Abstract
Effective communication among healthcare professionals in the intensive care unit (ICU) is a particular imperative, with accurate and efficient interdisciplinary communication being a critical prerequisite for high-quality care. Nurses and physicians are highly important parts of the healthcare system workforce. Thus, identifying strategies that would improve communication between these two groups can provide evidence for practical improvement in the ICU, which will ultimately improve patient outcomes. This integrative literature review aimed to identify interventions that improve communication between nurses and physicians in ICUs. Three databases (Medline, CINAHL, and Science Direct) were searched between September 2014 and June 2016 using 11 search terms, namely, nurse, doctor, physician, resident, clinician, ICU, intensive care unit, communication, teamwork, collaboration, and relationship. A manual search of the reference lists of found papers was also conducted. Eleven articles met the inclusion criteria. These studies reported on the use of communication tools/checklists, team training, multidisciplinary structured work shift evaluation, and electronic situation–background–assessment–recommendation documentation templates to improve communication. Although which intervention strategies are most effective remains unclear, this review suggests that these strategies improve communication to some extent. Future studies should be rigorously designed and outcome measures should be specific and validated to capture and reflect the effects of effective communication.
Keywords: Communication, Intervention, Intensive care units, Nurses and physicians
1. Introduction
Improving quality and safety has become a priority for hospitals worldwide in recent decades. Effective communication among healthcare team members is one of the hallmarks of safe and highly reliable patient care [1]. Improving the communication between healthcare team members under rapidly changing social and medical conditions is becoming increasingly important.
Nurses and physicians are among the most important healthcare professional groups in hospital settings. They undertake separate and distinct tasks in clinical practice, yet they are expected to communicate effectively to provide effective services for patients [2]. Effective nurse–physician communication is a two-way process that involves sending the right message while being correctly received and understood by the other person [3].
Effective nurse–physician communication has positive effects on the quality of patient outcomes, such as increased patient satisfaction [4], shortened length of stay (LOS) [5], and decreased adverse events [6]. On the contrary, ineffective nurse–physician communication may compromise patient safety and increase healthcare costs [7], [8], [9], [10]. The Joint Commission [11] reported that failure in communication causes two-thirds of sentinel events in healthcare. Sutcliffe et al. [12] identified that dysfunctional communication accounts for 91% of the medical errors reported by resident physicians, which are linked with increased costs in healthcare institutions [6]. Poor nurse–physician communication may also lead to work dissatisfaction and lack of autonomy [13], [14] among nurses. Such working relationships have caused nurses to leave the profession [14], making retention and recruitment of nurses increasingly difficult [15], [16], [17]. Physicians are reported to be easily frustrated when orders are not carried out timely. Unclear communication contributes to significant work dissatisfaction among physicians [16], [18]. These influences on nurses and physicians all in turn affect the quality and safety of patient care.
In the modern healthcare system, the intensive care unit (ICU), which provides critically ill patients with high-quality care, is an essential component of most large hospitals. ICU patients are often critically ill and unstable, their clinical conditions change frequently, and their care often involves a multidisciplinary approach [19], [20]. In the complex environment of the ICU, the potential for adverse events is high [21]. Donchin [22] showed that 37% of all errors are due to some form of poor communication between nurses and physicians in the ICU, many of which are preventable [23].
Effective communication between nurses and physicians is important for the safety and quality of patient care. Identifying strategies that would improve communication between these two groups could provide evidence for practical improvements in the ICU, which will ultimately improve patient outcomes. However, to our knowledge, no review conducted on interventions to improve communication between nurses and physicians in intensive care is available.
2. Aims and methods
2.1. Aims
This integrative review aimed to identify strategies that were used to improve communication between nurses and physicians in the ICU.
2.2. Design
We conducted an integrative literature review. Integrative reviews are considered as an appropriate approach because it encompasses empirical or theoretical literature, or both, depending on the review purpose [24]. Unlike meta-analyses and systematic reviews, which only include quantitative study of similar methodology, integrative reviews combine qualitative and quantitative studies and allow for the inclusion of diverse methodologies (i.e., experimental and nonexperimental study). The richness of the sampling frame can contribute to a comprehensive understanding of the phenomenon of interest, which can extend the generalizability of the results [25].
2.3. Search methods
We searched three databases (Medline, CINAHL, and Science Direct) between September 2014 and June 2016. Search terms that were included in various combinations were: nurse AND (doctor or physician or resident or clinician) AND (ICU or intensive care unit) AND (communication or teamwork or collaboration or relationship).
2.4. Study selection
Studies were included if they were original research, were peer reviewed, had ICU nurses and physicians as participants, explored communication between the two groups, were published in English, and had no year restriction.
Studies were excluded if they were not conducted in the ICU and/or did not focus on strategies to improve communication between nurses and physicians.
2.5. Search results
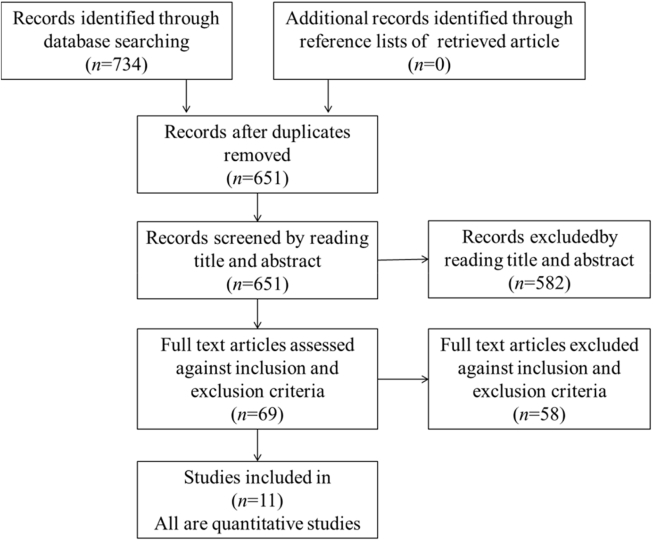
Our search for published literature yielded 734 original records for initial review. Following the removal of duplicates, 651 records were screened by examining titles and abstracts, which then excluded 582 papers. A further 58 papers did not meet the inclusion criteria after review of the full text, which left a final total of 11 studies to be included in this review. The reference lists of 11 retrieved articles were reviewed for additional relevant journals. Fig. 1 shows the flow chart of the literature search (Fig. 1).
Fig. 1.
Flow chart describing details of literature search.
2.6. Quality assessment
Quality assessment is not essential for integrative reviews and is not an inclusion criterion in integrative reviews [25]. Thus, all 11 studies were retained. Two evaluators (YYW and a research assistant) appraised the 11 retrieved publications independently using a quality assessment evaluation instrument developed by Kmet [26]. The instrument includes two evaluation checklists: one, with 10 criteria, for qualitative studies, and another, with 14 criteria, for quantitative studies. All 11 articles in this review were evaluated using the quantitative checklist (see Appendix A). This approach normally involves appraisal of 14 items (objective, design, method, subjects, random allocation, blinding of investigators, blinding of subjects, outcome, sample size, analytic methods, variance, confounding, result description, and conclusion). Studies were scored depending on how fully they met all criteria (yes = 2, partial = 1, no = 0). If a criterion was not applicable, then it was excluded from the score calculation. Summary score for each paper was calculated by dividing the total score by the total possible score (excluding nonapplicable criteria).
An intraclass correlation coefficient (ICC) was calculated as the indicator of agreement between the two evaluators with a two-way mixed model using SPSS version 18 [27]. No fixed limit to the interpretation of ICC was found in the existing literature; however, one suggestion was that the value should be interpreted as follows: values < 0.4 as poor, values 0.4–0.59 as fair, values 0.6–0.74 as good, and values 0.75–1 as excellent [28].
The ICC for average measures between evaluators for absolute agreement was medium (ICC = 0.428, 95% CI −0.360 to 0.733, P = 0.196). Due to the evident variation between evaluator scores, the evaluators discussed their understanding of the evaluation guidelines. Consensus concerning the criteria was reached, and each evaluator revised their evaluation scores. A new ICC for average measures was calculated, with an excellent result (ICC = 0.984, 95% CI 0.891 to 0.992, P < 0.001). Quality of the studies varied from 0.60 to 1.00. According to the evaluation guidelines, a study can be included if it has a quality score ranging from 0.55 (relatively liberal) to 0.75 (relatively conservative) [26](Table 1).
Table 1.
Results of quality assessment showing degree of agreement between evaluators.
| Evaluator | Study |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pronovost P et al. (2003) | Boyle DK and Kochinda C (2004) | Sluiter JK et al. (2005) | Narasimhan M et al. (2006) | Phipps LM and Thomas NJ (2007) | Agarwal S et al. (2008) | Rehder KJ et al. (2012) | Ainsworth CR et al. (2013) | Meurling L et al. (2013) | Panesar RS et al. (2014) | Justice LB et al. (2016) | |
| Evaluator1 | 0.65 | 0.90 | 0.80 | 0.68 | 0.85 | 1.00 | 0.82 | 0.68 | 0.82 | 0.70 | 0.60 |
| Evaluator2 | 0.65 | 0.82 | 0.80 | 0.68 | 0.85 | 1.00 | 0.82 | 0.68 | 0.86 | 0.70 | 0.60 |
Quality scores range from 0 (poor quality) to 1 (excellent quality).
2.7. Data extraction and analysis
Given the heterogeneity of the included literature, meta-analysis was not possible; therefore, thematic analysis was undertaken [29]. To facilitate analysis, data were extracted into an evidence table and categorized according to author/year, country, design, setting and sample, intervention strategy, outcome measure, and result (Table 2). Tabulation of quantitative findings within a single matrix supported the fusion of both narrative and statistical data [25]. Data analysis results were reviewed by all authors of the paper. The first author of this paper (YYW) screened all included papers and extracted data independently. Another author (FL) reviewed the extracted results. Discrepancies between two reviewers were resolved by discussing with the remaining authors (QQW, WJZ, and SMS) to reach a consensus. The remaining authors (QQW, WJZ, and SMS) reviewed the results after data extraction.
Table 2.
Summary of reviewed studies.
| Authors | Country | Design | Setting and sample | Interventions | Outcome measures/statistical significance | Result |
|---|---|---|---|---|---|---|
| (1) Pronovost P et al. [31] 2003 |
United States | Prospective cohort study | A 16-bed surgical ICU, academic hospital Physicians: 6 Nurse practitioners: 3 |
Daily goal form: Tasks to be completed, care plan, and communication plan (discussions with patient/family or other caregivers) Duration: 1 year |
|
|
| (2) Boyle DK and Kochinda C [30] 2004 |
Japan | Pre–post study design |
|
Team training Training for 6 modules: leadership, trust, helping others adapt to change, guiding conflict resolution, core skills for communication, core skills for teams (team culture, team communication, and team coordination) Duration: 6 months |
|
|
| (3) Sluiter JK et al. [35] 2005 |
Netherlands | Prospective repeated measurement design | PICU, university-affiliated medical center 61 staff members (physicians, nurses, department assistants) |
Multidisciplinary structured work shift evaluation: 30 min at the end of day shift, evaluate how well the working day went and what had happened during work Duration: 6 months |
|
|
| (4) Narasimhan M et al. [33] 2006 |
United States | Pre–post study design | A 16-bed medical ICU, medical center Physicians: 8 Nurses: 8 Fellow: 1 |
Daily goal worksheet: Take Pronovost's as a model Tests or procedures, medications, sedation, analgesia, catheters, consultations, nutrition, mobilization, family discussions, consents, and transfer Duration: 9 months |
|
|
| (5) Phipps LM and Thomas NJ [34] 2007 |
United States | Pre–post study design | A 12-bed medical–surgical PICU Nurses: first survey 40 second survey 42 |
Daily goal sheet: Take Pronovost's as a model Safety risk and main goal, pain and sedation, respiratory, cardiac, GI, nutrition, electrolytes, hematology, tests or procedures, medications, discharge planning Duration: 1 year |
Nurses' perception of team communication using a self-design four-item survey |
|
| (6) Agarwal S et al. [36] 2008 |
United States | Pre–post study design | A 12-bed PICU, children's hospital Physicians: 59 Nurses: 68 Fellows: 5 |
Daily patient goal sheet: Take Pronovost's as a model Fluid, nutrition, cardiac, respiratory, hematology, infectious disease, endocrine, neurologic, studies for today, consults, tests, risk, discharge plan, catheters, family communication Duration: 4 months |
|
|
| (7) Rehder KJ et al. [38] 2012 |
United States | Prospective cohort study | PICU, tertiary hospital |
|
|
|
| (8) Ainsworth CR et al. [37] 2013 |
United States | Pre–post study design | A 20-bed surgical ICU, academic military medical center | Door communication card: Major goals for the patient and the priority of the goals The cards were placed on patients' doors Duration: 1 month |
Alignment rates of goals between healthcare team members | Goal alignment among healthcare team members was low before and did not improve after intervention |
| (9) Meurling L et al. [32] 2013 |
Sweden | Pre–post study design | A general ICU, tertiary hospital Physicians: 51 Nurses: 75 Nurse assistants: 25 |
Systematic simulation-based team training: Safe teamwork during times of stress, in which the main learning objectives were knowledge and understanding of safety in complex organizations Duration: 2 year project period |
|
|
| (10) Panesar RS et al. [42] 2014 |
United States | Pre–post study design | A 12-bed PICU, tertiary hospital | Electronic SBAR documentation template Duration: - |
|
|
| (11) Justice LB et al. [41] 2016 |
United States | Pre–post study design | A 25-bed cardiac ICU, academic freestanding pediatric hospital | Visual display of patient daily goals through a write-down and read-back process Duration: 3 months |
|
|
3. Results
The 11 reported studies were all quantitative studies that were published between 2003 and 2016. A total of 8 studies were undertaken in the USA, 1 in Japan, 1 in Sweden, and 1 in the Netherlands. A total of 10 studies were single site, and 1 study [30] was conducted in 2 hospitals. Sample sizes for studies were small and ranged from as low as 9 participants [31] to as high as 151 participants [32]. Of the 7 studies that reported sample size, 4 [30], [31], [33], [34] had less than 60 participants (4/7, 57.1%) and the other 3 [32], [35], [36] ranged from 61 to 151 participants. The overwhelming majority of participants in the 6 studies that reported profession were nurses. Duration of intervention ranged from 1 month to 2 years. Of the 10 studies that reported duration, 2 lasted less than 3 months [37], [38] and 7 lasted 3–12 months [30], [31], [34], [36], [39], [40], [41], and 1 study [32] had a 2-year project period.
3.1. Types of interventions
Interventions to improve nurse–physician communication were categorized into four: communication tools/checklists, team training, multidisciplinary structured work shift evaluation, and electronic situation–background–assessment–recommendation (SBAR) documentation template. Seven studies focused on using tools/checklists to improve communication between nurses and physicians [31], [34], [36], [37], [38], [40], [41], two on team training [30], [32], one on multidisciplinary structured work shift evaluation [35], and one on electronic SBAR documentation template [42] (Table 2).
3.1.1. Communication tools/checklists
Tools used to improve communication included a daily goal sheet or form, bedside whiteboard, and door communication card. Majority of the studies involved a daily goal sheet or form. Despite a variety of formats, the sheets and forms were all innately oriented to patient treatment and needs. Pronovost et al. [31] explored the effectiveness of a daily goal form consisting of three sections: tasks to be completed, care plan, and communication plan. Findings showed that after 6 weeks of implementation, the percentage of physicians and nurses who understood the daily goals increased. Moreover, this study found a significant decrease in patient ICU LOS. Narasimhan et al. Phipps and Thomas, and Agarwal et al. [33], [34], [36] took Pronovost's model to develop specific daily goal sheet interventions (see Table 2) and obtained similar results with Pronovost. Justice et al. [41] conducted a quality improvement program in a pediatric hospital to test the effectiveness of visual display of patient daily goals through a write-down and read-back process; the percentage of agreement of patients' goals among team members and family satisfaction improved. Rehder et al. [38] designed sequential interventions that were timed 8–12 weeks apart: (1) implementing a new resident daily progress note format, (2) creating a performance improvement dashboard, and (3) documenting patients' daily goals on bedside whiteboards, in a 9 month period. Shared agreement of patients' daily goals among key healthcare providers increased with each intervention.
A door communication card is one of the modalities of a daily goal sheet or form. Ainsworth et al. [37] developed a door communication card that recorded the major priority goals for the patient, with the cards placed on patients' doors. However, communication between the healthcare team members did not change significantly after one month of implementation. According to the authors [37], the reasons were as follows: (1) no specific training was provided about how to use these goal cards; (2) no scheduled review of the goals was listed as Pronovost did [31]; it was difficult for all team members to be kept familiar with the planned goals; (3) the short study period was not enough to achieve increases in goal alignment.
3.1.2. Team training
Boyle and Kochinda [30] conducted an interventional study in Japan whereas Meurling et al. [32] did one in Sweden; both of them aimed at exploring the effectiveness of team training. Boyle and Kochinda [30] provided evidence on the effectiveness of team training in improving the communication skills of ICU nurse and physician leaders. They found that ICU nurse–physician communication improved significantly when both professions interacted with great respect and trust and gained deep insight into each other's roles and responsibilities. Meurling et al. [32] conducted systematic simulation-based team training on safe teamwork during times of stress, in which the main learning objectives were to improve the participants' knowledge and understanding of safety in complex organizations. Nurse assistants perceived an increased quality of collaboration and communication with physician specialists.
3.1.3. Multidisciplinary structured work shift evaluation
Using a quantitative study design, Sluiter et al. [35] conducted a multidisciplinary structured work shift evaluation program in a tertiary pediatric ICU. All staff members received training before the implementation, and eight staff members were trained to act as shift evaluation leaders. Multidisciplinary structured work shift evaluation was implemented on two predetermined days per week at the last 30 min of the day shift. All staff members working on that shift gathered and evaluated the events of the working day and how well they went. The study revealed that implementation of multidisciplinary shift evaluations had a positive effect on the perceived level of team communication and mean amount of problems relating to emotional exhaustion decreased significantly.
3.1.4. Electronic SBAR documentation template
SBAR is an abbreviation for situation–background–assessment–recommendation. Situation refers to the current condition of the patient and working diagnosis. Background refers to the history of presenting illness, past medical history, and patient medication. Assessment refers to the examiner's evaluation and assessment of the disease or condition. Recommendation refers to the plan of care and anticipated changes in condition or treatment [42]. Panesar et al. [42] implemented an electronic SBAR documentation template for organizing information in a clear and concise format in the electronic medical record system. The effectiveness of the program was evaluated by the frequency and completeness of documentation and the documentation of attending physician and bedside nurse notification. The increase in frequency of documentation was not statistically significant, but the completeness of documentation and notification of the nurses and attending physicians improved.
3.2. Evaluation of interventions
Evaluation of interventions across these studies was categorized into efficacy and feasibility. Efficacy evaluation consisted of patient and staff outcomes. The most commonly used patient outcome identified in this review was LOS (3/11, 27.3%) [31], [36], [40]. The most common staff outcome was the understanding of daily patient goals (6/11, 54.5%); however, measurement varied considerably across the studies. Three studies [31], [36], [40] used self-designed surveys to compare the pre–post scores of goal understanding for nurses or physicians. Three studies [37], [38], [41] used a relatively objective method through questionnaires to evaluate goal alignment between nurses and physicians pre- and post-intervention. Another major staff outcome measure was communication quality experienced and scored by staff (4/11, 36.4%) [30], [32], [39], [40]. Other staff outcome measures included self-reported communication skills, staff satisfaction, self-efficacy, job stress, and intention to leave. Only three (3/11, 27.3%) studies reported feasibility of intervention [30], [39], [40]. Staff attendance, planned time span, usefulness experienced by staff, staff's desire to use the intervention, and leaders' satisfaction were used as feasibility evidence for these interventions.
4. Discussion
Considerable variation in strategies to improve communication was observed, making comparison among findings difficult; therefore, this review did not find an intervention that is highly effective for improving nurse–physician communication. However, majority of the reviewed studies strongly supported the implementation of strategies to improve nurse–physician communication. These strategies included four categories: communication tools/checklists, team training, multidisciplinary structured work shift evaluation, and electronic SBAR documentation template.
Communication is defined as the verbal and nonverbal exchange of ideas, feelings, beliefs, and attitudes that enable a common understanding between the sender and receiver of a message. These communication tools (daily goal sheet, bedside whiteboard, or door communication card) are designed to share information to achieve collaboration and may use the same mechanism. As types of common reference points about goals [2], concerns, and plans for ICU patients, these tools allow nurses and physicians to be aware of and have access to the information about the same patients effectively and to improve communication between the staff professional groups [43].
A daily goal sheet could help the exchange of ideas and information; however, team training may improve communication and foster a collaborative working environment. ICU outcomes depend on the ability of the individual staff to function collectively as a team, because quality and safety of patient care require high-functioning multidisciplinary teams. A team can efficiently realize its shared goals if the team members have relevant teamwork skills. Nevertheless, staff in healthcare settings are rarely trained to work as teams in current education systems [1], [44]. Traditional training for health professionals has focused on technical ability and individual competence in patient care. Individuals are assumed to acquire adequate competency in teamwork [45]. Team training involves behaviors that professionals must acquire to function effectively as part of an interdependent team [46] and may improve trust, thereby improving conflict resolution and communication skills.
Multidisciplinary structured work shift evaluation could provide open communication opportunities for the healthcare team and simultaneously foster a collaborative working environment by cultivating an atmosphere for staff to talk freely about emotional events, teamwork, work roles, and organizational aspects in predefined models [39]. This method may help team members have improved understanding of each member's roles and responsibilities and respect each other. Moreover, this method may provide ways for collaborative problem solving and learning among the interdisciplinary team [47]. Ultimately, communication among team members would improve.
For communication to be effective, it must be complete (including all relevant information), clear (in a manner that is easily understood), brief (given in a concise manner), and timely (offered within an appropriate time frame for effective clinical actions) [48], [49]. The SBAR tool was designed as a documentation template for organizing information in a clear and concise format within the electronic medical record system. This tool provides a data entry structure that prompts the resident to document each of the four components of SBAR and serves as a reminder to the resident to provide detailed and complete records of the changes in the patient's condition accurately. An additional data field is included in the SBAR template to document the nurse caring for the patient, to prompt closed-loop communication among the residents and the bedside nurse in the electronic medical record system [42]. SBAR could also be used as a communication model. After formal patient assessment to establish the situation and background, nurses give recommendations to the physicians using the SBAR model. When nurses structure their communication following this model, physicians may obtain improved understanding of the situation, prioritize effectively, give effective orders, and make correct decisions [50], and vice versa. The SBAR communication model has demonstrated its positive influence on the effectiveness of communication in general wards [50], [51].
Evaluation of interventions generally includes both efficacy and feasibility [52]. This review found that outcome measures for intervention efficacy varied considerably, especially the staff outcomes. Understanding daily patient goals has been widely used to reflect the effectiveness of nurse–physician communication in the ICU. However, no standard method exists to evaluate understanding of daily patient goals. Additionally, no specific instrument or measurement has been presented for the communication between nurses and physicians. Communication quality is scored by staff using various self-designed items. Therefore, comparing the intervention efficacy among studies was difficult. Outcome measures for intervention feasibility need to be focused on, because only a small part of studies reported feasibility of intervention [30], [39], [40].
5. Limitations
Results of this review provide improved understanding on strategies used for improving the communication between ICU nurses and physicians; however, some limitations should be considered. First, relevant studies may have been missed because we only included papers published in English. Second, none of these studies were randomized controlled trials (RCTs) and all of them used convenience nonprobability sampling. None of the studies included a sample that was both randomly selected and representative of the studies' local/national contexts. Third, the majority of included studies were single site, which potentially affected the generalizability of findings beyond the samples. Finally, the lack of consistency in study design complicated the comparison among studies. Moreover, outcome measures varied considerably and did not have specific instruments or measurements for communication between nurses and physicians.
6. Implications for future research
Multiple strategies are needed to improve communication between nurses and physicians to ensure best possible patient outcomes. The daily goal sheet is the most commonly used intervention in the ICU with positive effects. Our findings indicated that although various interventions are effective in improving communication in ICU populations, the intervention strategy that is most effective remains unclear. Rigorously designed intervention studies using RCTs are required, with increased sample sizes with sufficient power to detect group mean differences, sampling plans that allow recruitment of large-enough sample sizes, and strategies to minimize attrition. Development of instruments that precisely capture and reflect the impact of good communication will facilitate the accurate evaluation of communication-related interventions and decrease outcome measure variation. Moreover, intervention feasibility should be considered.
7. Conclusion
This integrative review uniquely contributes to current knowledge of the strategies used to improve nurse–physician communication in the ICU, which includes communication tools (daily goal sheet or form, bedside whiteboard, and door communication card), team training, multidisciplinary structured work shift evaluation, and electronic SBAR documentation template. The heterogeneity of study designs and outcome measures prevented the meta-analytic approach; therefore, this review did not find an intervention that is most effective for improving nurse–physician communication. However, results suggested that these strategies improve communication to some extent. Future rigorously designed studies are needed to investigate the effectiveness of the strategies.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
No conflict of interest has been declared by the authors.
Acknowledgements
The authors acknowledge our research assistant MS Yingyan Chen's contribution in assisting paper quality assessment.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Appendix A. Checklist for assessing the quality of quantitative studies
| Question | Criteria | Yes (2) | Partial (1) | No (0) | N/A |
|---|---|---|---|---|---|
| 1 | Question/objective sufficiently described? | ||||
| 2 | Study design evident and appropriate? | ||||
| 3 | Method of subject/comparison group selection or source of information/input variables described and appropriate? | ||||
| 4 | Subject (and comparison group, if applicable) characteristics sufficiently described? | ||||
| 5 | If interventional and random allocation was possible, was it described? | ||||
| 6 | If interventional and blinding of investigators was possible, was it reported? | ||||
| 7 | If interventional and blinding of subjects was possible, was it reported? | ||||
| 8 | Outcome and (if applicable) exposure measure(s) well defined and robust to measurement/misclassification bias? means of assessment reported? | ||||
| 9 | Sample size appropriate? | ||||
| 10 | Analytic methods described/justified and appropriate? | ||||
| 11 | Some estimate of variance is reported for the main results? | ||||
| 12 | Controlled for confounding? | ||||
| 13 | Results reported in sufficient detail? | ||||
| 14 | Conclusions supported by the results |
Appendix A displays checklist for assessing the quality of quantitative studies from Kmet et al. [26].
References
- 1.Weller J., Boyd M., Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J. 2014;90(1061):149–154. doi: 10.1136/postgradmedj-2012-131168. [DOI] [PubMed] [Google Scholar]
- 2.O'Leary K.J., Sehgal N.L., Terrell G., Williams M.V. Interdisciplinary teamwork in hospitals: a review and practical recommendations for improvement. J Hosp Med. 2012;7(1):48–54. doi: 10.1002/jhm.970. [DOI] [PubMed] [Google Scholar]
- 3.Courtney M. Effective Communication. Effective-Communication.Net. 2010. Available at: http://www.effective-communication.net/(Accessed on July 11 2014).
- 4.Larrabee J.H., Ostrow C.L., Withrow M.L., Janney M.A., Hobbs G.R., Burant C. Predictors of patient satisfaction with inpatient hospital nursing care. Res Nurs Health. 2004;27(4):254–268. doi: 10.1002/nur.20021. [DOI] [PubMed] [Google Scholar]
- 5.Tschannen D., Kalisch B.J. The impact of nurse/physician collaboration on patient length of stay. J Nurs Manag. 2009;17(7):796–803. doi: 10.1111/j.1365-2834.2008.00926.x. [DOI] [PubMed] [Google Scholar]
- 6.Riga M., Vozikis A., Pollalis Y., Souliotis K. MERIS (Medical Error Reporting Information System) as an innovative patient safety intervention: a health policy perspective. Health policy. 2015;119(4):539–548. doi: 10.1016/j.healthpol.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Fassier T., Azoulay E. Conflicts and communication gaps in the intensive care unit. Curr Opin Crit Care. 2010;16(6):654–665. doi: 10.1097/MCC.0b013e32834044f0. [DOI] [PubMed] [Google Scholar]
- 8.Williams M., Hevelone N., Alban R.F., Hardy J.P., Oxman D.A., Garcia E. Measuring communication in the surgical ICU: better communication equals better care. J Am Coll Surg. 2010;210(1):17–22. doi: 10.1016/j.jamcollsurg.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 9.Arriaga A.F., Elbardissi A.W., Regenbogen S.E., Greenberg C.C., Berry W.R., Lipsitz S. A policy-based intervention for the reduction of communication breakdowns in inpatient surgical care: results from a Harvard surgical safety collaborative. Ann Surg. 2011;253(253):849–854. doi: 10.1097/SLA.0b013e3181f4dfc8. [DOI] [PubMed] [Google Scholar]
- 10.Vardaman J.M., Cornell P., Gondo M.B., Amis J.M., Townsend-Gervis M., Thetford C. Beyond communication: the role of standardized protocols in a changing health care environment. Health Care Manage Rev. 2012;37(1):88–97. doi: 10.1097/HMR.0b013e31821fa503. [DOI] [PubMed] [Google Scholar]
- 11.The Joint Commission.Sentinel event data: root causes by event type. Retrieved from http://www.jointcommission.org/assets/1/18/Root_Causes_Event_Type_2004-2Q_2015.pdf.
- 12.Sutcliffe K.M., Lewton E., Rosenthal M.M. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194. doi: 10.1097/00001888-200402000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Saber D.A. Frontline registered nurse job satisfaction and predictors over three decades: a meta-analysis from 1980 to 2009. Nurs Outlook. 2014;62(6):402–414. doi: 10.1016/j.outlook.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Zhang L., Huang L., Liu M., Yan H., Li X. Nurse-physician collaboration impacts job satisfaction and turnover among nurses: a hospital-based cross-sectional study in Beijing. Int J Nurs Pract. 2016;22(3):284–290. doi: 10.1111/ijn.12424. [DOI] [PubMed] [Google Scholar]
- 15.Nelson G.A., King M.L., Brodine S. Nurse-physician collaboration on medical-surgical units. Medsurg Nurs. 2008;17(1):35–40. [PubMed] [Google Scholar]
- 16.Rosenstein A.H. Original research: nurse-physician relationships: impact on nurse satisfaction and retention. Am J Nurs. 2002;102(6):26–34. doi: 10.1097/00000446-200206000-00040. [DOI] [PubMed] [Google Scholar]
- 17.Thomson S. Nurse-physician collaboration: a comparison of the attitudes of nurses and physicians in the medical-surgical patient care setting. Medsurg Nurs. 2007;16(2):87–91. 104. [PubMed] [Google Scholar]
- 18.Rosenstein A.H., O'Daniel M. Disruptive behavior and clinical outcomes: perceptions of nurses and physicians. Am J Nurs. 2005;105(1):54–64. doi: 10.1097/00000446-200501000-00025. [DOI] [PubMed] [Google Scholar]
- 19.Despins L.A. Factors influencing when intensive care unit nurses go to the bedside to investigate patient related alarms: a descriptive qualitative study. Intensive Crit Care Nurs. 2017;4:3. doi: 10.1016/j.iccn.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Hartog C.S., Benbenishty J. Understanding nurse-physician conflicts in the ICU. Intens Ccare Med. 2015;41(2):331–333. doi: 10.1007/s00134-014-3517-z. [DOI] [PubMed] [Google Scholar]
- 21.Rothschild J.M., Landrigan C.P., Cronin J.W., Kaushal R., Lockley S.W., Burdick E. The Critical Care Safety Study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005;33(8):1694–1700. doi: 10.1097/01.ccm.0000171609.91035.bd. [DOI] [PubMed] [Google Scholar]
- 22.Donchin Y., Gopher D., Olin M., Badihi Y., Biesky M., Sprung C. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995;23(2):294–300. doi: 10.1097/00003246-199502000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Hu Y.Y., Arriaga A., Roth E.M., Peyre S.E., Swanson R.S., Osteen R.T. Protecting patients from an unsafe system. J Am Coll Surg. 2011;213(3) doi: 10.1097/SLA.0b013e3182602564. S111–S111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whittemore R. Combining evidence in nursing research; methods and implications. Nurs Res. 2005;54(54):56–62. doi: 10.1097/00006199-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Whittemore R., Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- 26.Kmet L.M., Lee R.C. 2004. Standard quality assessment criteria for evaluating primary research papers from a variety of fields AHFMRHTA Initiative20040213. [Google Scholar]
- 27.SPSS Inc . SPSS Inc; Chicago, IL: 2009. Released PASW statistics for windows, version 18.0. [Google Scholar]
- 28.Grossi D.B., Chaves T.C., Gonçalves M.C., Moreira V.C., Canonica A.C., Florencio L.L. Pressure pain threshold in the craniocervical muscles of women with episodic and chronic migraine: a controlled study. Arq Neuropsiquiatr. 2011;69(4):607–612. doi: 10.1590/s0004-282x2011000500007. [DOI] [PubMed] [Google Scholar]
- 29.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 30.Boyle D.K., Kochinda C. Enhancing collaborative communication of nurse and physician leadership in two intensive care units. J Nurs Adm. 2004;34(2):60–70. doi: 10.1097/00005110-200402000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Pronovost P., Berenholtz S., Dorman T., Lipsett P.A., Simmonds T., Haraden C. Improving communication in the ICU using daily goals. J Crit Care. 2003;18(18):71–75. doi: 10.1053/jcrc.2003.50008. [DOI] [PubMed] [Google Scholar]
- 32.Meurling L., Hedman L., Sandahl C., Felländertsai L., Wallin C.J. Systematic simulation-based team training in a Swedish intensive care unit: a diverse response among critical care professions. BMJ Qual Saf. 2013;22(6):485–494. doi: 10.1136/bmjqs-2012-000994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Narasimhan M., Eisen L.A., Mahoney C.D., Acerra F.L., Rosen M.J. Improving nurse-physician communication and satisfaction in the intensive care unit with a daily goals worksheet. Am J Crit Care. 2006;15(2):217–222. [PubMed] [Google Scholar]
- 34.Phipps L.M., Thomas N.J. The use of a daily goals sheet to improve communication in the paediatric intensive care unit. Intensive Crit Care Nurs. 2007;23(5):264–271. doi: 10.1016/j.iccn.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 35.Sluiter J.K., Bos A.P., Tol D., Calff M., Krijnen M., Frings-Dresen M.H. Is staff well-being and communication enhanced by multidisciplinary work shift evaluations? Intens Care Med. 2005;31(10):1409–1414. doi: 10.1007/s00134-005-2769-z. [DOI] [PubMed] [Google Scholar]
- 36.Agarwal S., Frankel L., Tourner S., Mcmillan A., Sharek P. Improving communication in a pediatric intensive care unit using daily patient goal sheets. J Crit Care. 2008;23(2):227–235. doi: 10.1016/j.jcrc.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 37.Ainsworth C.R., Pamplin J.C., Rn D.A., Linfoot J.A., Chung K.K. A bedside communication tool did not improve the alignment of a multidisciplinary team's goals for intensive care unit patients. J Crit Care. 2013;28(1):112–117. doi: 10.1016/j.jcrc.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 38.Rehder KJ, MD, Uhl TL, RN, CCNS, Meliones JN, et al. Targeted interventions improve shared agreement of daily goals in the pediatric intensive care unit. Pediatr Crit Care Med 2012; 13(1):6–10. [DOI] [PMC free article] [PubMed]
- 39.Sluiter J.K., Bos A.P., Tol D., Calff M., Krijnen M., Frings-Dresen M.H. Is staff well-being and communication enhanced by multidisciplinary work shift evaluations? Intensive Care Med. 2005;31(10):1409–1414. doi: 10.1007/s00134-005-2769-z. [DOI] [PubMed] [Google Scholar]
- 40.Narasimhan M., Eisen L.A., Mahoney C.D., Acerra F.L., Rosen M.J. Improving nurse-physician communication and satisfaction in the intensive care unit with a daily goals worksheet. Am J Crit Care. 2006;15(2):217–222. [PubMed] [Google Scholar]
- 41.Justice L.B., Cooper D.S., Henderson C., Brown J., Simon K., Clark L. Improving communication during cardiac ICU multidisciplinary rounds through visual display of patient daily goals. Pediatr Crit Care Med. 2016;17(7):677–683. doi: 10.1097/PCC.0000000000000790. [DOI] [PubMed] [Google Scholar]
- 42.Panesar R.S., Albert B., Messina C., Parker M. The effect of an electronic SBAR communication tool on documentation of acute events in the pediatric intensive care unit. Am J Med Qual. 2014;31(1):64–68. doi: 10.1177/1062860614553263. [DOI] [PubMed] [Google Scholar]
- 43.Lin F., Chaboyer W., Wallis M., Miller A. Factors contributing to the process of intensive care patient discharge: an ethnographic study informed by activity theory. Int J Nurs Stud. 2013;50(8):1054–1066. doi: 10.1016/j.ijnurstu.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 44.Lin F., Chaboyer W., Wallis M. A literature review of organisational, individual and teamwork factors contributing to the ICU discharge process. Aust Crit Care. 2009;22(1):29–43. doi: 10.1016/j.aucc.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 45.Murphy M., Curtis K., Mccloughen A. What is the impact of multidisciplinary team simulation training on team performance and efficiency of patient care? An integrative review. Australas Emerg Nurs J. 2015;19(1):44–53. doi: 10.1016/j.aenj.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 46.Miller K., Riley W., Davis S. Identifying key nursing and team behaviours to achieve high reliability. J Nurs Manag. 2009;17(2):247–255. doi: 10.1111/j.1365-2834.2009.00978.x. [DOI] [PubMed] [Google Scholar]
- 47.Robinson F.P., Gorman G., Slimmer L.W., Yudkowsky R. Perceptions of effective and ineffective nurse-physician communication in hospitals. Nurs Forum. 2010;45(3):206–216. doi: 10.1111/j.1744-6198.2010.00182.x. [DOI] [PubMed] [Google Scholar]
- 48.Deering S., Johnston L.C., Colacchio K. Multidisciplinary teamwork and communication training. Semin Perinatol. 2011;35(2):89–96. doi: 10.1053/j.semperi.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 49.Gittell J.H., Godfrey M., Thistlethwaite J. Interprofessional collaborative practice and relational coordination: improving healthcare through relationships. J Interprof Care. 2013;27(3):210–213. doi: 10.3109/13561820.2012.730564. [DOI] [PubMed] [Google Scholar]
- 50.Meester K.D., Verspuy M., Monsieurs K.G., Bogaert P.V. SBAR improves nurse–physician communication and reduces unexpected death: a pre and post intervention study. Resuscitation. 2013;84(9):1192–1196. doi: 10.1016/j.resuscitation.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 51.Joffe E., Turley J.P., Hwang K.O., Johnson T.R., Johnson C.W., Bernstam E.V. Evaluation of a problem-specific SBAR tool to improve after-hours nurse-physician phone communication: a randomized trial. Jt Comm J Qual Patient Saf. 2013;39(11):495–501. doi: 10.1016/s1553-7250(13)39065-5. [DOI] [PubMed] [Google Scholar]
- 52.Alves J., Magalhaes R., Thomas R.E., Goncalves O.F., Petrosyan A., Sampaio A. Is there evidence for cognitive intervention in Alzheimer disease? A systematic review of efficacy, feasibility, and cost-effectiveness. Alzheimer Dis Assoc Disord. 2013;27(3):195–203. doi: 10.1097/WAD.0b013e31827bda55. [DOI] [PubMed] [Google Scholar]