Abstract
Objectives
The prevalence and burden of disease of depression necessitates effective and accessible treatment options worldwide. Since April 2016, Japanese national health insurance has covered nurse-administered cognitive behavioral therapy (CBT) for mood disorders. However, empirical support for nurse-led CBT for depression in Asian countries, especially in Japan, is still lacking. This preliminary study aimed to examine the feasibility and acceptability of nurse-led group CBT for Japanese patients with depression.
Methods
In this single-arm study, we evaluated the effects of a 6-week group CBT, led by trained nurses, on patients with major depression. The primary outcome was the Beck Depression Inventory-II (BDI-II). Assessments were conducted at the beginning and end of the intervention.
Results
Of 25 participants screened, 23 were eligible for the study (of these, three dropped out during the trial but were included in the analysis). Nurse-led group CBT led to significant improvements in the severity of depression (BDI-II, P < 0.001). The mean total BDI-II score improved from 23.1 (SD = 7.56) to 12.4 (SD = 8.57), and the pre-to post-effect size was large (Cohen's d = 1.33). After CBT, 45% of the participants were judged to be treatment responders, and 34% met the remission criteria.
Conclusions
Our preliminary findings indicate that 6 weeks of nurse-led group CBT produced a favorable treatment outcome for individuals with major depression in a Japanese clinical setting. The results of this study might encourage more Asian nurses to provide CBT as a part of their nursing practice. Further controlled trials that address the limitations of this study are required.
Keywords: Behavior therapy, Cognitive therapy, Depressive disorder, Group psychotherapy, Nursing care
1. Introduction
Depression is a serious global social problem. According to the World Health Organization survey of the global burden of diseases, depression was ranked as the third most serious problem worldwide in 2004, and by 2030, depression is projected to become the leading burden of disease [1]. In Japan, the Japanese Ministry of Health, Labor, and Welfare estimated the number of individuals with depression to be greater than one million in 2009. Thus, effective and accessible treatment options for depression are greatly needed.
Cognitive behavioral therapy (CBT) has consistently been shown to be effective for depression in a large database of clinical trials [[2], [3], [4]], and patients often prefer psychological treatment to pharmacotherapy [5]. In Japan, CBT was introduced in the late 1980s. Since then, awareness of CBT has gradually spread, not only among health care professionals but also the general public. In April 2010, the inclusion of CBT for mood disorders in the national health insurance scheme marked a milestone in Japanese mental health services, where pharmacotherapy has historically been much more common. However, patient access to CBT services is extremely limited owing to an insufficient number of CBT providers in the current health insurance system, which requires CBT to be conducted only by skilled psychiatrists [6]. To solve this problem, the subsequent medical fee revision in FY 2016 expanded the range of eligible CBT providers to include nurses.
In several countries, especially in the United Kingdom, nurses have played a significant role in disseminating CBT. In the 1970s, registered mental health nurses became the first group to receive a three-year systematic CBT training primarily for selected adult neurotics at the Maudsley Hospital in London. Marks et al. [7] reported that these early behavioral nurse therapists were as effective at delivering CBT as psychiatrists and psychologists. Further, a 25-year follow-up of nurses administering CBT found a considerable contribution to mental health service provision, specifically in primary care settings [8]. Other studies have also demonstrated the efficacy of nurse-led CBT for a wide range of mental disorders [[9], [10], [11], [12], [13], [14]]. According to a document from Horatio (European Psychiatric Nurses), currently in the UK 90% of all CBT therapists have a psychiatric nursing background [15].
Incorporating CBT (effective psychotherapeutic approach) into nursing practice is the ideal vehicle for the nurse to use to guide counseling and education interactions with individuals. CBT gives nurses another method to use in addition to existing nursing practice. One of the earliest papers [16] described how psychological technologies and nursing fit together well, and how nurses could use additional skills to develop better relationships with their patients. Some of the fundamentals of CBT are the same as those of nursing: empathy, building relationships with patients, and engaging with them. The 2012 document from the Health Service Executives (the Irish public health provider) [17] – in an effort to change the orientation of the mental health services to a recovery approach – lists the skills and competencies required by mental health nurses to improve patient experiences and outcomes: Assessment skills, Risk Assessment skills, Psychosocial interventions, Interpersonal and communication skills, and Teamwork skills. Most of these are incorporated in CBT training. Basic CBT approaches can be used by nurses in many different settings, and indeed by nurses who want to bridge the mental/physical services gap in areas such as pain management, post-natal depression, gynecological disorders etc. One of the benefits of having nurses trained in CBT approaches is the implementation of CBT for depression in behavioral activation. Socratic questioning is also an useful technique which helps patients figure out their own problems and empowers them. Our previous study also supports the idea that there is a positive association between high-involvement in CBT (e.g. experience of receiving CBT training and providing CBT) and high levels of professional autonomy among Japanese psychiatric nurses [18]. Today, effective psychotherapeutic approaches (i.e. CBT) provided by nurses are viewed as being linked to a holistic nursing framework [19], and it has become clear that nurses providing psychotherapy for mental disorders are associated with being clinical nurse specialists as well as advanced nurse practitioners.
However, in Japan, there are some comparative studies of CBT in the field of psychiatric nursing, but CBT therapists are not only nurses in most studies [20]; thus, empirical support for the clinical effectiveness of nurse-led CBT is still lacking. Therefore, the purpose of the present study is to report the preliminary outcomes of a nurse-led group CBT program in a sample of Japanese patients with depression. The study had a single-arm, uncontrolled trial design. We employed CBT in a group format because it has several advantages over an individual format: higher cost- and time-efficiency, beneficial effects of group cohesion and normalization, provision of additional opportunities to engage in behavioral experiments, learning from others, and functioning as a co-therapist [11,[21], [22], [23]].
2. Material and methods
2.1. Participants
This study was carried out from April 2014 to December 2015, and the participants were recruited at one psychiatric hospital and one general hospital in Miyazaki Prefecture, Japan. The criteria for study inclusion were: a primary diagnosis of major depressive disorder (MDD) according to the Diagnostic and Statistical Manual of Mental Disorders-4th Edition (DSM-Ⅳ), assessed by their primary psychiatrist; having depressive symptoms (Beck Depression Inventory-II [BDI-II] score > 10) [24]; and being aged 18–65 years. The exclusion criteria were: organic brain disorders, alcohol dependency/abuse, dementia, active suicidality, and primary personality disorder.
The participants were required to gain the permission of their primary psychiatrist to participate in the study, and written informed consent was obtained from all participants after the study procedures had been fully explained. This study has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki). The study protocol was approved by the Ethics Committee of University of Miyazaki (reference number: 995), and was registered at the UMIN Clinical Trials Registry (ID: UMIN000032393).
2.2. Intervention
We used the CBT protocol for depression introduced by the Association of Cognitive Behavioral Group Therapy (2011), as a reference for generating our group CBT program [[25], [26], [27]]. The program had six 90-min weekly sessions, as shown in Table 1. Across the six sessions, the following elements were included: motivation and psychoeducation, cognitive techniques, behavioral techniques, and problem-solving techniques. Homework was assigned after every session. Each group contained 3–4 participants.
Table 1.
Overview of the program.
| Session | Purpose | Agenda/content | Homework/tool |
|---|---|---|---|
| 1 |
|
|
|
| 2 |
|
|
|
| 3 |
|
|
|
| 4 |
|
|
|
| 5 |
|
|
|
| 6 |
|
|
|
The program sessions were conducted by one leading nurse and one or two facilitators. The leading nurse especially contributed to set and follow a main agenda, presenting information as an educator (e.g. introducing CBT techniques), inviting and seeking feedback, summarizing the discussion and key leanings, and managing time. The facilitator (s) especially contributed to provide more detailed support for members' work and discussion during the program (e.g. individual support such as identifying key cognition and behavior, assigning and reviewing homework, and group facilitation). The leading nurses were two of the authors (HT and YS), who both had previously led more than three other group CBT programs. Facilitators were nurses working in outpatient departments and/or clinical psychologists. All leading nurses and facilitators had more than 5 years of clinical experience and 2 years of CBT training experience.
The participants were permitted to continue concomitant medication regimens provided by their primary psychiatrists (e.g. antidepressant and anxiolytic medications). All medication changes on patients' electronic medical records were monitored throughout the study.
2.3. Outcomes
All outcome measures were administered pre- and post-treatment. The primary outcome measure was the most widely used self-report measure of depression, as measured on the BDI-II [24,28]. The severity of depression is categorized based on the following BDI-II scores: a score of 10 or less is classified as normal (minimal); 11 to 18 as mild; 19 to 29 as moderate; and 30 or greater as severe [[29], [30], [31]]. The Japanese version of BDI-II has been shown to have good reliability with Cronbach's α = 0.87, and adequate correlation (r = 0.69, P = 0.001) between the total score of the BDI-II and that of the Center for Epidemiological Studies Depression Scale (CES-D) [24].
Secondary outcomes were measured using the Quick Inventory of Depressive Symptomatology-Self Rated (QIDS-SR) [32,33] which is also the commonly used self-reporting measure for assessing depression, the Medical Outcomes Study 36-Item Short-Form Health Survey version 2 (SF-36v2) [34,35] for measuring self-reported generic health-related quality-of-life, and the Rosenberg Self-Esteem Scale (RSES) [36,37] for assessing global self-esteem. Good reliability and the validity of the Japanese versions have also been reported for all secondary outcome measures (Fujisawa et al., 2010; Fukuhara, Bito, Green, Hsiao, & Kurokawa, 1998; Mimura & Griffiths, 2007) [33,34,37].
2.4. Statistical analysis
The analyses for all outcomes were conducted twice; once based on the intention-to-treat (ITT) principle, whereby all the dropouts were considered to be non-responders and their last obtained data points were carried forward, and once among the treatment completers (defined as attendance of at least 4 out of 6 sessions).
We compared the baseline and endpoint scores (BDI-II, QIDS-SR, RSES, and a three component summary of the SF-36v2) using paired t-tests. The cutoff point for remission according to the BDI-II was defined as an endpoint score of 10 or less, and treatment response was defined as a reduction in BDI-II score of at least 50% [[29], [30], [31],38]. Treatment effect sizes were calculated as Cohen's d. According to Cohen [39], we categorized effect sizes as follows: small (0.20–0.49), medium (0.50–0.79), and large (≥0.80). Daily doses of medication were calculated based on the imipramine-equivalent for antidepressants and diazepam-equivalent for anxiolytics.
All statistical tests were two-tailed, and α = 0.05 was employed. Statistical analyses were performed using IBM SPSS Statistics, version 24.0 (IBM, Armonk, New York, USA).
3. Results
3.1. Baseline data
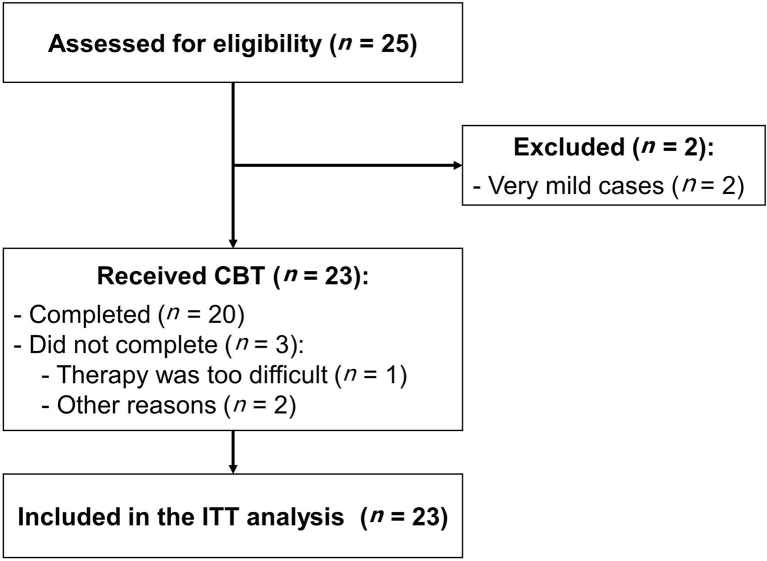
The selection process and flow are shown in Fig. 1. Twenty-five patients were recruited for the study, of which two patients were excluded (not clinically depressed: BDI-II ≤ 10). The remaining patients (n = 23) met the eligibility criteria. Six of the patients (25%) were diagnosed with recurrent episode MDD and the others (75%) were diagnosed with single episode MDD. The average age was 36.1 (standard deviation, SD = 11.4) years. Table 2 shows more details about the clinical characteristics of the patients.
Fig. 1.
Participants' flow.
CBT: cognitive behavioral therapy; ITT: intention-to-treat.
Table 2.
Baseline characteristics (n = 23).
| Characteristics | Value |
|---|---|
| Gender | |
| Female | 11 |
| Male | 12 |
| Age (years, Mean ± SD) | 36.1 ± 11.4 |
| Marital status | |
| Single | 11 |
| Married or cohabitant | 11 |
| Divorced | 1 |
| Employment | |
| Employed | 10 |
| Housewife | 2 |
| Unemployed | 11 |
| Depression episode | |
| Single episode | 17 |
| Recurrent episode | 6 |
| Duration of current depression episode (years, Mean ± SD) | 3.1 ± 1.6 |
| Comorbidity | |
| No comorbid condition | 18 |
| Concomitant antidepressants or anxiolytics use | |
| Yes | 20 |
3.2. Treatment acceptability
The mean number of CBT sessions attended was 5.67 (SD = 0.56) and 20 patients (87%) completed the program (three dropped out) (Fig. 1). The following reasons were given for dropping out: the therapy was too difficult (n = 1), and absence due to other problems (e.g. schedule conflict because of family problems, a marked increase in the severity of secondary illness) (n = 2). We observed no serious adverse events during the study.
3.3. Outcomes
Table 3 presents the pre- and post-treatment scores with respect to the outcome measures. Significant improvements were observed in the primary outcome (BDI-II) between the baseline and week 6, not only for the ITT sample but also for the treatment completers (P < 0.01). The mean total BDI-II score for the ITT sample decreased from 23.1 (SD = 7.56) to 12.4 (SD = 8.57), which corresponds with clinical improvement from moderate to minimal depression. The pre-to post-effect size was large (Cohen's d = 1.33). Ten patients (45.4%) were judged to be treatment responders and eight patients (36.3%) were judged to be treatment remitters. As for secondary outcomes, significant changes were observed in QIDS-SR, RSES, and the role/social component summary of SF36v2 scores (but not for the physical and mental component summary of SF-36v2) (all P < 0.05).
Table 3.
Outcome measures at pre- and post-treatment.
| Intention-to-treat (n = 23) |
Completers (n = 20) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Pre (Mean ± SD) |
Post (Mean ± SD) |
Improvement (%) | ES | Pre (Mean ± SD) |
Post (Mean ± SD) |
Improvement (%) | ES | |
| BDI-II | 23.14 ± 7.56 | 12.36 ± 8.57 | 47 | 1.33∗∗ | 23.35 ± 7.78 | 12.35 ± 8.67 | 47 | 1.34∗∗ |
| QIDS-SR | 11.91 ± 3.98 | 6.95 ± 5.04 | 42 | 1.09∗∗ | 11.60 ± 4.03 | 6.70 ± 4.92 | 42 | 1.09∗∗ |
| RSES | 25.80 ± 9.06 | 31.36 ± 10.20 | 22 | 0.58∗ | 25.84 ± 9.41 | 32.06 ± 10.46 | 24 | 0.62∗ |
| SF-36v2 | ||||||||
| PCS | 50.41 ± 10.77 | 48.15 ± 10.80 | −4 | −0.21 | 49.4 ± 10.77 | 46.90 ± 10.80 | −5 | −0.23 |
| MCS | 38.74 ± 9.38 | 42.60 ± 12.30 | 10 | 0.35 | 38.74 ± 9.72 | 42.60 ± 12.62 | 10 | 0.34 |
| RCS | 26.25 ± 14.97 | 34.79 ± 12.51 | 33 | 0.60∗ | 26.30 ± 14.61 | 35.74 ± 11.38 | 36 | 0.72∗ |
Note: Higher scores on the BDI-II and QIDS-SR indicate greater pathology or severity of depression. ∗∗P < 0.01.∗P < 0.05.
BDI-II: Beck depression inventory-II score; ES: Effect size of Cohen's d; QIDS-SR: Quick inventory of depressive symptomatology – self-rated; RSES: Rosenberg self-esteem scale; SF-36v2: MOS 36-item short-form health survey version 2; PCS: Physical component summary; MCS: Mental component summary; RCS: role/social component summary.
No significant differences were found between groups in terms of antidepressant (imipramine-equivalent) or anxiolytic (diazepam-equivalent) doses throughout the study. The mean imipramine-equivalent dose was 46.7 (SD = 75.5) at baseline and 46.25 (SD = 81.1) at week 6. The mean diazepam-equivalent dose was 7.83 (SD = 10.7) at baseline and 6.53 (SD = 8.59) at week 6.
4. Discussion
Our results indicate that 6 weeks of nurse-led group CBT led to a significant reduction in MDD severity among Japanese patients. The treatment also had excellent acceptability. Generally, around 25% of patients with MDD drop out from CBT programs: the dropout rate for individual CBT is 42%, and for group CBT about 17% [40]. The program investigated in the current study had a low dropout rate (13%).
Our CBT program was administered solely by nurses and was relatively short compared with those in previous studies, the treatment led to considerable improvements (effect size of 1.33 on BDI-II). Most previous studies comprised CBT programs with 8–12 sessions (with each session lasting 90–120 min) and had effect sizes in terms of BDI-II score (0.5–1.0) that were lower than those observed in this study [40]. There may be three reasons for this. First, our study therapists (both leading nurses and facilitators) received sufficient training and clinical experience before the trial. Second, our program was conducted in small groups (only 3–4 patients) to allow for maximal individual attention while retaining the advantages of a group format (e.g. group cohesion, role playing, and learning through peers). Therefore, our program can be thought to have a more individualized format compared with many other group format studies (5–7 patients per group, and fixed sessions) [40]. In addition, patients in this study may have had high expectations, preferences, motivations, and allegiances to CBT. As mentioned in the introduction, in Japan the effectiveness of CBT has recently become known, not only among professionals but also in the general public. However, there are few competent CBT therapists, and patients' access to CBT is severely limited in Japan. These factors might contribute to a larger treatment effect.
The following limitations should be considered with respect to the current findings. First, this study employed a single-group design without a control group (pre-post comparison); therefore, we cannot conclusively state that our group CBT was effective. The presence of the Hawthorne effect, which is typically observed in uncontrolled trials, cannot be denied in our study design; thus, future controlled studies are required. Second, our study had a limited number of participants. The distribution of the participating patients was somewhat skewed from the distribution of previous surveys in Japan [[41], [42], [43]]. This study had a relatively younger sample, a smaller proportion of patients who were married/cohabitant, a small number of patients who were either employed or housewives, and few patients with comorbid conditions. Third, although having a relatively small number of participants in each session/group (3–4 patients) allowed for a more individualized format, it was also a limitation (most programs include 5–7 patients). Future study should address the issue of adequate numbers, both in the entire study and in each group session. Fourth, both therapists were nurses who were acquainted with the participants. This may have contributed to the reduced dropout rate. Fifth, there is no long-term follow-up data, which limits the generalizability of the study's conclusions to longer-term outcomes. Sixth, the lack of patient commentaries limits our understanding of the effectiveness and acceptance of the program.
Several obstacles remain in the process of making CBT widely available to Japanese patients suffering from MDD. According to Yoshinaga et al. [20,44], the most important issue hindering the dissemination of CBT in Japan is the paucity of training opportunities for all health care professionals. Opportunities are limited because of the scarcity of CBT experts. Pre- and post-qualification training programs should be established across Japan so that more health professionals can receive adequate training. This will enable more patients to access such services in their local areas. In addition, research on efficient ways to disseminate treatment procedures, including the efficacy of CBT by trainees, would be useful in addressing empirical questions about how to best train therapists.
5. Conclusions
In conclusion, this study shows that 6 weeks of nurse-led group CBT has excellent acceptability, and is associated with positive outcomes in Japanese patients with MDD in a clinical setting. The results of this study, demonstrating the feasibility and acceptability of nurse-led CBT for depression, might encourage more Asian nurses to provide CBT as a part of their nursing practice. Further controlled trials that address the limitations of this study are required.
Declarations
Funding
This work was financially supported by the Grants-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Science (JSPS), Grant Number 25463556 to YS.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ijnss.2018.06.005.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.WHO World Health Organization. The global burden of disease: 2004 update. 2008. http://apps.who.int/iris/bitstream/10665/43942/1/9789241563710_eng.pdf
- 2.Hofmann S.G., Asnaani A., Vonk I.J.J., Sawyer A.T., Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. 2012;36(5):427–440. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cuijpers P., Andersson G., Donker T., van Straten A. Psychological treatment of depression: results of a series of meta-analyses. Nord J Psychiatr. 2011;65(6):354–364. doi: 10.3109/08039488.2011.596570. [DOI] [PubMed] [Google Scholar]
- 4.Butler A.C., Chapman J.E., Forman E.M., Beck A.T. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26(1):17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Dwight-Johnson M., Sherbourne C.D., Liao D., Wells K.B. Treatment preferences among depressed primary care patients. J Gen Intern Med. 2000;15(8):527–534. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ono Y. Insurance scoring and future challenges of cognitive behavioral therapy. Jpn J Cogn Ther. 2011;4:1–7. [in Japanese] [Google Scholar]
- 7.Marks I., Bird J., Lindley P. Behavioural nurse therapists 1978—developments and implications. Behav Cognit Psychother. 1978;6(2):25–36. [Google Scholar]
- 8.Gournay K., Denford L., Parr A.M., Newell R. British nurses in behavioural psychotherapy: a 25-year follow-up. J Adv Nurs. 2000;32(2):343–351. doi: 10.1046/j.1365-2648.2000.01482.x. [DOI] [PubMed] [Google Scholar]
- 9.Nance D.C. Pains, joys, and secrets: nurse-led group therapy for older adults with depression. Issues Ment Health Nurs. 2012;33(2):89–95. doi: 10.3109/01612840.2011.624258. [DOI] [PubMed] [Google Scholar]
- 10.Curran J., Brooker C. Systematic review of interventions delivered by UK mental health nurses. Int J Nurs Stud. 2007;44(3):479–509. doi: 10.1016/j.ijnurstu.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Tucker M., Oei T.P.S. Is group more cost effective than individual cognitive behaviour therapy? The evidence is not solid yet. Behav Cognit Psychother. 2007;35(1):77–91. [Google Scholar]
- 12.Menzel N.N., Robinson M.E. Back pain in direct patient care providers: early intervention with cognitive behavioral therapy. Pain Manag Nurs. 2006;7(2):53–63. doi: 10.1016/j.pmn.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Turkington D., Kingdon D., Rathod S., Hammond K., Pelton J., Mehta R. Outcomes of an effectiveness trial of cognitive-behavioural intervention by mental health nurses in schizophrenia. Br J Psychiaty. 2006;189:36–40. doi: 10.1192/bjp.bp.105.010884. [DOI] [PubMed] [Google Scholar]
- 14.Hyun M.S., Chung H.I., Lee Y.J. The effect of cognitive-behavioral group therapy on the self-esteem, depression, and self-efficacy of runaway adolescents in a shelter in South Korea. Appl Nurs Res. 2005;18(3):160–166. doi: 10.1016/j.apnr.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 15.Horatio: European psychiatric nurses. Psychiatric/mental health nursing and psychotherapy: the position of Horatio: European psychiatric nurses. http://www.horatio-web.eu/downloads/Psychotherapy_position_paper.pdf. Accessed 30 Aug 2017.
- 16.Schmahl J.A. The psychiatric nurse and psychotherapy. Nurs Outlook. 1962;10:460–465. [PubMed] [Google Scholar]
- 17.Cusack E, Killoury F. A vision for psychiatric/mental health nursing: a shared journey for mental health care in Ireland. http://www.hse.ie/eng/services/publications/NursingMidwifery%20Services/A%20Vision%20for%20Psychiatric%20Mental%20Health%20Nursing.pdf. Accessed 30 Aug 2017.
- 18.Shiraishi Y., Aoishi K., Tanoue H. Influence of cognitive behavioral therapy on "Nurse's professional autonomy" for psychiatric nurses. J Jpn Acad Psychiat Ment Health Nurs. 2014;23(2):58–64. [in Japanese] [Google Scholar]
- 19.APRN Joint Dialogue Group Report. Consensus model for APRN regulation: licensure, accreditation, certification & education. http://www.nursingworld.org/ConsensusModelforAPRN. Accessed 30 Aug 2017.
- 20.Yoshinaga N., Nosaki A., Hayashi Y., Tanoue H., Shimizu E., Kunikata H., Okada Y., Shiraishi Y. Cognitive behavioral therapy in psychiatric nursing in Japan. Nurs Res Pract. 2015;2015:529107. doi: 10.1155/2015/529107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whitfield G. Group cognitive–behavioural therapy for anxiety and depression. Adv Psychiatr Treat. 2010;16(3):219–227. [Google Scholar]
- 22.Vos T., Corry J., Haby M.M., Carter R., Andrews G. Cost-effectiveness of cognitive-behavioural therapy and drug interventions for major depression. Aust N Z J Psychiatr. 2005;39(8):683–692. doi: 10.1080/j.1440-1614.2005.01652.x. [DOI] [PubMed] [Google Scholar]
- 23.Morrison N. Group cognitive therapy: treatment of choice or sub-optimal option? Behav Cognit Psychother. 2001;29(3):311–332. [Google Scholar]
- 24.Kojima M., Furukawa T.A., Takahashi H., Kawai M., Nagaya T., Tokudome S. Cross-cultural validation of the beck depression inventory-II in Japan. Psychiatr Res. 2002;110(3):291–299. doi: 10.1016/s0165-1781(02)00106-3. [DOI] [PubMed] [Google Scholar]
- 25.Association of Cognitive Behavioral Group Therapy . Institute of A-V Medical Education INC; ToKyo: 2011. Let's try to start a group cognitive behavioral therapy. [in Japanese] [Google Scholar]
- 26.Suzuki S., Okamoto Y., Matsunaga M. Nihon-Hyoronsha; Tokyo: 2011. Group cognitive behavioral therapy practice manual for depression: towards the relapse prevention and return to work support. [in Japanese] [Google Scholar]
- 27.Okada Y., Tajima M., Nakamura S. Institute of A-V Medical Education INC; Tokyo: 2008. Come on ! Let's start ! Group cognitive behavioral therapy for depression. [in Japanese] [Google Scholar]
- 28.Beck A., Steer R.A., Brown G.K. second ed. Psychological Corporation; San Antonio, TX: 1996. BDI-II: Beck depression inventory manual. [Google Scholar]
- 29.Ahola K., Honkonen T., Kivimaki M., Virtanen M., Isometsa E., Aromaa A., Lonnqvist J. Contribution of burnout to the association between job strain and depression: the health 2000 study. J Occup Environ Med. 2006;48(10):1023–1030. doi: 10.1097/01.jom.0000237437.84513.92. [DOI] [PubMed] [Google Scholar]
- 30.Aben I., Verhey F., Lousberg R., Lodder J., Honig A. Validity of the beck depression inventory, hospital anxiety and depression scale, SCL-90, and Hamilton depression rating scale as screening instruments for depression in stroke patients. Psychosomatics. 2002;43(5):386–393. doi: 10.1176/appi.psy.43.5.386. [DOI] [PubMed] [Google Scholar]
- 31.Lasa L., Ayuso-Mateos J.L., Vazquez-Barquero J.L., Diez-Manrique F.J., Dowrick C.F. The use of the Beck Depression Inventory to screen for depression in the general population: a preliminary analysis. J Affect Disord. 2000;57(1–3):261–265. doi: 10.1016/s0165-0327(99)00088-9. [DOI] [PubMed] [Google Scholar]
- 32.Rush A.J., Trivedi M.H., Ibrahim H.M., Carmody T.J., Arnow B., Klein D.N., Markowitz J.C., Ninan P.T., Kornstein S., Manber R., Thase M.E., Kocsis J.H., Keller M.B. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatr. 2003;54(5):573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 33.Fujisawa D., Nakagawa A., Tajima M., Sado M., Kikuchi T., Iba M., Watanabe Y., Yamaguchi Y., Henomatsu K., Eto R. Cross-Cultural adaptation of the Quick inventory of depressive symptomatology-self report (QIDS-SR-J) Jpn J Stress Sci. 2010;25(1):43–52. [in Japanese] [Google Scholar]
- 34.Fukuhara S., Bito S., Green J., Hsiao A., Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol. 1998;51(11):1037–1044. doi: 10.1016/s0895-4356(98)00095-x. [DOI] [PubMed] [Google Scholar]
- 35.Ware J., Kosinski M. Health Assessment Lab; Boston, MA: 1996. The SF-36 health survey (version 2.0) technical note. [Google Scholar]
- 36.Rosenberg M. Princeton University Press; Princeton, NJ: 1965. Society and the adolescent self-image. [Google Scholar]
- 37.Mimura C., Griffiths P.A. Japanese version of the Rosenberg Self-Esteem Scale: translation and equivalence assessment. J Psychosom Res. 2007;62(5):589–594. doi: 10.1016/j.jpsychores.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 38.Bech P., Cialdella P., Haugh M.C., Hours A., Boissel J.P., Birkett M.A., Tollefson G.D. Meta-analysis of randomised controlled trials of fluoxetine v. placebo and tricyclic antidepressants in the short-term treatment of major depression. Br J Psychiatry. 2000;176(5):421–428. doi: 10.1192/bjp.176.5.421. [DOI] [PubMed] [Google Scholar]
- 39.Cohen J. Lawrence Earlbaum Associates; Hillsdale, NJ: 1988. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 40.Thimm J.C., Antonsen L. Effectiveness of cognitive behavioral group therapy for depression in routine practice. BMC Psychiatr. 2014;14:292. doi: 10.1186/s12888-014-0292-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Inaba A., Thoits P.A., Ueno K., Gove W.R., Evenson R.J., Sloan M. Depression in the United States and Japan: gender, marital status, and SES patterns. Soc Sci Med. 2005;61(11):2280–2292. doi: 10.1016/j.socscimed.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 42.Fujise N., Abe Y., Fukunaga R., Nakagawa Y., Nishi Y., Koyama A., Ikeda M. Comparisons of prevalence and related factors of depression in middle-aged adults between urban and rural populations in Japan. J Affect Disord. 2016;190:772–776. doi: 10.1016/j.jad.2015.11.020. [DOI] [PubMed] [Google Scholar]
- 43.Fujisawa D., Nakagawa A., Tajima M., Sado M., Kikuchi T., Hanaoka M., Ono Y. Cognitive behavioral therapy for depression among adults in Japanese clinical settings: a single-group study. BMC Res Notes. 2010;3:160. doi: 10.1186/1756-0500-3-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yoshinaga N., Matsuki S., Niitsu T., Sato Y., Tanaka M., Ibuki H., Takanashi R., Ohshiro K., Ohshima F., Asano K., Kobori O., Yoshimura K., Hirano Y., Sawaguchi K., Koshizaka M., Hanaoka H., Nakagawa A., Nakazato M., Iyo M., Shimizu E. Cognitive behavioral therapy for patients with social anxiety disorder who remain symptomatic following antidepressant treatment: a randomized, assessor-blinded, controlled trial. Psychother Psychosom. 2016;85(4):208–217. doi: 10.1159/000444221. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.