and productivity; 3. The effects of healthy work environments on patient care quality; 4. The influences of healthy work environments on hospital accidental safety; and 5. The relationships between nurse leadership and work environments.
3.2.1. The impacts of healthy work environments on nurses' outcomes
3.2.1.1. Nurses' psychological health and emotional strains
Nurses' psychological health in this article was referred to as gratified social interactions at workplace, job satisfaction, and compassion satisfaction. Nurses' emotional strains were denoted as emotional exhaustion, burnout, compassion fatigue, and stress. Assuring nurses' physical and psychological safety represented a significant priority in healthcare organizations [43]. Based on the studies reviewed, healthy work environments were positively associated with nurses' psychological health and negatively correlated with nurses' emotional strains.
Findings of the review indicated that nurses' stress levels were directly associated with their workload, the number of patients assigned [63]. However, when nurses perceived higher caring behaviors at workplace, they had significantly lower scores on compassion fatigue, stress, and burnout, and higher scores on work relationships, job satisfaction, and compassion satisfaction [29]. The quality of nurse work environments and nurse staffing had a negative relationship with nurse burnout [22]. Nurses working in Magnet Designated® hospitals reported significantly lower emotional exhaustion than nurses in counterpart hospitals [38].
3.2.1.2. Nurses' job satisfaction and retention
The impact of healthy work environments on nurses' job satisfaction and retention was one of the major study foci in the past decade. Findings of the studies reviewed indicated that the health of nurse work environments was significantly positively correlated with job satisfaction and retention. Nurses' job satisfaction was a significant determining factor for nurse retention.
Healthy work environments had a positive relationship with nurses' perceptions of their autonomy, control over practice, nurse-physician relationships, and organizational support [33]. Healthy work environments were negatively correlated with nurse burnout, dissatisfaction, and intent-to-leave [48]. For new graduate nurses especially, nurse work environments were a significant factor determining the success of their immersion in their first nursing job [47].
Nurse work environments were a noteworthy factor for new graduate nurses' three-year retention rate [46]. When working on units that were rated as healthy or very healthy work environments, newly graduated nurses' three-year-retention rates were significantly higher than those on units where work environments needed improvement [46]. Significantly more newly graduated nurses resigned within the first six months of hire from units where environments needed improvement than from units where work environments were rated as healthy or very healthy [46].
3.2.2. The associations between healthy work environments and nurse workplace interpersonal relationships, job performance, and productivity
3.2.2.1. Workplace interpersonal relationships
Exploring workplace relationships was another major study focus of this body of literature. Workplace interpersonal relationships were those occurring among colleagues and collaborators at a workplace. The main interpersonal workplace relationships found in this review were nurse-nurse, nurse-manager, and nurse-physician relationships.
Nurse workplace relationships were a significant factor affecting nurses' psychological health, job performance, and productivity. Poor workplace relationships significantly affected nursing staff's psychological health [43]. Negative workplace relationships could intensify nurses' intent-to-leave, making nurses not only leave their work units as a clinical nurse, but also give up nursing as a profession [56].
Workplace relationships were vital in establishing and maintaining a healthy work environment. This review found that workplace incivility was a widely reported phenomenon in nursing. One study surveyed 659 nurses, among whom 553 (85%) reported workplace incivility and 239 (37%) indicated that they had actually instigated workplace incivility to other colleagues [49]. In another study, among the 1783 nurses surveyed, 28% of them reported violence at work, and 16% of the nurses reported sexual harassment [68]. Verbal abuse was also a common experience by nurses at workplaces [28,49].
Nurses perceived that having a sense of physical and mental safety was a basic need at work [68]. However, in a study with 4034 members of American Association of Critical-care Nurses, 18.2% of the participants reported sexual harassment, 26.6% discrimination, 64.4% verbal abuse, and 22.2% physical abuse [69]. A 2014 nurse survey showed that nurses reported deterioration of overall work environments in critical units from 2008 to 2013 [73].
3.2.2.2. Nurses' job performance and productivity
Workplace incivility occurred with a high price tag. The loss of productivity due to workplace incivility was estimated to be about 20%, which was computed to $11,581 per nurse per year [49]. Workplace incivility significantly affected nurses' job satisfaction, retention, and performance [49]. When working in a healthier work environment, nurses were more satisfied with their job and reported higher intent-to-stay [22]. To promote nurses' job performance and productivity, the focus should be not only on the care that nurses provided to patients, but also on the needs of nurses' self-care and their physical and psychosocial well-being [25,63].
To promote nurses' performance and productivity, both nurses' intrinsic and extrinsic factors should be achieved. Extrinsic factors included nurse work environments where direct patient care took place, communications at work, personal benefits, transit, and teaching/learning opportunities. Intrinsic factors included nurses' memory, sleep quantity and quality, perceived workload, and stress [63]. An optimal work environment was one that valued employee's strengths and contributions, encouraged effective two-way communication and the support between staff and organizations [25], and empowered staff for active decision-making, involvement, teamwork, and peer cohesion [44].
Nurse workplace relationships, job performance, and healthy nurse work environments were complementary to one another. One study reported that colleagues' social contacts outside work could impact nurses' caring behaviors and contentment at work [29]. Nurses' collegial social interactions outside their workplace and caring behaviors toward one another decreased their job-related stress and burnout and increased their job satisfaction [29]. These findings suggested that to promote healthy work environments, creating a culture of caring could be an important strategy.
Studies reviewed also compared nurse outcomes between Magnet® Designated and non-Magnet® designated Hospitals. Nurses from Magnet Designated® hospitals reported lower emotional exhaustion [38], perceived higher quality of care [20], and reported less workplace incivility than nurses in non-Magnet hospitals [49]. With a focus on providing excellent care, Magnet Designation® could play a significant role in building and sustaining a healthy nurse work environment.
3.2.3. The effects of healthy work environments on patient care quality
Patient care quality was significantly associated with nursing work environments. Patient care quality indicators in the studies reviewed included patients' 30-day inpatient mortality, failure-to-rescue, in-hospital cardiac arrest survival, readmission rate, and satisfaction. Healthy work environments had a direct relationship with patients' cardiac arrest survival rate [54] and were negatively associated with patients' 30-day inpatient mortality rate [22].
This review found that nurse work environments, patient–nurse staffing ratios, and patients' care quality were significantly correlated. In healthier work environments where nurses were more satisfied with their job and had higher intent-to-stay, patients' risks of death and failure-to-rescue were significantly lower [22]. Patients who were taken care of in hospitals with poor work environments had 16% less chance of surviving in-hospital cardiac arrests than those in hospitals with respectable work environments [54].
Appropriate patient–nurse staffing ratio and healthy work environments were complementary to one another in improving patient care outcomes [22,23]. In hospitals with the poorest nurse staffing, healthier environments could reduce the chance of patient deaths and failure-to-rescue by about 2% and 3%; and in hospitals with the best nurse staffing, healthier environments decreased the odds of patient deaths and failure-to-rescue by a significantly higher rate, 12% and 14% correspondingly [23]. The same study also reported that improving patient-to-nurse ratio could improve patient care outcomes significantly in hospitals with healthy work environments, somewhat in hospitals with mixed work environments, and no effect in hospitals with poor work environments [23]. These findings indicated that nurse work environments could positively moderate the effects of nurse staffing ratio on patients' outcomes [23].
3.2.4. The influences of healthy work environments on hospital accidental safety
Accidental safety was defined as unintended events that occurred unplanned and could have been avoided with appropriate efforts. Examples of unintended events included medication errors and nurse sharps injuries. Healthy work environments were significantly associated with hospital safety climate and culture. A poorer hospital safety climate and nurse work environments were significantly correlated with increased risk of patients' mortality rate [57].
Establishing a safe workplace culture was a key in preventing medical errors and mortality rate. Nurses rated the following aspects as top strategies to promote a safety culture: a) nurses had input to prevent errors; b) leadership placed patient safety as a top priority; and c) nurses did not feel their mistakes would be held against them [57]. The most frequent reasons that nurses cited for not reporting medication errors were fear of a) adverse consequences from reporting errors, b) other nurses' perceptions of their competence, and c) blame focused on individuals who committed the errors rather than system [58].
The prevention and interception of medical errors were multi-factorial. A trusting and supportive work environment, however, could play a role in decreasing medication error rates and increasing nurses' error interceptions [37]. Findings of this review indicated that to reach patient safety goals, forming a supportive and blameless culture is foundational.
Healthy work environments were inversely correlated with nurses' occupational injuries. In a healthier work environment, nurses had one-third less of a chance to be injured by sharps [31]. Nurses from Magnet Designated® hospitals reported lower rates of musculoskeletal injury and exposures to blood or body fluids [65]. Units within Magnet® hospitals had a 21% lower likelihood of developing hospital-acquired pressure ulcers than units from non-Magnet® hospitals [51]. Healthy work environments played a key role in hospitals' safety culture.
3.2.5. The relationships between nurse leadership and healthy work environments
Healthy work environments and nurse leadership are mutually interdependent. The studies in this review demonstrated that nurse leaders played a vital role in establishing healthy work environments, patient care quality, and nurse job performance; vice versa, healthy work environments could also facilitate nurse leaders' leadership capabilities. Findings of the studies reviewed indicated that nurse leadership was a significant component of healthy work environments as well as a substantial determinant of nurses' retention and patient quality of care. Nurse managers' leadership ability was significantly positively associated with nurses' perceptions of the work environments [27,32]. Supervisor support was a significant decisive factor for nurses' intent-to-leave or stay [26,32].
Nurse leadership was also a significant contributing factor to patient and nurse satisfaction. Nurses' favorable perceptions of their managers' leadership and ability had a significant positive relationship with better patients' satisfaction scores [27,69]. Supportive leadership could lead to contented nurses and satisfied patients [27,68]. Findings in this review demonstrated that nurse leadership capability is fundamental in establishing healthy work environments, maintaining a stable nursing workforce, and promoting patient care quality.
While workplace incivility was a significant phenomenon in healthcare, nurse leaders could make a difference. Nurse leaders' competence in handling workplace incivility and conflicts could either positively or negatively affect nurses' perceptions of its occurrence and severity [49]. Nurses who worked in a work environment with better support reported less workplace incivility [49,70].
Among nurses who planned to leave their positions, better leadership was the most frequently cited change that could make them alter their minds [69]. There was a significant positive correlation between nurse–manager relationships and nurse job satisfaction and retention [69]. These findings indicated that nurse leaders were anchors for a healthier work environment and a suite of enhanced patients' and nurses' outcomes.
4. Discussion
This article has focused on the state of the science of nurse work environments of the United States in the past decade. The concept of healthy work environment is not new. The American Association of Critical-Care Nurses (AACN) published standards to establish and sustain healthy work environments in 2005 [75] and then in 2016 [76]. Even though the concept of nurse work environment is not new, the interest in exploring and improving healthcare work environment has continued. The foci of the studies reviewed are mainly on relationships between healthy work environments and nurses', patients', and organizations' outcomes.
The intention of this review is to provide a comprehensive overview of the concept of healthy work environments. The findings of this review demonstrate that a healthy work environment is a broad construct and explored as a collective term signifying healthcare organizational culture and patient care environments. A healthy work environment may represent higher nurses' job satisfaction and retention in one study and nurse leadership, staff empowerment and engagement, and optimal patients' safety and quality of care in others, depending on the purposes and instruments researchers used for their studies. This review shows that a healthy work environment plays a significant role in healthcare delivery and is fundamental in providing high quality patient care.
This review finds that nurses, as frontline providers of patient care, are the foundation for patient safety and care quality. Promoting nurse empowerment, engagement, and interpersonal relationships at a workplace is rudimental to achieve a healthy work environment and quality of patient care. Under the current value-based purchasing system, patients' care quality and safety are underpinnings for organizations' reputation and financial returns [6]. The findings of the current review indicate that healthy work environments are advantageous in maintaining a stable and sufficient nursing workforce, promoting hospital safety, encouraging nurse performance and productivity, improving patient care quality, and supporting healthcare organizations' financial viability.
Based on the findings of this review, nurse leadership is a key factor in building and sustaining a healthy work environment. Effective nurse leadership is an antecedent for a healthy work environment and journey of nursing excellence [11]. This review suggests that the impacts of nurse leadership could be seen in many areas of nurse performance and patient care outcomes. While patient care quality is the driving force for healthcare, nurse leadership is a facilitator and determining factor in the process of achieving nursing care excellence.
It is also noteworthy that when healthy work environments are explored, nurses' and patients' outcomes are often compared between Magnet® and non-Magnet Designated hospitals. The findings indicate that the Magnet® designation status is a significant defining factor for nursing care excellence. Hospitals with Magnet® designation are recognized for their qualities of promoting healthy work environments, improving nurse satisfaction and retention, and decreasing medical errors [8]. A recommendation could be that research intervention studies be designed alongside hospitals' or organizations' Magnet Designation® application process. With studies about nurse work environments being at a descriptive level currently, incorporating Magnet Designation® process and intervention studies may be a win-win for all entities involved.
5. Strategies to promote nurse work environments
To establish and sustain a healthy work environment, AACN has put forward six standards. The AACN standards for creating and maintaining healthy work environments include: a) Skilled communication, b) True collaboration, c) Effective decision-Making, d) Appropriate staffing, e) Meaningful recognition, and f) Authentic leadership [75,76]. This review demonstrates that these standards have provided a framework and guidance for healthcare organizations to support nurses and promote patient care outcomes. Based on the findings of this review, some specific strategies are summarized to promote organizations' caring culture and nurse work engagements from nurses', nurse leaders', and organizations' perspectives.
5.1. Strategies from nurses' perspectives
Nursing is a key discipline and major workforce in healthcare. Nurses are frontline healthcare providers and therefore, are in a crucial position to build and sustain a healthy work environment. To act as frontrunners in healthcare, nurses should a) promote self-care, finding ways to effectively rejuvenate and to give the best to self and others including patients and colleagues; b) cultivate resilience, looking for resources that can help to stay positive; and c) be a collaborator and change agent in promoting nurse work environments.
5.2. Strategies from nurse leaders' perspectives
Nurse leaders are anchors for nurses. Nurse leaders are situated to promote nurse performance, patient care quality, and healthy work environments. To lead prudently, nurse leaders need to a) be inspirational, inspiring nurses' sense of commitment, engagement, and enthusiasm; b) be proactive not reactive, willing to be risk takers in innovation and making changes; and c) lead with a vision, motivating others to rise to the occasion.
5.3. Strategies from organizations' perspectives
A healthcare organization's culture is an ultimate determinant for its success or failure. This review indicates that a positive organizational culture that is filled with support and team collaborations is an underpinning for a healthy work environment. To establish a healthy nurse work environment, healthcare organizations need to a) have a clear organizational vision and mission, providing guidance and directions for organizations' goals; b) lead in transformation and empowerment, making staff feel that they are part of the organization and what they do is meaningful and appreciated; and c) create a culture of caring, establishing an innovative environment that is rich in caring at both micro and macro levels.
6. Limitations
The concept of healthy work environments was one of the study foci of healthcare research worldwide in the past decade. This article focused on the studies conducted in the United States. Although this review did not give a global view of nurse work environments, it offered an outlook on research about nurse work environments in the United States, a homogeneous sample without cultural and political differences that might affect organizational and perceptual differences in work environments. Further studies may expand this review to include studies from other countries, especially those with different healthcare systems.
7. Recommendations for future research
Research about nurse work environments currently still stays at a descriptive level. Future research is needed to design and test interventions to promote healthy work environments. The published body of literature lacks information about the impacts of leadership's caring actions on nurse work environments. It also lacks research studies investigating nurses' contributions to building and maintaining a healthy work environment.
8. Conclusion
As healthcare reform continues to evolve in the United States, improving patient care quality and safety will continue to be the focus of healthcare organizations and healthcare-related research. The key to ensuring patients' quality of care is a healthy nurse work environment, which is essential in promoting nurse satisfaction, retention, and performance. Healthier work environments lead to more satisfied nurses who will result in better job performance and higher quality of patient care, which will subsequently improve healthcare organizations' financial viability. Fostering a healthy work environment is a continuous effort.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author contributions
WEI conceived the study, conducted the initial literature search, organized the team, and designated the search and writing tasks. SEWELL conducted an independent literature search which was compared with WEI's initial search. WEI and SEWELL extracted data independently and cross-checked each other's work. WOODY and ROSE independently checked the data extracted after WEI and SEWELL. WEI drafted the manuscript and all authors contributed substantially to its revision. WEI is the corresponding author and takes responsibility for the paper as a whole.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ijnss.2018.04.010.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.American Nurses Association . 2018. Healthy work environment.https://www.nursingworld.org/practice-policy/work-environment/ Retrieved from. (Accessed on January 2, 2018) [Google Scholar]
- 2.Committee on Quality of Health Care in America . Institute of Medicine, National Academies Press; 2000. To Err is human: building a safer health system. [PubMed] [Google Scholar]
- 3.Committee on Quality of Health Care in America . National Academy Press; Washington, D.C: 2001. Crossing the quality chasm: a new health system for the 21st century. [Google Scholar]
- 4.Makary M.A., Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353 doi: 10.1136/bmj.i2139. i2139. [DOI] [PubMed] [Google Scholar]
- 5.NSI Nursing Solutions INC . 2017. 2017 national health care retention & RN staffing report.http://www.nsinursingsolutions.com/Files/assets/library/retention-institute/NationalHealthcareRNRetentionReport2017.pdf retrieved from: [Google Scholar]
- 6.Centers for Medicare & Medicaid Services . 2017. Hospital value-based purchasing.https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/Hospital_VBPurchasing_Fact_Sheet_ICN907664.pdf Retrieved from. [Google Scholar]
- 7.Page A. National Academies Press; Washington, D.C: 2004. Institute of Medicine (U.S.). Committee on the work environment for nurses and patient safety. Keeping patients safe: transforming the work environment of nurses. [PubMed] [Google Scholar]
- 8.American Nurses Credentialing Center . 2018. ANCC Magnet Recognition Program®.http://www.cgfns.org/services/credentials-evaluation/ancc/ Retrieved from. (Accessed on January 2, 2018) [Google Scholar]
- 9.Blake N. The healthy work environment standards: ten years later. AACN Adv Crit Care. 2015 Apr;26(2):97–98. doi: 10.1097/NCI.0000000000000078. [DOI] [PubMed] [Google Scholar]
- 10.Copanitsanou P., Fotos N., Brokalaki H. Effects of work environment on patient and nurse outcomes. Br J Nurs. 2017;26(3):172–176. doi: 10.12968/bjon.2017.26.3.172. [DOI] [PubMed] [Google Scholar]
- 11.Shirey M.R. Leadership practices for healthy work environments. Nurs Manag. 2017;48(5):42–50. doi: 10.1097/01.NUMA.0000515796.79720.e6. [DOI] [PubMed] [Google Scholar]
- 12.Ma C., Shang J., Stone P. "Can nurse work environment influence readmission risk?" - a systematic review. Nurs Res Rev. 2014;2014:91–101. [Google Scholar]
- 13.Moher D., Liberati A., Tetzlaff J., Altman D.G., Altman D., Antes G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buccheri R.K., Sharifi C. Critical appraisal tools and reporting guidelines for evidence-based practice. Worldviews Evidence-Based Nurs. 2017 Dec;14(6):463–472. doi: 10.1111/wvn.12258. [DOI] [PubMed] [Google Scholar]
- 15.Miles M.B., Huberman A.M., Saldaña J. third ed. SAGE Publications, Inc; Thousand Oaks, California: 2014. Qualitative data analysis: a methods sourcebook. [Google Scholar]
- 16.Donabedian A. The quality of care: how can it Be assessed? JAMA. 1988;260(12):1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 17.Brewer B.B., Verran J.A., Stichler J.F. The systems research organizing model: a conceptual perspective for facilities design. HERD: Health Environ Res Des J. 2008;1(4):7–19. doi: 10.1177/193758670800100402. [DOI] [PubMed] [Google Scholar]
- 18.Donaldson L. Sage Publications; Thousand Oaks, Calif: 2001. The contingency theory of organizations. [Google Scholar]
- 19.Lake E.T. Development of the practice environment scale of the nursing work index. Res Nurs Health. 2002;25(3):176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- 20.Schmalenberg C., Kramer M. Essentials of a productive nurse work environment. Nurs Res. 2008;57(1):2–13. doi: 10.1097/01.NNR.0000280657.04008.2a. [DOI] [PubMed] [Google Scholar]
- 21.AACN Healthy work environment assessment tool; Available from: https://www.aacn.org/nursing-excellence/healthy-work-environments/aacn-healthy-work-environment-assessment-tool. [DOI] [PubMed]
- 22.Aiken L.H., Clarke S.P., Sloane D.M., Lake E.T., Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm: J Nurs Adm. 2008;38(5):223–229. doi: 10.1097/01.NNA.0000312773.42352.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aiken L.H., Cimiotti J.P., Sloane D.M., Smith H.L., Flynn L., Neff D.F. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care. 2011;49(12):1047–1053. doi: 10.1097/MLR.0b013e3182330b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baernholdt M., Baernholdt M., Mark B.A. The nurse work environment, job satisfaction and turnover rates in rural and urban nursing units. J Nurs Manag. 2009;17(8):994–1001. doi: 10.1111/j.1365-2834.2009.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beal J.A., Riley J.M., Lancaster D.R. Essential elements of an optimal clinical practice environment. J Nurs Adm: J Nurs Adm. 2008;38(11):488–493. doi: 10.1097/01.NNA.0000339475.65466.d2. [DOI] [PubMed] [Google Scholar]
- 26.Blake N., Leach L.S., Robbins W., Pike N., Needleman J. Healthy work environments and staff nurse retention: the relationship between communication, collaboration, and leadership in the pediatric intensive care unit. Nurs Adm Q. 2013;37(4):356–370. doi: 10.1097/NAQ.0b013e3182a2fa47. [DOI] [PubMed] [Google Scholar]
- 27.Boev C. The relationship between nurses' perception of work environment and patient satisfaction in adult critical care: work environment and patient satisfaction. J Nurs Scholarsh. 2012;44(4):368–375. doi: 10.1111/j.1547-5069.2012.01466.x. [DOI] [PubMed] [Google Scholar]
- 28.Budin W.C., Brewer C.S., Chao Y., Kovner C. Verbal abuse from nurse colleagues and work environment of early career registered nurses. J Nurs Scholarsh. 2013;45(3):308–316. doi: 10.1111/jnu.12033. [DOI] [PubMed] [Google Scholar]
- 29.Burtson P.L., Stichler J.F. Nursing work environment and nurse caring: relationship among motivational factors. J Adv Nurs. 2010;66(8):1819–1831. doi: 10.1111/j.1365-2648.2010.05336.x. [DOI] [PubMed] [Google Scholar]
- 30.Carthon J.M.B., Lasater K.B., Sloane D.M., Kutney-Lee A. The quality of hospital work environments and missed nursing care is linked to heart failure readmissions: a cross-sectional study of US hospitals. BMJ Qual Saf. 2015;24(4):255–263. doi: 10.1136/bmjqs-2014-003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clarke S.P. Hospital work environments, nurse characteristics, and sharps injuries. AJIC: Am J Infect Contr. 2007;35(5):302–309. doi: 10.1016/j.ajic.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 32.Cohen J.J., Stuenkel D., Nguyen Q. Providing a healthy work environment for nurses: the influence on retention. J Nurs Care Qual. 2009;24(4):308–315. doi: 10.1097/NCQ.0b013e3181a4699a. [DOI] [PubMed] [Google Scholar]
- 33.Cortelyou-Ward K.H., Unruh L., Fottler M.D. The effect of work environment on intent to leave the nursing profession: a case study of bedside registered nurses in rural Florida. Health Serv Manag Res. 2010 Nov;23(4):185–192. doi: 10.1258/hsmr.2010.010008. [DOI] [PubMed] [Google Scholar]
- 34.Cox K.S., Teasley S.L., Lacey S.R., Carroll C.A., Sexton K.A. Work environment perceptions of pediatric nurses. J Pediatr Nurs. 2007;22(1):9–14. doi: 10.1016/j.pedn.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 35.Farag A.A., Anthony M.K. Examining the relationship among ambulatory surgical settings work environment, nurses' characteristics, and medication errors reporting. J PeriAnesthesia Nurs: Offic J Am Soci PeriAnesthesia Nurs/Am Soci PeriAnesthesia Nurs. 2015;30(6):492–503. doi: 10.1016/j.jopan.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 36.Fennessey A.C. The relationship of burnout, work environment, and knowledge to self-reported performance of physical assessment by registered nurses. Medsurg Nurs. 2016;25(5):346. [Google Scholar]
- 37.Flynn L., Liang Y., Dickson G.L., Xie M., Suh D. Nurses' practice environments, error interception practices, and inpatient medication errors. J Nurs Scholarsh. 2012;44(2):180–186. doi: 10.1111/j.1547-5069.2012.01443.x. [DOI] [PubMed] [Google Scholar]
- 38.Friese C.R. Nurse practice environments and outcomes: implications for oncology nursing. Oncol Nurs Forum. 2005;32(4):765–772. doi: 10.1188/05.ONF.765-772. [DOI] [PubMed] [Google Scholar]
- 39.Gormley D.K. Are we on the same page? Staff nurse and manager perceptions of work environment, quality of care and anticipated nurse turnover. J Nurs Manag. 2011;19(1):33–40. doi: 10.1111/j.1365-2834.2010.01163.x. [DOI] [PubMed] [Google Scholar]
- 40.Hartung S.Q., Miller M. Communication and the healthy work environment: nurse managers' perceptions. J Nurs Adm. 2013;43(5):266–273. doi: 10.1097/NNA.0b013e31828eeb3c. [DOI] [PubMed] [Google Scholar]
- 41.Hinsley K.E., Marshall A.C., Hurtig M.H., Thornton J.M., O'Connell C.A., Porter C.L. Monitoring the health of the work environment with a daily assessment tool: the REAL - relative Environment Assessment Lens - indicator. Cardiol Young. 2016;26(6):1082–1089. doi: 10.1017/S1047951115001808. [DOI] [PubMed] [Google Scholar]
- 42.Huddleston P., Gray J. Measuring nurse leaders' and direct care nurses' perceptions of a healthy work environment in an acute care setting, Part 1: a pilot study. J Nurs Adm. 2016;46(7–8):373–378. doi: 10.1097/NNA.0000000000000361. [DOI] [PubMed] [Google Scholar]
- 43.Huddleston P.P., Gray J. Describing nurse leaders' and direct care nurses' perceptions of a healthy work environment in acute care settings, Part 2. J Nurs Adm. 2016;46(9):462–467. doi: 10.1097/NNA.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 44.Kotzer A.M., Koepping D.M., LeDuc K. Perceived nursing work environment of acute care pediatric nurses. Pediatr Nurs. 2006;32(4):327–332. [PubMed] [Google Scholar]
- 45.Kramer M., Maguire P., Brewer B.B. Clinical nurses in Magnet hospitals confirm productive, healthy unit work environments. J Nurs Manag. 2011;19(1):5–17. doi: 10.1111/j.1365-2834.2010.01211.x. [DOI] [PubMed] [Google Scholar]
- 46.Kramer M.M., Halfer D., Maguire P., Schmalenberg C. Impact of healthy work environments and multistage nurse residency programs on retention of newly licensed RNs. J Nurs Adm. 2012;42(3):148–159. doi: 10.1097/NNA.0b013e31824808e3. [DOI] [PubMed] [Google Scholar]
- 47.Kramer M.M., Brewer B.B., Maguire P. Impact of healthy work environments on new graduate nurses' environmental reality shock. West J Nurs Res. 2013;35(3):348–383. doi: 10.1177/0193945911403939. [DOI] [PubMed] [Google Scholar]
- 48.Kutney-Lee A., Wu E.S., Sloane D.M., Aiken L.H. Changes in hospital nurse work environments and nurse job outcomes: an analysis of panel data. Int J Nurs Stud. 2013;50(2):195–201. doi: 10.1016/j.ijnurstu.2012.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lewis P.S., Malecha A. The impact of workplace incivility on the work environment, manager skill, and productivity. JONA: J Nurs Adm. 2011;41(1):41–47. doi: 10.1097/NNA.0b013e3182002a4c. [DOI] [PubMed] [Google Scholar]
- 50.Ma C., Olds D.M., Dunton N.E. Nurse work environment and quality of care by unit types: a cross-sectional study. Int J Nurs Stud 2014. 2015;52(10):1565–1572. doi: 10.1016/j.ijnurstu.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 51.Ma C., Park S.H. Hospital magnet status, unit work environment, and pressure ulcers. J Nurs Scholarsh. 2015;47(6):565–573. doi: 10.1111/jnu.12173. [DOI] [PubMed] [Google Scholar]
- 52.Manojlovich M., DeCicco B. Healthy work environments, nurse-physician communication, and patients' outcomes. Am J Crit Care. 2007;16(6):536–543. [PubMed] [Google Scholar]
- 53.Mathias J.M.J. Nursing work environment linked to better surgical value. OR Manag. 2016;32(3):5. [PubMed] [Google Scholar]
- 54.McHugh M.D., Rochman M.F., Sloane D.M., Berg R.A., Mancini M.E., Nadkarni V.M. Better nurse staffing and nurse work environments associated with increased survival of in-hospital cardiac arrest patients. Med Care. 2016;54(1):74–80. doi: 10.1097/MLR.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mixer S.J., Lindley L., Wallace H., Fornehed M.L., Wool C. The relationship between the nursing environment and delivering culturally sensitive perinatal hospice care. Int J Palliat Nurs. 2015;21(9):423–429. doi: 10.12968/ijpn.2015.21.9.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Moore L.W., Leahy C., Sublett C., Lanig H. Understanding nurse-to-nurse relationships and their impact on work environments. Medsurg Nurs: Offic J Acad Med-Surg Nurs. 2013;22(3):172–179. [PubMed] [Google Scholar]
- 57.Olds D.M., Aiken L.H., Cimiotti J.P., Lake E.T. Association of nurse work environment and safety climate on patient mortality: a cross-sectional study. Int J Nurs Stud. 2017;74:155–161. doi: 10.1016/j.ijnurstu.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Patrician P.A., Brosch L.R. Medication error reporting and the work environment in a military setting. J Nurs Care Qual. 2009;24(4):277–286. doi: 10.1097/NCQ.0b013e3181afa4cb. [DOI] [PubMed] [Google Scholar]
- 59.Rathert C., May D.R. Health care work environments, employee satisfaction, and patient safety: care provider perspectives. Health Care Manag Rev. 2007;32(1):2–11. doi: 10.1097/00004010-200701000-00002. [DOI] [PubMed] [Google Scholar]
- 60.Schmalenberg C., Kramer M. Types of intensive care units with the healthiest, most productive work environments. Am J Crit Care. 2007;16(5):458–469. [PubMed] [Google Scholar]
- 61.Schmalenberg C., Kramer M. Clinical units with the healthiest work environments. Crit Care Nurse. 2008;28(3):65–77. [PubMed] [Google Scholar]
- 62.Shirey M.R. Authentic leadership, organizational culture, and healthy work environments. Crit Care Nurs Q. 2009;32(3):189–198. doi: 10.1097/CNQ.0b013e3181ab91db. [DOI] [PubMed] [Google Scholar]
- 63.Shively M., Rutledge T., Rose B.A., Graham P., Long R., Stucky E. Real-time assessment of nurse work environment and stress. J Healthc Qual. 2011;33(1):39–48. doi: 10.1111/j.1945-1474.2010.00093.x. [DOI] [PubMed] [Google Scholar]
- 64.Silber J.H., Rosenbaum P.R., McHugh M.D., Ludwig J.M., Smith H.L., Niknam B.A. Comparison of the value of nursing work environments in hospitals across different levels of patient risk. JAMA Surg. 2016;151(6):527–536. doi: 10.1001/jamasurg.2015.4908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stone P.W., Gershon R.R.M. Nurse work environments and occupational safety in intensive care units. Pol Polit Nurs Pract. 2006;7(4):240–247. doi: 10.1177/1527154406297896. [DOI] [PubMed] [Google Scholar]
- 66.Teclaw R., Osatuke K. Nurse perceptions of workplace environment: differences across shifts. J Nurs Manag. 2015;23(8):1137–1146. doi: 10.1111/jonm.12270. [DOI] [PubMed] [Google Scholar]
- 67.Trinkoff A.M., Johantgen M., Storr C.L., Gurses A.P., Liang Y., Han K. Linking nursing work environment and patient outcomes. J Nurs Regul. 2011;2(1):10–16. [Google Scholar]
- 68.Ulrich B.T., Buerhaus P.I., Donelan K., Norman L., Dittus R. How RNs view the work environment: results of a national survey of registered nurses. JONA: J Nurs Adm. 2005;35(9):389–396. doi: 10.1097/00005110-200509000-00008. [DOI] [PubMed] [Google Scholar]
- 69.Ulrich B.T., Lavandero R., Hart K.A., Woods D., Leggett J., Taylor D. Critical care nurses' work environments: a baseline status report. Crit Care Nurse. 2006;26(5):46–57. [PubMed] [Google Scholar]
- 70.Ulrich B.T., Woods D., Hart K.A., Lavandero R., Leggett J., Taylor D. Critical care nurses' work environments value of excellence in beacon units and magnet organizations. Crit Care Nurse. 2007;27(3):68–77. [PubMed] [Google Scholar]
- 71.Ulrich B.T., Buerhaus P.I., Donelan K., Norman L., Dittus R. Magnet status and registered nurse views of the work environment and nursing as a career. JONA: J Nurs Adm. 2007;37(5):212–220. doi: 10.1097/01.NNA.0000269745.24889.c6. [DOI] [PubMed] [Google Scholar]
- 72.Ulrich B.T., Lavandero R., Hart K.A., Woods D., Leggett J., Friedman D. Critical care nurses' work environments 2008: a follow-up report. Crit Care Nurse. 2009;29(2):93–102. doi: 10.4037/ccn2009619. [DOI] [PubMed] [Google Scholar]
- 73.Ulrich B.T., Lavandero R., Woods D., Early S. Critical care nurse work environments 2013: a status report. Crit Care Nurse. 2014;34(4):64–79. doi: 10.4037/ccn2014731. [DOI] [PubMed] [Google Scholar]
- 74.Zori S., Nosek L.J., Musil C.M. Critical thinking of nurse managers related to staff RNs' perceptions of the practice environment: critical thinking of nurse managers. J Nurs Scholarsh. 2010;42(3):305–313. doi: 10.1111/j.1547-5069.2010.01354.x. [DOI] [PubMed] [Google Scholar]
- 75.American Association of Critical-Care Nurses American Association of Critical-Care Nurses. AACN standards for establishing and sustaining healthy work environments: a journey to excellence. Am J Crit Care. 2005;14(3):187–197. [PubMed] [Google Scholar]
- 76.American Association of Critical-Care Nurses . second ed. American Association of Critical-Care Nurses; Aliso Viejo, California: 2016. AACN standards for establishing and sustaining healthy work environments: a journey to excellence. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.