Abstract
Purpose
To optimize the gypsum mold temperatures for pressed PEEK, and to estimate the impact, tensile strength and flexural properties of pressed and milled PEEK. Where appropriate, these properties were compared with those of PMMA.
Materials and Methods
Since the mold temperature could affect the properties of the injected parts, the temperature of 20 gypsum specimens was monitored using the multi-thermocouple system (n = 5). A total of 210 specimens were prepared for mechanical tests according to the ISO standard for denture base polymer (n = 10). The Izod impact, tensile strength, and flexural behavior were assessed. PEEK-OptimaNI1 (PEEK-pressed) was tested after processing via the pressing method at4 different mold temperatures. Machining PEEK-Juvora (PEEK-milled) specimens were prepared using the CAD-CAM production method. Data were analyzed via one-way ANOVA performed at a confidence level of 95% and a significant P-value of (P ≤ 0.05).
Results
In comparison to the furnace temperature more heat was required to preheat the gypsum mold up to 100, 150, 175 and 200 °C for pressing purposes. The highest impact strength was 5.7 kJ/m2 for PEEK-pressed at 100 °C mold temperature and 4 kJ/m2 for PEEK-milled. The latter had a higher tensile strength of 118 MPa. The best result for PEEK-pressed was 97 MPa at 200 °C mold temperature. Under a 4-point bending test, Young’s modulus of PEEK-milled was 5591 MPa, while the highest for PEEK-pressed was 4936 MPa at 200 °C mold temperature.
Conclusions
Compared to PMMA, given the superior mechanical properties of PEEK, it may become the material of choice for future use. Dentures constructed from PEEK polymer could well be routinely constructed in the near future.
Keywords: Polyetheretherketone, Denture base material, Impact strength, 4-point bend, Tensile strength, Mold temperature, Injection molding, CAD-CAM
1. Introduction
In dentistry, several materials have been introduced over the last century for dentures such as cellulose products, phenol- formaldehyde (Bakelite), vinyl resins and vulcanite (Tandon et al., 2010, Van Noort and Barbour, 2014). The poor performance of these materials led to Polymethylmethacrylate (PMMA) suggested as a replacement (Little, 1982, Van Noort and Barbour, 2014) and it has now become the most commonly used material for the fabrication of dentures. However, PMMA dentures are susceptible to fracture during use or when dropped onto hard surfaces. These fractures are due to either flexural fatigue or impact (Vallittu, 1997, Jagger et al., 1999) which is generally associated with material properties (Vallittu and Kokkonen, 1997, Sato et al., 2003) and/or framework design integrity (Rudd and Rudd, 2001a, Rudd and Rudd, 2001b, Rudd and Rudd, 2001c).
Since PMMA is relatively low in cost and easy to use both clinically and in the laboratory, it remains the most popular choice for polymeric removable prosthodontics (Phoenix, 1996, Rahme et al., 2005). Nevertheless, many studies have proposed various techniques to improve upon PMMA through the inclusion of other materials (Bowman and Manley, 1984, Carroll and Von Fraunhofer, 1984, Jagger et al., 1999, Vuorinen et al., 2008, Young, 2010, Ahmed et al., 2016) the addition of metal reinforcement (Hahnel et al., 2015) fibers (Uzun et al., 1999, Çağlar et al., 2002, Çökeliler et al., 2007) hydroxyapatite filler or Silica (Mc Nally et al., 2006, Young, 2010) and modification the chemical properties of the PMMA. Some research has proposed the use or development of alternative materials (Ucar et al., 2012). Although PMMA is a non-metallic denture base material, there is still the possibility of toxic reactions or irritations for the wearer (Alanko et al., 1996, Kanerva et al., 1997, Lung and Darvell, 2005) and for dental technicians involved in handling and fabrication (Kanerva et al., 1993, Kiec-Swierczynska, 1996).
There has been interested in discovering materials that of very similar to PMMA but have better properties. Polysulfone (PSF), nylon and polycarbonate (PC) are suggested for patients who are allergic to acrylic (Stafford et al., 1986, Tanoue et al., 2005). However, shortcomings in some of their properties have limited their use (Pfeiffer and Rosenbauer, 2004, Pfeiffer et al., 2005) and it seems that as yet no material fully satisfies the ideal criteria for a denture base.
Biocompatibility is a primary requirement in all restorative materials, followed by mechanical and physical properties that guarantee appropriate function and structural permanence over long periods of time (Anusavice et al., 2013, Teoh et al., 2016). Polyetheretherketone (PEEK) is a semi-crystalline thermoplastic biomaterial with a chemical formula of (-C6H4-O-C6H4-O-C6H4-CO-)n. It is one of the Polyaryletherketones (PAEKs) polymer group family, which is characterized by ultra-high molecular weight polyethylene (UHMWPE) (Reinhart and Clements, 1993, Merrett et al., 2002, Callister and Rethwisch, 2007). It has increasingly employed in industry and as a biomaterial that can be used for medical purposes (Kurtz, 2012, Li et al., 2017) and has attracted more interest than any other implantable material for medical devices in the last 20 years (Rae et al., 2007, Koutouzis et al., 2011, Hahnel et al., 2015, Lee et al., 2017). PEEK available for medical purposes as granules to be pressed and blank disks to mill. Exceptional solvent resistance, low modulus of elasticity, and biocompatibility with bone make this polymer a good candidate to replace the use of metals in the body (Brillhart and Botsis, 1994, Sobieraj and Rimnac, 2012). The injection molding system is one of the most commonly used processing technologies in the plastics industry, and the temperature of the mold is an important factor in determining the final quality of the injected product. Unfortunately, the non-uniform distribution of mold temperature is a problem that can affect injection molding (Pawlak and Galeski, 2005, Chen et al., 2006). The mold temperature has perhaps a less obvious but often more dominant effect on the properties of the final product. In semi-crystalline materials such as PEEK, the mold temperature is an important factor in determining the parameters of the injected product for performance (Blundell and Osborn, 1983, Cebe et al., 1987, Hamdan and Swallowe, 1996, Invibio, 2004a, Invibio, 2004b). PEEK demonstrates greater strength than many metals on a per mass basis (Johnson et al., 2000). Some studies on industrial purposes have suggested using a typical metal mold temperature of 175–220 °C for PEEK polymer (Wilfong, 1989, Invibio, 2004a, Invibio, 2004b). However, in the dental application using gypsum products to create the mold is the only commonly used method to fabricate a positive reproduction for patients’ arches and associated structures.
PEEK could be considered as an innovative material to replace PMMA, but there have been no detailed studies in dentistry evaluating the PEEK polymer as a restorative dental material. Therefore, the aim of this study is to determine the mechanical properties of PEEK as a denture base material. Thus, the purpose of this study is to optimize the proper gypsum mold temperatures for pressed PEEK, evaluate the impact strength, tensile strength and flexural properties of PEEK-pressed and PEEK-milled in comparison with PMMA.
2. Materials and methods
In this study, a granular form of medical grade PEEK-OptimaNI1 polymer and PEEK-Juvora disks were used (Invibio and JuvoraLtd. UK).
2.1. Mold/furnace optimizing temperature
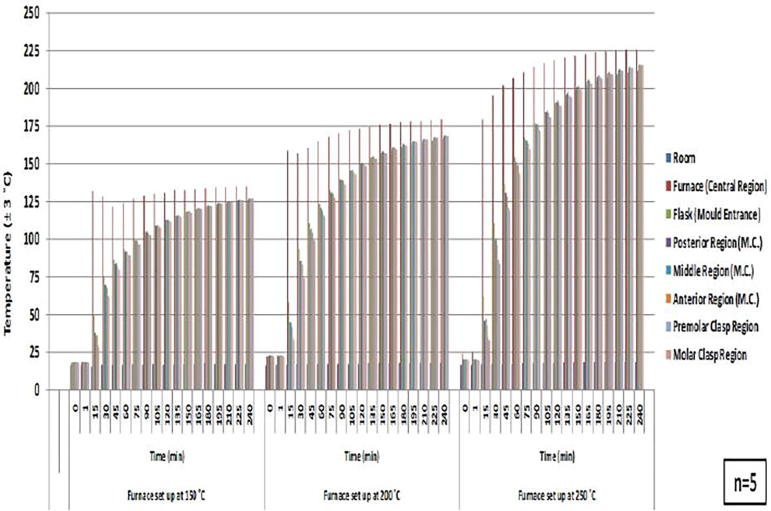
The optimization of the mold temperature is essential for thermo-pressing injection methods (Čatić, 1979, Wilfong, 1989, Despa et al., 1999, Invibio, 2004a, Invibio, 2004b). The temperature of the molds made of hard diestone gypsum material optimized at the range below and above the PEEK glass transition temperature at 100, 150, 175, and 200 °C mold temperature (PEEK Tg = 143 °C). The multiple-thermocouple technique was used, as it has the advantages of detecting specific temperatures in different places at the same time throughout long-term periods. Eight digital thermocouples embedded in different positions inside the gypsum mold cavity of the designed framework, furnace and laboratory room (LCD, Yct717); as seen in Fig. 1, Fig. 2, Fig. 3 (n = 5). The furnace was set up for 4 h at 150, 200 and 250 °C (Vecstar). The data were monitored digitally and recorded at one-minute intervals.
Fig. 1.
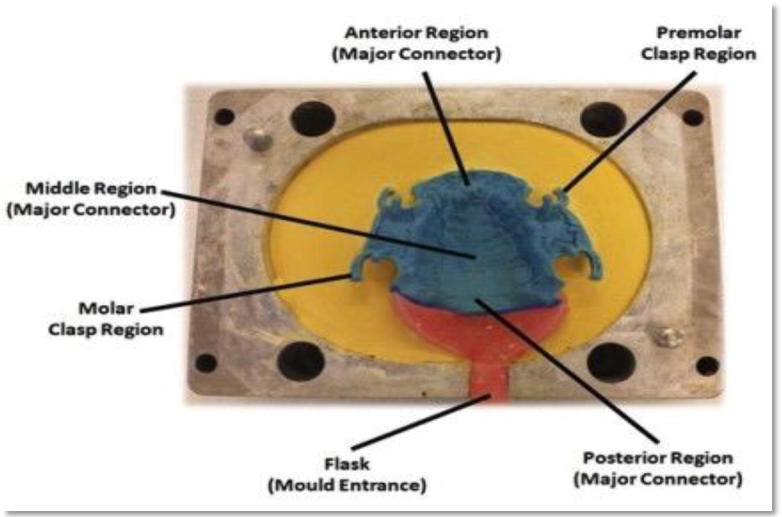
Molded removable partial denture (RPD) wax framework showing location of different thermocouples inside mold cavity.
Fig. 2.
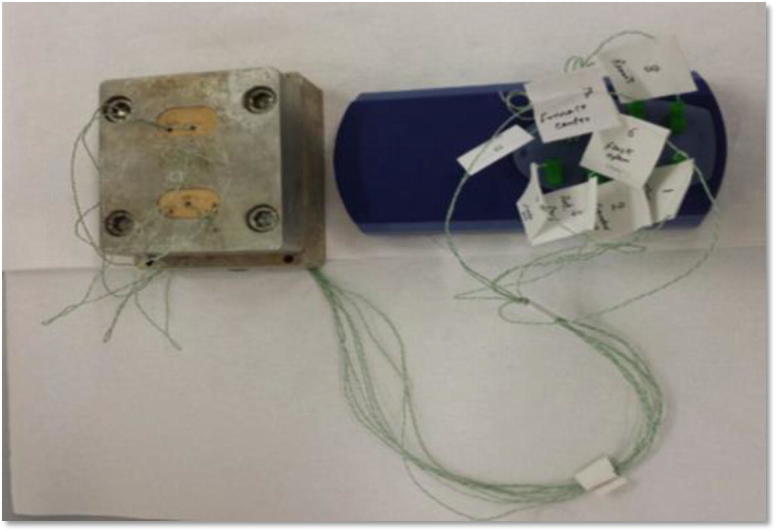
Multi-channel digital thermometer with multi-thermocouples of sensitive sensors inserted inside mold cavity at different locations.
Fig. 3.
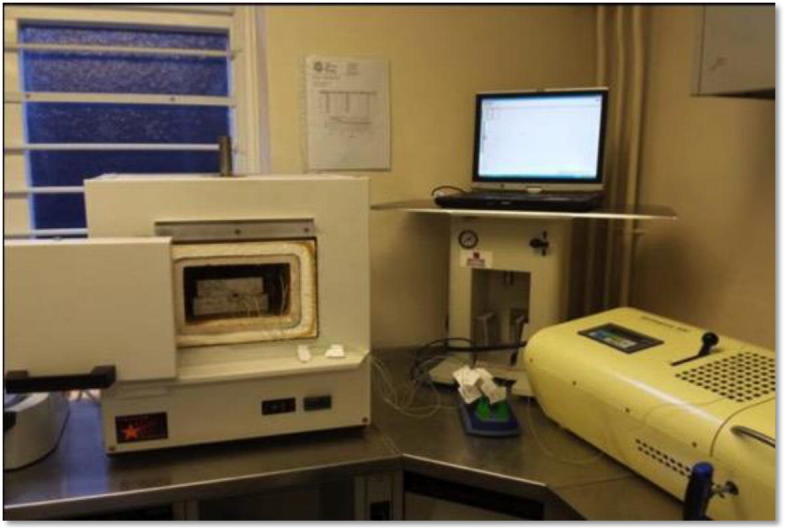
Molded flask with thermocouple sensors inside furnace connected to computer system to collect data at one-minute interval for 4 h.
2.2. Mechanical properties
In this study, the Izod impact strength, tensile strength, and flexural mechanical properties were evaluated. All test specimens prepared, and machine-polished using 600 and 1200 grit metallographic grinding papers (Metallo-graphical), and the dimensions measured using a digital caliper with 0.02 mm accuracy (6″ Skjutmatt) and were tested at 23 (±2 °C). Prior to mechanical testing, the specimens were stored in water at a temperature of 37 (±1 °C) for 50 (±2) h. The specimen dimensions were stated respectively according to the test method.
2.2.1. Izod impact strength
The Izod impact test specimens (n = 10) were prepared according to the dimensions recommended by (ASTM D 256, ISO 180) (Keener et al., 2004, D256 A, 2005, da Costa et al., 2007, Chen and Evans, 2009, Ozcelik et al., 2010). A specimen was prepared with dimensions of 10 (±0.2) × 4 (±0.2) × 80 (±2) mm depth, width, and length respectively. The specimen notch base radius was 0.25 ± 0.05 mm and its depth was 2 mm. It was prepared using an autocycle notching cutting machine (Ray Ran Polytest). To calculate the Izod impact strength of notched specimens (αiN), the impact tester machine was used to compute the absorbed energy of the breaking specimens (Ec) (Tinius Olsen's, IT 503) based on the following equation:
| (1) |
where Ec is the impact energy absorbed by breaking the test specimen (mm); h is the width or thickness of the test specimen (mm), and bN is the remaining depth of the test specimens (mm). The readings reported in kJ/m2.
Fracture surface morphologies examined with a scanning electron microscope (SEM). The micrographs were taken after specimens were fractured, dissected, mounted, and sputtered with gold to promote electrical conductivity to reduce charging.
2.2.2. Tensile strength
Tensile test specimens prepared according to ISO 527-1 and 2: 2012 (ISO, 2012) (n = 10). Each specimen was dumbbell-shaped with an overall length of 60 ± 2 mm and thickness of 2 ± 0.2 mm. Narrow sections had a width of 3 ± 0.2 mm and gauge length of 12 ± 0.5 mm. The length reduced parallel section was 16 ± 1 mm with a fillet radius of 12 ± 1 mm. The width of grip section was 12 ± 1 mm and distance between grips was 40 ± 1 mm. The measurements were taken via a universal testing machine. The jig grips the specimen on both ends at about 5 ± 1 mm with a 50 mm grip-to-grip distance of 2.5 KN-load cell and a testing speed of 30 mm/minute (Instron Lloyd, 2000) (Takabayashi, 2010).
2.2.3. Flexural properties using 4-point bending test
Despite the fact that many methods have been established to test the flexural strength of denture base polymers, it seems that none of these methods has demonstrated very accurate values (Chitchumnong et al., 1989). According to a pilot study, under biaxial fractural strength (BFS) PEEK exhibited no tendency to fracture in fatigue testing; however, plastic deformation was observed. Thus, further investigation of PEEK’s flexural behavior is required. In this study, four-point test specimens (n = 10) prepared according to ISO-1567:2001 dentistry denture base polymers (Standardization, 2001). A specimen was prepared with dimensions of 10 (±0.3) × 2.5 (±0.03) × 64 (±1) mm depth, width, and length respectively (Reis et al., 2006). A Lloyds universal machine of 2.5 KN loading capacity was used. A flexural test jig with two loading plungers and two polished cylindrical supports of 3.2 mm in radii was used with (50 ± 0.1) mm distance between the support centers. The supports were parallel to within 0.1 mm and were at right angles to the longitudinal centerline. Following procedures by Chitchumnong et al. (1989), Standardization (2001), Reis et al. (2006) and Barbosa et al. (2007) the force on the loading plungers was increased uniformly from 5 N using a constant crosshead speed of 5(±1) mm/minute but up to maximum load of 100 N (Instron Lloyd, 2000, England). The 4-point flexural properties (σ) were obtained based on the following formula (Chitchumnong et al., 1989, Junior et al., 2008):
| (2) |
where P is the maximum load exerted on the specimen (Newton), l is the distance between the supports (mm), w is the specimen width and d is the specimen depth (height), Specimen dimension was measured immediately prior to water storage.
The mold for the heat-polymerized and denture injection method was created using hard dental stone investment material and mixed according to the manufacturer’s instructions (Esthetic base gold, type IV hard diestone).
2.3. Mold and specimen preparation
The PMMA-HC specimen followed the conventional dental laboratory procedures. These include the preparation of the wax pattern and the mold. For the compression method, after boiling out the wax, a cold mold seal separating medium was applied to the mold surfaces while the mold material was still warm. The mixing of the PMMA (P/L: 100 g/10 ml) ratio followed the manufacturer’s instructions (Candulor, Swaziland), and the heat polymerization was carried out for 9 h [(7 h/74 °C (±3°C), then 2 h/95 °C (±3°C)] using the water bath curing technique.
The thermopress 400 injection molding system was used to preheat and press the materials according to the set programs (Bredent, Germany). Each aluminum cartridge filled with 25 g of pressed granules; once the set preheating temperature reached the optimum level, the cartridge was inserted into the heated chamber after lubrication with special thermo-paste grease. The preheating time for PEEK was 20 min, while for PMMA it was 17 min. Once the press temperatures were optimized, the flasks were removed from the furnace and left for 30 s to release any steam generated inside the mold due to the preheating process. The molten PEEK was pressed within 60 s into the mold cavity with a pressing pressure of 150 MPa and at 100, 150, 175 and 200 °C mold temperatures (PEEK melting temperature: 380 °C) (Invibio Ltd.UK). However, PMMA-pressed injected at a pressure of 165 MPa at 40 °C mold temperature (PMMA melting temperature: 280 °C) (BrecrystalHP, Bredent, Germany). The injected molds were left overnight to allow slow bench-cooling to room temperature.
PEEK-milled specimens were designed in a 3D form using 3D modeling designer (Google SketchUp, 2013). The designs were then converted to (.Stl) files and exported for fabrication using the machining CAM production method. PEEK-Juvora disks were machined using a dental milling machine (Roland, DWX-50) to produce the PEEK-milled specimens.
3. Results
Analysis of the results of this study was conducted using SPSS software (V-22). These statistical tests included inferential statistical analysis of variation (ANOVA). Tests were performed at a confidence level of 95% and with a significant P-value of (P ≤ 0.05). A one- way ANOVA (Post-hoc, Tukey test) showed statistically significant differences in temperatures at different points between the mold and furnace (P < .05), as seen in Fig. 4. The mold exhibited a temperature lower than that of the heated furnace. However, at selected mean values of the suggested mold temperature for this study, the temperatures of around 100, 150, 175, and 200 °C showed a non-significant difference (P > .05) at particular times. Table 1 illustrates the mold temperatures that were optimal and selected for PEEK-pressed using denture injection method.
Fig. 4.
Mold-furnace-lab room temperature using multi-thermocouple technique.
Table 1.
Select molding temperatures and times for testing material.
| Furnace set up temperature (°C) | Mold temperature (°C) | Time (min) |
|---|---|---|
| 150 | 100 | 90 |
| 200 | 150 | 120 |
| 250 | 175 | 90 |
| 250 | 200 | 150 |
One-way ANOVA (Games-Howell) was used to evaluate the mechanical properties of study materials. They exhibited statistically different mechanical properties using different processing conditions, as shown in Table 2, Table 3. Generally, a statistically significant difference noticed (P < .05) in values of impact and tensile strength in the machined and pressed PEEK when compared with the conventional PMMA-HC and PMMA-pressed. Also, there was a statistically significant difference (P < .001) between the modulus of elasticity, flexural deflection of the PMMA and those of the PEEK-milled and PEEK-pressed.
Table 2.
Mechanical properties of tested materials.
| Test materials | Izod impact strength (kJ/m2) |
Tensile strength (MPa) |
Flexural properties (4-point bend) |
||
|---|---|---|---|---|---|
| Young’s modulus (MPa) | Bending deflection (mm) | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| PEEK-milled | 4 (±1) | 118 (±5) | 5591 (±33) | 3.2 (±0.2) | |
| PEEK-pressed | 100 °C | 5.7 (±0.4) | 91 (±3) | 4773 (±42) | 4 (±0.3) |
| 150 °C | 5 (±0.4) | 96 (±2) | 4840 (±28) | 3.9 (±0.4) | |
| 175 °C | 5.3 (±0.5) | 93 (±5) | 4686 (±16) | 4 (±0.2) | |
| 200 °C | 4.8 (±0.4) | 97 (±4) | 4936 (±28) | 3.7 (±0.1) | |
| PMMA-HC | 2.3 (±0.2) | 65 (±5) | 3632 (±23) | 5.4 (±0.4) | |
| PMMA-pressed | 2.2 (±0.1) | 68 (±9) | 3784 (±29) | 5.5 (±0.4) | |
PEEK: PolyEtherEtherKetone.
PMMA: Polymethylmethacrylate.
HC: Heat-cured.
Table 3.
P-value of tested materials with different mechanical properties.
| Materials | P-value |
||||
|---|---|---|---|---|---|
| Izod impact strength | Tensile strength | Young’s modulus | Bending deflection | ||
| PEEK-milled | PEEK-pressed (100 °C) | 0.004 | <0.001 | 0.003 | <0.001 |
| PEEK-pressed (150 °C) | >0.05 | <0.001 | ≤0.001 | <0.001 | |
| PEEK-pressed (175 °C) | 0.034 | <0.001 | <0.001 | <0.001 | |
| PEEK-pressed (200 °C) | >0.05 | <0.001 | 0.003 | <0.001 | |
| PMMA-HC | 0.005 | <0.001 | <0.001 | ≤0.001 | |
| PMMA-pressed | 0.004 | <0.001 | <0.001 | <0.001 | |
| PEEK-pressed (100 °C) | PEEK-pressed (150 °C) | 0.015 | 0.018 | >0.05 | >0.05 |
| PEEK-pressed (175 °C) | >0.05 | >0.05 | >0.05 | >0.05 | |
| PEEK-pressed (200 °C) | 0.002 | 0.013 | >0.05 | >0.05 | |
| PMMA-HC | <0.001 | <0.001 | <0.001 | <0.001 | |
| PMMA-pressed | <0.001 | <0.001 | <0.001 | <0.001 | |
| PEEK-pressed (150 °C) | PEEK-pressed (175 °C) | >0.05 | >0.05 | >0.05 | >0.05 |
| PEEK-pressed (200 °C) | >0.05 | >0.05 | >0.05 | 0.010 | |
| PMMA-HC | <0.001 | <0.001 | <0.001 | <0.001 | |
| PMMA-pressed | <0.001 | <0.001 | <0.001 | <0.001 | |
| PEEK-pressed (175 °C) | PEEK-pressed (200 °C) | >0.05 | >0.05 | >0.05 | 0.025 |
| PMMA-HC | <0.001 | <0.001 | <0.001 | <0.001 | |
| PMMA-pressed | <0.001 | <0.001 | <0.001 | <0.001 | |
| PEEK-pressed (200 °C) | PMMA-HC | <0.001 | <0.001 | <0.001 | <0.001 |
| PMMA-pressed | <0.001 | <0.001 | <0.001 | <0.001 | |
| PMMA-HC | PMMA-pressed | >0.05 | >0.05 | >0.05 | >0.05 |
PEEK: PolyEtherEtherKetone.
PMMA: Polymethylmethacrylate.
HC: Heat-cured.
4. Discussion
The present study found a lack of uniformity in temperature across different locations inside and outside the mold cavity. As Čatić described in a study established in 1979, cavity temperature considered as a complex function of static and dynamic parameters and should be kept constant during the injection procedure (Čatić, 1979). Elevating the temperature of the mold above the injected material Tg could prevent premature freezing of the mold. On the other hand, Despa et al. in 1999 concluded that the cold mold could increase the risk of premature freezing of the melt front, resulting in incomplete mold filling (Despa et al., 1999). Therefore, heating the mold to a temperature around the melting point of the injected polymer may ensure complete penetration into the mold cavity. Thus, the mold must be heated to ease penetration into the depths of the cavity. Crystals can only form at temperatures below melting point but above the Tg of the polymer. When molding semi-crystalline materials such as PEEK (Tg:143 °C), the ideal mold temperature will be above the Tg in order to give the polymer adequate time to crystallize. The optimal mold temperature for PEEK-pressed achieved as shown in Table 1. The tested mechanical properties of PEEK-pressed evaluated at these suggested temperatures.
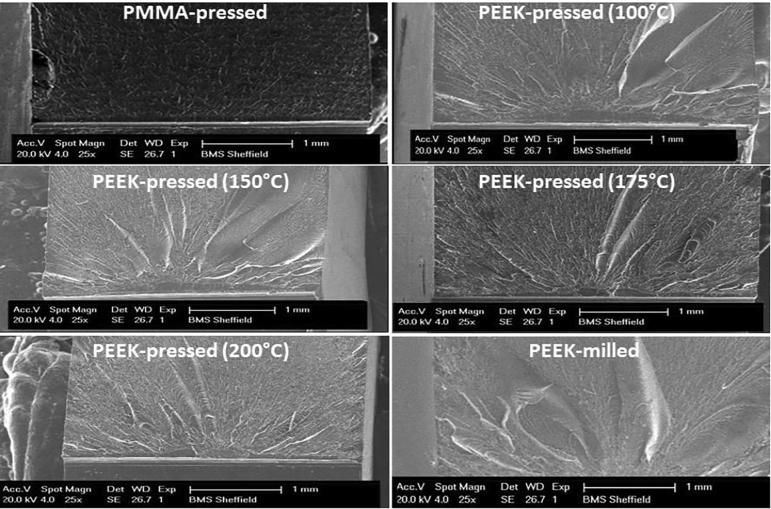
As the mold temperature increased above the PEEK Tg, a tendency for impact strength to decrease observed. The impact strength of the PEEK was higher than that of the PMMA-HC (2.3 kJ/m2) and PMMA-pressed (2.2 kJ/m2). The PEEK-pressed at mold temperatures above the PEEK Tg showed the same impact strength with a range of 4.8–5.3 kJ/m2. This could in agree with a study by Rae et al. (2007). They concluded that PEEK material appeared to have less resistance to fracture tendency at many elevated temperatures (Rae et al., 2007). On the other hand, the PEEK-milled had a lower impact strength of 4 kJ/m2. Although the PEEK considered as a notch weakening material, its impact strength was mainly higher than that of the PMMA. Regarding fracture morphology; as shown in Fig. 5, the number of semi-brittle fractures occurring in the PEEK specimen increased as the mold temperature increased above the PEEK Tg. Polymers with matrixes that have amorphous components of low Tg become tougher with the presence of Izod impact energy. This result confirmed almost what was concluded by Brillhart and Botsis (1994), PEEK at 100 °C mold temperature may exhibit a high number of intermediate fractures, perhaps because it suffers huge plastic deformation, and probably absorbs more energy during an impact strength test (Brillhart and Botsis, 1994). According to Pawlak and Galeski, elastic cavitation may occur in semi-crystalline polymers with crystals of higher resistance to the onset of plastic behavior, while plastic deformation occurs in crystals of lower plastic resistance (Pawlak and Galeski, 2005). This explanation supported by the fracture surface appearance of the notched geometries, which showed that propagation of cracks through crazed regions left behind patchwork morphology. However, in agreement with Sobieraj and Rimnac (2012) studies, the numbers of semi-brittle fractures were found in the PEEK-milled. These exhibited a notch weakening deformation mechanism with cracking growth behavior that led to final fracture (Sobieraj and Rimnac, 2012) and a semi-brittle behavior with very little plastic deformation impact energy. This may agree with Invibio polymer processing guide, as they referred to the high crystalline percentage when PEEK annealed for machining purposes and this lead to a more brittle product (Invibio, 2004a, Invibio, 2004b). Alternatively, as per many reported studies, PMMA showed a number of brittle fracture characteristics, as the polymer resins can primarily demonstrate brittle fractures (Reinhart and Clements, 1993, Merrett et al., 2002, Callister and Rethwisch, 2007).
Fig. 5.
SEM of fractured surfaces of Izod impact tested materials.
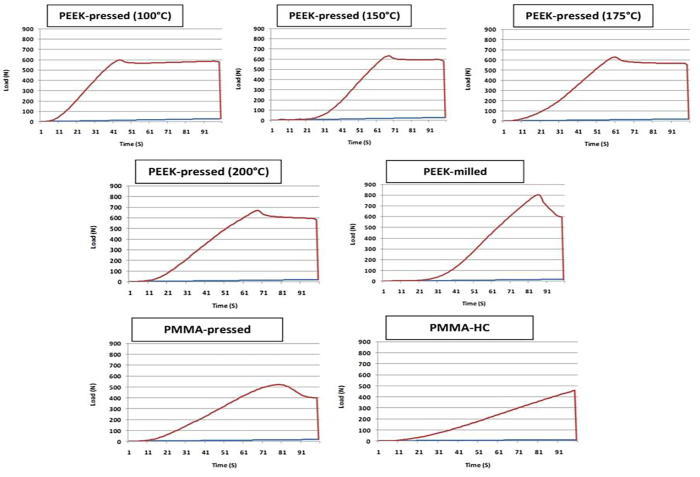
The base material may elongate under tension load; however, beyond the elastic region, there may be plastic deformation whereby the original form might not completely regain after unloading. As seen in Fig. 6, Fig. 7 and Table 2, machined PEEK revealed the highest tensile strength of 118 MPa, which was superior to that of the PEEK-pressed at 200 °C mold temperature. However, both specimens fractured at the midpoint reflecting the even distribution of the load along the specimen up to break. This may derive from the inherent characteristics of stable crystalline-amorphous parts of the PEEK-milled that were controlled by manufacturers in processing phases (Invibio, 2004a, Invibio, 2004b). As the study conclusions by Blundell and Osborn (1983), Cebe et al. (1987) and Hamdan and Swallowe (1996), the mold temperature can affect the tensile strength of PEEK-pressed because it influences the unstable crystalline-amorphous parts within the mold at temperatures around the PEEK Tg. However, the PEEK demonstrated superior tensile strength and lower plastic deformation in elastic regions compared to PMMA. Furthermore, the flexibility and highly elastic nature of the PEEK polymer could potentially decrease the stress on abutment teeth, which in turn could be advantageous in designing clasps using deep undercuts on the remaining teeth, thus eliminating denture pain due to excessive local pressure.
Fig. 6.
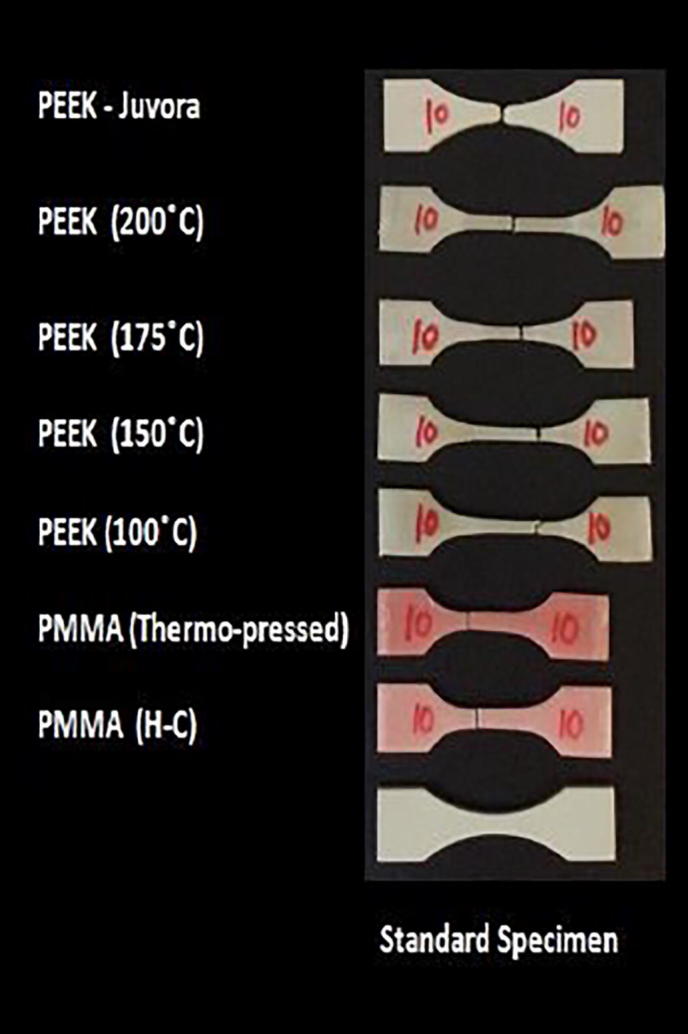
Specimens after tensile strength testing at load of break.
Fig. 7.
Elastic deformation of tested materials under tensile testing at load of break.
Under 4-point bend load, the PEEK polymer exhibited superior Young’s modulus compared to PMMA processed by two techniques; see Table 2. According to ISO standardization alongside a study by Takabayashi (2010), the modulus of elasticity of the denture base material should be 2000 MPa. Therefore, all of the tested materials correlated with standard values (Takabayashi, 2010). The PEEK-milled specimens revealed the lowest bend deflection among the tested groups. Also, the PEEK-pressed at 200 °C mold temperature had lower bend deflection than that pressed at different mold temperatures. Nevertheless, the maximum bend deflection was lower than that noticed with the PMMA specimen. High flexibility material may not be the ideal choice as a denture base, but flexibility is crucial for clasp design in Removable Partial Dentures (RPDs). These results are in agreement with the results of most of the previously mentioned study by Ucar et al. (2012); hence, flexural modulus and rigidity are more important than higher deflection rates (Ucar et al., 2012).
5. Conclusions
Within the limitations imposed by the methods of the current study, the following conclusions may be made:
The mold/furnace temperature recorded data achieved by this study identified differences in the mold temperature at different locations inside the cavity compared to furnace temperature. The mold temperature was lower than that of the actual furnace temperature when monitored by multiple thermocouples. Therefore, more heated energy was needed to elevate the gypsum mold temperature up to 100, 150, 175, and 200 °C.
The PEEK polymer could be considered as a resistant material to notch concentration as it revealed higher Izod impact strength than the PMMA. Denture frameworks made of PEEK with notches for labial, buccal frenum, or a special design for partial dentures could be less susceptible to fracture.
Both PEEK specimens of milled and pressed at 200 °C mold temperature had higher tensile strength. In addition, in both specimens load break occurred at the midline which suggests that it could provide dentures with good load distribution to the underlying tissues in function.
PEEK offers higher Young's modulus but lower bend deflection than the PMMA. This potentially might decrease the load applied to the underlying tissue, which in turn minimizes the possibility of relining the base after a few weeks.
To sum up, under laboratory assessment the PEEK polymer that was milled or pressed at 200 °C mold temperature demonstrates proper and superior mechanical properties compared to PMMA. These findings indicate the promise offered by PEEK as an alternative denture material. However, further studies are required to determine how best to bond PEEK to artificial teeth. Further research is also required to determine suitable designs for partial framework including component such as clasps. Finally, further evaluation is required under clinical load performance to confirm long-term success in real structure.
Ethical Statement
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support not mentioned within the manuscript for this work that could have influenced its outcome.
Conflict of interest
None.
Acknowledgment
The author(s) thanks the Higher Committee of Educational Development in Iraq (HCED), the scholarship program that supports the most talented students in Iraq. Also thanks Invibio® and Juvora™ Ltd for supplying the PEEK material for this study and finally the University of Sheffield for technical and lab facilities.
Footnotes
Peer review under responsibility of King Saud University.
References
- Ahmed M.A. Effect of titanium dioxide nano particles incorporation on mechanical and physical properties on two different types of acrylic resin denture base. World J. Nano Sci. Eng. 2016;6(03):111. [Google Scholar]
- Alanko K. Oral mucosal diseases investigated by patch testing with a dental screening series. Contact Dermat. 1996;34(4):263–267. doi: 10.1111/j.1600-0536.1996.tb02197.x. [DOI] [PubMed] [Google Scholar]
- Anusavice K.J. Elsevier Health Sciences; 2013. Phillips' Science of Dental Materials. [Google Scholar]
- Barbosa D.B. Flexural strength of acrylic resins polymerized by different cycles. J. Appl. Oral Sci. 2007;15(5):424–428. doi: 10.1590/S1678-77572007000500010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blundell D., Osborn B. The morphology of poly (aryl-ether-ether-ketone) Polymer. 1983;24(8):953–958. [Google Scholar]
- Bowman A., Manley T. The elimination of breakages in upper dentures by reinforcement with carbon fibre. Br. Dent. J. 1984;156(3):87. doi: 10.1038/sj.bdj.4805275. [DOI] [PubMed] [Google Scholar]
- Brillhart M., Botsis J. Fatigue crack growth analysis in PEEK. Int. J. Fatigue. 1994;16(2):134–140. [Google Scholar]
- Çağlar A. Effect of glass fiber reinforcement on the flexural strength of different denture base resins. Quint. Int. 2002;33(6) [PubMed] [Google Scholar]
- Callister W.D., Rethwisch D.G. John wiley & sons; New York: 2007. Materials Science and Engineering: An Introduction. [Google Scholar]
- Carroll C., Von Fraunhofer J. Wire reinforcement of acrylic resin prostheses. J. Prosthet. Dent. 1984;52(5):639–641. doi: 10.1016/0022-3913(84)90132-x. [DOI] [PubMed] [Google Scholar]
- Čatić I.J. Cavity temperature—an important parameter in the injection molding process. Polym. Eng. Sci. 1979;19(13):893–899. [Google Scholar]
- Cebe P. Effect of thermal history on mechanical properties of polyetheretherketone below the glass transition temperature. J. Appl. Polym. Sci. 1987;33(2):487–503. [Google Scholar]
- Chen B., Evans J.R. Impact strength of polymer-clay nanocomposites. Soft Matter. 2009;5(19):3572–3584. [Google Scholar]
- Chen S.C. Dynamic mold surface temperature control using induction heating and its effects on the surface appearance of weld line. J. Appl. Polym. Sci. 2006;101(2):1174–1180. [Google Scholar]
- Chitchumnong P. Comparison of three-and four-point flexural strength testing of denture-base polymers. Dent. Mater. 1989;5(1):2–5. doi: 10.1016/0109-5641(89)90082-1. [DOI] [PubMed] [Google Scholar]
- Çökeliler D. Modification of glass fibers to improve reinforcement: a plasma polymerization technique. Dent. Mater. 2007;23(3):335–342. doi: 10.1016/j.dental.2006.01.023. [DOI] [PubMed] [Google Scholar]
- D256 A, 2005 . American Society for Testing Materials International; Philadelphia, PA: 2005. Standard Test Method for Determining The Izod Pendulum Impact Resistance of Plastics. [Google Scholar]
- da Costa H.M. Degradation of polypropylene (PP) during multiple extrusions: thermal analysis, mechanical properties and analysis of variance. Polym. Test. 2007;26(5):676–684. [Google Scholar]
- Despa M. Injection molding of polymeric LIGA HARMs. Microsyst. Technol. 1999;6(2):60–66. [Google Scholar]
- Hahnel S. Biofilm formation on the surface of modern implant abutment materials. Clin. Oral Implant Res. 2015;26(11):1297–1301. doi: 10.1111/clr.12454. [DOI] [PubMed] [Google Scholar]
- Hamdan S., Swallowe G. The strain-rate and temperature dependence of the mechanical properties of polyetherketone and polyetheretherketone. J. Mater. Sci. 1996;31(6):1415–1423. [Google Scholar]
- Invibio, B.S., 2004. PEEK-Optima Polymer Processing Guide. Invibio Ltd.
- Invibio B.S. Invibio Inc.; Lancashire, United Kingdom: 2004. PEEK-Optima Polymer: Performance Purity Flexibility Endurance. [Google Scholar]
- ISO, 2012. 527-1 & 2: Plastics—determination of tensile properties. British Standards Institution.
- Jagger D. The reinforcement of dentures. J. Oral Rehabil. 1999;26(3):185–194. doi: 10.1046/j.1365-2842.1999.00375.x. [DOI] [PubMed] [Google Scholar]
- Johnson A. Design of composite wing access cover under impact loads. Appl. Compos. Mater. 2000;7(4):219–229. [Google Scholar]
- Junior S.A.R. Flexural strength and Weibull analysis of a microhybrid and a nanofill composite evaluated by 3-and 4-point bending tests. Dent. Mater. 2008;24(3):426–431. doi: 10.1016/j.dental.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Kanerva L. Occupational allergic contact dermatitis caused by exposure to acrylates during work with dental prostheses. Contact Dermat. 1993;28(5):268–275. doi: 10.1111/j.1600-0536.1993.tb03430.x. [DOI] [PubMed] [Google Scholar]
- Kanerva L. 10 years of patch testing with the (meth) acrylate series. Contact Dermat. 1997;37(6):255–258. doi: 10.1111/j.1600-0536.1997.tb02460.x. [DOI] [PubMed] [Google Scholar]
- Keener T. Maleated coupling agents for natural fibre composites. Compos. Part A: Appl. Sci. Manuf. 2004;35(3):357–362. [Google Scholar]
- Kiec-Swierczynska M. Occupational allergic contact dermatitis in Lodz: 1990–1994. Occup. Med. 1996;46(3):205–208. doi: 10.1093/occmed/46.3.205. [DOI] [PubMed] [Google Scholar]
- Koutouzis T. Comparative soft and hard tissue responses to titanium and polymer healing abutments. J. Oral Implantol. 2011;37(sp1):174–182. doi: 10.1563/AAID-JOI-D-09-00102.1. [DOI] [PubMed] [Google Scholar]
- Kurtz S.M. Elsevier; 2012. An Overview of PEEK Biomaterials, PEEK Biomaterials Handbook; pp. 1–7. [Google Scholar]
- Lee J.H. Cold-spray coating of hydroxyapatite on a three-dimensional polyetheretherketone implant and its biocompatibility evaluated by in vitro and in vivo minipig model. J. Biomed. Mater. Res. B Appl. Biomater. 2017;105(3):647–657. doi: 10.1002/jbm.b.33589. [DOI] [PubMed] [Google Scholar]
- Li Q. Porous polyether ether ketone: a candidate for hard tissue implant materials. Mater. Des. 2017;116:171–175. [Google Scholar]
- Little D. The relevance of prosthodontics and the science of dental materials to the practice of dentistry. J. Dent. 1982;10(4):300–310. doi: 10.1016/0300-5712(82)90023-9. [DOI] [PubMed] [Google Scholar]
- Lung C., Darvell B. Minimization of the inevitable residual monomer in denture base acrylic. Dent. Mater. 2005;21(12):1119–1128. doi: 10.1016/j.dental.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Mc Nally L. An in vitro investigation of the effect of the addition of untreated and surface treated silica on the transverse and impact strength of poly (methyl methacrylate) acrylic resin. Bio-Med. Mater. Eng. 2006;16(2):93–100. [PubMed] [Google Scholar]
- Merrett K. Surface analysis methods for characterizing polymeric biomaterials. J. Biomater. Sci. Polym. Ed. 2002;13(6):593–621. doi: 10.1163/156856202320269111. [DOI] [PubMed] [Google Scholar]
- Ozcelik B. Influence of injection parameters and mold materials on mechanical properties of ABS in plastic injection molding. Int. Commun. Heat Mass Transf. 2010;37(9):1359–1365. [Google Scholar]
- Pawlak A., Galeski A. Plastic deformation of crystalline polymers: the role of cavitation and crystal plasticity. Macromolecules. 2005;38(23):9688–9697. [Google Scholar]
- Pfeiffer P. Flexural strength and moduli of hypoallergenic denture base materials. J. Prosth. Dent. 2005;93(4):372–377. doi: 10.1016/j.prosdent.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Pfeiffer P., Rosenbauer E.-U. Residual methyl methacrylate monomer, water sorption, and water solubility of hypoallergenic denture base materials. J. Prosth. Dent. 2004;92(1):72–78. doi: 10.1016/j.prosdent.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Phoenix R.D. Denture base materials. Dent. Clin. North Am. 1996;40(1):113–120. [PubMed] [Google Scholar]
- Rae P. The mechanical properties of poly (ether-ether-ketone)(PEEK) with emphasis on the large compressive strain response. Polymer. 2007;48(2):598–615. [Google Scholar]
- Rahme H. Physical properties of four acrylic denture base resins. J. Contemp. Dent. Pract. 2005:093–100. [PubMed] [Google Scholar]
- Reinhart T.J., Clements L.L. Introduction to composites. Eng. Mater. Handbook. 1993;1:27–34. [Google Scholar]
- Reis J.M.d.S.N. Effect of relining, water storage and cyclic loading on the flexural strength of a denture base acrylic resin. J. Dent. 2006;34(7):420–426. doi: 10.1016/j.jdent.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Rudd R.W., Rudd K.D. A review of 243 errors possible during the fabrication of a removable partial denture: part I. J. Prosth. Dent. 2001;86(3):251–261. doi: 10.1067/mpr.2001.118021. [DOI] [PubMed] [Google Scholar]
- Rudd R.W., Rudd K.D. A review of 243 errors possible during the fabrication of a removable partial denture: part II. J. Prosth. Dent. 2001;86(3):262–276. doi: 10.1067/mpr.2001.118452. [DOI] [PubMed] [Google Scholar]
- Rudd R.W., Rudd K.D. A review of 243 errors possible during the fabrication of a removable partial denture: part III. J. Prosth. Dent. 2001;86(3):277–288. doi: 10.1067/mpr.2001.118456. [DOI] [PubMed] [Google Scholar]
- Sato Y. The effect of occlusal rest size and shape on yield strength. J. Prosth. Dent. 2003;89(5):503–507. doi: 10.1016/s0022-3913(02)52739-6. [DOI] [PubMed] [Google Scholar]
- Sobieraj M.C., Rimnac C.M. Elsevier; 2012. Fracture, Fatigue, and Notch Behavior of PEEK, PEEK Biomaterials Handbook; pp. 61–73. [Google Scholar]
- Stafford G. The use of nylon as a denture-base material. J. Dent. 1986;14(1):18–22. doi: 10.1016/0300-5712(86)90097-7. [DOI] [PubMed] [Google Scholar]
- Standardization, I.O.f., 2001. ISO 1567: 2001: Dentistry: denture base polymers, ISO Geneva.
- Takabayashi Y. Characteristics of denture thermoplastic resins for non-metal clasp dentures. Dent. Mater. J. 2010;29(4):353–361. doi: 10.4012/dmj.2009-114. [DOI] [PubMed] [Google Scholar]
- Tandon R. Denture base materials: from past to future. Indian J. Dent. Sci. 2010;2(2):33–39. [Google Scholar]
- Tanoue N. Use of a light-polymerized composite removable partial denture base for a patient hypersensitive to poly (methyl methacrylate), polysulfone, and polycarbonate: a clinical report. J. Prosth. Dent. 2005;93(1):17–20. doi: 10.1016/j.prosdent.2004.09.022. [DOI] [PubMed] [Google Scholar]
- Teoh, S. et al., 2016. Thermoplastic Polymers In Biomedical Applications: Structures, Properties and Processing. Handbook of Biomaterial Properties, 261.
- Ucar Y. Mechanical properties of polyamide versus different PMMA denture base materials. J. Prosth.: Implant, Esth. Reconstr. Dent. 2012;21(3):173–176. doi: 10.1111/j.1532-849X.2011.00804.x. [DOI] [PubMed] [Google Scholar]
- Uzun G. Effect of five woven fiber reinforcements on the impact and transverse strength of a denture base resin. J. Prosth. Dent. 1999;81(5):616–620. doi: 10.1016/s0022-3913(99)70218-0. [DOI] [PubMed] [Google Scholar]
- Vallittu P., Kokkonen K. Deflection fatigue of cobalt-chromium, titanium, and gold alloy cast alloy cast denture clasp. Int. J. Fatigue. 1997;3(19):265–266. doi: 10.1016/s0022-3913(05)80384-1. [DOI] [PubMed] [Google Scholar]
- Vallittu P.K. Glass fiber reinforcement in repaired acrylic resin removable dentures: preliminary results of a clinical study. Quint. Int. 1997;28(1) [PubMed] [Google Scholar]
- Van Noort R., Barbour M. Elsevier Health Sciences; 2014. Introduction to Dental Materials. [Google Scholar]
- Vuorinen A.-M. Effect of rigid rod polymer filler on mechanical properties of poly-methyl methacrylate denture base material. Dent. Mater. 2008;24(5):708–713. doi: 10.1016/j.dental.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Wilfong D.L. Effects of sorbed caprolactam on the crystallinity, morphology, and deformation behavior of polyetheretherketone and poly (phenylene sulfide) Polym. Compos. 1989;10(2):92–97. [Google Scholar]
- Young B.C. University of Glasgow; 2010. A Comparison of Polymeric Denture Base Materials. [Google Scholar]