Abstract
Objective
The aim of this study was to summarize the evidence of health literacy and health outcomes in hypertensive patients.
Methods
Articles published in English were searched from six databases: MEDLINE, CINAHL, Embase, ERIC, psycINFO, and SCOPUS. The articles published up to September 2017 were included.
Results
Nineteen publications were included in the review. There was quality and consistent evidence that hypertensive patients with lower literacy had poorer knowledge. There was inconsistent evidence to show the relationship between health literacy and clinical outcomes, of systolic and diastolic blood pressure, and blood pressure control; behavioral outcomes, of self-care, self-efficacy, adherence; patient-physician interactions outcomes, of patient-physician communication, patient trust, involvement in decision making and other outcomes.
Conclusion
The person with low health literacy is likely to have poor knowledge of hypertension. However, there is insufficient evidence to suggest that health literacy is associated with outcomes of hypertension independently.
Keywords: Health literacy, Hypertension, Outcomes, Integrative review
1. Introduction
Health literacy (HL) is the degree to which individuals have the ability to obtain, process, and understand basic health information and services needed to make appropriate health care decisions [1]. People with adequate HL have the ability to read and understand educational written materials (functional skills); to communicate with health care professionals (interactive skills); to make appropriate health decisions (critical skills); and to measure medication dosages (numeracy skills) [2,3]. Low HL is recognized as a major risk factor in blood pressure control and has adverse effect on health outcomes [[4], [5], [6]]. Low HL rate is much higher in minority groups, among people who are poor or with less education or whose native language is not English in immigrant countries [[7], [8], [9]].
It is predicted that about 1.5 billion people worldwide will live with hypertension by 2025 [10]. Hypertension may cause stroke, heart disease [11], and renal dysfunction as a major risk predictor [12]. The global disease burden study showed that hypertension was the leading risk factor for disability-adjusted life-years among diseases [13]. Elevated blood pressure is a major public health problem worldwide [14]. Although extensive knowledge about ways to prevent and treat hypertension, its global incidence, and cardiovascular complications are not reduced, partly due to inadequacies in prevention of the disorder [15].
Hypertension can be controlled by changing lifestyles, such as increasing physical activity, keeping healthy weight, and having healthy diet [16]. So that it needs good self-management. In fact, the hypertensive patients will need to have higher HL in order to better understand the printed health educational materials. Although hypertensive patients with low HL could follow instructions with pictures, they can't communicate with health care professionals well [17]. In recent years, there have been increasing studies that focus on HL and health outcomes. However, research provides different and even conflicting results on hypertensive patients' blood pressure control, medication adherence and others.
2. Aims
To better understand the relationship between HL and health outcomes on hypertension, we conducted the integrative review.
3. Methods
3.1. Literature search methods
We conducted a search through MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Education Resources Information Center (ERIC), Embase, psycINFO, and SCOPUS databases. The searching time was from data base to September 2017. The searches were not limited to any type of published paper. Numeracy is a component of HL. But previously, numeracy and HL were used separately. If we excluded, it would have eliminated research studies worthy of examination. Adequate numeracy skills are very important for proper dosing, weight monitoring, management of sodium intake, and higher-level self-management skills such as titrating diuretics. The search strategy included Mesh and keywords that broadly represented the patient population under study (“hypertension” OR “high blood pressure” OR “elevate or raise blood pressure”), the terms that would capture the patients' abilities (“health literacy” OR literacy* OR “numeracy”) and the names of HL instruments, such as the Rapid Estimate of Adult Literacy in Medicine (“REALM”), the original form of the “TOFHLA”, the Short Version of the Test of Functional HL in Adults (“S-TOFHLA”), the Newest Vital Sign (“NVS”), the Medical Achievement Reading Test (“MART”), and the Short Assessment of HL for Spanish-speaking Adults (“SAHLSA”). Combined using the Boolean operator AND. Electronic searches were supplemented by manual searches.
Articles were included if (1) the sample included hypertensive patients with adult (aged 18 and over), (2) they focused on the relationship between HL or numeracy and health outcome, (3) they were published in English language, and (4) they were full-text articles. As low HL is very common in minority groups in immigrant countries, whose official language is English, so only English language studies were selected. The studies were excluded as follows: (1) the sample didn't just involve individuals with hypertension, (2) the studies didn't use any health literacy instrument, (3) the studies didn't report any of the outcomes of interest.
3.2. Search outcomes
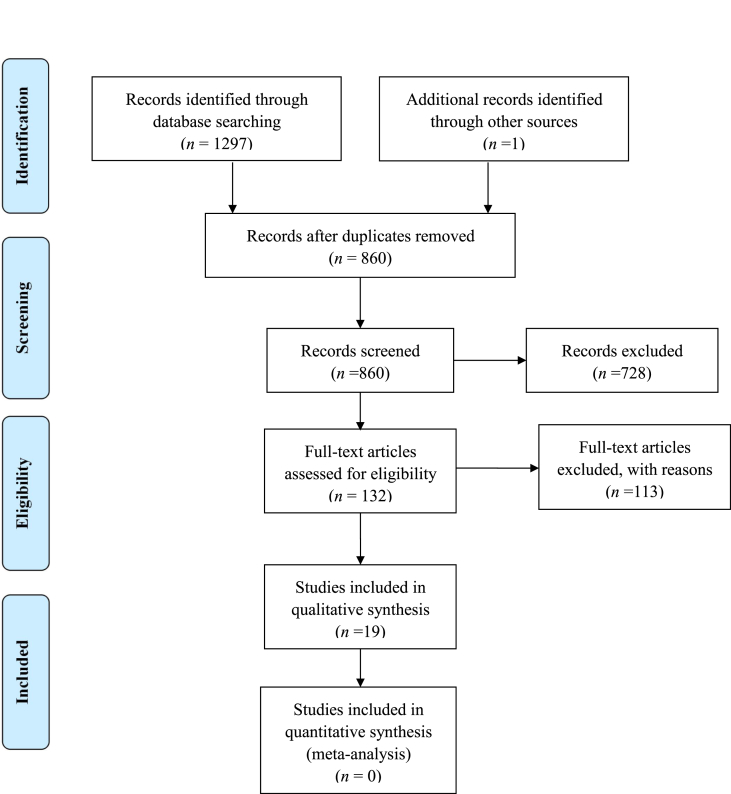
Totally 1,297 citations were yielded across all databases (see details in Fig. 1). Additional one study was included through the reference list screen. After removal of duplicates, 860 remained. Titles and abstracts were screened for relevance, and the main reason for the exclusion was that the article did not address HL or numeracy in people with hypertension. Based on that, 132 publications were included for full-text review. Of these, 19 publications met our criteria and were included.
Fig. 1.
PRISMA diagram of literature search and retrieval.
3.3. Data abstraction and quality assessment
Two reviewers screened the identified articles, read the full text of included papers, and performed data abstraction and quality assessment separately. A third author served as an adjudicator to help resolve discrepancies between the first two reviewers.
The general characteristics of the articles included design, HL measurement, quality rating, study sample, outcomes, analysis, and variables used in multivariate analysis (Table 1). We summarized evidence on the outcomes, including: clinical, behavioral, patient-provider relationship, and other outcomes. When data from the same study was presented in more than one manuscript, the recent publication would be chosen. Since all the identified studies were observational, each article was rated based on the criteria in the quality rating for observational studies by the Agency for Healthcare Research and Quality (AHRQ) [18] (Appendix A). The quality of studies was rated by 2 reviewers separately. The inter-rater agreement for including or excluding articles was 92.67% and Cohen's kappa was 0.84 (95%CI: 0.61–0.97).
Table 1.
The general characteristics of the articles.
| Study, Year (Reference) | Design | Instrument | Quality score | Study sample | Outcomes | Analysis | Variables Used in Multivariate Analysis |
|---|---|---|---|---|---|---|---|
| Aboumatar et al., 2013 [23] |
Cross-sectional | REALM | Fair | 275 patients from 14 USA primary care sites Mean age, 61 yr Female, 65.8% White, 36.7% |
BP control Medical decision making Patient-physician communication Patient's trust in their physician |
Fisher's exact tests Jonckheere-Terpstra tests Two sample t-tests Generalized linear models regression analysis |
Age, gender, race, education, annual income; blood pressure controlled; insurance pays prescriptions; age of physician seen, seen by female physician, seen by white physician |
| Ahn et al., 2016 [33] | Cross-sectional | REALM | Fair | 289 hypertensive patients from south Korea Mean age, 68.92 yr Female, 77.2% |
Medication adherence | Descriptive statics Hierarchical regression |
Age, gender, marital status, place of residence; self-efficacy, comorbidities |
| Bosworth et al., 2008 [26] |
Cross-sectional | REALM | Fair | 608 patients from 2 Duke University Health System Primary care clinics Mean age, 61yr Female, 365 Inadequate income, 18% Less than 12th grade, 36% |
BP control | Logistic regression Multivariable model |
Age, gender, recall; medication barriers score, medication non-adherent, low hypertension knowledge, often feel stressed, participatory decision-making, hypertension worry score, lack personal control of health, have emotion support, have home BP monitor, >5yr since high BP diagnosis, number of medication side effects, no weekly exercise, diabetes, current smoker, family history of hypertension |
| Gazmararian et al., 2003 [29] |
Cross-sectional | S-TOFHLA | Fair | 653 patients from Cleveland; Houston; South Florida, including Ft. Lauderdaleand Miami; and Tampa, USA Mean age, 72 yr Female, 61.7% Black, 16.1% Less than 12th grade, 67.1% Inadequate literacy, 24% |
Chronic disease knowledge | Description statistic Multiple linear regression analysis |
Age, disease duration, attended a class |
| Hall et al., 2016 [25] |
Cross-sectional | SAHLSA | Good | 45 Latino Migrant Seasonal Farm workers at Georgia and Ellenton Clinic, USA |
BP control Medication adherence BP knowledge BP self-care |
Descriptive statistic Hierarchical regression Mann-Whitney U test Logistic regression |
Education, blood pressure knowledge, perceived stress, acculturation level |
| Ingram et al., 2013 [32] |
Cross-sectional | REALM | Fair | 121 African American participants at USA Forsyth county Mean age, 59 yr Female, 50% Less than 12th grade, 70% |
Adherence to antihypertensive regiments |
Spearman Rho correlations Multiple regression analysis |
Age, education level, annual income; understanding of health/prescription information, health status, access to health care, comorbidities |
| Ko et al. 2013 [28] |
Cross-sectional | STOFHLA Singapore |
Fair | 306 patients at the Singapore Government-funded primary care clinic Mean age, 58 yr Female, 36.3% Chinese, 69.0% Duration of hypertension, 8yr |
Hypertension knowledge BP control |
Independent t-test Chi-squared test Multiple linear regression analysis |
Age, gender, ethnicity, education, housing type; comorbidities, |
| Lenahan et al., 2013 [34] |
Cross-sectional | S-TOFHLA | Fair | 215 participants from six USA primary care safety net clinics Mean age, 60 yr Female, 68.2% African American, 80.4% Limited literacy, 47.0% |
Medication non-adherence BP control Emergency department and Hospitalization visits |
One-way analysis of variance Chi-square analyses Generalized linear models Robust error estimation |
Age, gender, race; number of antihypertensive medications taken, number of chronic conditions, medication identification |
| Mcnaughton et al., 2014 [24] |
Cross-sectional | REALM | Fair | 423 participants an inner city primary care clinic in Atlanta, Georgia, USA Mean age, 64 yr Female, 56% African American, 91% Mean education, 12 yr |
BP control Medication adherence |
Descriptive statistics Logistic regression Planned exploratory linear regression |
Age, gender, race, education, employment status |
| Osborn et al., 2011 [30] |
Cross-sectional | S-TOFHLA | Fair | 330 patients from 6 primary USA care safety net clinics in Grand Rapids, Michigan; Chicago, Illinois; and Shreveport, Louisiana Mean age, 53 yr Female, 67.9% African American, 78.5% Less than 12th grade, 39.3% Married, 30.6% |
Hypertension knowledge Self-efficacy Self-care behaviors Health status |
Independent samples t-test Chi-square tests Two path analytic models |
Age, race, education; knowledge, self-efficacy, self-care |
| Pandit et al., 2009 [4] |
Cross-sectional | S-TOFHLA | Fair | 330 patients from 6 primary USA care safety net clinics in Grand Rapids, Michigan; Chicago, Illinois; and Shreveport, Louisiana. Mean age, 53 yr Female, 67.9% African American, 78.5% Less than 12th grade, 39.3% Married, 30.6% |
Hypertension knowledge BP control |
Chi-square Student's t-tests Multivariate logistic regression Mediation analysis |
Age, gender, race, marital status, employment status, insurance coverage; number of comorbid conditions, years treated for hypertension, clinic site, education level |
| Perez, 2015 [36] |
Cross-sectional | NVS | Good | 144 patients from various USA churches in the St. Louis, Missouri, and metro east Illinois area and Hispanic Community Mean age, 47 yr Female, 52.1% Less than 8 yr education, 30% Foreign-born Hispanics, 92.4% |
Illness perception | Hierarchical multiple regression Analysis of variance t-tests |
Age, gender, years of education, acculturation |
| Persell et al., 2007 [19] |
Cross-sectional | S-TOFHLA | Fair | 119 patients from three USA primary care clinics in Grand Rapids, Michigan affiliated with a federally qualified health center Mean age, 55 yr Female, 69.5% Black, 60.5% Less than 12th grade, 32.77% |
Blood pressure The number of medications for high blood pressure The number of medications patients can name them |
Chi-square tests Fisher's exact test Student's t-test Multivariable logistic regression |
Age, household income |
| Shi et al., 2017 [27] |
Cross-sectional | Chinese health literacy scale for hypertension | Fair | 360 patients from Jinyang community health center in Chengdu, China. Mean age, 66.6 yr Female, 55.8% |
Blood pressure control Health quality Risk for ischemic cerebral vascular disease Brachial-ankle artery pulse wave velocity |
Independent t tests Mann–Whitney U test Wilcoxon test Chi-square test Multiple logistic regression analysis |
Age, gender, education level, work status, monthly income; course of hypertension |
| Rao et al., 2015 [31] |
Cross-sectional | REALM Three-item numeracy scale |
Fair | 409 participants from 12 primary care clinics in central North Carolina, USA Mean age, 47.9 yr Female, 56% |
The completeness of home blood pressure monitoring | Student's t-test Logistic regression |
None |
| Wang et al., 2017 [35] |
Cross-sectional | BHLS | Fair | 882 patients from six China towns Mean age, 65.87 yr Female, 56.1% |
Health quality | Frequencies, percentages Mann–Whitney U test Kruskal–Wallis test Structural equation modeling |
Age, gender, education, family yearly income, family yearly medical costs, |
| Wannasirikul et al., 2016 [21] |
Cross-sectional | Functional, communicative, critical health literacy scale | 600 patients from a Primary Health Care Center in Sa Kaeo Province, Thailand Mean age, 65.3 yr Female, 75.8% |
Blood pressure Medication adherence |
Descriptive statistics Path analysis |
Age, gender, marital status, income per month, education level, occupation; perception on vision, perception on hearing, perception on mental health, duration of diagnosed HT, social support |
|
| Willens et al., 2013 [22] |
Cross-sectional | BHLS | Good | 23483 patients from three USA primary care clinics Mean age, 65 yr Female, 58.3% Black, 23.1% Less than high school, 15.2% |
Blood pressure BP control |
Bivariate analysis Wilcoxon rank-sum test Pearson's chi-square |
Age, gender, race, education years, location |
| Williams et al. 1998 [20] |
Cross-sectional | TOFHLA | Fair | 504 patients from 2 USA urban public hospitals Mean age, 59 yr Female, 87.5% Black, 59.52% Less than 12th grade, 83.9% |
Knowledge of disease | Chi-square tests One-way analysis of variance Multiple linear regression Multivariate logistic regression |
Age, sex, race, years of schooling, native language |
Note: REALM = the Rapid Estimate of Adult Literacy in Medicine; TOFHLA = the Test of Functional Health Literacy in Adults; SAHLSA = the Short Assessment of Health Literacy for Spanish-speaking Adults; S-TOFHLA = the Short Version of the Test of Functional Health Literacy in Adults; NVS = the Newest Vital Sign; BHLS = the Brief of Health Literacy Screen.
4. Results
4.1. Characteristics of included studies
All of them addressed the relationship between HL and health outcomes, and only one article addressed numeracy. All of the studies were cross-sectional and there were no intervention studies. Participants in all included articles were diagnosed with primary hypertension. However, whether the patients were in different grades of hypertension was not reflected. Fourteen studies were conducted in the United States, 2 were in China, 1 was in Singapore, 1 was in Thailand and 1 was in Korea. The mean age of patients was from 47yr to 72yr, and the sample sizes were from 45 to 23,483. The majority of studies focused on ethnic minority (African-American, Hispanic-American), low income or vulnerable populations.
4.2. HL and numeracy measures
The investigators used a different measurement to assess patients' HL status, and classified HL according to different levels or thresholds - either as a continuous measure or categories. HL was usually classified into inadequate, marginal, adequate or low versus adequate. Some studies combined inadequate and marginal HL into one category. In most of the studies, the analysis paid attention to the differences between the lowest and highest HL. The use of different research instruments (research questionnaires) in different included studies may be an important reason for contributing to different research findings across studies. The commonly used research instruments for HL assessments in the included studies were REALM, TOFHLA, S-TOFHLA, TOFHLA Singapore and SAHLSA, which were just used to assess the patients' functional HL (reading and numeracy ability). Research instruments such as NVS and BHLS were also used in four of the included studies, which could assess the patients' interactive and critical HL. The three-item numeracy scale was used in one study to assess patients' numeracy.
4.3. HL and health outcomes
Twenty two health outcomes were divided into four aspects: Clinical, behaviors, patient-physician communication, and other outcomes (see details in Table 2).
Table 2.
Health literacy and outcomes in hypertension: Summary of findings.
| Category | Outcome | Total# of studies by study design = N (# of studies Controlling for confounding = n1; # of studies NOT controlling for confounding = n2) |
Summary of results |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Studies controlling for confounding (n1) |
Studies not controlling for confounding (n2) |
||||||||
| Design | N (n1; n2) | Positive resultsa | Negative resultsb | Positive resultsa | Negative resultsb | ||||
| Clinic outcomes |
Systolic blood pressure | Cross-sectional | 4 (4; 0) | 2 | 2 | – | – | ||
| Diastolic blood pressure | Cross-sectional | 4 (4; 0) | 2 | 2 | – | – | |||
| Blood pressure control | Cross-sectional | 8 (7; 1) | 7 | 1 | – | 1 | |||
| Behavioral outcomes |
Hypertension knowledge | Cross-sectional | 5 (3; 2) | 3 | – | 2 | – | ||
| Self-efficacy | Cross-sectional | 1 (0; 1) | – | – | – | 1 | |||
| Self-care | Cross-sectional | 2 (1; 1) | – | 1 | – | 1 | |||
| Self-reported completeness of home blood pressure monitoring | Cross-sectional | 1 (1:0) | – | 1 | – | – | |||
| Compliance | Adherence to antihypertensive regiments | Cross-sectional | 1 (1; 0) | – | 1 | – | – | ||
| Medication adherence | Cross-sectional | 4 (4; 0) | 3 | 1 | – | – | |||
| Medical refill adherence | Cross-sectional | 1 (1; 0) | – | 1 | – | – | |||
| Patient- physician interaction |
Patient-physician communication | Cross-sectional | 1 (1; 0) | 1 | – | – | – | ||
| Patient trust | Cross-sectional | 1 (1; 0) | – | 1 | – | – | |||
| Involvement in decision making | Cross-sectional | 1 (1; 0) | – | 1 | – | – | |||
| Other outcomes |
identify their medications by name | Cross-sectional | 2 (2; 0) | 2 | – | – | – | ||
| Take the number of antihypertensive medication |
Cross-sectional | 1 (1; 0) | – | 1 | – | – | |||
| The agreement between self-reported and medical record-reported antihypertensive medication |
Cross-sectional | 1 (1; 0) | 1 | – | – | – | |||
| Illness perception |
Perception of personal control of hypertension |
Cross-sectional | 1 (0; 1) | – | – | 1 | – | ||
| perception that hypertension was a threatening illness |
Cross-sectional | 1 (0; 1) | – | – | – | 1 | |||
| Health status | Cross-sectional | 1 (0; 1) | – | – | – | 1 | |||
| Health quality | Cross-sectional | 2 (1:1) | 1 | – | 1 | – | |||
| Risk for ICVD | Cross-sectional | 1 (1; 0) | 1 | – | – | – | |||
| BaPWV | Cross-sectional | 1 (1; 0) | 1 | – | – | – | |||
ICVD: Ischemic Cerebral Vascular Disease.
BaPWV: brachial-ankle artery Pulse Wave Velocity.
Indicates that the study found a significant association between health literacy level and the outcomes.
Indicates that the study did not find a significant association between health literacy level and the outcomes.
4.3.1. HL and clinical outcomes
4.3.1.1. Systolic and diastolic blood pressure
Four studies examined the relationships between HL and systolic and diastolic blood pressure. Persell et al. used multivariable logistic regression to examine the relationship between HL and blood pressure. The model showed that HL was not associated with systolic and diastolic blood pressure after adjusting for age and household income [19]. For systolic and diastolic blood pressure, in a multivariable logistic regression model, HL was not significantly associated with systolic and diastolic blood pressure [20]. However, Wannasitikul et al. used structural equation modeling to identify the relationship between functional HL and systolic blood pressure, and found that functional HL had the significantly largest negative direct effect on systolic and diastolic blood pressure level (β = −0.14, P<0.05) [21]. In contrast to these findings, Willes et al. compared systolic blood pressure between two groups-encounters with BHLS≤9 and BHLS≥9 found that no significance between two group, however, in multivariable linear regression model, the BHLS sum scores is significantly associated with systolic and diastolic blood pressure [22].
4.3.1.2. Blood pressure control
Eight studies examined the relationship between HL and blood pressure control. Panit et al. used multivariable analyses to examine the relationship between HL and blood pressure control, and found that low HL was significantly associated with uncontrolled blood pressure [4]. Aboumatar et al. found that a lower percentage of patients with low versus adequate HL had controlled blood pressure [23]. In both unadjusted and adjusted logistic regression, HL was found to be an independent predictor of uncontrolled blood pressure [24]. In adjusted multivariable analyses, Willens et al. found that patients with higher HL had slightly lower odds of controlling blood pressure [22]. Hall et al. used Hierarchal and logistic regression to identify the relationship between HL and blood pressure control, and found that higher HL was associated with better blood pressure control [25]. In both unadjusted and adjusted logistic regression, Bosworth et al. found that low HL was significantly associated with poor blood pressure control [26]. In a multivariable logistic regression model, Shi et al. found that higher HL was associated with the higher rate of hypertension control [27]. Ko et al. used Chi-squared test to examine the association between HL and blood pressure control, and found that the achievement of target blood pressure was not associated with HL level [28].
4.3.2. HL and behavioral indicators and patient-reported outcomes
4.3.2.1. Hypertension knowledge
Five studies elucidated that lower HL was associated with less hypertension knowledge; three of which controlled for confounders [4,20,29] and two of which did not [28,30]. Panit et al. used multivariable analyses to examine the relationship between HL and hypertension knowledge, and low HL was found to be a significant independent predictor of poorer hypertension knowledge [4]. Ko et al. used Independent t-test to examine the association between HL and hypertension knowledge, and found that the hypertension knowledge scores were significantly associated with HL level (P<0.001) [28]. In a multivariable linear regression model, Willams et al. found that hypertension knowledge was strongly related to HL [20]. In multivariable analysis, Gazmararian et al. found that patients with inadequate HL knew significantly less about their disease than those with adequate HL [29]. Osborn et al. performed path analyses to identify the relationship between HL and hypertension knowledge, and found that higher HL scores were associated with more hypertension knowledge [30].
4.3.2.2. Self-efficacy
Osborn et al. performed path analyses to identify the relationship between HL and self-efficacy, and found that HL scores were not directly associated with self-efficacy [30].
4.3.2.3. Self-care
In a Hierarchal and logistic regression model, Hall et al. found that HL was not significantly associated with self-care [25]. Osborn et al. performed path analyses to identify the relationship between HL and self-care, and found that HL scores were not directly associated with self-care [30].
4.3.2.4. Self-reported completeness of home blood pressure monitoring
An adjusted study [31] found that the completeness of home blood pressure monitoring was not associated with HL level. In an adjusted logistic regression model, Rao et al. found that HL was not associated with completeness of home blood pressure monitoring, which was calculated as the percentage of total number of recorded measurements that were supposed to be taken by the patients during the 2 week period that patients performed home blood pressure monitoring [31].
4.3.2.5. Compliance
Five studies examined the relationship between HL and compliance. McNaughton et al. used planned exploratory linear regression analysis to identify the relationship between HL and medication adherence and cumulative medication gap (CMG), and found that higher HL was associated with lower self-reported medication adherence, and not associated with CMG [24]. Wannasitikul et al. used structural equation modeling to identify the relationship between HL and medication adherence, and found that HL had not only a direct effect on medication adherence but was also the mediator [21]. Hall et al. used Hierarchal and logistic regression to identify the relationship between HL and medication adherence, and found that HL was not associated with medication adherence [25]. Ingram et al. found that compliance to antihypertensive regiments was not related to HL [32]. Ahn et al. performed hierarchical regression analysis, and found that patients with higher HL was more likely to have higher medication adherence [33].
4.3.3. HL and patient-physician interaction indicators
4.3.3.1. Patient-physician communication
Aboumatar et al. used generalized linear model regress analysis to identify the relationship between HL and patient-physician communication behaviors, and found that patients with low HL asked their physicians fewer questions about medical, but not psychosocial issues. And no statistically significant differences in total number of patient or physician statements, visit length, or verbal dominance ratio between low and adequate HL group [23].
4.3.3.2. Patient trust
One study explored whether patient trust their physician was significantly different by HL. In generalized linear model regress analysis, Aboumatar et al. found that whether patient trust their physician was not related to HL level [23].
4.3.4. Involvement in decision making
In generalized linear model regress analysis, Aboumatar et al. found that patients with low or adequate HL had no significant differences in their desire of making medical decision with their physician [23].
4.3.5. Other outcomes
4.3.5.1. The number of medications to be consumed
In a multivariable logistic regression model, Persell et al. found that no significant differences between HL and the number of antihypertensive agent that was consumed by patient [19].
4.3.5.2. The ability to identify medication by name
Persell et al. used multivariable logistic regression analysis to identify the relationship between HL and the ability to identify their medication by name, and found that patients with higher HL had more possibility to identify their medication by name [19]. Lenahan et al. performed generalized linear models analysis, and found that HL was associated with the ability to properly name medications [34].
4.3.5.3. The agreement between patient-reported and medical record-reported antihypertensive medications
In a multivariable logistic regression model, Persell et al. found that higher HL was associated with higher agreement between patient-reported and medical record-reported antihypertensive medications [19].
4.3.5.4. Health quality
Wang et al. performed structural equation model analysis to examine the relationship between HL and health quality, and found HL have a significant impact on health quality [35]. Shi et al. found that patients with high HL had better health quality than those with low HL [27].
4.3.5.5. The risk for ischemic cerebral vascular disease (ICVD)
Shi et al. found that compared with High HL, patients with low HL had a much higher risk for ICVD [27].
4.3.5.6. The brachial-ankle artery pulse wave velocity (baPWV)
Shi et al. found that the average baPWV values of the high HL group were lower than the low HL group [27].
4.3.5.7. Illness perceptions
Perez et al. performed hierarchical multiple regression to identify the relationship between HL and illness perceptions, and found that higher HL was associated with perceived better in personal control of hypertension and misconception that hypertension was a life threatening illness [36].
4.3.5.8. Health status
Osborn et al. performed path analyses to identify the relationship between HL and health status, and found that no significant relationship between HL and health status [30].
4.4. Numeracy and health outcomes
Only one research examined the relationship between numeracy and health outcomes (see details in Table 3).
Table 3.
Numeracy and outcomes in hypertension: Summary of findings.
| Category | Outcome | Total# of studies by study design = N (# of studies Controlling for confounding = n1; # of studies NOT controlling for confounding = n2) |
Summary of results |
||||
|---|---|---|---|---|---|---|---|
| Studies controlling for confounding (n1) |
Studies not controlling for confounding (n2) |
||||||
| Design | N (n1; n2) | Positive results* | Negative results† | Positive results* | Negative results† | ||
| Behavioral outcomes |
Self-reported completeness of home blood pressure monitoring | Cross-sectional | 1 (1; 0) | – | 1 | – | – |
In an adjusted logistic regression model, Rao et al. found that higher numeracy was associated with more completeness of home blood pressure monitoring [31].
4.5. Limitation of included studies
Several discrepancies were found in our research. First, the measuring tool [37] and the marginal values between different HL levels were different [38]. The psychometric properties of the instruments in the included studies were different. Most of them focused on functional skills, and only two instruments assessed the patients' interactive and critical HL. Second, only several articles in the review were solely focused on hypertensive patients, while others included patients with other disease, such as diabetes. The target for systolic blood-pressure is different between patients with hypertension and diabetes. Third, there were limited articles addressed the relationship between HL and self-efficacy, patient trust and decision making.
Furthermore, there was another underlying factor for the discrepancy. It was adjusting for confounding factors which can help analyze the cause of poor health outcomes [39]. Most of the articles adjusted for age, sex, nation, income, and educational level. However, a few articles also adjusted for hypertension duration, attending classes about the disease condition and many others. There were likely to be over adjustment, if the factors were the intermediate variable between HL and outcomes [40,41].
5. Discussion
The purpose of our study was to summarize the evidence of HL and health outcomes in hypertensive patients. We identified several outcomes associated with HL in hypertensive patients. The relationship between HL and hypertension knowledge was evident. This could help improve knowledge of hypertensive patients.
All the included studies were cross-sectional and there were no intervention studies. A potential cause for investigators' preference for conducting non-experimental studies rather than experimental and interventional studies may be due to the unclear relationship between HL and health outcomes.
Most of the studies conducted in the developed countries, and only three research conducted in developing countries. Further research is needed to conduct in developing countries and focus on intervention. The registered nurses worked in these countries also have the responsibility of knowing the HL level in hypertensive patients and take measures tailored to the patients.
In our study, many researchers believed that patients with higher HL were likely to have more knowledge [4,20,[28], [29], [30]]. It is not surprising, as literacy skills embody one's ability to obtain, and comprehend health information [42,43].
With regard to self-care, two studies showed that it was not related to HL. The result was different from previous studies [44,45]. This was partly because of the previous studies were based on an elderly sample.
Kripalani found that patients with adequate literacy were more likely to identify their medications by name [46]. We got the same results. It was due to patients with limited literacy often rely on pill characteristics for identification [47].
With regard to quality of life, Wang et al. found that hypertension markedly impaired quality of life, and comorbidity further deteriorated quality of life [48]. It was due to HL influenced the mental component summary.
In our research, several differences were found between HL and clinical outcomes (systolic or diastolic blood pressure and blood pressure control). Two studies that controlled for confounders (age, gender, race, educational and financial situation) showed that HL was not associated with systolic or diastolic blood pressure [19,20]. The other adjusted study [22] revealed that higher HL was associated with higher systolic or blood pressure. On the contrary, another adjusted study [21] found that higher health literacy was relevant to lower systolic or diastolic blood pressure. This was probably because the patients and instruments involved in these studies were different. Further studies are required to further identify the relationship between them.
Also, there were limited articles concentrate on the relationship between HL and patient-physician interaction and other outcomes. Future studies would be focused on interactive skills, critical skills, and numeracy skills in hypertensive patients.
There were also systematic reviews of HL and health outcomes. Most of them focused to investigate the patients from specific study population [[49], [50], [51], [52]], such as older Latinos with heart failure [53], diabetic patients [54], and emergency room patients [55]. Others focused to investigate the relationship between HL and cost, and the use of health care service [56]. All have shown similar results on the relationship between HL and knowledge.
6. Conclusion
Our review indicates that the current understanding of the relationship between HL and health outcomes on hypertensive patients is limited. We found that the person with low HL is likely to have poor knowledge of hypertension. However, it is insufficient to say that HL is associated with hypertension-related care outcomes independently.
Further studies can build on previous work to further clarify the relationship between HL and health outcomes not only in developed countries, but also in developing countries. More HL instruments (research questionnaires) should be used to measure the patients' functional, interactive, numeracy and critical skills to rich the results. Future work should also examine more closely whether poor HL is the cause of adverse outcomes in hypertensive patients or it is just a marker for other problems which are the actual causes of poor health.
Author contributions
Yan Wang and Shaoying Du conceptualized the idea for this review and obtained research funding. Yan Wang, Shaoying Du, Xiaojing Du and Ran Xie contributed to the development of the search strategy and the study selection. Yi Zhou and Cong Fu contributed to the data extraction, quality assessment and the data synthesis. Yan Wang is the guarantor and Shaoying Du drafted the manuscript. Yi Zhou, Cong Fu, Xiaojing Du and Ran Xie revised he manuscript. All authors read and approved the final manuscript.
Funding
The work was supported by the Health and Family Planning Commission of Hebei (No. 20150485) in China.
Conflicts of interest
None.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ijnss.2018.06.001.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.U.S. Department of Health and Human Services. Healthy people 2010: Understanding and improving health (Chapter 11: Health communication). Washington, DC: Author; 2000. Retrieved September 10 2008, from http://www.healthypeople.gov/Document/HTML/Volume1/11HealthCom.htm.
- 2.Berkman N., Terry D., McCormack L. Health literacy: what is it? J Health Commun. 2010;15:9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- 3.Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67:2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 4.Pandit A.U., Tang J.W., Bailey S.C., Davis T.C., Bocchini M.V., Persell S.D. Education, literacy, and health: mediating effects on hypertension knowledge and control. Patient Educ Counsel. 2009;75(3):381–385. doi: 10.1016/j.pec.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Mcnaughton C.D., Jacobson T.A., Kripalani S. Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Counsel. 2014;96(2):165. doi: 10.1016/j.pec.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Son Y.J., Song E.K. Impact of health literacy on disease-related knowledge and adherence to self-care in patients with hypertension. J Korean Acad Nurs. 2012;19:6–15. [Google Scholar]
- 7.Wolf M., Gazmararian J., Baker D. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 8.Sudore R., Mehta K., Simonsick A., Harris T.B., Newman A.B., Satterfield S. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. 2006;54 doi: 10.1111/j.1532-5415.2006.00691.x. 770-6. [DOI] [PubMed] [Google Scholar]
- 9.Schultz S., Kopec J. Vol. 14. 2003. Impact of chronic conditions. Health Reports; pp. 41–56. Statistics Canada catalogue no. 82-003-XIE. [PubMed] [Google Scholar]
- 10.Kearney P.M., Whelton M., Reynolds K., Muntner P., Whelton P.K., He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 11.Deaton C., Froelicher E.S., Wu L.H., Ho C., Shishani K., Jaarsma T. The global burden of cardiovascular disease. Eur J Cardiovasc Nurs. 2011;26:5–14. doi: 10.1016/S1474-5151(11)00111-3. [DOI] [PubMed] [Google Scholar]
- 12.Huang Y., Cai X., Zhang J., Mai W., Wang S., Hu Y. Prehypertension and incidence of ESRD: a systematic review and meta analysis. Am J Kidney Dis. 2014;63:76–83. doi: 10.1053/j.ajkd.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 13.GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388:1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization International society of hypertension writing group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21(11) doi: 10.1097/00004872-200311000-00002. 1983-92. [DOI] [PubMed] [Google Scholar]
- 15.Olsen M.H., Angell S.Y., Asma S., Boutouyie P., Burger D., Chirinos J.A. A call to action and a life course strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. 2016;388:2665–2712. doi: 10.1016/S0140-6736(16)31134-5. [DOI] [PubMed] [Google Scholar]
- 16.Poulter N.R., Prabhakaran D., Caulfield M. Hypertension. Lancet. 2015;386:801–812. doi: 10.1016/S0140-6736(14)61468-9. [DOI] [PubMed] [Google Scholar]
- 17.White R., Wolff K., Cavanaugh K., Rothman R. Addressing health literacy and numeracy to improve diabetes education and care. Diabetes Spectr. 2010;23:238–243. doi: 10.2337/diaspect.23.4.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Viera A., Crotty K. Agency for Healthcare Research and Quality; Rockville, MD: 2011. Health literacy interventions and outcomes: an update of the literacy and health outcomes systematic review of the literature. Evidence Report/Technology Assessment no.199. [Google Scholar]
- 19.Persell S.D., Osborn C.Y., Richard R., Skripkauskas S., Wolf M.S. Limited health literacy is a barrier to medication reconciliation in ambulatory care. J Gen Intern Med. 2007;22(11):1523–1526. doi: 10.1007/s11606-007-0334-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams M.V., Baker D.W., Parker R.M., Nurss J.R. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158(2):166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 21.Wannasirikul P., Termsirikulchai L., Sujirarat D. Health Literacy, medication adherence, and blood pressure level among hypertension older adults treated at primary health care centers. Southeast Asian J Trop Med Publ Health. 2016;47(1):109–120. [PubMed] [Google Scholar]
- 22.Willens D.E., Kripalani S., Schildcrout J.S., Cawthon C., Wallston K., Mion L.C. Association of brief health literacy screening and blood pressure in primary care. J Health Commun. 2013;18(17):129–142. doi: 10.1080/10810730.2013.825663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aboumatar H.J., Carson K.A., Beach M.C., Roter D.L., Cooper L.A. The impact of health literacy on desire for participation in healthcare, medical visit communication, and patient reported outcomes among patients with hypertension. J Gen Intern Med. 2013;28(11):1469–1476. doi: 10.1007/s11606-013-2466-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mcnaughton C.D., Jacobson T.A., Kripalani S. Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Counsel. 2014;96(2):165–170. doi: 10.1016/j.pec.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hall E., Lee S.Y., Clark P.C., Perilla J. Social Ecology of adherence to hypertension treatment in latino migrant and seasonal farmworkers. J Transcult Nurs. 2016;27(1):33–41. doi: 10.1177/1043659614524788. [DOI] [PubMed] [Google Scholar]
- 26.Bosworth H.B., Powers B., Grubber J.M., Thorpe C.T., Olsen M.K., Orr M. Racial differences in blood pressure control: potential explanatory factors. J Gen Intern Med. 2008;23(5):692–698. doi: 10.1007/s11606-008-0547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shi D., Li J., Wang Y., Wang S., Liu K., Shi S. Association between health literacy and hypertension management in a Chinese community: a retrospective cohort study. Intern Emerg Med. 2017;12(2):1–12. doi: 10.1007/s11739-017-1651-7. [DOI] [PubMed] [Google Scholar]
- 28.Ko Y., Balasubramanian T.D., Wong L., Tan M.L., Lee E., Tang W.E. Health literacy and its association with disease knowledge and control in patients with hypertension in Singapore. Inc Jo Cardiol. 2013;168(4):116–117. doi: 10.1016/j.ijcard.2013.08.041. [DOI] [PubMed] [Google Scholar]
- 29.Gazmararian J.A., Williams M.V., Peel J., Baker D.W. Health literacy and knowledge of chronic disease. Patient Educ Counsel. 2003;51(3):267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 30.Osborn C.Y., Paascheorlow M.K., Bailey S.C., Wolf M.S. The mechanisms linking health literacy to behavior and health status. Am J Health Behav. 2011;35(1):118–128. doi: 10.5993/ajhb.35.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rao V.N., Tuttle L.A., Sheridan S.L., Turrle L.A., Lin F.C., Shimbo D. The effect of numeracy level on completeness of home blood pressure monitoring. J Clin Hypertens. 2015;17(1):39–45. doi: 10.1111/jch.12443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ingram R.R., Ivanov L.L. Examining the association of health literacy and health behaviors in African American older adults: does health literacy affect adherence to antihypertensive regimens? J Gerontol Nurs. 2013;39(3):1–10. doi: 10.3928/00989134-20130201-01. [DOI] [PubMed] [Google Scholar]
- 33.Ahn Y.H., Ham O.K. Factors associated with medication adherence among medical-aid beneficiaries with hypertension. West J Nurs Res. 2016;38(10):1–15. doi: 10.1177/0193945916651824. [DOI] [PubMed] [Google Scholar]
- 34.Lenahan J.L., McCarthy D.M., Davis T.C., Curtis L.M., Serper M., Wolf M.S. A drug by any other name: patients' ability to identify medication regimens and its association with adherence and health outcomes. J Health Commun. 2013;18:31–39. doi: 10.1080/10810730.2013.825671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang C., Lang J., Xuan L., Li X., Zhang L. The effect of health literacy and self-management efficacy on the health-related quality of life of hypertensive patients in a western rural area of China: a cross-sectional study. Int J Equity Health. 2017;16(1):58. doi: 10.1186/s12939-017-0551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Acculturation Perez A. Health literacy, and illness perceptions of hypertension among hispanic adults. J Transcult Nurs. 2015:26. doi: 10.1177/1043659614524785. [DOI] [PubMed] [Google Scholar]
- 37.Griffin J.M., Partin M.R., Noorbaloochi S., Grill J.P., Saha S., Snyder A. Variation in estimates of limited health literacy by assessment instruments and non-response bias. J Gen Intern Med. 2010;25(7):675–681. doi: 10.1007/s11606-010-1304-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wolf M.S., Feinglass J., Thompson J., Baker D.W. In search of ‘low health literacy’: threshold vs. gradient effect of literacy on health status and mortality. Soc Sci Med. 2010;70(9):1335–1341. doi: 10.1016/j.socscimed.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 39.Dewalt D.A., Berkman N.D., Sheridan S., Lohr K.N., Pignon M.P. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Osborn C., Cavanaugh K., Wallston K., Rothman R. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun. 2010;15:146–158. doi: 10.1080/10810730.2010.499980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bohanny W., Vivienne-Wu S.F., Liu C.Y., Yeh S.H., Tsay S.L., Wang T.J. Health literacy, self-efficacy, and self-care behaviors in patients with type 2 diabetes mellitus. J Am Assoc Nurse Practitioners. 2013;25(9):495–502. doi: 10.1111/1745-7599.12017. [DOI] [PubMed] [Google Scholar]
- 42.Gazmararian J.A., Baker D.W., Honig E.G., Lee T.M., Nowlan A. Health literacy and knowledge of chronic disease. Patient Educ Counsel. 2003;51:267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 43.Williams M.V., Baker D.W., Honig E.G., Lee T.M., Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–1015. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 44.Hanchate A.D., Ash A.S., Gazmararian J.A., Wolf M.S., Paasche-Orlow M.K. The Demographic Assessment for Health Literacy(DAHL): a new tool for estimating associations between health literacy and outcomes in national surveys. J Gen Intern Med. 2008;23(10):1561–1566. doi: 10.1007/s11606-008-0699-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cho Y.I., Lee S.Y., Arozullah A.M., Crittenden K.S. Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med. 2008;66(8):1809–1816. doi: 10.1016/j.socscimed.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 46.Kripalani S., Henderson L.E., Chiu E.Y., Robertson R., Kolm P., Jacobson T.A. Predictors of medication self-management skill in a low-literacy population. J Gen Intern Med. 2006;21:852–856. doi: 10.1111/j.1525-1497.2006.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wolf M.S., Davis T.C., Marin E., Arnold C., Bennett C.L. A qualitative study of literacy and patient response to HIV medication adherence questionnaires. J Health Commun. 2005;10:1–9. doi: 10.1080/10810730500228631. [DOI] [PubMed] [Google Scholar]
- 48.Wang R., Zhao Y., He X., Ma X., Yan X., Sun Y. Impact of hypertension on health-related quality of life in a population-based study in Shanghai, China. Publ Health. 2009;123(8):534–539. doi: 10.1016/j.puhe.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 49.Easton P., Entwistle V.A., Williams B. Health in the ‘hidden population’ of people with low literacy. A systematic review of the literature. BMC Publ Health. 2010;5(10):459. doi: 10.1186/1471-2458-10-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sanders L.M., Federico S. Klass, Abrams MA, Dreyer B. Literacy and child health: a systematic review. Arch Pediatr Adolesc Med. 2009;163(2):131–140. doi: 10.1001/archpediatrics.2008.539. [DOI] [PubMed] [Google Scholar]
- 51.DeWalt D.A., Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124:265–274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 52.Keller D.L., Wright J., Pace H.A. Impact of health literacy on health outcomes in ambulatory care patients: a systematic review. Ann Pharmacother. 2008;42(9):1272–1281. doi: 10.1345/aph.1L093. [DOI] [PubMed] [Google Scholar]
- 53.Delgado J.M., Ruppar T.M. Health literacy in older Latinos with heart failure: a Systematic review. J Cardiovasc Nurs. 2017;32:125–134. doi: 10.1097/JCN.0000000000000314. [DOI] [PubMed] [Google Scholar]
- 54.Sayah F.A., Majumdar S.R., Williams B., Robertson S., Johnson J.A. Health literacy and health outcomes in diabetes: a Systematic Review. J Gen Intern Med. 2013;28(3):444–452. doi: 10.1007/s11606-012-2241-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Herndon J.B., Chaney M., Carden D. Health literacy and emergency department outcomes: a systematic review. Ann Pharmacother. 2011;57(4):334–345. doi: 10.1016/j.annemergmed.2010.08.035. [DOI] [PubMed] [Google Scholar]
- 56.Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Pharmacother. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.